Embryology and Anatomy
GIT develops at 4th week of gestation- it derived from the endoderm and divided into three segments: foregut, midgut, and hindgut.
-Both midgut and hindgut contribute to the colon, rectum, and anus
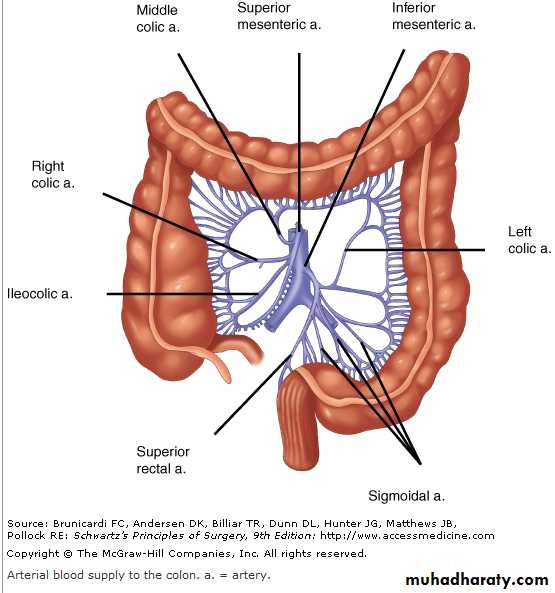
-The midgut develops into the small intestine, ascending colon, and proximal transverse colon, and receives blood supply from the superior mesenteric artery
The hindgut develops into
1- the distal transverse colon2- descending colon
3- rectum
4- proximal anus
all of which receive their blood supply from the inferior mesenteric artery
Anatomy
-The large intestine extends from the ileocecal valve to the anus.- It is divided anatomically and functionally into the colon, rectum, and anal canal.
- The wall of the colon and rectum consist of 4-layers:
1- mucosa
2- submucosa
3- muscular layer
- inner circular
- outer longitudinal muscle, the outer longitudinal muscle is separated into three teniae coli except at rectum and appendix is circumferential
4-serosa.
The intraperitoneal colon and proximal one third of the rectum are covered by serosa;
- the middle and lower rectum lack serosa.
Anatomy
-The large intestine extends from the ileocecal valve to the anus.
- It is divided anatomically and functionally into the colon, rectum, and anal canal.
- The wall of the colon and rectum consist of 4-layers:
1- mucosa
2- submucosa
3- muscular layer
- inner circular
- outer longitudinal muscle, the outer longitudinal muscle is separated into three teniae coli except at rectum and appendix is circumferential
4-serosa.
The intraperitoneal colon and proximal one third of the rectum are covered by serosa;
- the middle and lower rectum lack serosa.
Colon Nerve Supply
The colon is innervated by both sympathetic (inhibitory) and parasympathetic (stimulatory) nerves, which parallel to the course of the arteries.
- Sympathetic nerves arise from T6-T12 and L1-L3.
- The parasympathetic innervations to the right and transverse colon is from the vagus nerve
- the parasympathetic nerves to the left colon arise from sacral nerves S2-S4 to form the nervi erigentes.
The rectum
- Rectum start at rectosigmoid junction , which is at the level of the sacral promontory and at this point the three teniae coli of the colon coalesce to form the outer longitudinal smooth muscle of rectum
-The rectum is approximately 12 to 15 cm in length.
-Three distinct submucosal folds, the Houston`s valves extend into the rectal lumen , the upper and lower convex to right and middle convex to left
- the rectum is divided to three part
1-upper third covered anteriorly and laterally by peritoneum
2- middle third covered only anteriorly by peritoneum
3- lower third is exteraperitoneal
The lower part of the rectum separated from surrounding organ by fascia
Posteriorly
- At lower two sacrum and coccyx rectosacral fascia ( Waldeyer's fascia) is dense fascia is between the rectum and sacrum it separate the rectum from presacral venous plexus and pelvic nerves, and act as barrier for spread of tumor
anteriorly
Denonvilliers' fascia separates the rectum from the prostate and seminal vesicles in men and from the vagina in women
Laterally
- The lateral ligaments from rectum to lateral wall of pelvis , it support the lower rectum
Anorectal Vascular Supply
1-The superior rectal artery arises from the terminal branch of the inferior mesenteric artery and supplies the upper rectum.
2-The middle rectal artery arises from the internal iliac artery
3-The inferior rectal artery arises from the internal pudendal artery, which is a branch of the internal iliac artery.
A rich network of collaterals between these arteries
The venous drainage of the rectum parallels the arterial supply.
1-The superior rectal vein drains into the portal system via the inferior mesenteric vein.
2-The middle rectal vein drains into the internal iliac vein.
3-The inferior rectal vein drains into the internal pudendal vein, and subsequently into the internal iliac vein.
A submucosal plexus deep to Morgagni columns forms the hemorrhoidal plexus and Anorectum drains into all three veins
2/26/2014
2/26/201413
13
anal and rectal examination
Position:
- the left-lateral (Sims) position
- the knee-elbow position
- the lithotomy position:
a- left lateral position
b- elbow- knee position
Inspection:-
- With the buttocks opened, the anus is inspected. Note is made of any lesions,
e.g. inflammatory skin changes,
hemorrhoids,
fissure ('sentinel pile),
fistula
mass , tumor
Digital examination
with the index finger, to palpate for
Intraluminal-
- abnormal: polyp or carcinoma
- normal: sphincter muscles and anorectal angle
Intramural-
- abnormal: leiomyoma or carcinoma
- Extramural,
for prostate any abnormal mass at Douglas pouch
Digital examination
Digital examination
investigation
-Proctoscopy- regid sigmoidoscope
-Fexible sigmodoscope
- endoscopic ultrasound
- ultra sound of pelvis
- Ct-scan, MRI
- anorectal manometry,
defecography -
Symptoms:
1-Bleeding: This demands at least digital examination at any age.
2- Altered bowel habit: constipation ,or diarrhea
Early morning stool frequency ('spurious diarrhea') is a symptom of rectal carcinoma, while blood-stained frequent loose stools characteristic of the inflammatory diseases.
3-Discharge: Mucus and pus are associated with rectal pathology.
4-Tenesmus: desire to pass stool but there is noting
often described by the patient as '1 feel I want to go but nothing happens'; this is normally an ominous symptom of rectal cancer.
5-Prolapse: protrusion of rectum through anal orifice This usually indicates either mucosal (partial) or full thickness (complete) rectal wall descent.
6-Pruritis: This may be secondary to a rectal discharge.
7-Loss of weight: This usually indicates serious or advanced disease, e.g. metastases
Rectal injury
Causes:.1- falling in a sitting posture on to a spiked or blunt pointed object it also cause anal injury.
2-due to complication of labor. the fetal head during childbirth, especially forceps-assisted cause perineal tear which extend to the rectum
3-During the administration of an enema by a syringe.
4- by rigid sigmoidoscopy, usually when examining a patient suffering from ulcerative proctocolitis or amoebic dysentery.
- perforation is usually anteriorly through the rectosigmoid junctional zone.
5- Split perineum’. A lacerated wound of the perineum, involving the anal canal, is an occasional pillion-riding accident,
6-Compressed-air rupture (as a result of joke).
7-Insertion of a foreign body
Treatment
- good clinical examination.
- investigation such as proctoscope, sigmoidoscope if possible ,ultra-sound and ct-scan
A-If there is intraperitorteal rupture of the rectum
1- laparotomy
2- perforation is closed with sutures
3- defunctioning colostomy is constructed in the left iliac fossa.
4- antibiotic
B- If the rectal injury is below the pelvic floor, extraperitoneal
1- do wide drainage from below (pre-sacral drainage)
2- protective colostomy is advisable some time.
3-Care must be taken to preserve sphincter function during the debridement of the perineal wounds.
4-antibiotic cover
Rectal Prolapse
Rectal prolapse: protrusion of the rectum outside the anus.Types:
Partial prolapse: The mucous membrane and submucosa of the rectum protrude outside the anus for approximately 1-4 cm.
Complete prolapse: full thickness of the rectum protrudes outside the anus.
Aetiology
Partial prolapse
The condition occurs most often at the extremes of life.
A--In children it is common between 1 and 3 years of age and is probably result of combination of factors
1-undeveloped sacral curve ,the anus and rectum forming vertical tube.
2-straining
- at defecation due to prolonged diarrhea
- at severe cough in case of whooping cough
3- loss of weight.
which result in loss of supporting pararectal and ischiorectal fat
.
B-In elderly people it due to
1-usually associated with third-degree haemorrhoids
2-in the male, straining in case of urethral stricture
3- atony of sphincter mechanism
4- due to injury of anal sphincter in case of operation for fistula in ano or perineal tear in labor
clinical feature
Symptom
1- protrusion of the mucosa of the rectum on straining
it reduce spontaneously or digitally
In partial prolapse the protrusion is less than 5-cm but in complete is more
2- mucous discharge
3- fecal incontinence
4- feature of complication of irreducibility such as ulceration, gangrene
By the examination of partial prolapse between the thumb and finger ,you feel no more than two layers of the mucosa.
but in case of complete prolapse you feel much more thicker tissue which is two layers of the rectal wall
Differential diagnosis
- prolapsed hemorrhoid
- prolapsed polyp
- prolapsed intussusceptions
Treatment of partial collapse
In children
1-avoidence of constipation and straining
2-improve nutritional status
3-manual reduction of prolapse and strapping the buttock
4-sub mucosal injection of 5% phenol in almond oil for resistance cases
5- surgery rarely indicated (Thiersch`s operation)
In adults:
-sub mucosal injection of 5% phenol in almond- Excision of the prolapsed mucosa (Goodsall's ligature)
Complete prolapse (syn. procidentia)
- More common in the elderly.- Women are six times more often affected than men.
- Is less common than the partial variety.
- The protrusion consists of all layers of the rectal wall.
- It is more than 4 cm and commonly as much as 10-15 cm in length.
- On palpation between the finger and the thumb, the prolapse feels much thicker than a partial prolapse, and obviously consists of a double thickness of the entire wall of the rectum.
- The prolapsed mucous membrane is often arranged in a series of circular folds.
- The anal sphincter is characteristically patulous.
the real pathophsiology is not well known but there is multiple theory
1-failure of rectal support by elevators and pelvic fascia due to defective collagen maturation in the pelvic floor
2- rectal prolapse may be represent a sliding hernia
3-abnormal mobility of the mesorectum leading to lack of fixation of rectum to the sacrum
4-pelvic floor denervation due to repeated birth
Treatment of complete prolapse
usually need surgery ,there are multiple surgery
1- rectopexy (Well`s operation)
through abdominal approach, the rectum mobilized and pulled upward, polypropylene mesh or ivalon sponge is attached to presacral fascia then wrapped and sutured around the back and side of the rectum, this form fibrosis and fix the rectum to the sacrum
2- delorme`s operation
through perineal approach
a) The mucosa has been removed from the prolapsed rectum
b) interrupted sutures have been placed in the underlying muscle so that, when tied, the muscle is plicated
3- excision of redundant rectum either through perineal or abdominanal approach
4- thiersch`operation for older and tired patient
it is narrowing of the anus by the non-absorbable suture is tunneled subcutaneously around the anal canal so narrowed anus prevent the rectum from prolapse
Solitary Rectal Ulcer Syndrome
Solitary rectal ulcer syndrome is commonly associated with internal intussusception.
- Patients may complain of pain, bleeding, mucus discharge,.
- In solitary rectal ulcer syndrome, one or more ulcers are present in the distal rectum, usually on the anterior wall.
- Evaluation should include anorectal manometry,
defecography, and either colonoscopy or barium enema to exclude other diagnoses.
- Biopsy of an ulcer or mass is mandatory to exclude malignancy
Treatment
- non-operative therapy is effective in the majority of patients
1- high-fiber diet
2- defecation training to avoid straining
3- and laxatives or enemas.
-Surgery
- either abdominal or perineal repair of prolapse as described above.
- is reserved for highly symptomatic patients and not respond to conservative treatment