Baghdad College of Medicine / 4
th
grade
Student’s Name :
Dr. Mohammed Basil
Lec. 6
Neuropathic Bladder
Disorder
Tues. 26 / 4 / 2016
DONE BY : Ali Kareem
مكتب اشور لالستنساخ
2015 – 2016

Neuropathic Bladder Disorder Dr. Mohammed Basil
26-4-2016
2
©Ali Kareem 2015-2016
Neuropathic Bladder Disorder
ANATOMY & PHYSIOLOGY
The Bladder Unit
The functional features of the bladder include
1. A normal capacity of 400–500 mL,
2. A sensation of fullness,
3. The ability to accommodate various volumes without a change in
intraluminal pressure,
4. The ability to initiate and sustain a contraction until the bladder is empty.
5. Voluntary initiation or inhibition of voiding despite the involuntary
nature of the organ.
The Sphincteric Unit
In both males and females, there are 2 sphincteric elements:
1. An internal involuntary smooth-muscle sphincter at the bladder neck.
2. An external voluntary striated-muscle sphincter from the prostate to the
membranous urethra in males and at the mid urethra in females.
The uretrovesical junction
The function of the ureterovesical junction is to prevent backflow of urine from
the bladder to the upper urinary tract. Longitudinal muscle from the ureter
contributes to the makeup of the trigone. Stretching of the trigone has an
occlusive effect on the ureteral openings.
Nerve supply
o The lower urinary tract receives afferent and efferent innervation from
both the autonomic and somatic nervous systems.
o The parasympathetic innervation originates in the second to fourth sacral
segments. The cholinergic postganglionic fibers supply both the bladder
and smooth-muscle sphincter.
Neuropathic Bladder Disorder Dr. Mohammed Basil
26-4-2016
3
©Ali Kareem 2015-2016
o The sympathetic nerves originate at T10–L2. The noradrenergic
postganglionic fibers innervate the smooth muscles of the bladder base,
internal sphincter, and proximal urethra.
o Somatic motor innervation originates in S2–3 and travels to the striated
urethral sphincter via the pudendal nerve. Some motor neurons to the
tonic small muscle fibers of the striated sphincter may also project
through the pelvic nerve .
o There are both somatic and visceral afferents from the bladder and
urethra. The somatic afferent is carried by the pudendal nerve, while the
visceral afferent projects through the sympathetic and parasympathetic
nerves to their respective spinal areas.
The Micturition Reflex
o Intact reflex pathways via the spinal cord and the pons are required for
normal micturition. Afferents from the bladder are essential for the
activation of the sacral center, which then causes detrusor contraction,
bladder neck opening, and sphincteric relaxation.
o The pontine center, through its connection with the sacral center, may
send either excitatory or inhibitory impulses to regulate the micturition
reflex.
Cerebral (Suprapontine) Control
o Although micturition and urine storage are primarily functions of the
autonomic nervous system, these are under voluntary control from
suprapontine cerebral centers, so that other groups of muscles (arm, leg,
hand, bulbocavernosus) can be integrated to assist in urination at the
appropriate time and place.
o
Cerebral lesions (eg, from tumor,Parkinson’s disease, vascular accident)
are known to affect the perception of bladder sensation and result in
voiding dysfunction.
Neuropathic Bladder Disorder Dr. Mohammed Basil
26-4-2016
4
©Ali Kareem 2015-2016
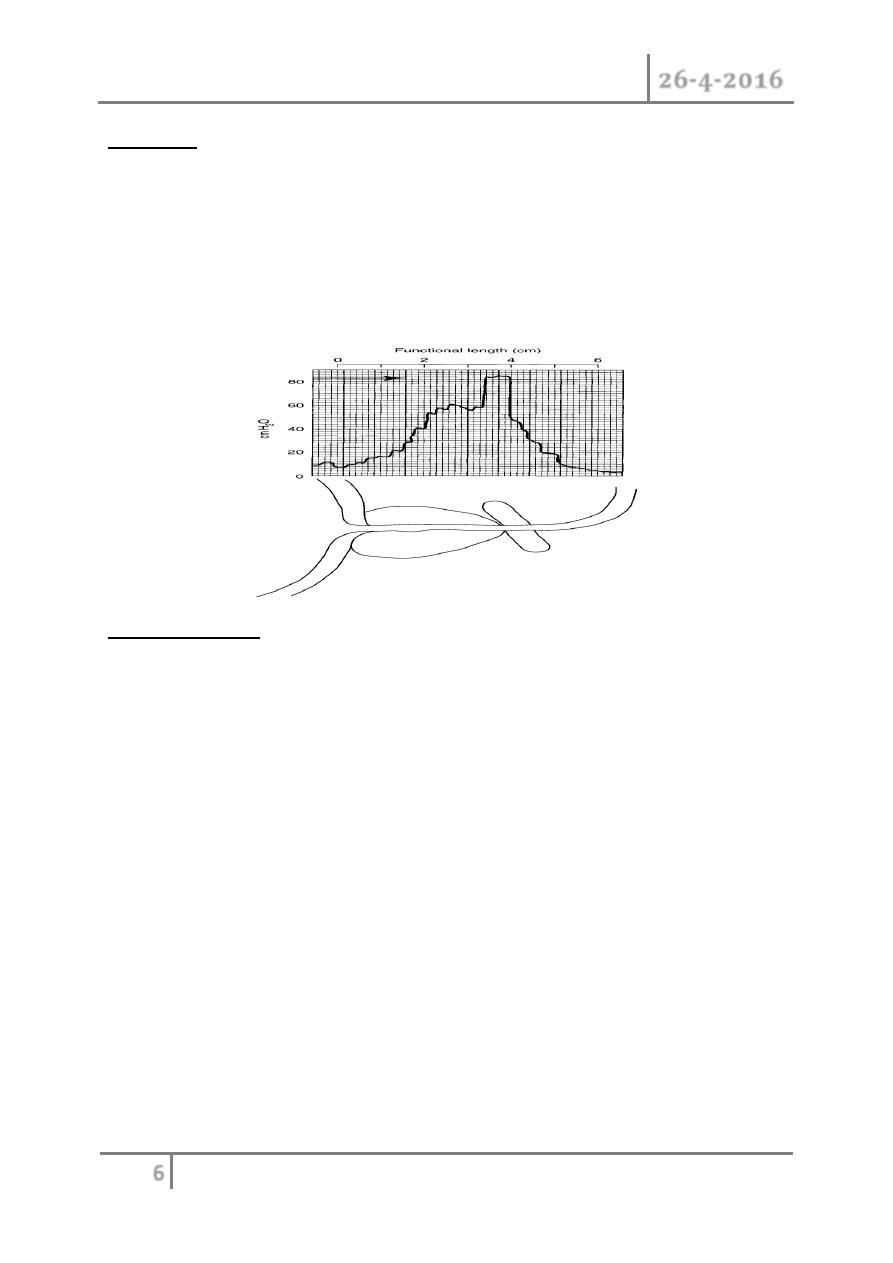
URODYNAMIC STUDIES
Urodynamic studies are techniques used to obtain
graphic recordings of activity in the urinary bladder,
urethral sphincter, and pelvic musculature.
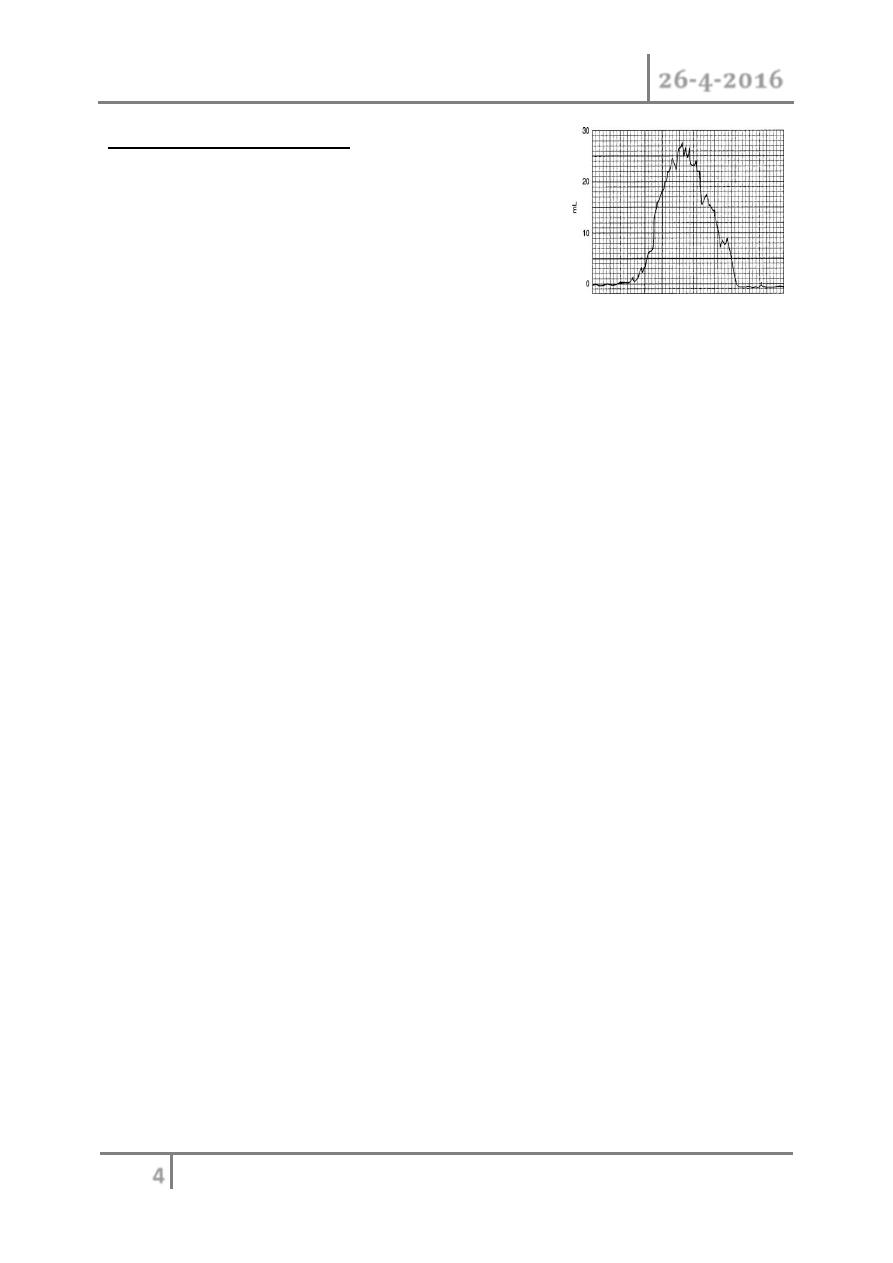
Figure . Classic normal flow rate,
Uroflowmetry
o Uroflowmetry is the study of the flow of urine from the urethra.
o BECAUSE URINARY FLOW RATE IS THE PRODUCT OF DETROSAL
ACTION AGAINST OUTLET RESISTANCE variation from the normal
flow rate might reflect dysfunction .
o The normal peak flow rate for males is 20–25 mL/s and for females 20–
30 mL/s.
o A flow rate less than 10 ml / sec is definitive evidence of obstruction.
o THE NORMAL UROGRAPH IS BELL SHAPED , IN OBSTRUCTED
PROSTATE WE WILL HAVE INTERUPTTED MULTIPLE BELL
SHAPES.
BLADDER FUNCTION
o The basic factors of normal bladder function are bladder capacity,
accommodation, sensation, contractility, voluntary control, and
response to drugs. All of them can be evaluated by cystometry. If all
are within the normal range, bladder physiology can be assumed to be
normal.
o Cystometry can be done by either of 2 basic methods:
1. Allowing physiologic filling of the bladder with secreted urine and
continuously recording the intravesical pressure throughout a
voiding cycle (starting the recording when the patient’s bladder is
empty and continuing it until the bladder has been filled—at which
time the patient is asked to urinate—and voiding begins) or
2. by filling the bladder with water and recording the intravesical
pressure against the volume of water introduced into the bladder.
Neuropathic Bladder Disorder Dr. Mohammed Basil
26-4-2016
5
©Ali Kareem 2015-2016
o The cystometrogram is obtained during the phase of bladder filling;
the volume of fluid in the bladder is plotted against the intravesical
pressure to show bladder wall compliance to filling.
SPHINCTERIC FUNCTION
o Urinary sphincteric function can be evaluated either by recording the
electromyographic activity of the voluntary component of the
sphincteric mechanism or by recording the activity of both smooth and
voluntary components by measuring the intraurethral pressure of the
sphincteric unit. The latter method is called pressure profile
measurement (profilometry).
CLASSIFICATION OF NEUROPATHIC BLADDER
1. Spastic Neuropathic Bladder(Neuropathic Bladder Due to Lesions
Above the Sacral Micturition Center)
Most lesions above the level of the cord where the micturition center is located
will cause bladder spasticity. Sacral reflex arcs remain intact, but loss of
inhibition from higher centers results in spastic bladder and sphincter behavior
on the segmental level.
The sphincter will behave according to the level of lesion as one of the
following three :
1. Normal sphincter pressure - the pt. have frequency
2. High intraurethral (sphincter)pressure - will have retention
3. Low sphincter pressure - incontinence
2. SPASTIC NEUROPATHIC BLADDER RESULT FROM PARTIAL
OR EXTENSIVE NEURAL DAMAGE ABOVE THE CONUS
MEDULARIS (T12)
Common lesion includes dementia ,vascular accidents , multiple sclerosis
,tumurs,and inflammatory disorder such as encephalitis or menengitis .
Neuropathic Bladder Disorder Dr. Mohammed Basil
26-4-2016
6
©Ali Kareem 2015-2016
Features :
(1) Reduced capacity,
(2) Involuntary detrusor contractions,
(3) High intravesical voiding pressures,
(4) Markedhypertrophy of the bladder wall,
(5) Spasticity of the pelvic striated muscle.
(6) Autonomic dysreflexia in cervical cord lesions.
Clinical Findings
SYMPTOMS
o The severity of symptoms depends on the site and extent of the lesion
as well as the length of time from injury.
o Symptoms include involuntary urination, which is often frequent,
spontaneous, scant, and triggered by spasms in the lower extremities
also urge incontinence
o The major nonurologic symptoms are those of spastic paralysis and
objective sensory deficits.
SIGNS
o A complete neurologic examination is most important.The sensory level
of the injury needs to be established, followed by assessment of the anal,
bulbocavernosal, knee, ankle, and toe reflexes. These reflexes vary in
degree of Hyperreflexia With high thoracic and cervical lesions,
distention of the bladder (due to a plugged catheter or during cystometry
or cystoscopy) can trigger a series of responses, including hypertension,
bradycardia, headache, piloerection, and sweating. This phenomenon is
Neuropathic Bladder Disorder Dr. Mohammed Basil
26-4-2016
7
©Ali Kareem 2015-2016
known as autonomic dysreflexia. Bladder volumes in established lesions
are usually less than 300 mL (not infrequently, <150 mL) and cannot be
detected by abdominal percussion.
LABORATORY FINDINGS
o Virtually all patients experience one or more urinary tract infections
during the recovery phase of spinal shock.
X-RAY FINDINGS
o Periodic excretory urograms and retrograde cystograms are essential
because complications are common. A trabeculated bladder of small
capacity is typical of this type of neuropathic dysfunction. The bladder
neck may be dilated.
o The kidneys may show evidence of pyelonephritic scarring,
hydronephrosis, or stone disease. The ureters may be dilated from
obstruction or reflux.
CYSTOSCOPY & PANDOSCOPY
o Bladder capacity, stones, competency of the ureteral orifices, changes
secondary to chronic infection or indwelling catheters, and the integrity
of the bladder neck and external urethral sphincter can be assessed.
URODYNAMIC STUDIES
o Combined recording of bladder and urethral sphincter activity during
filling will reveal a low-volume bladder with spastic dyssynergy of the
external sphincter (Figure 27–4).
o High voiding pressures in the bladder are not unusual. Ureteral reflux or
obstruction is more likely if voiding pressures exceed 40 cm of water.
3. Flaccid (Atonic) Bladder
o Direct injury to the peripheral innervation of the bladder or sacral
cord segments S2–4 results in flaccid paralysis of the urinary
bladder. Characteristically, the capacity is large, intravesical
pressure low, and involuntary contractions absent. Because smooth
muscle is intrinsically active, fine trabeculations in the bladder
may be seen. Common causes of this type of bladder behavior are
Neuropathic Bladder Disorder Dr. Mohammed Basil
26-4-2016
8
©Ali Kareem 2015-2016
trauma, tumors, tabes dorsalis, and congenital anomalies (eg,
spina bifida, meningomyelocele).
Clinical Findings
SYMPTOMS
o The patient experiences flaccid paralysis and loss of
sensationaffecting the muscles and dermatomes below the level of
injury. The principal urinary symptom is retention with overflow
incontinence. Male patients lose their erections.
SIGNS
o Neurologic changes are typically lower motor neuron.Extremity
reflexes are hypoactive or absent. Sensation is diminished or
absent.a palpable bladder might be felt
LABORATORY FINDINGS
o Repeated urinalysis at regular intervals is no less important in this
group than in others. Infection with white blood cells (leukocytes)
and bacteria may occur because of the need for bladder
catheterization.
X-RAY FINDINGS
o A plain film of the abdomen may reveal fracture of the lumbar
spine or extensive spina bifida. Calcific shadows compatible with
urinary stone may be seen. Excretory urograms should be
performed initially to check for calculus, hydronephrosis,
pyelonephritic scarring, or ureteral obstruction secondary to an
overdistended bladder.
o A cystogram may detect morphologic changes in the detrusor (it is
usually large and smooth walled)
INSTRUMENTAL EXAMINATION
o Cystoscopy and urethroscopy performed some months or weeks
after the injury will confirm the laxity and areflexia of the sphincter
Neuropathic Bladder Disorder Dr. Mohammed Basil
26-4-2016
9
©Ali Kareem 2015-2016
and pelvic floor; the bladder neck is usually funneled and open and
the bladder should be large and smooth walled.
URODYNAMIC STUDIES
o The urethral pressure profile reflects low smooth and striated
sphincter tone. Bladder filling pressures are low;
o Detrusor contractions are weak or absent; voiding is accomplished
by straining or by the Crede maneuver, if at all; and there is a
large volume of residual urine.
o Crede maneuver : appling sustaned pressure over the bladder
DIFFERENTIAL DIAGNOSIS OF NEUROPATHIC BLADDER
o Cystitis
o Chronic urethritis
o Vesical irritation secondary to psychic disturbance
o Myogenic damage
o Interstitial cystitis
o Cystocele and
o Infravesical obstruction
TREATMENT OF NEUROPATHIC BLADDER
The treatment of any form of neuropathic bladder is guided by the need to
restore low-pressure activity to the bladder. In doing so, renal function is
preserved, continence restored, and infection more readily controlled.
We are always afraid from the effect on the upper U. tract so the spastic
bladder is more serious .
1. Spinal Shock
o Intermittent catheterization using strict aseptic technique has proved to
be the best form of management of bladder rehabilatation. This avoids
urinary tract infection as well as the complications of an indwelling
catheter (eg, urethral stricture, abscess, erosions, stones).
Neuropathic Bladder Disorder Dr. Mohammed Basil
26-4-2016
10
©Ali Kareem 2015-2016
o If a Foley catheter becomes necessary, a few principles need to be
followed. The catheter should not be larger than 16F and preferably
should be made of silicon, and it should be taped to the abdomen.
o Some urologists advocate the use of suprapubic cystostomy rather than a
urethral catheter to avoid the risks associated with permanent indwelling
catheters.
o A cystogram is needed to rule out reflux ,The urodynamic study should
be repeated every 3 months as long as spasticity is improvingand then
annually to check for complications of the upper urinary tract.
o To control infection, a fluid intake of at least 2–3 L/ day should be
maintained (100–200 mL/h) if at all possible.
o Renal and ureteral drainage are enhanced by moving the patient
frequently, with ambulation in a wheelchair as soon as possible, and even
by raising the head of the bed. These measures improve ureteral
transport of urine, reduce stasis, and lower the risk of infection.
o Additional measures aid in prophylaxis for calculus formation (eg,
reduction of intake of calcium and oxalate and elimination of vitamin D
in the diet).
Spastic Neuropathic Bladder
A. PATIENT WITH REASONABLE BLADDER CAPACITY
o To consider a bladder rehabilitated to a functional state, a patient should
be able to go 2–3 hours between voiding and not be incontinent during
this interval.
o Voiding is initiated using trigger techniques—tapping the abdomen
suprapubically , tugging on the pubic hair, squeezing the penis, or
scratching the skin of the lower abdomen, genitalia, or thighs. They may
be helped by low dose anticholinergic medication (to decrease intravesicl
pressure)or by neural stimulation.
Neuropathic Bladder Disorder Dr. Mohammed Basil
26-4-2016
11
©Ali Kareem 2015-2016
B. PATIENT WITH MARKEDLY DIMINISHED FUNCTIONAL VESICAL
CAPACITY
o If the functional capacity of the bladder is under 100 mL, involuntary
voiding can occur as often as every 15 minutes.
o Satisfactory training of the bladder cannot be achieved, and alternative
measures must be taken
One of the following treatment regimens can then be administered:
1. A permanent indwelling catheter with or without anticholinergic
medication.
2. A condom catheter and a leg bag in males if residual urine volumes are
small and the patient does not have bladder pressures above 40 cm of
water on urodynamic evaluation.
3. Performance of a sphincterotomy in males. It is incontinence
4. Conversion of the spastic bladder to a flaccid bladder through sacral
rhizotomy. Retention
5. Neurostimulation of sacral nerve roots to accomplish bladder evaluation
6. Urinary diversion for irreversible, progressive upper urinary tract
deterioration. A variety of procedures are available, including the
standard ileal conduit, cutaneous ureterostomies,
transureteroureterostomy.
C. PARASYMPATHOLYTIC DRUGS
o Commonly used
drugs and dosages are as follows: oxybutynin chloride
(Ditropan), 5 mg 2–3 times daily; Ditropan XL, once
daily; dicyclomine
hydrochloride (Bentyl), 80 mg in 4
equally divided doses daily
D. BOTULINUM-A TOXIN
o Several centers have investigated injection of 85–300 Units
of botulinum-
A toxin into 30–40 sites in the detrusor
muscle in both children and
adults who have detrusor
hyperreflexia.
E. INTRAVESICAL INSTILLATION OF
CAPSAICIN OR
RESINIFERATOXIN
Neuropathic Bladder Disorder Dr. Mohammed Basil
26-4-2016
12
©Ali Kareem 2015-2016
o Capsaicin and resiniferatoxin are specific C-fiber afferent
neurotoxins.
After spinal cord injury, C-fiber afferents proliferate
proliferate
in the
bladder mucosa and are involved in detrusor
hyperreflexia.
F. NEUROSTIMULATION (BLADDER PACEMAKER)
o Neuroprosthetics are becoming an established alternative
to managing
selective neuropathic bladder disorders.
o Patients are evaluated for a bladder pacemaker primarily by
urodynamic
monitoring of bladder and sphincter responses
to trial stimulation of the
various sacral nerve roots.
o Sacral nerve stimulation(SNS) by the interstim procedure is performed in
two stages :stage one , a clinical trial of
temporary or permanent lead for
external stimulation and stage two , implantation of a subcutaneous
implantation plus generator (IPG)
لالطالع
3 . Flaccid Neuropathic Bladder
o If the neurologic lesion completely destroys the micturition center,
volitional voiding cannot be accomplished without manual suprapubic
pressure, that is, the Crede maneuver. Bladder evacuation can be
accomplished by straining, using the abdominal and diaphragmatic
muscles to raise intra-abdominal pressures.
A. BLADDER TRAINING AND CARE
o In partial lower motor neuron injury, voiding should be tried every 2
hours by the clock to avoid embarrassing leakage. This helps protect the
bladder from over distention due to a buildup of residual urine.
B. INTERMITTENT CATHETERIZATION
o Any patient with adequate bladder capacity can benefit from regular
intermittent catheter drainage every 3–6 hours. This technique eliminates
residual urine, helps prevent infection, avoids incontinence, and protects
against damage to the upper urinary tract. It simulates normal voiding
and is easily learned and adapted by patients.
Neuropathic Bladder Disorder Dr. Mohammed Basil
26-4-2016
13
©Ali Kareem 2015-2016
C. SURGERY
o Transurethral resection is indicated for hypertrophy of the bladder neck
or an enlarged prostate, either of which may cause obstruction of the
bladder outlet and retention of residual urine.
D. PARASYMPATHOMIMETIC DRUGS
o The stable derivatives of acetylcholine are at times of value in assisting
the evacuation of the bladder. Although they do not initiate or effect
bladder contraction, they do provide increased bladder tonus. They may
be helpful in symptomatic treatment of the milder types of flaccid
neuropathic bladder
o Bethanechol chloride is the drug of choice. It is given orally, 25–50 mg
every 6–8 hours.
COMPLICATIONS OF NEUROPATHIC BLADDER
1.Infection
o Infection is virtually inevitable with the neuropathic bladderSterile
intermittent catheterization is recommended at thisstage. Episodic renal
infection should be treated aggressively with appropriate antibiotics to
prevent renal loss. The source and cause of infection should be
eliminated if possible.
2.Hydronephrosis
o Two mechanisms lead to back pressure on the kidney. Early, the effect of
trigonal stretch secondary to residual urine and detrusor hypertonicity
becomes compounded by evolving trigonal hypertrophy. When ureteral
reflux is detected by cystography, previous methods of bladder care must
be radically adjusted. An indwelling catheter may manage the problem
temporarily.
o However, if the reflux persists after a reasonable period of drainage,
antireflux surgery must be considered.

Neuropathic Bladder Disorder Dr. Mohammed Basil
26-4-2016
14
©Ali Kareem 2015-2016
3. Calculus
o A number of factors contribute to stone formation in the bladder and
kidneys. Bed rest and inactivity cause demineralization of the skeleton,
mobilization of calcium, and subsequent hypercalciuria. Recumbency and
inadequate fluid intake both contribute to urinary stasis, possibly with
increased concentration of urinary calcium. Catheterization of the
neurogenic bladder may introduce bacteria. Subsequent infection is
usually due to a urea-splitting organism, which causes the urine to
become alkaline, with reduced solubility of calcium and phosphate.
END OF THIS LECTURE …
