Mohannad Al-Fallouji, PhD (London), FRCS, FRCSIUniversity Staff and Consultant SurgeonBaghdad’s Medical City Teaching HospitalsDirector: www.ihams.org
Cervical LNs
1992
19861998
Speaker’s Background
خلفية المحاضر
• I Love You (in Hebrew)
2012 - 2013
Magnum Opus1. To reveal details of Cervical LNs’ Surgical Anatomy.
2. To know the causes of Lymphadenopathy.3. To handle enlarged Supraclavicular LN management.
• How to diagnose the Cervical Lymphadenopathy.• How to treat Tuberculous Lymphadenopathy.
Objectives of Cervical LNs
Cervical Lymph Nodes .
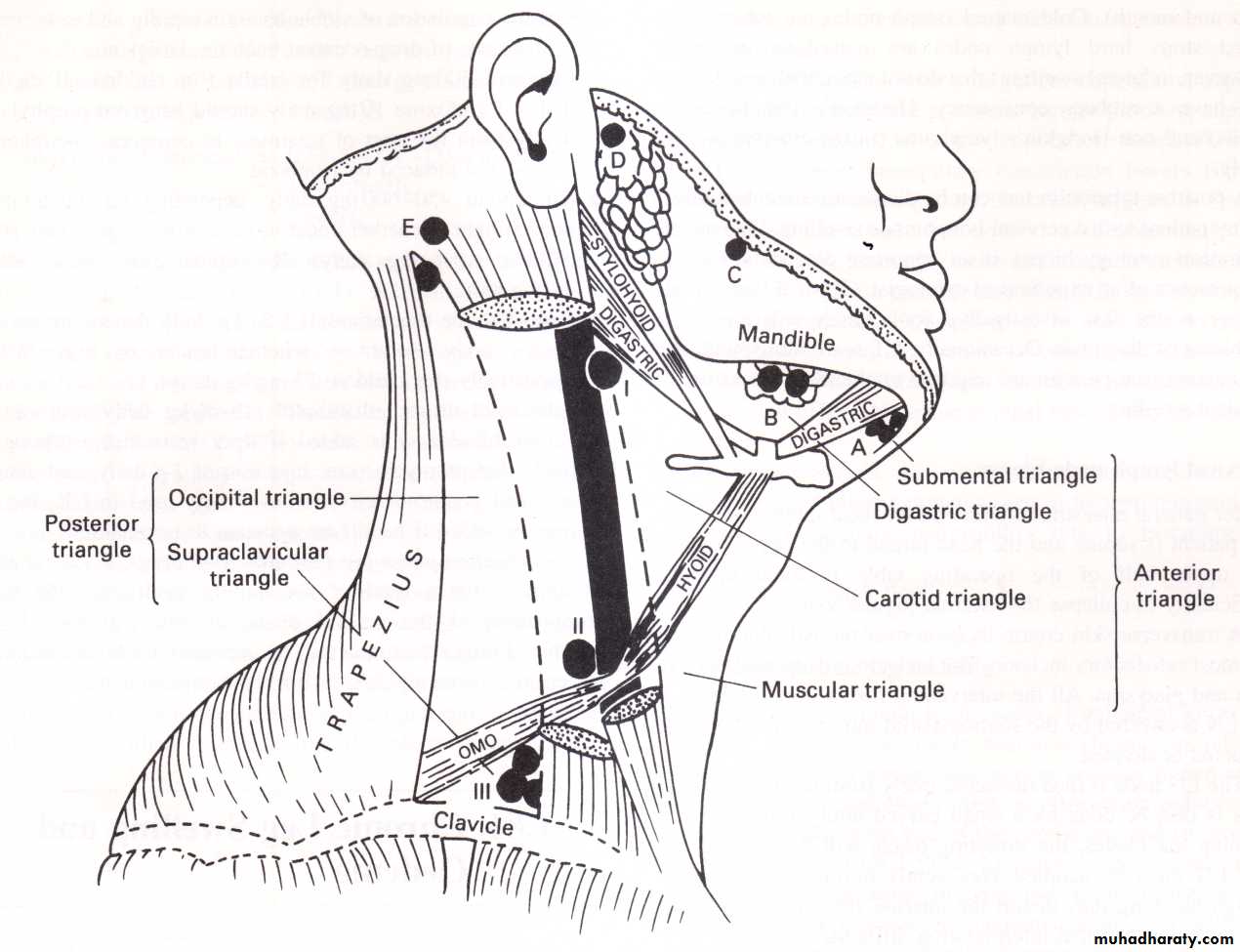
Surgical Anatomy:Cervical Lymph Nodes:
The human body contains about 800 lymph nodes (LN), of
which 300 are located in the neck.About 150 are in the Mesentery.
The lymphatic drainage of the head and neck is arranged
into superficial and deep.The superficial group has 2 'circles‘:
the inner circlethe outer circle.
The Superficial Lymph Nodes comprise following elements.
Outer circle of nodes from chin to occiput is made up of:A: The submental nodes: three or four nodes lie just beneath the chin. They drain the tip of the tongue. floor of the mouth lingual and labial gum. They drain into the submandibular group but a few efferents pass direct to the jugulo-omohyoid node.
B: The submandibular nodes drain a wide area from the centre of the forehead. nose and nearby cheek. upper lip and the anterior two-thirds of the tongue, floor of mouth and gums. They receive lymph from the upper and lower teeth, from the anterior half of the nasal cavity and from the frontal and maxillary and middle and anterior ethmoidal sinuses. Most of the submandibular nodes drain into the jugulo-omohyoid node; a few drain into the jugulo-diagastric node.
C: Buccal and mandibular nodes: a small node lies isolated on the baccinator muscle, another on the lower border of the mandible at the anterior border of the masseter. They drain part of the cheek and lower eyelid. Their efferents pass to the jugulo-digastric node.
The Superficial Lymph Nodes
Outer circle of nodes (continued)D: Pre-auricular nodes: these lie on and within the parotid gland: one or two are subcutaneous. The subcutaneous nodes drain the skin of the temple and vertex. forehead and eyelids. pinna and external acoustic meatus.
These drain through the deep cervical fascia into supraclavicular nodes.
The deep nodes receive from the back of the orbit, from the infratemporal fossa, and from the parotid gland itself.
They drain into the deep members of the deep group.
E. Occipital nodes: these drain the posterior part of the scalp and auricle. The efferents pass to the supraclavicular nodes.
The inner circle lies within the surrounding larynx, trachea, and pharynx.
It comprises pre-tracheal, para-tracheal andretro-pharyngeal LNs.
The pre-tracheal LNs drain the lower larynx, trachea and thyroid isthmus.
The retro-pharyngeal LNs drain the soft palate, posterior parts of hard palate and nose, as well as the pharynx itself.Tonsils, lingual tonsil, palatine tonsil and adenoids sometimes called inner ring of waldeyer.
These then drain into the Deep Cervical LNs.
Deep Cervical Lymph Nodes:found around the internal jugular vein from the base of the skull to the root of the neck. They are formed of 3 groups:
• The jugulo-digastric node lies below the posterior belly of the digastric between the angle of the mandible and the anterior border of sternomastoid.
• The jugulo-omohyoid node lies above the inferior belly of the omohyoid, behind the jugular vein.
III. The supraclavicular lymph nodes extend behind the border of sternomastoid into the posterior triangle. Lymph from the deep cervical nodes is collected into the jugular lymph trunk.
This joins the thoracic duct on the left side: on the right side, it usually opens independently into the internal jugular or brachiocephalic vein.
Causes of cervical lymphadenopathy
1. Infection• Acute pyogenic (tonsillitis, dental extraction, middle ear infections, parotitis, scalp infections)
• Chronic
• Non-specific (viral infection)
• Specific
• Glandular fever (infectious mononucleosis, EBV infection)
• Tuberculosis
• Syphilis
• Toxoplasmosis
• Cat scratch fever
2. Neoplastic
• Metastatic secondary tumours from primary tumours of :
squamous carcinoma of nasopharynx, skin of head, neck, chest, and abdomen.
• Primary tumours:
• Hodgkin's lymphoma (adult)
• Non-Hodgkin's lymphoma (elderly)
• Leukaemia (usually children and young adults)
3. Miscellaneous Sarcoidosis
Enlarged Supraclavicular Lymph Nodes take the name of the German pathologist Virchow (1821-1902): the classical enlarged supraclavicular LN (of Virchow) following metastasis from underlying gastric carcinoma is termed Troisier's sign (named after a French professor of pathology, 1844-1919).
Enlarged supraclavicular LN is of great surgical interest. since it is usually due to neoplastic lesions more than infective ones (the commonest cause of infective enlargement of supraclavicular lymph nodes is pulmonary tuberculosis).
While most upper limb infection can cause epitrochlear and axillary LN enlargement, infection of the middle finger and dorsum of the hand passes directly into the supraclavicular LNs.
Other causes of enlargement include bronchogenic carcinoma (Pancoast tumor), breast carcinoma, thyroid carcinoma(wrongly called ectopic thyroid), oesophageal carcinoma, pharyngolaryngeal carcinoma, Hodgkin's and non-Hodgkin's lymphoma. pancreatic carcinoma and testicular carcinoma (particularly choriocarcinoma). Hypernephroma can also give rise to enlarged supraclavicular nodes.
Superficial and Deep cervical lymph nodes ultimately drain into supraclavicular lymph nodes. So any enlargement of these glands (due to infections or neoplasms in the head and neck and upper limbs) will result in enlargement of the supraclavicular lymph nodes. Enlargement of supraclavicular may be part of a generalised lymphadenopathy due to leukemia, lymphoma and AIDS.
Careful history and meticulous physical examination can give the diagnosis in the majority of cases. Complete ENT examination of postnasal space, oral cavity, oropharynx and fibreoptic laryngoscopy. Examine other sites (axilla, epitrochlear, inguinal, spleen, and liver).
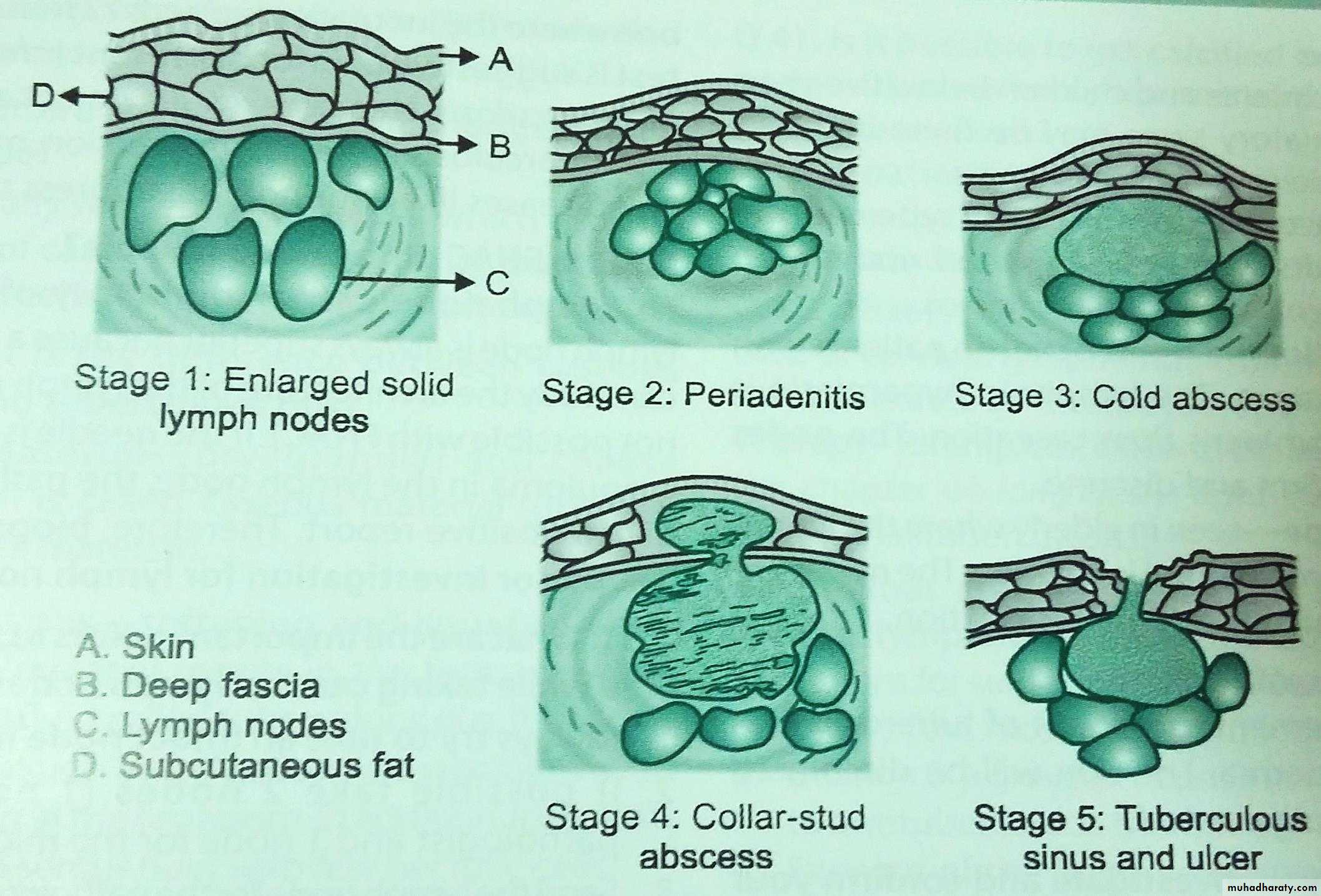
Lymph nodes are tender and hot with evidence of infection (of the respiratory tract and mouth). Cold matted lymph nodes are tuberculous.
Fixed stony-hard lymph nodes are metastatic in origin.
However, in lateral painless swellings that do not move with swallowing and have a rubbery consistency, Hodgkin's lymphoma (in adults) and non-Hodgkin's lymphoma (in the elderly) is most likely.
High ESR, Chest x-ray findings can be confirmed by Positive tuberculin test can be diagnostic for tuberculosis in any patient with a cervical lymph node swelling. Past infection with Eptein-Barr virus plays a role in some Hodgkin’s lymphoma patients.
Fine needle aspiration cytology biopsy is an important diagnostic tool, in the presence of an experienced cytologist.
Cervical lymph node biopsy is the last investigative tool which will solve the problems of diagnosis. CT scan, ultrasound, radioactive isotope scan, and positron emission tomography (PET) may be required to elucidate the nature of cervical swelling, staging, assessment of response, and direction of treatment..
Diagnosis of a Cervical Swelling
(due to Lymph Node enlargement)
Tuberculosis lymphadenitis stages in order
Treatment of tuberculosis: in 2 phases
Initial phase for 2 months. At least 3 drugs are used to reduce the population of viable bacteria rapidly and to prevent the emergence of drug-resistant bacteria.Drugs are: Isoniazid 300 mg daily for adults(for children 10 mg/k daily). Pyridoxine 10mg daily should be given prophylactically from the start of treatment to counteract peripheral neuropathy induced by isoniazid .
Rifampicin 450 mg daily, depending on the adult's body weight whether under or over 50 kg respectively (for children 10 mg/kg daily). Rifampicin may cause liver dysfunction.
Pyrazinamide (bactericidal) 1.5-2 g daily depending on an adult's body weight whether under or over 50 kg respectively(for children 35 mg/kg daily).
Additional drugs: ethambutol (15 mg/kg daily: can cause colour blindness) is added if drug resistance is thought likely. Streptomycin (i.m. injection of 1 g daily; can cause oto- and nephrotoxicity) is now rarely used in UK, but it may be added if bacilli are resistant to isoniazid.
Continuation phase for 4 months. Two drugs, isoniazid and rifampicin(for a total of six months each), are the key components of the second phase of any antituberculosis regimen. Longer treatment may be necessary for bone and joint infections, for meningitis, or for resistant organisms.