Esophagus
Esophagitis + Barrett
esophagus
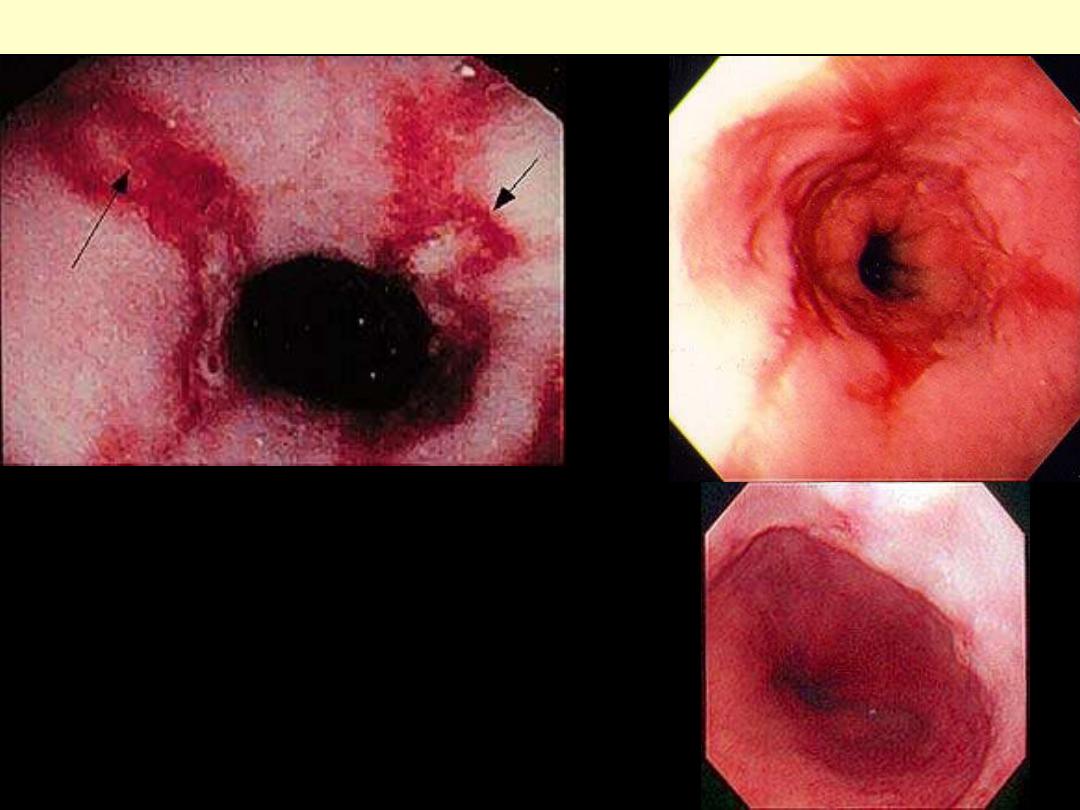
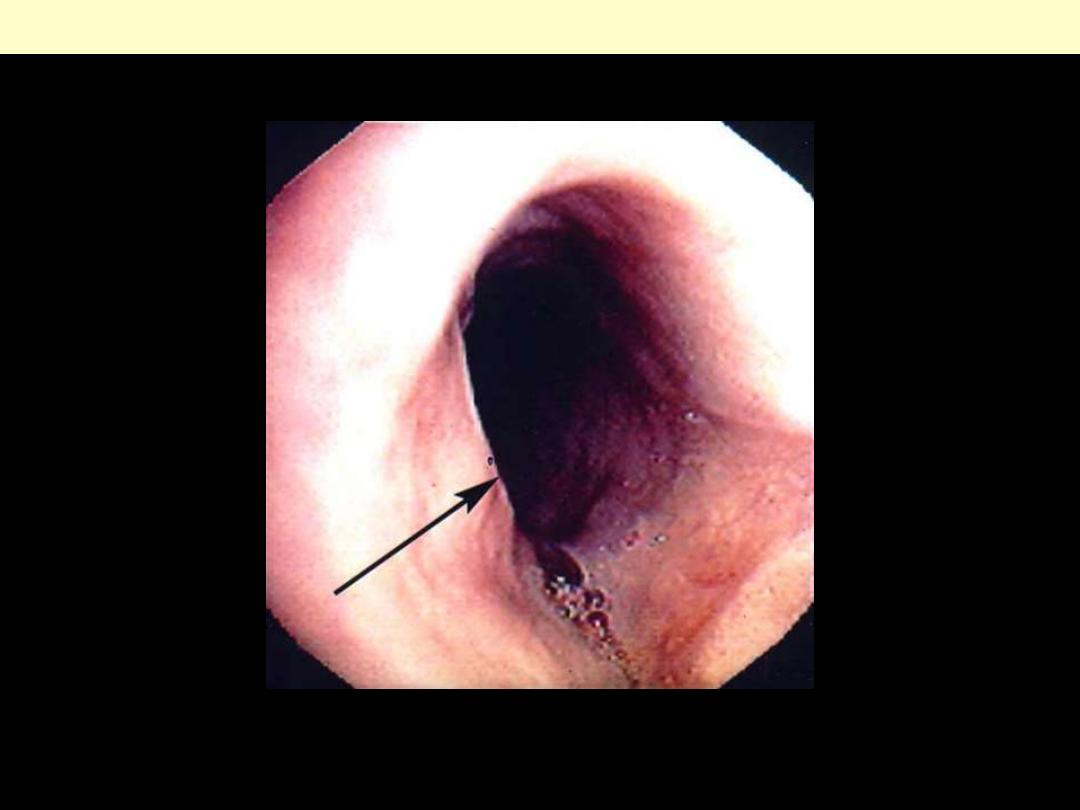
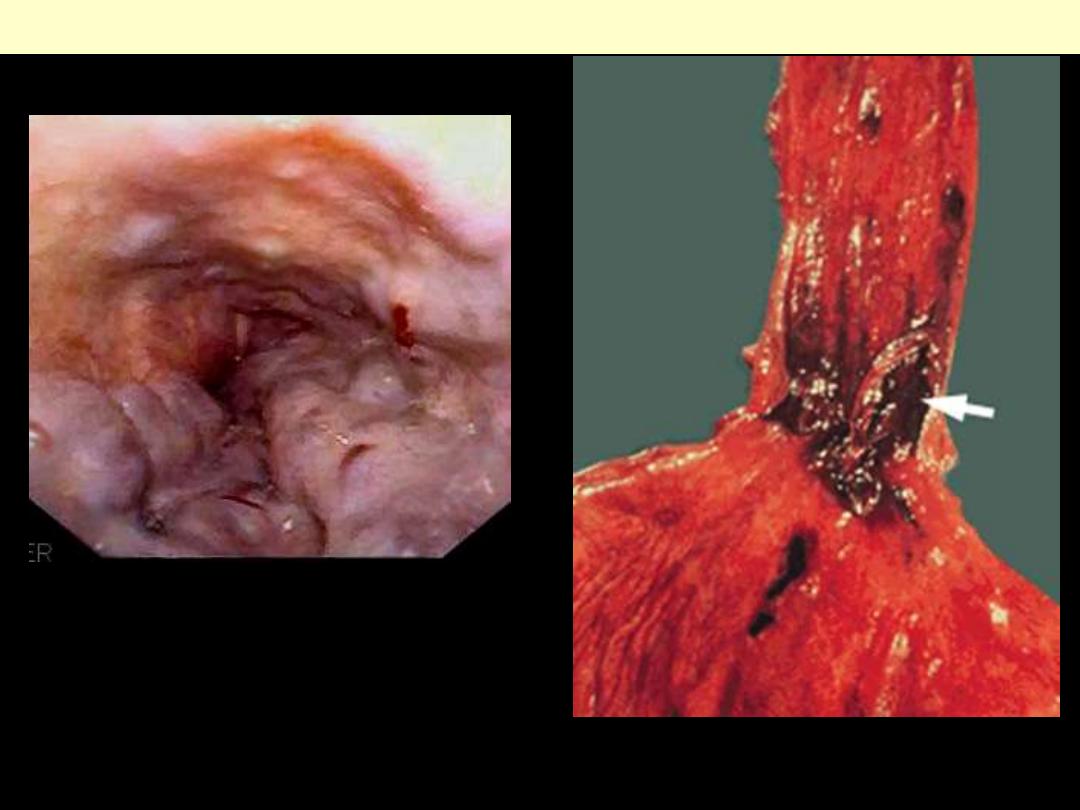
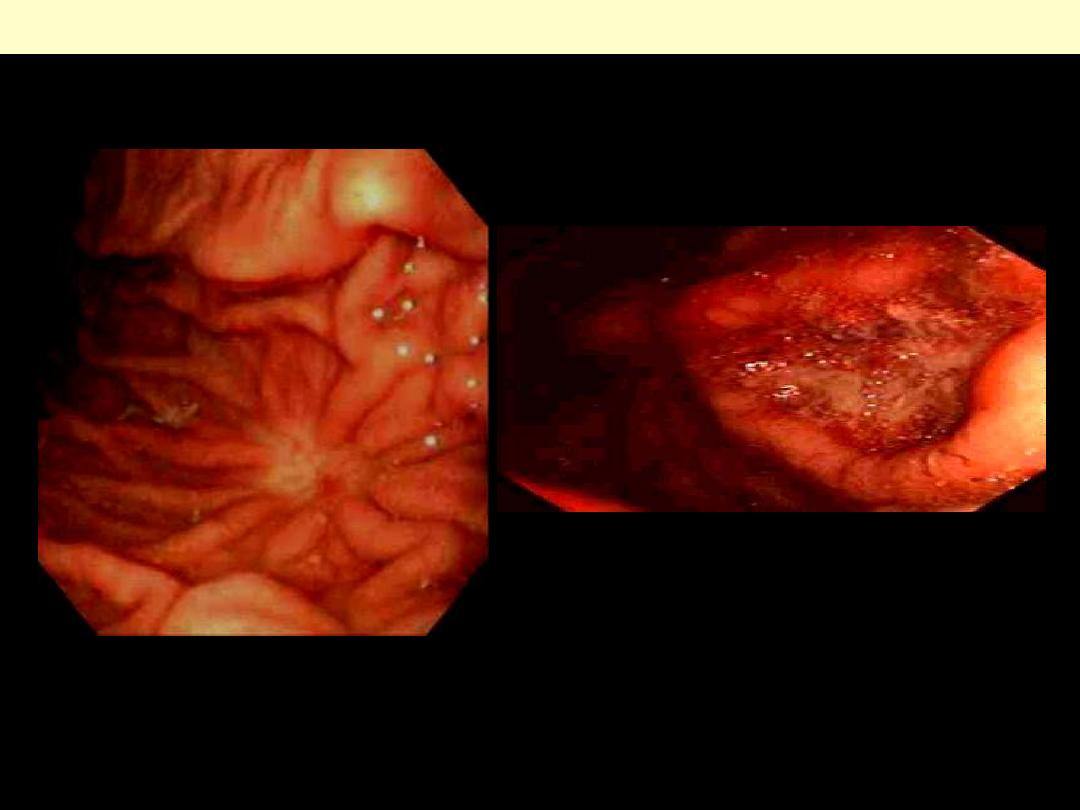
Reflux esophagitis endoscopy
There is marked hyperemia (focal or diffuse)
affecting the lower esophagus. Arrows point to
erosions.
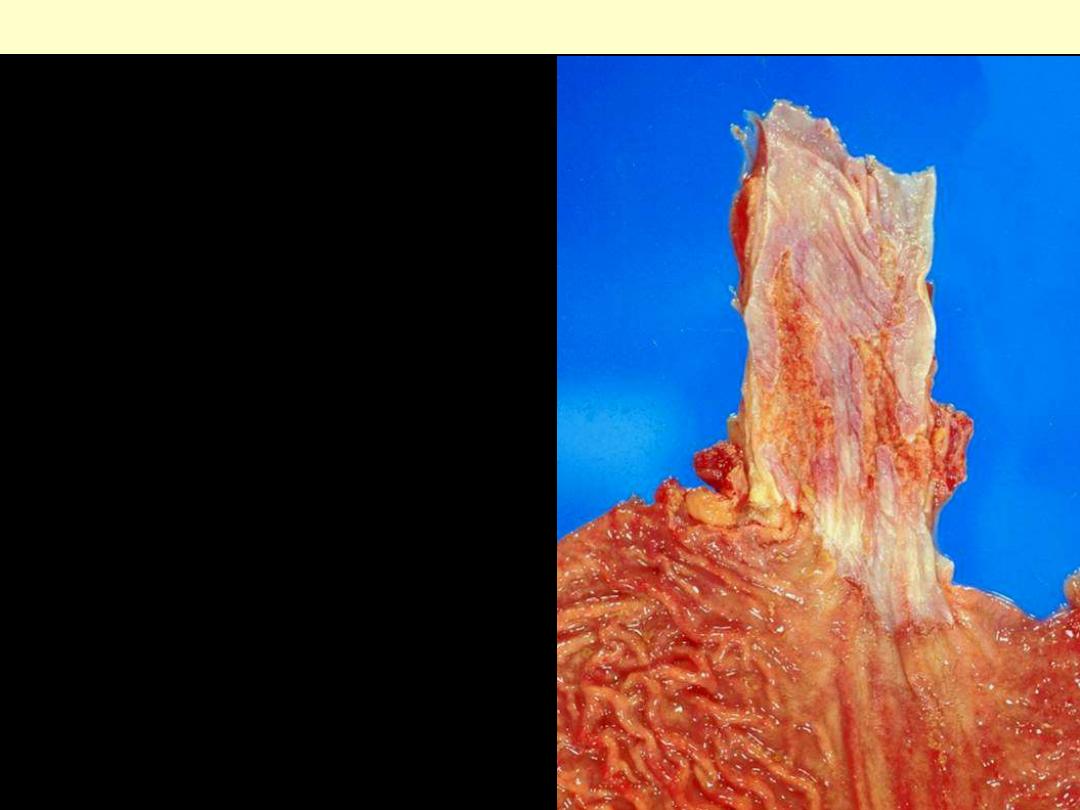
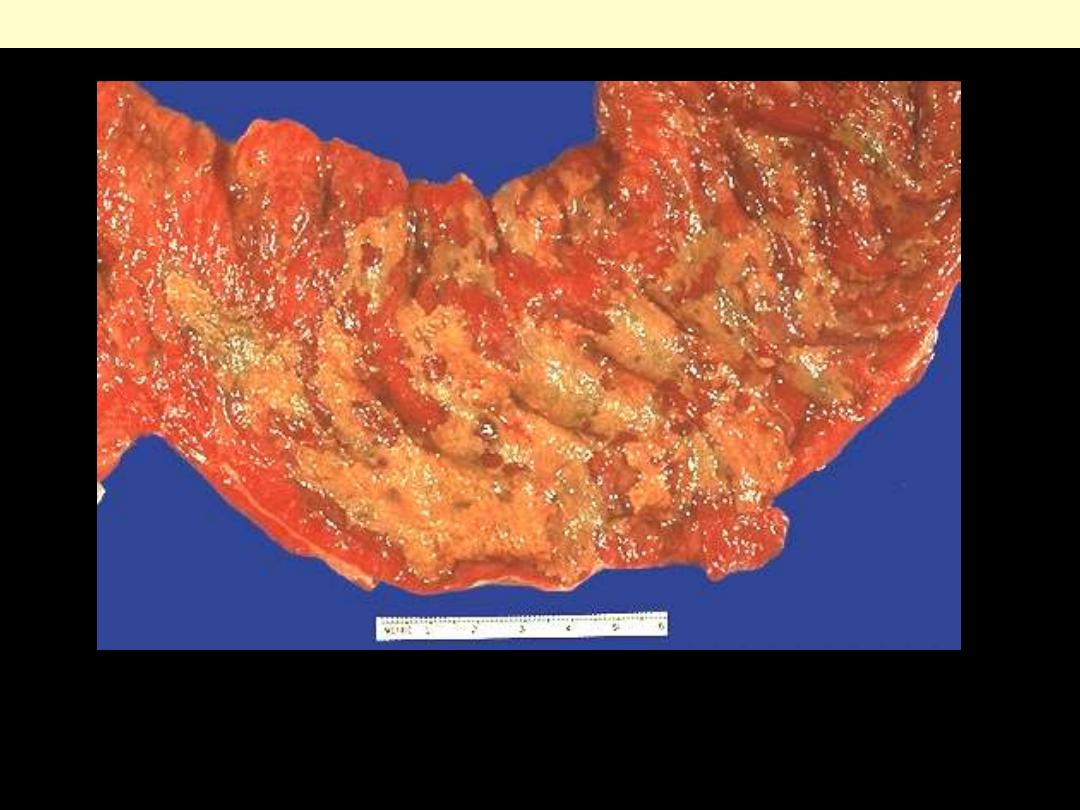
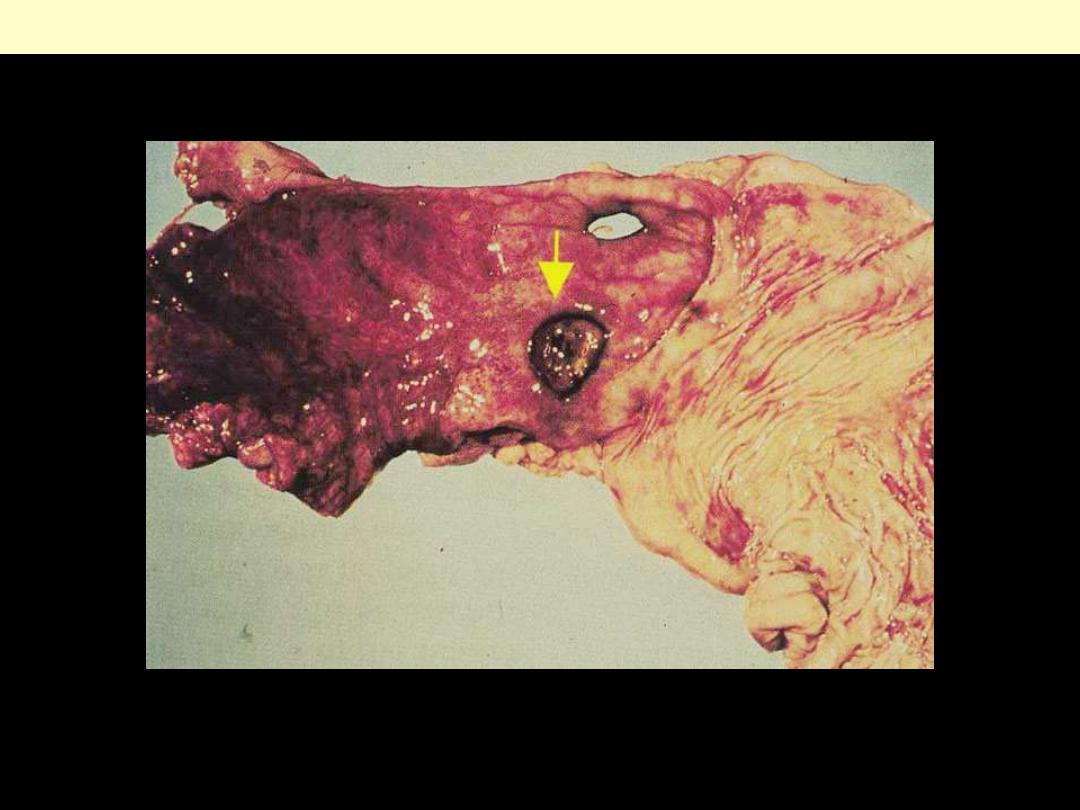
Reflux esophagitis
Gross appearance of a severe case of reflux esophagitis.
Marked hyperemia with focal hemorrhage is present in
the area of reflux.
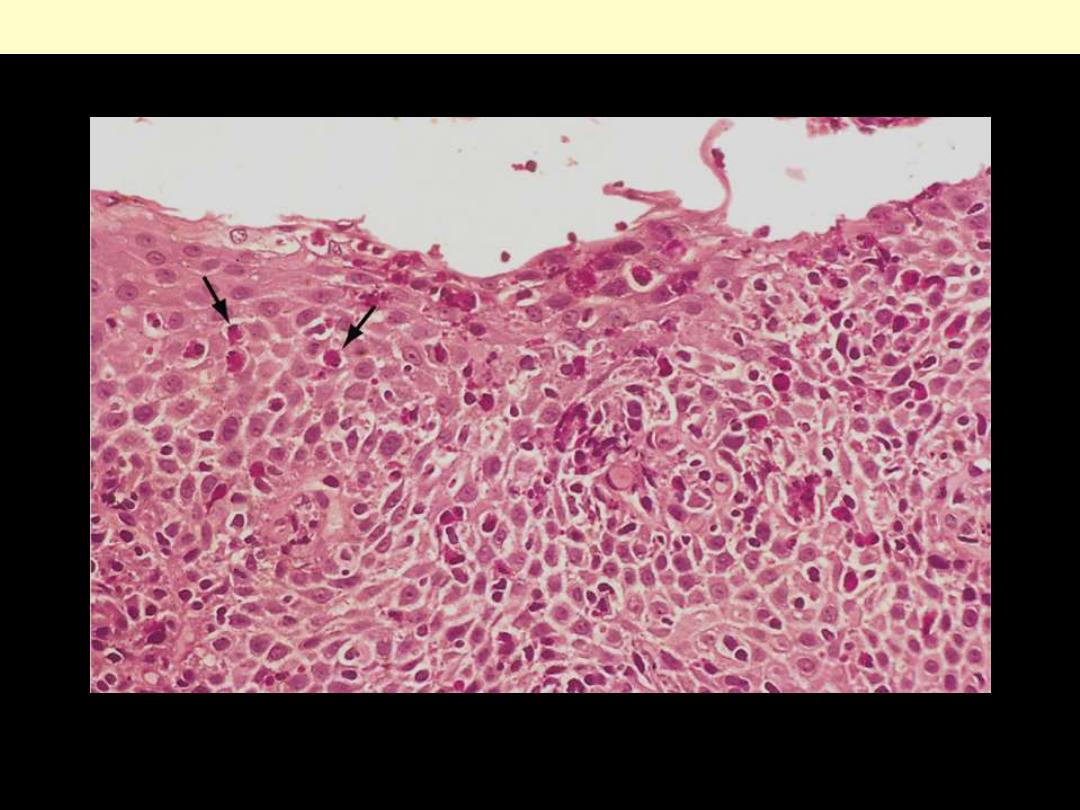
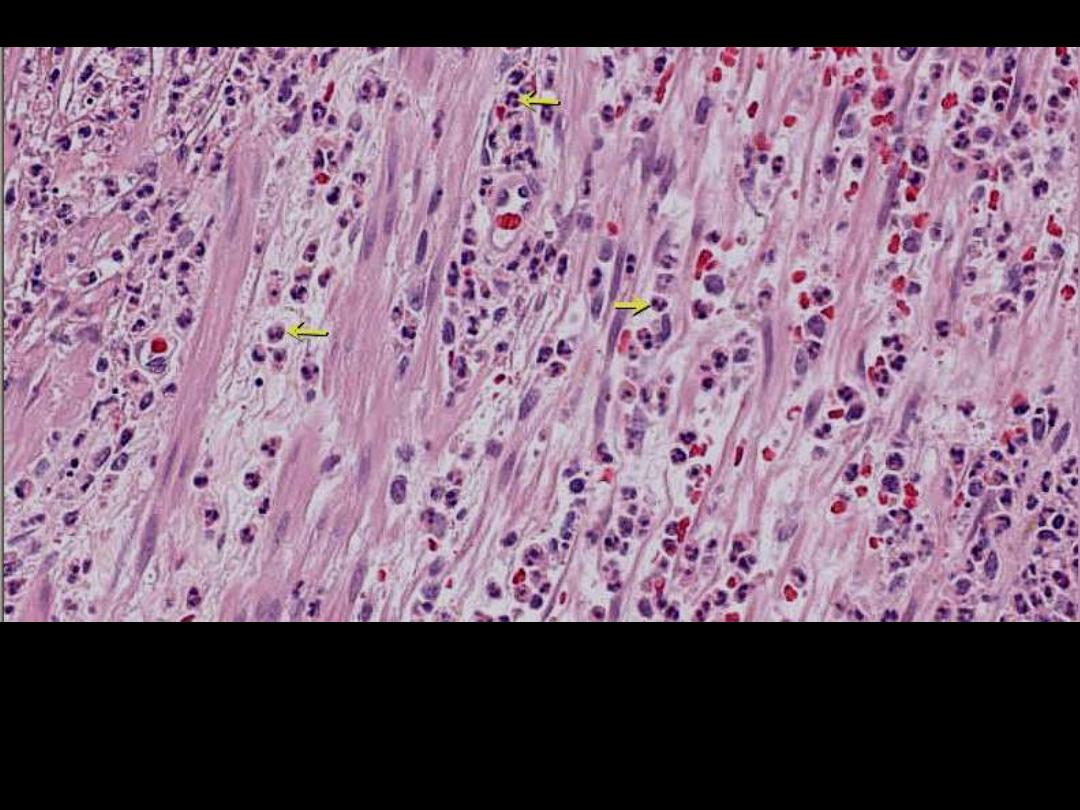
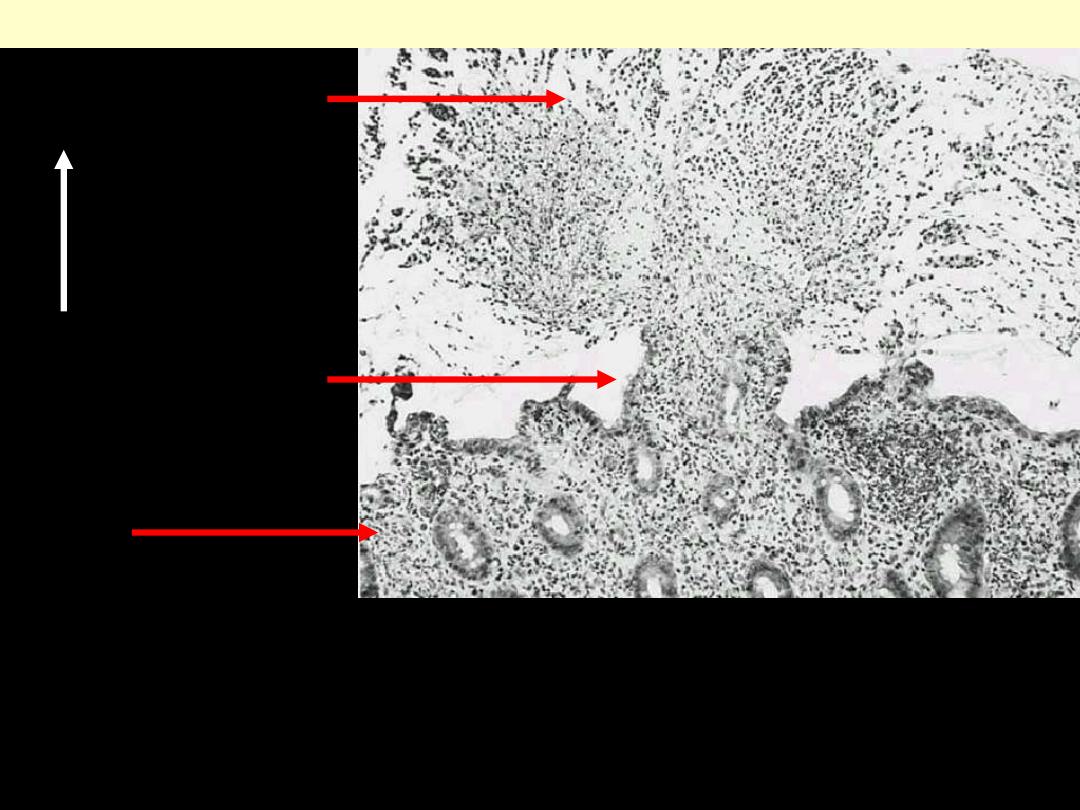
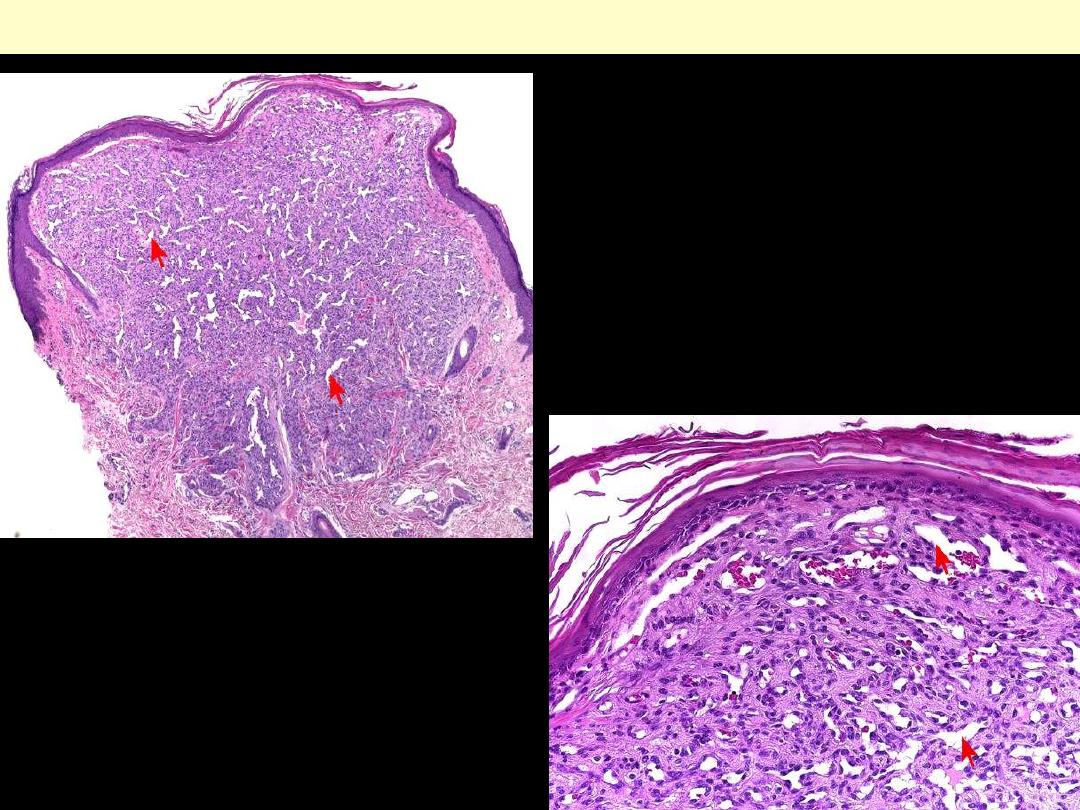
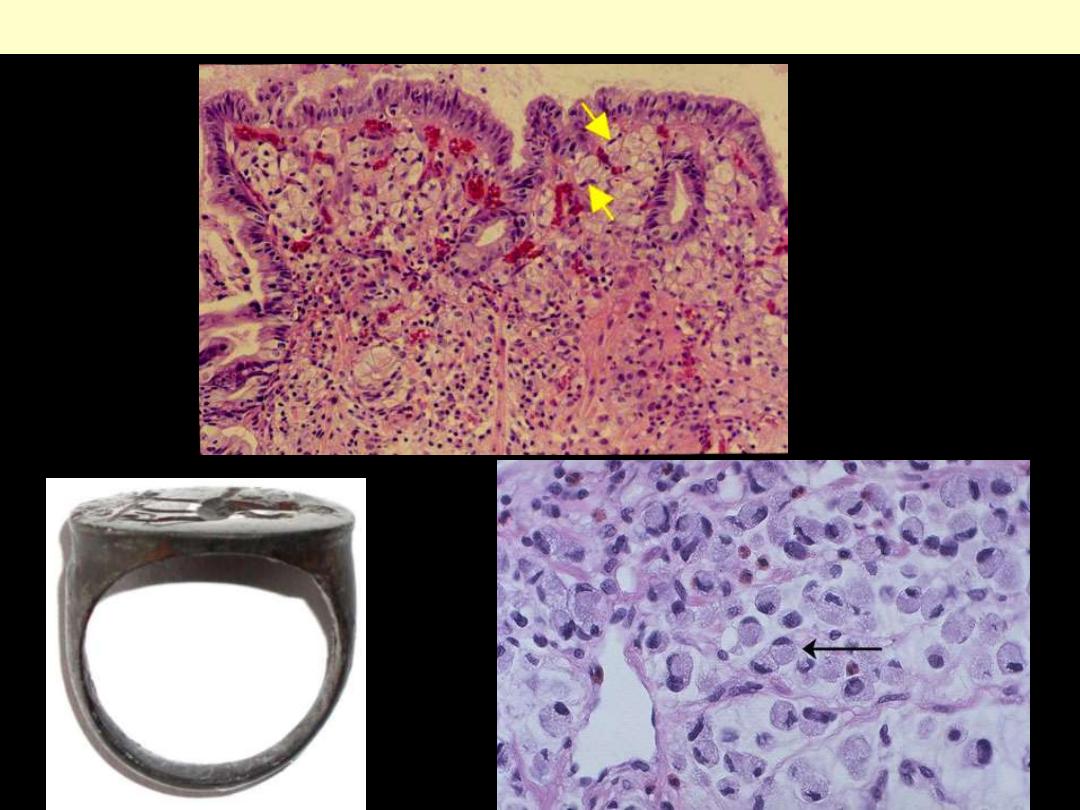
Reflux esophagitis showing the superficial portion of the mucosa. Numerous eosinophils (arrows) are
present within the mucosa, and the stratified squamous epithelium has not undergone complete
maturation because of ongoing inflammatory damage.
Reflux esophagitis
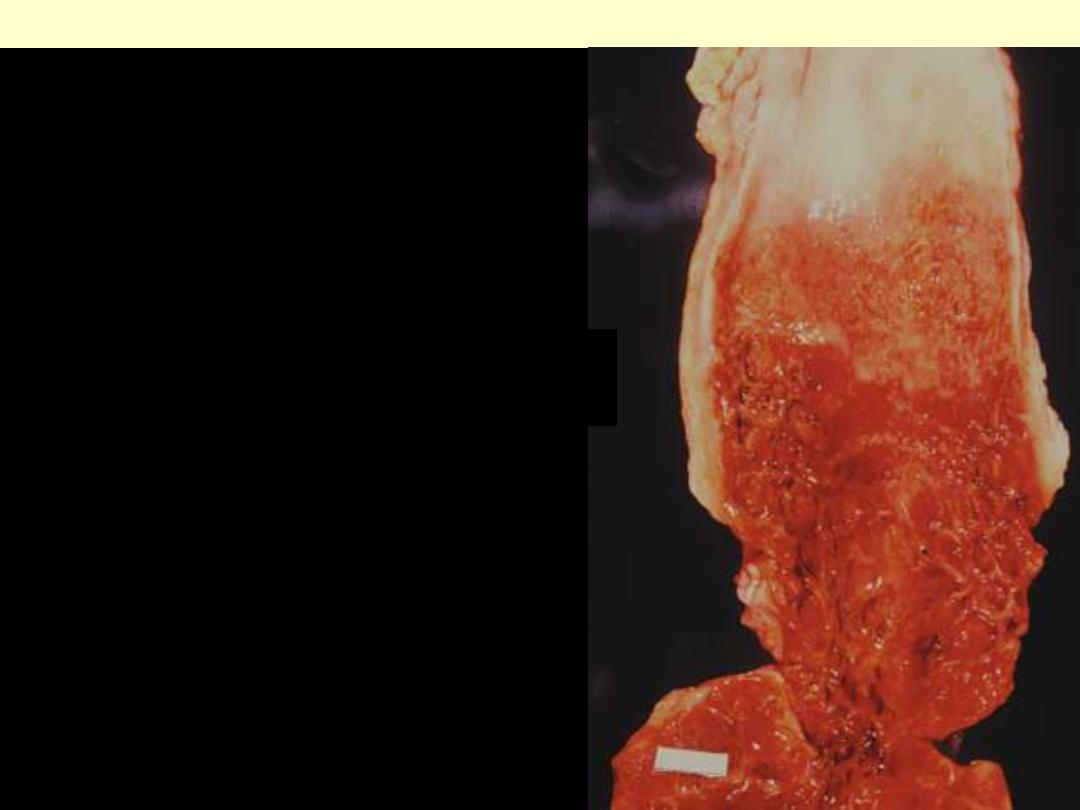
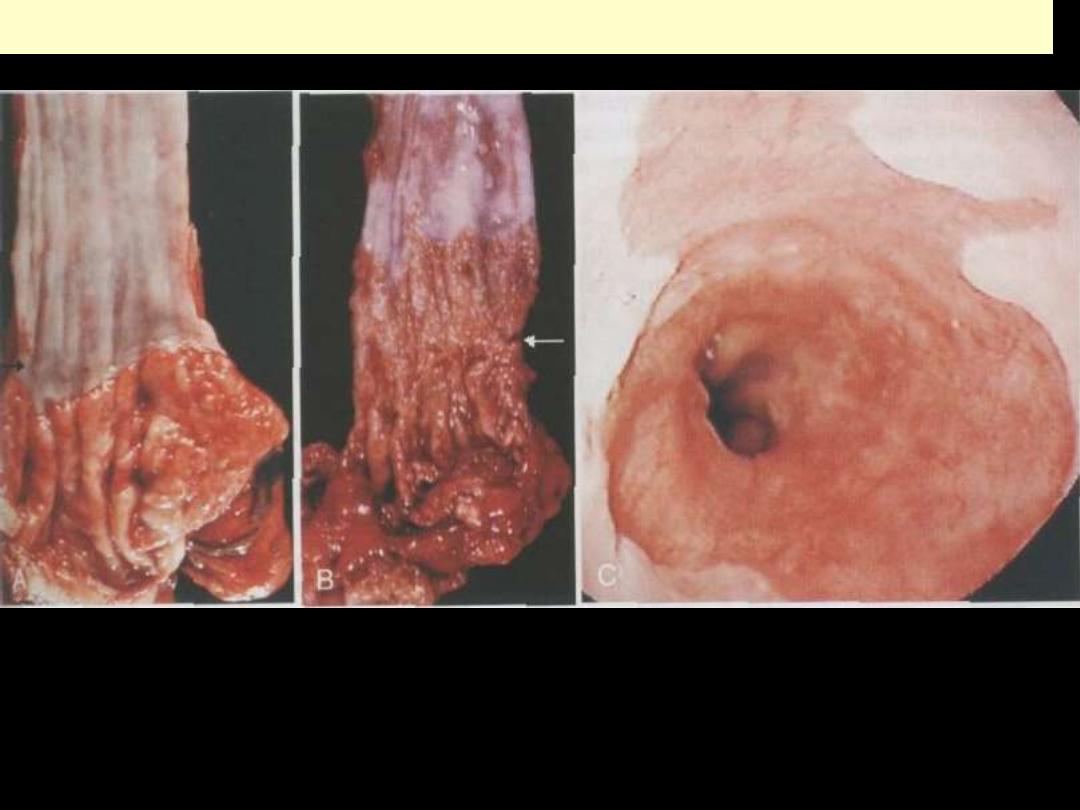
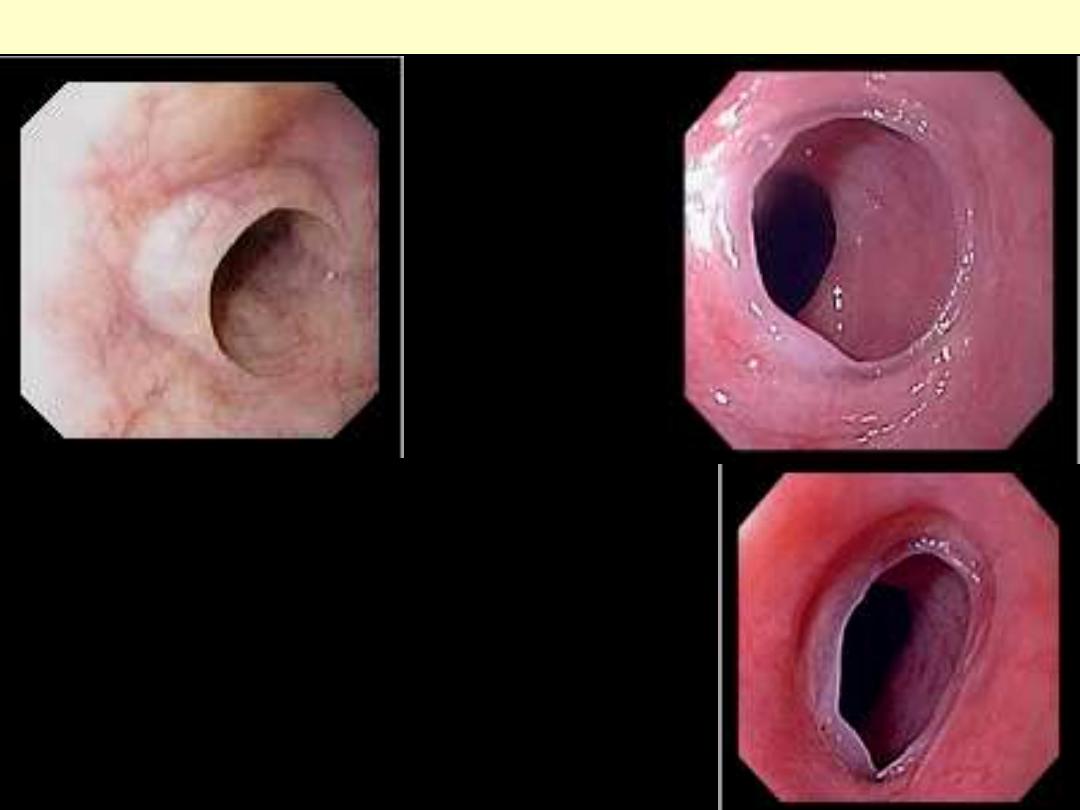
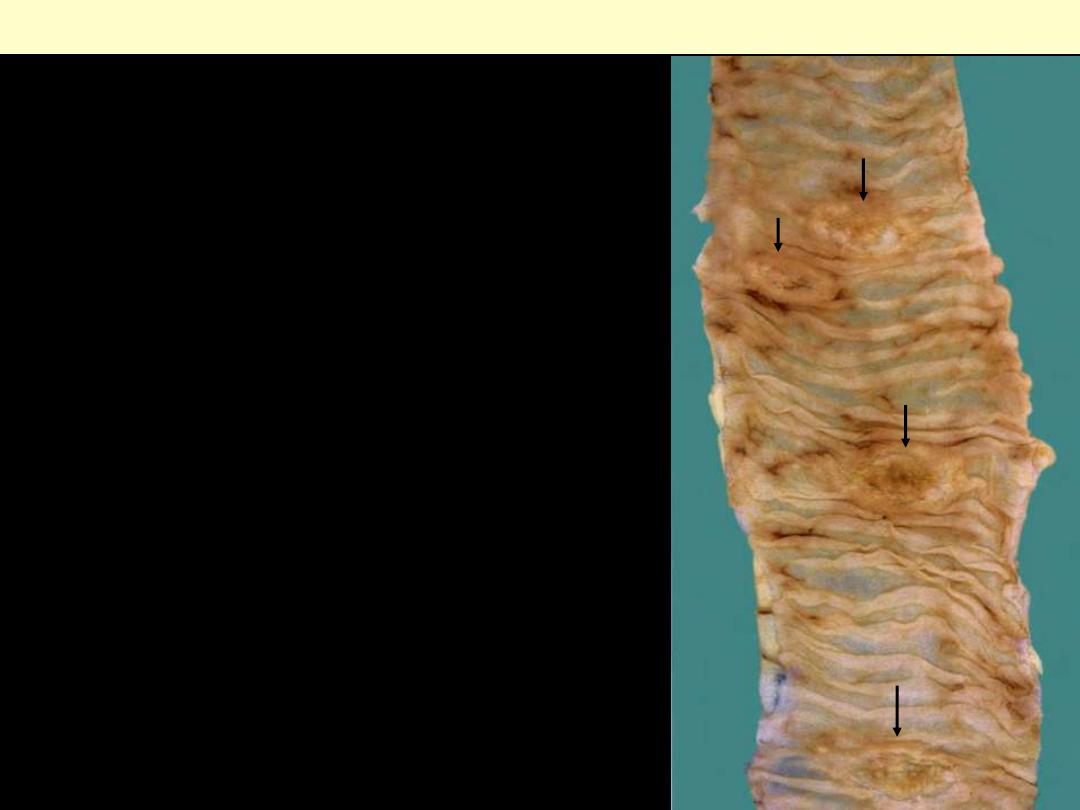
BARRETT ESOPHAGUS
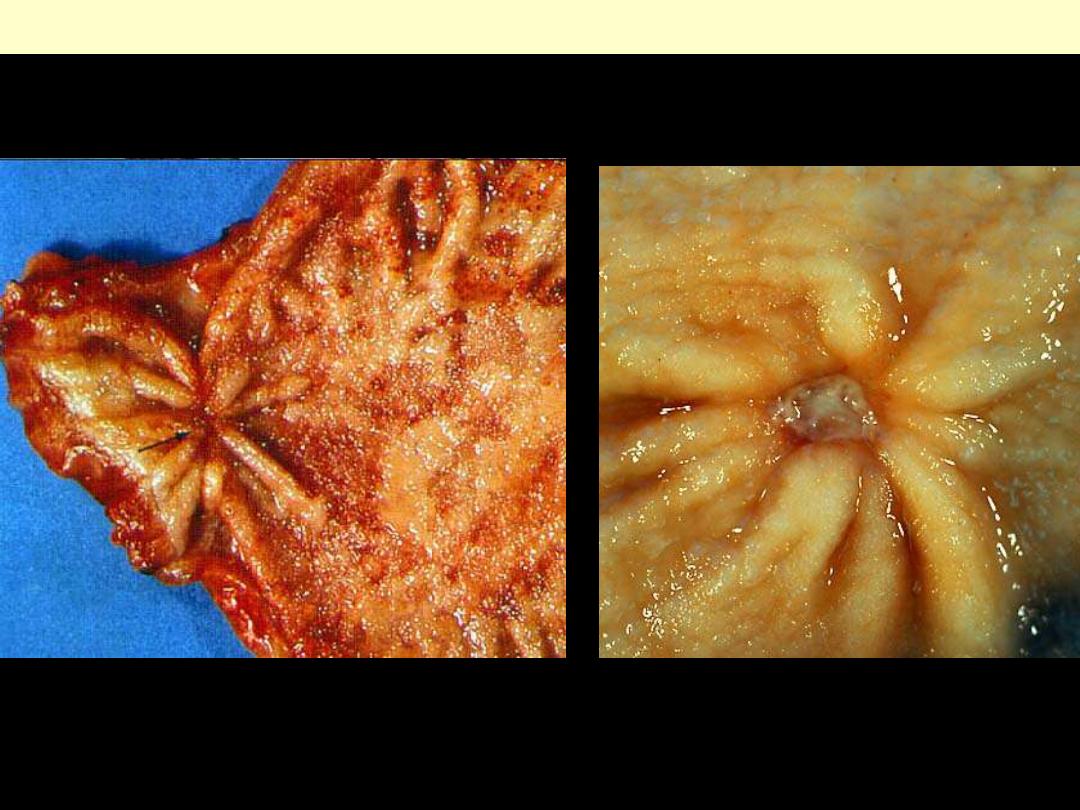
Relatively sharply limited patchy, red orange,
velvety mucosa of the middle and distal esophagus.
Barrett esophagus
A & B, gross view of distal esophagus and proximal stomach, showing Lt, the normal GEJ (arrow) and
middle, the granular zone of BE (arrow). C, endoscopic view of BE showing red orange velvety
gastrointestinal mucosa extending from the GE orifice. Note the paler squamous esophageal mucosa.
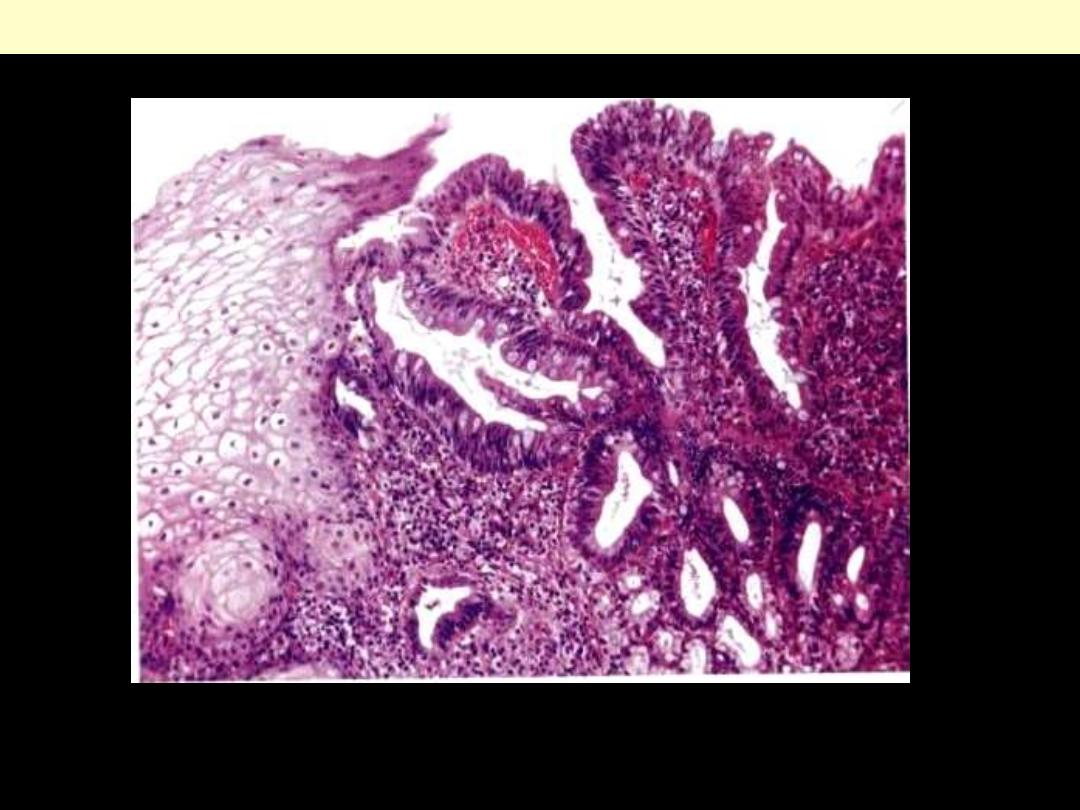
BE showing intestinal-type columnar epithelial cells (goblet cells) in a glandular villous mucosa
Barrett esophagus
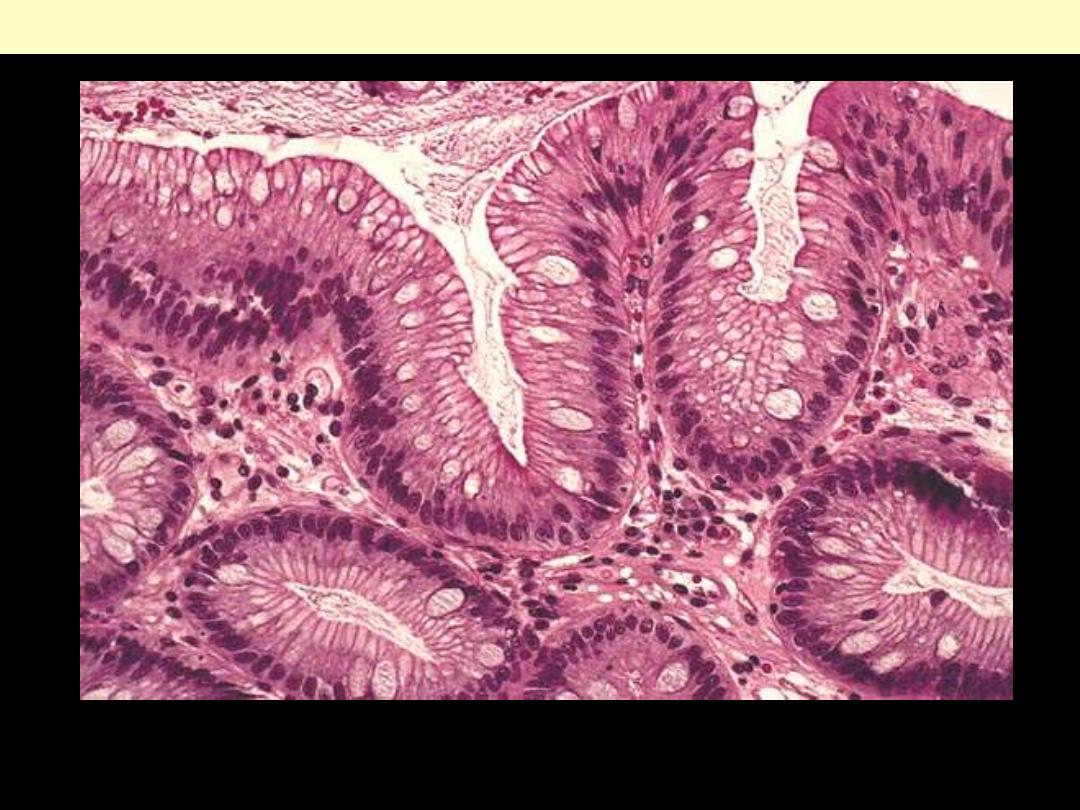
BE is characterized by the presence of specialized columnar epithelium with goblet cells.
Barrett esophagus
Esophagus – congenital
anomalies
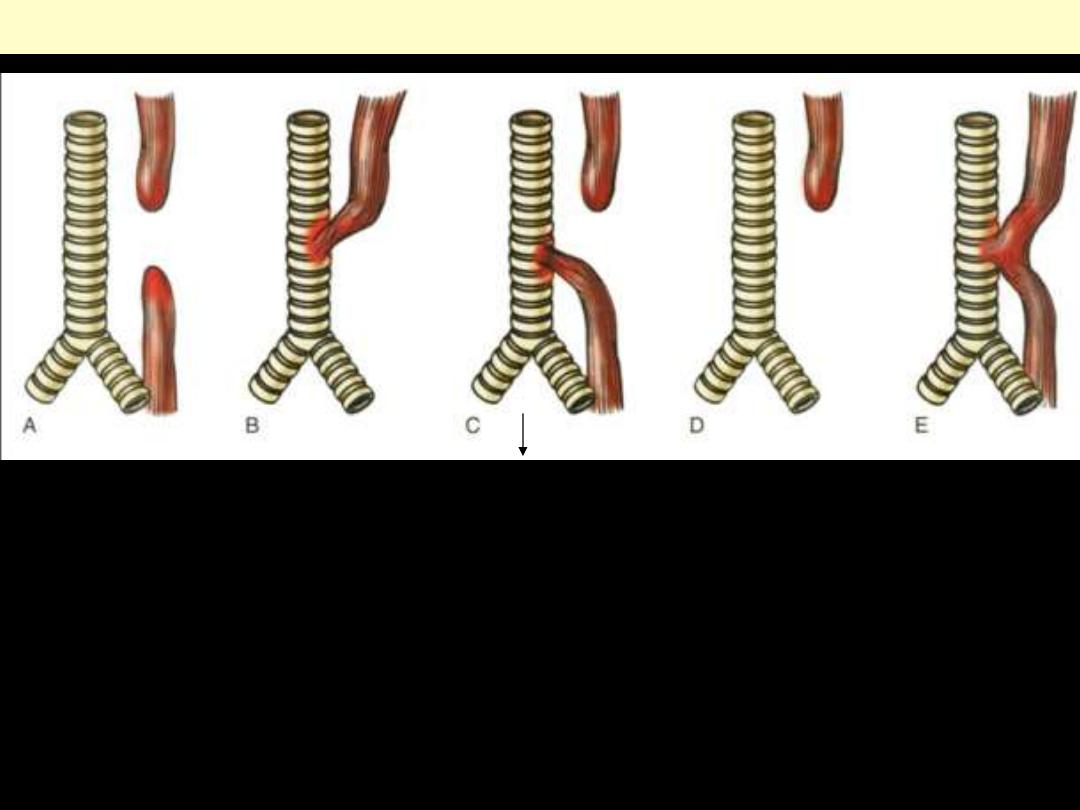
A. Blind upper and lower esophageal segments. B. Fistula between upper segment and trachea. C.
Blind upper segment, fistula between lower segment and trachea. D. Blind upper segment only. E.
fistula between patent esophagus and trachea. Type C is the most common.
Esophageal atresia and tracheoesophageal fistula
86%
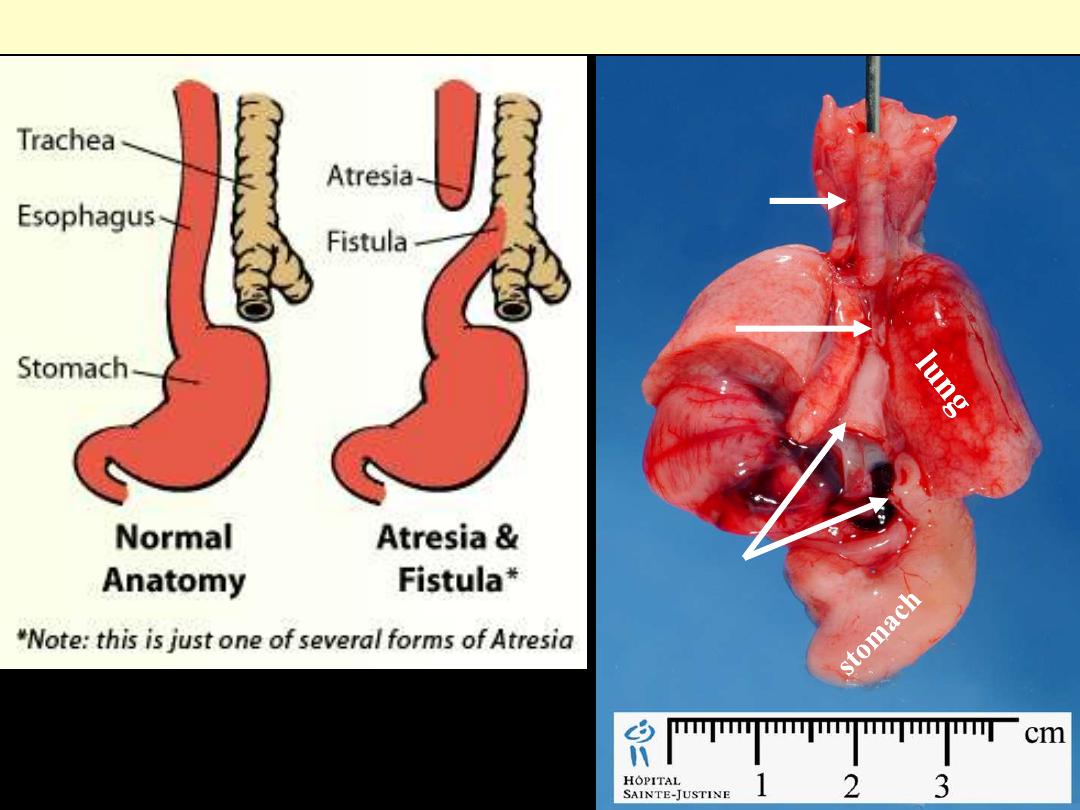
Atresia & fistula esophagus
Upper pouch
Lower pouch
Connection
Larynx
Esophageal web
An upper esophageal web (arrow) in a patient with Plummer-Vinson syndrome.
Smooth, circumferential ring of squamous mucosa, often
responsible for causing difficulty swallowing (dysphagia), which can
be located any where along the esophagus, or which may be
asymptomatic
Esophageal rings
Lye stricture esophagus (lye: detergent material)
Stenosis (stricture) esophagus
Barium swallow
Endoscopy
Esophagus – motor dysfunction
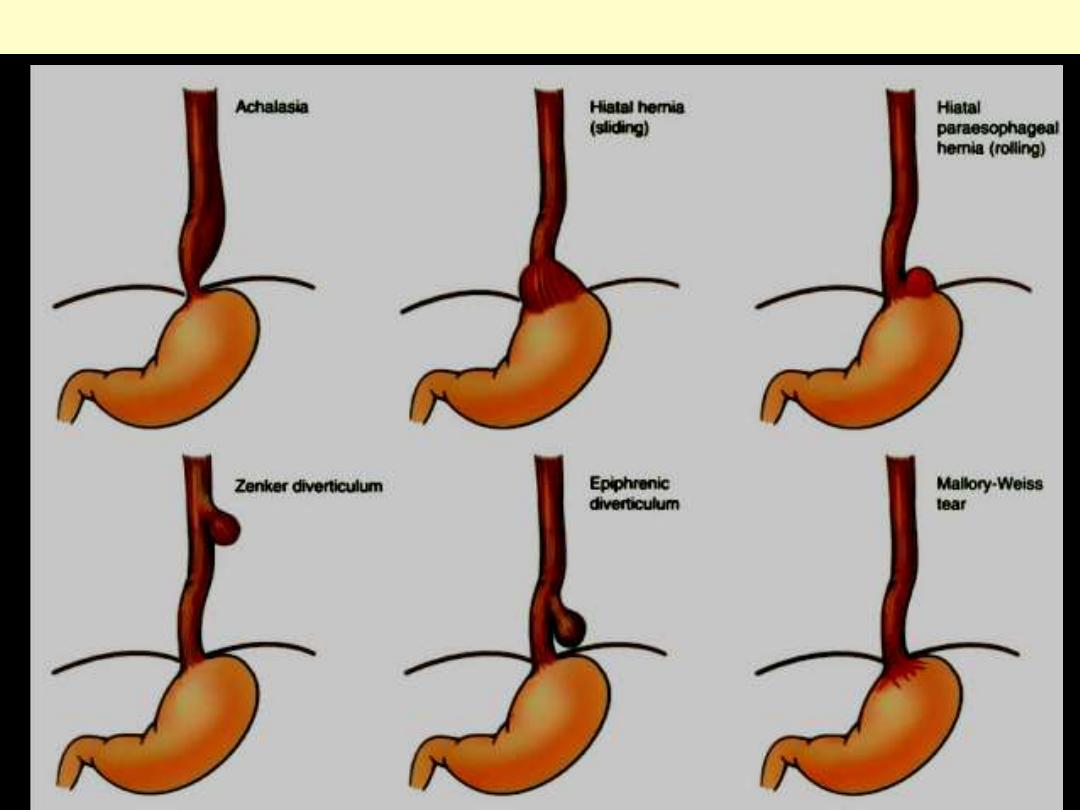
Major conditions associated with esophageal motor dysfunction
Achalasia esophagus
In patients with achalasia, the valve between the esophagus and stomach fails to open properly during
eating. In addition, the muscles of the esophagus don't effectively propel food into the stomach.
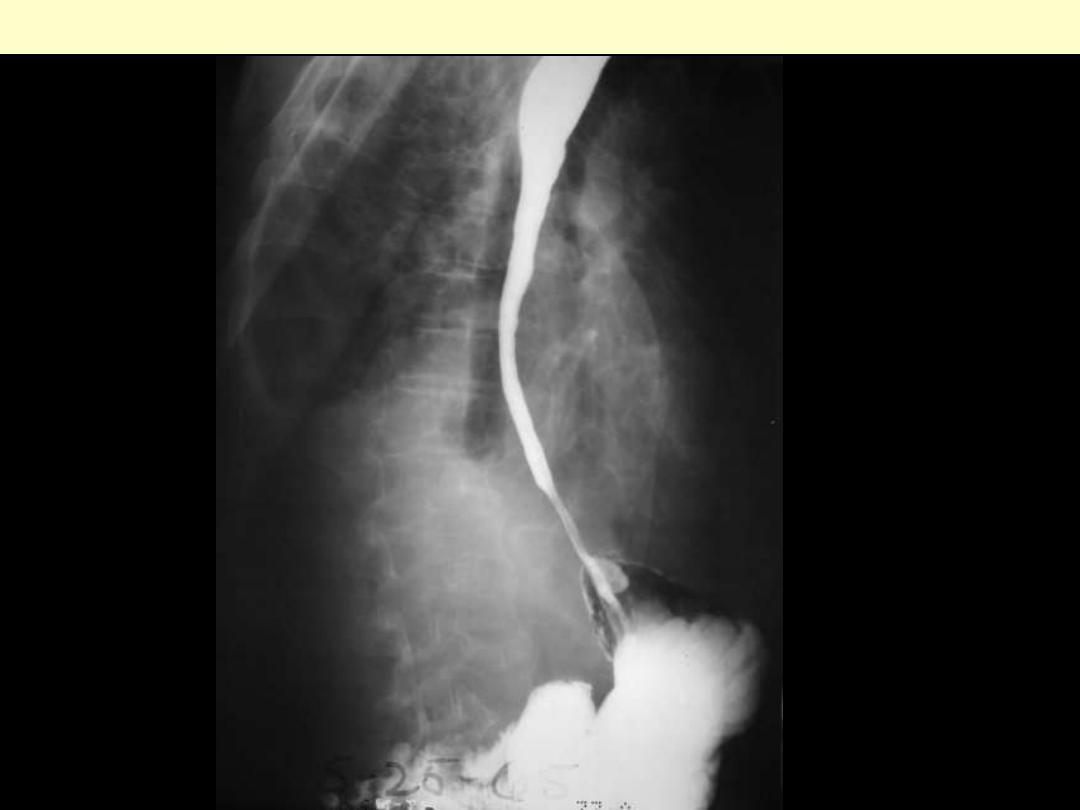
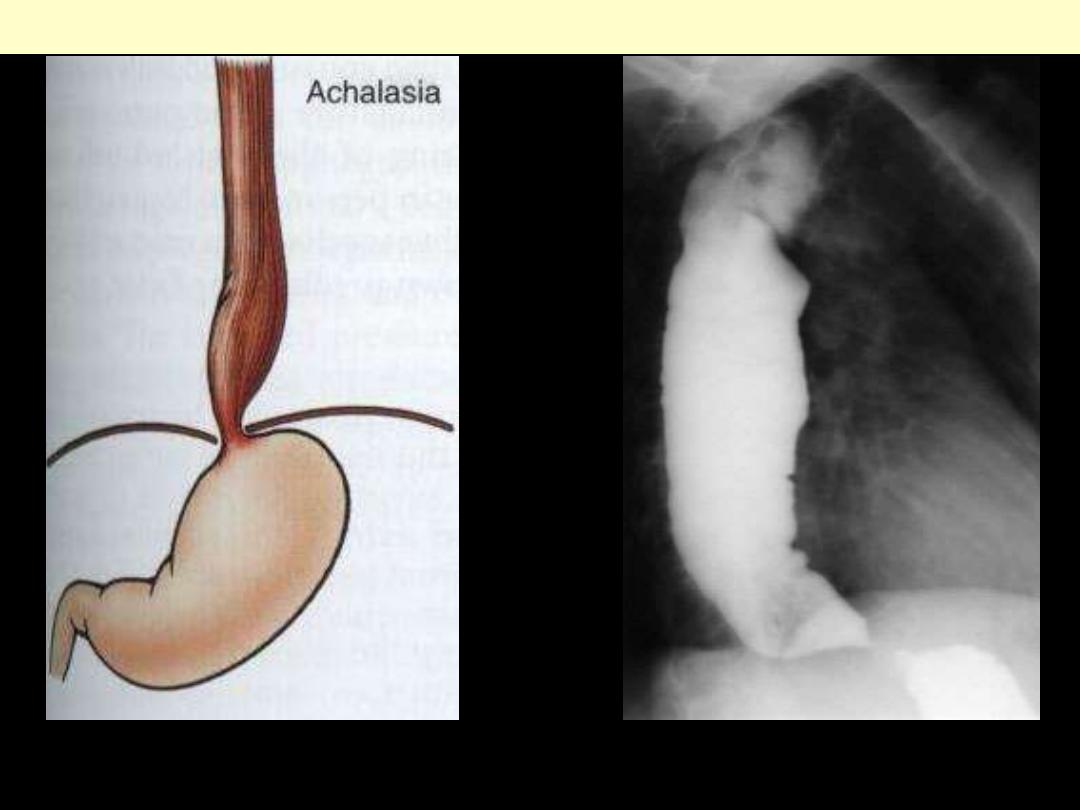
Achalasia. Inability to relax lower esophageal sphincter leads to massive esophageal dilation
Achalasia esophagus
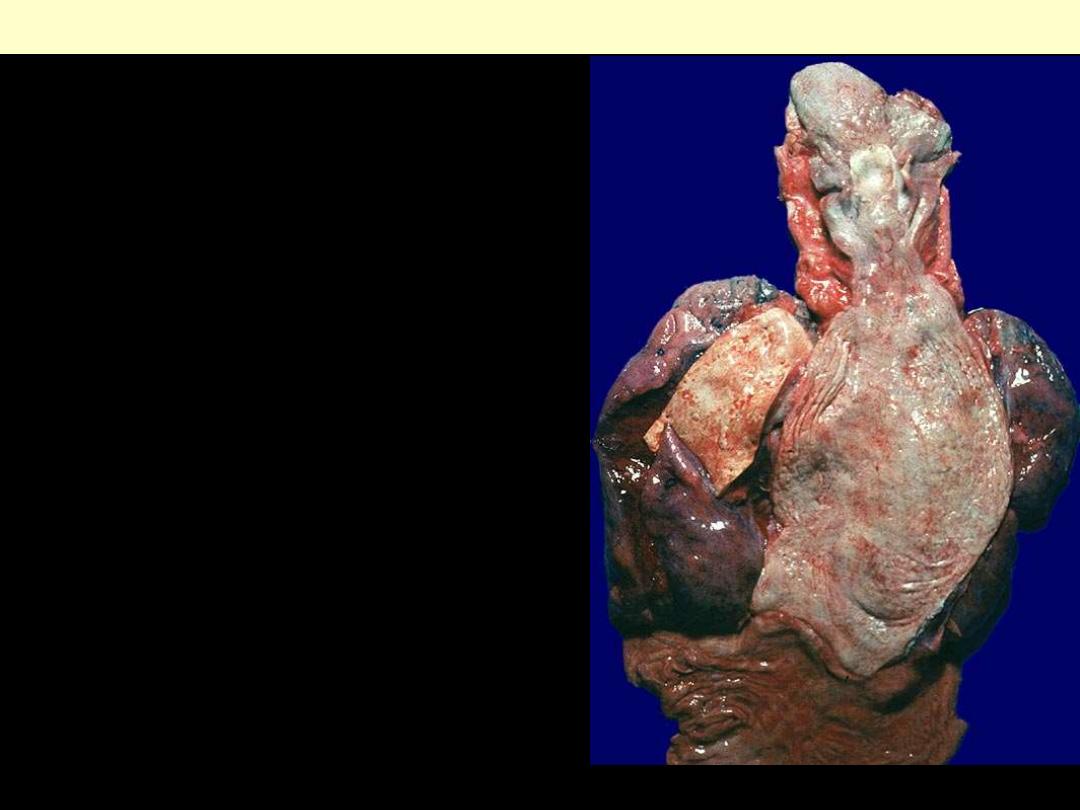
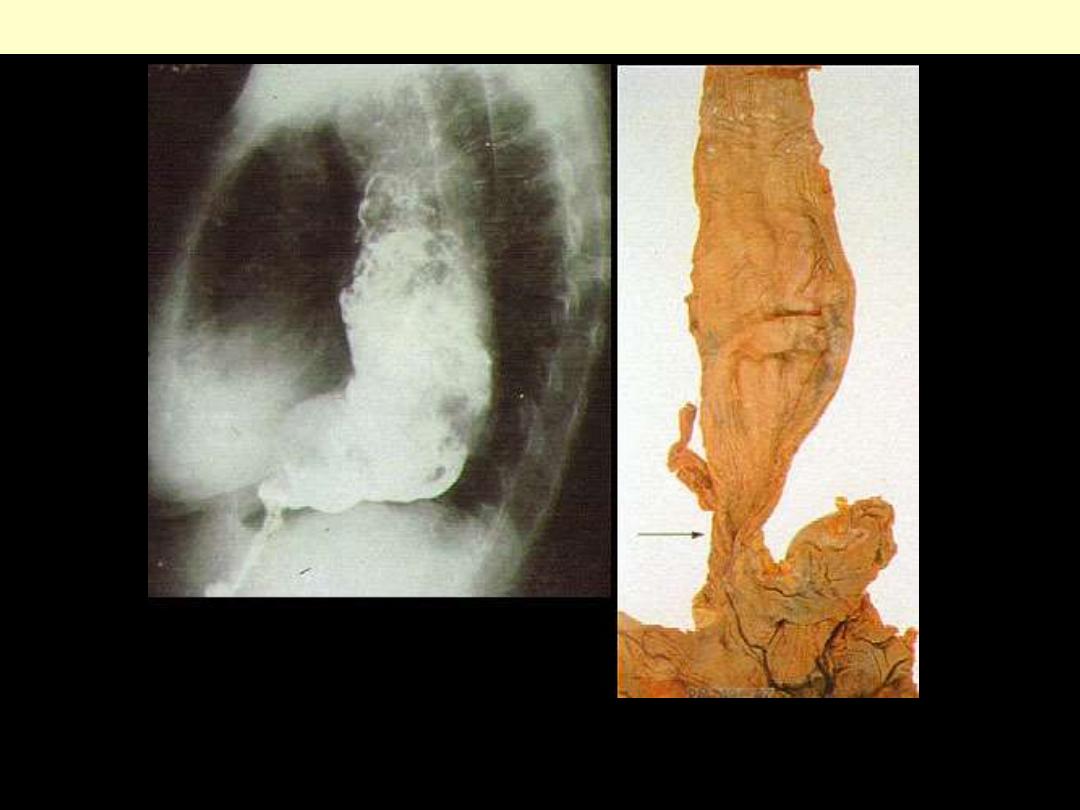
Achalasia
Dorsal view with the massively dilated esophagus
opened longitudinally.
Achalasia esophagus
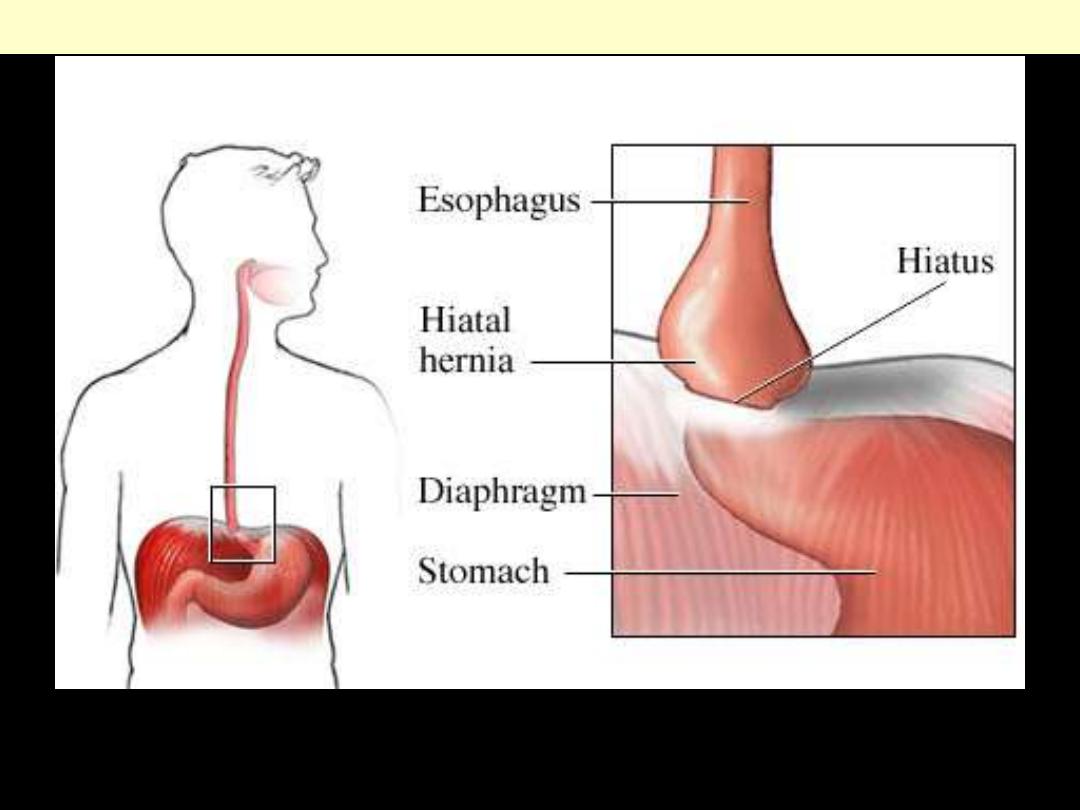
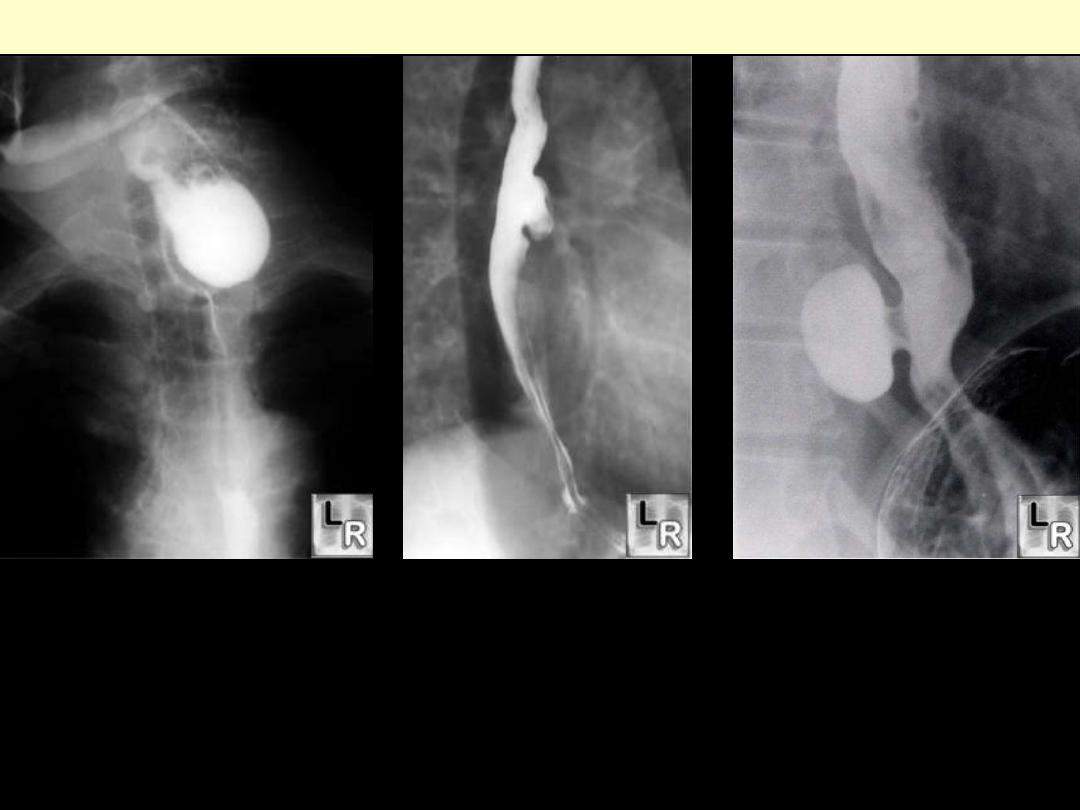
Sliding hiatal hernia
In a sliding hiatal hernia, part of the stomach moves through the diaphragm so that it is positioned
outside of the abdomen and in the chest. The lower esophageal sphincter (LES) often moves up above
its normal location in the opening of the diaphragm.
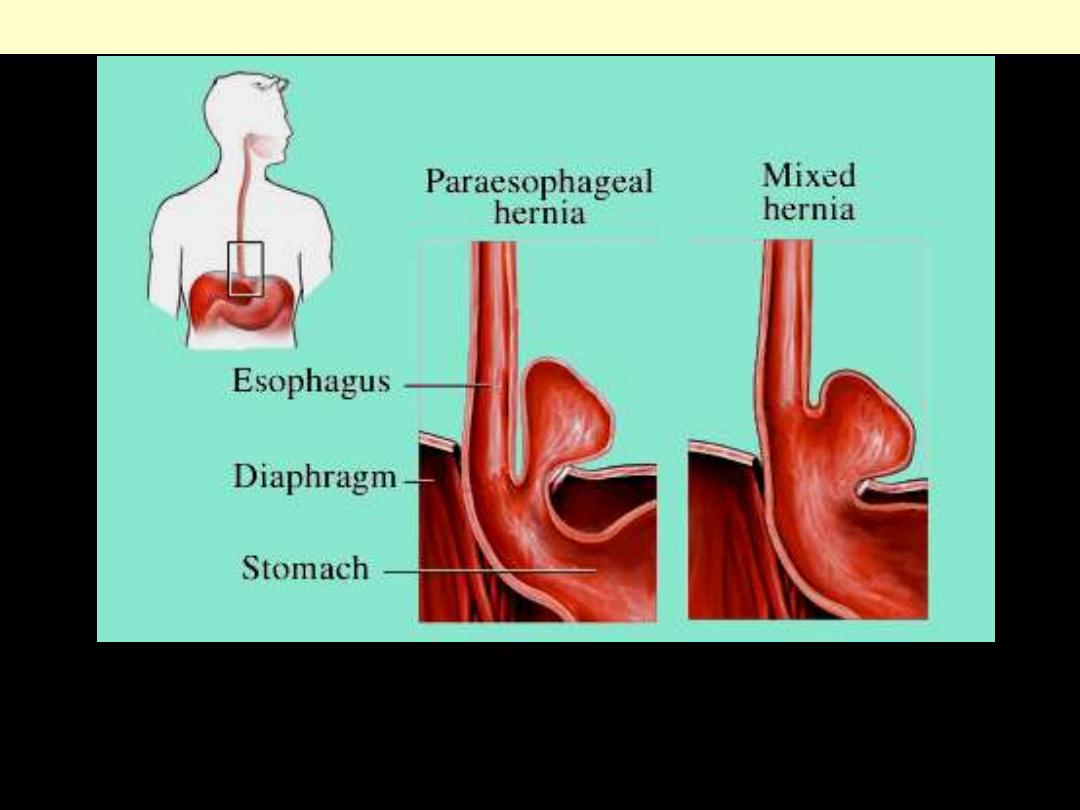
Hiatal hernia paraeosphgeal & mixed
In a paraesophageal hernia, the stomach bulges up through the opening in the diaphragm (hiatus) alongside the
esophagus (upside-down stomach). The LES remains in its normal location inside the opening of the diaphragm. This
type of hernia most commonly occurs when there is a large opening in the diaphragm next to the esophagus. The
stomach and, rarely, other abdominal organs (such as the intestine, spleen, and colon) may also bulge into the chest in
a paraesophageal hernia. MIXED HERNIA in a mixed hiatal hernia, the LES is above the diaphragm as in a sliding
hiatal hernia, and the stomach is alongside the esophagus as in a paraesophageal hiatal hernia.
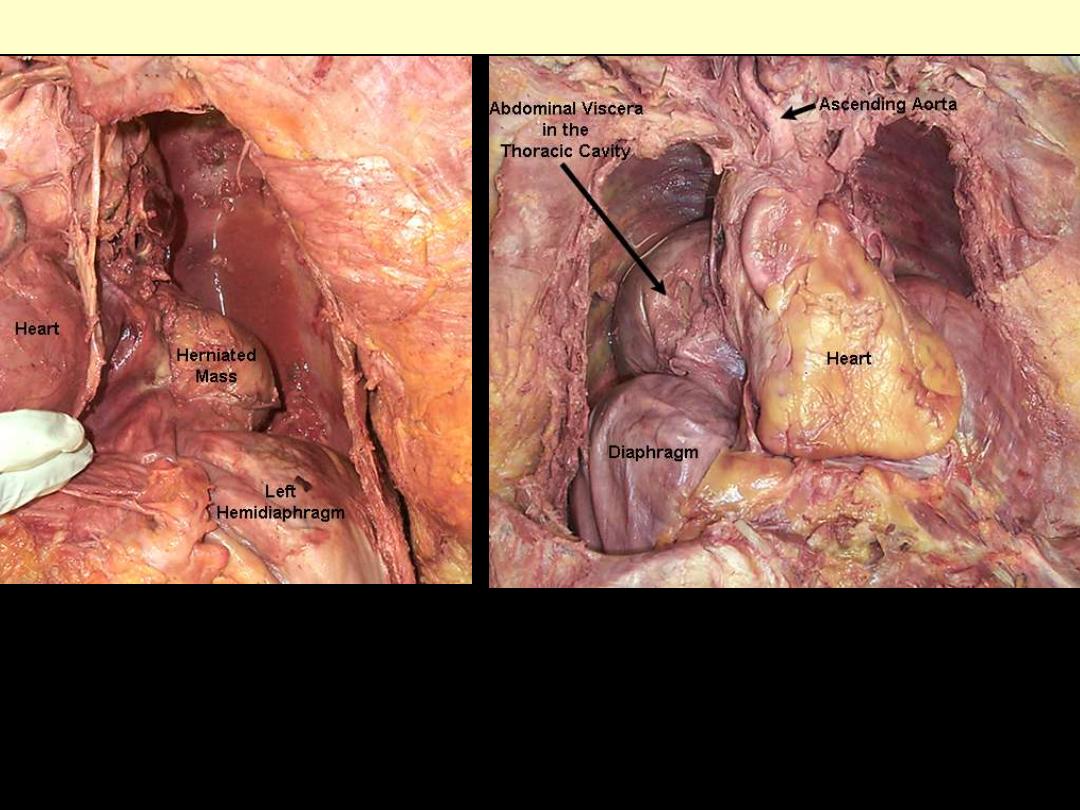
Hiatal hernia
A hiatal hernia is the protrusion of abdominal viscera, usually the stomach, into the thoracic cavity due
to a weakness in the region of the esophageal hiatus of the diaphragm. Two examples are shown above.
Diverticulum esophagus
Zenker’s Diverticulum
Midesophageal Diverticulum
Epiphrenic Diverticulum
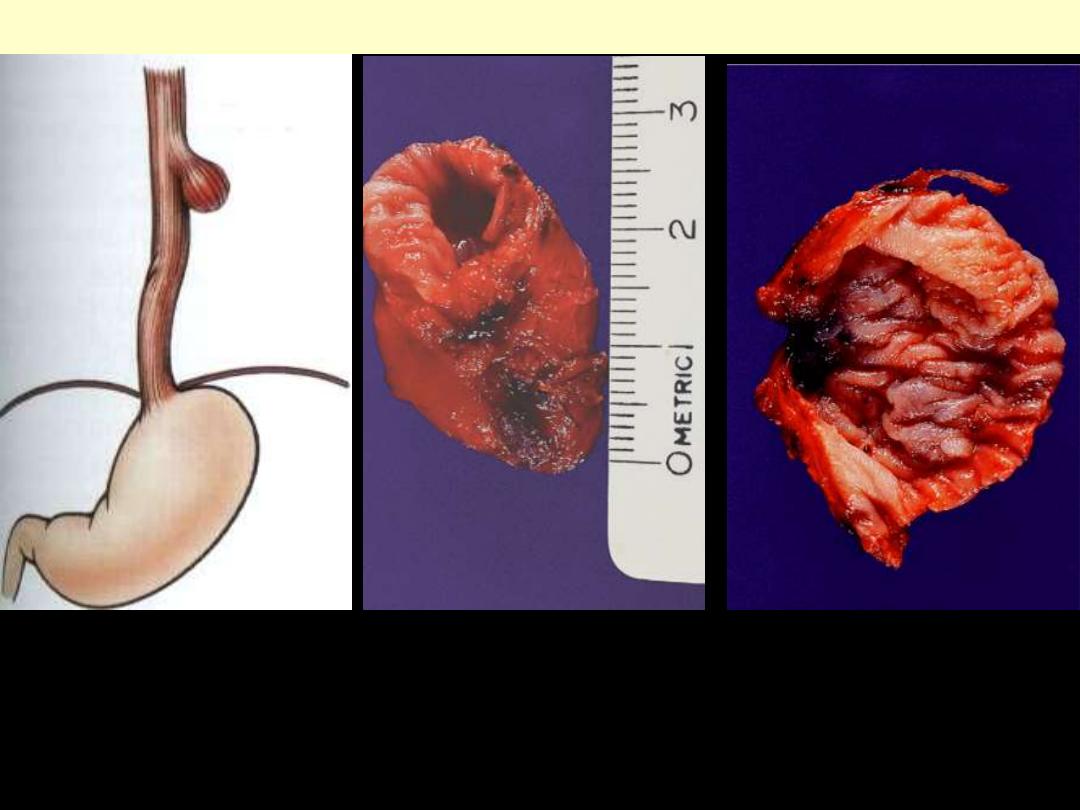
Zenker Diverticulum
Focal out pouching of the upper esophagus wall that contains all or some of its constituents
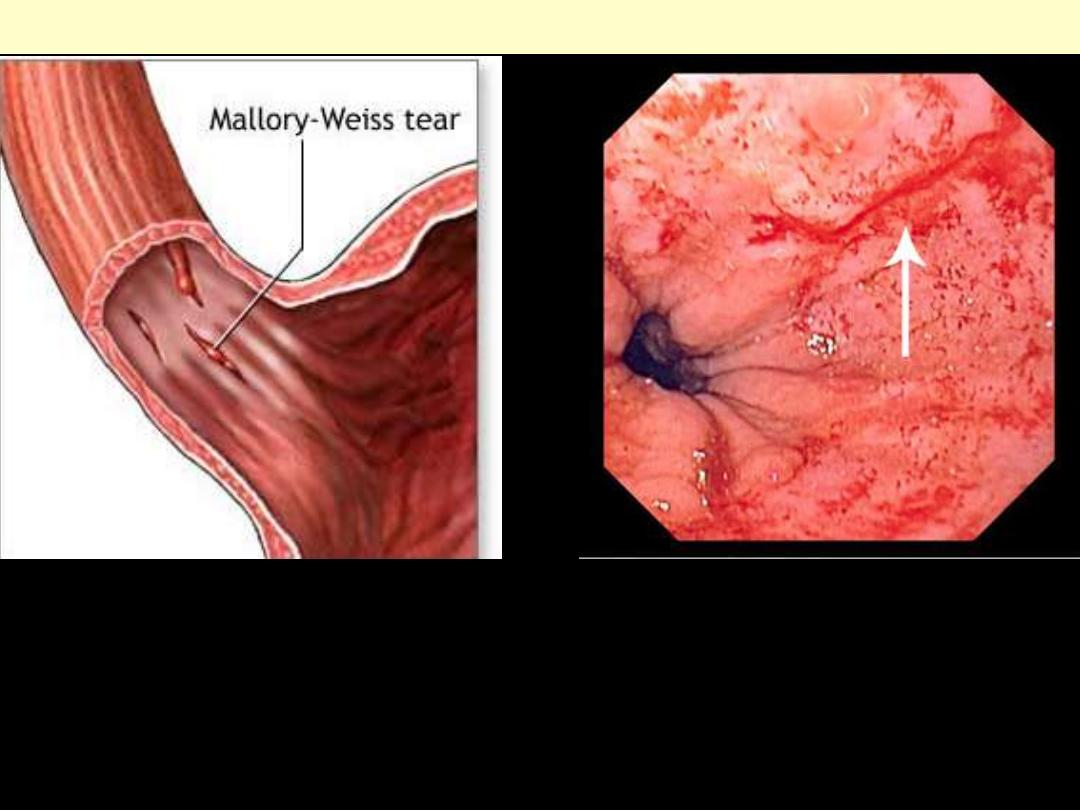
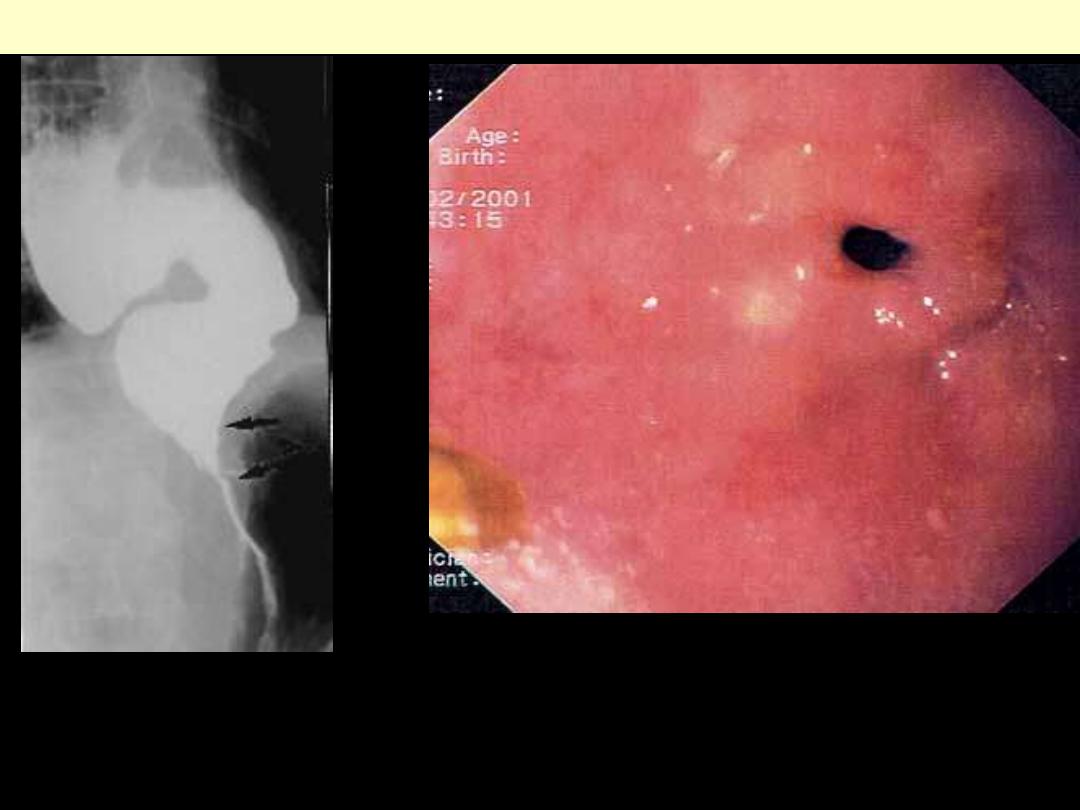
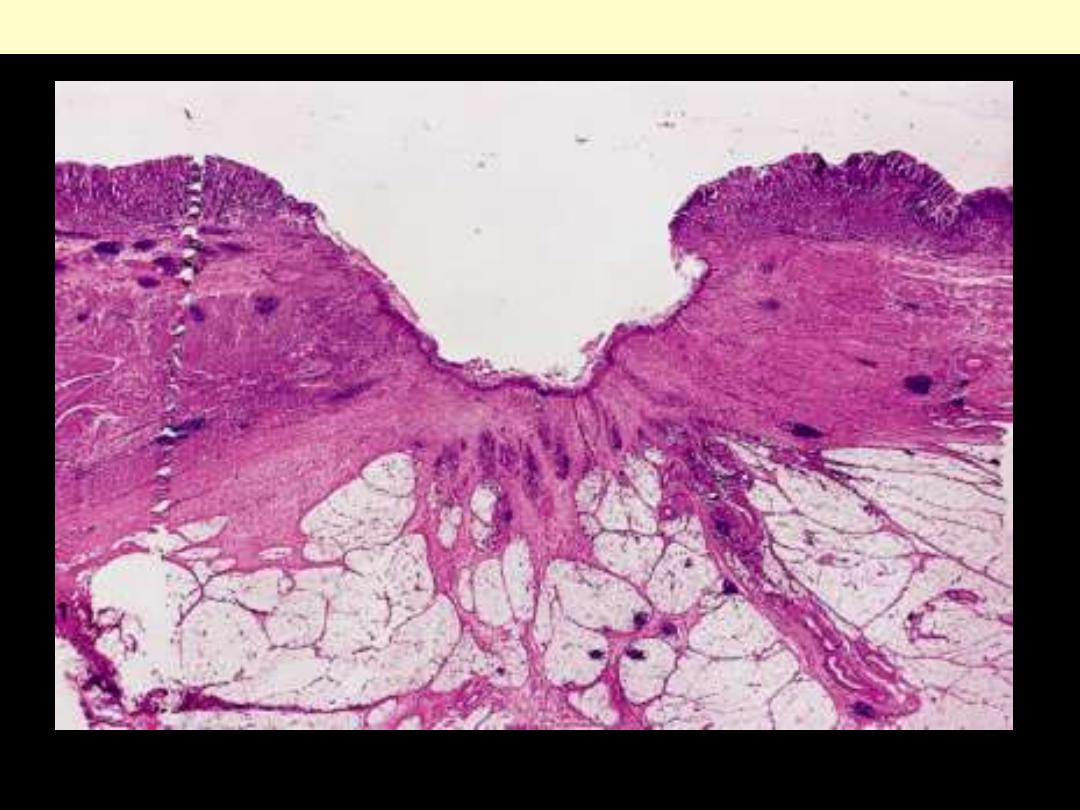
Mallory-Weiss tear
This is a tear in the mucosal layer at the
junction of the esophagus and stomach
Image demonstrates a thin, linear tear
(arrow) beginning just above the
squamocolumnar junction and extending
proximally.
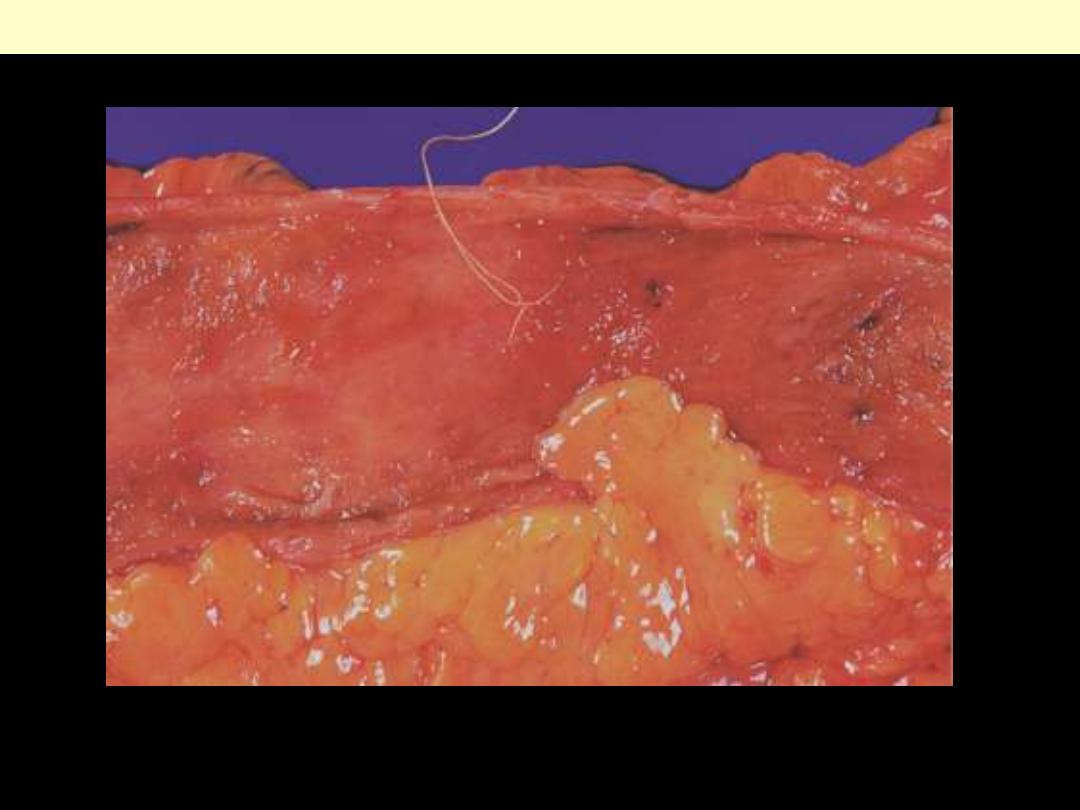
Esophageal lacerations (Mallory-Weiss syndrome)
Gross photograph demonstrating longitudinal lacerations oriented in the axis of the esophageal lumen
(
arrow
), extending from the esophageal mucosa to the stomach mucosa.
Esophageal
mucosa
Gastric
mucosa
Esophagus - tumors
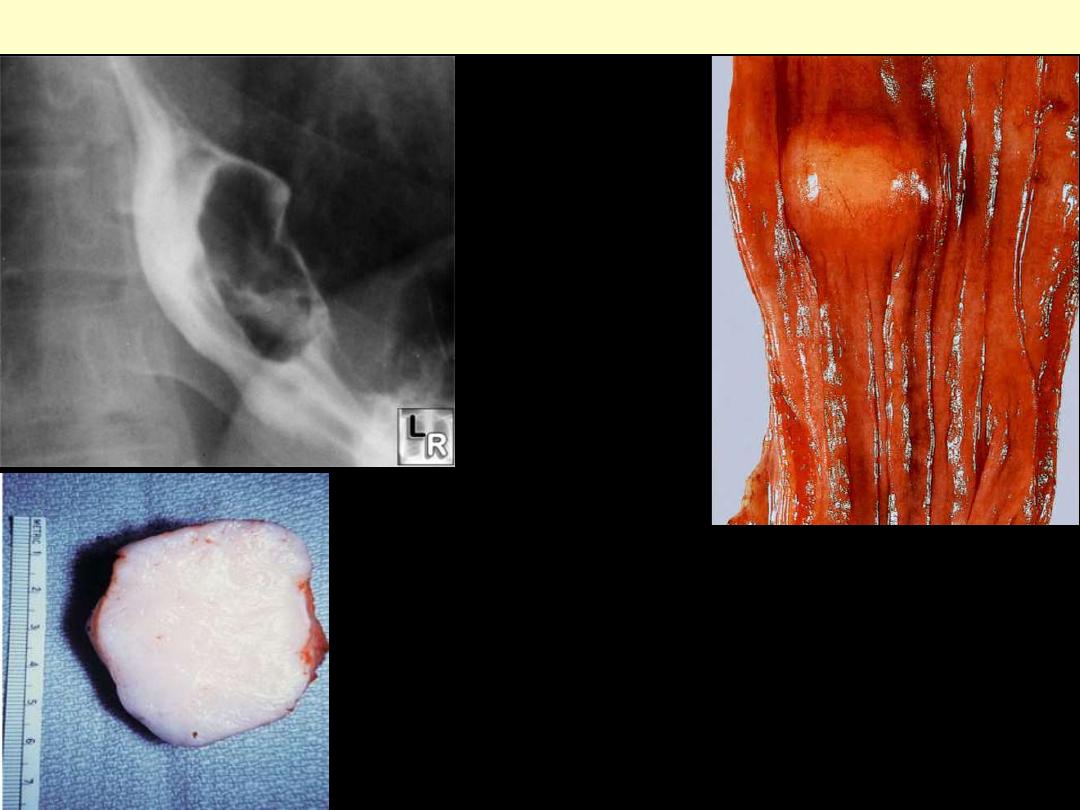
Leiomyoma esophagus
The sharply circumscribed tumor has a white
color and elastic consistency.
The mucosa over the tumor is
intact.
Barium meal
Esophageal leiomyoma
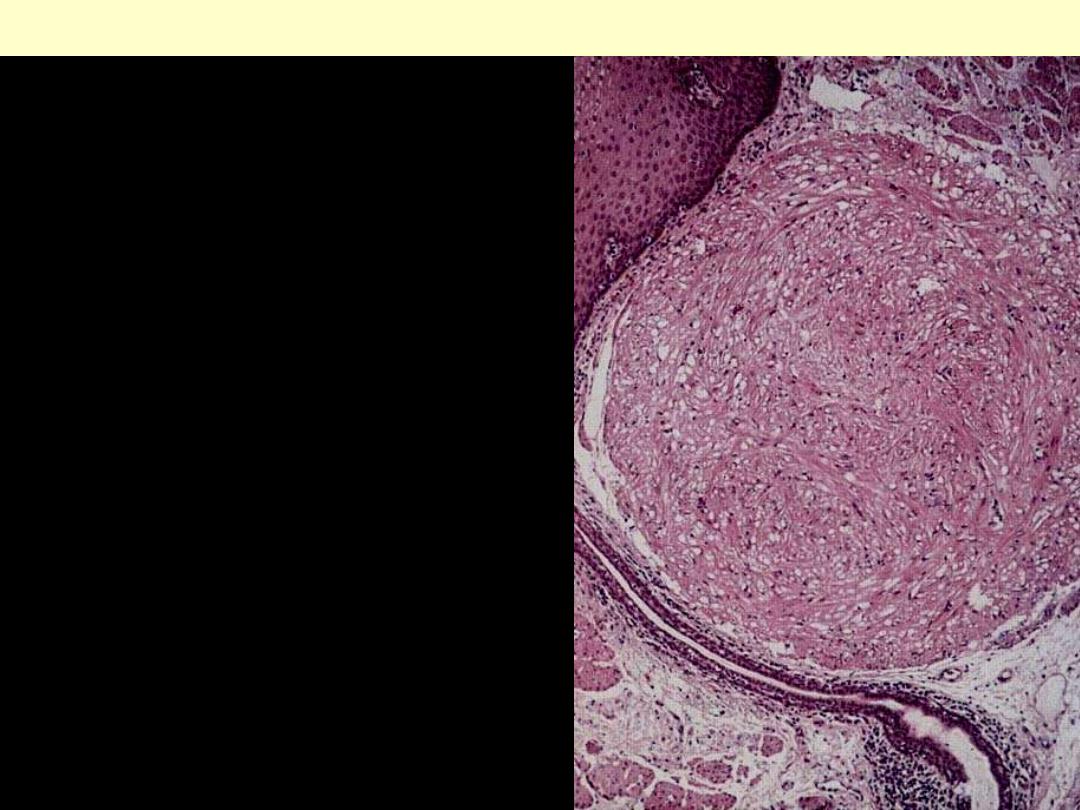
The sharply circumscribed tumor consists of
interlacing bundles of spindled smooth muscle
cells.
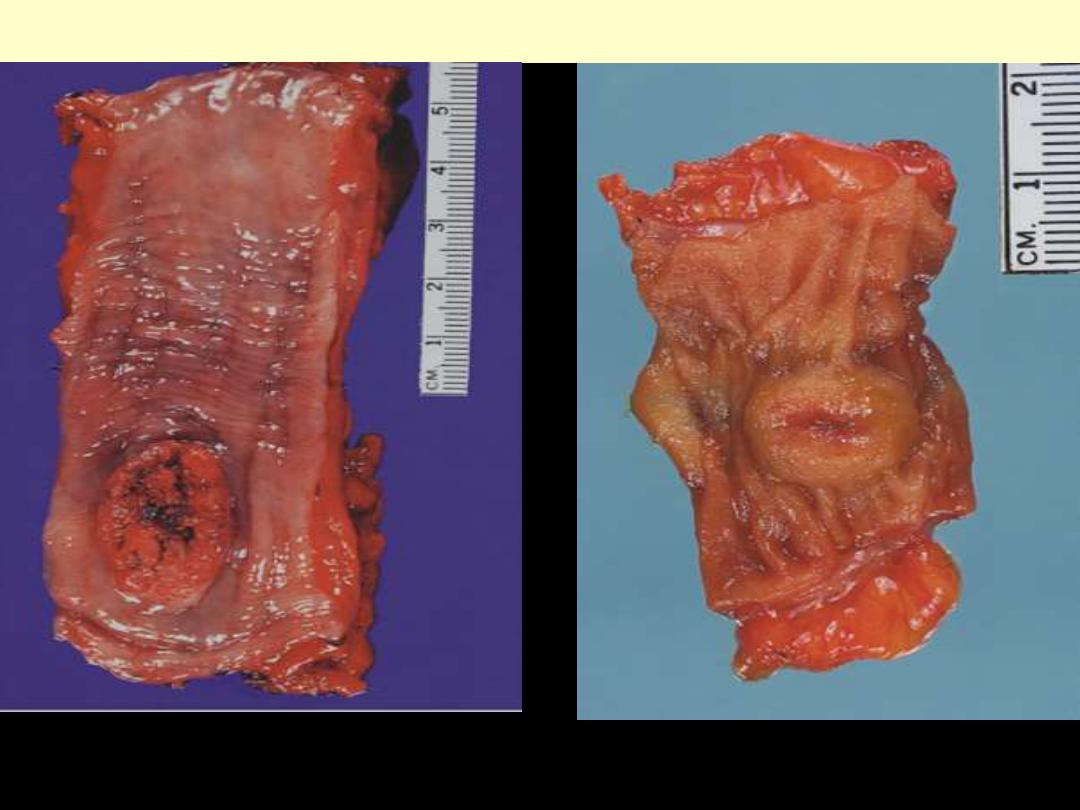
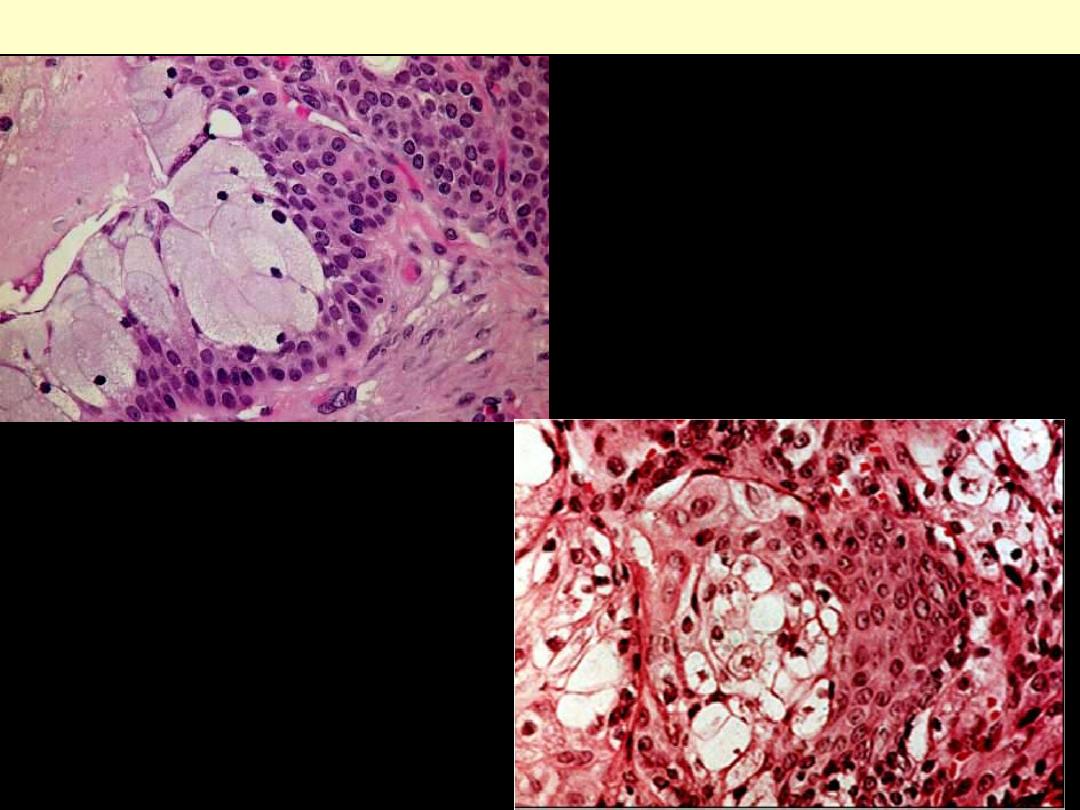
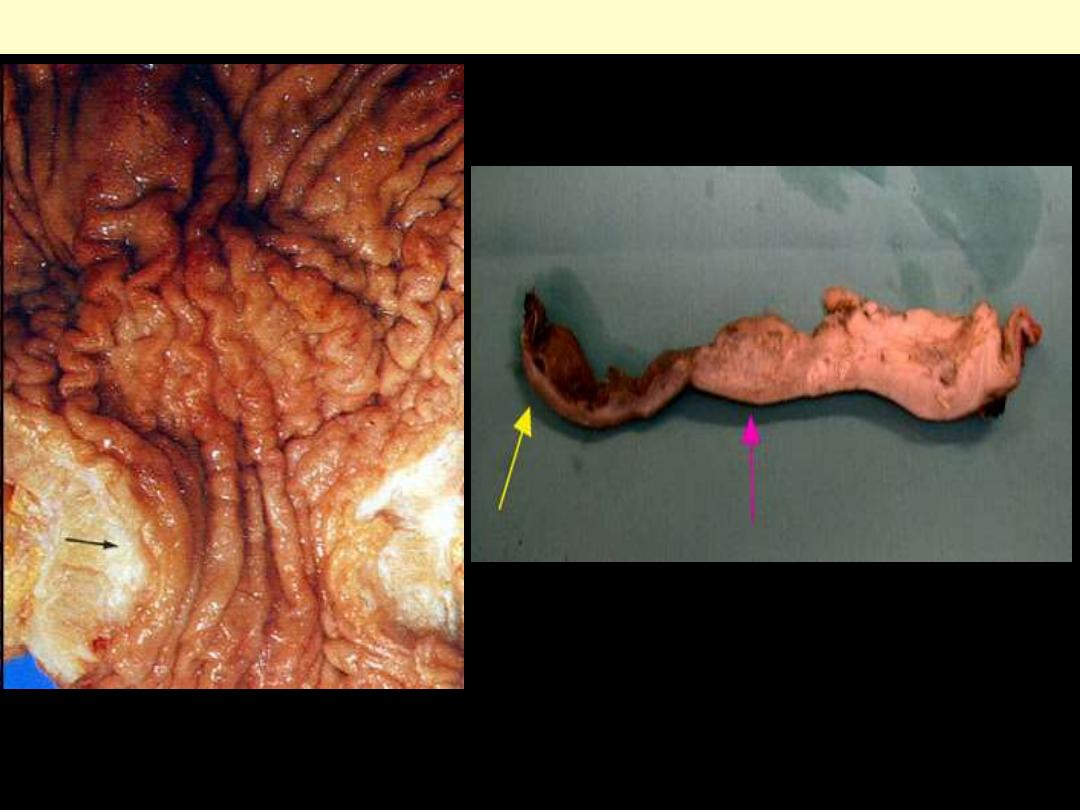
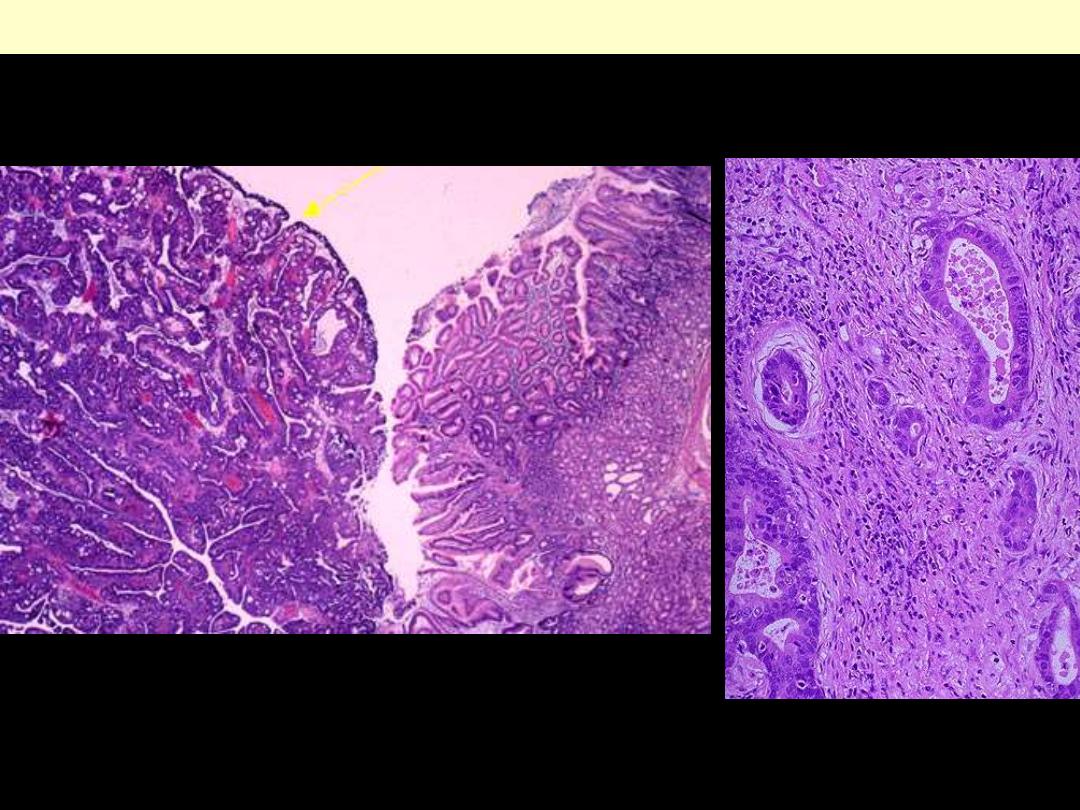
Squamous cell ca esophagus Exophytic
Cake-like exophytic mass.
Elevated round nodule with central
ulceration.

Circumferential constricting region.
Widely invasive lesion with deep
ulceration.
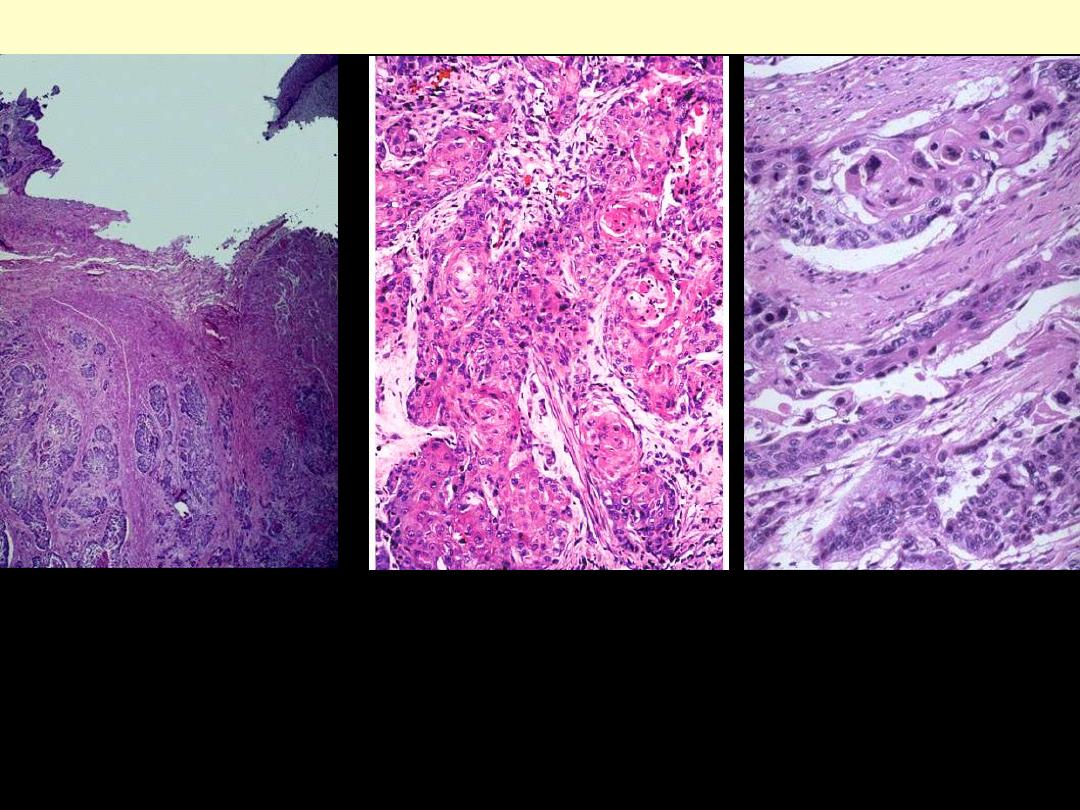
At the upper right is a remnant of
squamous esophageal mucosa that
has been undermined by an
infiltrating SCC. Nests of
neoplastic squamous epithelium
are infiltrating through the
submucosa at the right.
At high power, these infiltrating
nests of neoplastic cells have
abundant pink cytoplasm and
distinct cell borders typical for
squamous cell carcinoma.
squamous cell carcinoma esophagus
Invasive, moderately well
differentiated squamous cell
carcinoma of the esophagus.
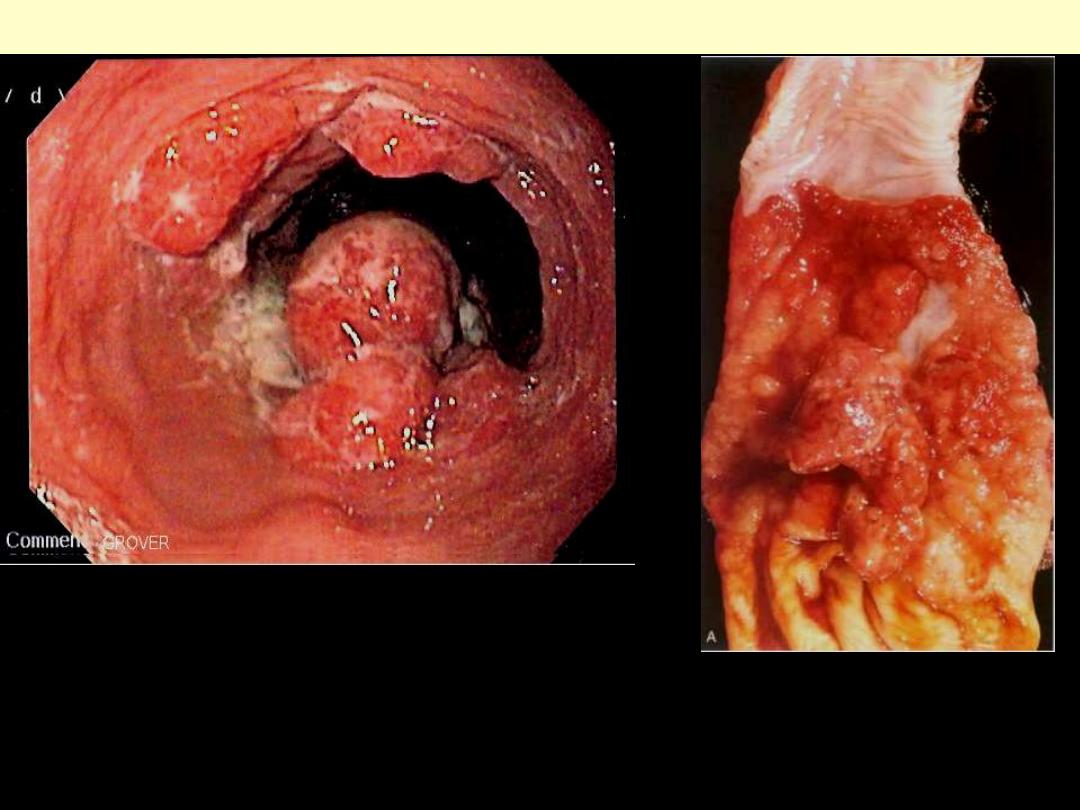
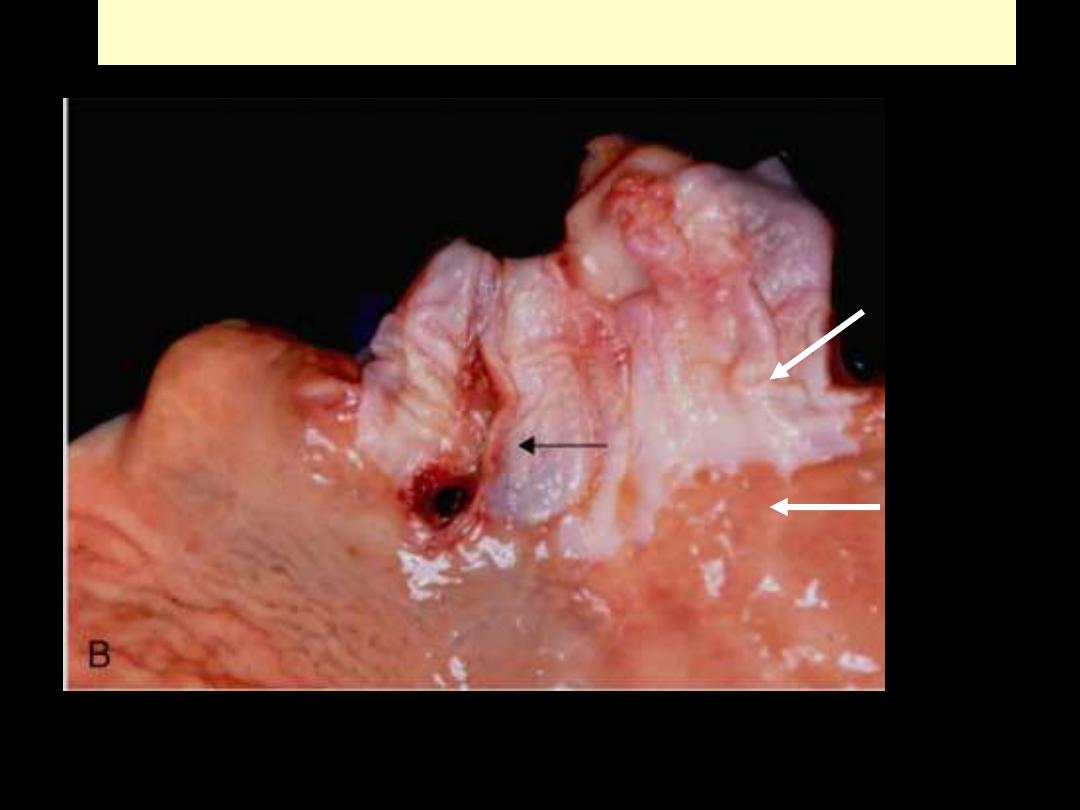
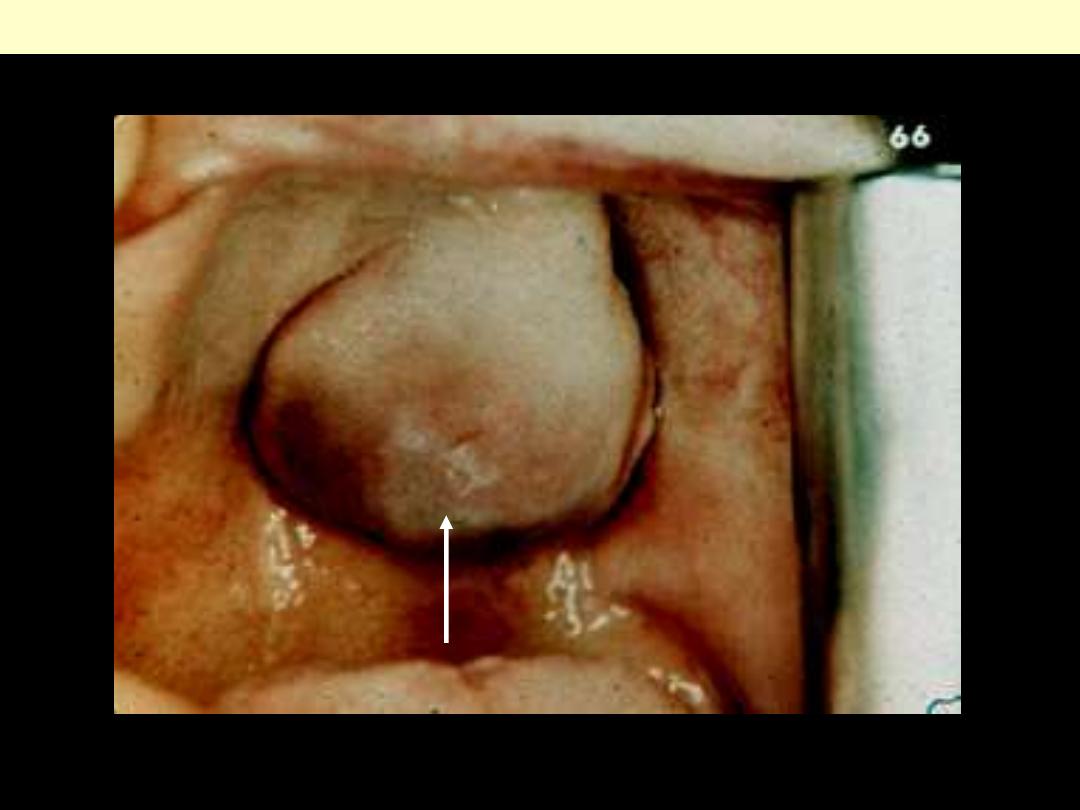
Adenocarcinoma esophagus exophytic
Gross view of an ulcerated, exophytic
mass at GE junction, rising from the
grnular mucosa of BE. The gray-white
esophageal mucosa is on the top, and
the folds of gastric mucosa are below.
Adenocarcinoma presenting as a polypoid growth.
Endoscopic view
Low & high power views of adenocarcinoma
Adenocarcinoma esophagus
Esophagus - Varices
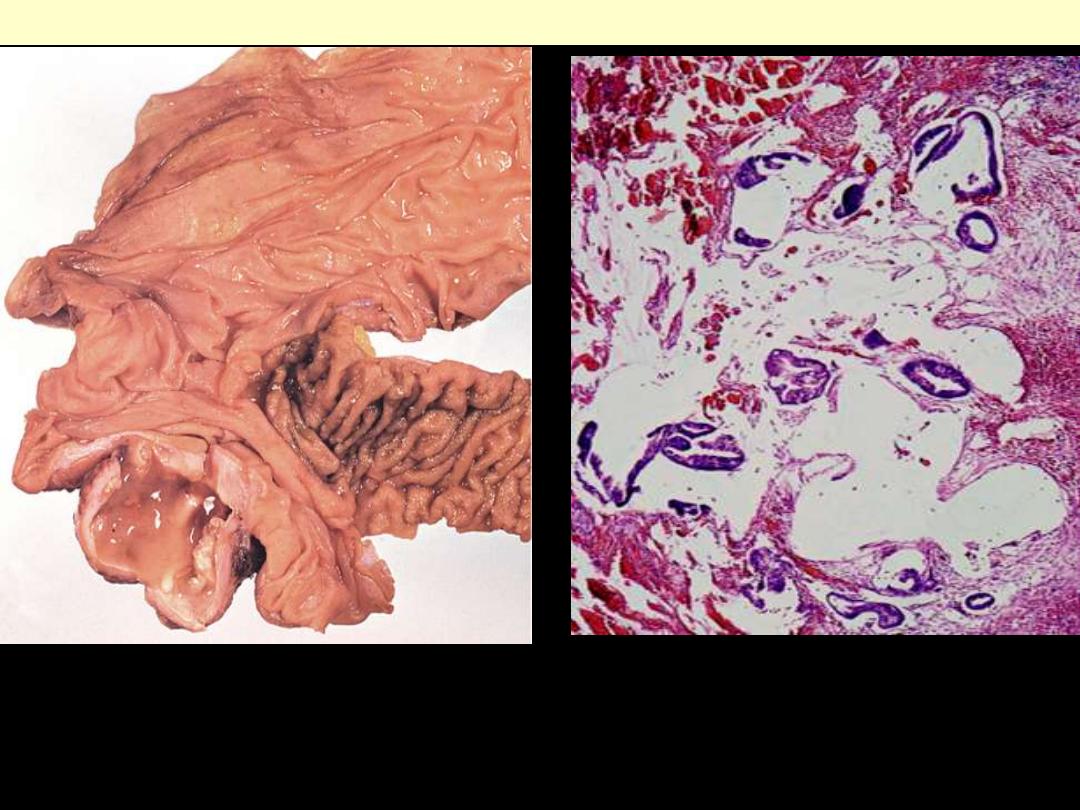
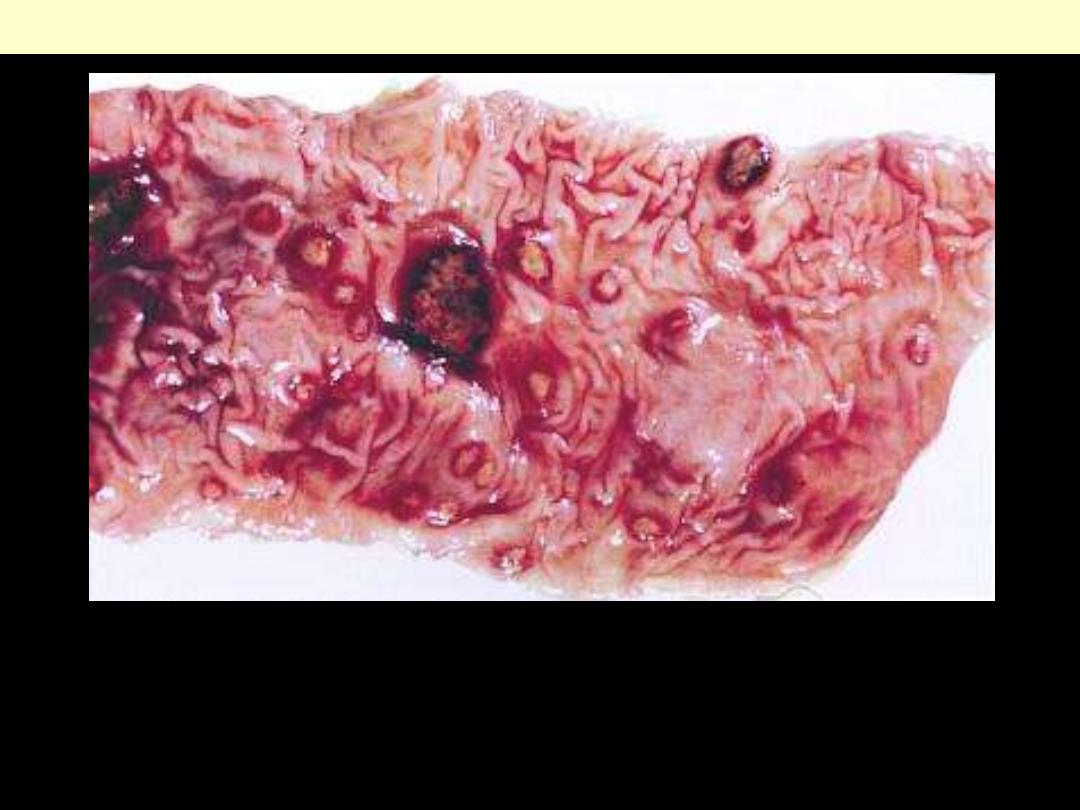
Esophageal varices
Tortuous dilated veins of the distal esophagus pushing the mucosa ahead & thus causing irregular
protrusion of the latter into the lumen. Variceal rupture produces massive hemorrhage into the lumen.
In this instance, the overlying mucosa appears ulcerated and necrotic.
Intestine
Appendix - appendicitis

This is acute appendicitis with yellow to tan exudate and hyperemia, including the periappendiceal fat
superiorly, rather than a smooth, glistening pale tan serosal surface.
Acute appendicitis
Acute appendicitis
Outer aspect of appendix involved by acute inflammation. A thick purulent coating is seen together
with marked hyperemia of the serosa.

This is the tip of the appendix from a patient with acute appendicitis. The appendix has been sectioned
in half. The serosal surface at the left shows a tan-yellow exudate. The cut surface at the right
demonstrates yellowish-tan mucosal exudation with a hyperemic border.
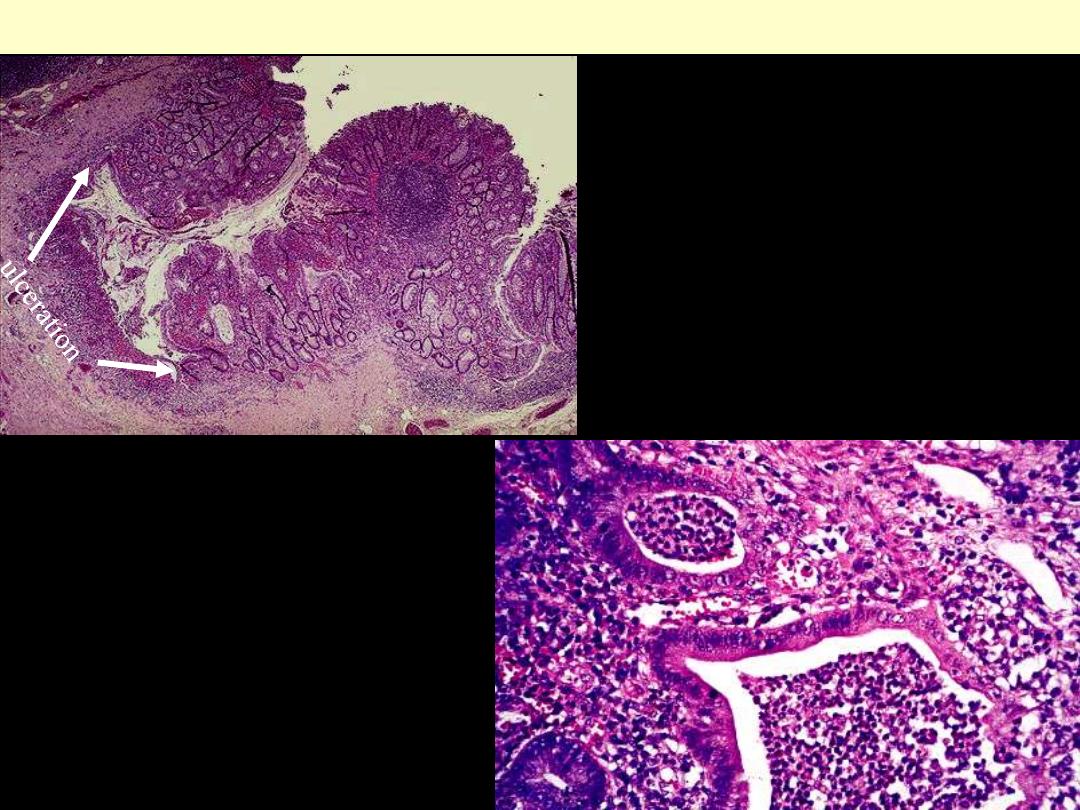
Acute appendicitis
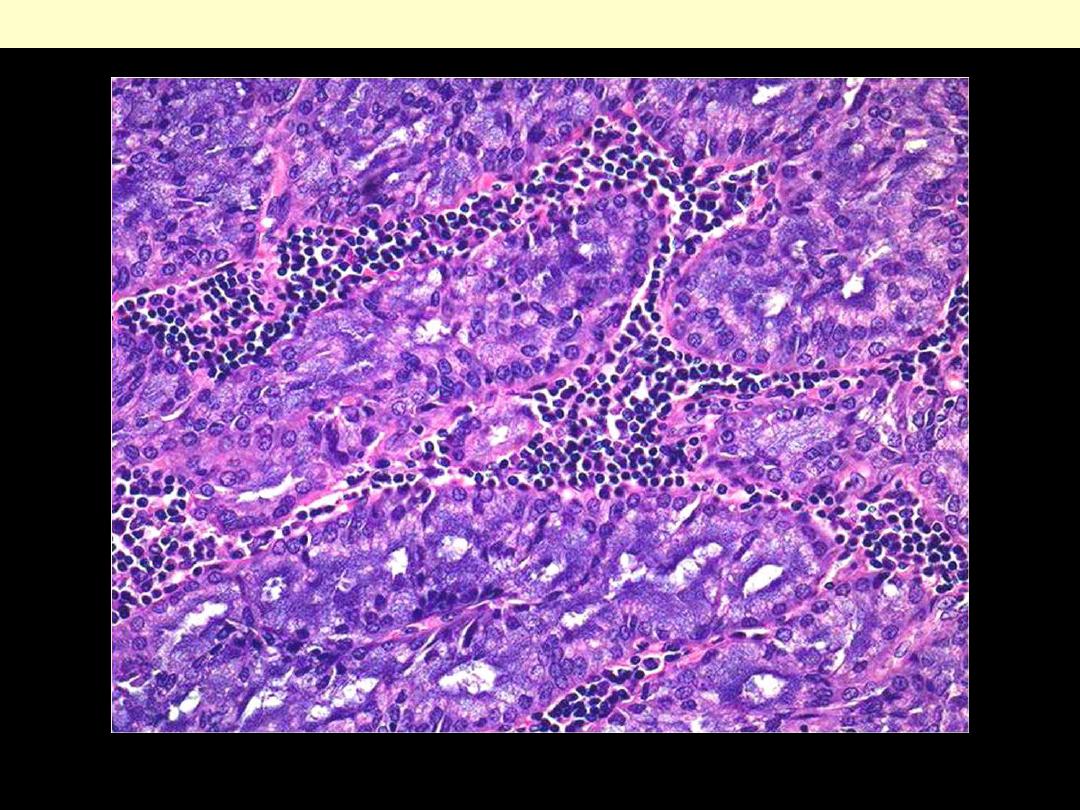
acute appendicitis is marked by mucosal
inflammation and necrosis.
the mucosa shows ulceration and
undermining by an extensive neutrophilic
exudate.
Neutrophils extend into and through the
wall of the appendix
This view shows acute inflammation (neutrophils) in the muscular wall of the appendix - the hallmark
of acute appendicitis.
Appendix - tumors
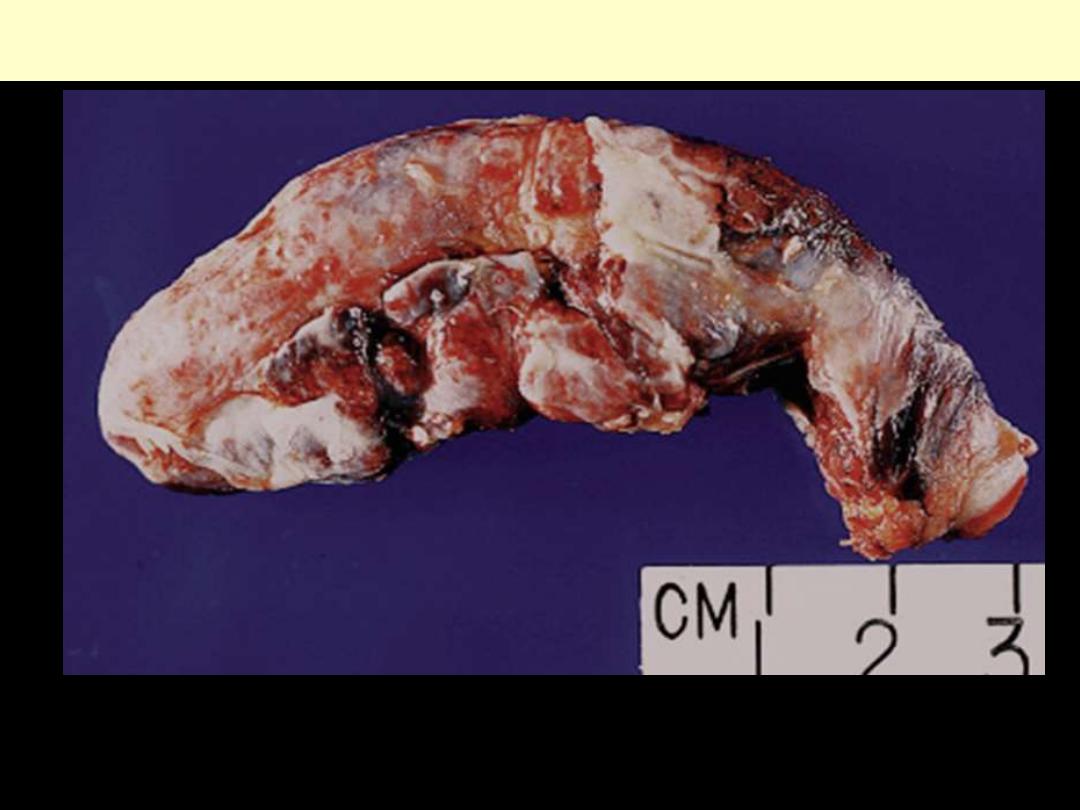
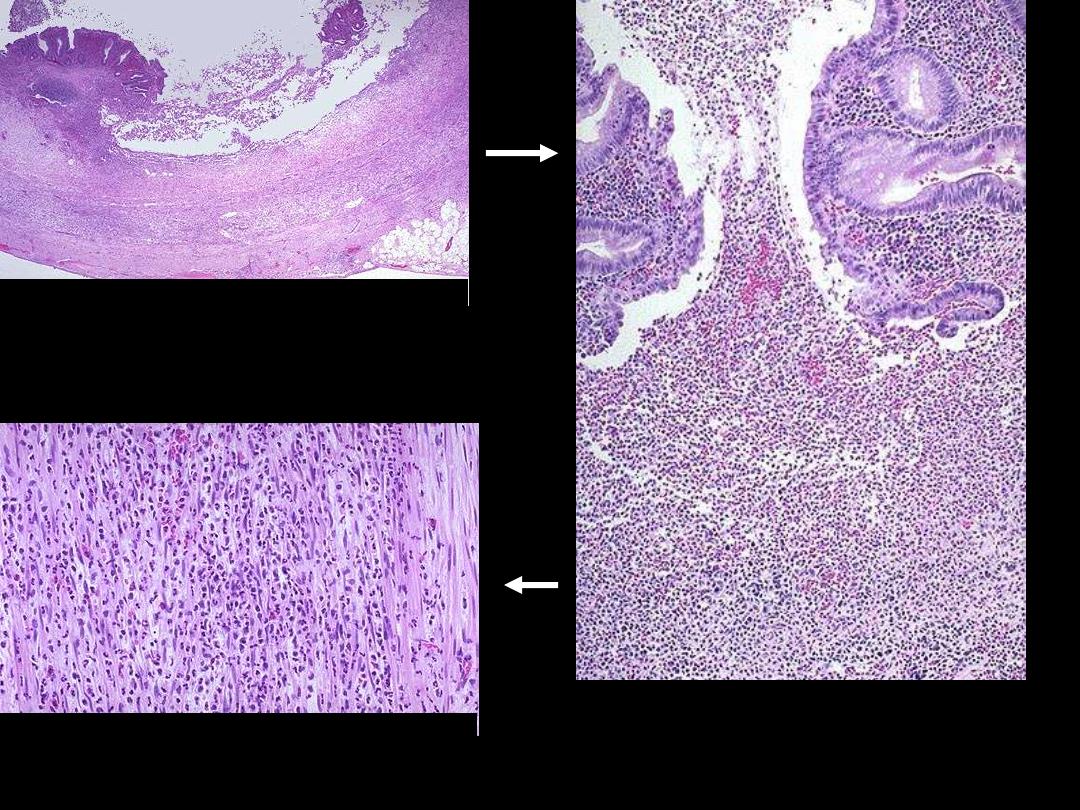
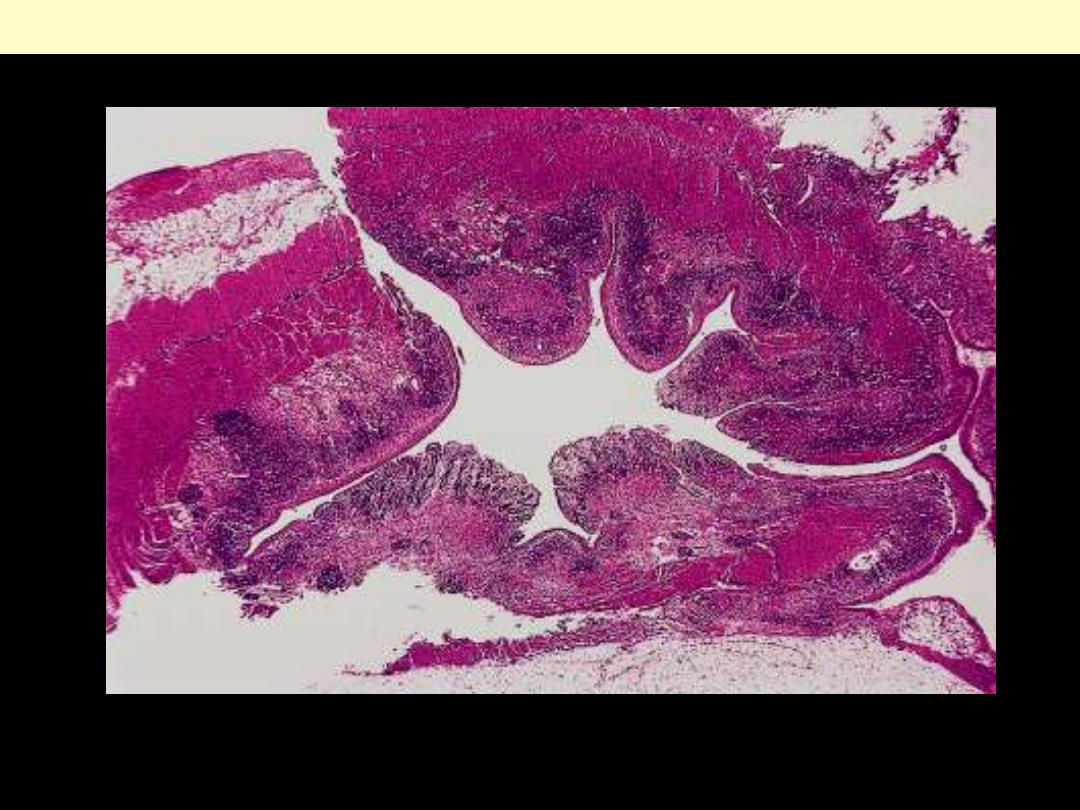
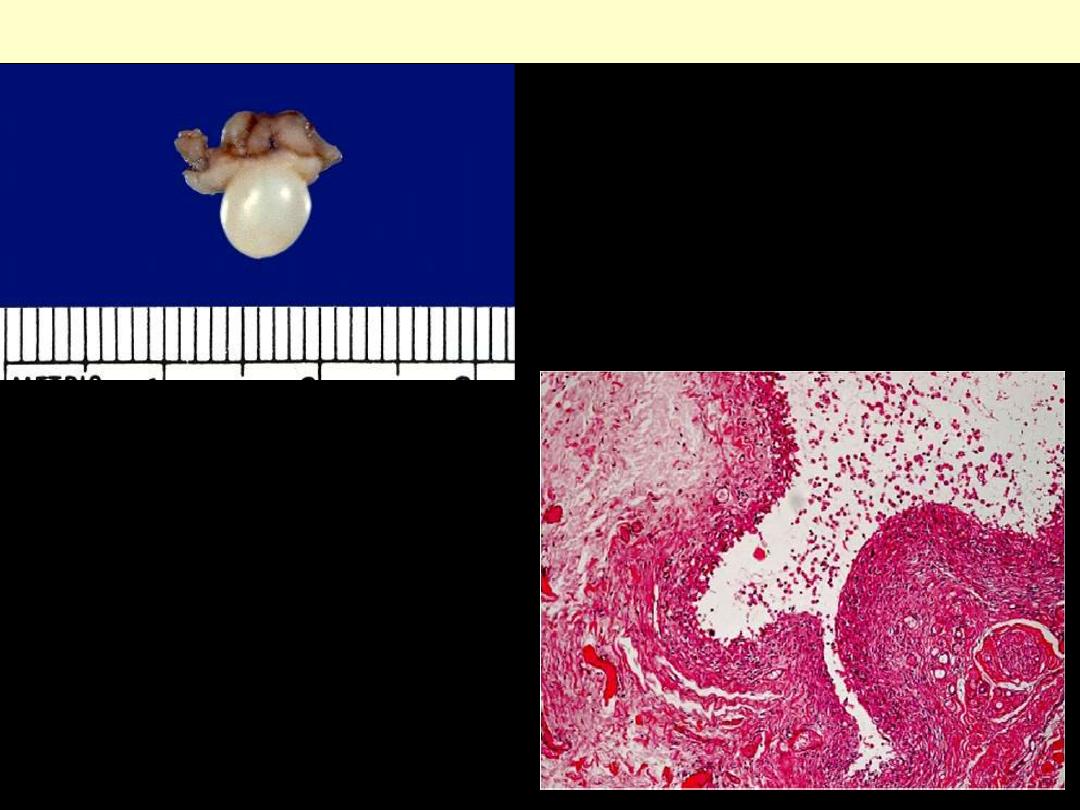
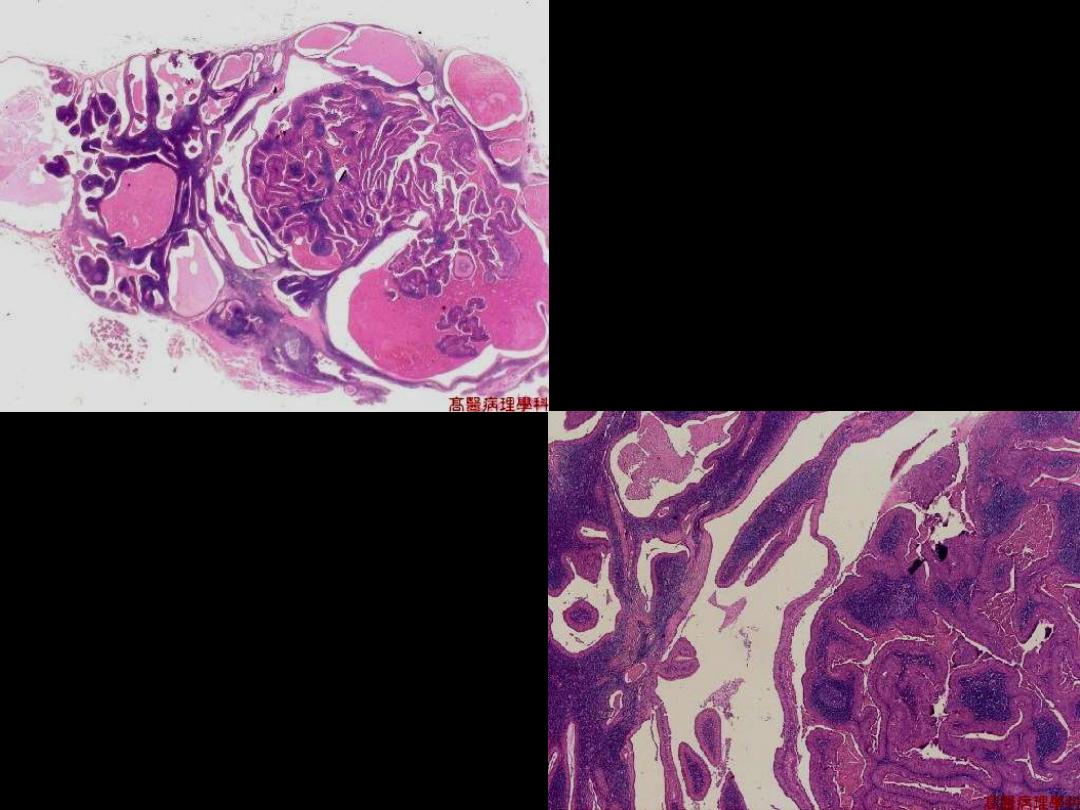
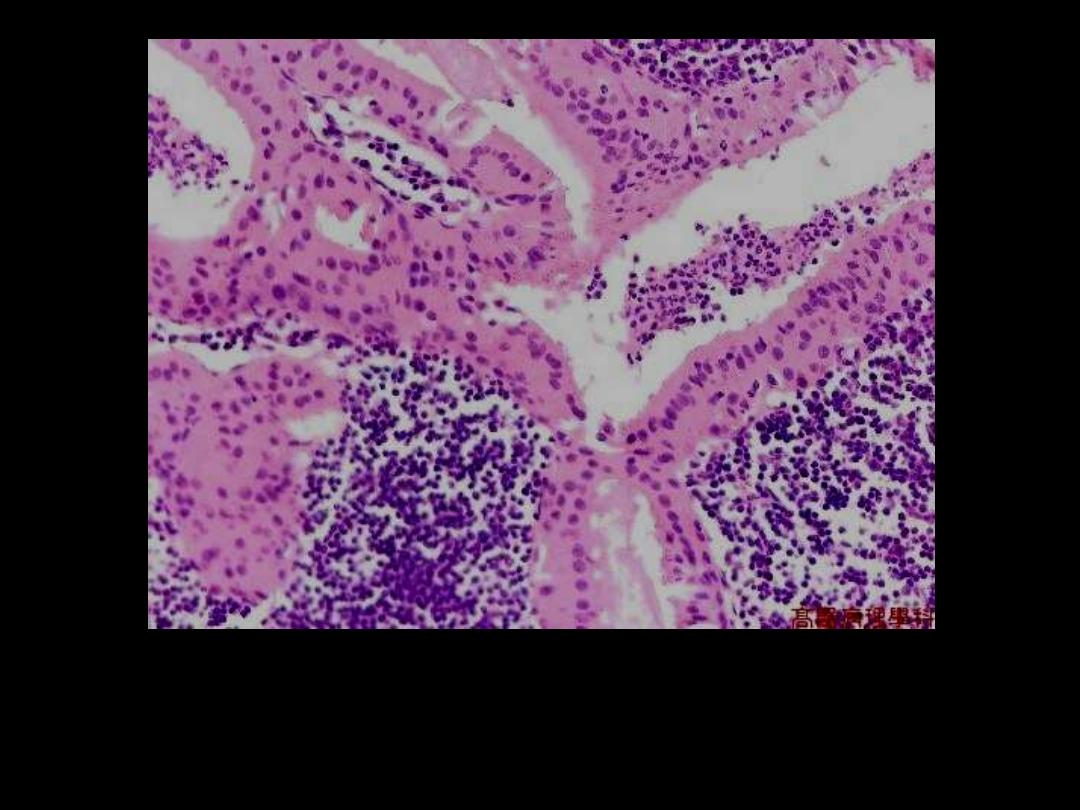
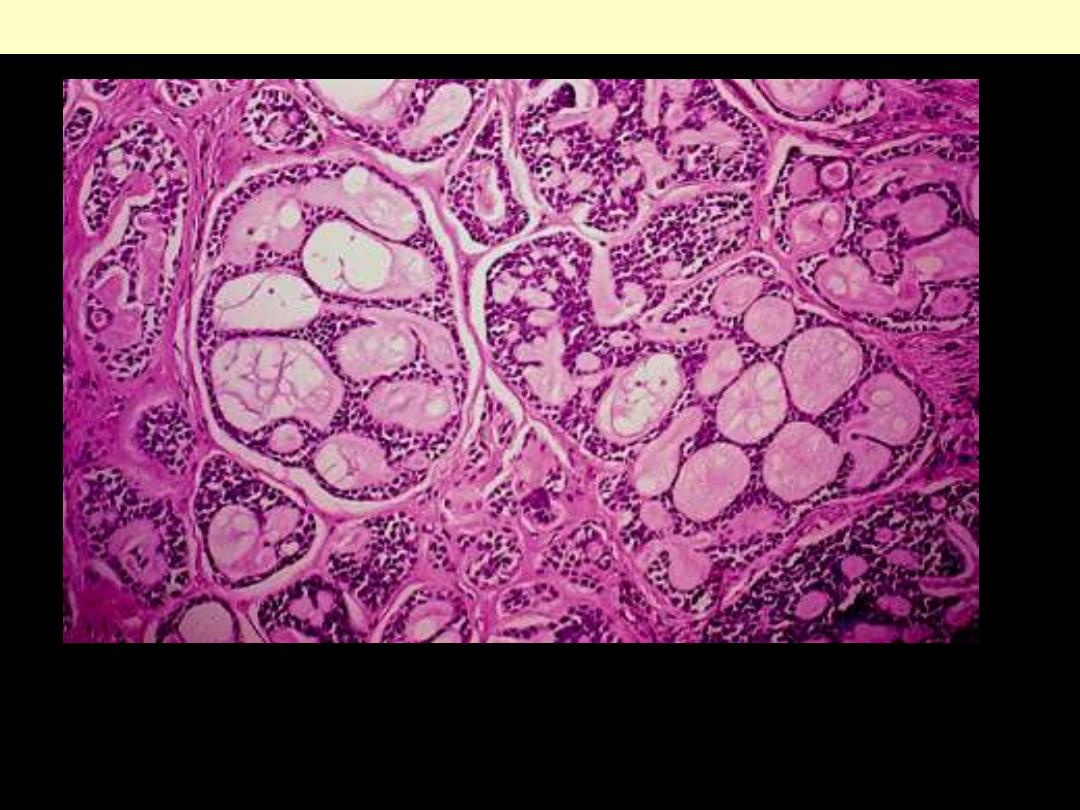
Mucinous cystadenocarcinoma appendix G
Mucinous cystadenocarcinoma of appendix.
The tumor is grossly indistinguishable from a
mucinous cystadenoma.
Pseudomyxoma peritonei. The diagnosis is made by
the presence of well-differentiated glandular
epithelium, admixed with extracellular mucin.
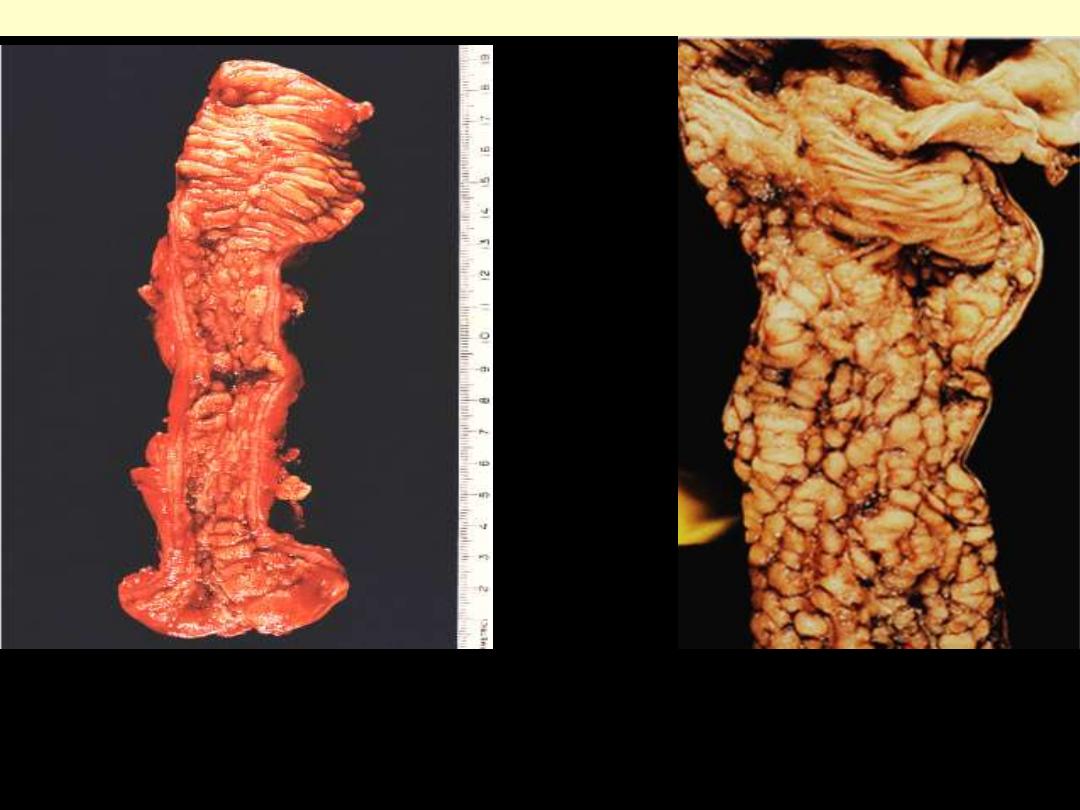
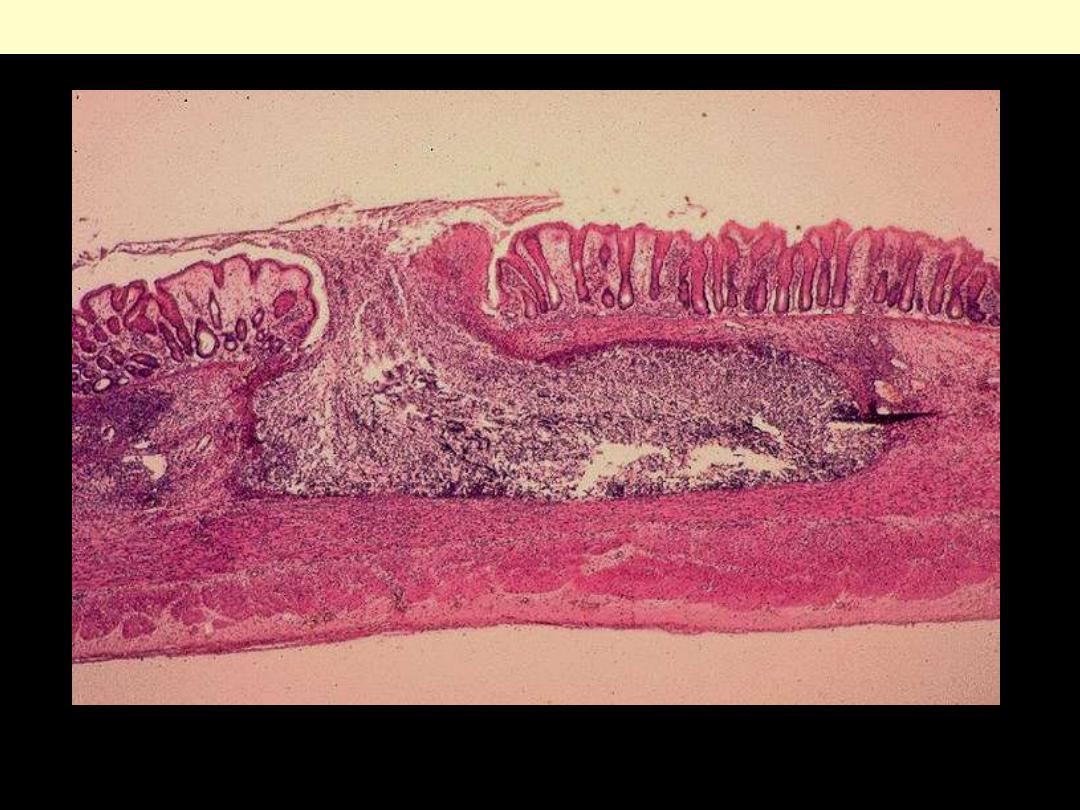
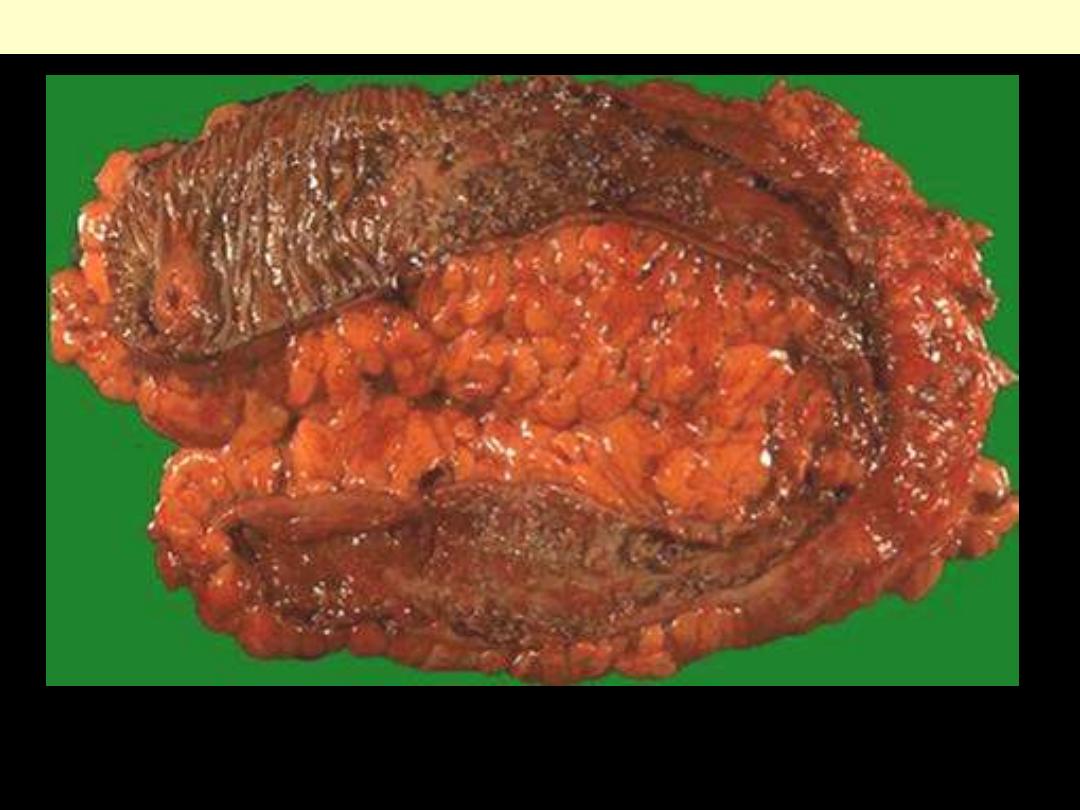
Intestine - CD
This portion of terminal ileum demonstrates the gross
findings with Crohn's disease. The middle portion has
a
thickened wall and the mucosa has lost the regular
folds.
The serosal surface demonstrates reddish
indurated adipose tissue that creeps over the surface.
Serosal inflammation leads to adhesions. The areas of
inflammation tend to be discontinuous throughout the
bowel.
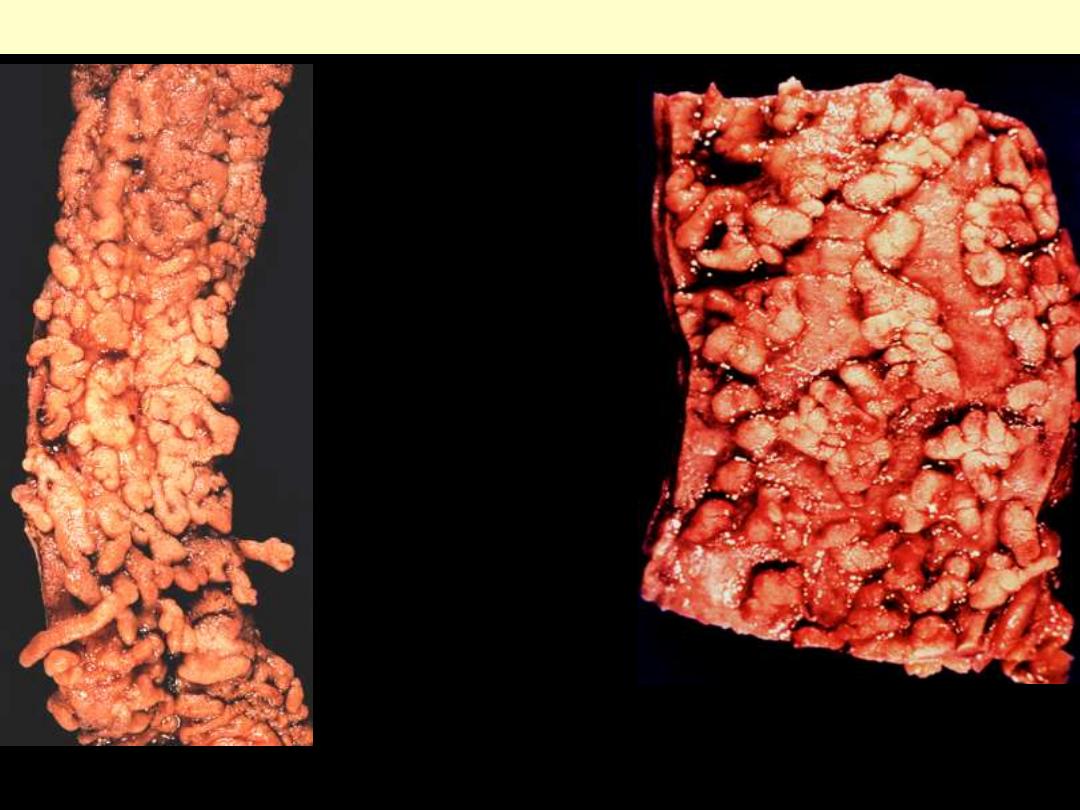
Crohn's disease, terminal ileum, G
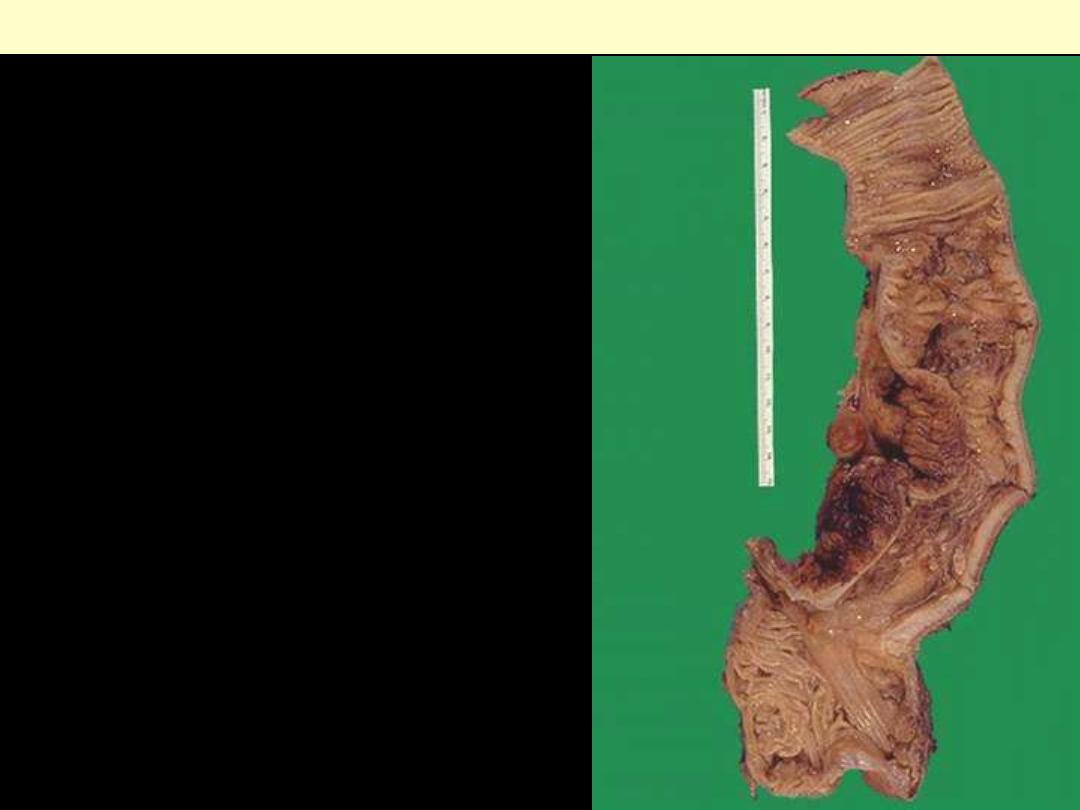
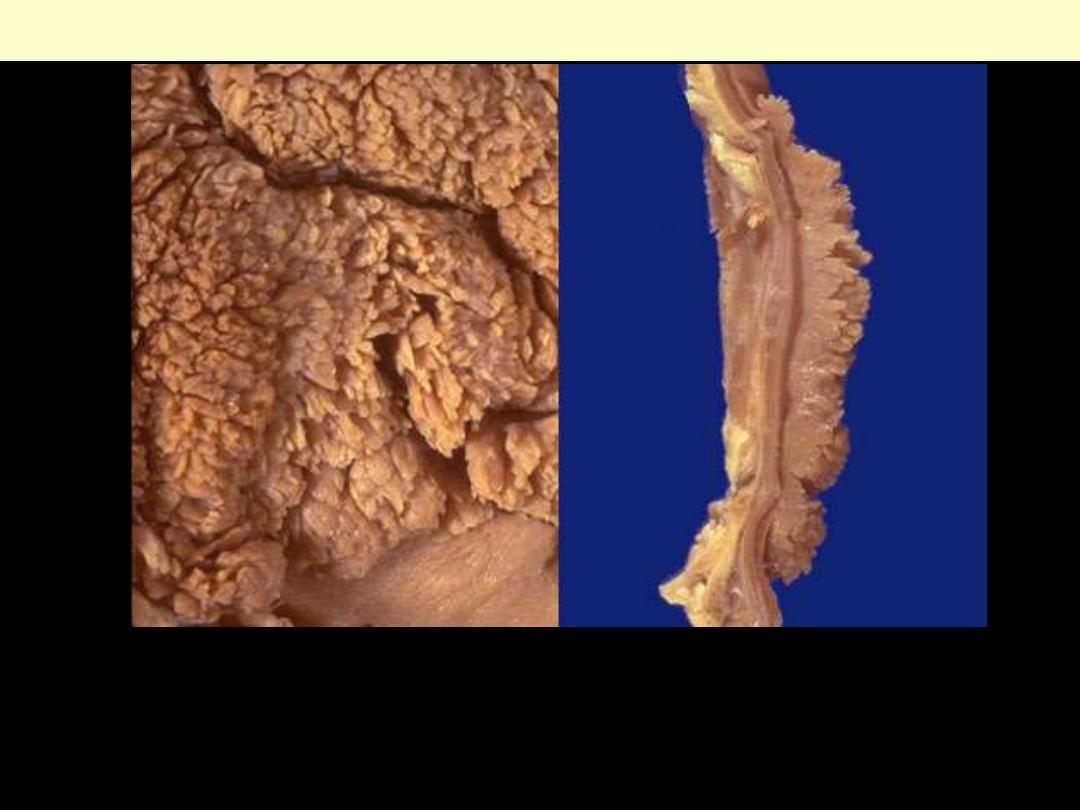
Crohn’s disease Small intestine
Gross appearance of Crohn’s disease. Note
the
segmental nature
of the inflammation,
and rigidity of the wall, and
cobble-stoning
of
the mucosa are characteristic.
Another example of
cobblestone
appearance.
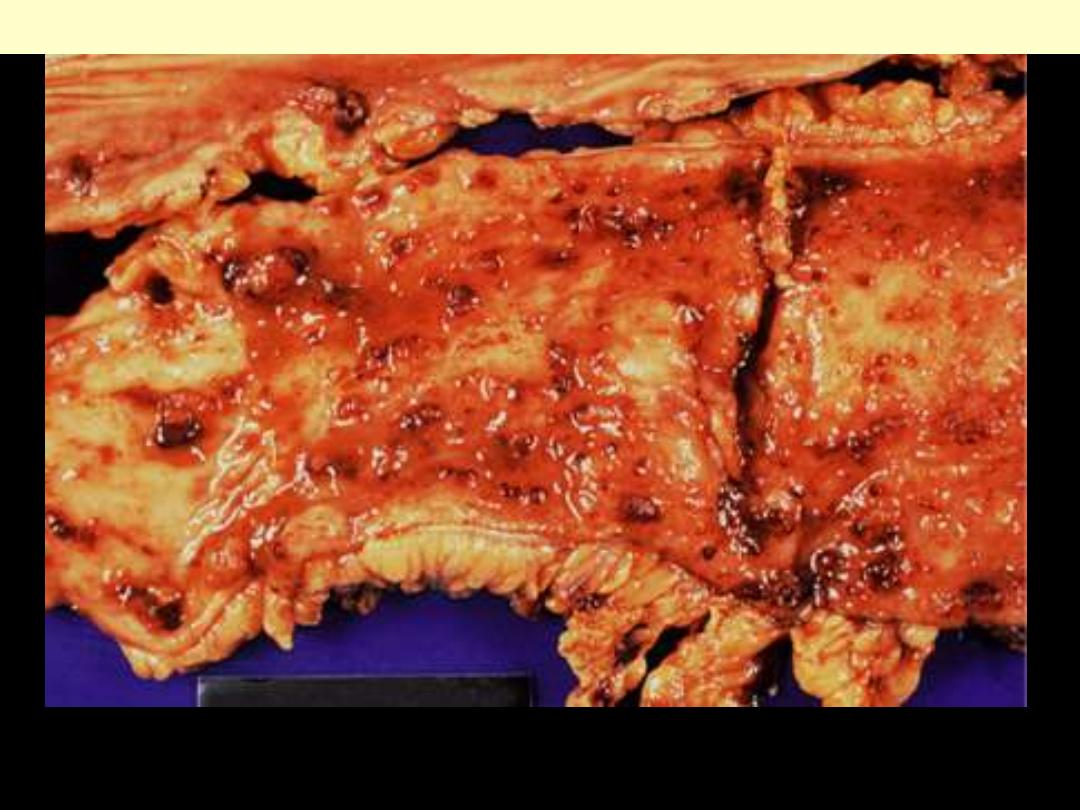
Crohn’s disease colon gross
Gross appearance of Crohn's
disease of large bowel; segmental
distribution
Gross appearance of Crohn’s disease of large bowel showing
typical cobblestone appearance.
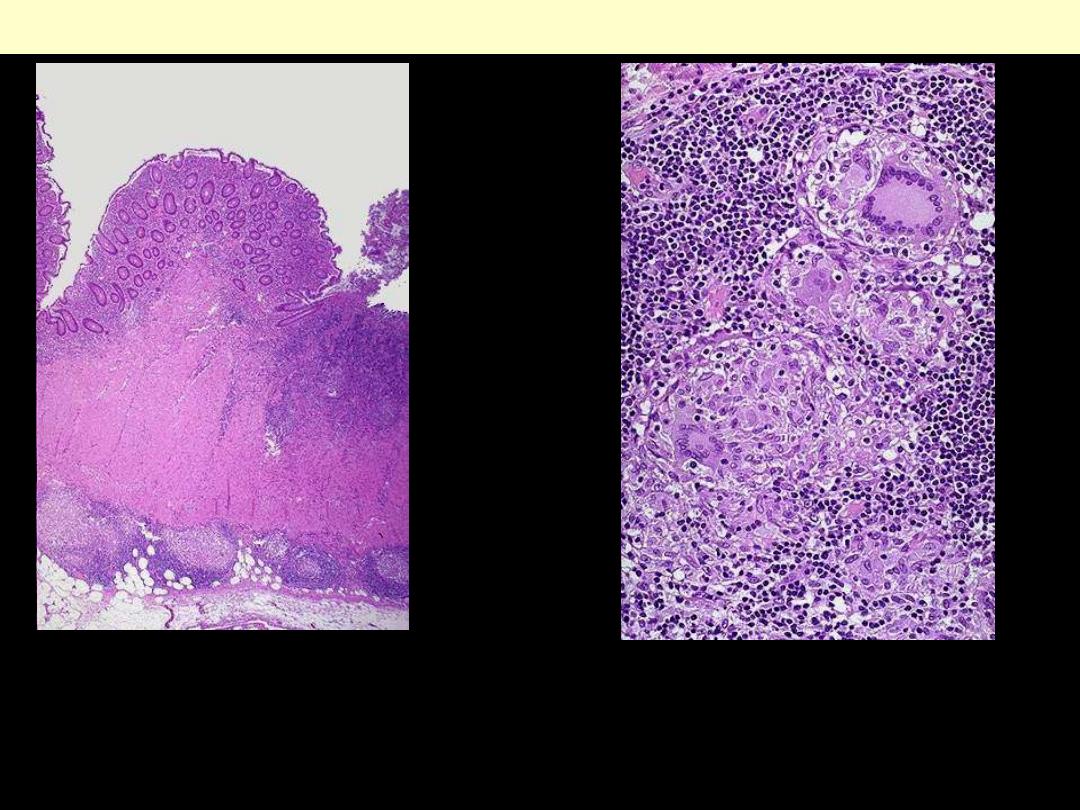
Crohn's disease appendix
There is transmural inflammation that is predominant in the mucosa and submucosa.
One complication of Crohn's disease is fistula formation. Seen here is a
fissure
extending through
mucosa at the left into the submucosa toward the muscular wall, which eventually will form a fistula
.
Fistulae can form between loops of bowel, bladder, and skin. With colonic involvement, perirectal
fistulae are common. There is also intense inflammation of the mucosa and submucosa.
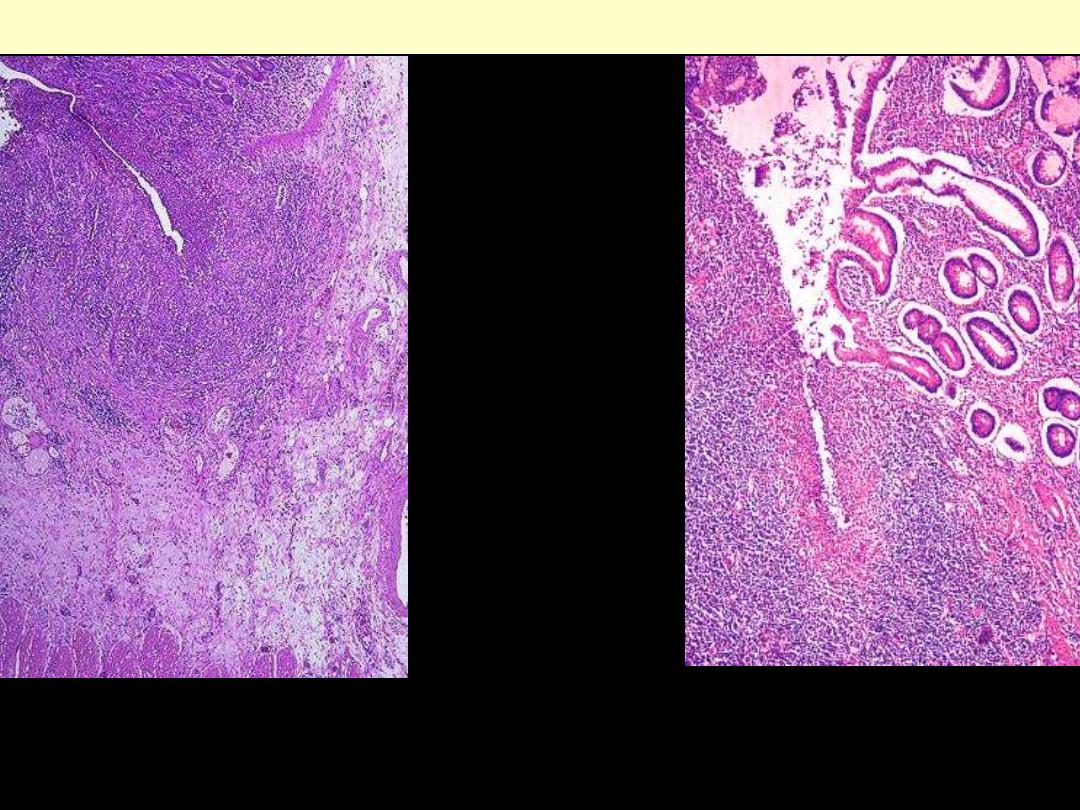
Crohn’s disease colon
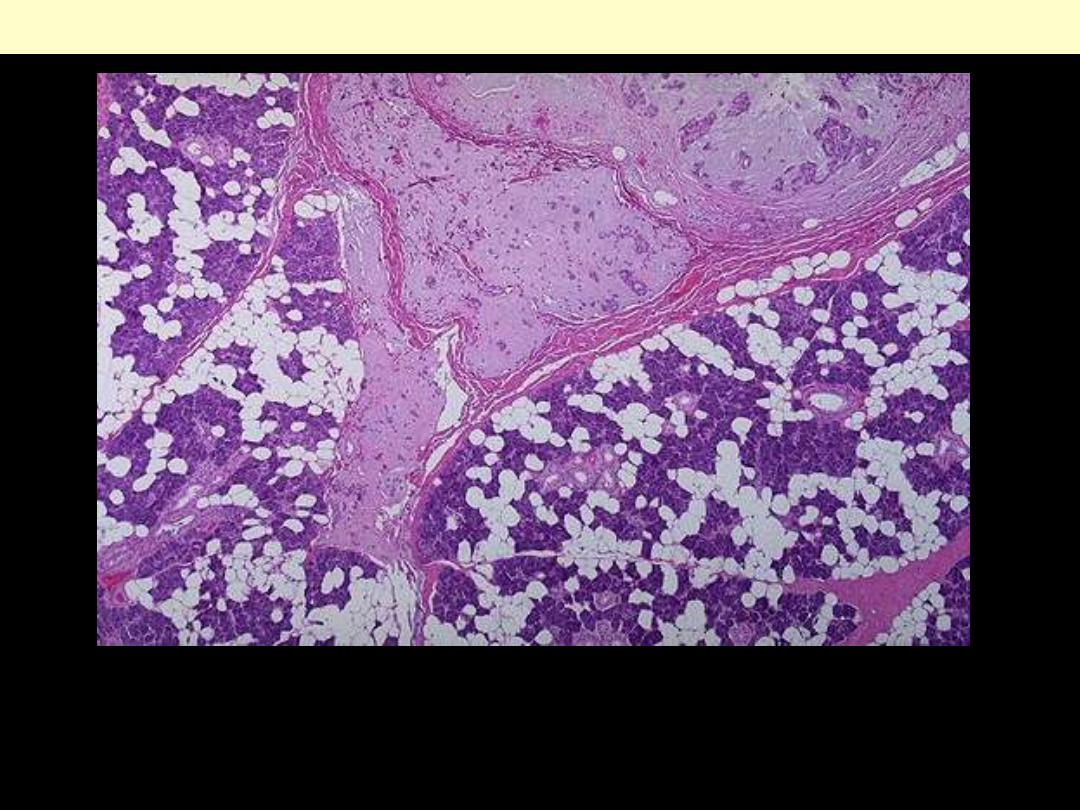
Microscopically, Crohn's disease is characterized
by transmural inflammation. Here, inflammatory
cells (the bluish infiltrates) extend from mucosa
through submucosa and muscularis and appear as
nodular infiltrates on the serosal surface with pale
granulomatous centers.
Crohn’s disease colon
At high magnification the granulomatous nature of the
inflammation of Crohn's disease is demonstrated here
with epithelioid cells, giant cells, and many
lymphocytes. Special stains for organisms are negative.
Intestine - enterocolitis
Pseudomembranous colitis
This is an example of pseudomembranous enterocolitis. The mucosal surface of the colon seen here is
hyperemic and is partially covered by a yellow-green exudate. The mucosa itself is not eroded.

Pseudomembranous colitis
There are multiple, discrete white plaques of
purulent exudate on the mucosal surface.
The patient was taking ampicillin.
Pseudomembranous colitis
Neutrophils in lamina
propria
Superficial damaged crypts
distended by a mucopurulent
exudate
mushrooming or volcano
cloud
Eruption
Postmortem specimen of small intestine. There are multiple
oval ulcers running transversely across the bowel (arrows).
The patient died from untreated disseminated tuberculosis.
Intestinal TB
• Characteristic rounded, slightly elevated areas of the mucosa with irregular yellow necrotic centers
surrounded by edematous hyperemic tissue. Some times Hgic centres
• The intervening mucosal folds have a mostly normal appearance, although one segment is congested
and edematous.
Amebic colitis
Amebic colitis
There is characteristic flask shaped ulcer extending into the submucosa
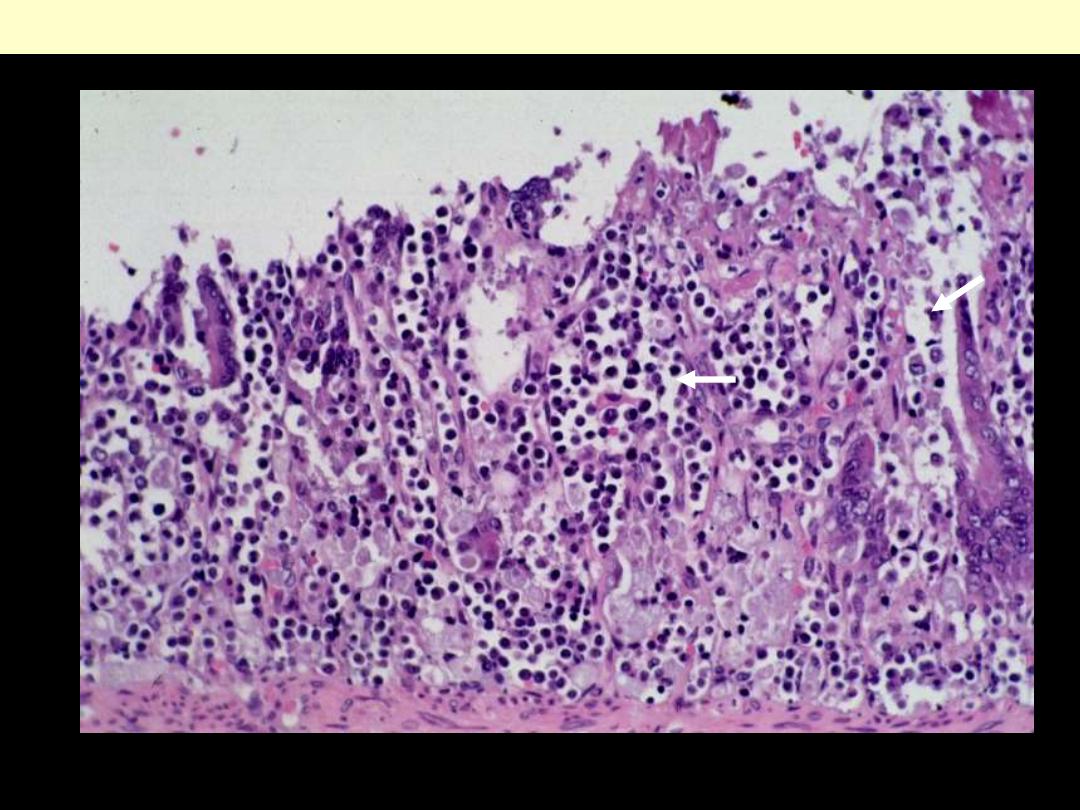
Amebic colitis
Numerous ameba trophs causing lysis (histolytica) of the mucosa. Trophs are pale stained;
Inflammatory cells dark stained
Amebic colitis
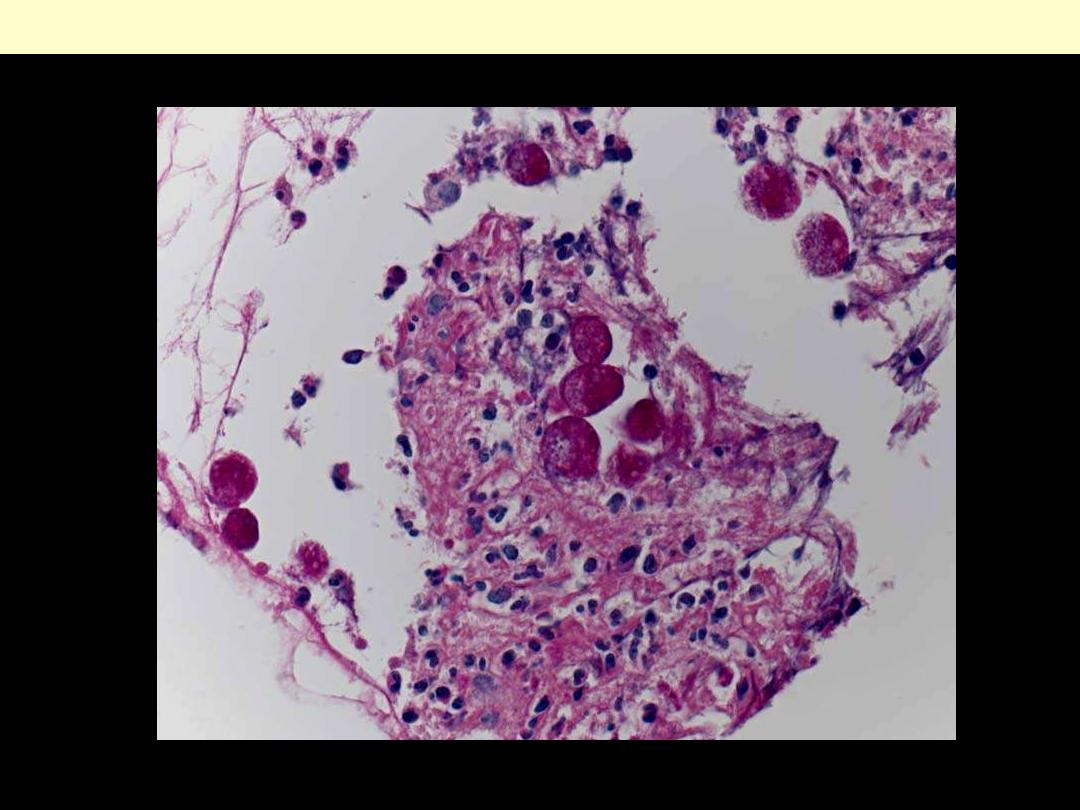
Amebae are round PAS positive organisms. Stain PAS
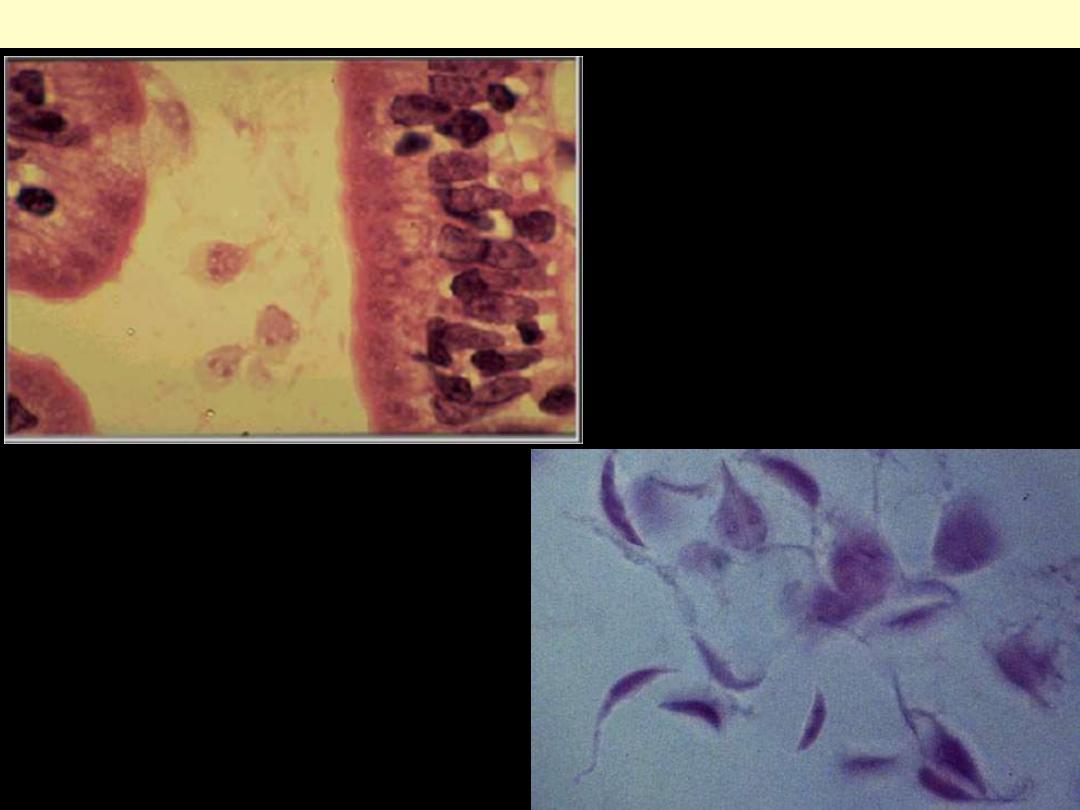
Giardia lamblia
Giardia lamblia infection of the small intestine.
The
small pear-shaped trophozoites
live in the
duodenum and become infective cysts that are
excreted. They produce a watery diarrhea. A
useful test for diagnosis of infectious diarrheas is
stool examination for ova and parasites.
Intestine - hemorrhoids
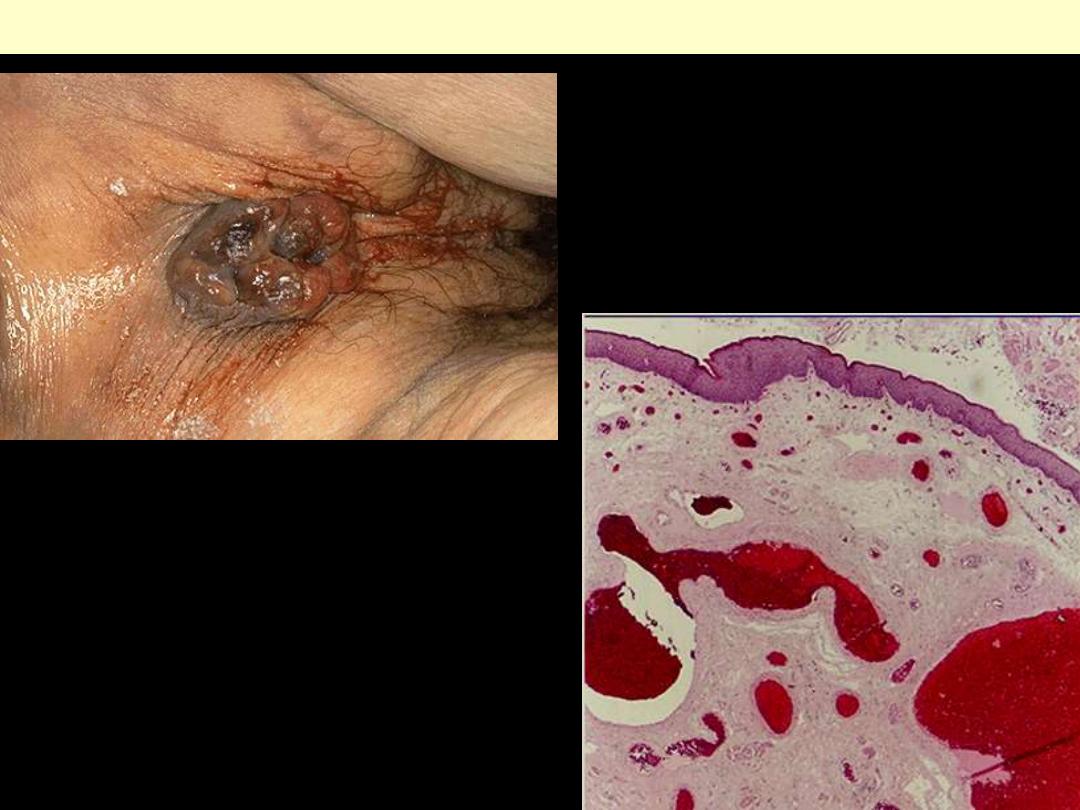
Seen here is the anus and perianal region with
prominent prolapsed internal hemorrhoids.
Hemorrhoids consist of dilated submucosal veins
which may thrombose and rupture with
hematoma formation.
Hemorrhoids
Thin-walled, dilated, submucosal varices that
protrude through the anus
Intestine - ischemic bowel
disease
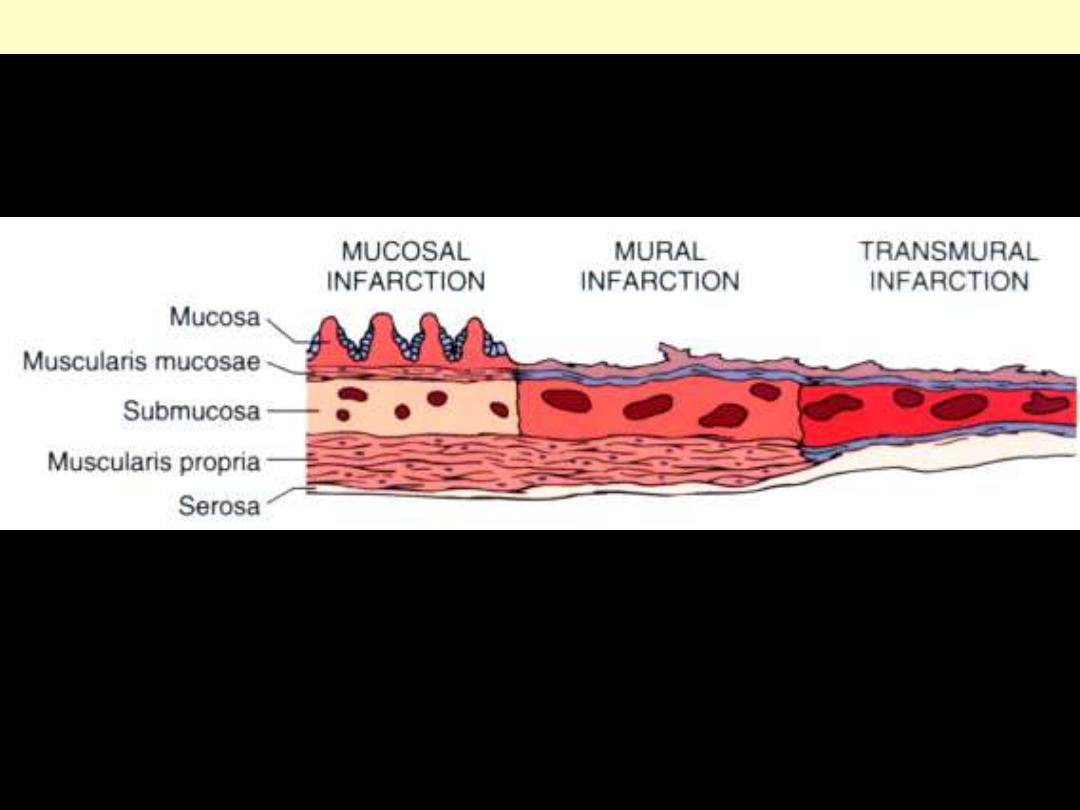
Acute ischemic bowel disease
Schematic of the three levels of severity, diagrammed for the small intestine.
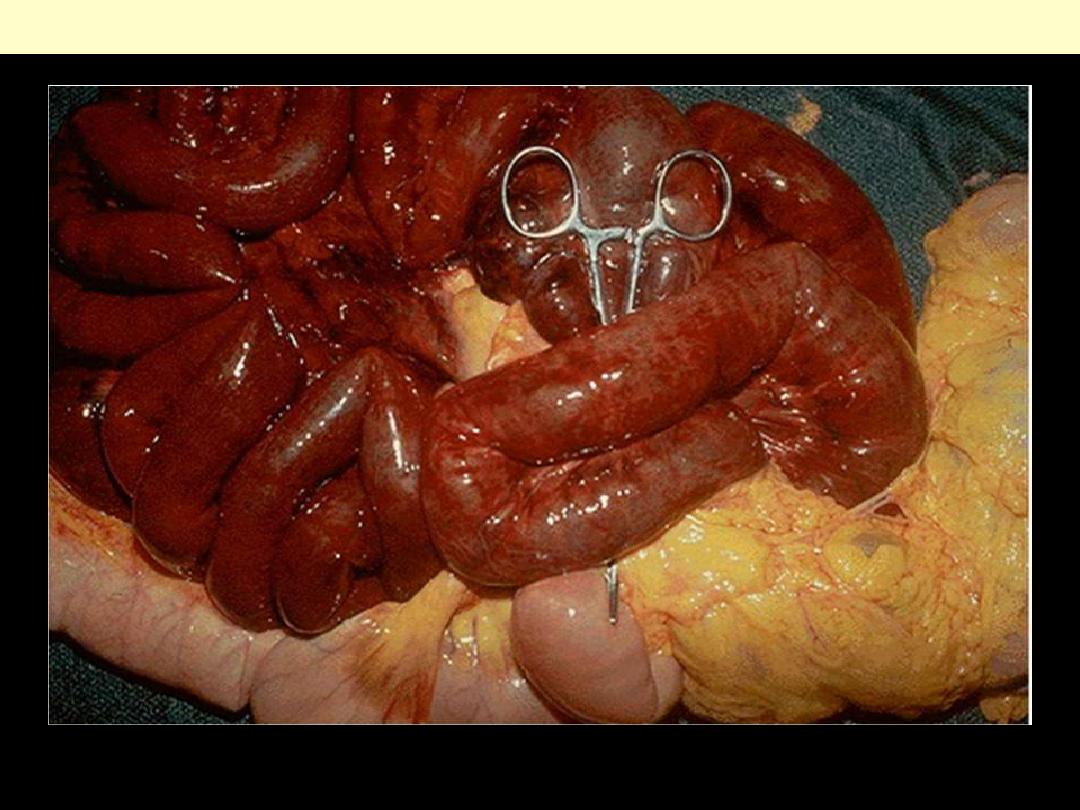
Gangrene small intestine
Infarcted small bowel, secondary to acute thrombotic occlusion of the superior mesenteric artery.
The mucosa demonstrates marked hyperemia
as a result of ischemic enteritis.
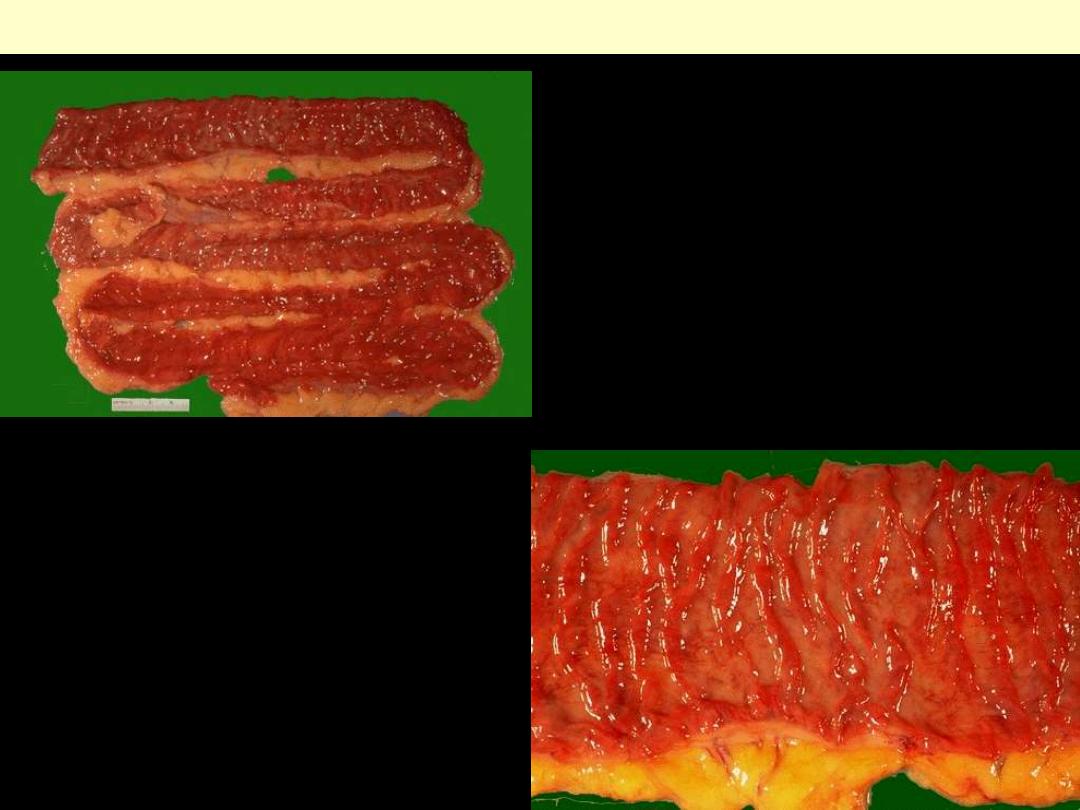
Ischemic enteritis
At closer view, early ischemic enteritis (or
colitis) involves the tips of the villi
.
In general,
bowel is hard to infarct from atherosclerotic
vascular narrowing or thromboembolization
because of the widely anastomosing blood
supply. Thus, most cases of ischemia and
infarction result from generalized hypotension
and decreased cardiac output.
Ischemic colitis. The lesion is typically located
in the splenic flexure. The mucosa is markedly
hyperemic and covered by a fibrinopurulent
exudate.
Ischemic colitis
Ischemic colitis showing a highly hyperemic
surface with ulceration

With more advanced necrosis, the small intestinal mucosa shows hemorrhage with acute inflammation
in this case of ischemic enteritis.
Ischemic entritis; mucosal necrosis
The upper mucosa is necrotic and degenerated with eosinophilic hyalinazation, inflammation and
edema of the lamina propria. The lower mucosa shows loss of crypts but with evidence of regeneration
Kryptenepithel abgeschilfert and degenerates. Lower Kryptenepithel regenerated with Becher cell
loss. Eosinophilic hyalines edema of the Tunica propria. There is an overlying pseudomembrane
Acute ischemic colitis
Intestine - obstruction
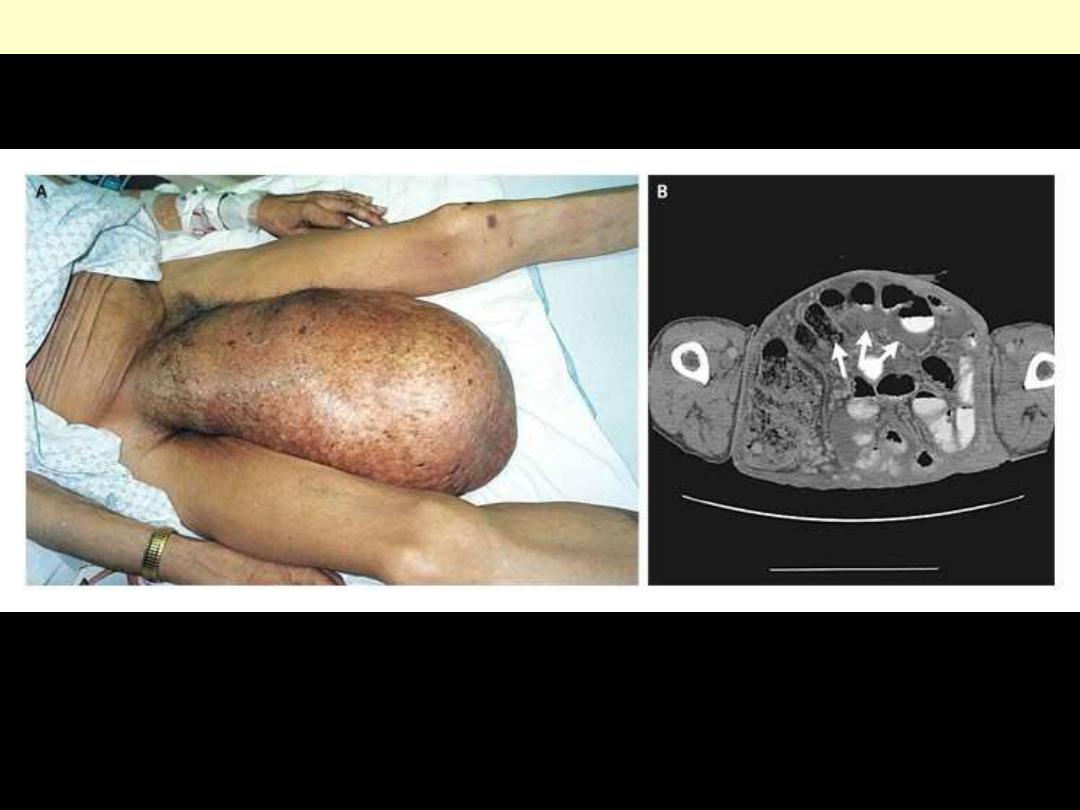
Large, right-sided inguinal hernia that had been enlarging for more than eight years (Panel A).
Computed tomography revealed unobstructed bowel within the hernia sac (Panel B, arrows).
Inguinal hernia
This is an adhesion between loops of small intestine. Such adhesions are typical
following abdominal surgery. More diffuse adhesions may also form following
peritonitis.
Adhesions small intestine

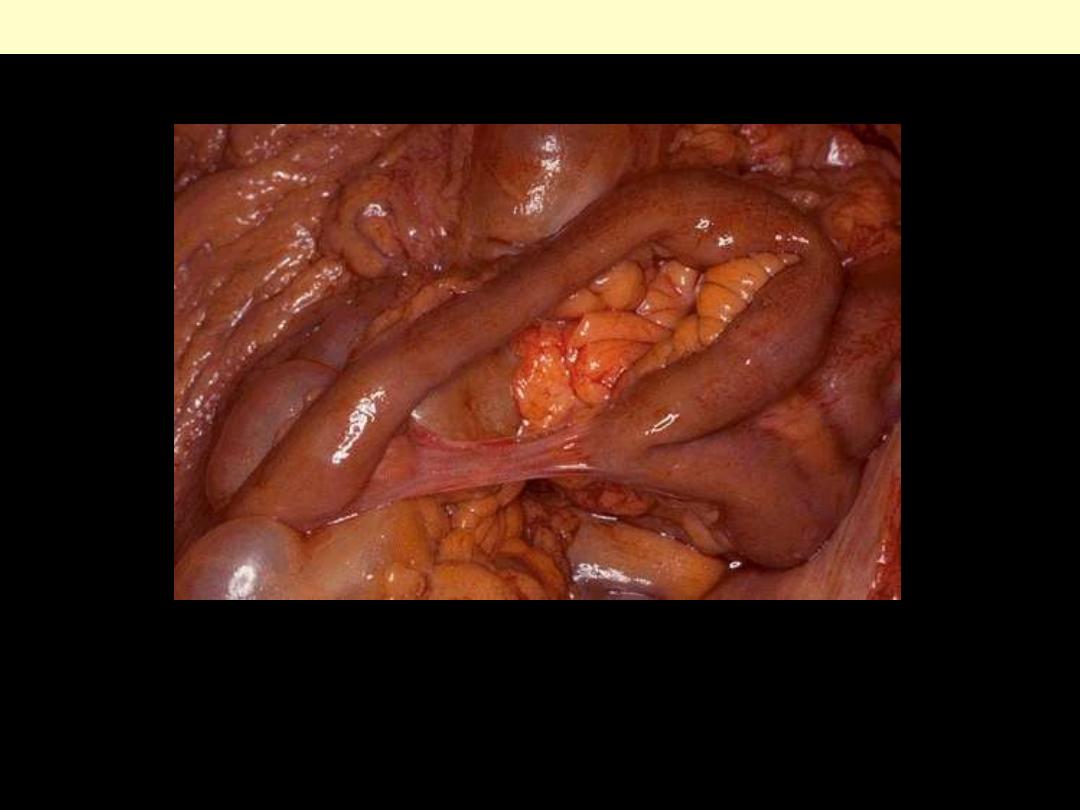
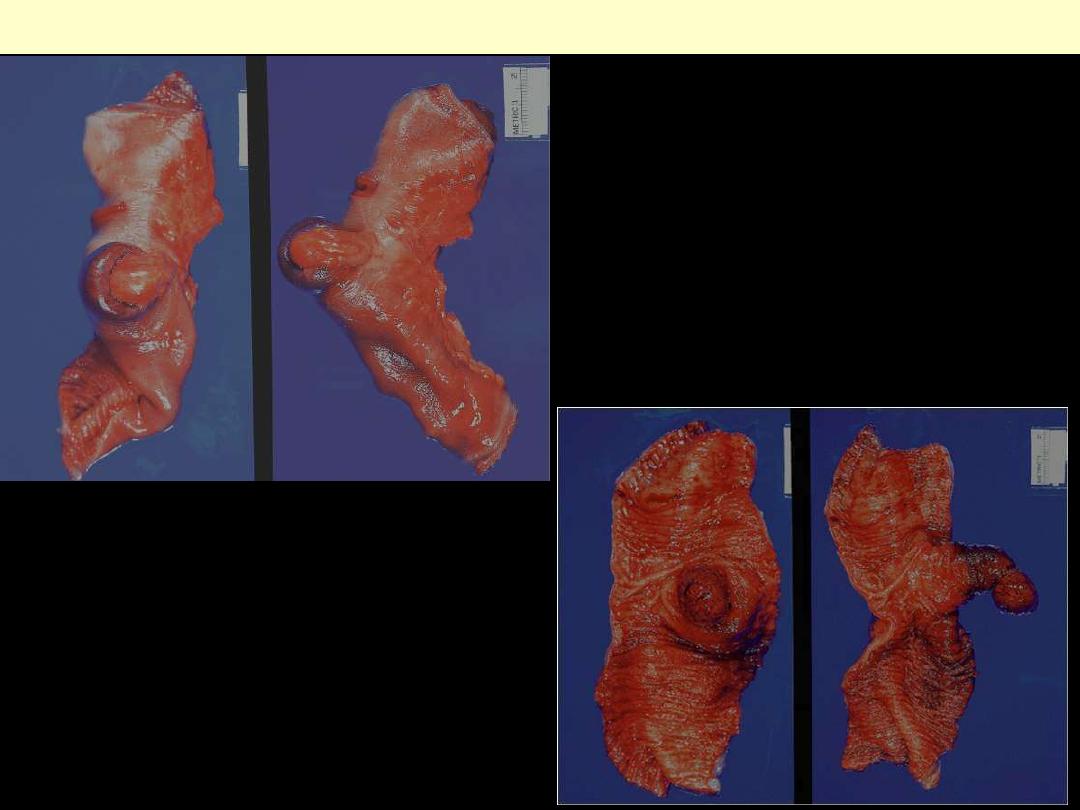
Intussuception
Small intestine
Outer aspect of small bowel in
intussusception.
Intussusception of small bowel caused
by an adenocarcinoma. The tumor,
located at the tip of the
intussusceptum, is ulcerated and
necrotic.
Volvulus is a twisting of the bowel.
Volvulus cecum
Intestine - tumors
Adenoma of the ampulla of vater
There is exophytic tumor at the ampullary orifice
Juvenile polyp Large intestine
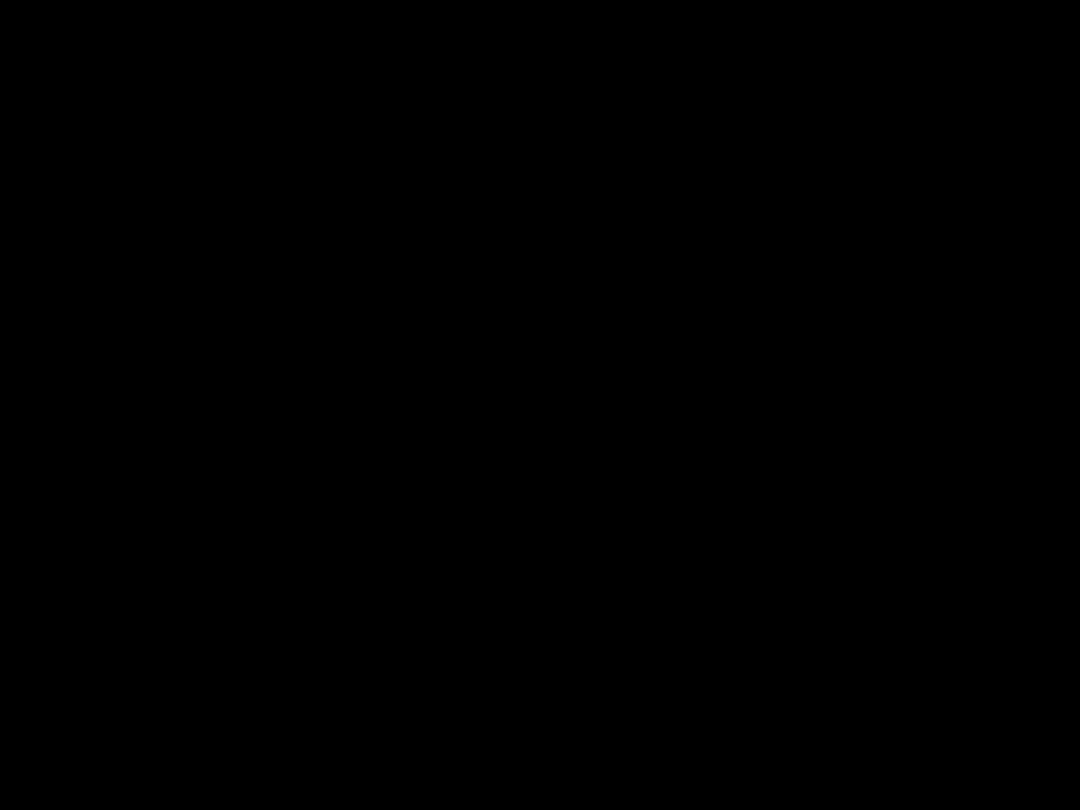
A and B, Outer aspect and cut surface of juvenile (retention) polyp. Note the ulcerated, highly
hyperemic surface (A), and the cystically dilated glands in an edematous stroma (B).

Juvenile polyp Large intestine
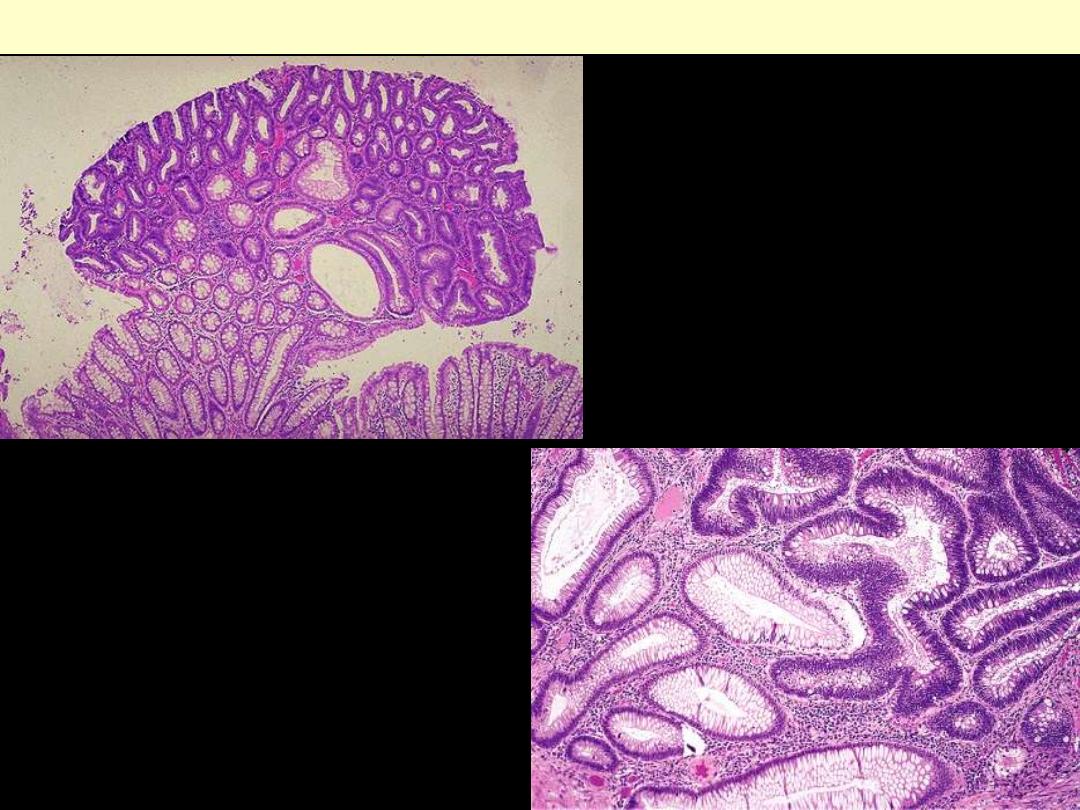
Whole-mount view of a juvenile (retention) polyp.
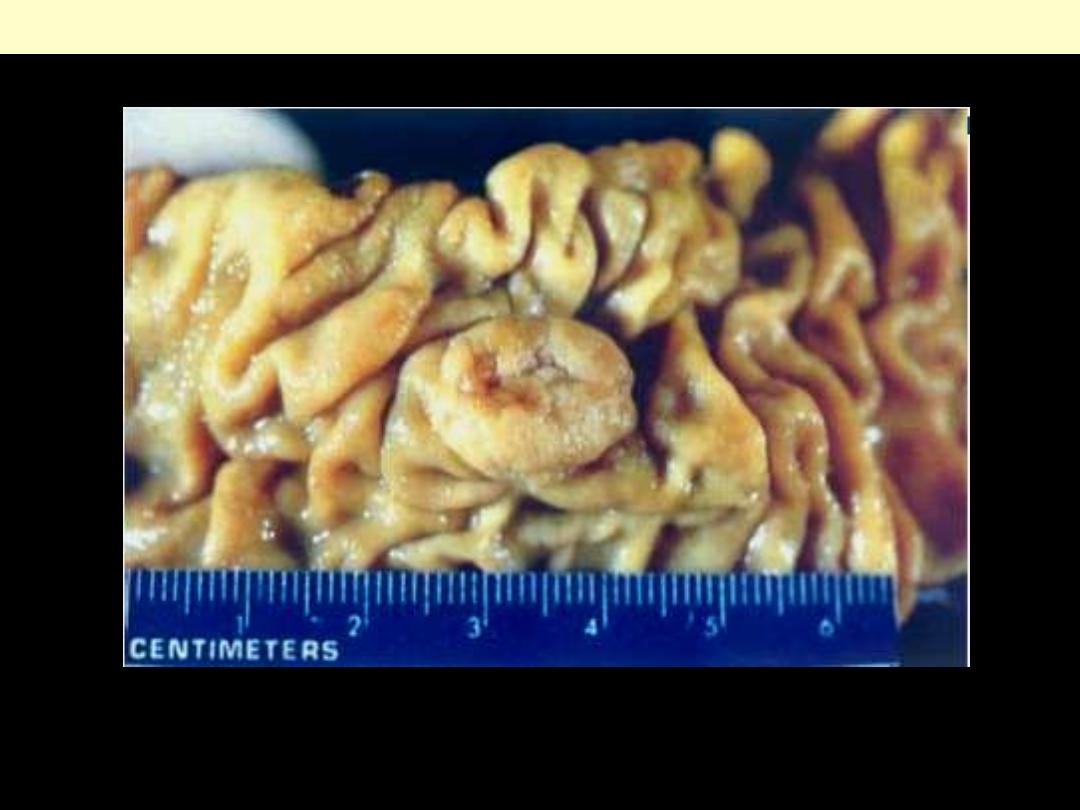
Mucocutaneous pigmentation with a predominant perioral disposition.
Oral pigmentation in Peutz-Jeghers syndrome

Hamartomatous polyp of small bowel in 12-year-old girl. Tumor, which had caused intussusception,
was not associated with other features of Peutz-Jeghers syndrome. A, Gross appearance of tumor,
showing distinct lobulation, short stalk, and multiple small cysts. B, Panoramic view of microscopic
section. Ramifying central stalk containing numerous muscle bundles supports florid epithelial
proliferation. Many of glands show cystic dilatation.
Peutz-Jeghers polyp large intestine
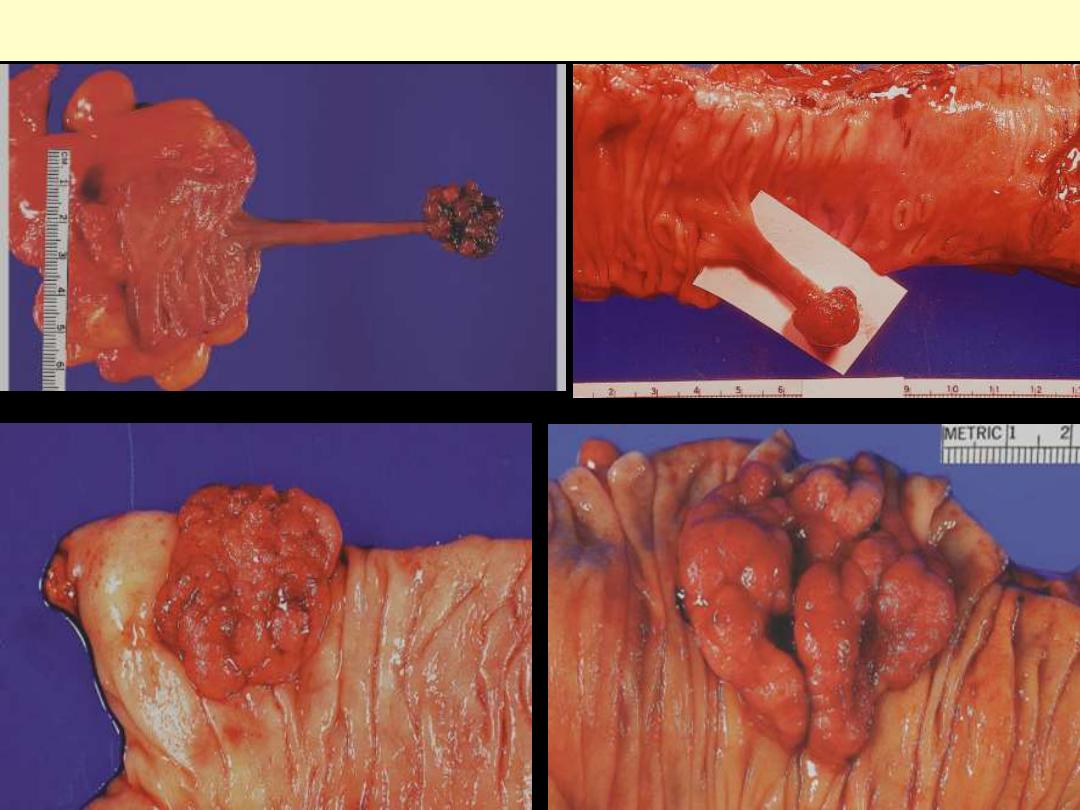
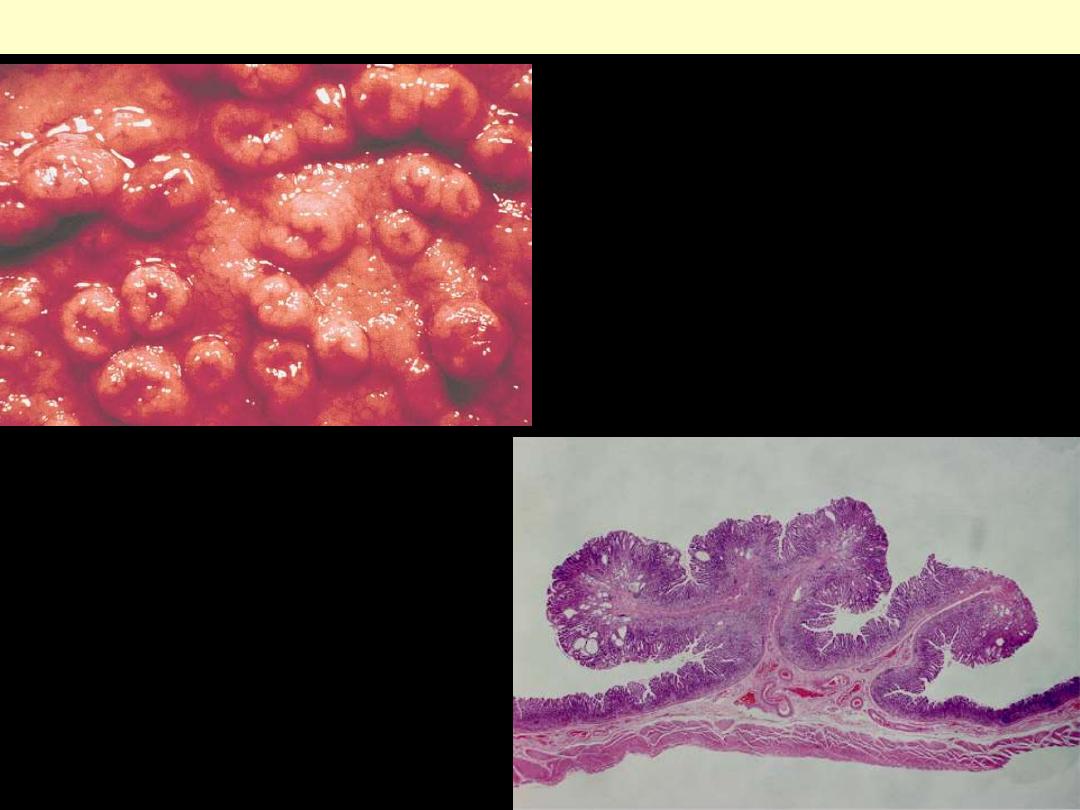
Pedunculated adenomatous polyps.
Adenomatous polyp (tubular adenoma), LP
The polyp is composed of neoplastic
glandular structures that appear darker then
the adjacent normal glandular elements.
Villous adenoma colon
Lt., surface view; Rt., cross section at the right. Note that this type of adenoma is sessile, rather than
pedunculated, and larger than a tubular adenoma (adenomatous polyp). A villous adenoma averages
several centimeters in diameter, and may be up to 10 cm.
Villous adenoma
Low-power microscopic appearance: long villi are arranged in parallel, perpendicularly to the mucosa.

Villoglandular polyp
.
There is an admixture of villous and
glandular structures.
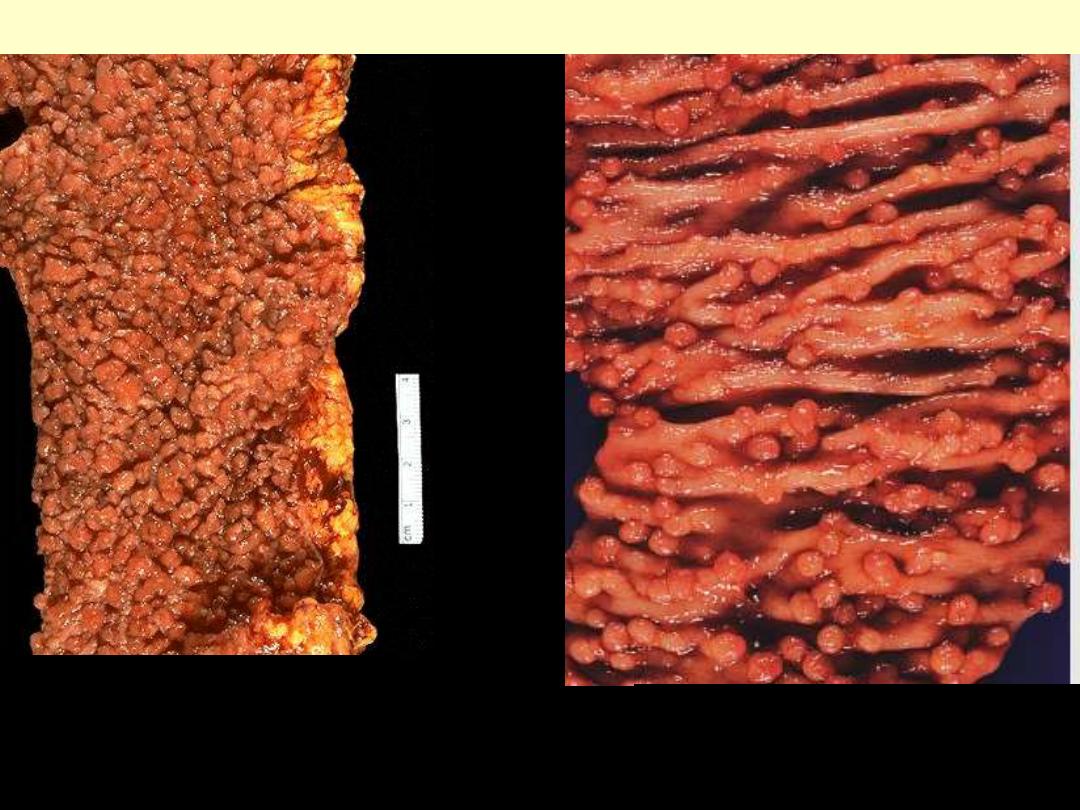
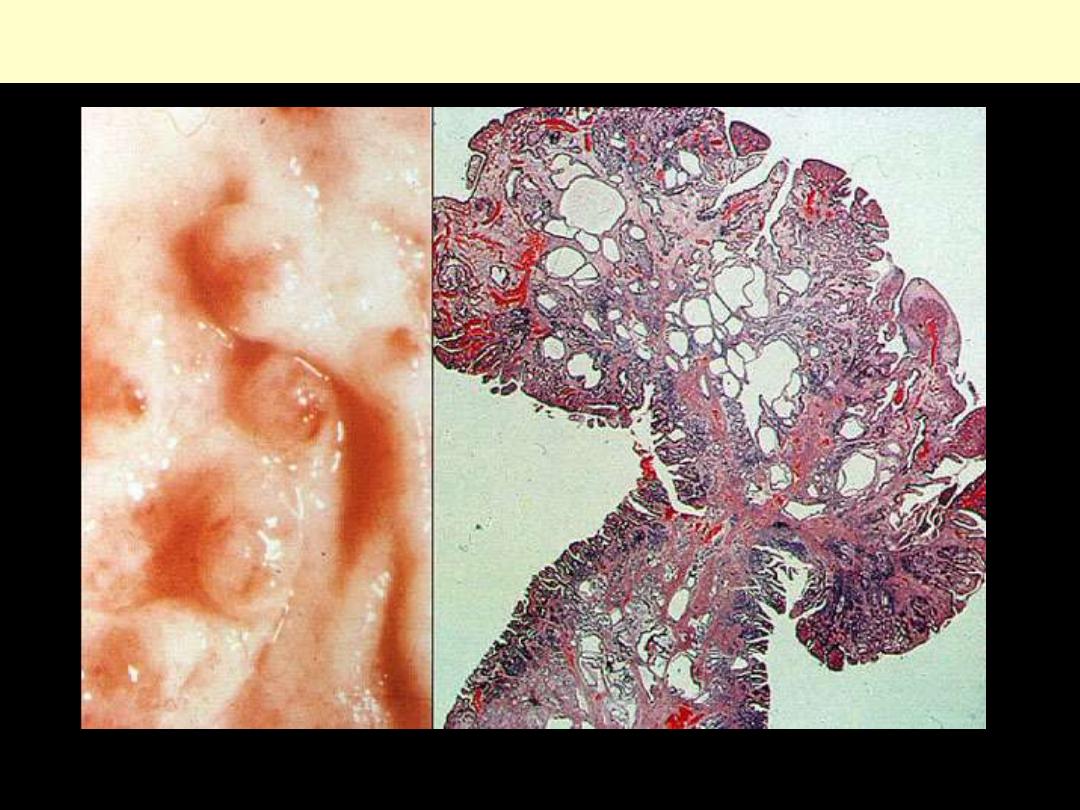
Gross appearance of familial polyposis. The
entire large bowel was involved. Note the
fact that practically all of the polyps are
small and sessile.
Polyposis with numerous small
polyps covering the colonic mucosa.
18-year-old woman
. The mucosal
surface is carpeted by innumerable
polypoid adenomas.
Adenomatous Familial Polyposis (AFP)
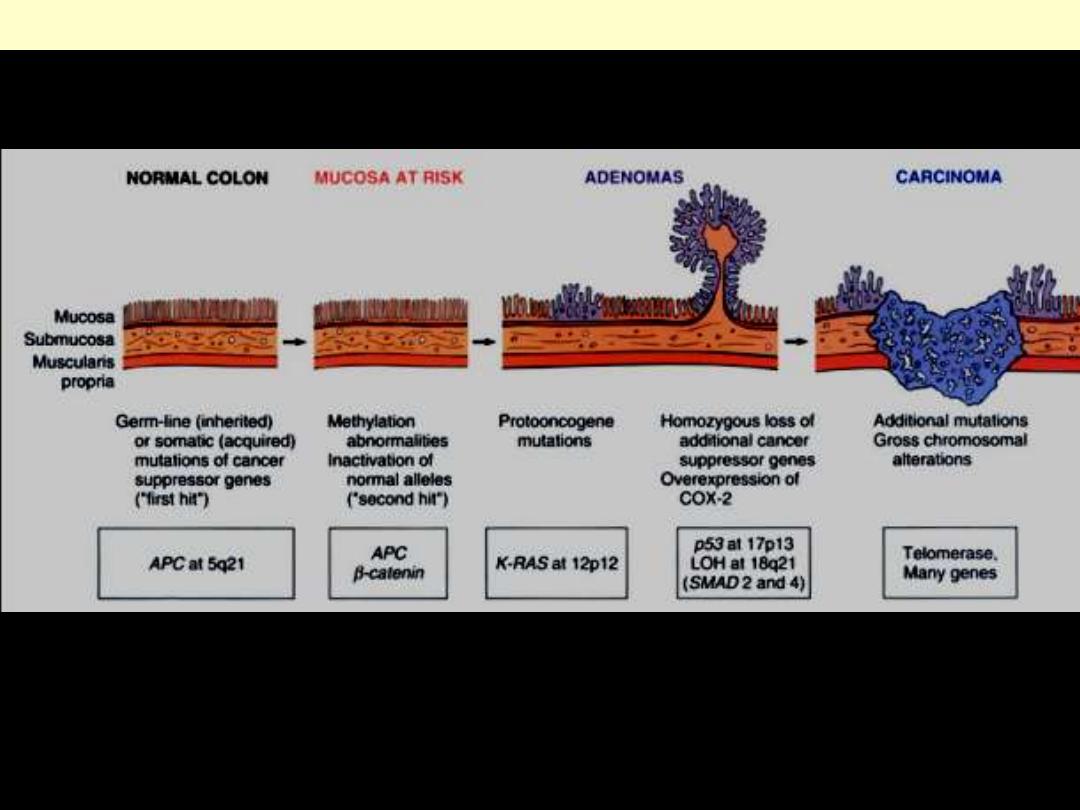
Morphologic & molecular changes in the adenoma-carcinoma sequence
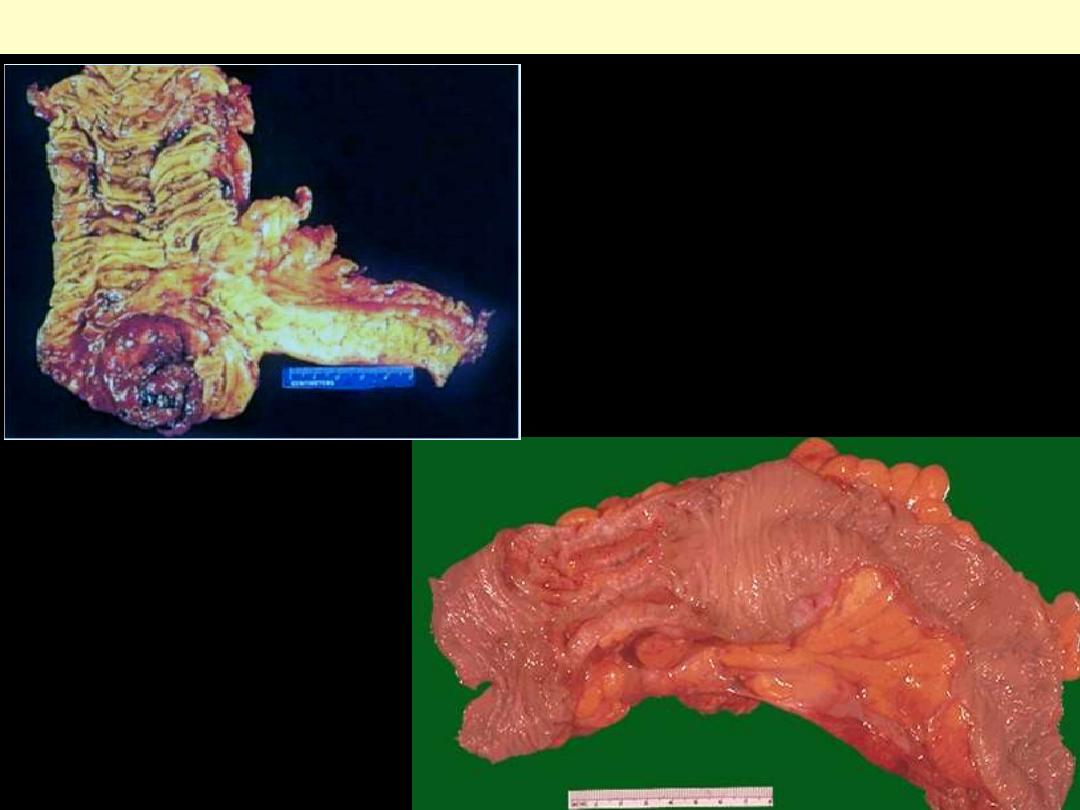
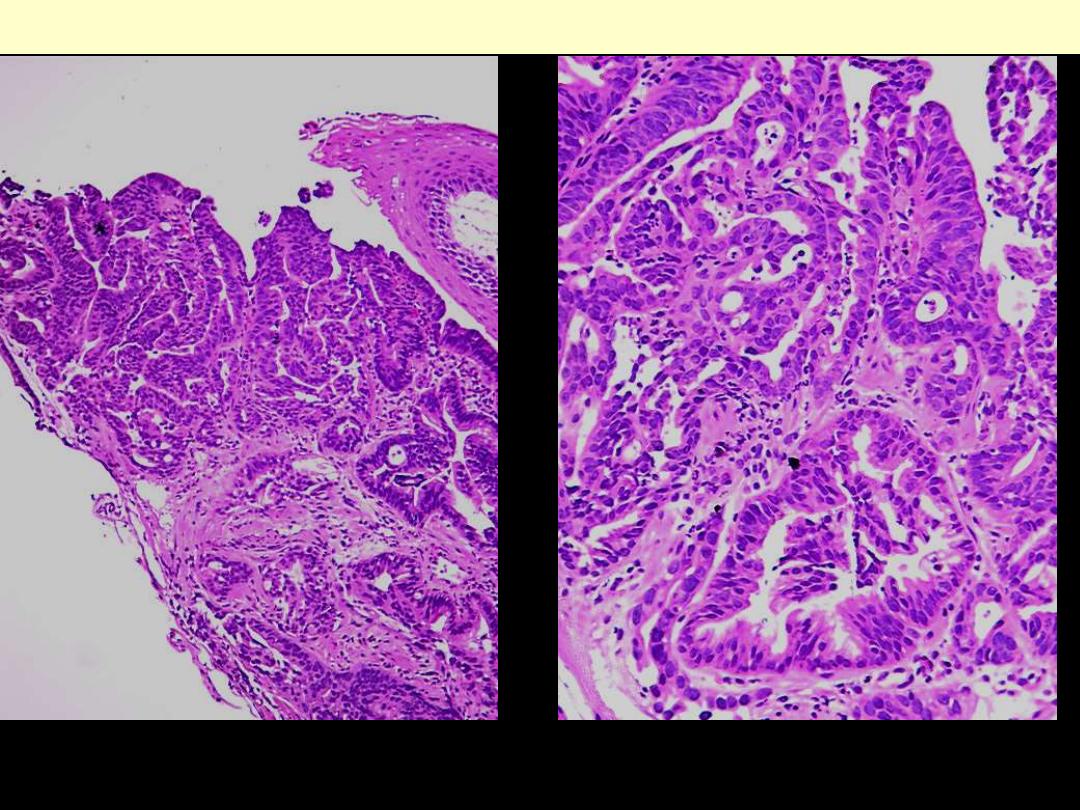
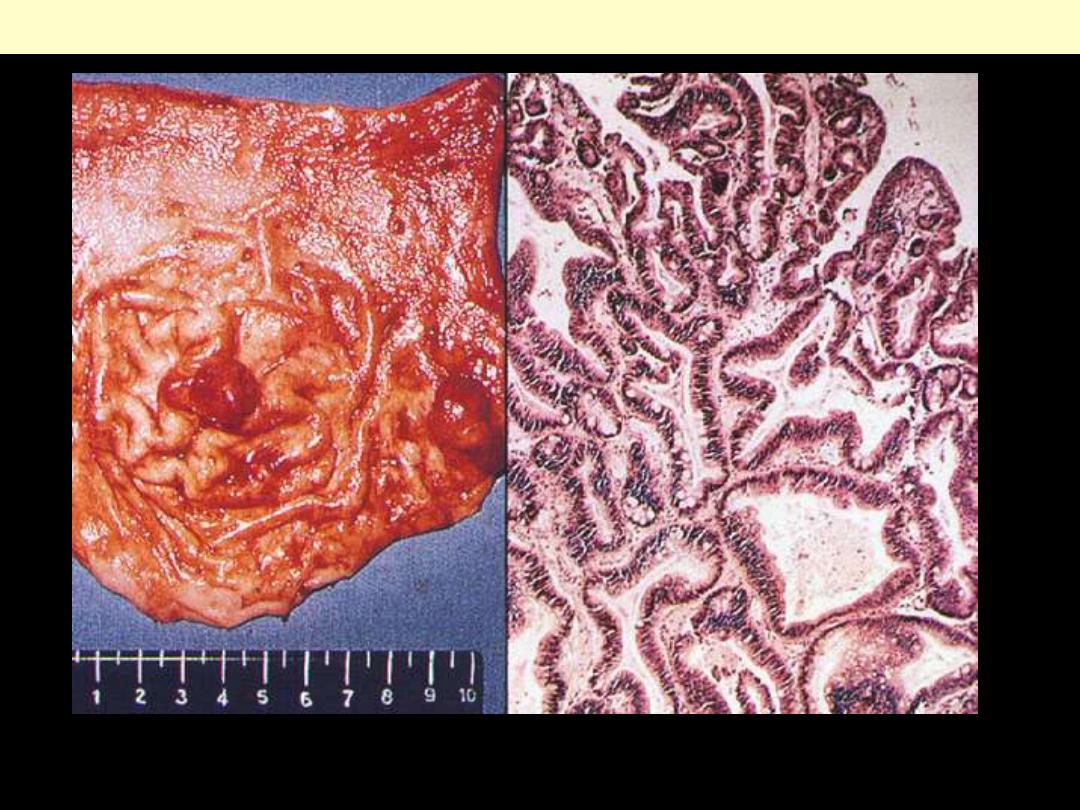
Carcinoma large intestine
Carcinoma of the cecum. The fungating carcinoma
projects into the lumen but has not caused
obstruction.
Adenoca descending colon
The encircling mass of firm
adenocarcinoma in this colon at the
left is typical for adenocarcinomas
arising in the descending
Colon.
MP: the glands are large and filled
with necrotic debris.
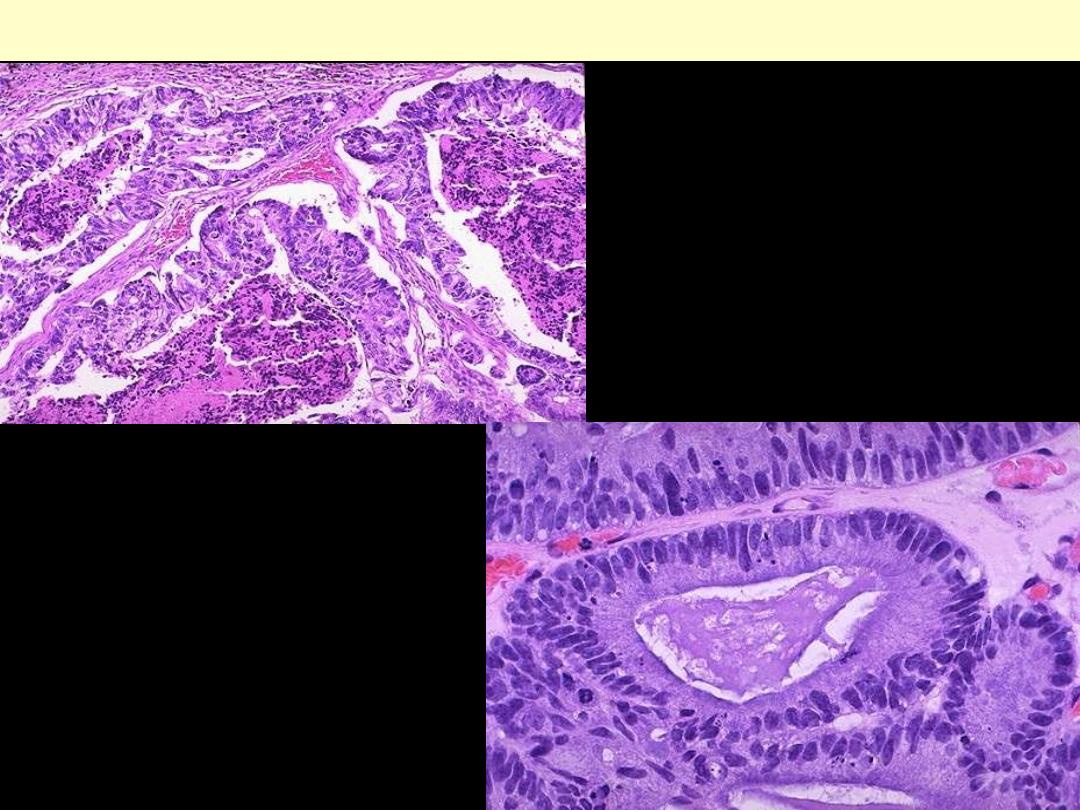
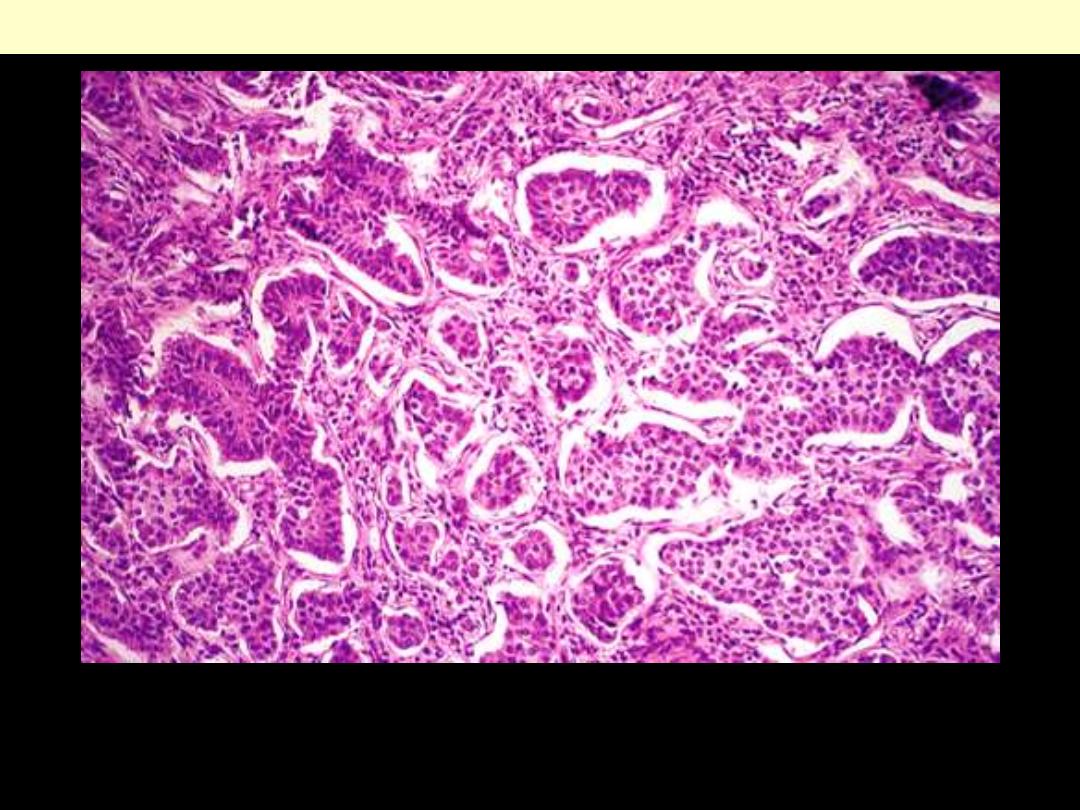
Adenocarcinoma colon
HP, the neoplastic glands of
adenocarcinoma have crowded
nuclei with hyperchromatism and
pleomorphism.
No normal goblet
cells are seen.
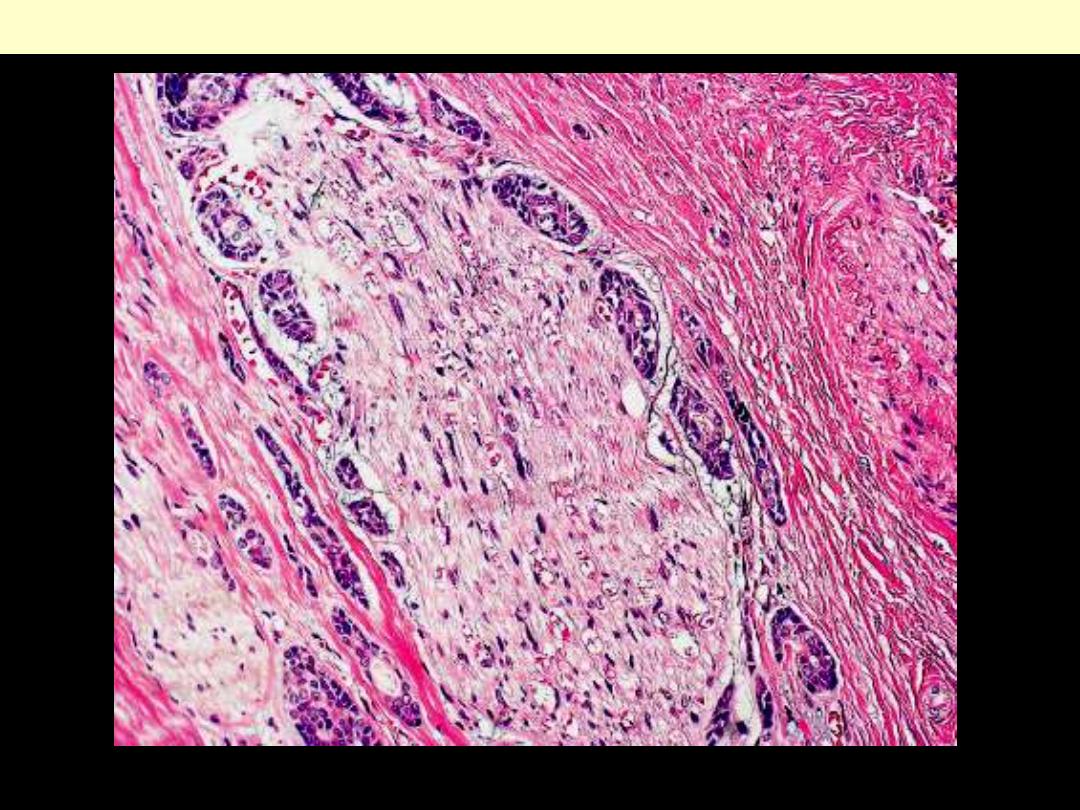
Invasive adenocarcinoma of colon, showing
malignant glands infiltrating the muscle wall.
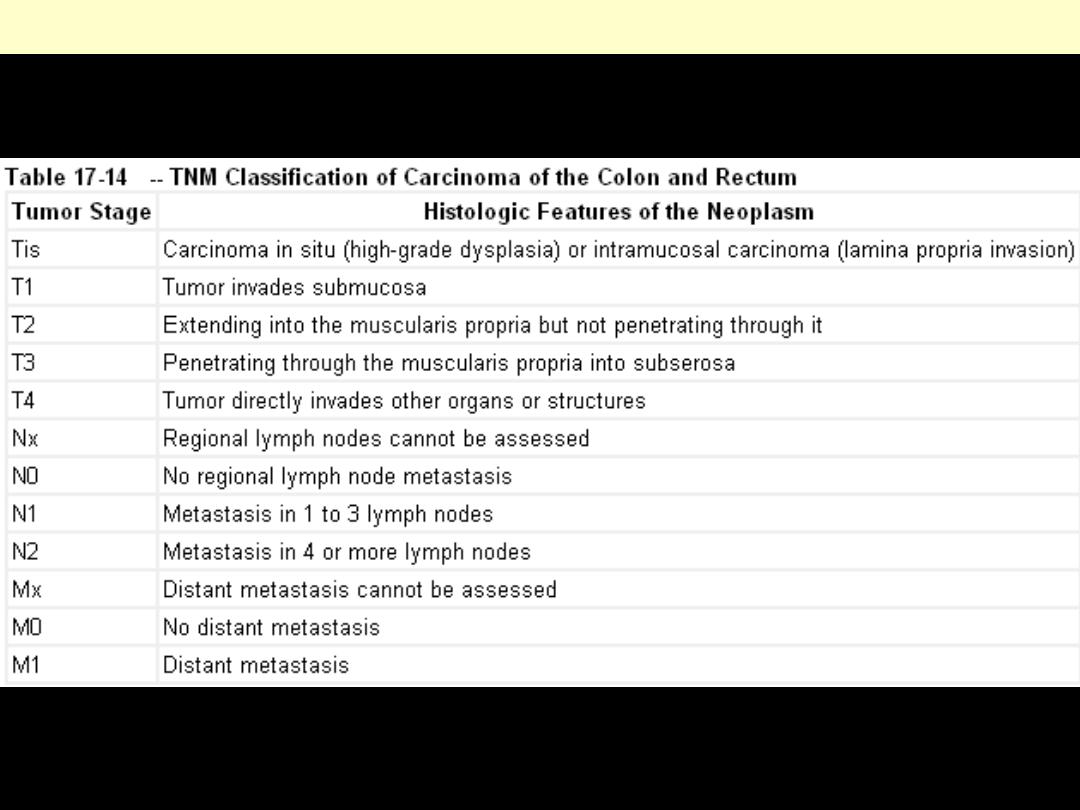
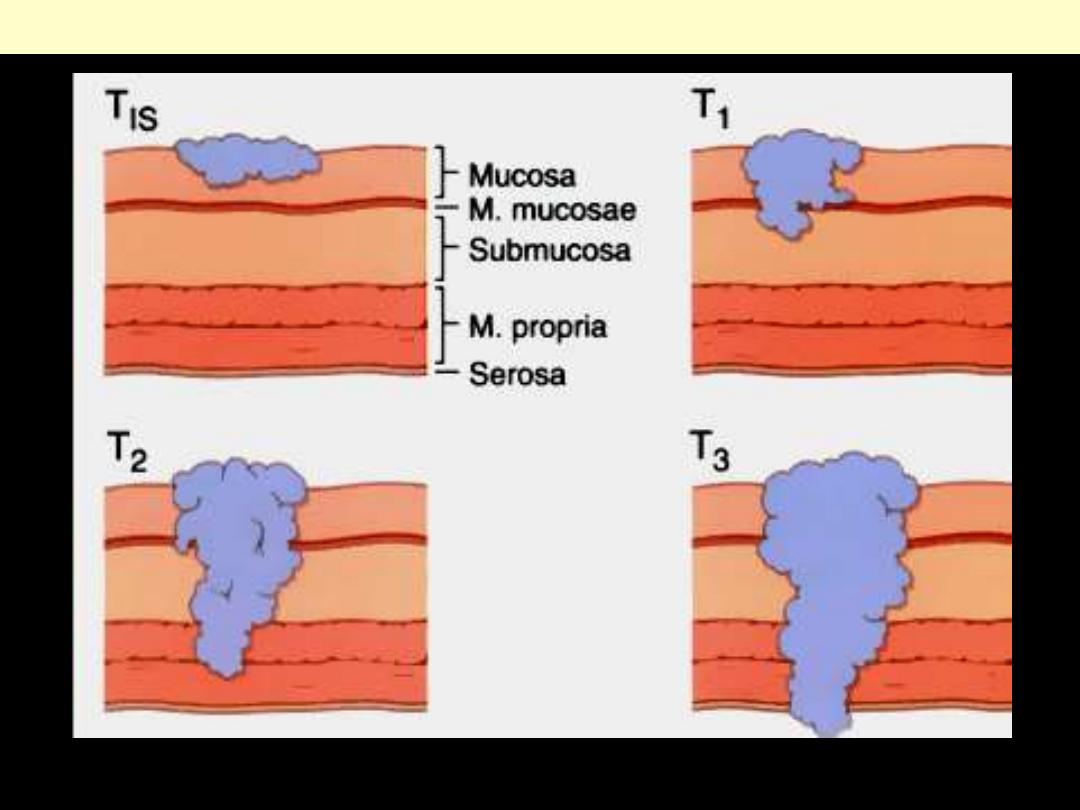
TNM classification of colo-rectal carcinoma
Pathologic staging of colorectal cancer. Staging is based on the depth of tumor invasion.
H
D
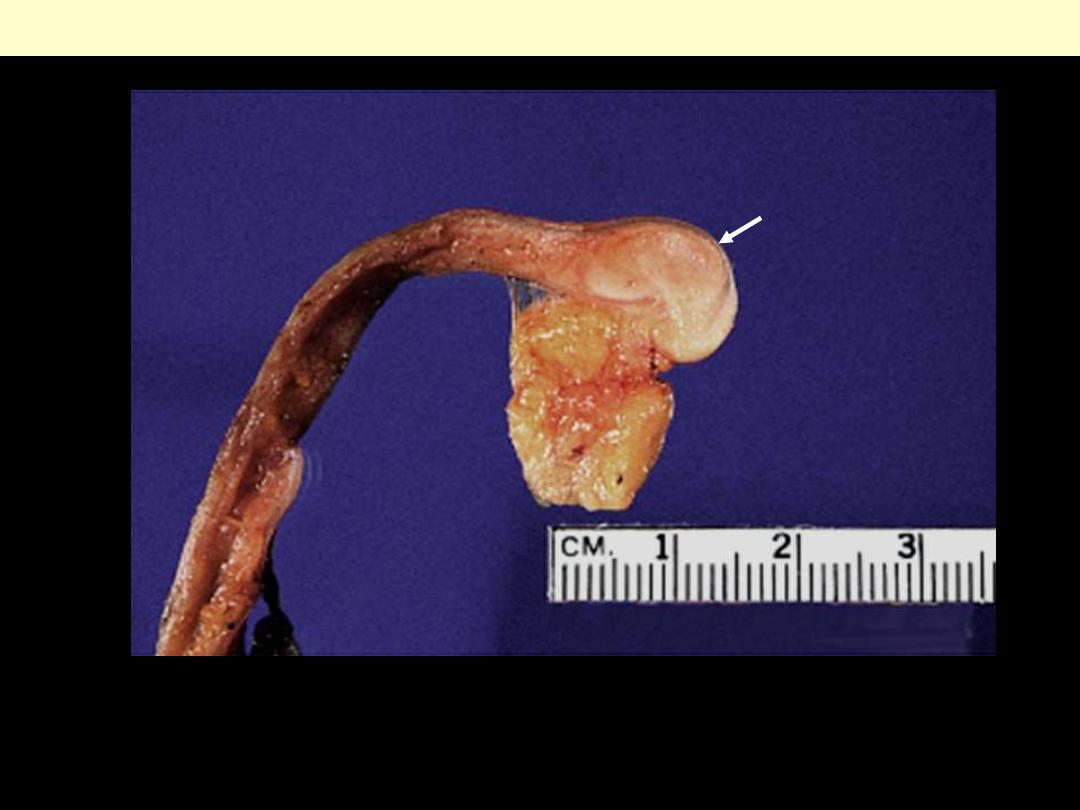
Carcinoid appendix
The tumor has a solid appearance and a whitish color and is characteristically located in the tip.
Microscopically, it was of the classic (insular) type.
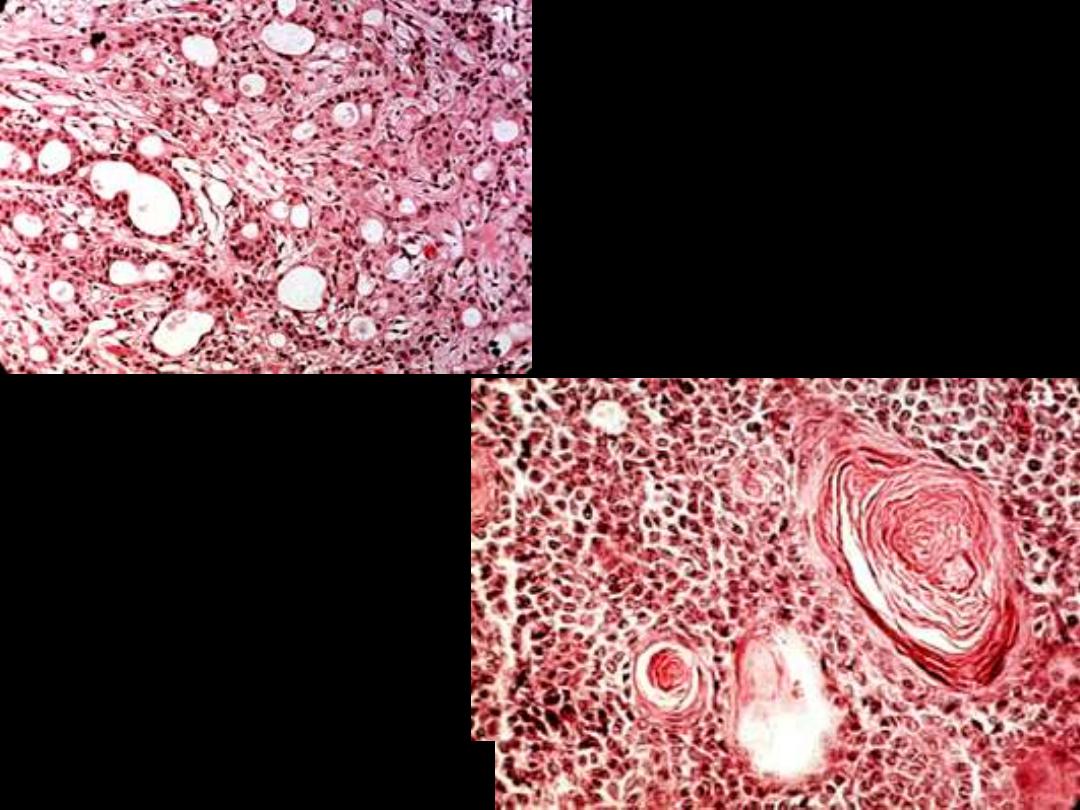
Carcinoid tumor classic type appendix
solid nests of small monotonous cells with occasional acinar or rosette formation. Mitoses are
exceedingly rare. A peculiar retraction of the tumor periphery from the stroma is evident
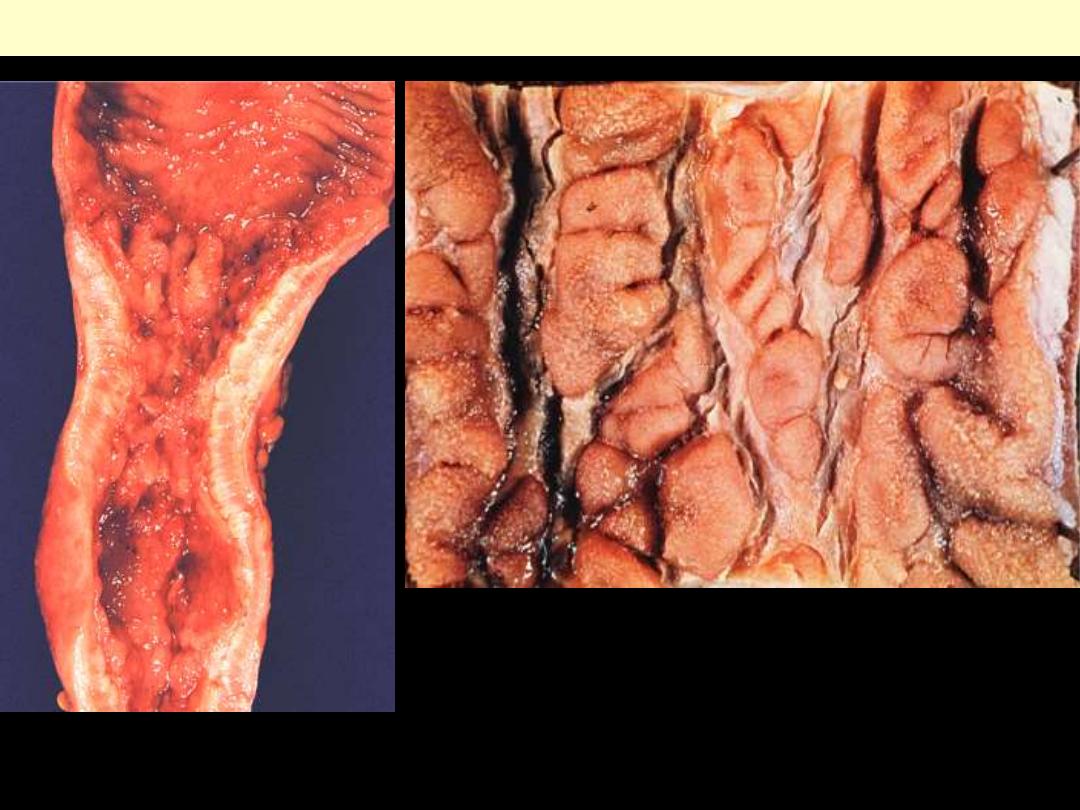
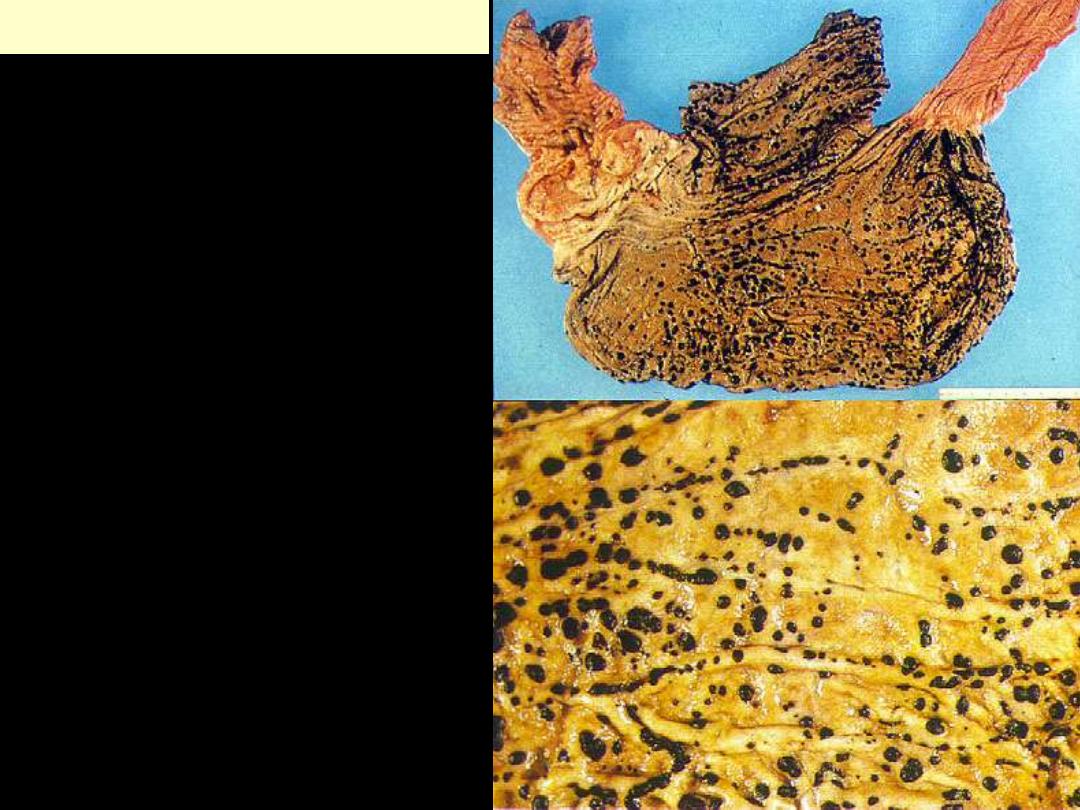
Intestine - UC
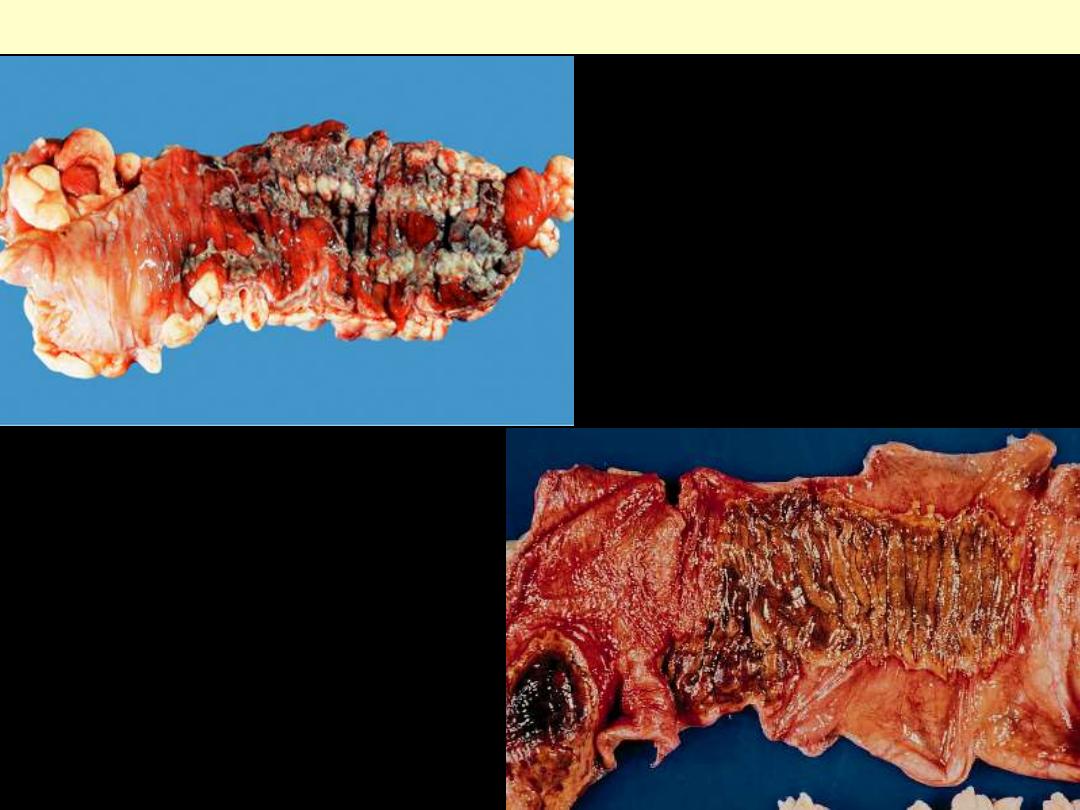
The ileocecal valve is seen at the upper left. Just distal to this begins increasing mucosal inflammation.
There is diffuse mucosal hyperemia with large, irregular, rather superficial ulcers.
Extensive ulcerative colitis (pancolitis)

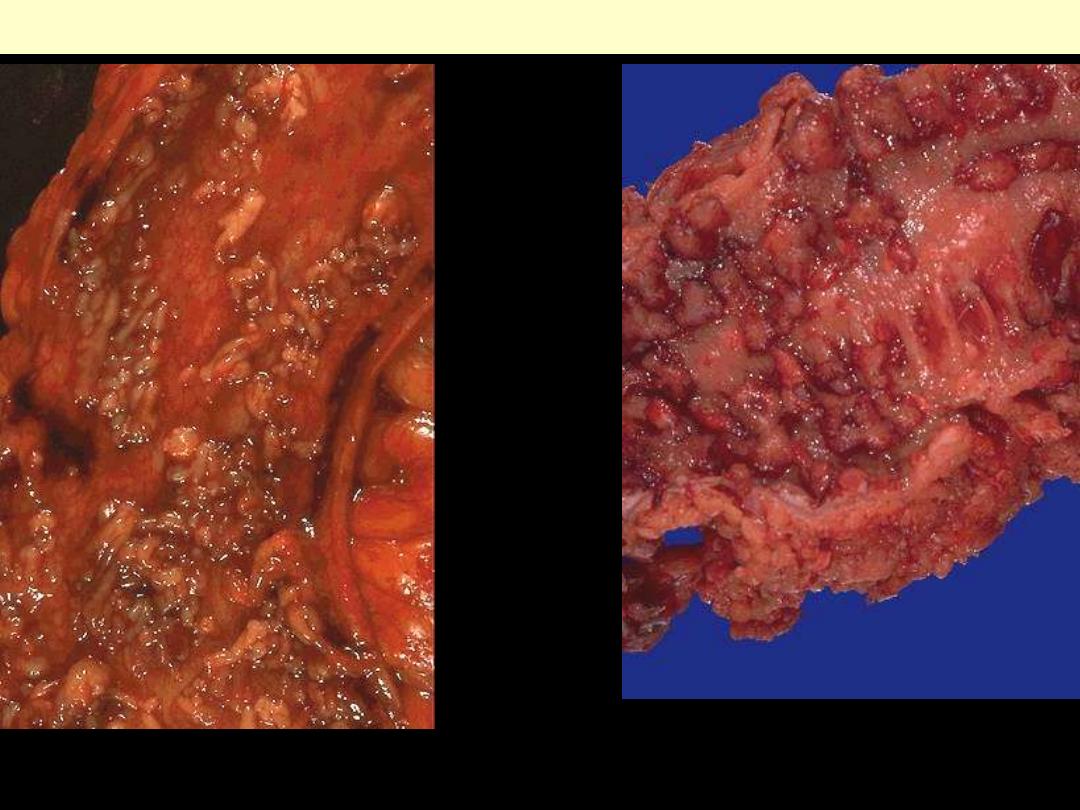
Active ulcerative colitis
There is diffuse, marked mucosal hyperemia and sanguineous exudate.
Chronic form, showing mucosal ulceration with residual foci of elevated and hyperemic mucosa.
Chronic ulcerative colitis
Late stage of chronic ulcerative colitis,
There is total mucosal atrophy; there is total absence of mucosal folds
Pseudopolyps in ulcerative colitis
At higher magnification, the pseudopolyps can be
seen clearly as raised red islands of inflamed mucosa.
Between the pseudopolyps is only remaining
muscularis.
Pseudopolyps are seen here. The remaining mucosa
has been ulcerated away and is hyperemic.
Pseudopolyps in ulcerative colitis
At higher magnification, the pseudopolyps can be
seen clearly as raised red islands of inflamed mucosa.
Between the pseudopolyps is only remaining
muscularis.
Pseudopolyps are seen here. The remaining mucosa
has been ulcerated away and is hyperemic.
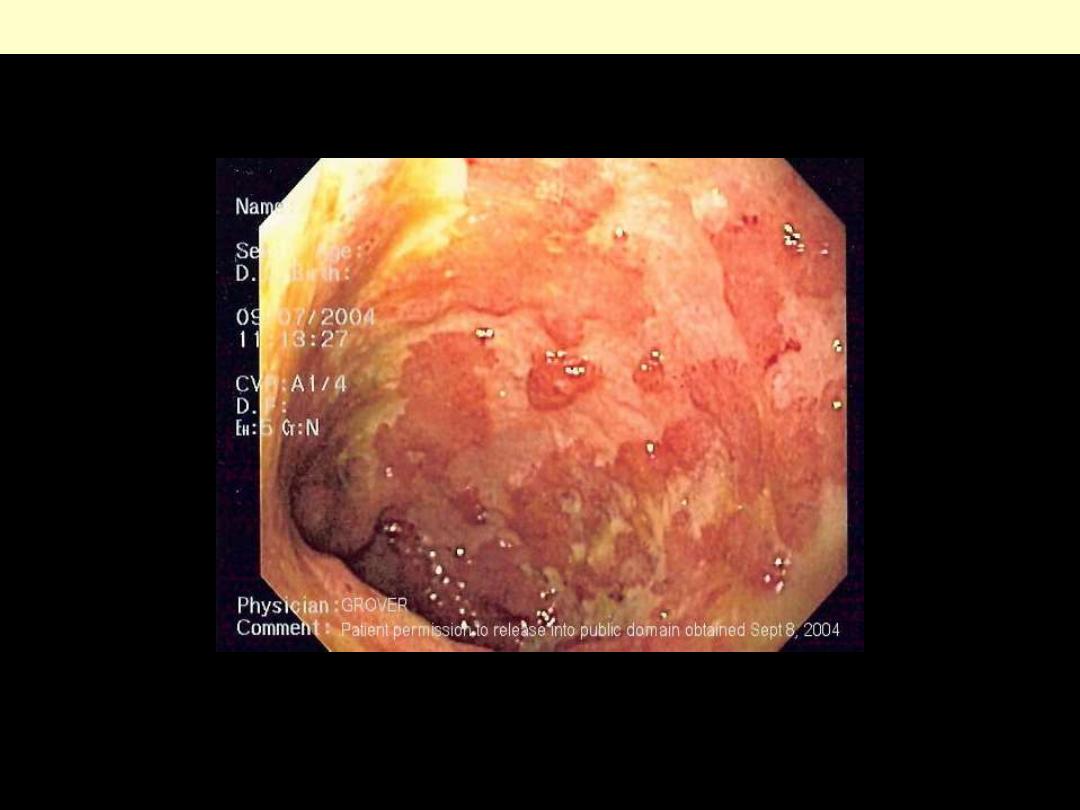
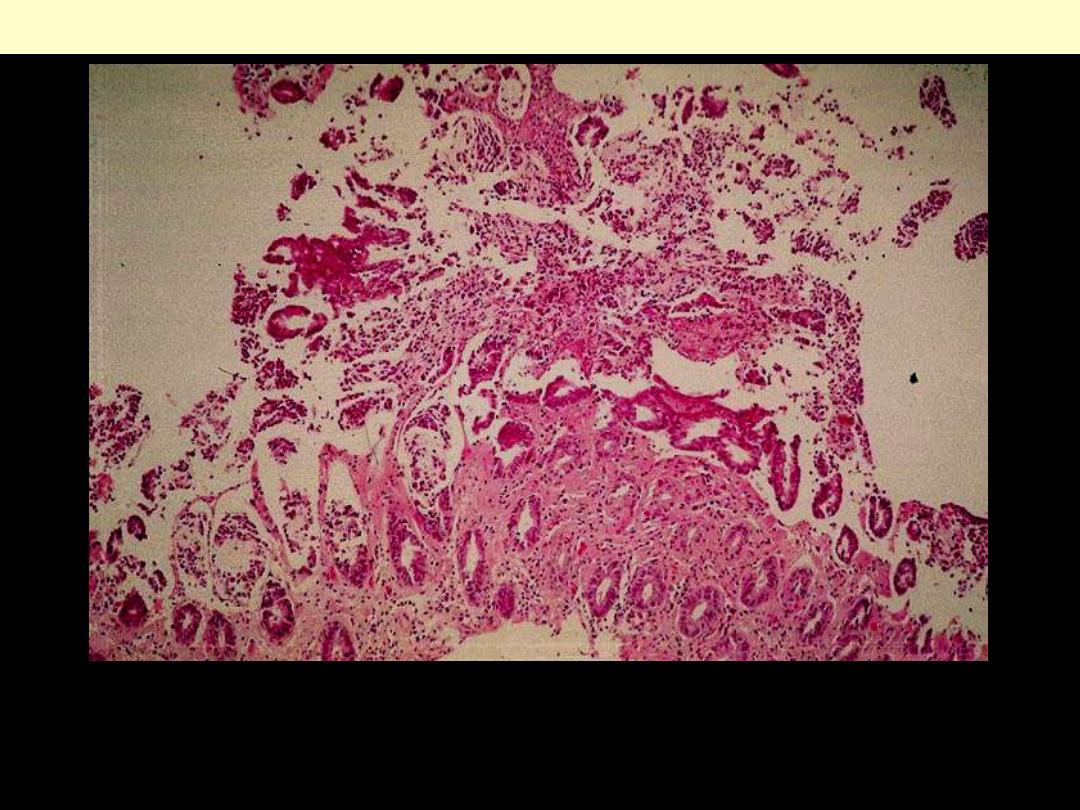
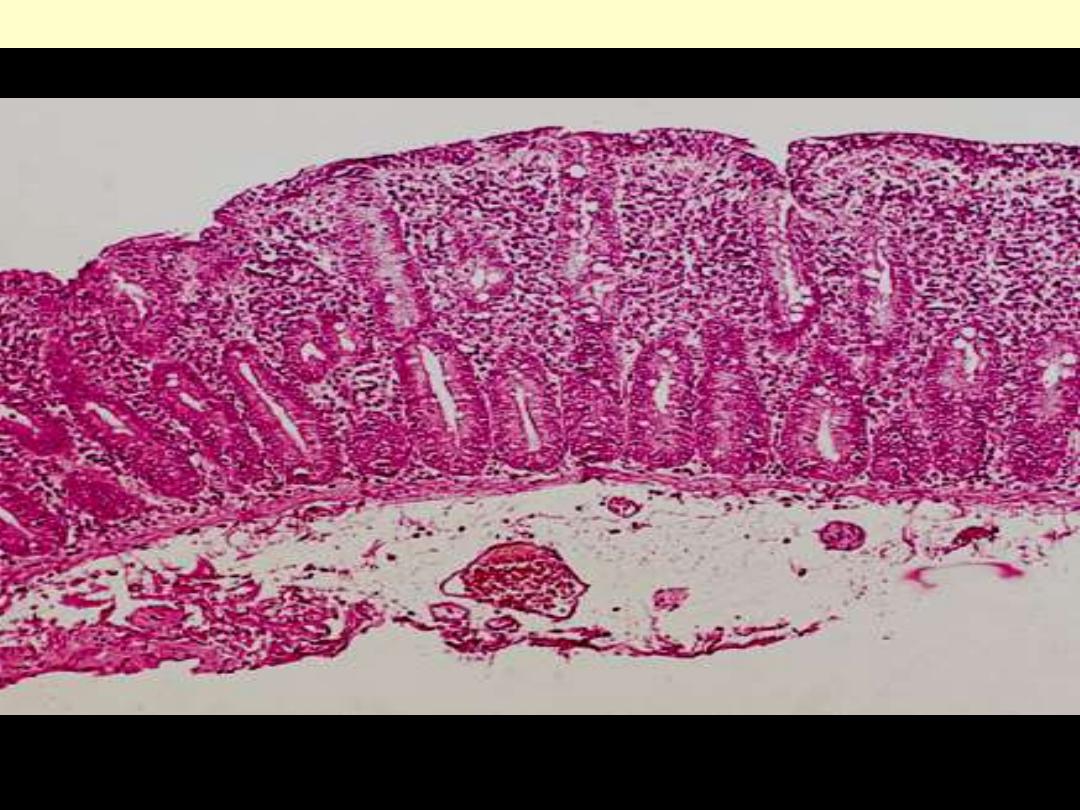
There is confluent superficial ulceration and loss of mucosal architecture. Crohn's disease may be
similar in appearance, a fact that can make diagnosing UC a challenge
Endoscopic image of ulcerative colitis affecting left colon

Toxic megacolon
Complete cessation of colon neuromuscular activity has led to massive dilatation of the colon and
black-green discoloration signifying gangrene and impending rupture.
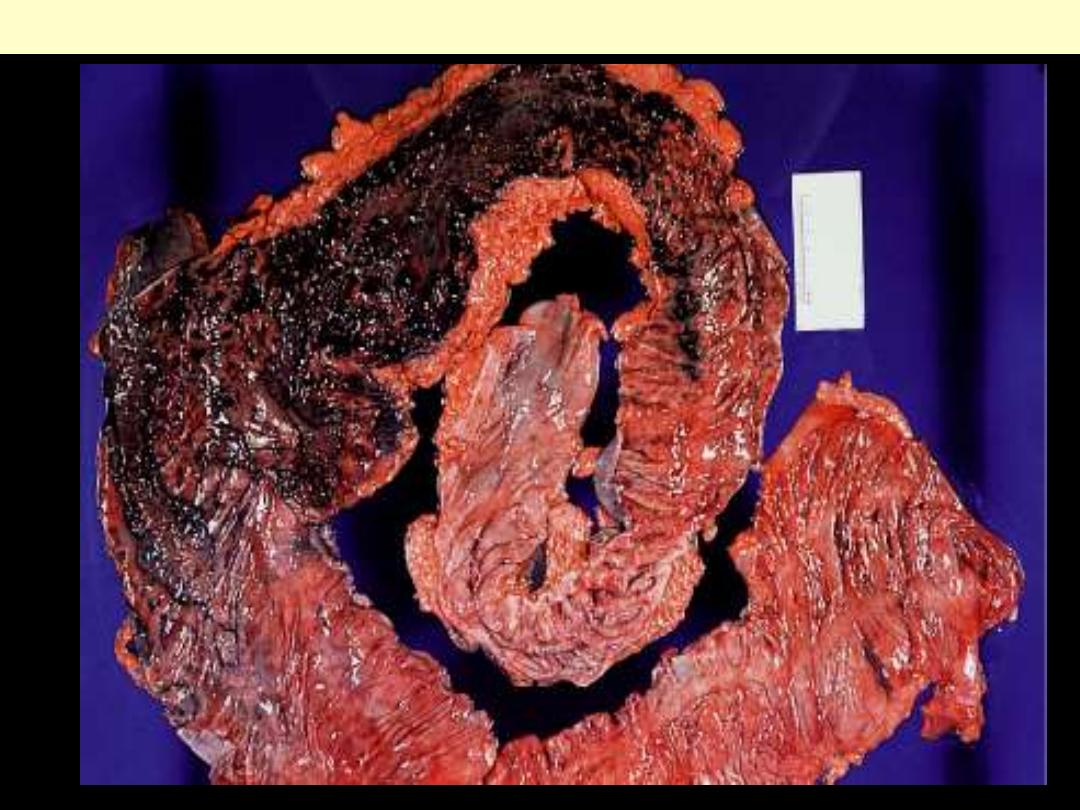
Toxic megacolon complicating ulcerative colitis
the inflammation is confined
primarily to the mucosa. The mucosa
is eroded by an ulcer that
undermines surrounding mucosa
Active chronic ulcerative colitis
Ulcerative colitis featuring crypt abscesses.
LI – Aganglionic megacolon
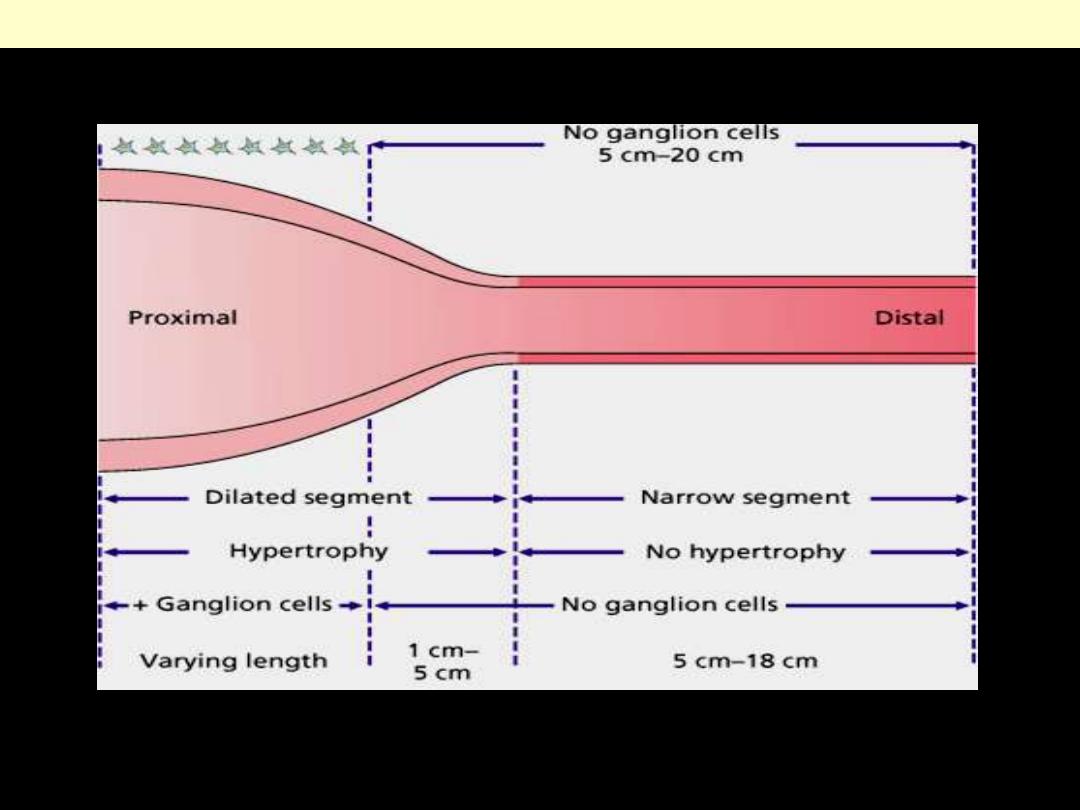
Hirschsprung’s disease colon
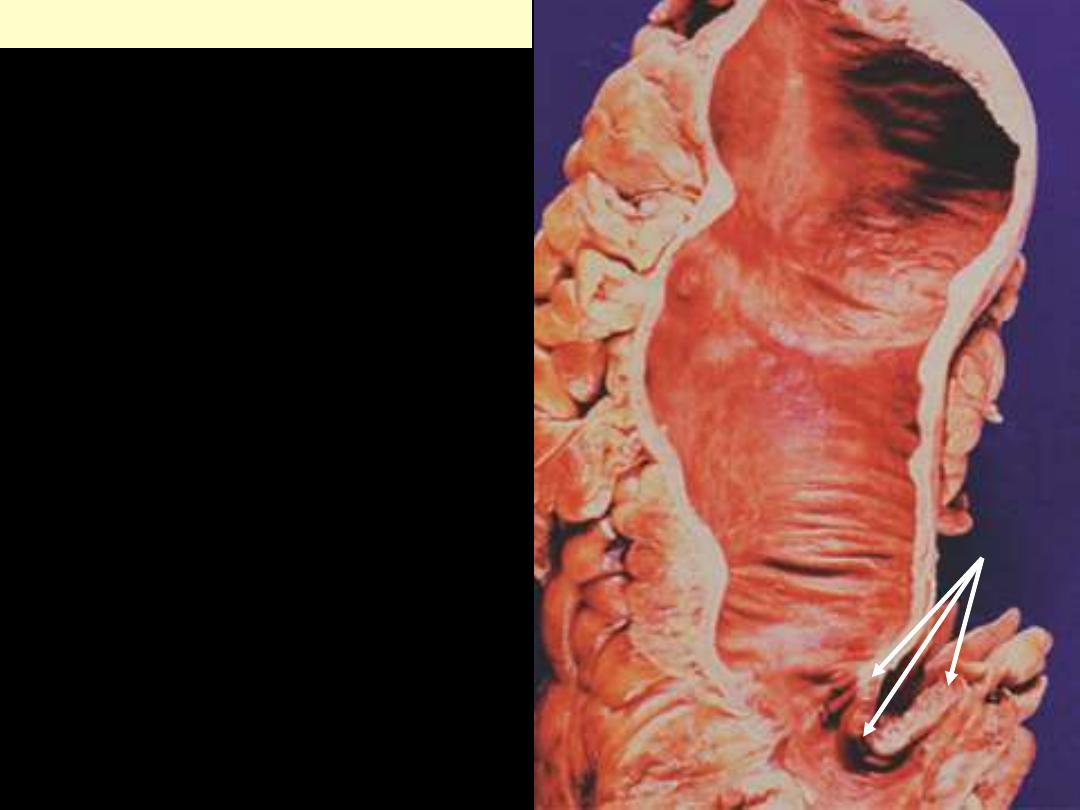
Hirschsprung’s disease colon
In this congenital disorder there is absence of
ganglia of the submucosal and myenteric
neural plexuses, within a portion of the
intestinal tract. The outcome is contraction
and functional obstruction of the aganglionic
segment (arrows) with secondary proximal
dilation.
SI - Malabsorption
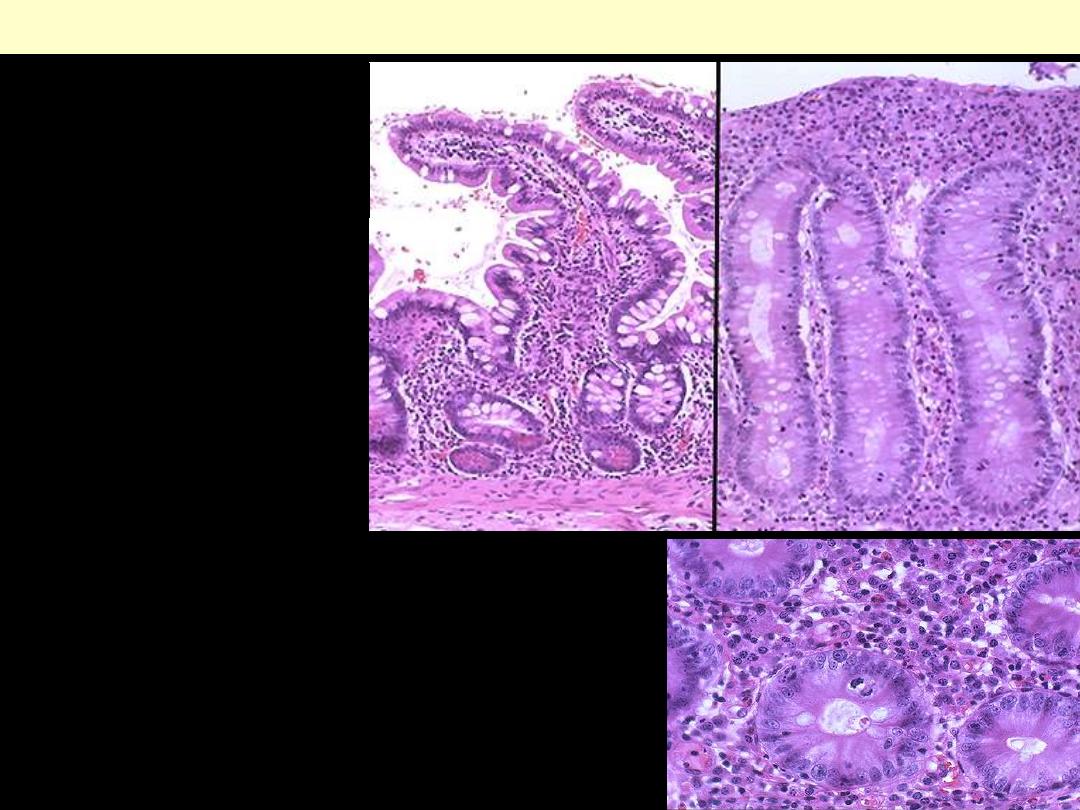
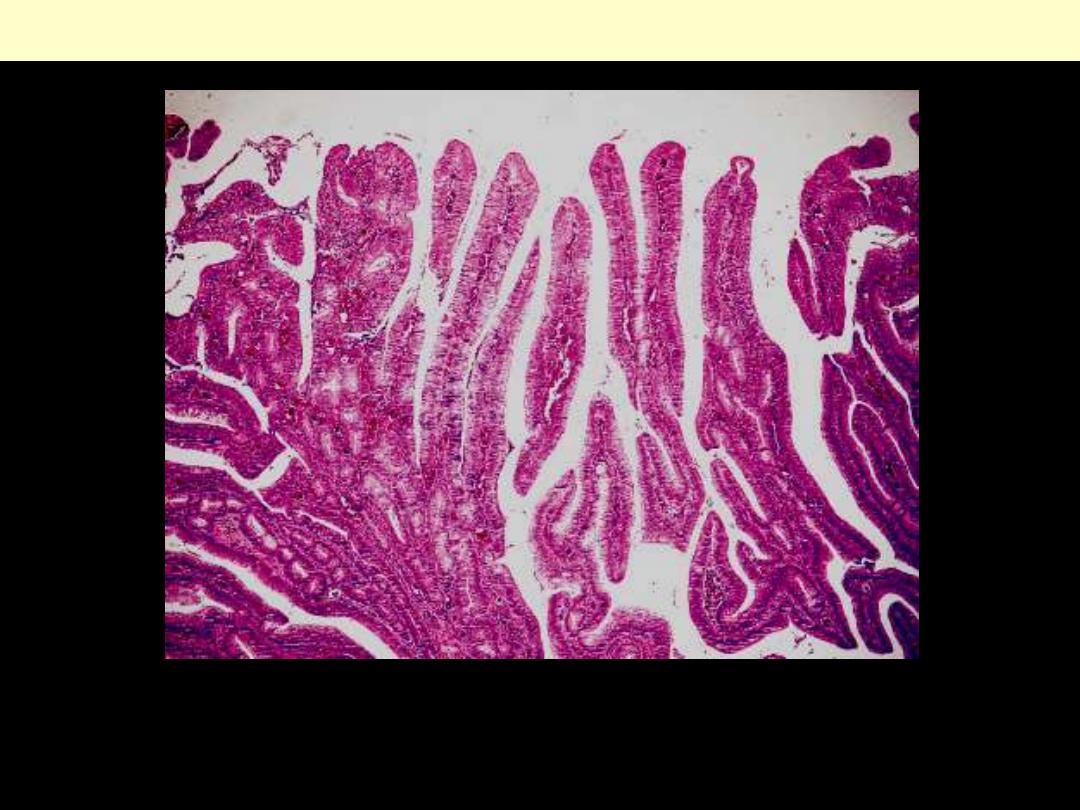
Normal small intestinal mucosa is
seen at the left, and mucosa
involved by celiac sprue at the
right. There is loss of villi with
flattening of the mucosa
*
.
Comparison between normal mucosa and that of celiac disease
The small intestinal mucosa at high magnification shows marked
chronic inflammation in celiac sprue. The enteropathy shown here has
loss of crypts, increased mitotic activity, loss of brush border, and
infiltration with lymphocytes and plasma cells.
Celiac disease small intestine mic
Jejunal mucosa in celiac disease. It is totally flat and devoid of villi, but its height is not decreased.
SI – Meckel’s diverticulum
A to D, Meckel’s diverticulum that
has undergone intussusception, as
seen from the serosal side (A, B) and
the mucosal side (C, D).
Meckel's diverticulum

This is a Meckel's diverticulum from an adult that was excised because of blood loss from ulceration (a
small red ulcer is seen. Meckel's diverticula may contain ectopic gastric mucosa (which can ulcerate
surrounding mucosa with pain and bleeding) or ectopic pancreas (which is of no consequence unless it
forms a mass large enough to predispose to
intussusception).
.
Meckel's diverticulum
Oral cavity
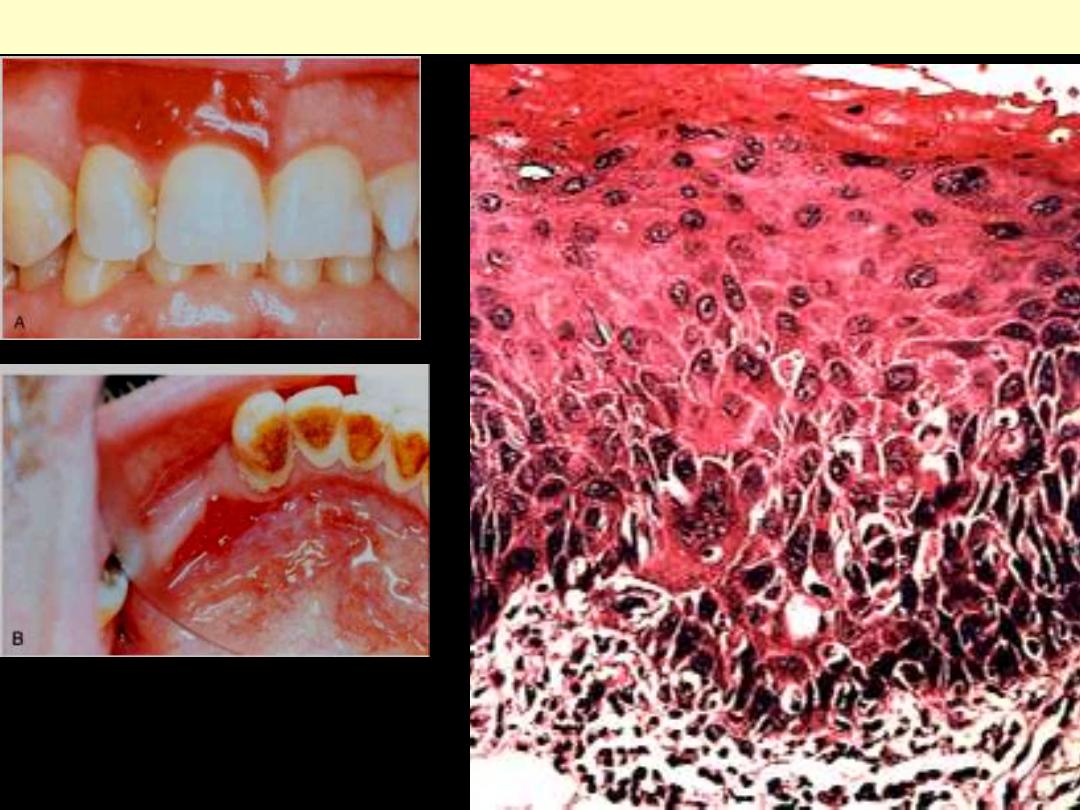
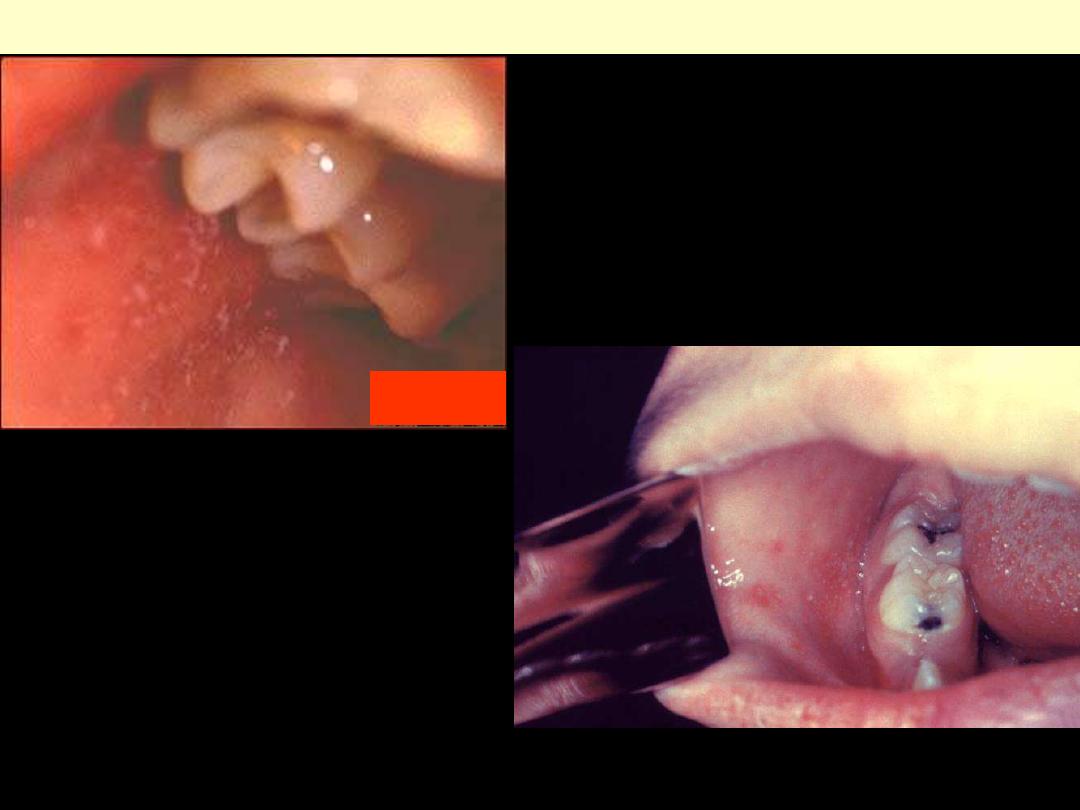
Gingivitis

Chronic gingivitis with dental plaques & calculi
The gingiva is congested & swollen with the
deposition of plaques at those portions of the teeth
near the gingiva. Note gum recession and loss
(arrow).
Conversion of the plaques into calculi.
Inflammatory lesions

Aphthous ulcer
Single ulceration with an erythematous halo
surrounding a yellowish fibrinopurulent membrane.
This is a picture of aphthous ulcers which are
often confused with cold sores, but they are not
caused by the herpes virus. Apthous ulcers can
occur anywhere in the mouth but
do not
involve the outside of the lip.
Someone who has
herpetic stomatitis (herpes ulcers throughout
the mouth caused by an initial oral herpes
infection) may have ulcers in the mouth, but
they will typically have cold sores on the lip
also.
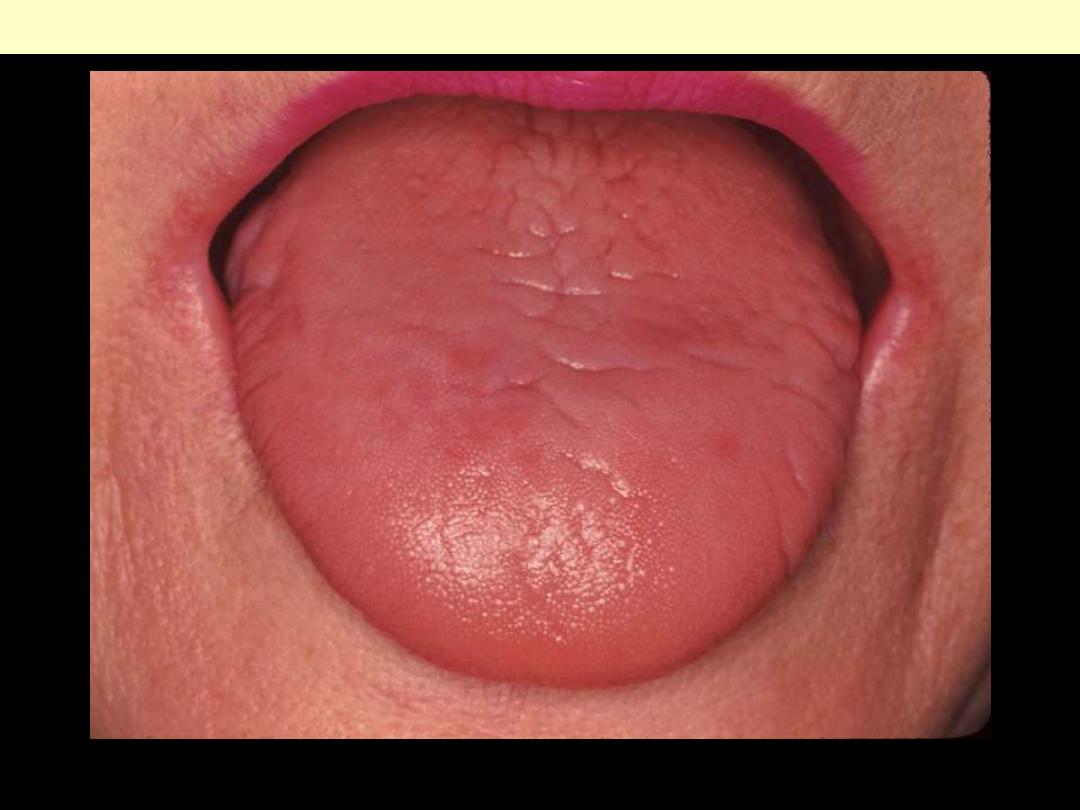
Glossitis
Smooth red tongue secondary to atrophy of the papillae
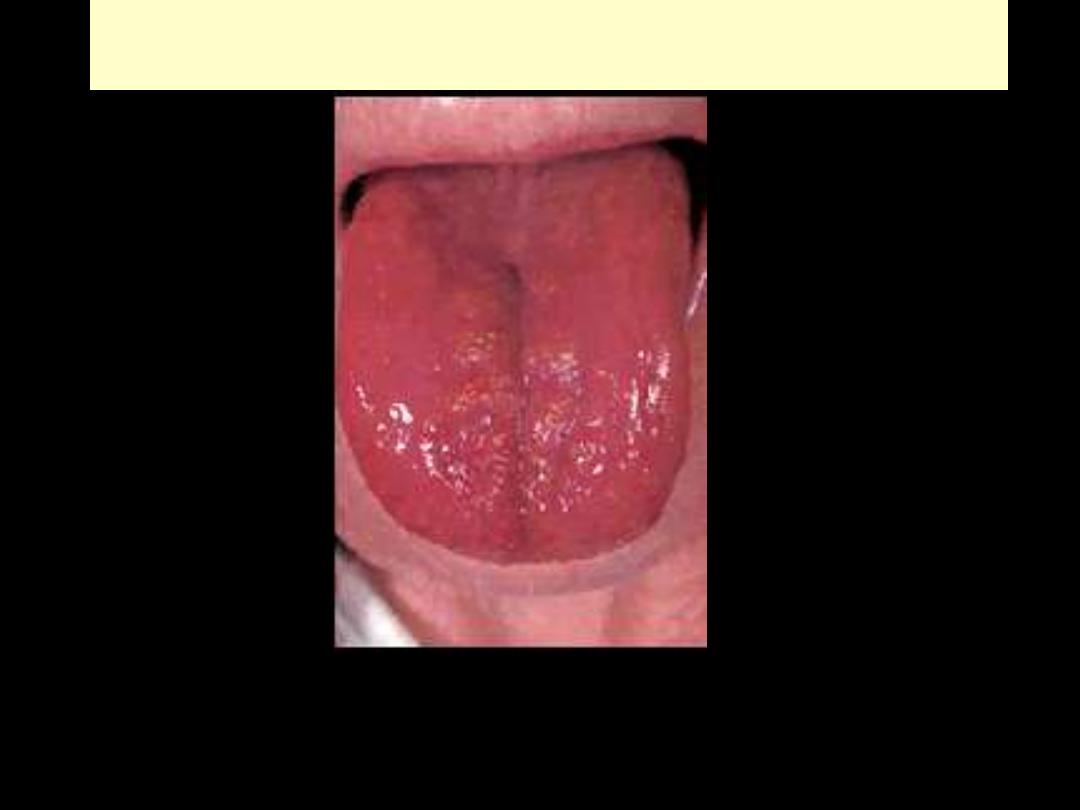
Glossitis
A red, smooth tongue may be seen in patients with nutritional deficiencies.
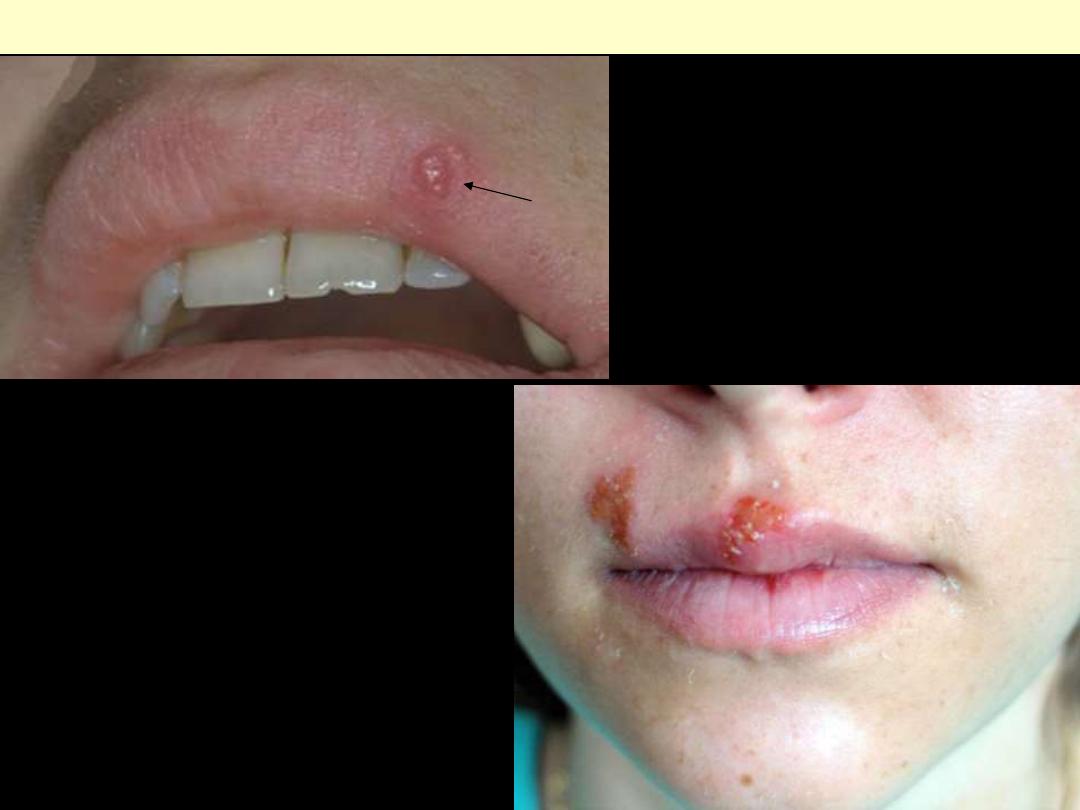
Herpes labialis
Typical appearance of cold sores; to begin
with there is formation of vesicles followed
by rupture with the ulcer having
hyperemic borders & covered by honey-
colored scales.

Gingivostomatitis Herpetica
acute herpetic gingivostomatitis,
characterized by vesicles and ulcerations
throughout the oral cavity including the lips.
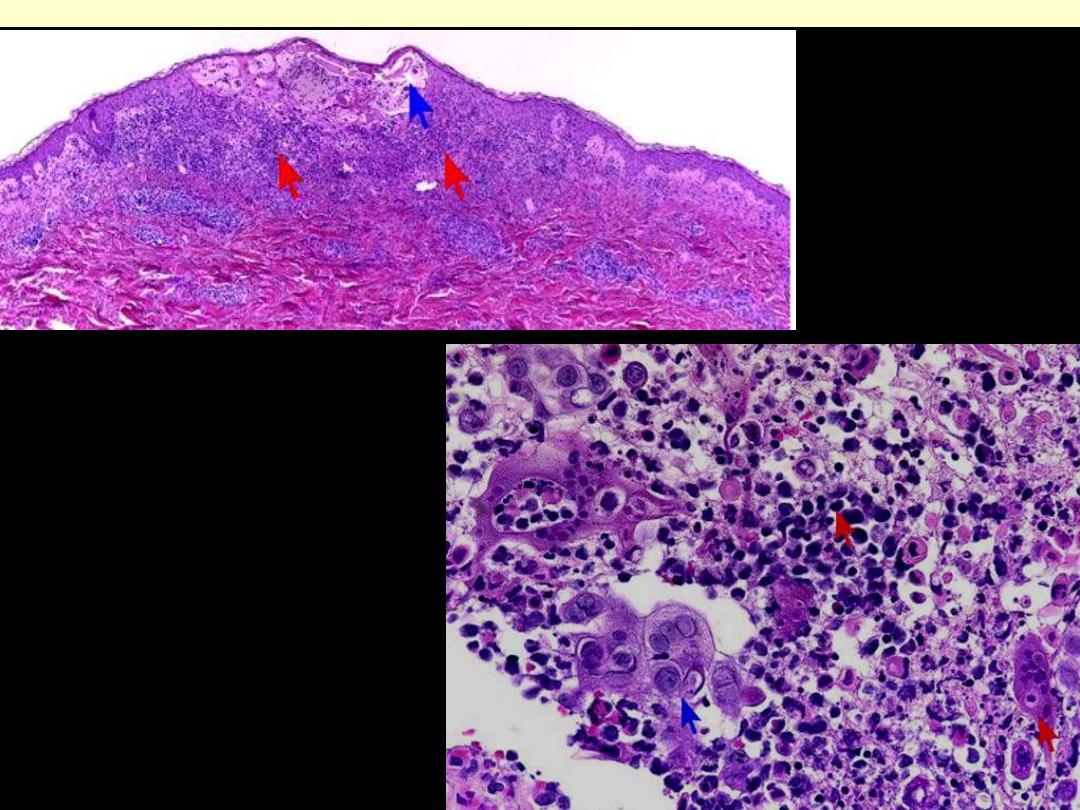
Vesicle in the epidermis
due to squamous cell
ncrosis & acantholysis
Characteristic nuclear changes:
Multinucleation, Molding,
Chromatin margination
Herpes simplex infection of the lip

Oral thrush in a child
Oral thrush in an adult
Oral candidiasis
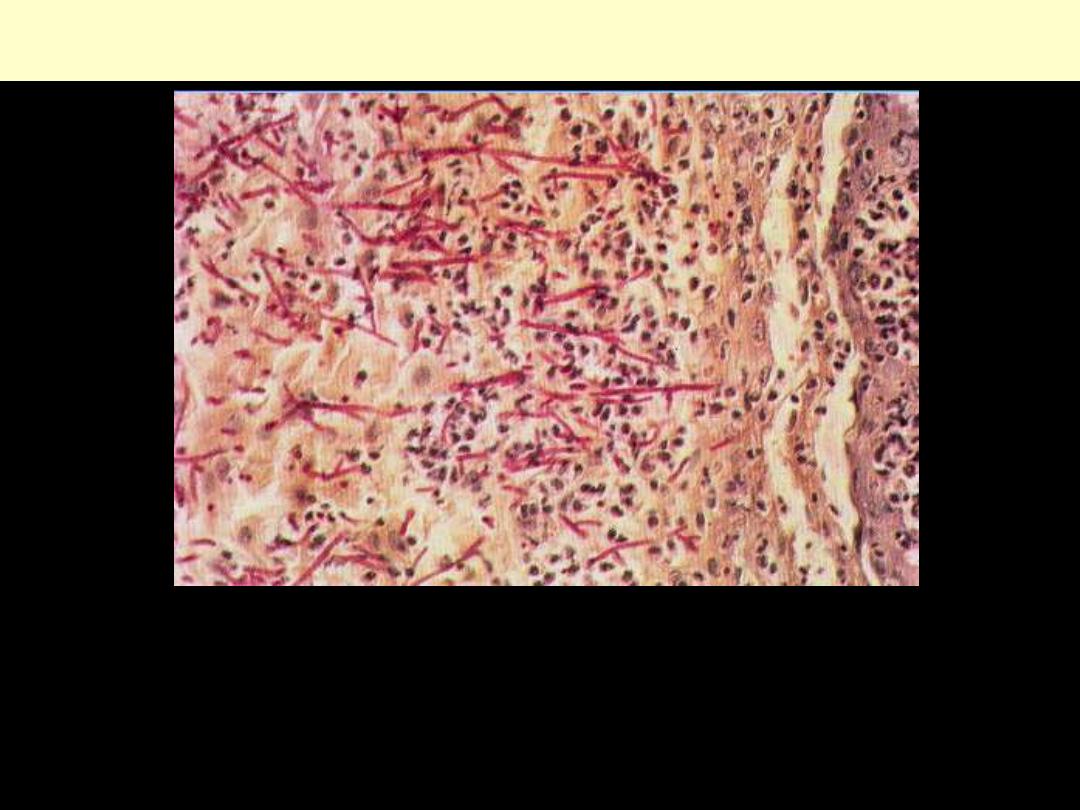
Candida albicans hyphae PAS stain
Oral Candidiasis: (PAS x 360); the periodic acid-Schiff (PAS) method stains the hyphae of Candida
albicans purplish-red. Dense clumps of hyphae (approx. 1 mm thick), present on the surface of the
stratified squamous epithelium, are invading the epithelium almost to the basal layer (right).
Desquamating cells (left) mingle with the hyphae. The epithelium is tending to separate from the basal
layers (right). Inflammatory cells (polymorph leukocytes and lymphocytes) are present throughout
the epithelium and in the submucosa (right). All the constituents mentioned above form the clinically
seen thrush

DIPHTHERIA
Dirty white, fibrinosuppurative, tough, inflammatory pseudomembrane over tonsils & posterior
pharynx
Proliferative lesions
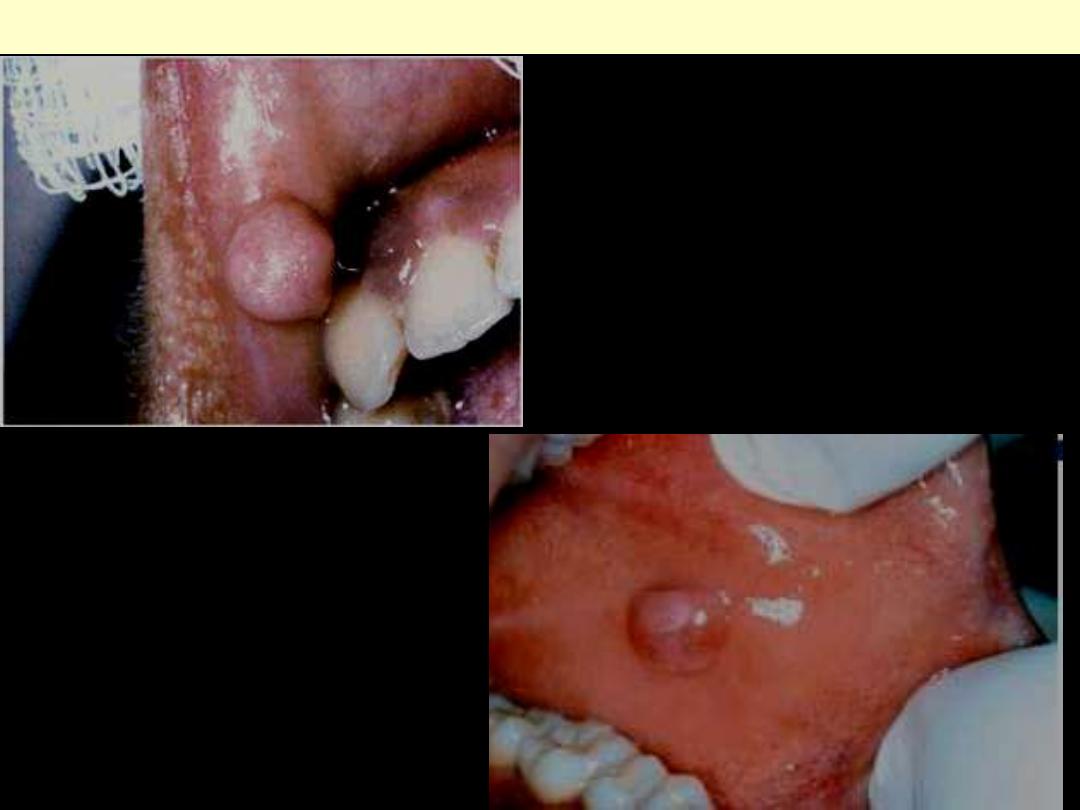
A mucosa-covered nodule firm mass (of fibrous
tissue) that occurs mainly in the buccal mucosa
along the bite line.
Irritation fibroma
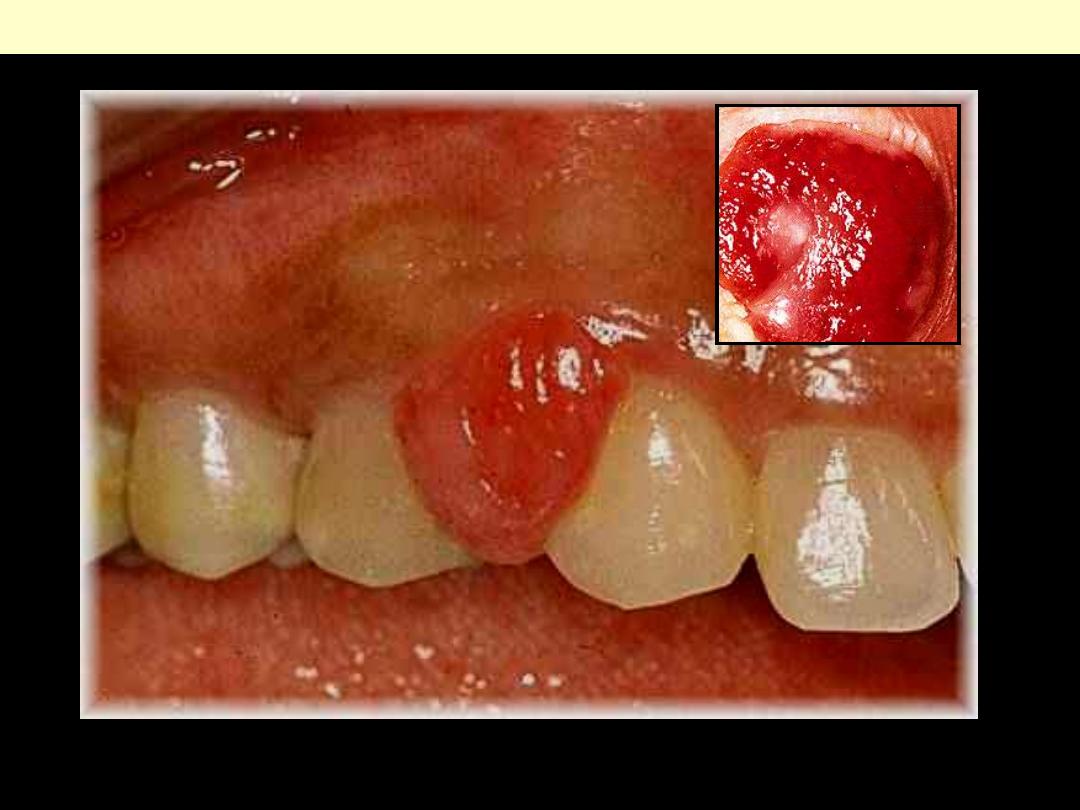
PYOGENIC GRANULOMA
A localized bright red gingival mass. Inset is a close up view
The lesion consists of proliferating small blood
vessels within a connective tissue stroma. It is
covered by stratified squamous epithelium (oral
mucosa)
PYOGENIC GRANULOMA
Higher magnification of the above.
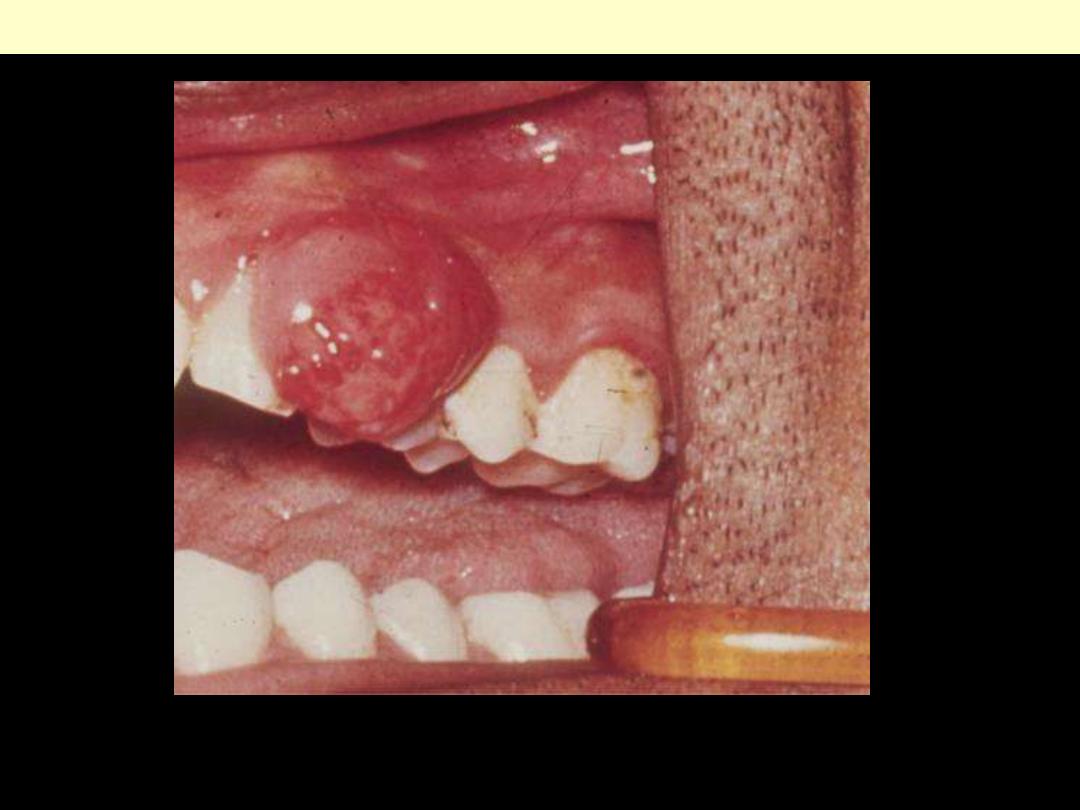
Peripheral Giant Cell Granuloma
A protruding reddish gingival mass
Peripheral Giant Cell Granuloma
Aggregates of multinucleate giant cells separated by a
fibro-vascular stroma.
Tumors

LEUKOPLAKIA
This is highly variable and can range from A, smooth and thin with well-demarcated borders. B,
diffuse and thick. C, irregular with a granular surface. D, diffuse and corrugated.
ERYTHROPLAKIA
A, Lesion of the maxillary gingiva. B, Red
lesion of the mandibular alveolar ridge.
Biopsy of both lesions revealed severe
dysplasia amounting to CIS
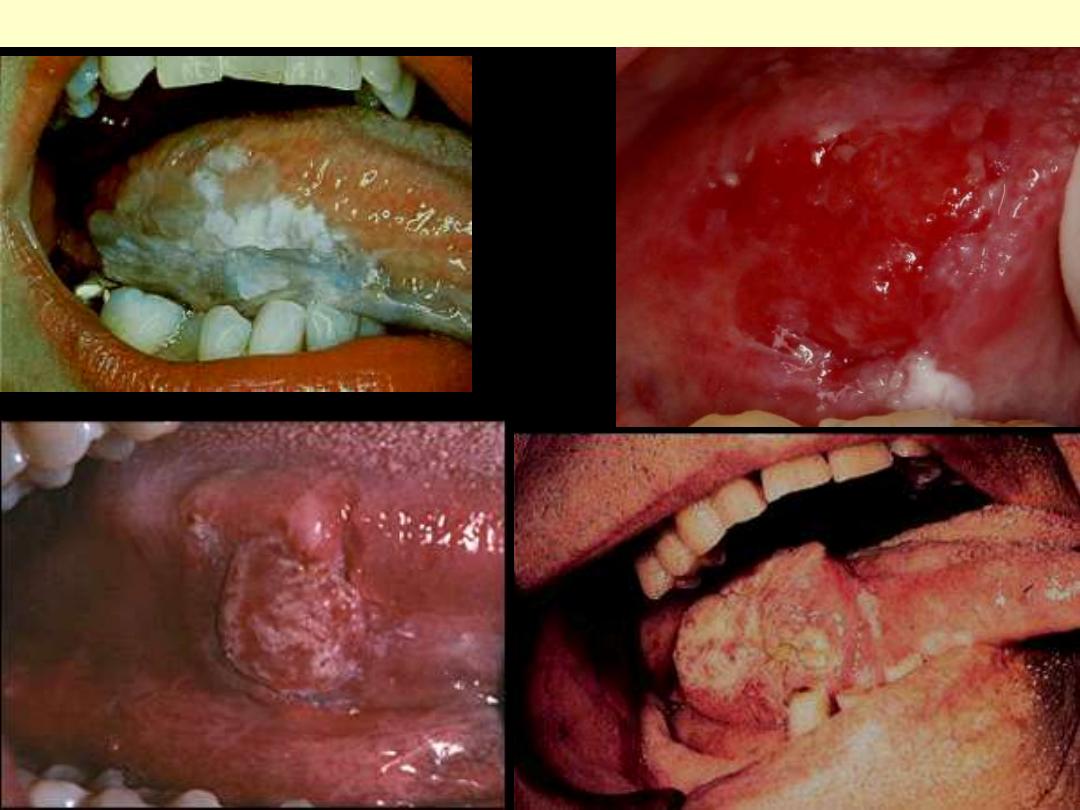
SQUAMOUS CELL CARCINOMA LATERAL BORDER OF TONGUE
Leukoplakia-like
ulcerative
Fungating
Erythroplakia-like

A squamous cell carcinoma presenting as a
verroucous keratotic lesion of the marginal
gingiva, in a 54 year old male patient.
D
Squamous cell carcinoma of the lower gingiva.
Presenting as a deeply ulcerative lesion, in a
65 year old female patient.
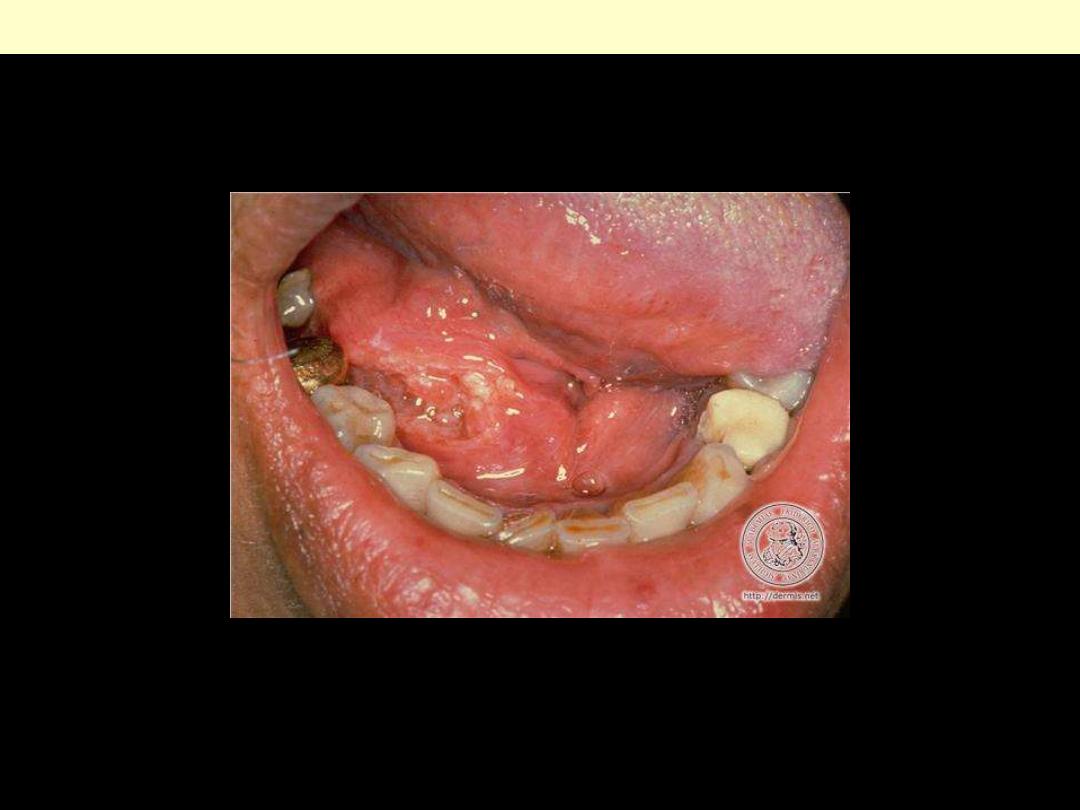
Floor of Mouth Squamous Cell Carcinoma
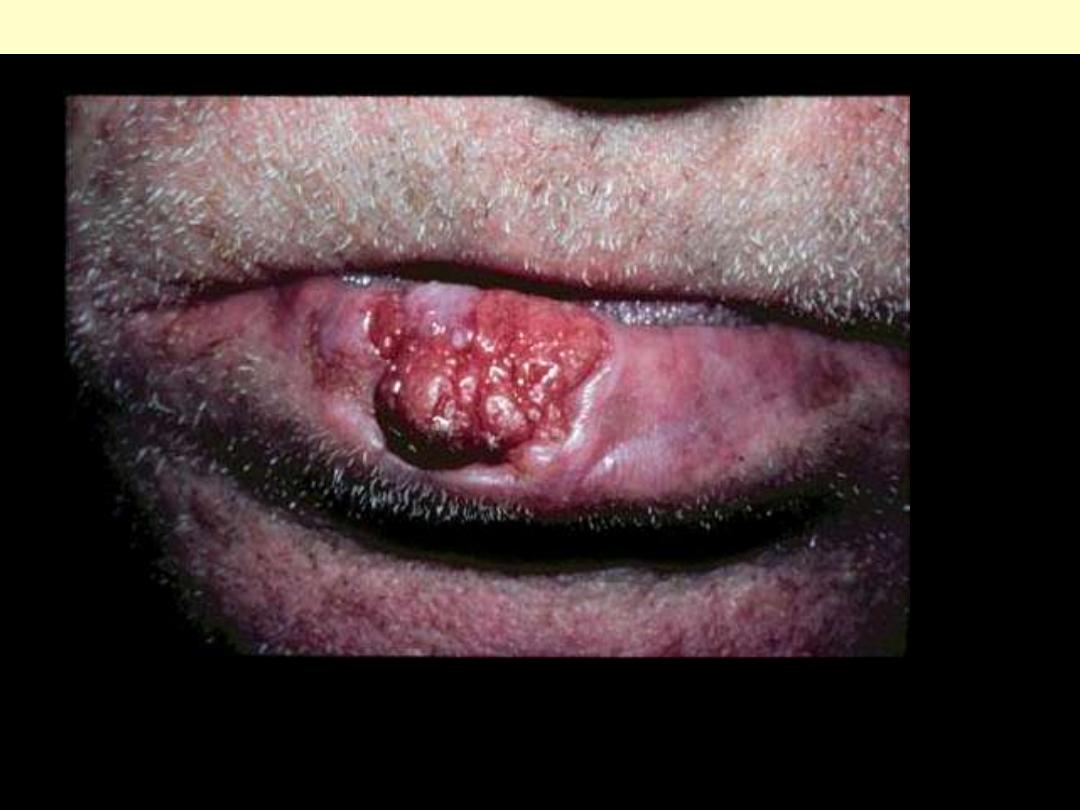
Indurated, slowly growing lesion of the lower lip.
SCC Lip
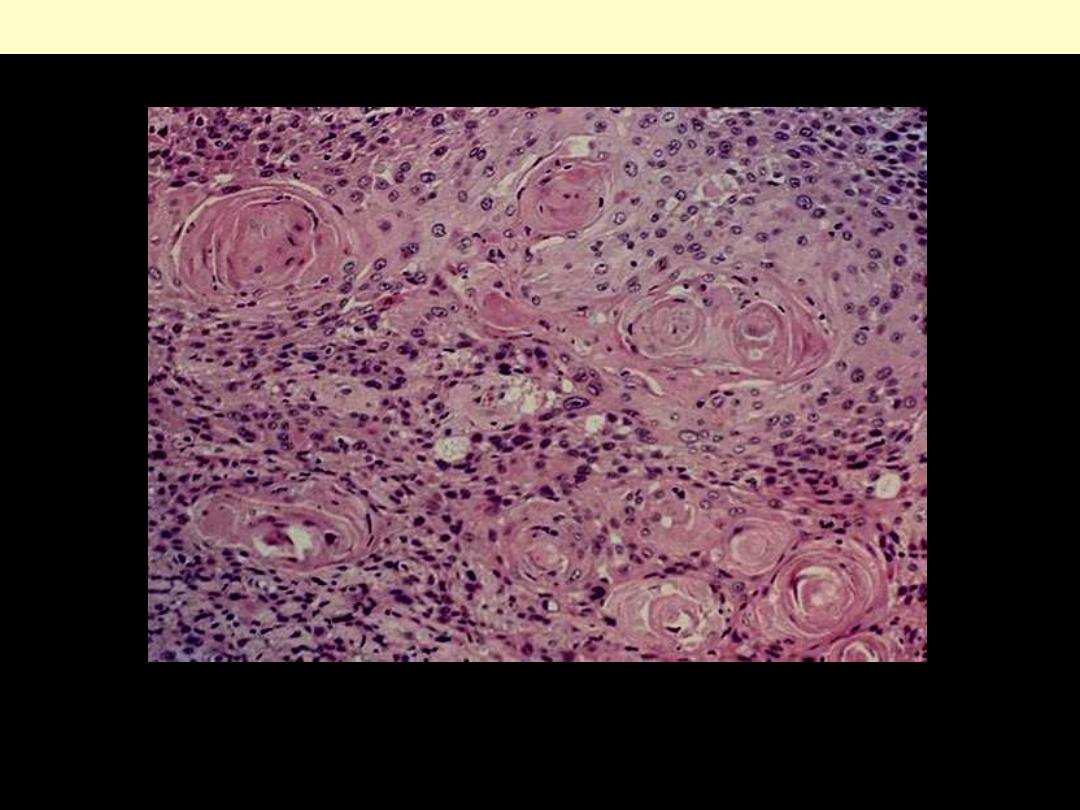
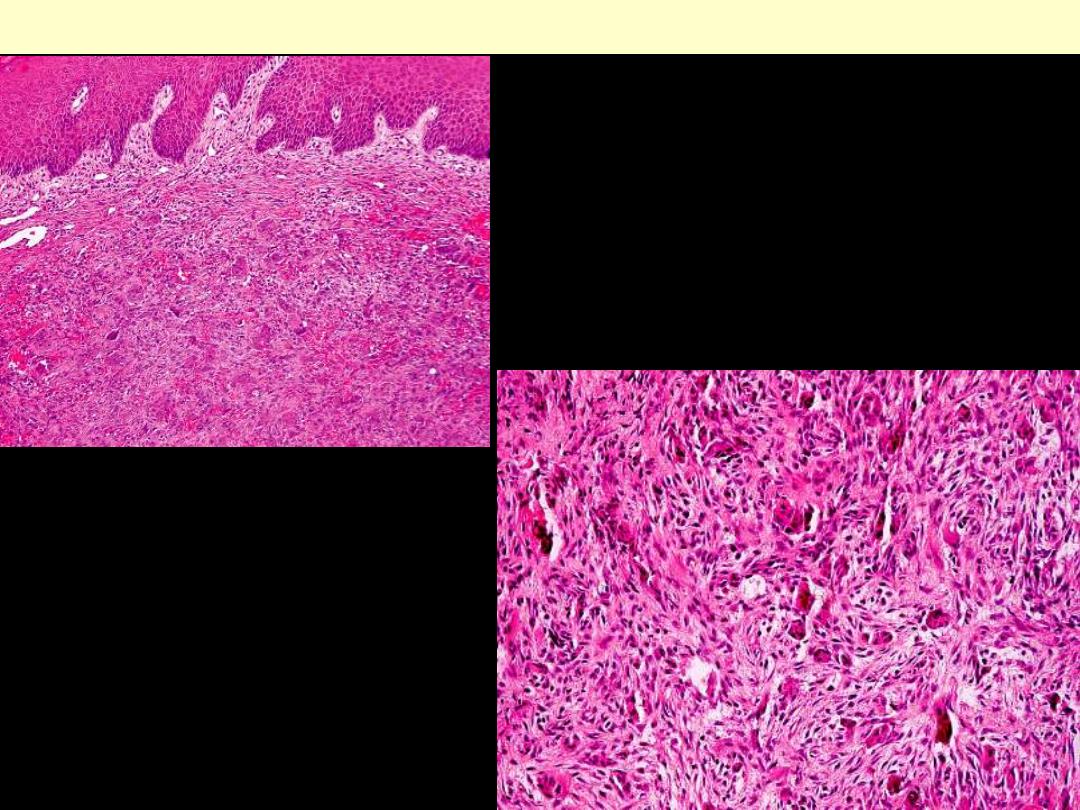
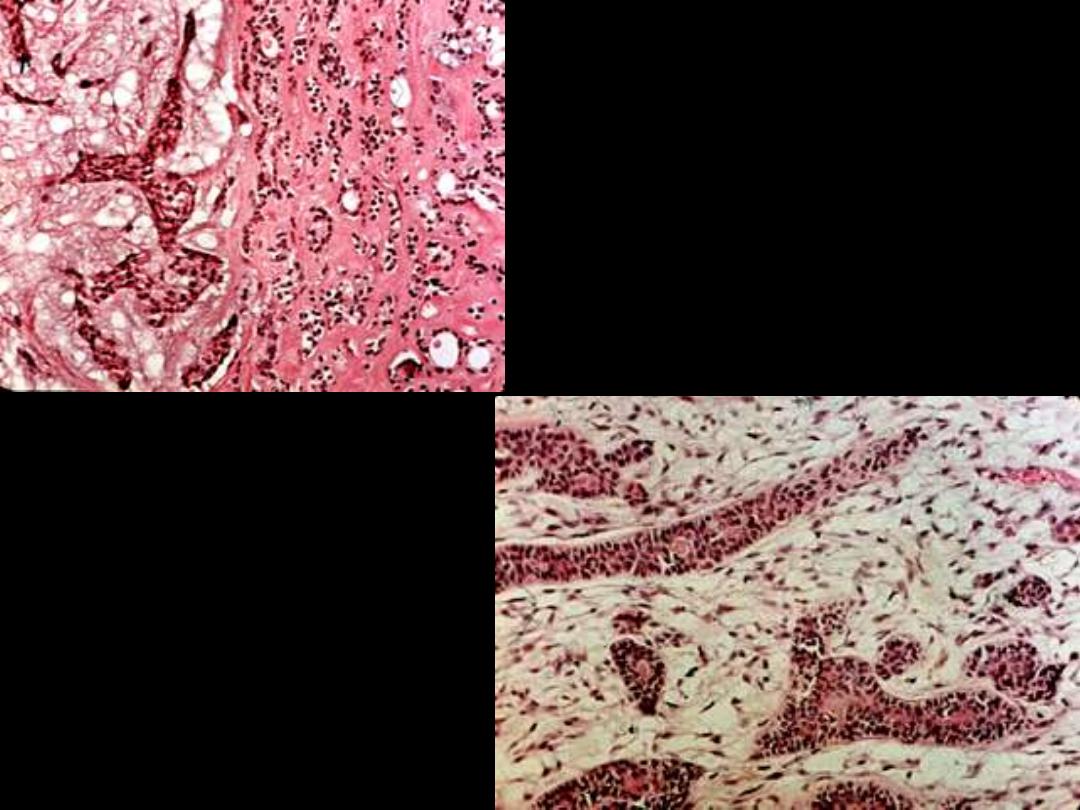
Well-differentiated SCC
Sheets of well-differentiated SCC showing keratin nests.
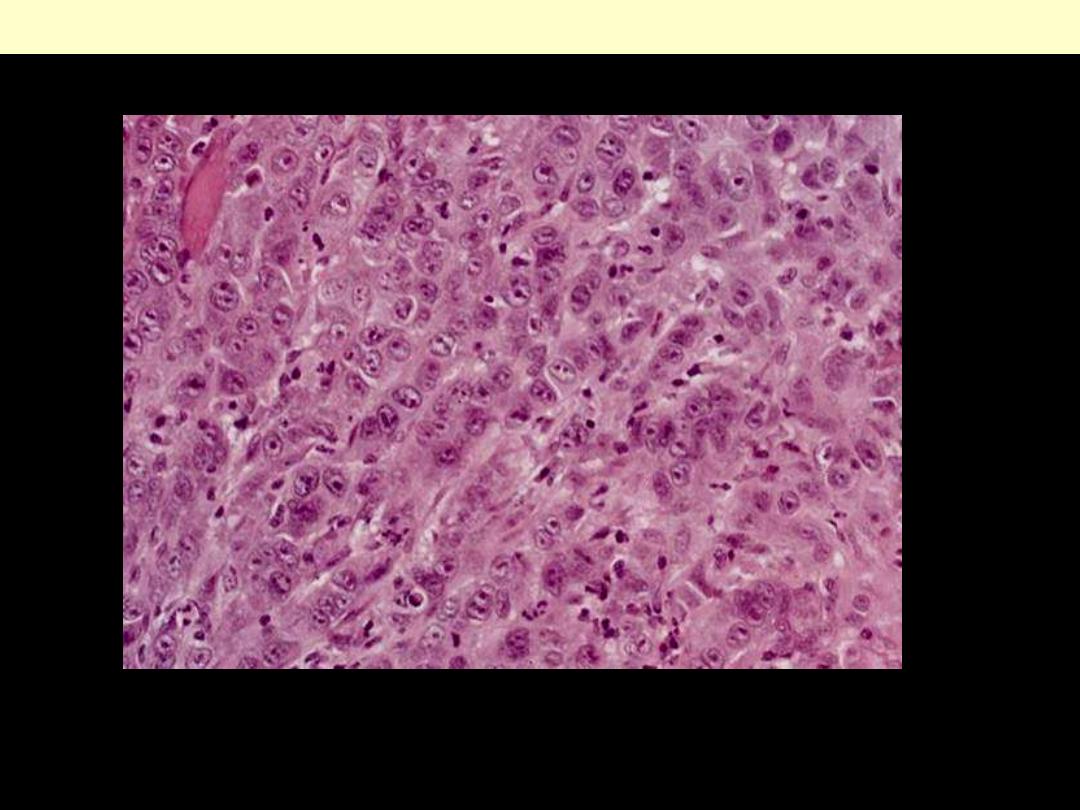
Round cells without obvious squamous differentiation
Poorly-differentiated SCC
Oral manifestations of systemic
diseases
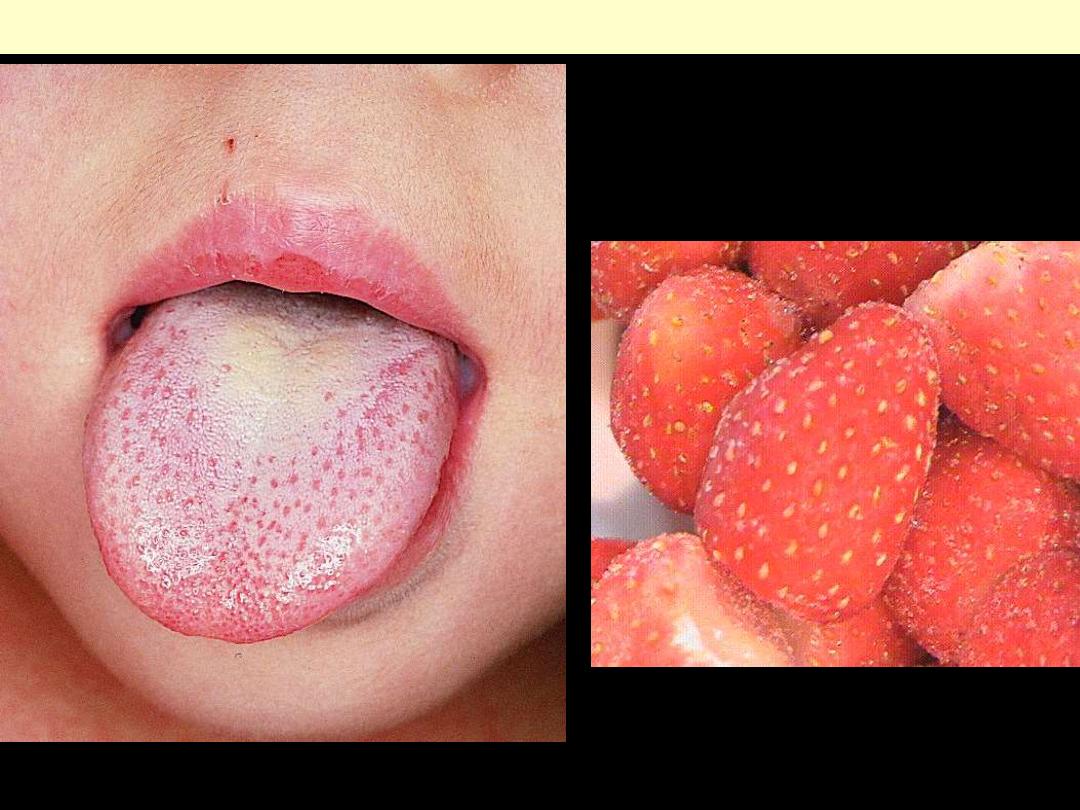
Strawberry tongue of scarlet fever
White coated tongue with hyperemic papillae projecting
Small, white ulcers (spots) on a reddened background that occur on the inside of the cheeks
early in the course of measles.
Koplik spots of measles
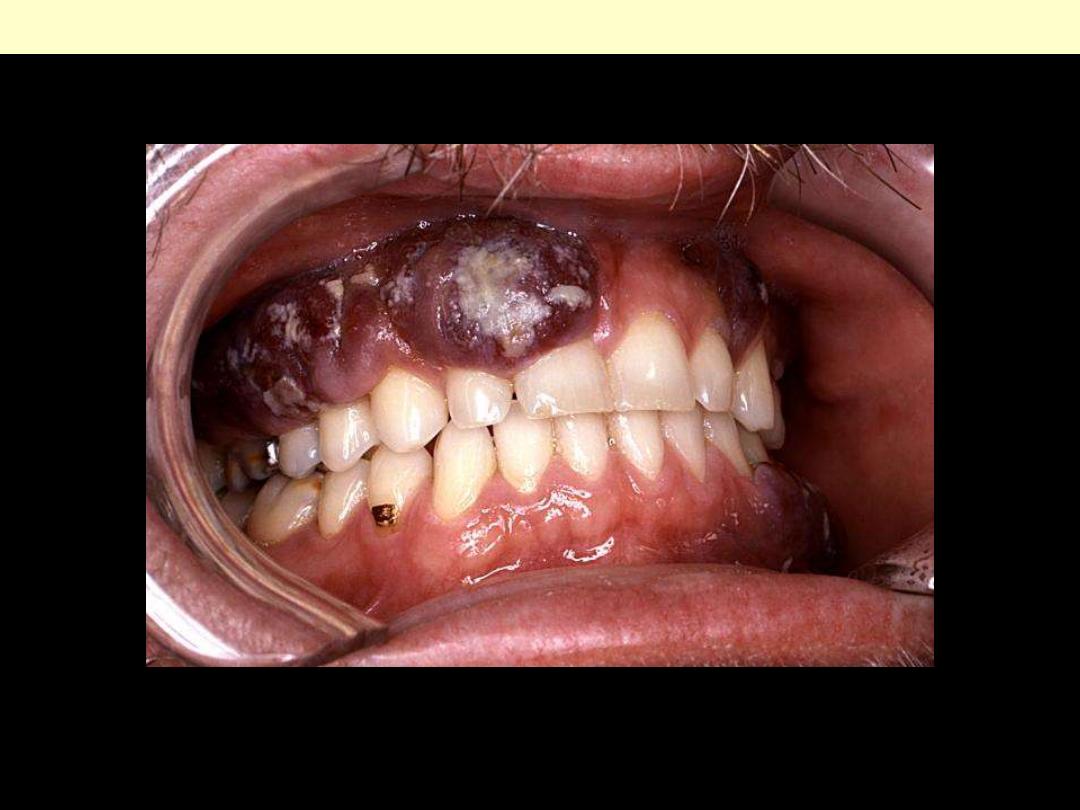
This HIV-positive patient presented with an intraoral Kaposi’s sarcoma lesion with an overlying
candidiasis infection. Initially, the KS lesions are flattened and red, but as they age they become raised,
and darker, tending to a purple coloration.
Kaposi sarcoma of AIDS

Gum in AML
Acute myeloid leukemia may present as gum infiltrates, especially in cases of acute
myelomonocytic leukemia (FAB M4) and monoblastic leukemia (FAB M5).
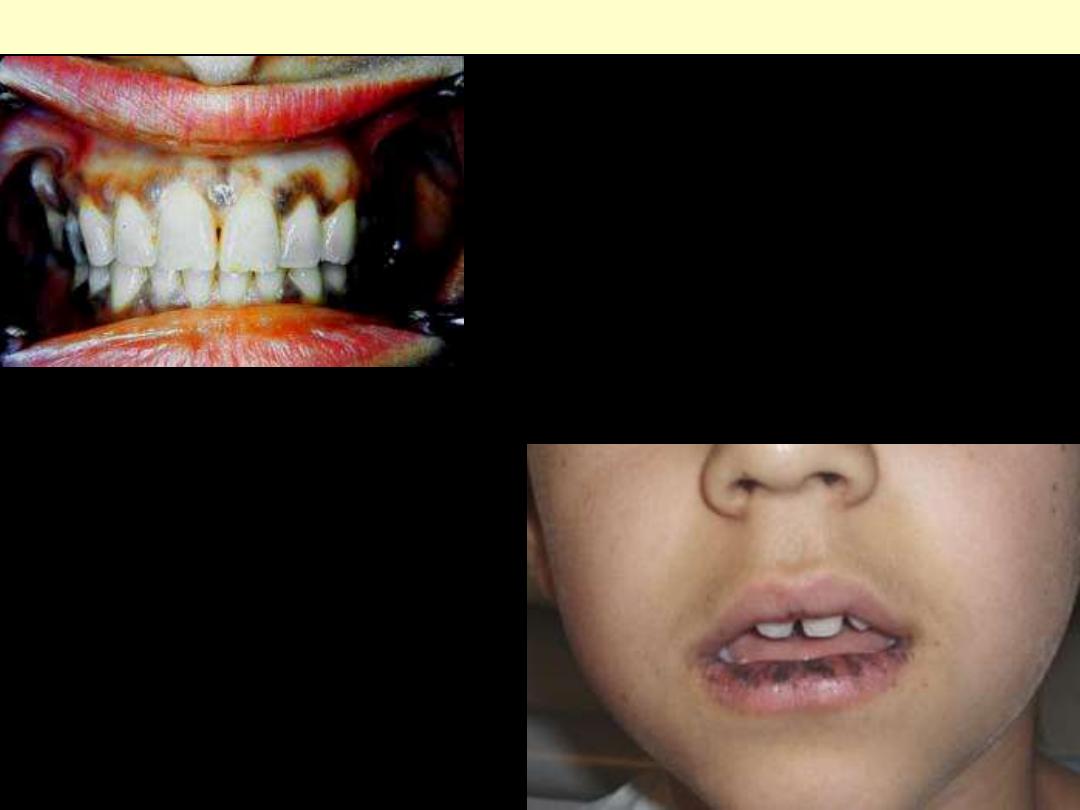
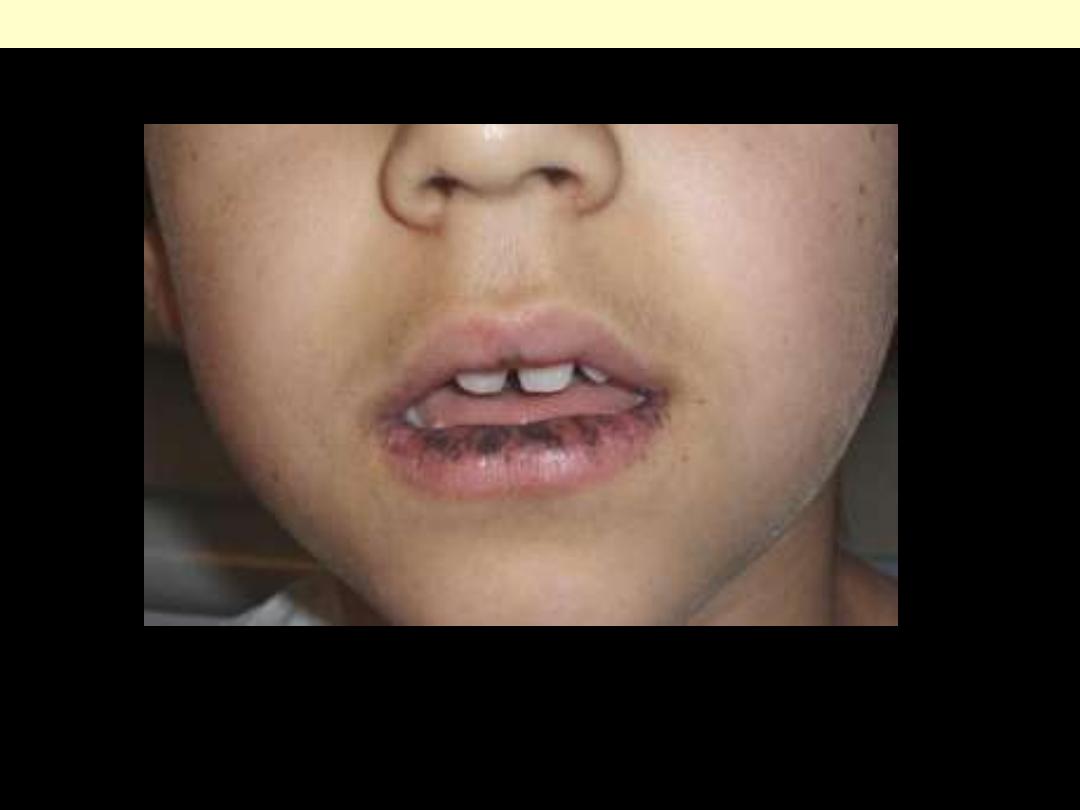
Mouth melanotic pigmentation in various diseases
Addison disease
Peutz Jegher syndrome
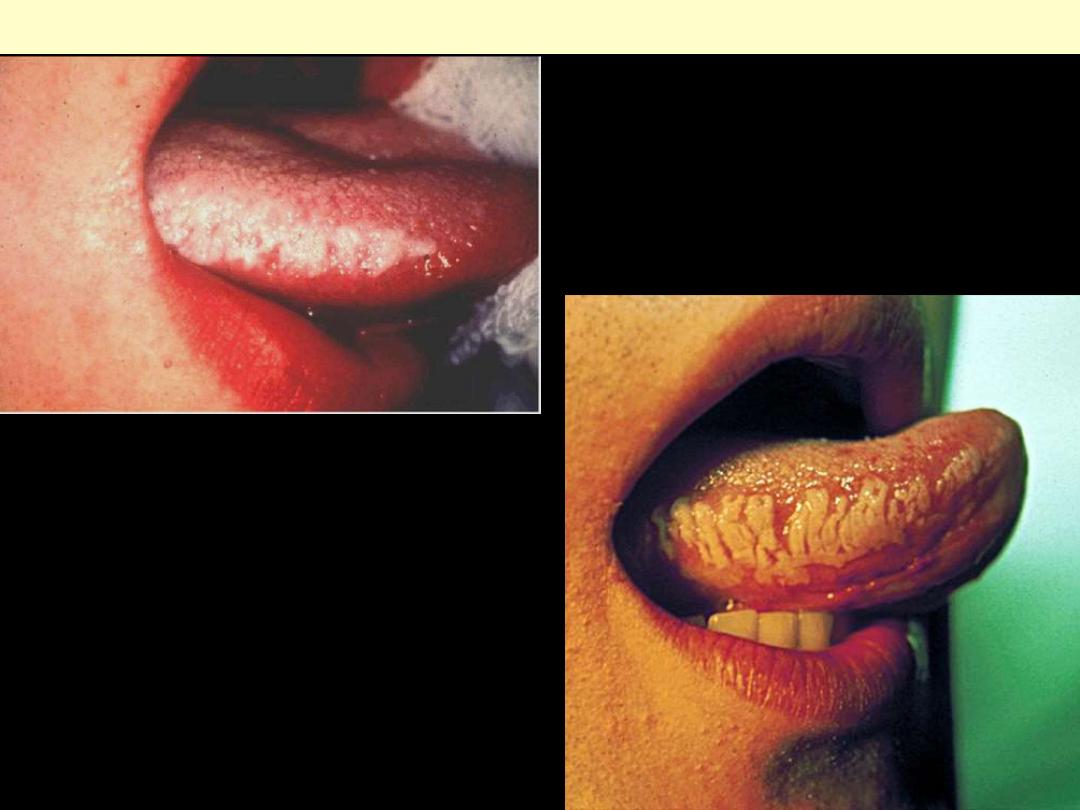
White, confluent patches of fluffy
("hairy"), hyperkeratotic thickenings,
almost always situated on the lateral border
of the tongue.
Hairy leukoplakia tongue
Salivary glands
Mucocele

Bluish dome-shaped fluctuant swelling, lower left labial
mucosa
Mucocele
Mucocele: nodule involving the lower
labial mucosa.
Mucocele
Cystic space containing mucin and inflammatory
cells is surrounded by inflammatory tissue with
dilated vessels. The lining of the cyst is made up of
histiocytes rather than epith. cells
This is mucocele (mucous retention cyst)
involving a minor salivary gland of the oral
cavity which was removed surgically. The duct
from the small gland became obstructed and led
to the expansion of the gland with secretions to
form the small, smooth-surfaced mass seen.
Sialolithiasis

Salivary sialolithiasis
Sialolithiasis with secondary chronic sialadenitis. A
large stone is blocking a major salivary duct.
Wharton's duct is much more commonly
involved by a sialolith than is Stensen's duct.
chronic inflammatory cell infiltrates
along with fibrosis and acinar atrophy
At HP, the numerous lymphocytes of chronic
sialadenitis are seen adjacent to a duct
Chronic sialadenitis
Tumors
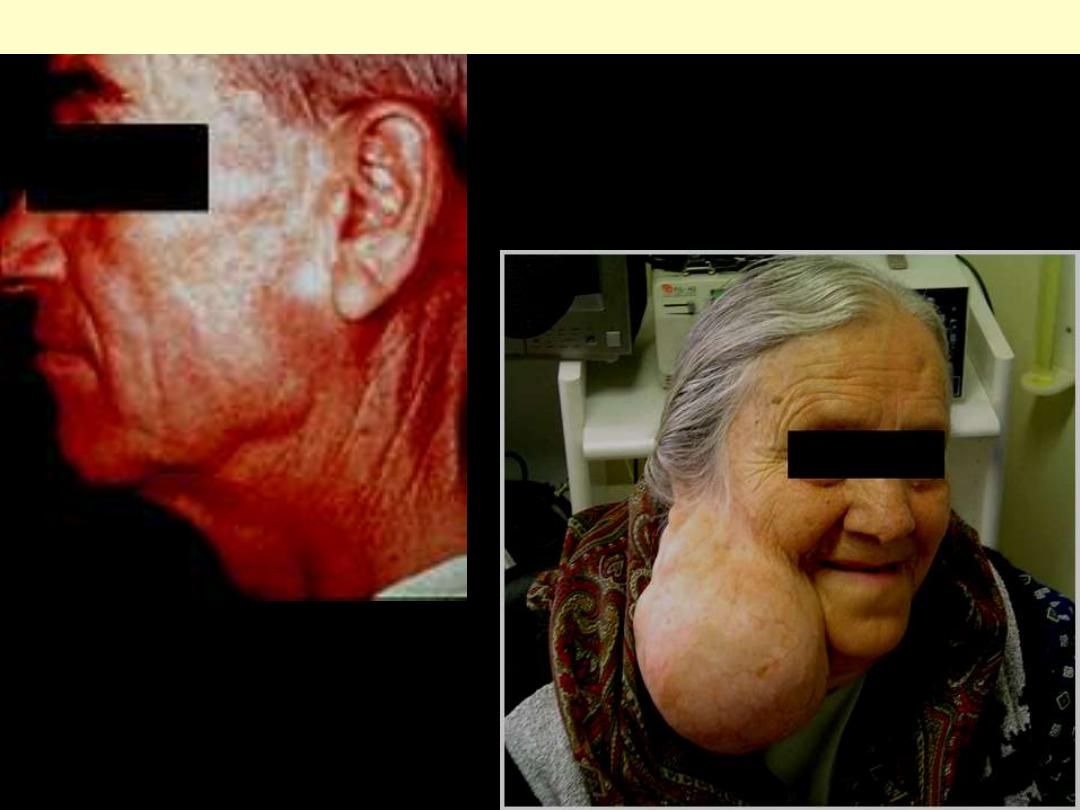
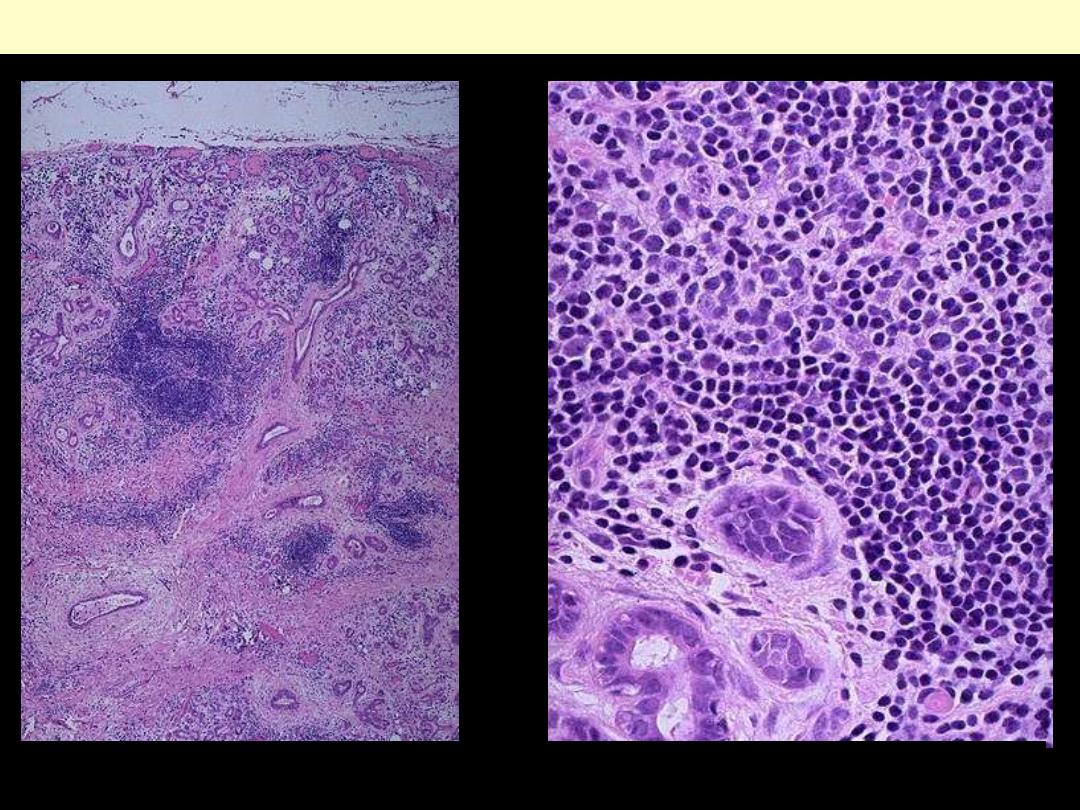
Clinical presentation of parotid gland tumors
Rounded, encapsulated mass/rarely exceed 6 cm Ө. C/S gray-white with myxoid and blue translucent
areas of chondroid tissues
Pleomorphic adenoma of the parotid gland
The LP pleomorphic adenoma (mixed tumor) of salivary gland is shown extending into surrounding
normal parotid gland*.
Pleomorphic salivary adenoma
Epithelial duct-like structures are seen in loose
and dense connective tissue stroma
The neoplastic ducts are surrounded by a
myxomatoid stroma. Also note the
eosinophilic secretory product in the
epithelial duct.
The glandular epithelium dominates this
section.
Sheets of epithelial cells with some keratin
"pearls" are evident in this section.
The stroma has a "cartilagenous" appearance;
blood vessels are also prominent in this section.
Epithelial ducts in a dense c.t. stroma that
resemble ostoid material, an observation
supported by the nearby calcified bone.
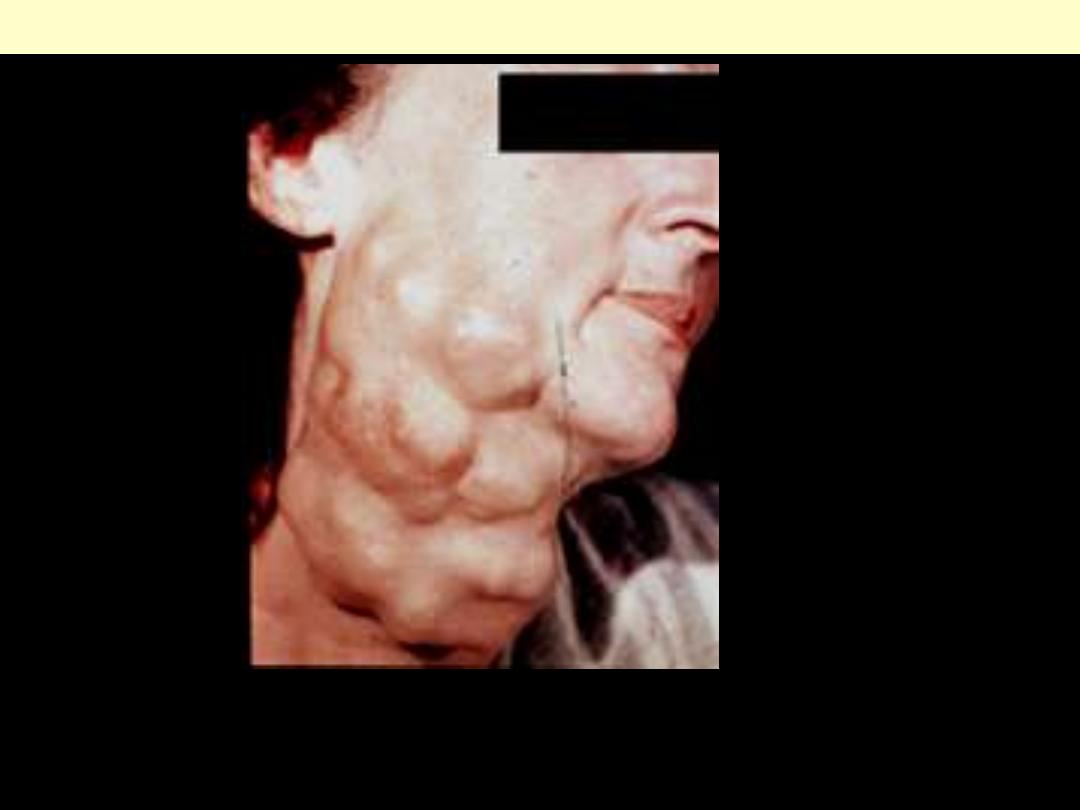
Recurrence of mixed tumor Although this is a bizarre example, it demonstrates well the
multinodularity so typical of recurrent tumor. The reason for this is that during the first surgical
procedure many small pieces of tumor were distributed throughout the operative site and each
formed the nidus for a recurrent mass.
Recurrent mixed salivary gland tumor
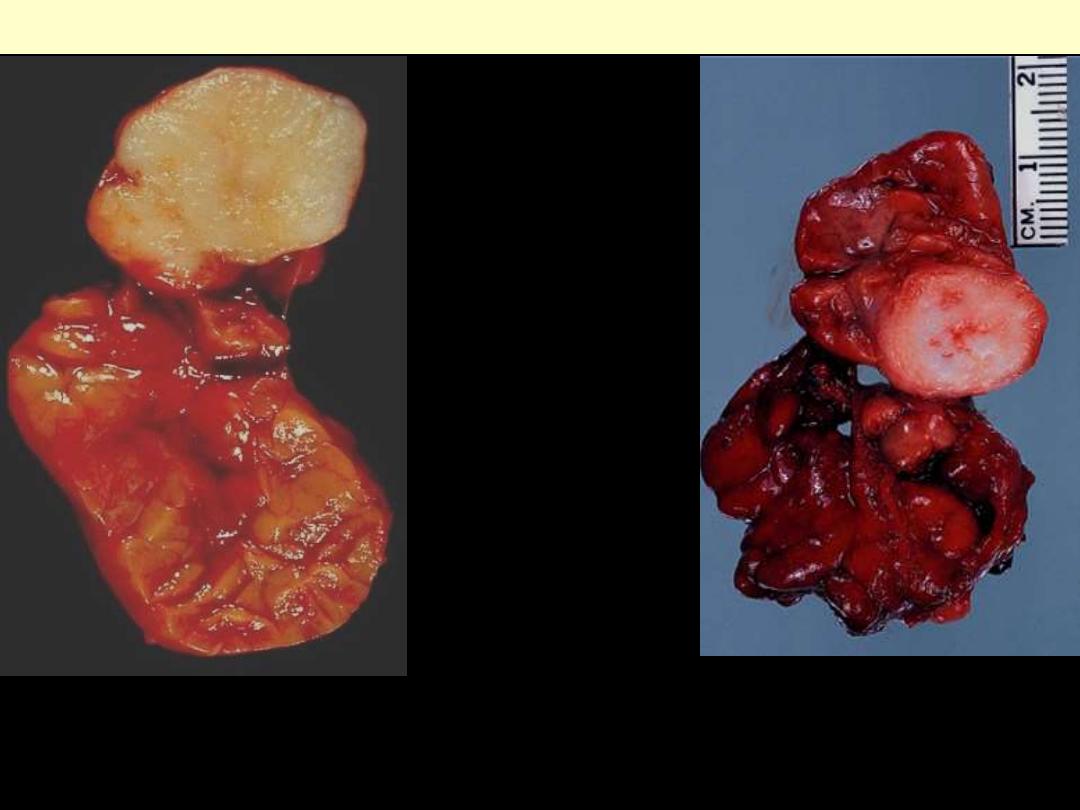
Round to oval encapsulated mass, up
to 5 cm Ө/pale gray surface
punctuated by cleft-like spaces/ filled
with a mucinous/serous secretion.
Warthin tumor
These tumours are
multicystic. The cysts are
filled with mucus, as
indicated. They are benign
tumours and are the second
most frequent tumour of the
parotid gland, following
pleomorphic adenoma.
Cystic spaces narrowed by lymphoepithelial
papillary structures
- Double layer of oncocytic epithelial cells resting on a lymphoid stroma/germinal centers
- Oncocytes: eosinophilic granular cytoplasm: stuffed with mitochondria
MUCOEPIDERMOID CARCINOMA
Sheets of squamous and mucous-secreting cells
In the minor salivary glands esp. palate (the most common malignant tumor)
Adenoid cystic carcinoma palate
Adenoid cystic carcinoma
•
Small cells with dark nuclei & scant cytoplasm
• Disposed in cribriform pattern
• Spaces filled with mucin & excess BM material
Adenoid cystic carcinoma with prominent perineurial invasion.
Adenoid cystic carcinoma
Nerve
Acinic cell ca microfollicular
The cells are reminiscent of normal acinar cells with basophilic granular cytoplasm. They are disposed
as lobules with glandular arrangement (as in normal salivary glands).
Stomach
Congenital pyloric stenosis
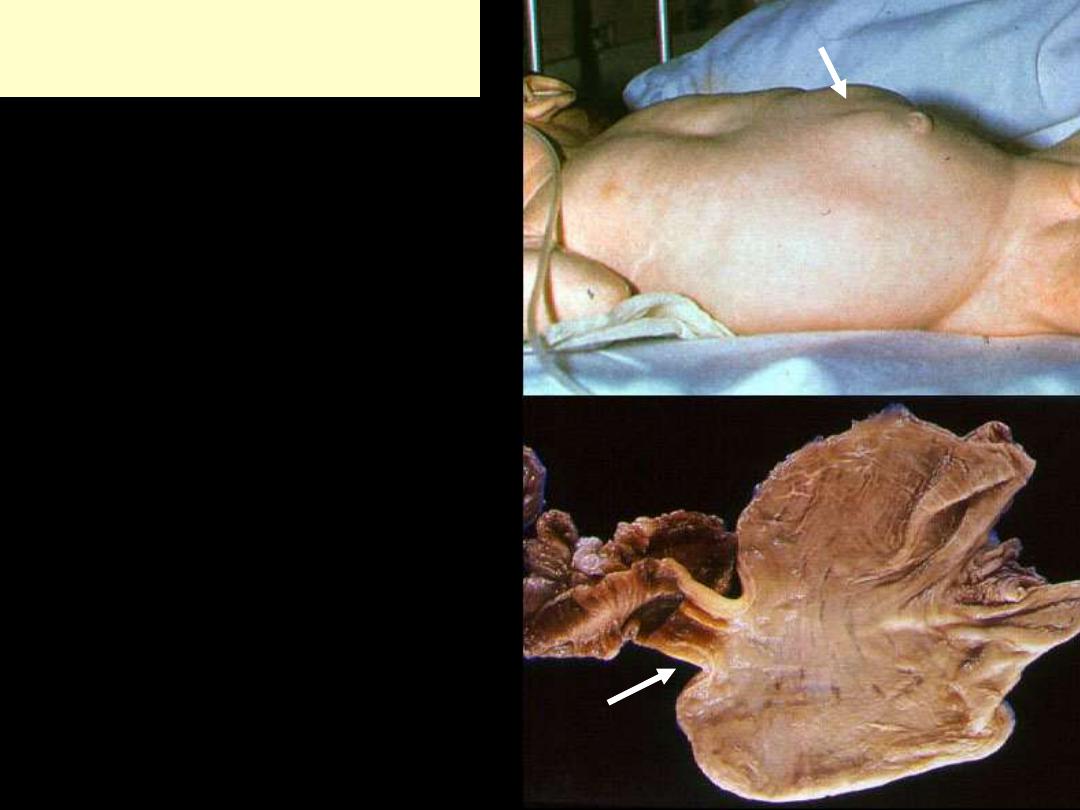
Congenital hypertrophic
pyloric stenosis
There is visible peristalsis (arrow) and a firm,
ovoid palpable mass in the region of the pylorus
Below, there is resulting thickening of the
muscularis propria of the pylorus resulting in
obstruction.
Gastritis
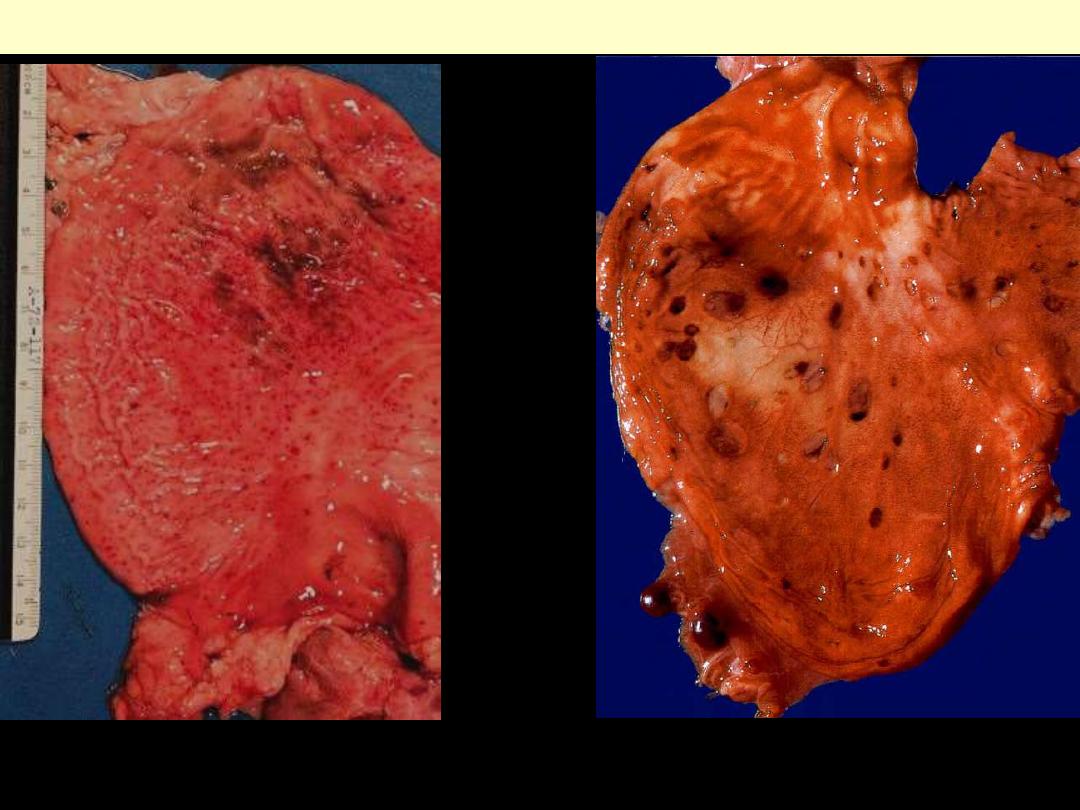
Acute hemorrhagic & erosive gastritis
Diffuse hyperemia with punctate
haemorrhages
Multiple generally small ulcers & erosions are
present.
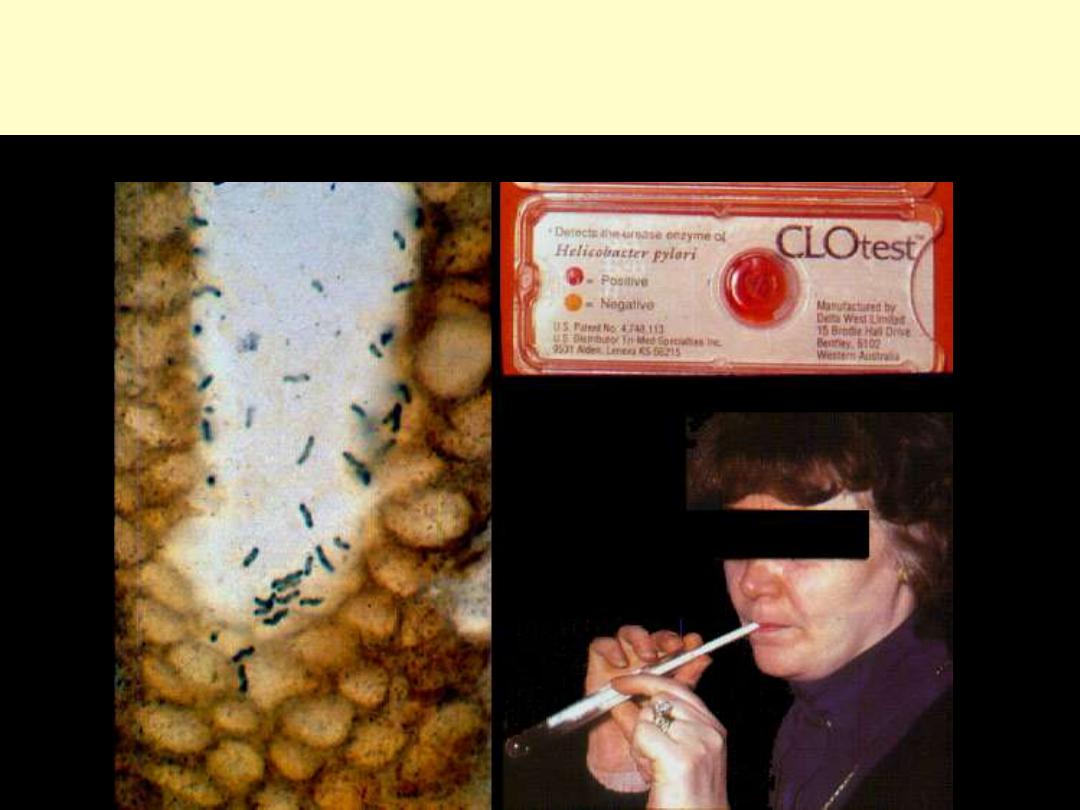
Helicobacter gastritis
Staining of the gastric biopsy shows the characteristic curved rods embedded in the mucin
layer of the stomach. Helicobacter organisms may be tested for urease activity.
Rod-shaped organisms are present along the luminal surfaces of the epithelium and in the
luminal mucus. They do not invade the mucosa. They are best seen on giemsa stain, where
they stain bluish-purple.
H. pylori gastritis (Giemsa stain)
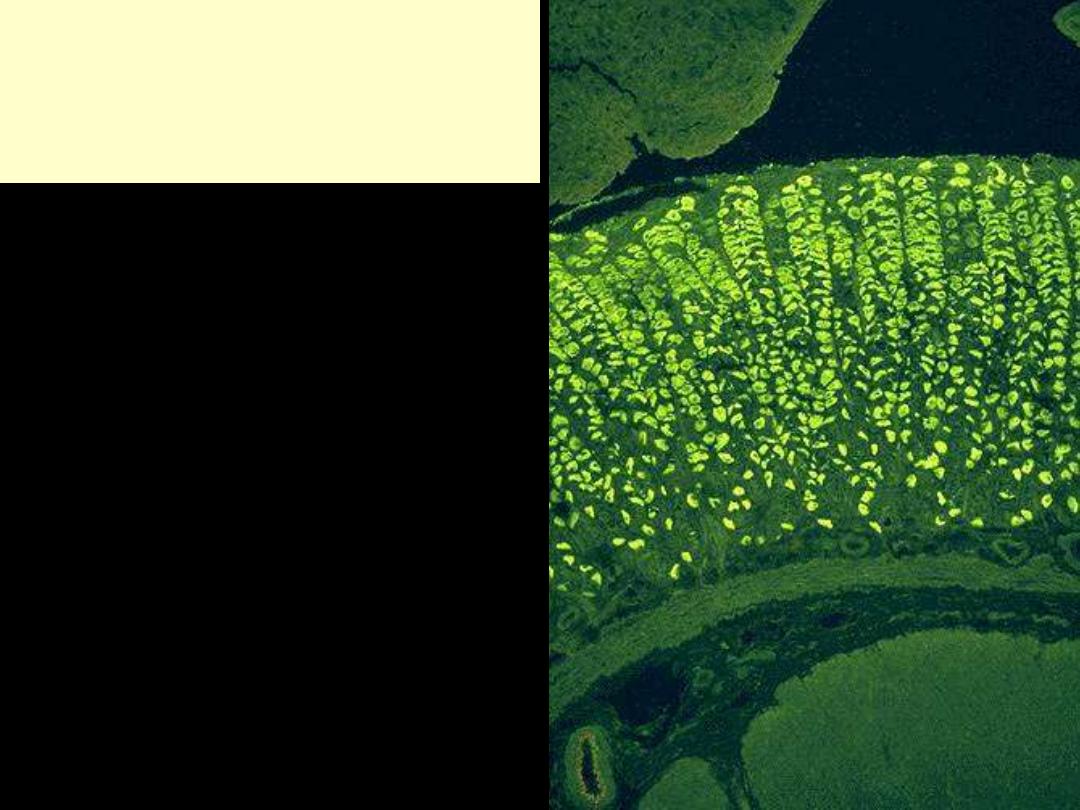
Autoimmune chronic gastritis
Anti-parietal cell antibody
Immunofluorescence technique
Heavy mainly chronic inflammatory cell infiltration of the lamina propria with glandular destruction
(mucosal atrophy)
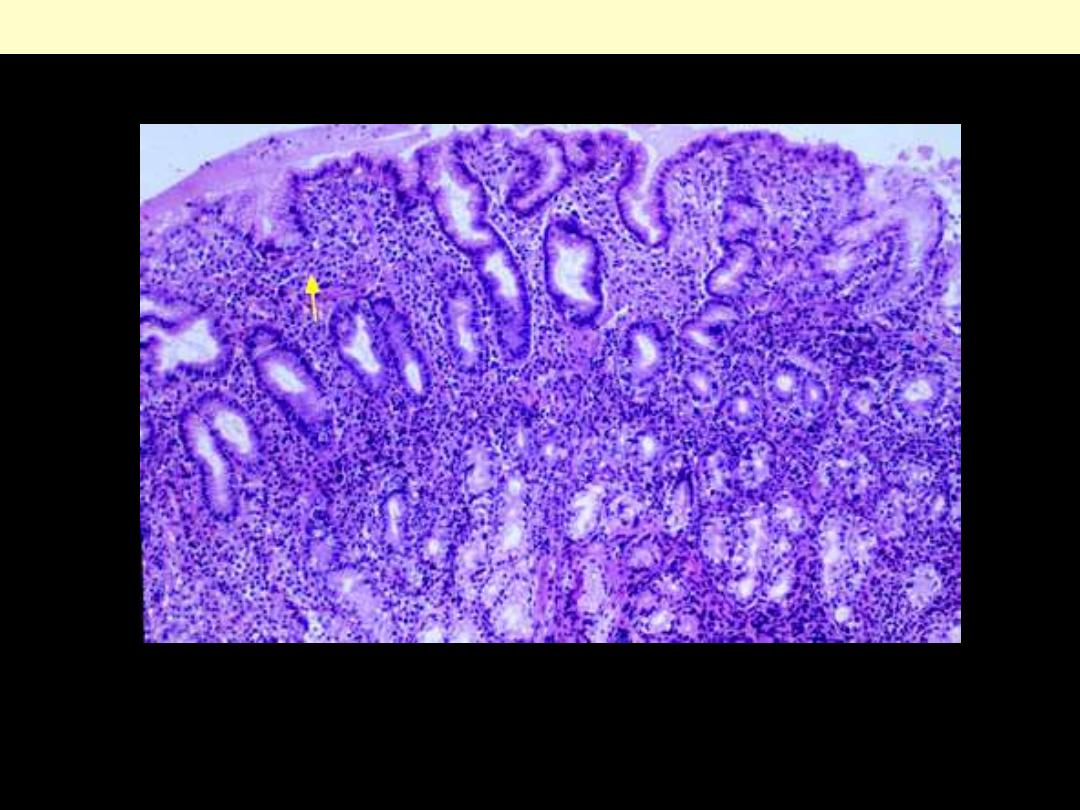
Chronic gastritis
Chronic gastritis
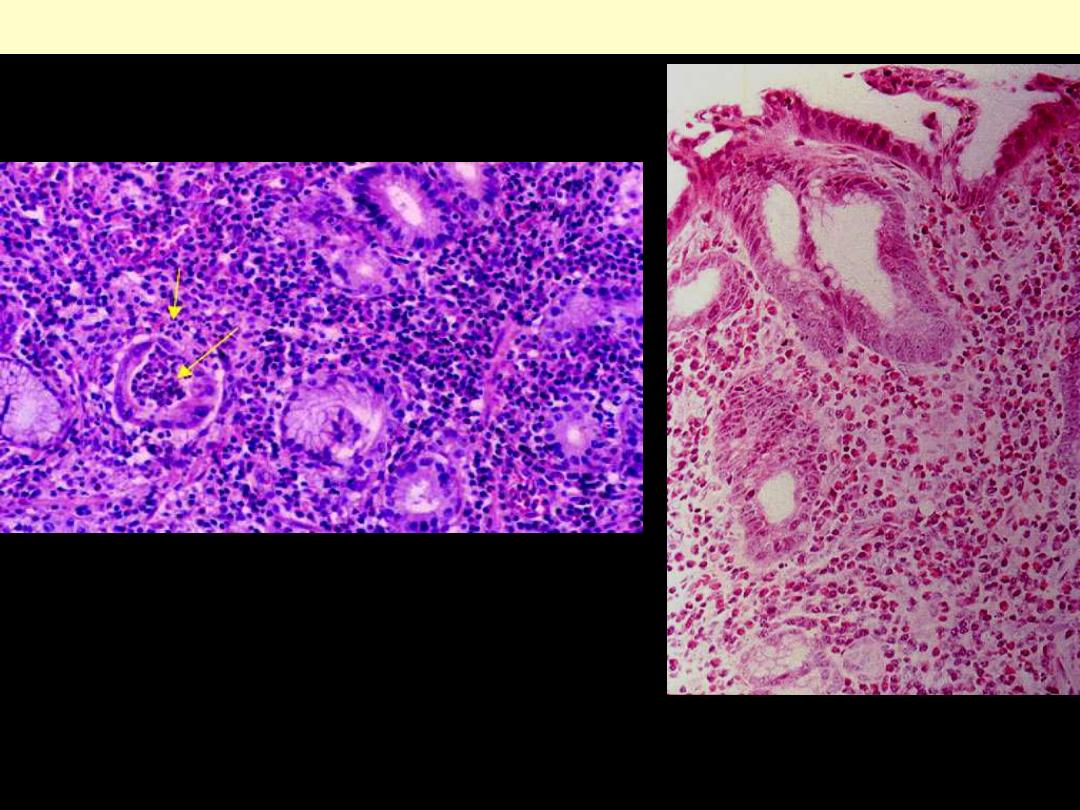
Lt. heavy chronic inflammatory cell infiltration of the lamina propria with acute neutrophilic
component; a collection of neutrophils is present within & outside one of the glands (arrows).
Rt. Heavy infiltration by plasma cells with glandular destruction.

Chronic atrophic gastritis with intestinal metaplasia
The surface & the crypts are lined by columnar epithelium interspersed with goblet cells. Note the
marked mucosal atrophy and the presence of some chronic inflammatory cell infiltration.
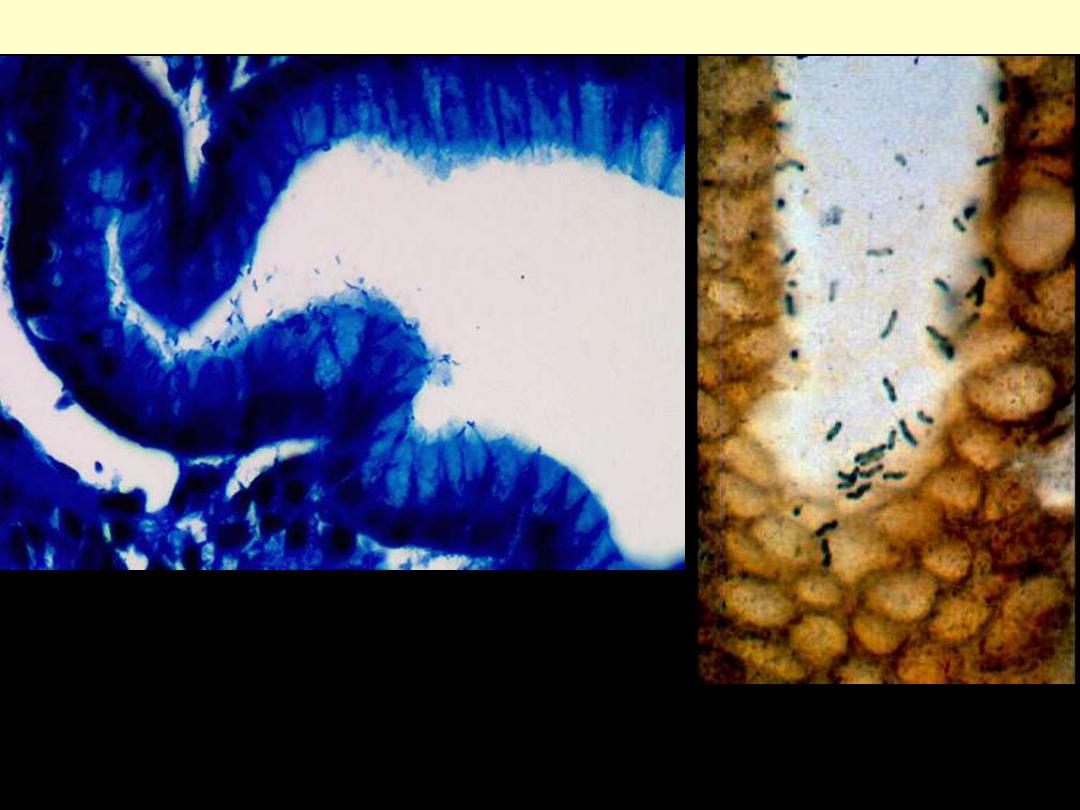
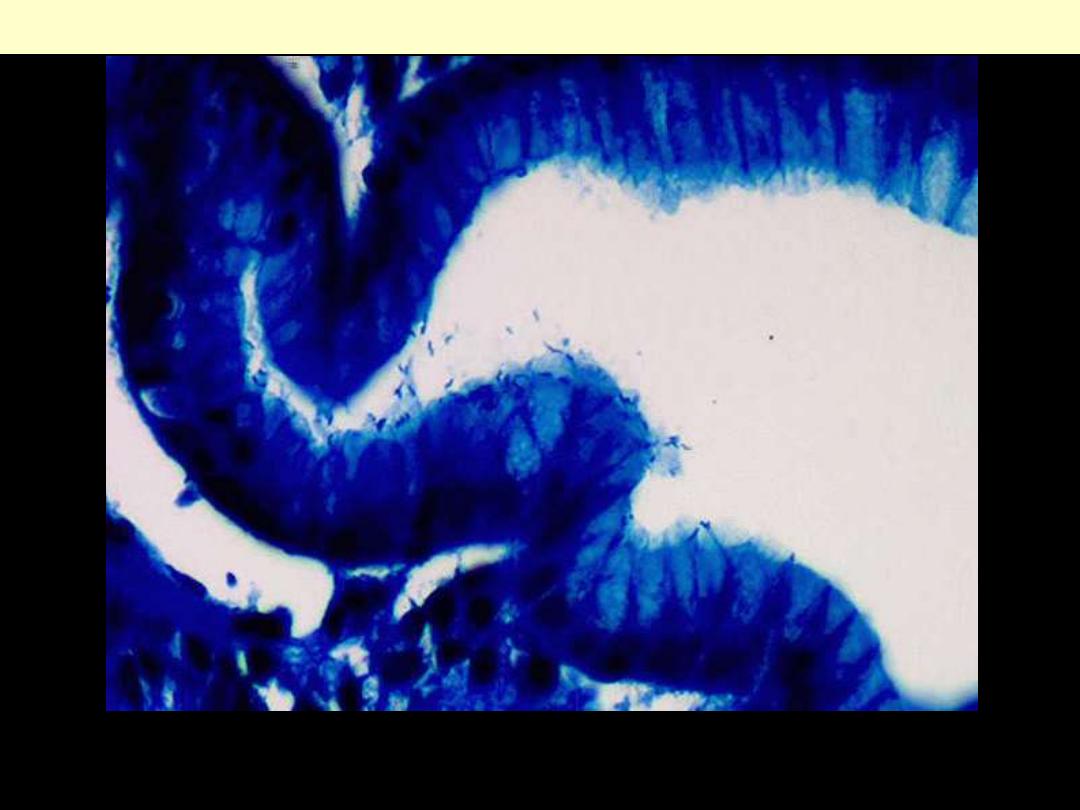
H. pylori gastritis (Giemsa stain Lt. & silver stain Rt.)
These special stains highlight the curvilinear H. pylori. The bacteria are disposed along the surface of
the epithelium within the mucus layer; they are noninvasive.
Peptic ulcer
Well-defined rounded ulcer with undermined edge. There is diffuse hyperemia due to associated
duodenitis.
Chronic peptic ulcer duodenum
Seen above are gastric ulcers of small, & large size on upper endoscopy. All gastric ulcers are biopsied,
since gross inspection alone cannot determine whether a malignancy is present. Smaller, more sharply
demarcated ulcers are more likely to be benign.
Gastric ulcers of various sizes (Endoscopic views)
Chronic peptic ulcer
Sharply delimited chronic peptic ulcer with converging folds of mucosa (due to underlying fibrosis).
This gives a spoke- or star-like appearance.

"Hourglass" stomach
Due to chronic peptic ulceration there is fibrosis and contracture of the stomach leading to an
hourglass shape as well as altered mobility.
Whole mount view of chronic peptic ulcer. The external muscle layer has been totally destroyed. Note
the overhanging mucosa on one edge and the sloping mucosa on the other.
Chronic peptic ulcer stomach
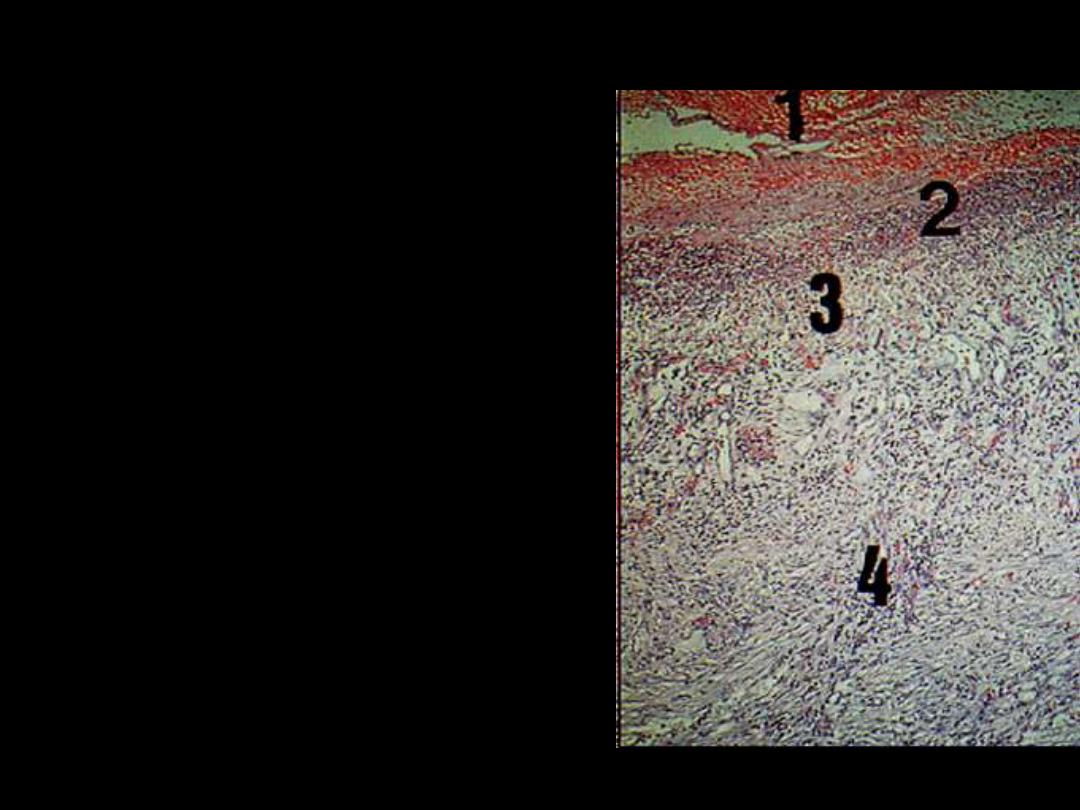
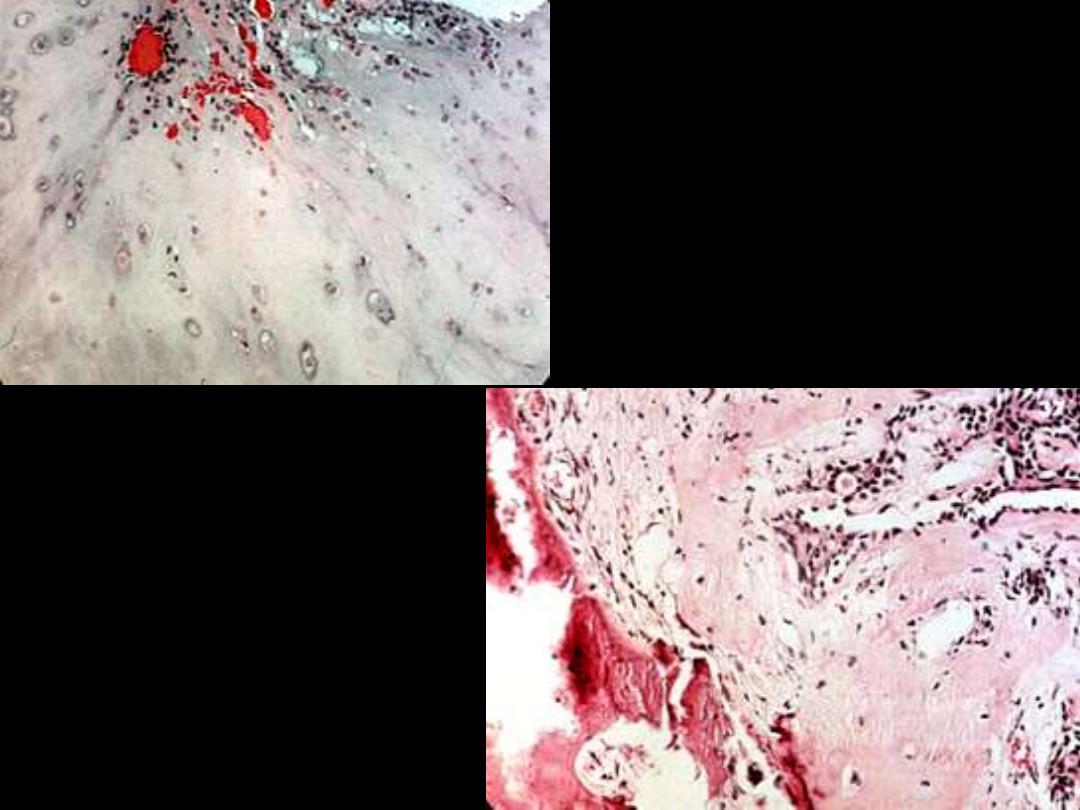
Chronic peptic ulcer shows four layers
1.
The base and walls have a superficial thin layer of
necrotic fibrinoid necrosis.
2.
Beneath this layer is a zone of predominantly
neutrophilic inflammatory infiltrate.
3.
Deeper still, there is granulation tissue infiltrated
with inflammatory cells. This rests on
4.
Fibrous or collagenous scar.
There are multiple, small (less than 1 cm)
and circular defects. The ulcer base is
frequently stained a dark brown by the acid
digestion of blood. The related mucosal
folds (rugae) are normal (cf. chronic peptic
ulcer, which show convergence on the ulcer)
Acute gastric ulcers
Tumors
Gross appearance of gastric polyps of hyperplastic
type. Many of the lesions show central
umbilication.
Low-power microscopic view of gastric polyps
of hyperplastic type. The cystic dilatation of the
glands is more evident on the left side.
Hyperplastic polyp stomach
Hyperplastic polyp
Polyps are due to proliferation of foveolar cells.
The adenoma is composed of dysplastic epithelial cells with a high risk for progression into malignancy.
Gastric adenomatous polyp (adenoma)
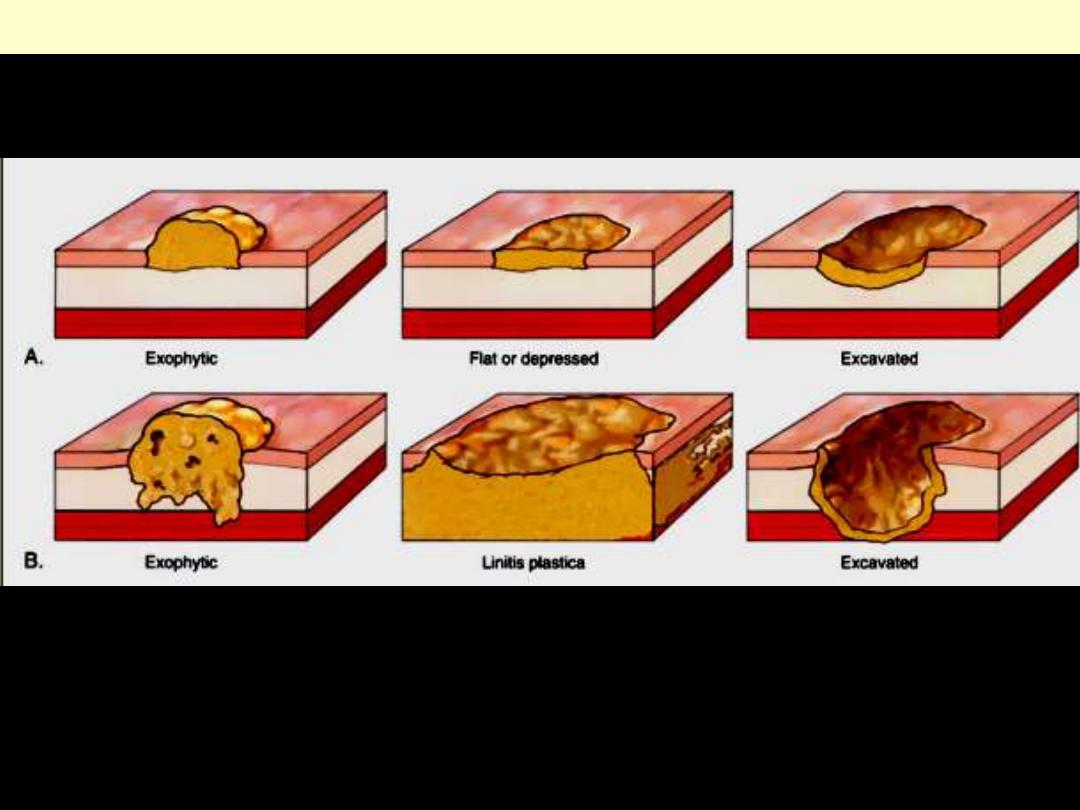
Diagram of growth patterns and spread of gastric carcinoma
In early gastric carcinoma (A), the tumor is confined to the mucosa and submucosa and may exhibit an
exophytic, flat or depressed, or excavated conformation.
Advanced gastric carcinoma (B) extends into the muscularis propria and beyond. Linitis plastica is an
extreme form of flat or depressed advanced gastric carcinoma.
Early
Advanced

d
Polypoid (Fungating, exophytic) adenocarcinoma of the stomach

Adenocarcinoma-ulcerative (excavating)
Ulcerative carcinoma may closely mimic chronic peptic ulcers. However, in advanced cases, there are
heaped-up, beaded margins and necrotic bases. The neoplastic tissue extends into the surrounding
mucosa and wall; this leads to flattening of the mucosa surrounding the ulcer.
The wall of the stomach is thickened and rubbery hard due to an extensive infiltration with diffuse type
carcinoma: signet ring cells.
Linitis plastic/diffuse type carcinoma
Adenocarcinoma-intestinal type
Diffuse-type carcinoma showing signet ring cells
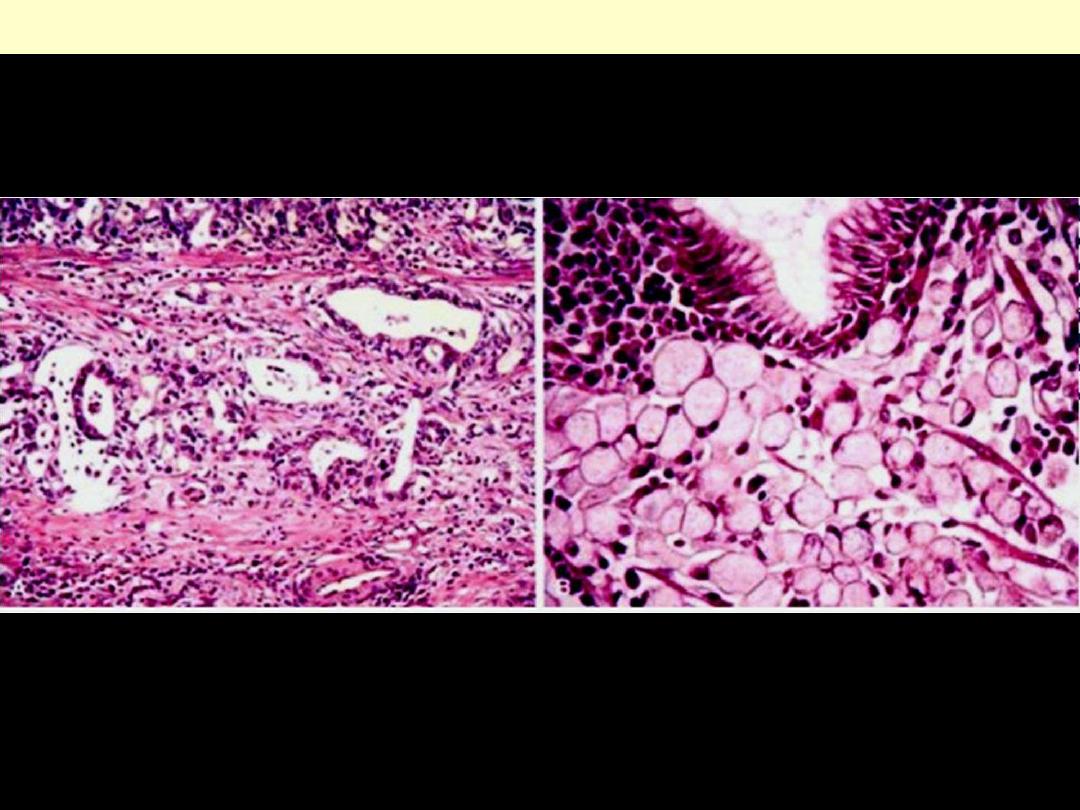
Gastric carcinoma intestinal Vs diffuse
Gastric carcinoma. A, Intestinal type demonstrating gland formation by malignant cells, which are
invading the muscular wall of the stomach. B, Diffuse type demonstrating signet-ring carcinoma cells.
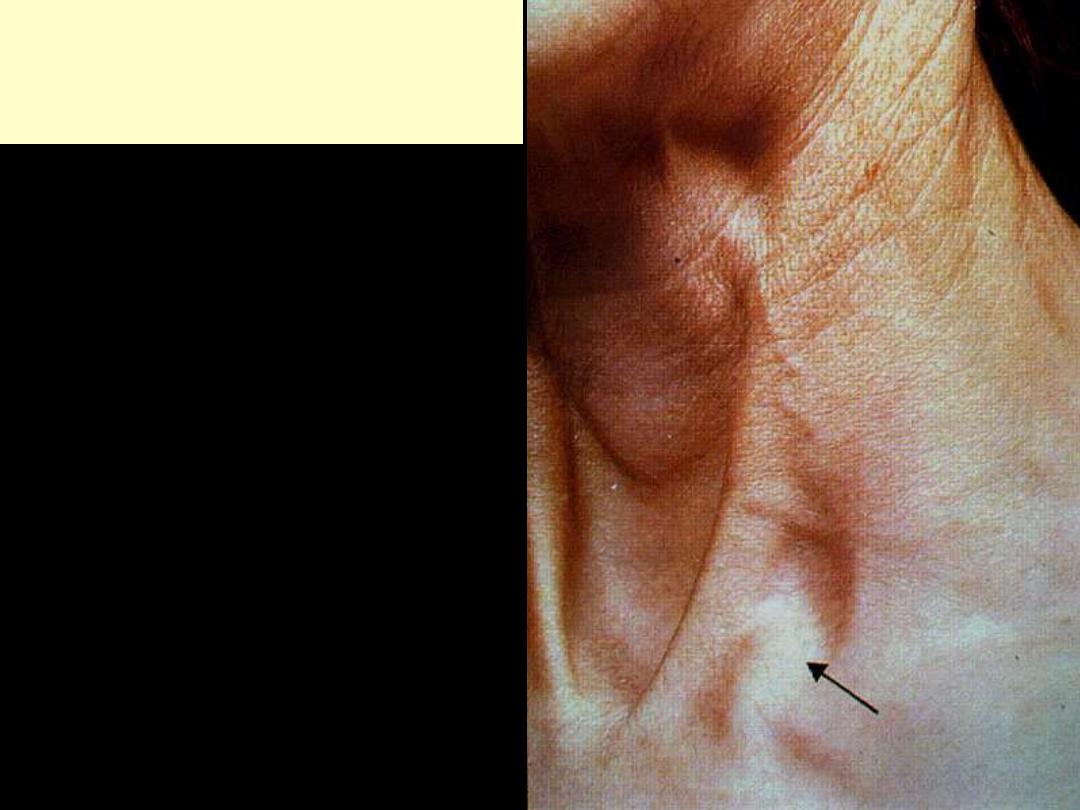
Virchows Node
Metastases from gastric carcinoma can
spread to the left supraclavicular area.
Scattered duct structures were seen in the
dermis.
Sister Mary Joseph nodule
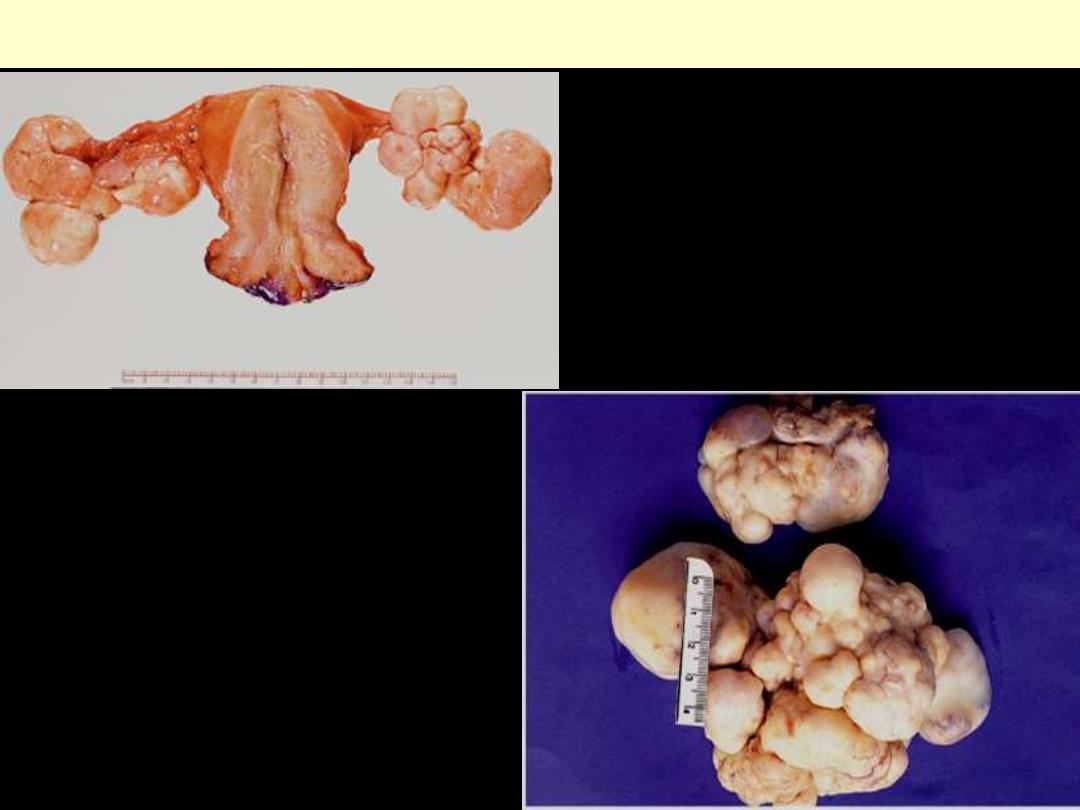
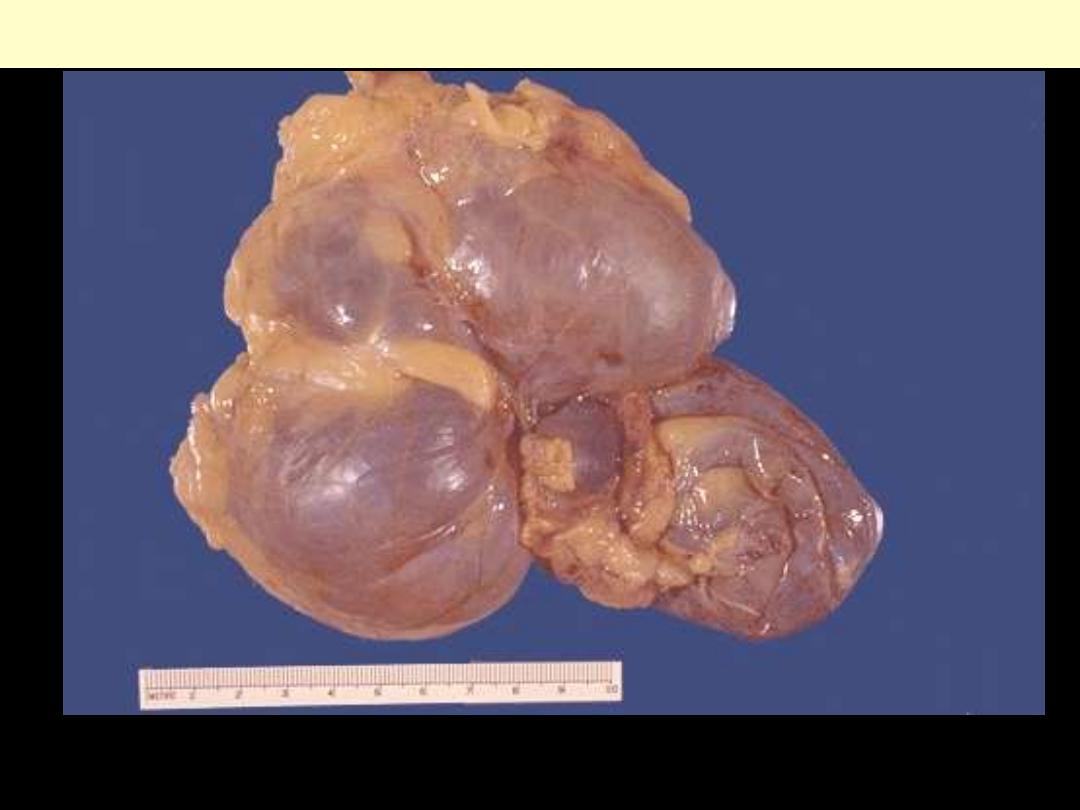
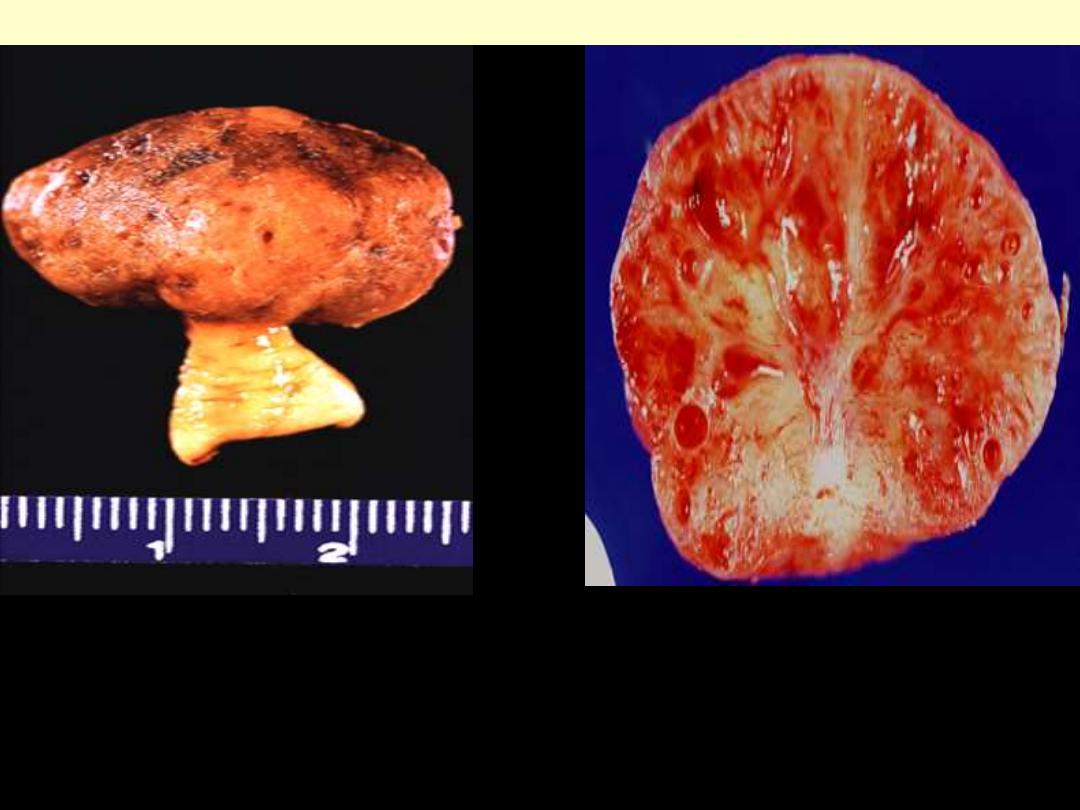
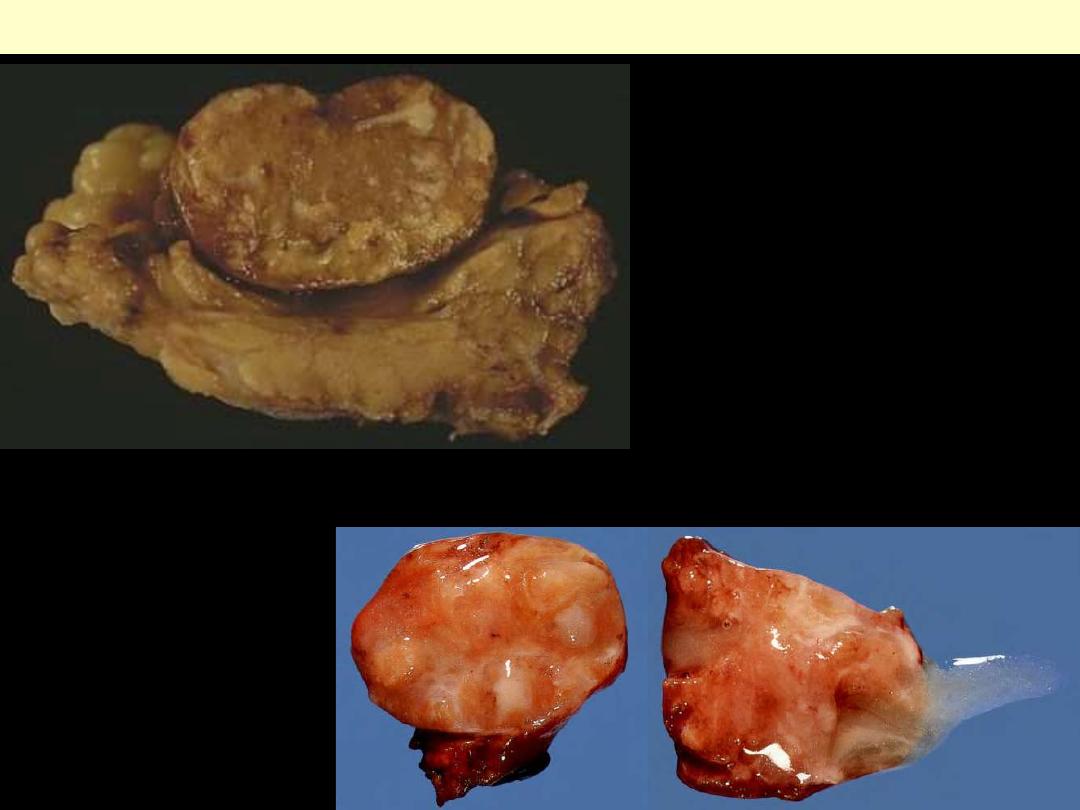
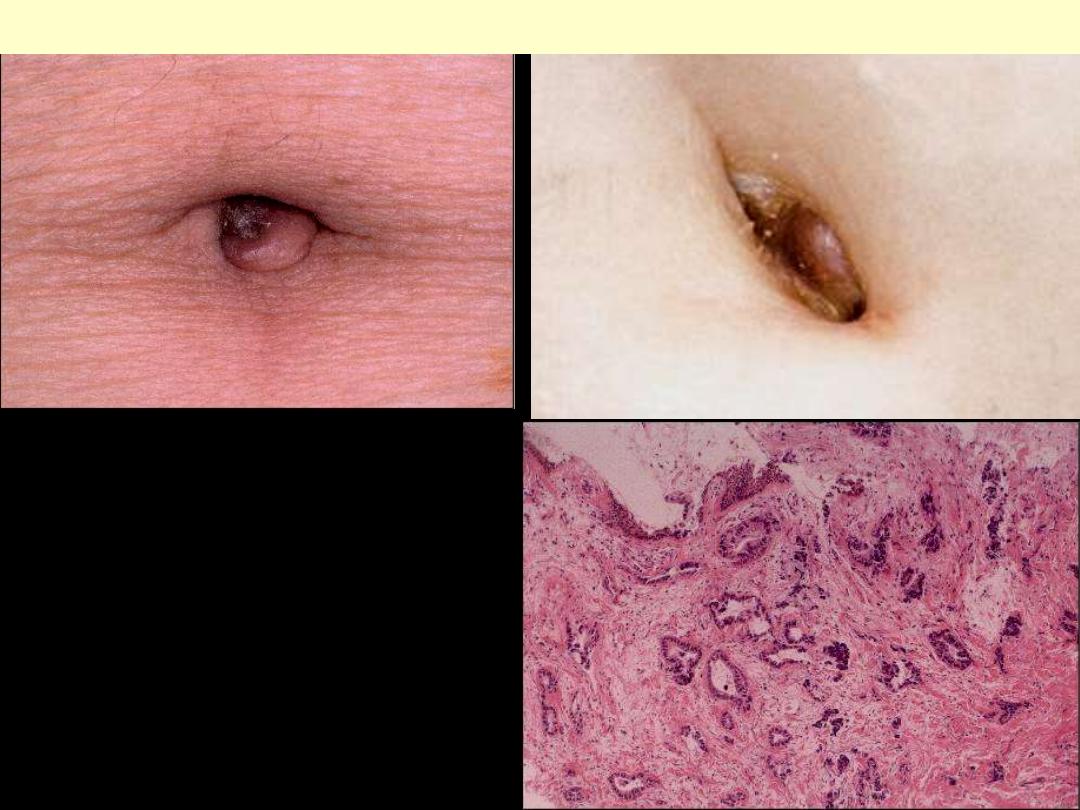
Typical gross appearance of
Krukenberg tumors of ovary. The
involvement is bilateral and the
tumors are characterized by a
multinodular outer appearance.
Krukenberg tumors ovary
The multinodular quality of the ovarian
metastasis is typical of Krukenberg tumor.
A case of metastatic lobular ca breast
