1
Professor Nada Al Alwan
THE BREAST
ANATOMY and HISTOLOGY
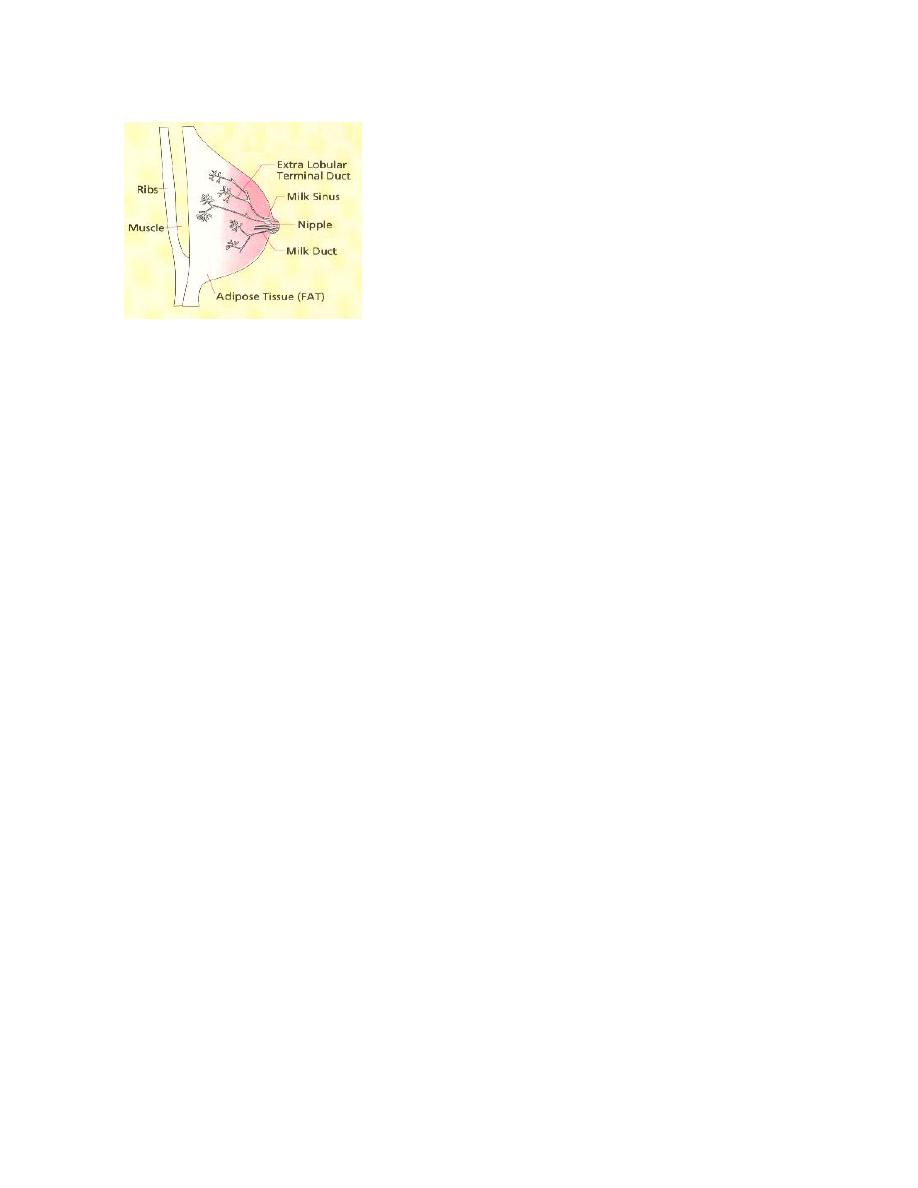
The size and structure of the breast vary with the age, sex, hormonal status and heredity
of the individual. The areola is the circular pigmented area that contains sebaceous
glands. In its center, the elevated nipple is covered by wrinkled skin lined by stratified
squamous epithelium. It contains 15-20 lactiferous ducts (lined by two-layered cuboidal
cell mucosa) which branch successively distally, leading eventually into the terminal
ducts. Before puberty, this complex system ends blindly but at menarche, it proliferates
distally giving rise to 30- epithelium lined ductules or acini. Each terminal duct and its
ductules compose the terminal duct lobular unit. The ductules are covered by cuboidal
and myoepithelial lining cells. In addition to ramifying ducts, the female breast consists
of connective and adipose tissue, although few alveoli may develop and involute
concomitantly with the menstrual cycle. In the male breast, there are only rudimentary
ducts surrounded by connective tissue
The female breast is in the unique position of being a gland which is non-functioning
except during lactation. However, its extreme sensitivity to hormonal influences disposes
it to a number of pathological conditions.
PATHOLOGICAL CLASSIFICATION OF BREAST DISEASES
Inflammatory and Related lesions:
Acute Infections (Pyogenic Mastitis and Breast Abscess)
(Fig. 11-6)
Mastitis, a local or generalized inflammation of the breast, is precipitated by lactation,
trauma or infection through the ducts or nipple abrasions. Usually caused by Staph.
Aureus which may invade the breast tissue and may progress to the formation of single or
multiple abscesses where by the localized collection of pus causes conspicuous
tenderness. Less commonly Strept. Pyogenes may cause cellulites. If extensive necrosis
occurs the destroyed breast substance will be replaced by fibrous scar which may cause
retraction of the overlying skin or nipple, stony hardness and axillary lymphadenopathy;
changes mimicking a malignant neoplasm. Chronic inflammation if neglected may lead
to fistula formation.
Chronic Infections and Granulomatous Inflammations
Granulomas are caused by different infectious agents:

2
Tuberculomas: Involving the breast have been described. Although it is relatively rare,
but it usually arise from hematogenous , lymphatic or direct spread. It presents as a
single caseating lesion which sometimes discharges through the skin
(Fig. 11-7)
.
Sarcoidosis: Reveals similar picture without caseation or acid-fast bacilli.
Fungal infection: Coccidiodomycosis and actinomycosis are associated with necrotizing
granulomas. These are diagnosed by special stains such as PAS or tissue culture.
Idiopathic Granulomatous mastitis
(IGM) (Fig. 11-8)
This rare condition is seen mainly in young women, usually after pregnancy. Patients
present with firm tender mass. It may be complicated by overlying skin ulcerations &
multiple draining sinuses.
Non-Infective Inflammatory Lesions
including:
1.
Mammary Duct Ectasia
(Fig. 11-9)
This disorder tends to affect perimenopausal women usually in the fifth decade of life.
Patients are often multiparus and have lactated, but may have had trouble in nursing due
to inverted nipples. It begins with dilatation of the terminal collecting ducts beneath the
nipple and areola where they become distended with cellular derbies and lipid containing
material. This may be followed by marked periductal and interstitial chronic
granulomatous inflammatory reaction and fibrosis, sometimes associated with a large
number of plasma cells (plasma cell mastitis). Rarely palpable as a “bag of worms”.
Fibrosis may cause skin retraction which may be mistaken for carcinoma. Often
symptomless but there may be nipple discharge. Hyper-prolactinemia has been suggested
to play a role in its pathogenesis. The pathology described above results in firm mass
with adjacent skin dimpling and nipple retraction.
2.
Traumatic Fat Necrosis
(Fig. 11-10)
It often follows trauma and presents clinically as a firm hard mass ( in the fatty tissue of
an obese pendulous breast and sometimes associated with skin retraction. It consists of a
central focus of liquefactive fat necrosis, surrounded by lipid-layden macrophages and
numerous neutrophilic inflammatory infiltration. This is followed by fibroblastic
proliferation, foreign-body giant cell infiltration and ending into scar tissue (which
together with the calcification accounts for the hardness of the lump). Extensive fibrous
reaction may further cause nipple retraction and fixation thus simulating malignancy.
3. Galactocele
This is a cystic dilatation of a duct occurring during lactation and presenting as a tender
mass. It results from obstruction of the lactiferous duct, distention by milk and
desquamated epithelial cells. Secondary obstruction may convert these single and
multiple cysts to foci of acute mastitis or abscesses, or may induce granulomatous
reaction. The aspirated material is usually yellowish-white, creamy fluid, sometimes
curd-like or blood-tinged containing histeocytes, and foamy ductal cells within a
background of abundant protein and lipid deposit.
(Fig. 11-1)

3
4. Fibrocystic Changes or Cystic Mastopathy
This is a pleomorphic disorder in which variable morphological patterns are encountered
in different patients, different areas within the same lesion and even in different
microscopical fields within the same slide. It develops in females between puberty and
menopause and considered the commonest cause for a lump in the breast. Patients usually
present with ill defined tender thickness of the breast tissue, palpable lumps or
physiological nodularity which may vary during the period of the menstrual cycle. It has
been been postulated that those changes are related to imbalance between estrogens and
progestins (with excessive estrogenic stimulation).
Fibrocystic Changes are of clinical significance for 3 reasons:
they may coexist with carcinoma.
They may predispose to the development of carcinoma.
some variants may clinically mimic carcinoma.
In general, it is possible to distinguish 3 dominant patterns of morphological changes:
a) Cystic Formation and Fibrosis (Simple Fibrocystic Changes)
(Fig. 11-2)
This is the most common type of alteration characterized by an increase in fibrous stroma
associated with ductal diltation and formation of cysts of various sizes, probably due to
obstruction. Unopened cysts are brown to blue in colour due to the contained
semitranslucent turbid fluid. Sometimes haemorrhage or rupture leads to secondary
inflammation. Cysts are lined by columnar, cuboidal or flattened epithelium that may be
atrophic in larger ones. The epithelium may consist of large polygonal cells with
abundant granular eosinophilic cytoplasm and small hyperchromatic nuclei (apocrine
metaplasia), which is virtually always benign. In general, the breast should be palpated
again after cystic aspiration and any residual mass should be reaspirated.
b) Epithelial Hyperplasia (Epitheliosis)
(Fig. 11-3)
Hyperplasia affecting mammary ducts and ductules is the histological variant that
increases the risk of subsequent development of malignancy; especially if it is associated
with atypia. May take three main forms: solid, cribriform or papillary.
The degree of hyperplasia can be mild, moderate, or severe. In some instances the
hyperplastic cells show complex architectural patterns and approaching morphologically
those of ductal carcinoma in situ, such hyperplasia is called atypical.
Atypical lobular hyperplasia
(Fig. 11-4)
describes hyperplasias that cytologically
resemble lobular carcinoma in situ, but the cells do not fill or distend more than 50% of
the acini within a lobule.
Atypical lobular hyperplasia is associated with an increased risk of invasive carcinoma.
Epithelial hyperplasia per se does not often produce a clinically discrete breast mass.
Microscopically, proliferation causes increase in the layers of the ductal epithelium ,
sometimes encroaching to completely fill the duct lumen obliterating it (solid) or forming
fenestrations with gland-like spaces (cribriform). Papillary epithelial projections may
grow into the lumen (ductal or florid papillomatosis). The presence of ductal
papillomatosis or moderate-severe atypia increase the risk of malignancy.

4
Atypical ductal or lobular hyperplasia may show various degrees of cellular or
achietectural atypias that should be differentiated from carcinoma in situ.
c) Adenosis and Sclerosing Adenosis
Adenosis:
i.e., enlargement of the lobules and/or formation of new lobules, could be a
physiological process which occurs during pregnancy and reproductive life; however, it
tends to be accentuated in fibrocystic changes.
Sclerosing Adenosis
:
a significant variant of FCC because its clinical and morphologic
features may be deceptively similar to those of carcinoma. Grossly, the lesion has a hard,
rubbery consistency, & thus simulates that of breast cancer. Microscopically, this variant
is characterized histologically by intralobular fibrosis and proliferation of small ductules
or acini which yield small glandular masses or cellular cords within a fibrous stroma
(Fig. 11-5).
Well-defined glands may be closely aggregated and backed to each other
(adenosis). Stromal overgrowth may distort and compress the glands creating solid cords.
Cells from sclerosing adenosis form clusters of up to 30 cells with some nuclear piling
and minimal anisonucleosis. Sclerosing adenosis is associated with only a minimally
increased risk of progression to carcinoma.
The relationship of the various patterns of fibrocystic Changes to Cancer:
Minimal or no increased risk of breast carcinoma: Fibrosis, Cystic changes,
Apocrine metaplasia, Mild hyperplasia & Fibroadenomatosis.
Slightly increased risk (1.5-2 times): Moderate to florid hyperplasia (without
atypia), Ductal papillomatosis & Sclerosing adenosis.
Significantly increased risk (5 times): Atypical hyperplasia, ductular or lobular.
A family history of breast cancer may increase the risk in all categories (e.g., to about
10-fold with atypical hyperplasia).
Benign Tumours:
Fibroadenoma
This is the most common benign tumor of the female breast. It is a new growth composed
of both fibrous and glandular tissue occurring commonly in young women (before the
age of 30), and probably caused by hormonal imbalance. Areas resembling fibroadenoma
sometimes occur in Fibrocystic Changes (Fibroadenomatosis).
Clinically, palpation reveals a dominant discrete, well-circumscribed elastic round or oval
firm mass which resists penetration by the aspiration needle but proves to be mobile
when penetrated. Usually small (2-4 cm.) but may reach 7 cm with a uniform tan-white
color on cut section
(Fig. 11-11 A).
They are usually encapsulated affecting one breast,
and rarely multiple in both breasts.
Microscopically, there are two varieties: the ”intracanalicular” type which encroaches
into and obliterates the ducts with broad, polypoidal branches of loose connective tissue

5
lined by cuboidal ductal cells. The ”pericanalicular” type encircles the ducts, with
dense, concentric mesenchyme.
(Fig. 11-11 B).
The clinical and cytological presentation of both types are identical. Rarely insitu lobular
or ductal carcinoma arise in
fibroadenoma.
Adenomas
These are variants of fibroadenoma with glandular rather than stromal proliferation. It is
a homogenous sharply demarcated epithelial tumour that is composed either of tubules
(tubular adenoma) or dilated alveoli containing secretory foamy material (lactationg
adenoma). Microscopically, the small rounded acini lined by cuboidal or (during
pregnancy) secretory columnar cells are tightly packed with little intervening stroma.
Because of the lack of mesenchyme and the presence of eosinophilic macronucleoli, the
lesion may resemble well-differentiated adenocarcinoma.
Adenoma of the Nipple
This is a benign epithelial tumor arising in one of the ducts of the nipple. It demonstrates
intraductal proliferation which may be papillary, solid or tubular. Occasionally the lesion
may extend through the overlying skin and thus mistaken clinically as malignant.
Intraductal Papilloma
The main secretory ducts are the most common sites of this neoplasm, which is often
associated with hemorrhagic discharge from the nipple. Often solitary and present
clinically as a result of:
Appearance of serrous or bloody nipple discharge.
Presence of small subareolar tumour.
Rarely nipple retraction.
According to WHO definition, duct papilloma is a regular papillary overgrowth without
mitosis or hyperchromatism”. Histologically it is composed of multiple papillae, each
having a connective tissue axis covered by cuboidal or cylindrical epithelium with
myoepithelial cells
(Fig. 11-13)
.
Phyllodes Tumour (Cystosarcoma Phyllodes)
Infrequently fibroadenoma may grow rapidly often to 10 cm. or more in diameter (Giant
Fibroadenoma). Most are benign but few are malignant. On palpation, these are usually
large circumscribed , mobile and some may become lobulated and cystic. Grossly they
exhibit leaf-like clefts or finger-like projections (phyllodes). They may distort the breast
producing pressure necrosis and skin retraction and ulceration. Histologically, these
lesions tend to have a more cellular myxoid stroma than do the usual fibroadenoma.
Features suggesting its aggressive nature include lack of encapsulation, large dimentions,
remarkable nuclear anaplasia, and abnormal mitosis
(Fig. 11-12)
.

6
Malignant Mammary Lesions (Breast Cancer):
Is the commonest type of malignancy among Iraqi women accounting for approximately
one third of the registered female cancers (according to the latest Iraqi Cancer Registry).
Worldwide, most of the data point to three sets of influences that may be important
in increasing the risk for breast cancer: genetic predisposition, hormonal imbalance and
environmental factors.
In general, the recorded
risk factors
for breast cancer include:
Genetic Predisposition and Family History:
Up to 10% of BRCA are related to specific inherited mutations. Women are more likely
to carry a breast cancer susceptibility gene if they have:
a. Premenopausal breast cancer
b. Bilateral cancer
c. Other associated cancers (e.g., ovarian cancer)
d. A significant family history (i.e., multiple relatives affected before menopause)
About 50% of women with hereditary BRCA have mutations in gene BRCA1, and an
additional 30% have mutations in BRCA2. Both BRCA 1 & 2 seem to be involved in
DNA repair and act as tumor suppressor genes. Cancer arises when both alleles are
inactive (defective); one due to a germ-line mutation and the second by a subsequent
somatic mutation. It is possible that other mechanisms, such as methylation of regulatory
regions, act to inactivate the genes in sporadic (nonhereditary) cancer.
Overexpression of the HER2/NEU proto-oncogene has been found to be amplified in up
to 30% of invasive breast cancers Mutations of the well-known tumor suppressor genes
RB and p53 may also be present.
Reproductive Factors and Ovarian Activity:
i- Age at Menarche and Menopause (length of reproductive life)
It has been noted that women who had menarche before twelve years of age and women
with natural menopause at age 55 or older are at increased risk.
ii- Pregnancy
It is well-known that breast cancer is more frequently encountered in nulliparus than in
multiparus women. Several studies reported that the risk is inversely proportional to the
number of children borne.
iii- Lactation
Through its inhibitory activity on ovarian function, lactation has been thought to lower
the risk of breast cancer. Nevertheless, other studies indicated that breast cancer has no
relationship with lactation.
iv- Oopherectomy
It has been reported that bilateral oopherectomy before age 44 may protect against breast
cancer. All the above mentioned factors imply increased risk with increased exposure to
estrogen peaks during the menstrual cycle.

7
Exogenous Hormones
:
Several trials and reports have indicated that women using contraceptive pills or hormone
replacement therapy for a long term might be at increased risk for developing breast
cancer.
Effect of Age:
Breast cancer has been reported in various age groups, but it is more often seen in
patients over fourty years; as the risk increases with age. The risk also increases regularly
with the increase of age at first childbirth.
Geographical Influence:
Breast cancer rates are 5 or 6 times higher in Western Europe and North America than in
Japan and other Asian and African populations; probably attributable to environmental,
nutritional or life style factors .
History of Fibrocystic Changes:
It has been shown that patients who exhibited a remarkable degree of ductal hyperplasia
(florid papillomatosis) had a slightly increased risk (1.5-2 times) of developing
subsequent breast cancer. This risk was increased significantly (5 times) when atypical
hyperplasia (ductal or lobular) was observed .
Multiple Primary Cancers:
It has been found that carcinoma of the contralateral breast increases the risk . Similarly,
it was shown that women with endometrial cancer have a breast carcinoma risk of 1-2
times more than that of the general population . Breast cancers displaying a familial
association with ovarian and colonic cancers have been also reported.
Diet and Nutrition:
It has been proposed that breast cancer is a disease of high socioeconomic status with
good qualify food :
i- Fat Consumption
Epidemiological evidence supported by experimental data strongly suggest that dietary
fats play a vital role in breast cancer pathogenesis. This association may include the
hypothesis that intestinal flora produce estrogens from ingested fat.
ii- Protein Consumption
It has been concluded that women whose diets contained high levels of animal proteins
(including meat, dairy products, bovine milk, high-fat cheese and butter) showed
significantly increased risk.
iii- Effect of Caloric, Vitamin Intake and Acohol Consumption
Caloric restriction inhibited the development of tumors of the mammary glands and other
organs in mice and rats .The protective roles of vitamins A, C and E have been also
suggested. Recent studies demonstrated that the risk is increased with alcohol intake in

8
patients who consumed more than three pints (drinks) per day.
Obesity:
In postmenopausal women, obesity seems to be associated with an increased breast
cancer risk since it has been reported that these women have increased peripheral
conversion of Androstenedione to estrone; the latter being considered as a carcinogenic
agent . Obese patients were also found to have greater chance of early recurrence and
shorter survival than do non-obese patients .
Ionizing radiations:
Studies reported that female survivors of atomic bomb explosions in Japan as well as
patients exposed to high doze of 90 R or more developed breast cancer at a rate 2-4 times
more than that for non-exposed individuals. That was specifically obvious when exposure
targeted adolescent females (immature breasts).
Viruses:
Although still debatable, yet three animal models exist for the viral induction of breast
cancer, namely Mouse Mammary Tumor Virus (MMTV), Mazon Pfizer Monkey Virus
(MPMV), and Rat Mammary Tumor Virus (R-35 Virus. It has been demonstrated that a
filterable agent transmitted through the mother’s milk caused breast cancer in suckling
mice. This MMTV was later identified as retrovirus.
WHO Pathological Classification of Breast Tumours
I.
Epithelial Tumors
:
A. Benign
1. Intraductal papilloma
2. Adenoma of the nipple
3. Adenoma
a. Tublar
b. Lactating
B. Malignant
1. Non-invasive
a. Intraductal carcinoma
b. Lobular carcinoma in situ
2. Invasive
a. Invasive ductal carcinoma
b. Invasive ductal carcinoma with predominant intraductal

9
component
c. Invasive lobular carcinoma
d. Mucinous carcinoma
e. Medulary carcinoma
f. Papillary carcinoma
g. Tubular carcinoma
h. Adenoid cystic carcinoma
i. Secretory (juvenile) carcinoma
j. Apocrine carcinoma
k. Carcinoma withmetaplasia
i. Squamous type
ii. Spindle-cell type
iii. Cartilaginous and osseous type
iv. Mixed type
3. Paget’s disease of the nipple
II.
Mixed Connective Tissue and Epithelial Tumors :
A. Fibroadenoma
B. Phyllodes tumor (cystosarcoma phyllodes)
C. Carcinosarcoma
III.
Miscellaneous Tumors
:
A. Soft tissue tumors
B. Skin tumors
C. Tumors of Haemopoietic and Lymph tissues
IV.
Unclassified Tumors
V.
Mammary Dysplasia
/ Fibrocystic Change
VI.
Tumor-like Lesions :
A. Duct ectasia
B. Inflammatory pseudotumors
C. Hamartoma
D. Gynecomastia

10
Non-Invasive Carcinomas
:
Intraductal Carcinoma
Carcinoma limited to the ducts (Ductal Carcinoma in situ DCIS) is reported in different
age groups with increasing frequency, mainly attributable to the benefits of screening
mammography. It begins with an atypical ductal proliferation which completely fills and
plugs the ducts with neoplastic proliferation. When the breast is sectioned, cord-like ducts
are observed filled with necrotic, cheesy tumour cells which can be extruded upon slight
pressure (comedocarcinoma)
(Fig. 11-15).
. The growth may be (cribroform) indicating
the presence of duct-like structure within the primary dilated ducts, or there may be a
predominant papillary pattern.
In Situ Lobular Carcinoma
It is generally a non-palpable lesion diagnosed by mammography which may be located
adjacent to fibrocystic changes or occurs concomitantly with infiltrative lobular
carcinoma. Histologically, the terminal ducts and/or acini are distended by relatively
uniform cells obliterating the lumens
(Fig. 11-17
). Intracellular mucin vacuoles (signet
ring cells) are common.
.
Invasive Carcinomas:
Invasive Duct Carcinoma – NOS
( Not Otherwise Specified)
This is the most common type exhibiting marked increase in dense fibrous stroma or
desmoplastic response giving the tumour a hard consistency (Scirrhous). This type of
cancer is usually associated with DCIS. The tumor margins are usually irregular
(Fig. 11-
18
). On palpation, this manifests as stony hard nodules, which may have infiltrative
attachments to the chest wall and skin resulting in dimpling and nipple retraction
(Fig.
11-19). .
Histologically, there are anaplastic duct cells arranged in glands, cords or solid
nests. Because of the remarkable fibrosis, aspirates may yield only few cancer cells.
Therefore a tissue biopsy may be recommended to confirm the cytological diagnosis.
Lobular Carcinoma
Probably arises from the terminal ductules of the breast lobule. This type tends to be
bilateral and multicentric . Histologically, the classical type is characterized by small
uniform strands of infiltrating tumour cells often one cell in width ( Indian-file) dispersed
through a fibrous matrix. Neoplastic cells could be arranged in concentric rings around
normal ducts (targetoid).) Occasionally they surround cancerous or normal-appearing
acini or ducts, creating a so-called bull's-eye pattern
(Fig. 11-21
). Because of the
considerable amount of fibrosis, cells may be difficult to aspirate and thus the few
aspirated isolated monomorphic cells may yield a false negative cytology report. In
general these cells exhibit a high nucleocytoplasmic ratio with small cytoplasmic
vacuoles containing a central condensation
of mucus.
Mucinous ( Colloid Carcinoma )
Tends to accur in older patients and often produces large masses which gives the tumour
its soft consistency on palpation. Histologically, there are large lakes of lightly staining
amorphous mucin within which floates small islands of isolated neoplastic cells,

11
sometimes forming glands or cohesive cell clusters exhibiting slight nuclear
abnormalities. A positive mucicarmine stain can confirm the diagnosis.
Medullary Carcinoma
This defined by WHO as a well-circumscribed carcinoma composed of poorly
differentiated cells with scanty stroma and prominant lymphoid infiltration. These
tumours present with fleshy masses more yielding on palpation. A lymphoid component
at the periphery and within the tumour is often present (which gives it its special
significance and better prognosis). Histologically, this carcinoma is characterized by
solid syncytium-like sheets of large cells with vesicular pleomorphic nuclei containing
prominent nucleoli and frequent mitosis.
Papillary Carcinoma
Is described by WHO as a rare carcinoma in which invasive pattern is predominantly in
the form of papillary structures. It may be adjacent to the nipple causing bloody or
serosanguinous discharge. Histologically, it could be distinguished from intraductal
papilloma
mainly by the absence of double cell layer and myoepithelium, scanty stroma,
necrosis and invasion. Severe cytological atypia, abnormal mitotic figures, and absence
of apocrine metaplasia also favours a malignant process. It is recommended that all
papillary lesions should be surgically excised and examined histologically since
differentiation between both entities on the bases of cytology alone may be very difficult.
Tubular Carcinoma
These tumours occur as small, firm, discrete masses. The WHO describes it as well-
differentiated carcinoma whose cells are arranged in regular well defined tubules
typically lined by one epithelial layer and accompanied by abundant fibrous stroma,.
Cytologically, there are minor nuclear abnormalities.
Apocrine Carcinoma
The tumour is composed predominantly of cells with apocrine type epithelium, i.e., large
cells with eosinophilic granular cytoplasm . The differentiation of benign from malignant
is sometimes difficult. However, cancer cells often show variability in their nuclear size
and prominent nucleoli and as a rule, they are usually dispersed whereas benign apocrine
cells often form cohesive sheets
.
Adenoid Cystic Carcinoma
Uncommon tumours, having characteristic cribriform pattern and are of the type seen
more typically in the salivary gland. Cells are usually small, basaloid, with scanty
cytoplasm and minimal anisonucleosis. Cell clusters containing mucoid cores are
characteristics.
Paget’s Disease of the Nipple
It is a specialized form of ductal carcinoma arising in the main secretory ducts and extend
to involve the skin of the nipple and areola, which exhibit eczematous changes
(Fig. 11-
16)
. Ductal carcinoma with or without invasion frequently antedates the skin changes.
The histological landmark is the involvement of the epidermis by (Paget’s Cells).These
are large oval, polyhedral, pale-staining cells with clear cytoplasm, hyperchromatic
nuclei and perinuclear halos. These are usually observed in exfolitaive specimens.

12
Secretory (Juvenile) Carcinoma
Defined by WHO as a carcinoma which is composed of pale-staining cells showing
prominant secretory activity of the type seen in pregnancy and lactation. This tumour is
more frequently seen in young girls.
Inflammatory Carcinoma
Is defined clinically by an enlarged, swollen, erythematous breast, usually without a
palpable mass. The underlying carcinoma is generally poorly differentiated and diffusely
invades the breast parenchyma. The blockage of numerous dermal lymphatic spaces by
carcinoma results in the clinical appearance
(Fig. 11-20)
True inflammation is minimal or
absent. Most of these tumors have distant metastases, and the prognosis is poor.
Features Common to All Invasive Cancers:
In all forms of BRCA discussed previously, progression of the disease leads to certain
local morphologic features. These include a tendency to become adherent to the pectoral
muscles or deep fascia of the chest wall, with consequent fixation of the lesion, as well as
adherence to the overlying skin, with retraction or dimpling of the skin or nipple. The
latter is an important sign, because it may be the first indication of a lesion, observed by
the woman herself during self-examination. Involvement of the lymphatic pathways may
cause localized lymphedema. In these cases the skin becomes thickened around
exagerated hair follicles, a change known as peau d'orange (orange peel)
(Fig. 11-20).
The Male Breast:
Gynecomastia
It is an endocrine related enlargement of the male breast that occurs most frequently in
adolescents and elderly; mainly in response to excessive esrogenic stimulation.
Generalized hypertrophy is usual, but there may be a descrete tumour adjacent to the
nipple
(Fig. 11-22)
. Microscopically, there is ductal hyperplasia and dilatation with loose
stromal proliferation and an inflammatory infiltrate. Because of the cellularity,
anisonucleosis and nucleoli, caution should be experienced in diagnosing these lesions
cytologically.
Carcinoma
Rare, occurring in advanced age, with a frequency ration to female breast cancer
approximating 1:100. Because of the scanty amount of breast tissue, male mammary
carcinoma tend to infiltrate rapidly and ulcerate through the skin with prominent axillary
nodal involvement.
GRADING of Mammary Ductal Carcinoma
The prognosis of Breast Cancer depends on the degree of anaplasia (tumour
differentiation). Different systems of grading have been successfully applied for better
evaluation of cancer evolution. In general, the classification of Scarff, Bloom and
Richardson (SBR) is the most currently used and recommended by the WHO. It
comprises the description of three characters:
13
A. The Degree of Tubular Differentiation
B. The Nuclear Pleomorphism
C. The Mitotic Activity
Accordingly, mammary carcinoma could be classified histopathologically into Grade I
which carries a favorable prognosis; Grade II corresponding to moderate prognosis, and
Grade III indicating bad prognosis.
STAGING of Mammary Carcinoma
According to the Committee of the Clinical Staging of the International Union Against
Cancer (UICC), the recommended following staging system was adopted in 1989 by the
American Joint Committee on Cancer (AJCC). The classification depends upon the
size of the primary tumor (T), extent of regional lymph node metastases (N) and
distant metastases (M). The designation TNM has been chosen for clinical staging and
pTNM refers to pathological staging.
Clinical staging is important for precise individualized treatment planning and estimation
of prognosis. However clinical staging is less accurate than the pathological since there is
a tendency to overestimate the size of the primary tumor and inaccurately assess the
axillary lymph nodes for the presence of metastatic carcinoma.
TNM CLASSIFICATION OF BREAST CANCER
T-
Primary
Tumor
Tx
Primary tumor cannot be assessed.
To
No evidence of primary tumor.
Tis
Carcinoma in situ.
T
1
Tumor 2 cm or less in greatest dimension
T
1a
0.5 cm or less in greatest dimension
T
1b
more than 0.5 cm but not more than 1 cm
T
1c
more than 1 cm but not more than 2 cm
T
2
Tumor more than 2 cm but not more than 5 cm
T
3
Tumor more than 5cm in greatest dimension.
T
4
Tumor of any size with direct extension to chest wall or skin.
T
4a
with fixation to chest wall (including ribs, intercostal
muscles and serratus anterior muscle but not pectorals
muscle.
T
4b
with edema (including peau d’orange), ulceration of
skin, or satellite skin nodules on same breast.
T
4c
Both T
4a
and T
4b
T
4d
Inflammatory carcinoma.
14
N-
Regional
Lymph Nodes
N
x
Regional lymph nodes cannot be assessed (e.g. previously
removed).
N
0
No regional lymph node metastasis.
N
1
Metastasis to movable ipsilateral axillary node (s).
N
1a
only micrometastasis (not larger than 0.2 cm)
N
1b
Metastasis to lymph node (s), any larger than 0.2 cm.
N
2
Metastasis to ipsilateral axillary node (s) fixed to one another
N
3
Metastasis to ipsilateral internal mammary lymph node (s).
M-
Distant
Metastasis
M
x
Presence of distant metastasis cannot be assessed.
M
0
No distant metastasis
M
1
Distant metastasis (including metastasis to supraclavicular LNs).
PROGNOSTIC FACTORS in Breast Cancer
Prognosis
– the prediction of the duration, course and outcome of the disease in a patient
is an essential part of medical practice. In breast cancer patients, prognosis of
individual cases depend on several factors that include:
Age:
Higher mortality rates due to breast cancer are usually recorded before 35
and after 70 years of age.
Pregnancy
: There is a general agreement that breast cancer manifesting during
pregnancy and lactation is associated with a poor prognosis. On the other hand it
has been shown that pregnancy two years following treated breast cancer is not
unfavorable..
Early Diagnosis
: The relative 5 and 10 years survival rates for asymptomatic
breast cancer detected in a large screening project (BCDDP) were 88% and 79%
respectively. This is attributable to the fact that most of these tumors were small,
devoid of axillary metastasis and a high percentage were of microscopically
favorable types.
Tumour Stage
which depends upon:
- The Size of the Tumour:
Tumors measuring less than 2cm. are often
associated with favorable prognosis, compared to larger tumors.
- Lymph Node Involvement: This is one of the most important prognostic
parameters. With no histological nodal involvement, the 5-year survival rate is

15
about 80%, falling to 21% in the presence of four or more nodes.
Histological Grade
: The 10-year survival rate for patients harbouring Grade I
tumors is around 80%, dropping to 45% in Grade III.
Histological Type:
Morphological variants of invasive ductal carcinoma with a
more favorable prognosis are tubular, cribriform, pure mucinous, medullary,
papillary, adenoid cystic and juvenile carcinomas. There is no significant
prognostic difference detected between ordinary invasive ductal and invasive
lobular carcinoma .
Other Microscopical Findings
such as:
i- Type of Tumor Margins : Tumors with pushing margins have better
prognosis than those with infiltrative margins.
ii- Stromal Reactions : While necrosis is associated with increased incidence
of lymph node metastases, the absence of necrosis within the tumor and the
presence of elastosis are claimed to be associated with better prognosis.
Presence or Absence of invasion:
The importance of this valuable prognostic denominator is demonstrated by the fact
that in situ cancer is 100% curable with mastectomy. Nipple involvement is found to
be associated with a higher incidence of axillary metastases. The presence of tumor
emboli in lymphatics or blood vessels increases the risk of tumor recurrence.
The Proliferative Rate and Presence of Aneuploidy:
The fraction of cells scattered outside the modal peaks of DNA histograms correlates
with poor behaviour. Euploid mammary carcinoma have a significantly better
prognosis than aneuploid carcinomas.
Hormone Receptors:
Esstrogen and Progesterone Receptors in breast cancer are found proportional to the
degree of cellular differentiation. Patients having hormone receptor positive
carcinomas carry a better prognosis.
Other Tumour Markers: e.g. C erb or Her 2
oncogenes are correlated with
aggressive behavior.
Presence of Growth factors or Amplified Oncogenes:
Some experimental evidence exist linking Epidermal Growth Factor (EGF)
Receptors with carcinogenesis.

16
