Gall bladder
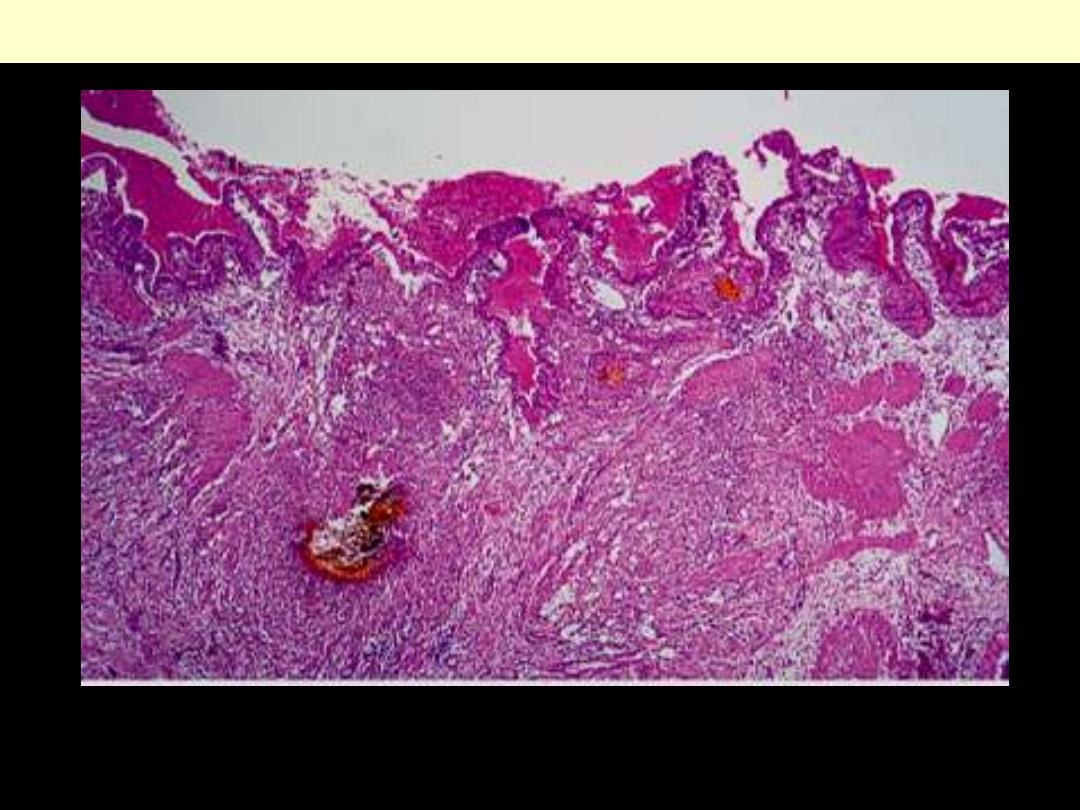
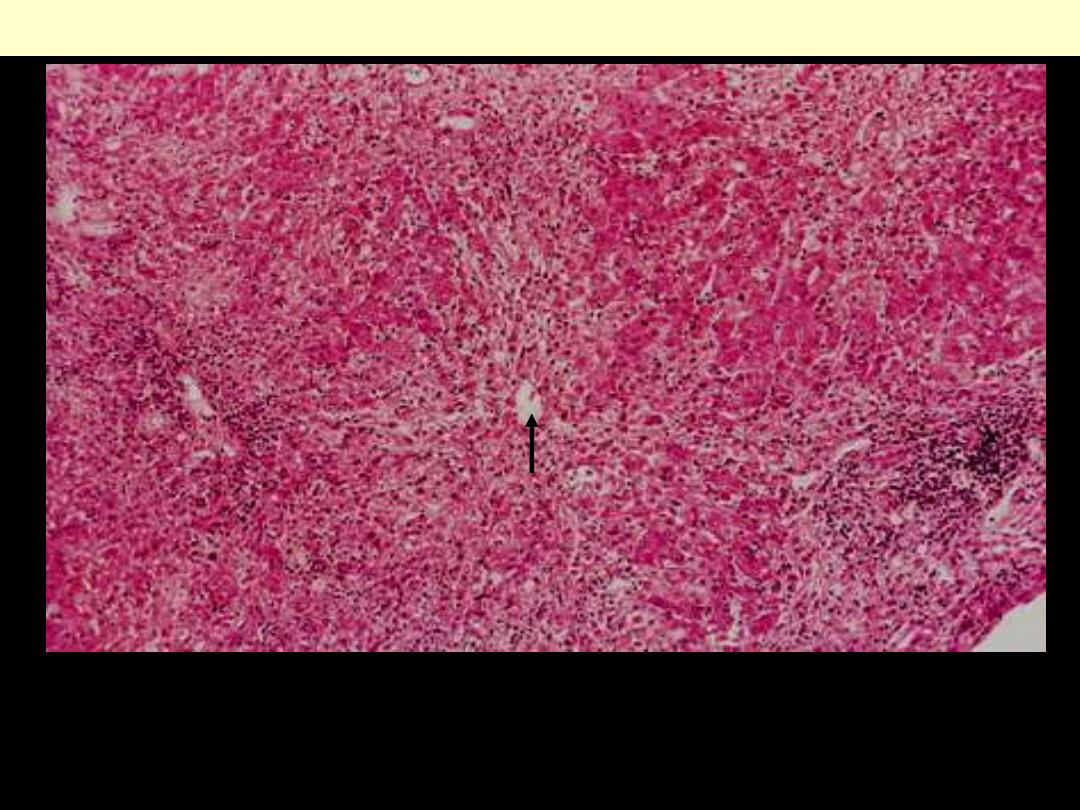
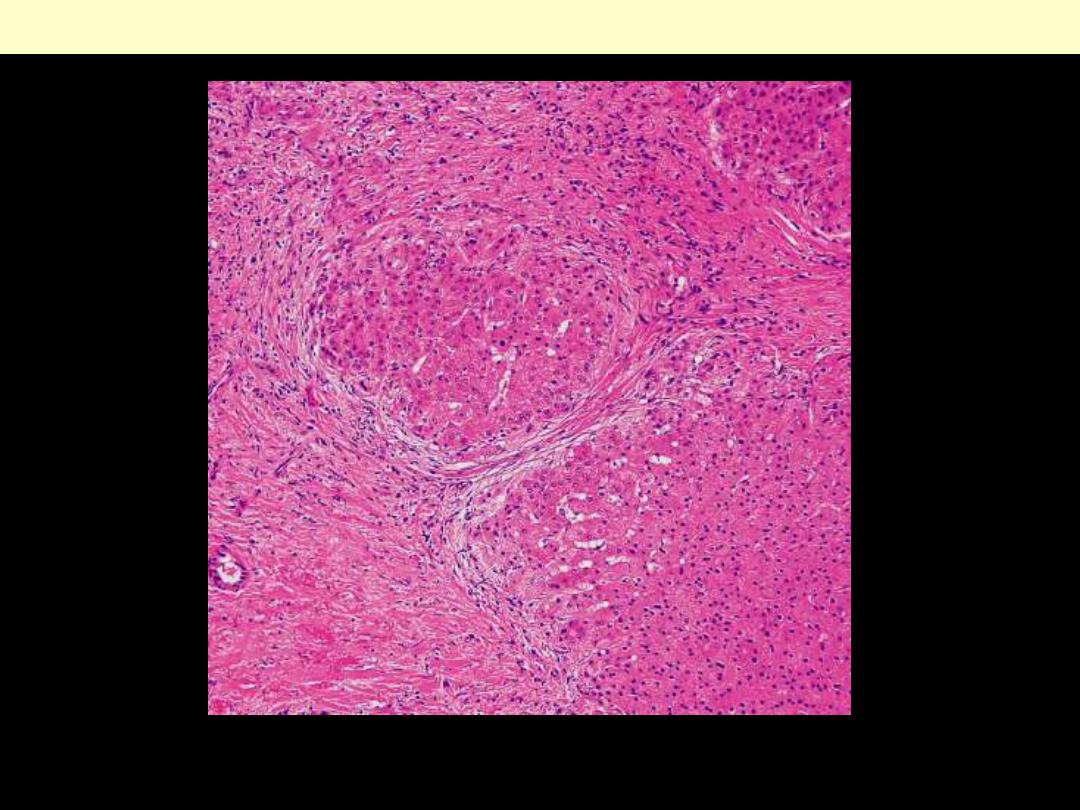
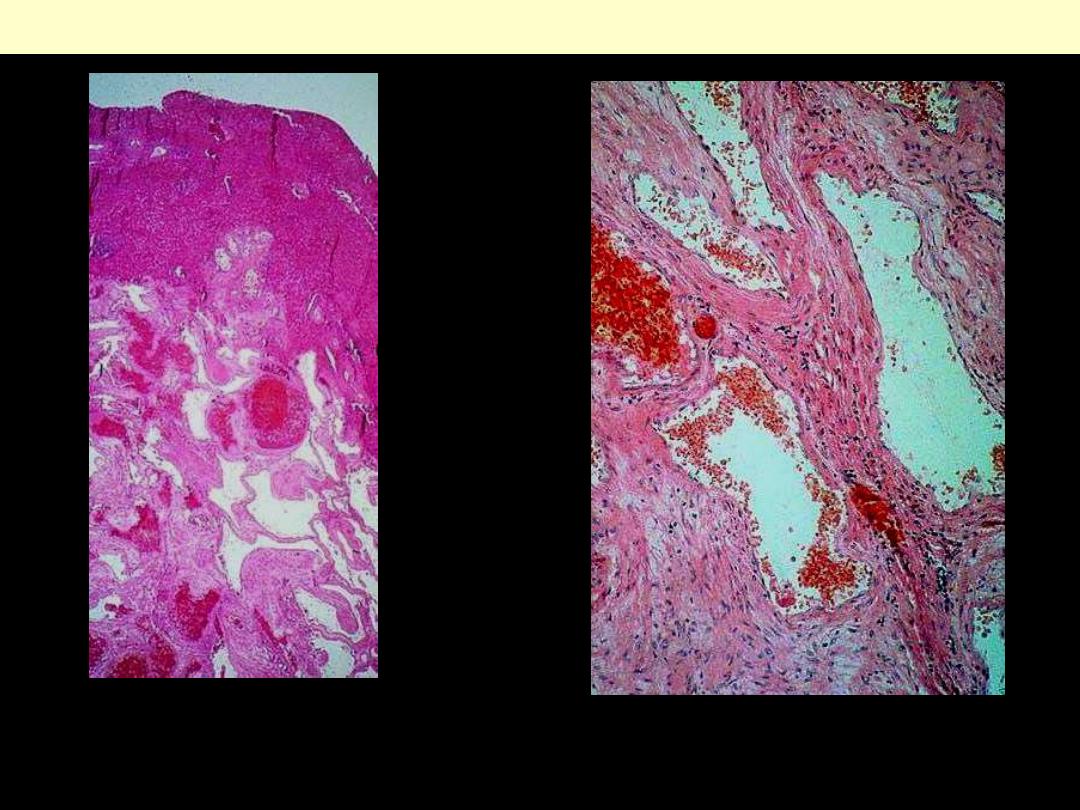
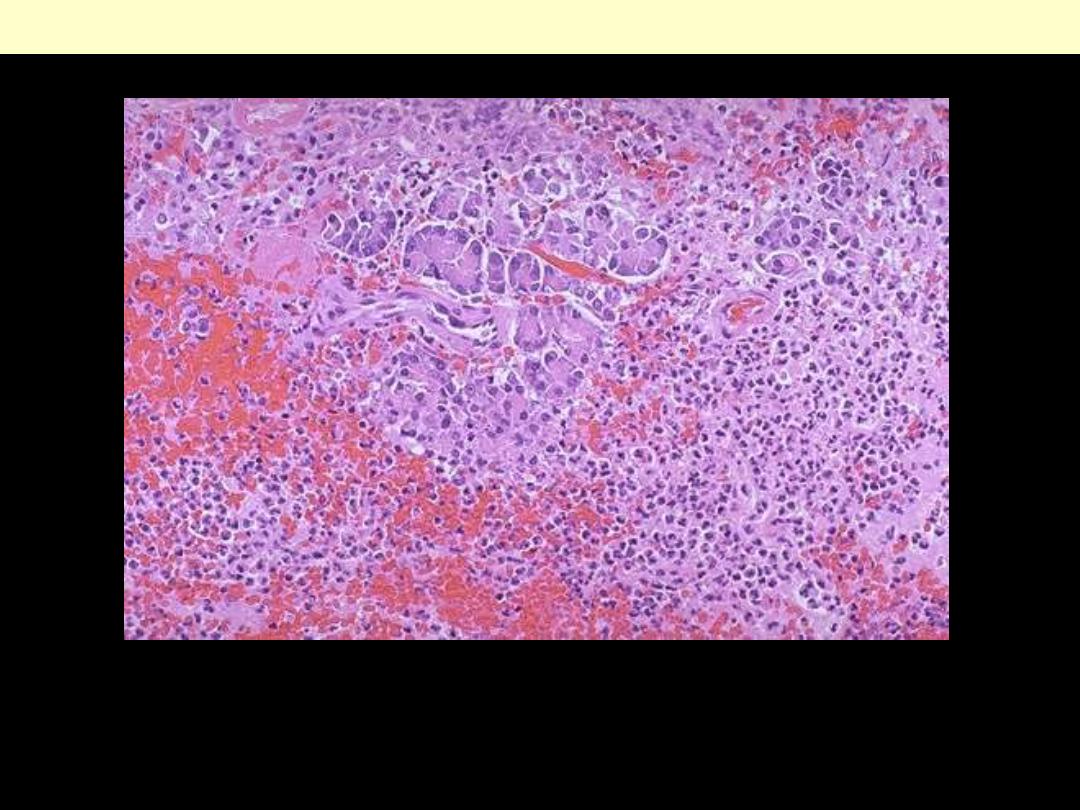
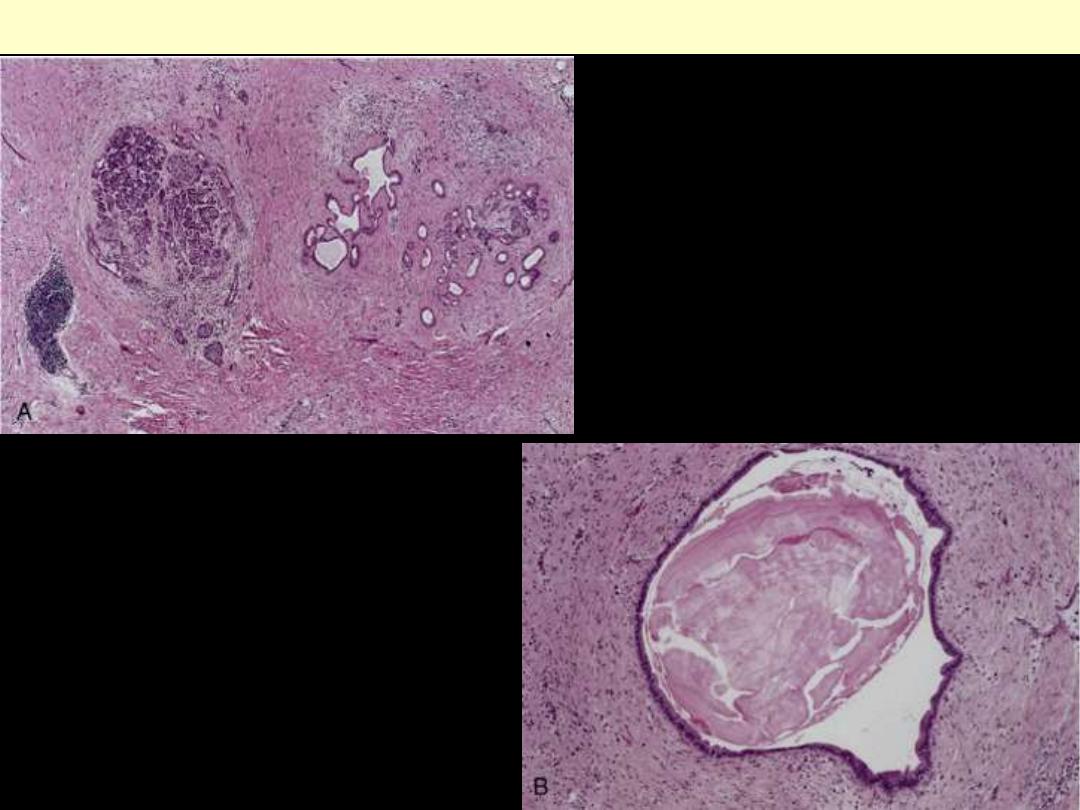
Primary sclerosing cholangitis
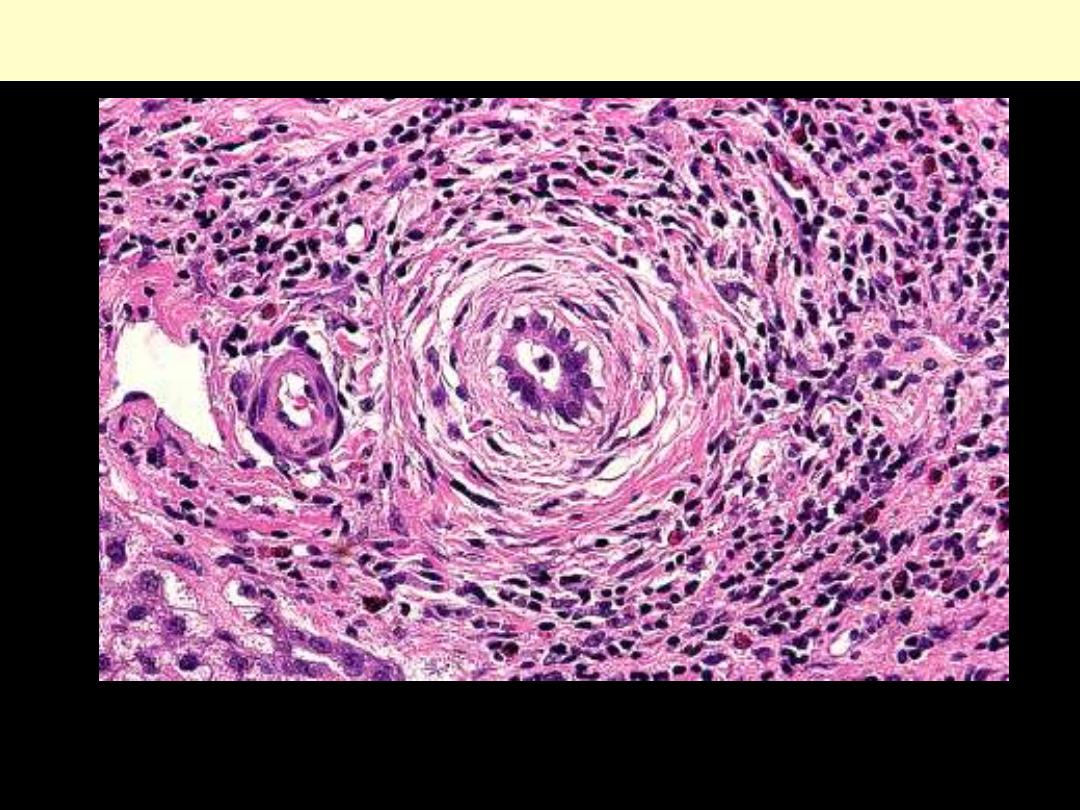
Primary sclerosing cholangitis
Primary sclerosing cholangitis. Detail of portal tract with moderately dense inflammatory infiltrate
(mainly lymphocytes, some eosinophils) and concentric, lamellated, periductal fibrosis ("onion skin"
fibrosis) around the interlobular bile duct (center). (H&E)
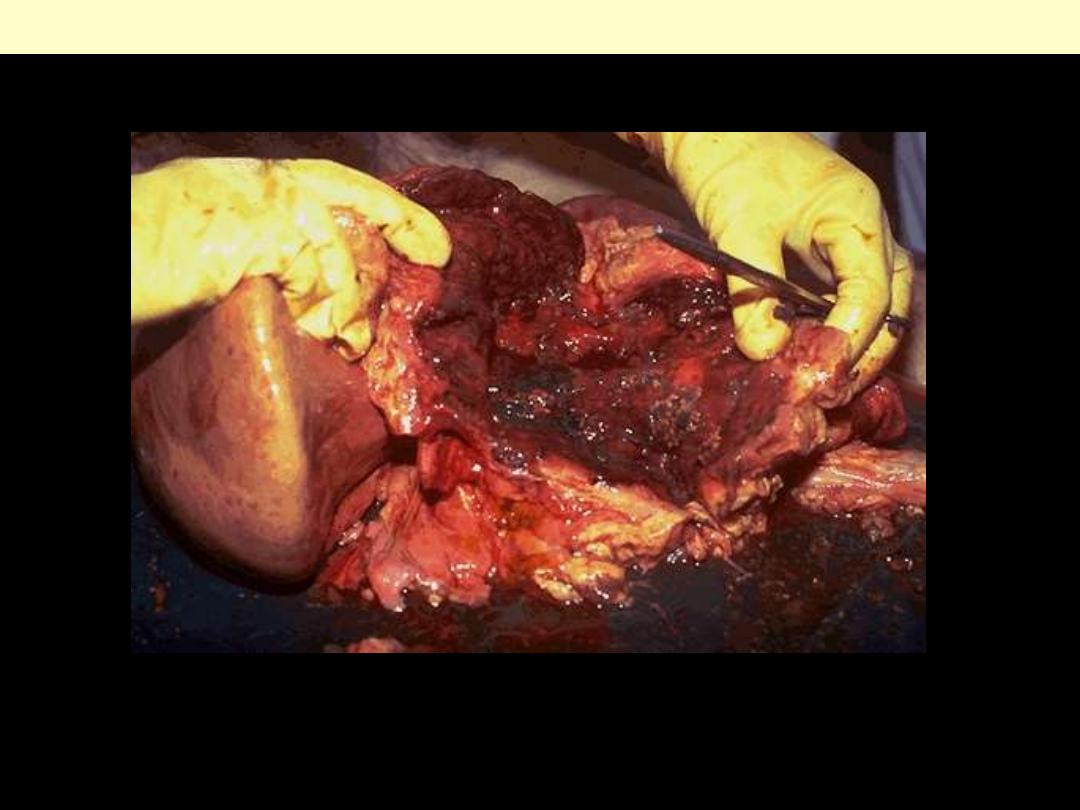
Stones + inflammation
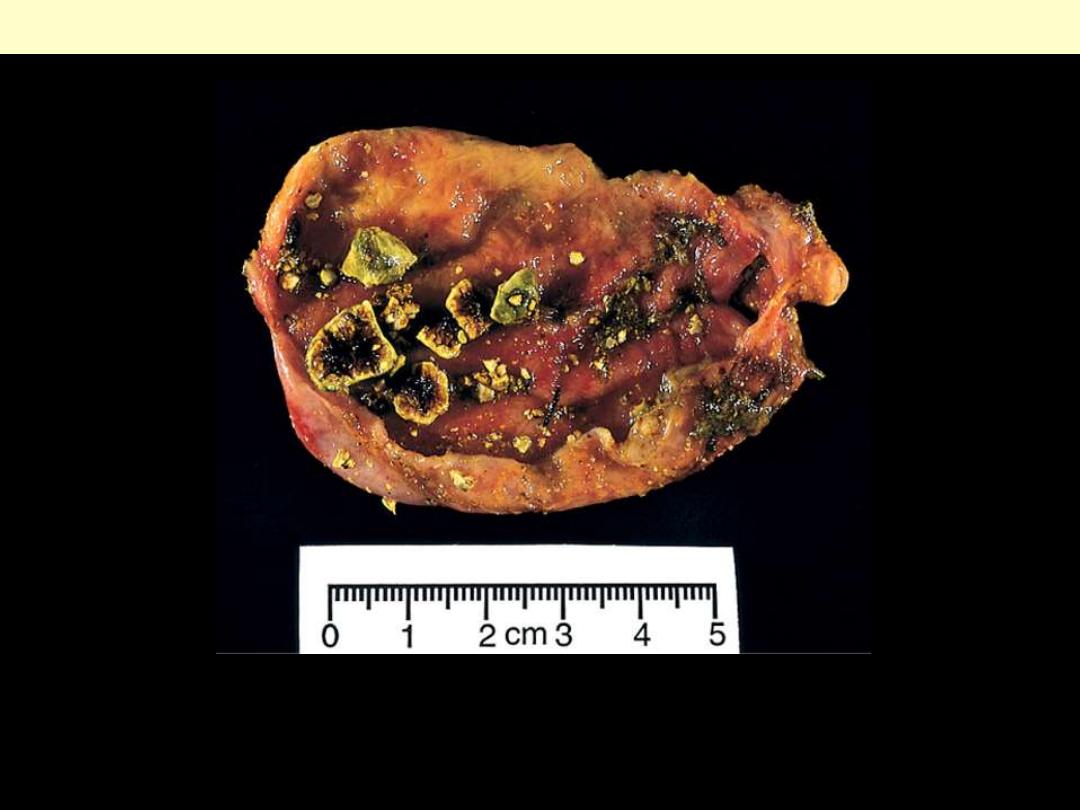
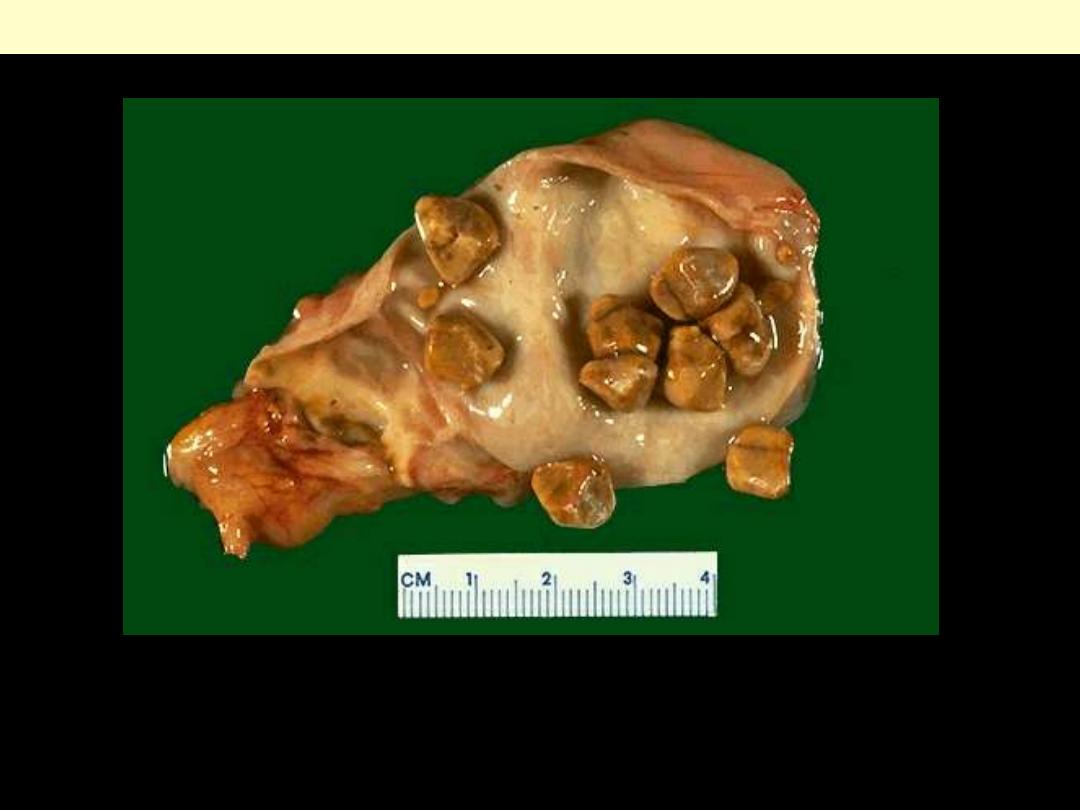
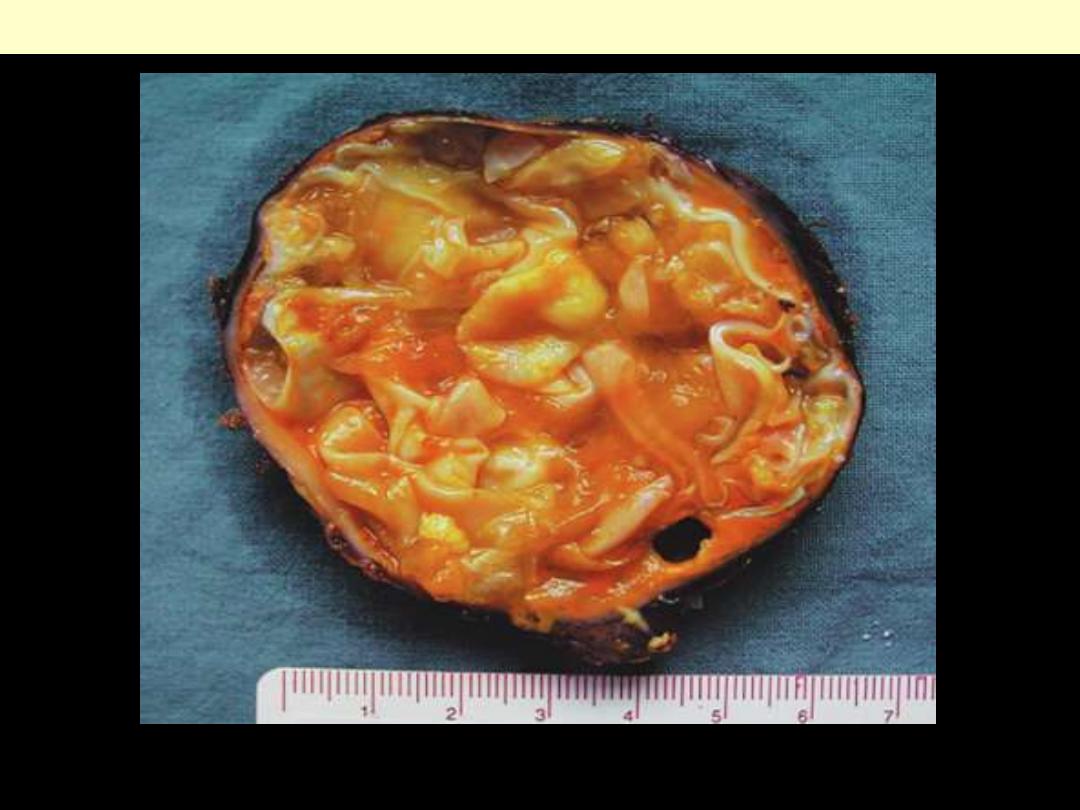
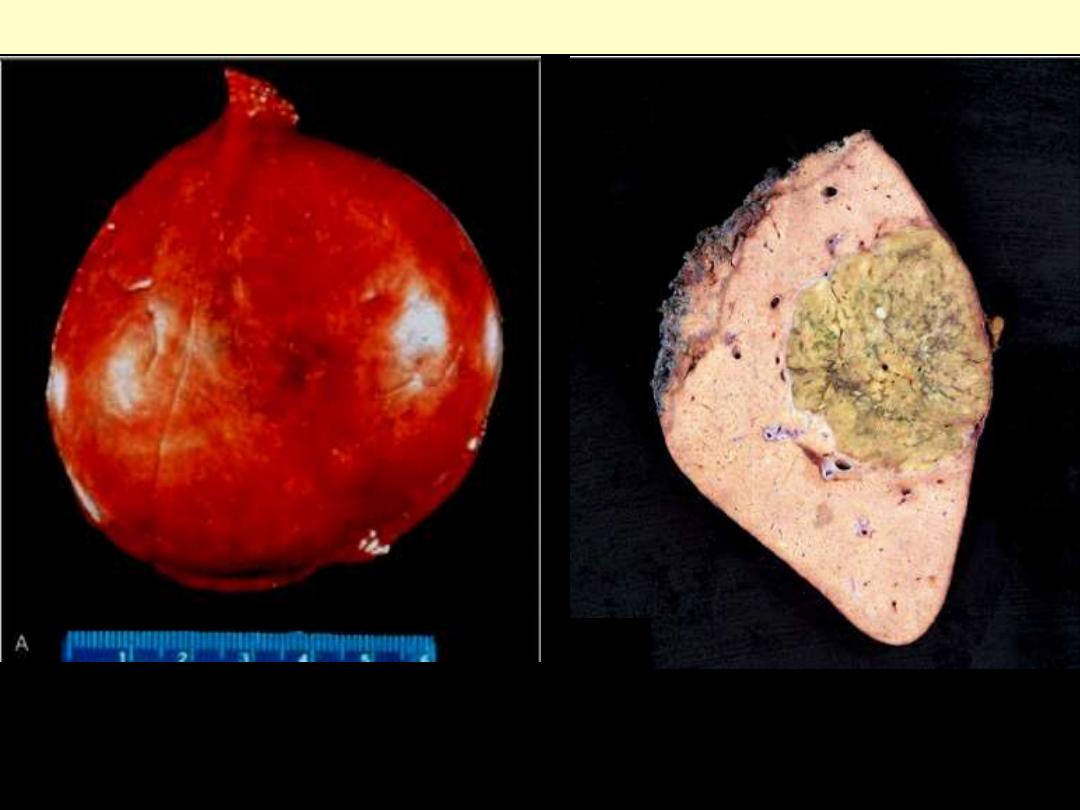
Cholesterol gallstones
Mechanical manipulation during laparoscopic cholecystectomy has caused fragmentation of several
yellow cholesterol gallstones, the interiors are black because of entrapped bile pigments. Note the
faceted outlines. The gallbladder mucosa is reddened and irregular as a result of coexistent acute and
chronic cholecystitis.
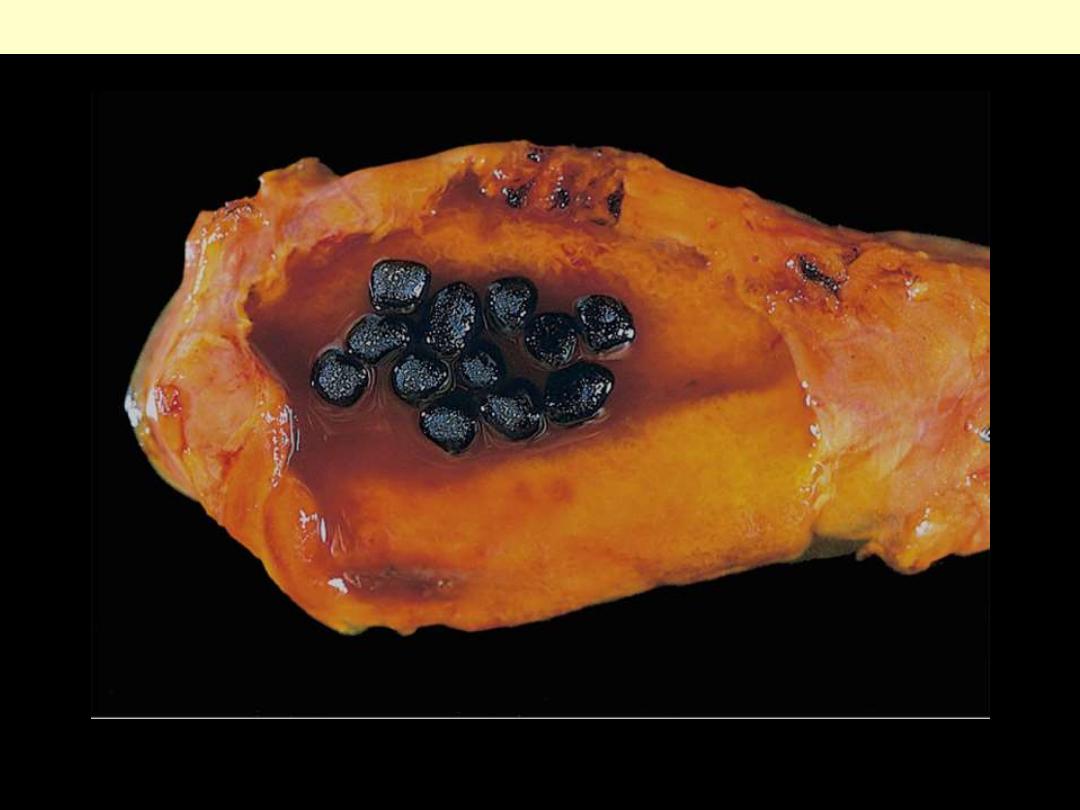
Pigmented gallstones
Several faceted black gallstones are present in the gallbladder from a person with a mechanical mitral
valve prosthesis, leading to chronic intravascular hemolysis.
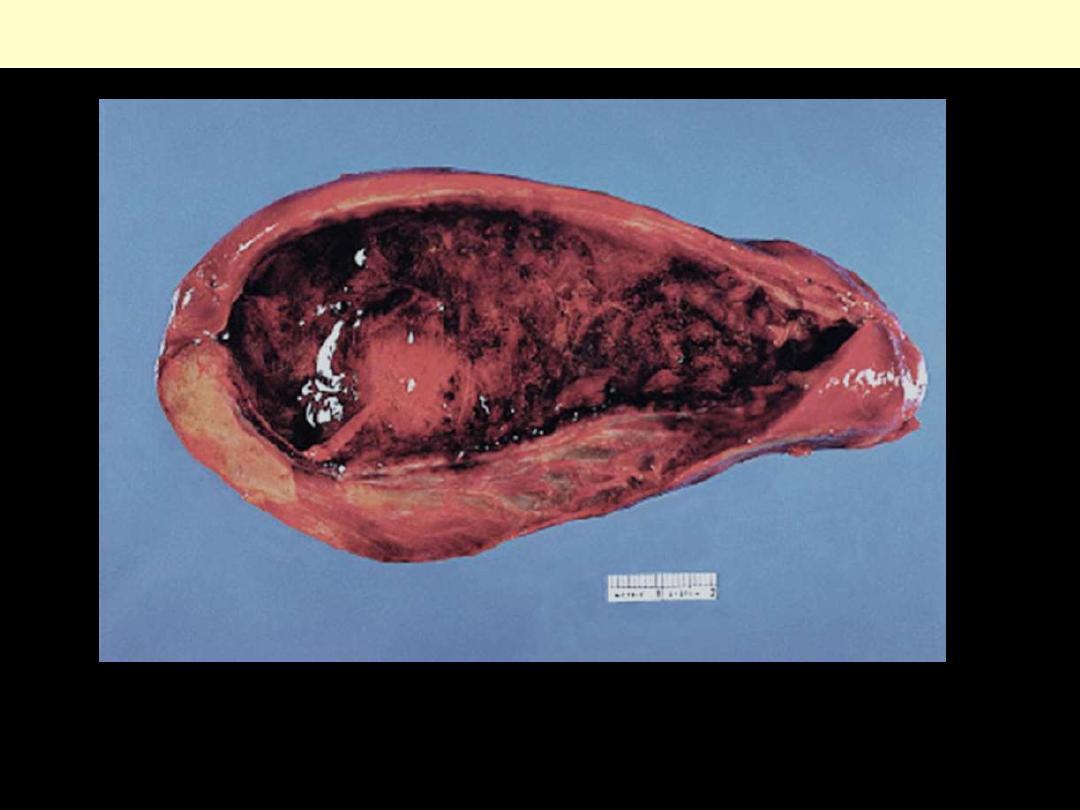
Acute cholecystitis
The mucosa has a characteristic "angry red" color. Note the marked edema of the wall and the serosal
hyperemia. (normally the wall is paper-thin
Acute cholecystitis showing extensive ulceration, hemorrhage, and edema & inflammation
Acute cholecystitis
There is thickening of the wall. The gallbladder is of normal size but it may be contracted, or enlarged.
The mere presence of stones within the gallbladder, even in the absence of inflammation, is often taken
as sufficient justification for the diagnosis.
Chronic cholecystitis with cholelithiasis
Tumors
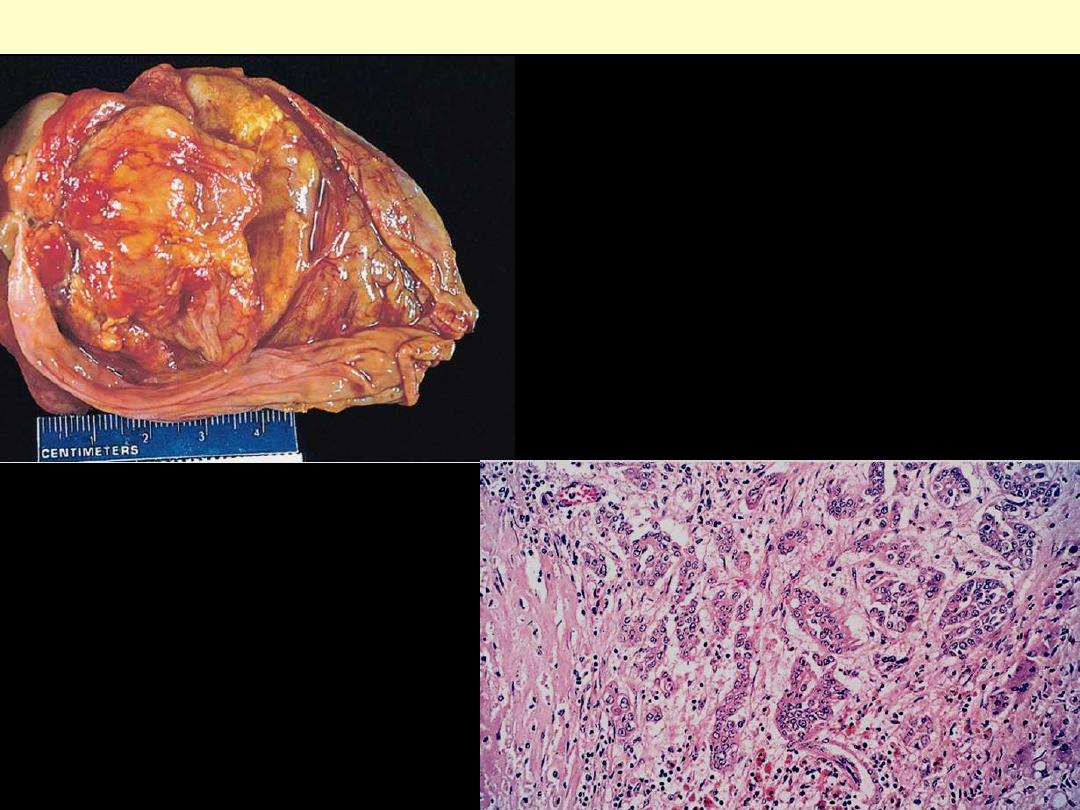
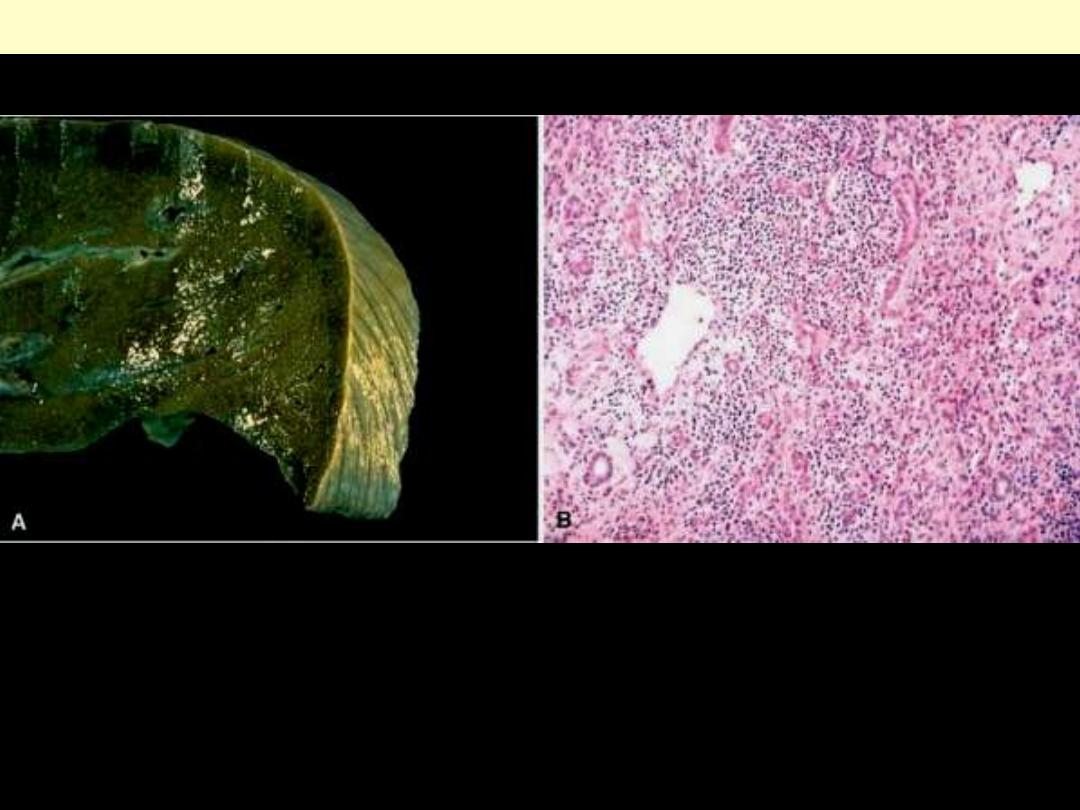
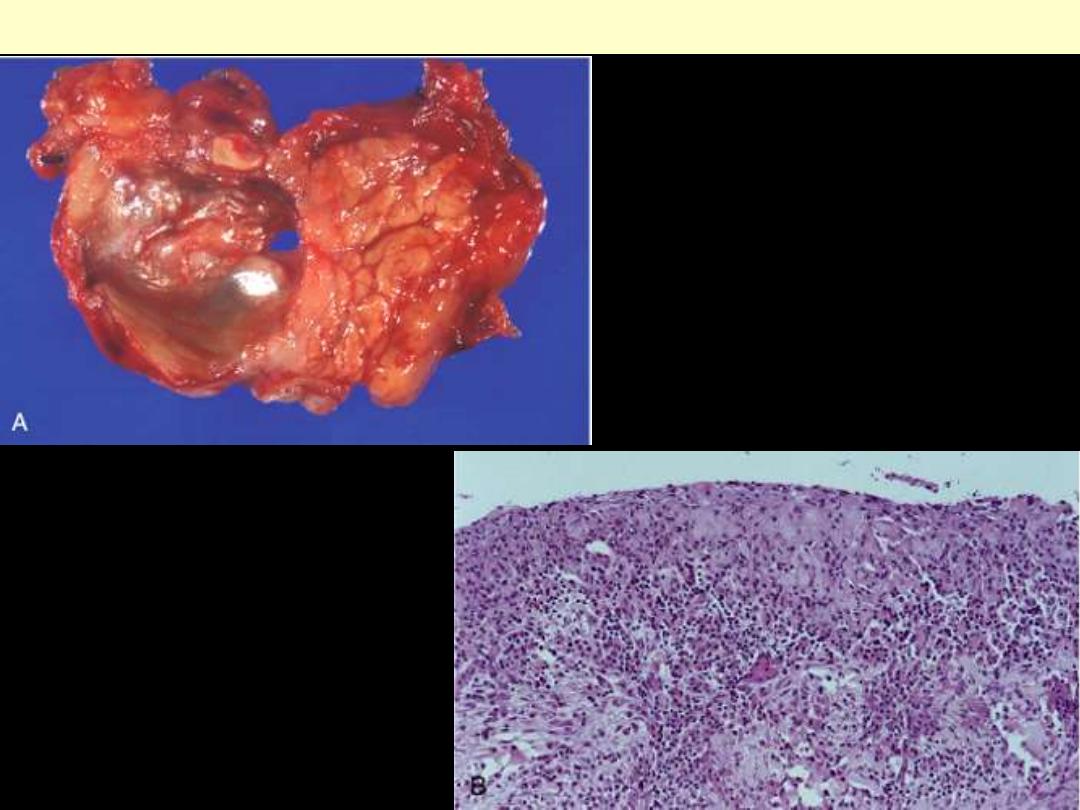
Adenocarcinoma of the gallbladder
A.
The opened gallbladder contains a large,
exophytic tumor that virtually fills the lumen.
B.
Malignant glandular structures are present
within the gallbladder wall, which is fibrotic.
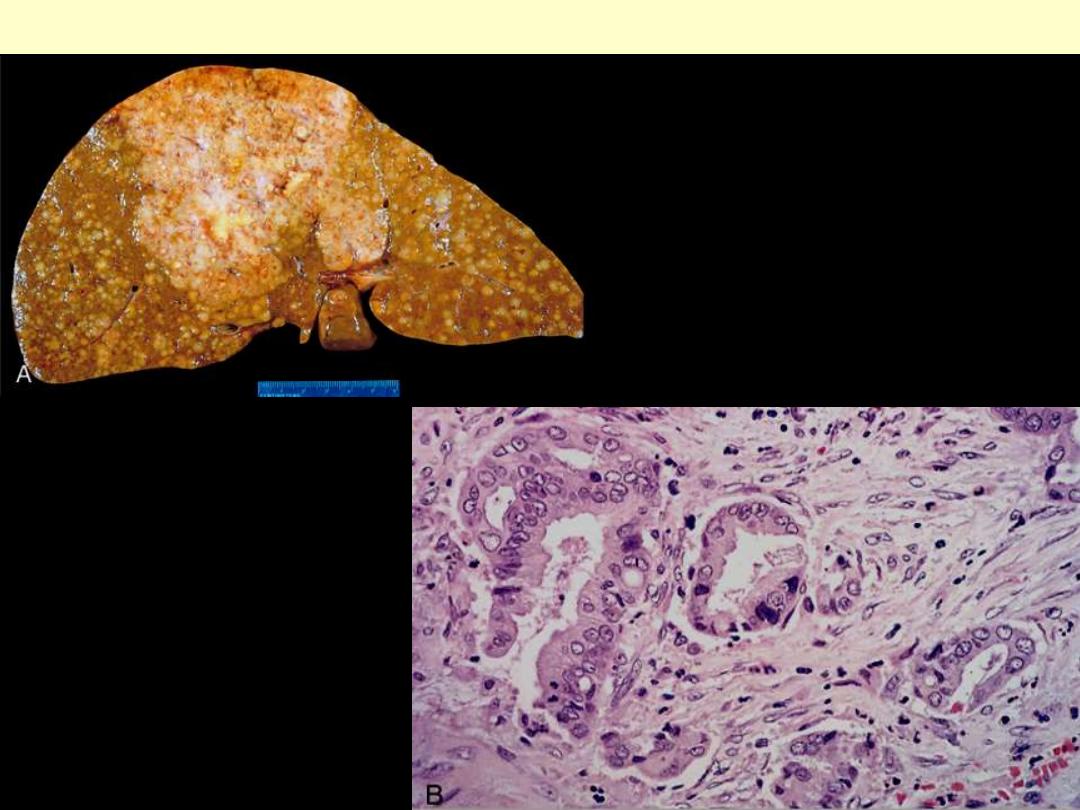
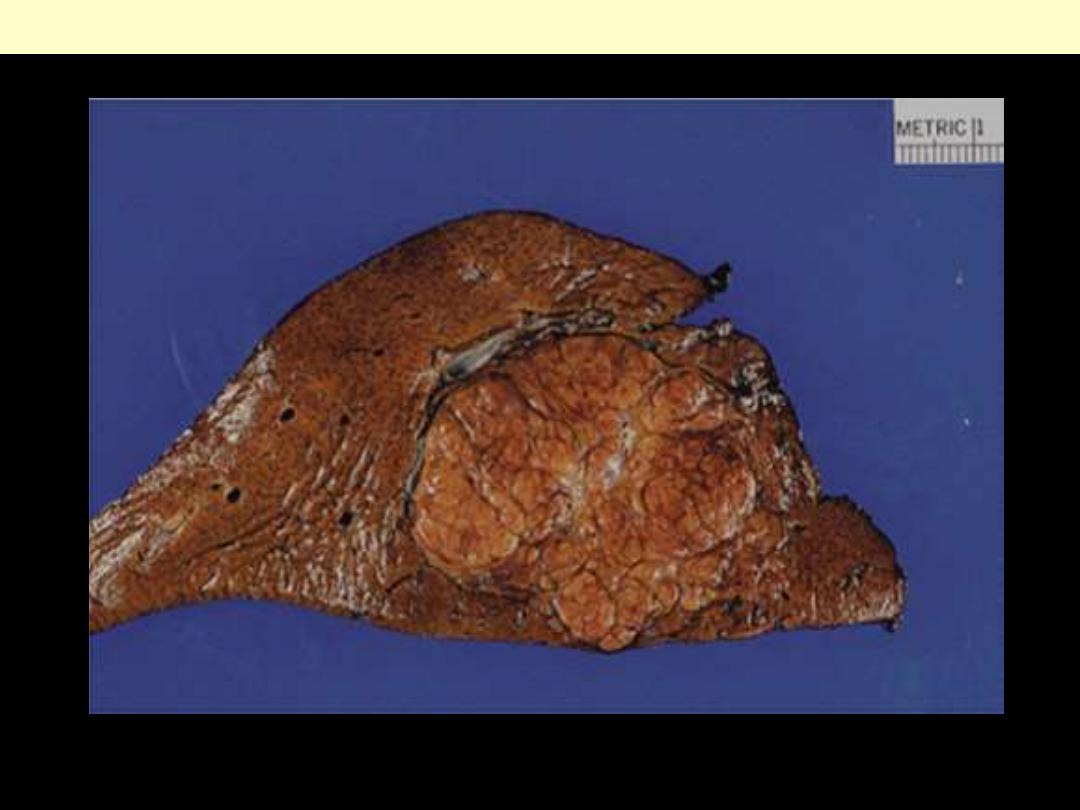
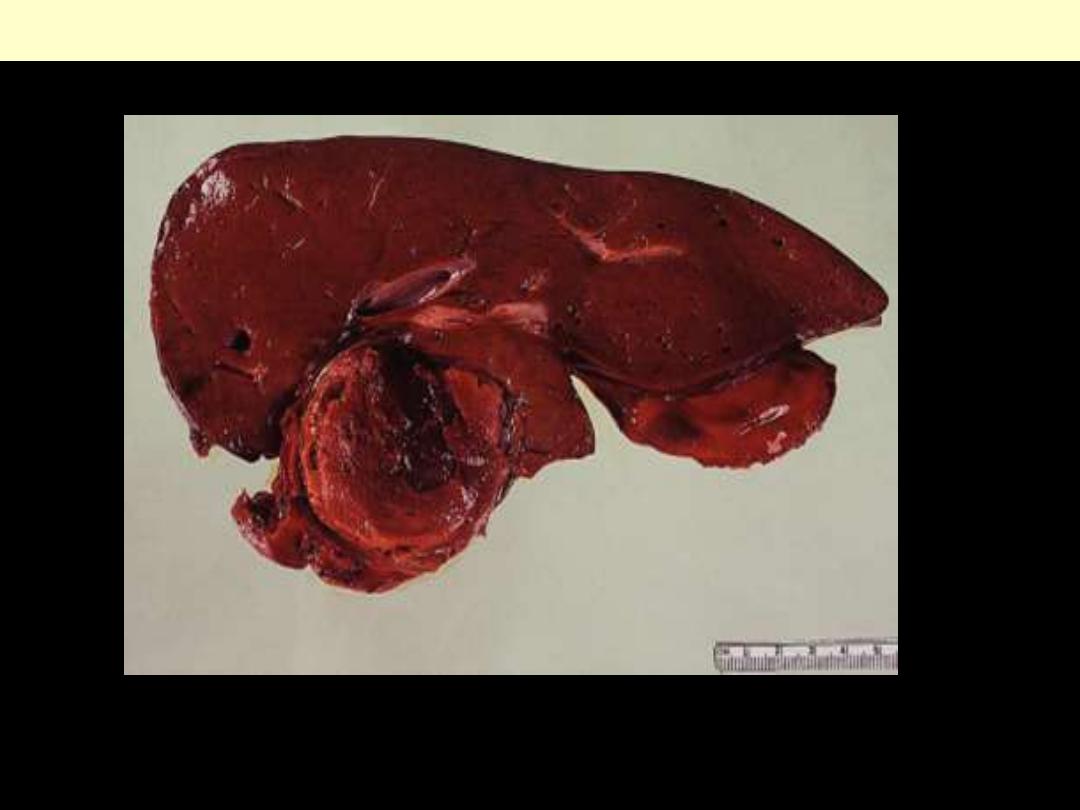
Cholangiocarcinoma
A, Massive neoplasm in the right lobe and
multiple metastases throughout the liver. B,
Tumor cells forming glandular structures
surrounded by dense sclerotic stroma.
Liver
Abscess
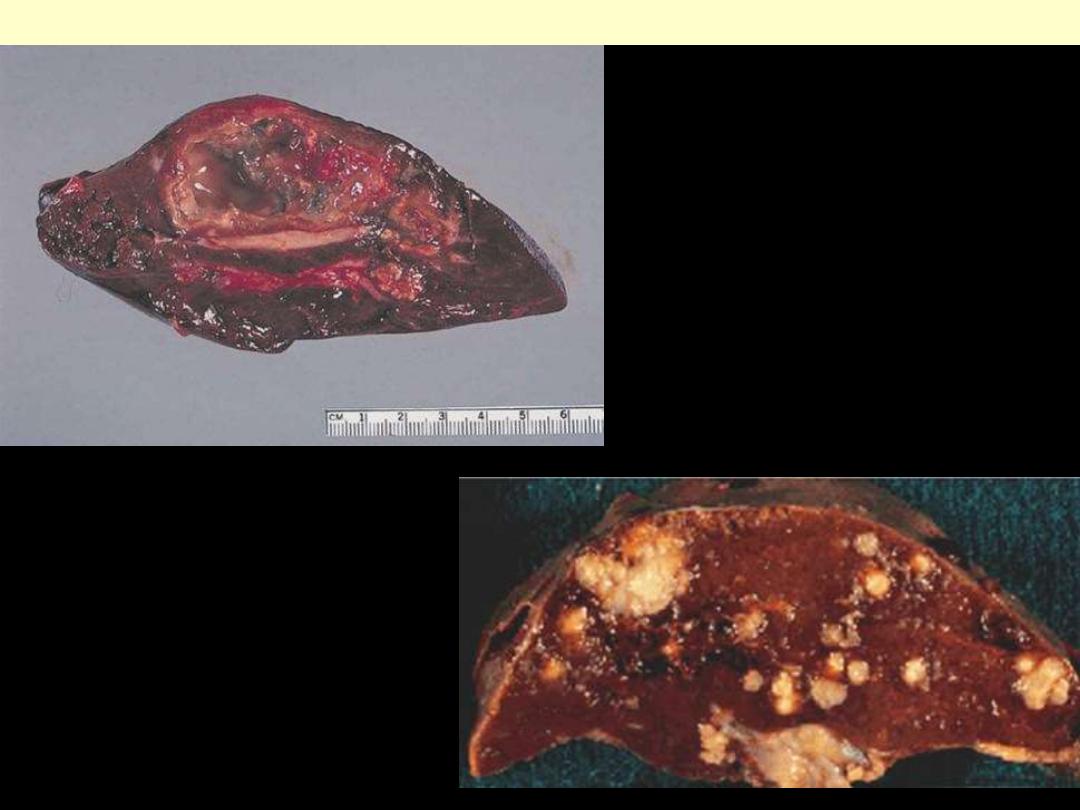
Liver abscess
Large liver abscess surrounded by a
thick fibrous wall. It has
liquefactive center.
•
Multiple tan white nodules of
varying size.
•
Some have whiter, softer
centers.
•
Most are surrounded by a
darker colored region which
may represent hemorrhage.
Abscesses in liver may also occur with
hematogenous spread from other areas of the
body with septicemia. Here are seen many
microabscesses in the liver in a patient with
Candida septicemia.
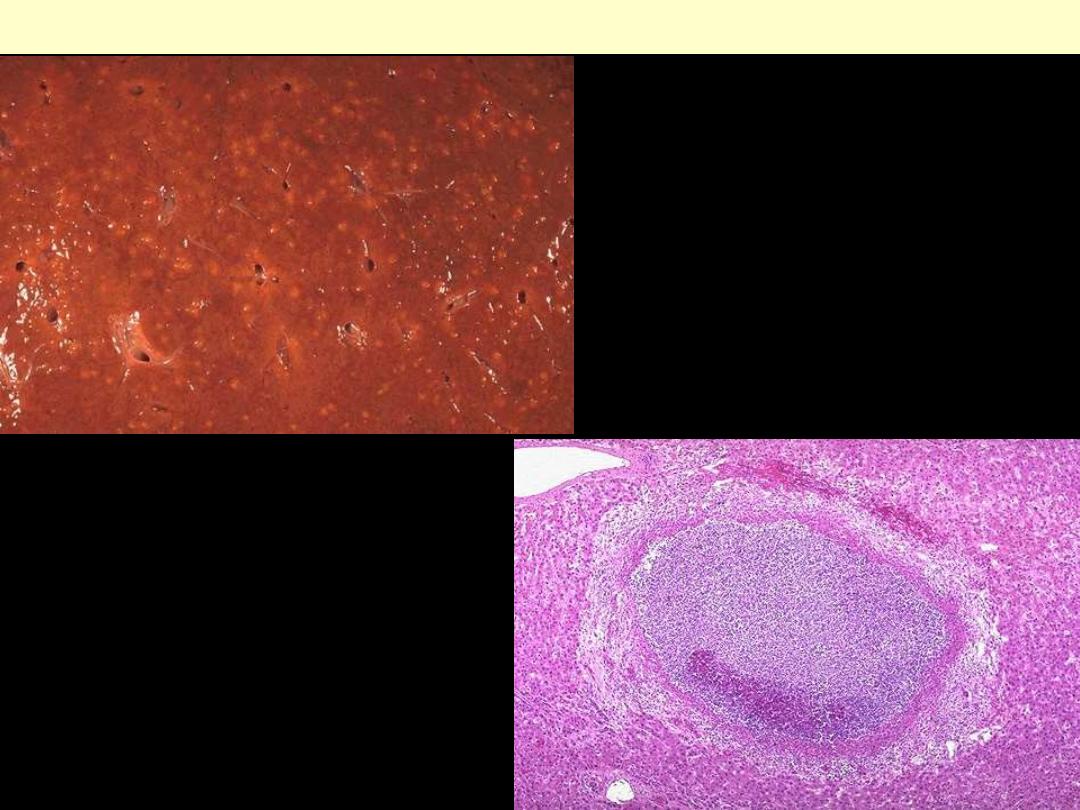
Micro-abscesses liver
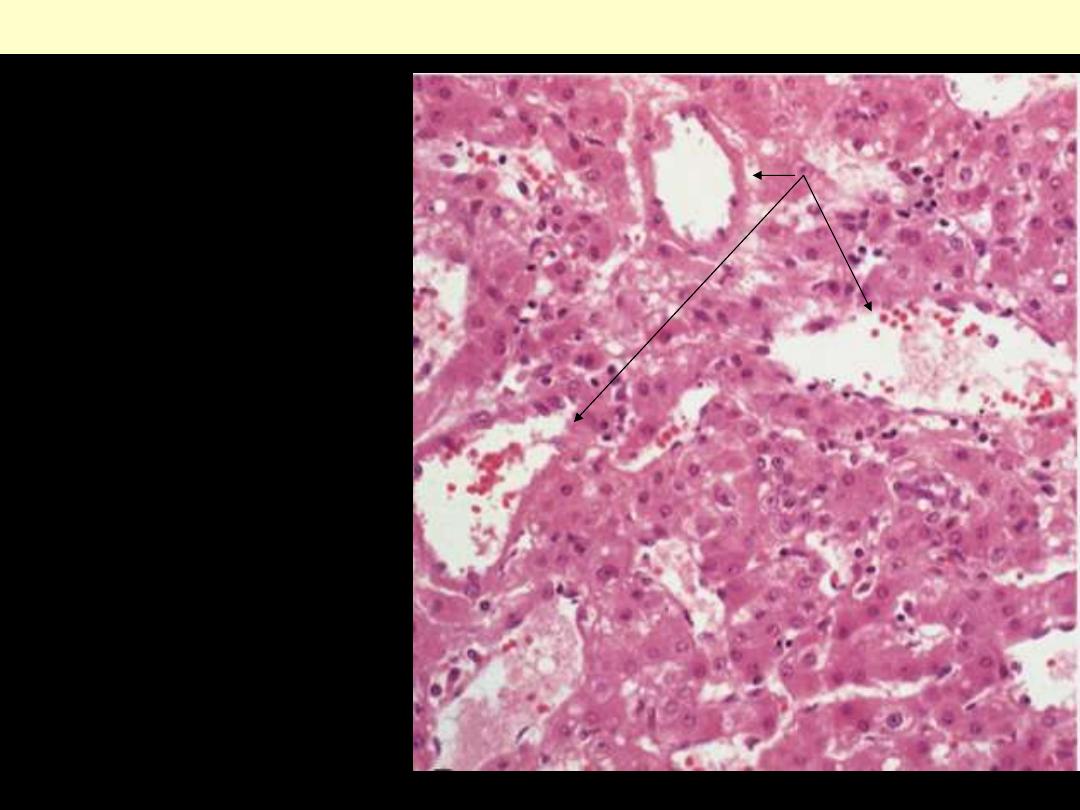
A microabscess of liver contains numerous
neutrophils in the center. The beginning of
an organizing abscess wall with some pink
fibrin is seen here.
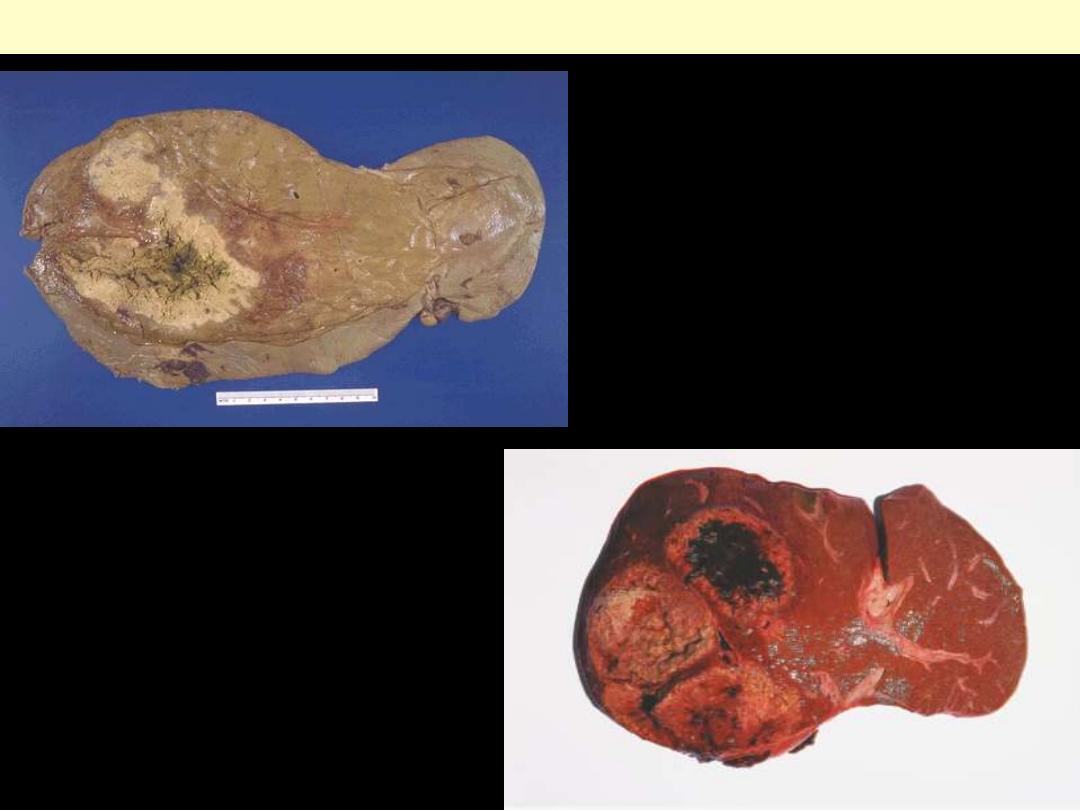
Amebic abscess liver
Abscesses may arise in liver when there is seeding
of infection from the bowel, because the infectious
agents are carried to the liver from the portal
venous circulation.
Amebic abscesses occupying most of the right
lobe of the liver. Three distinct lobules are seen.
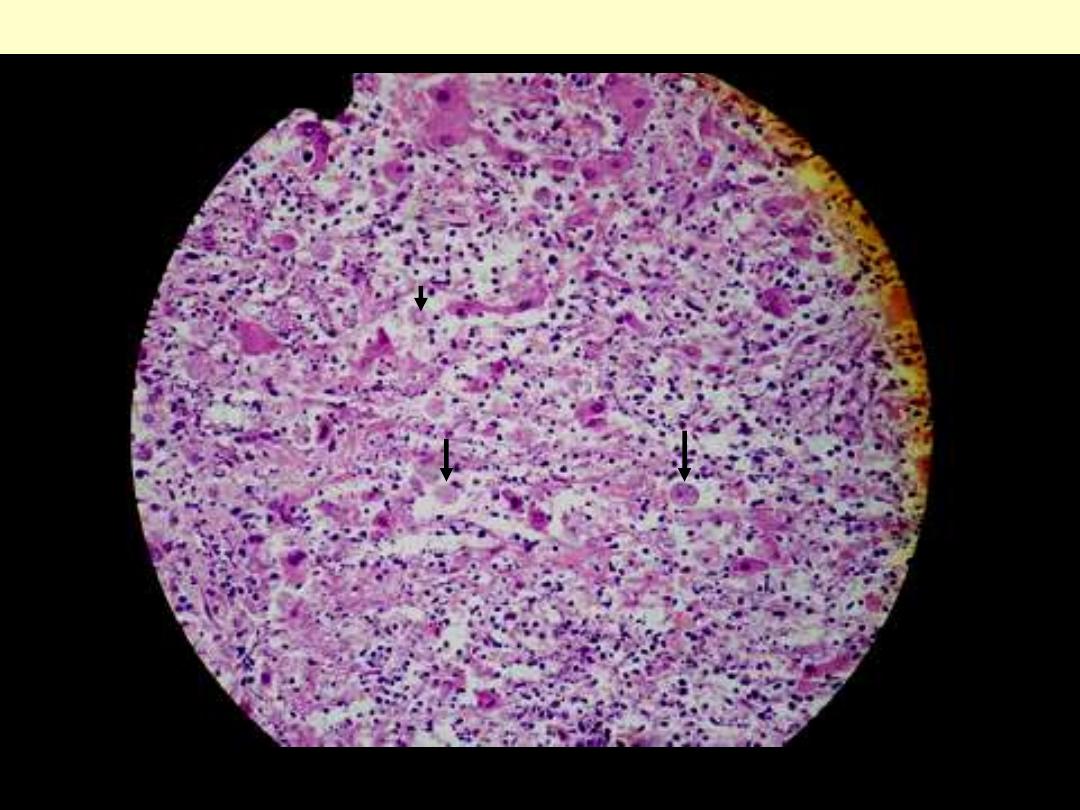
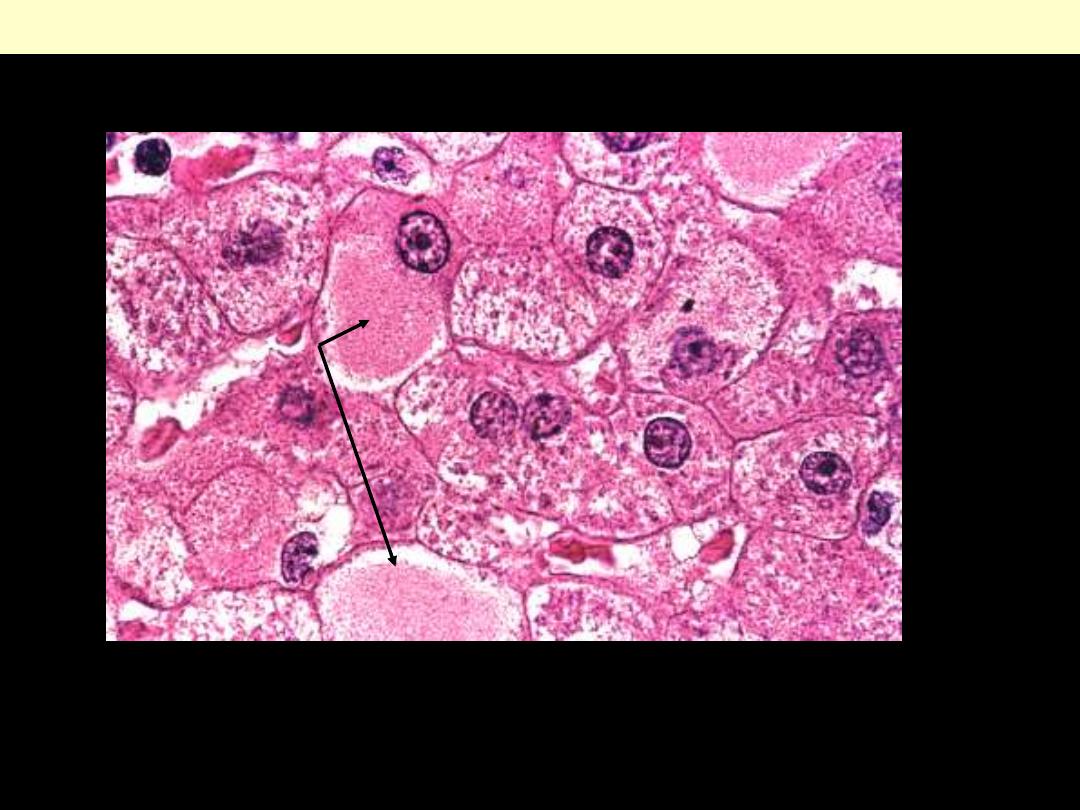
Amebic liver abscess in human. Trophozoites of Entamoeba histolytica are well observed (arrow).
H&E, X400.
Amebic abscess liver
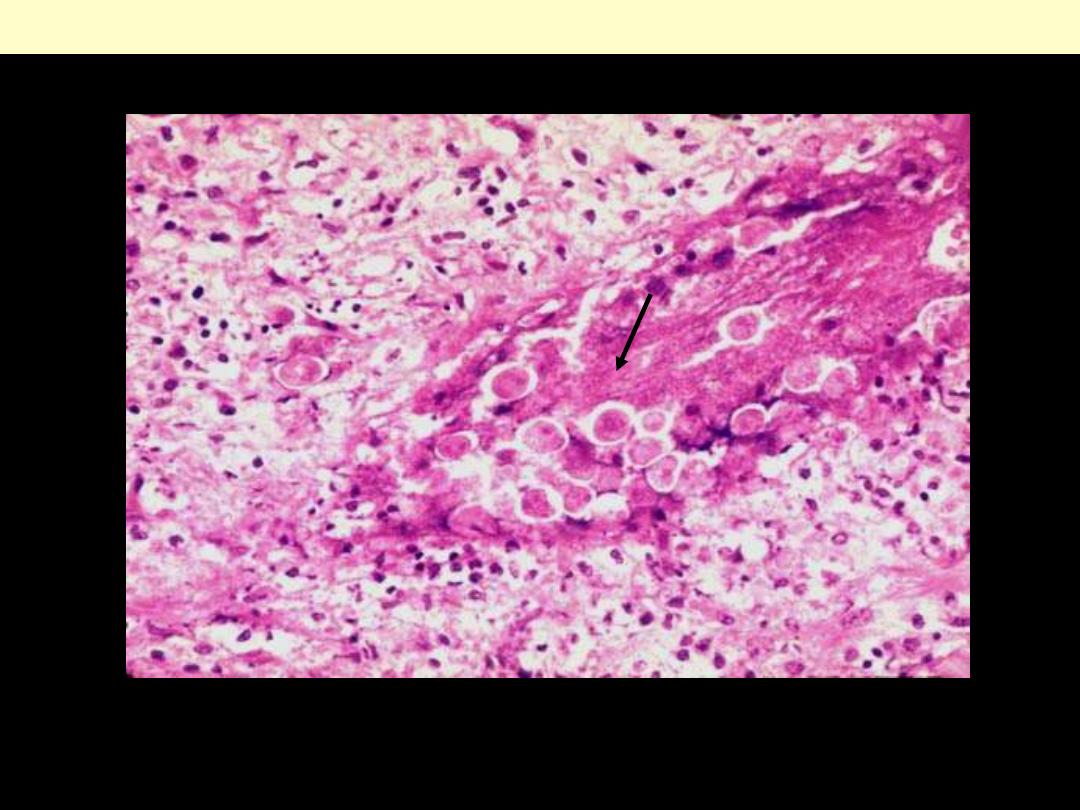
Clusters of trophozoites
Amebic abscess liver
Alcoholic liver disease
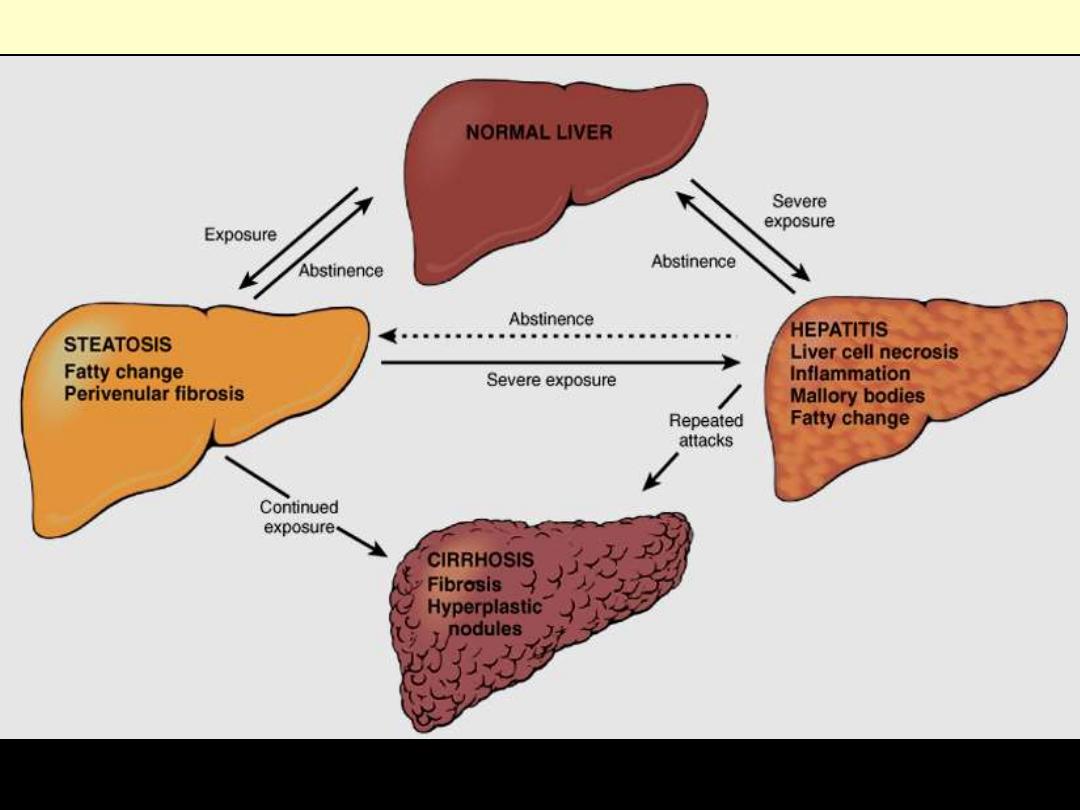
The interrelationships among hepatic steatosis, hepatitis, and cirrhosis are shown, along with a
depiction of key morphologic features at the microscopic level.
Alcoholic liver disease
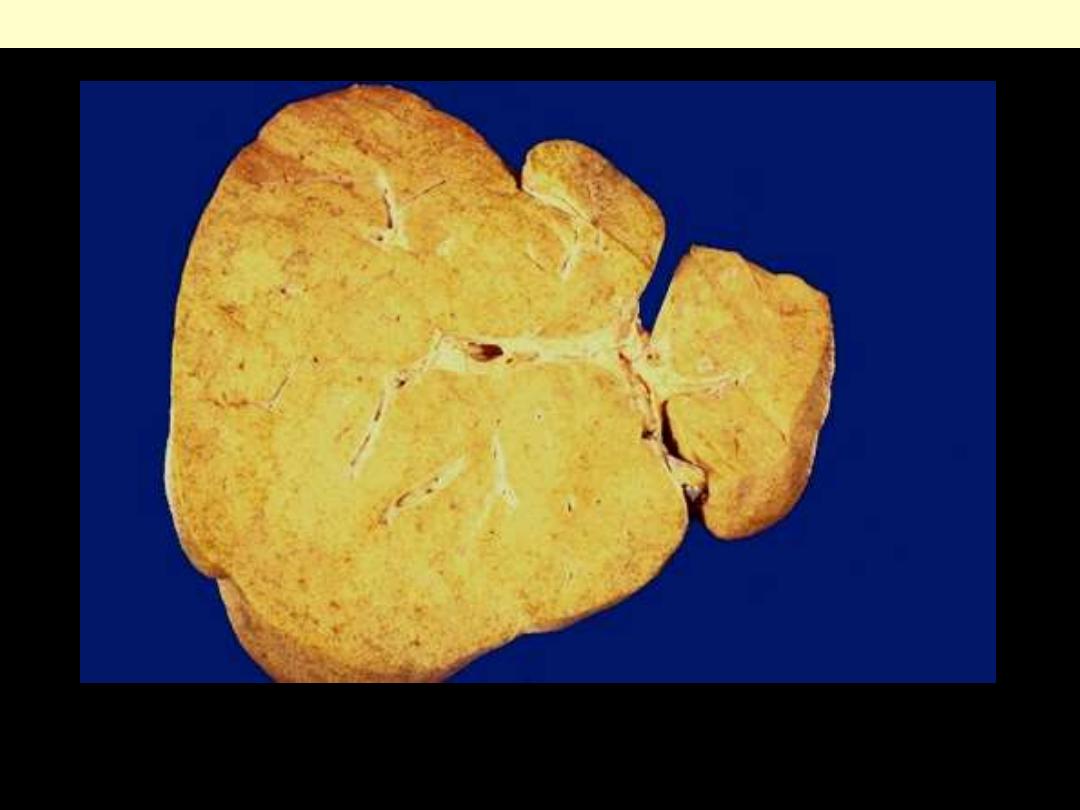
Severe fatty change liver
The liver is enlarged, soft, greasy and diffusely yellow in color.
Fatty change liver
Normal
Fatty change
•
Initially small lipid droplets accumulate in hepatocytes
Alcoholic Microvesicular Steatosis
Alcoholic steatosis
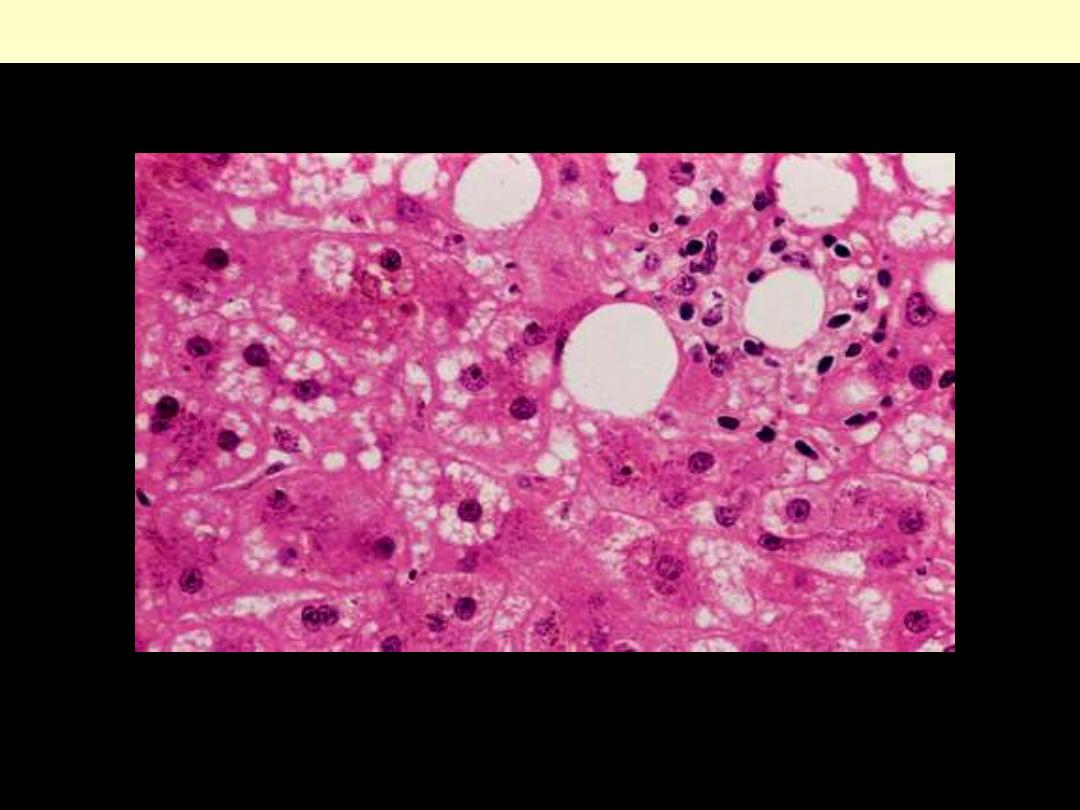
Hepatic steatosis in patient with alcohol abuse. The picture shows a mixture of macrovesicular and
microvesicular steatosis and a lipogranuloma (upper right corner). (H&E)
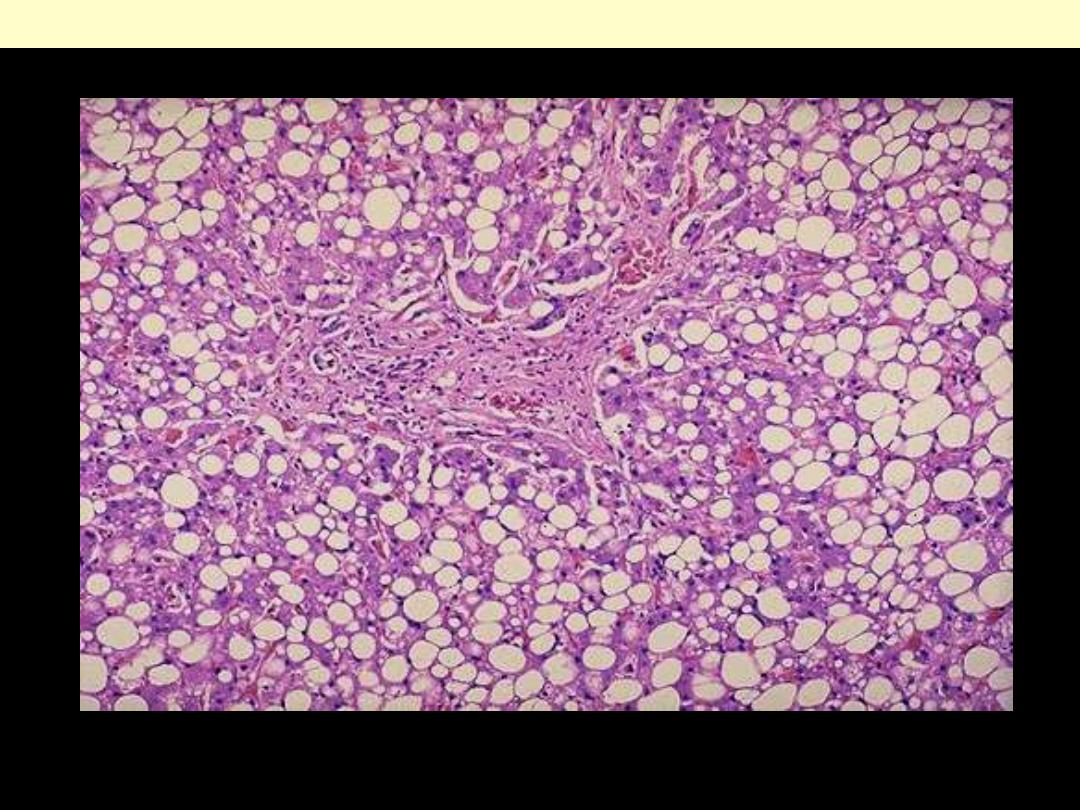
Alcoholic steatosis
Moderately severe degree of alcoholic macrovesicular steatosis
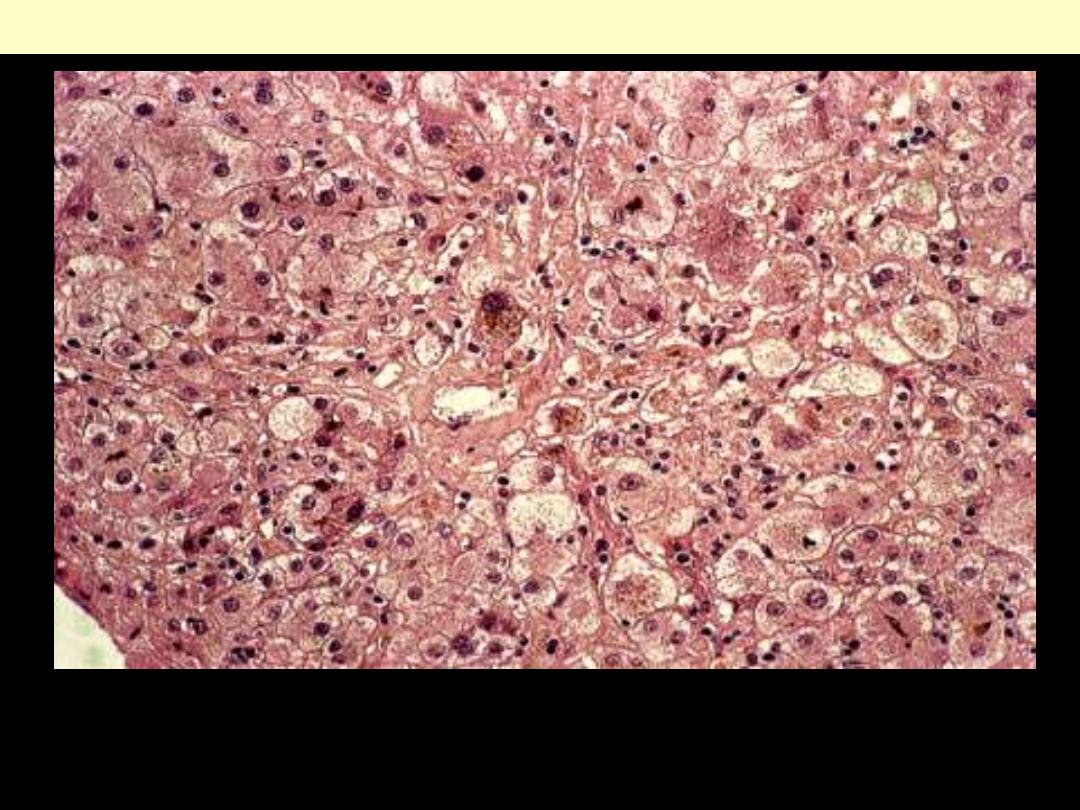
Alcoholic hepatitis (ASH)
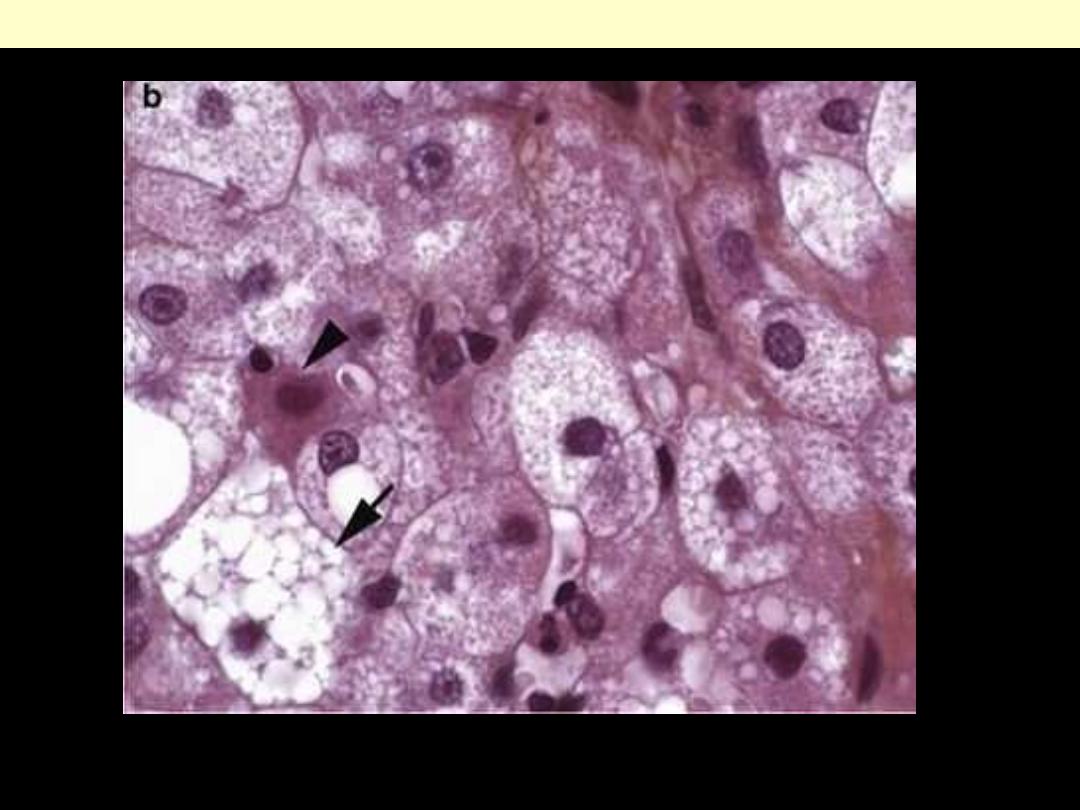
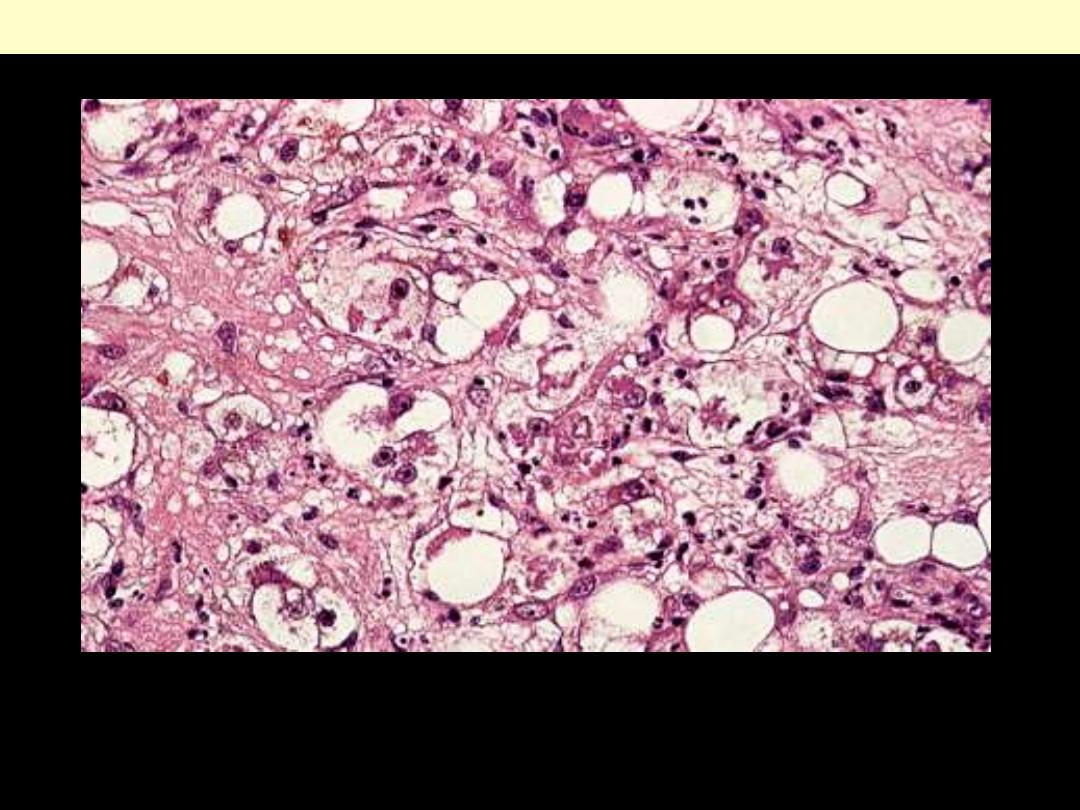
Detail of centrilobular parenchyma, characterized by pericellular fibrosis, steatosis, hydropic swelling
of several hepatocytes containing Mallory bodies. (H&E)
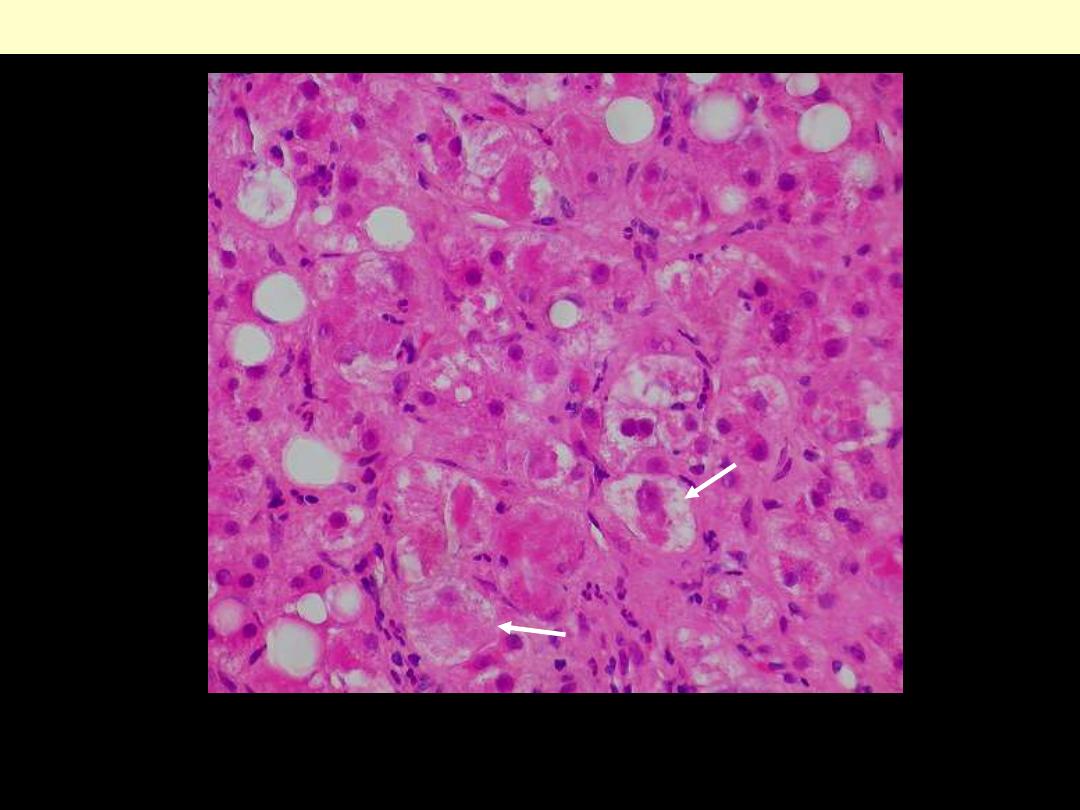
This is from a core biopsy of the liver of a patient who denied use of alcohol (despite her family's claims
to the contrary). Features of alcoholic liver disease, include steatosis, Mallory hyalin, & ballooning
degeneration (arrow).
Alcoholic hepatitis
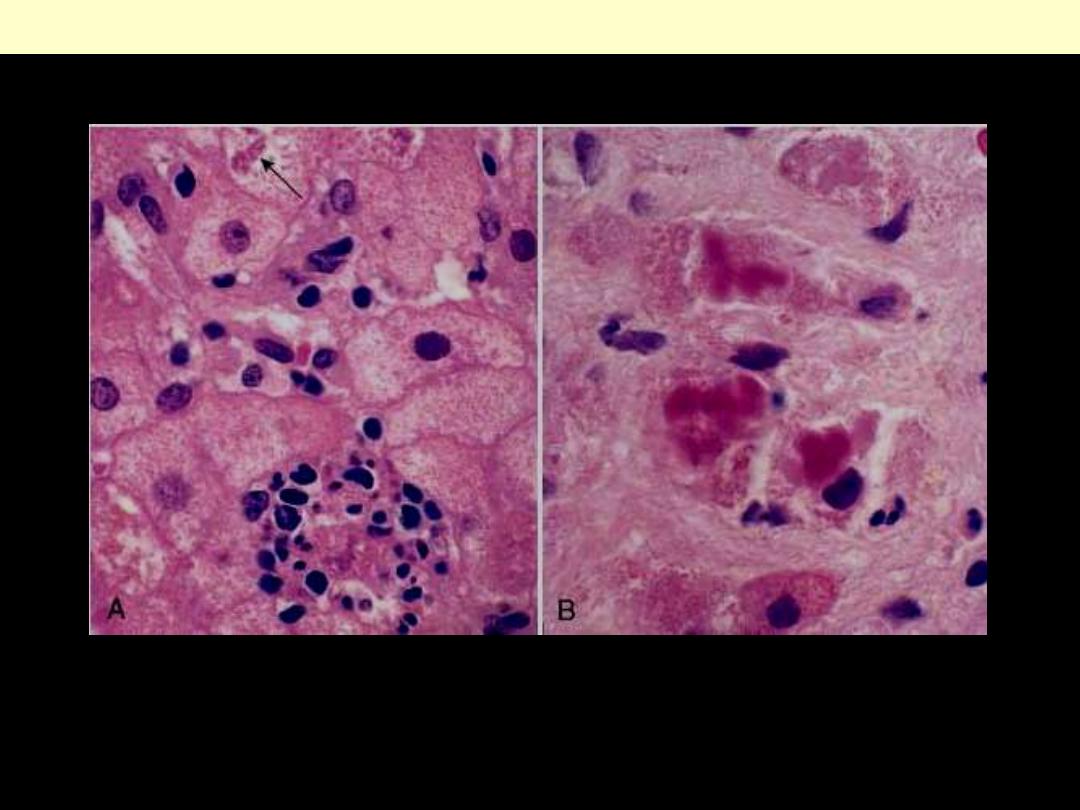
Alcoholic hepatitis
A, The cluster of inflammatory cells marks the site of a necrotic hepatocyte. A Mallory body is present
in a second hepatocyte (arrow).
B, Eosinophilic Mallory bodies are seen in hepatocytes. (H&E).
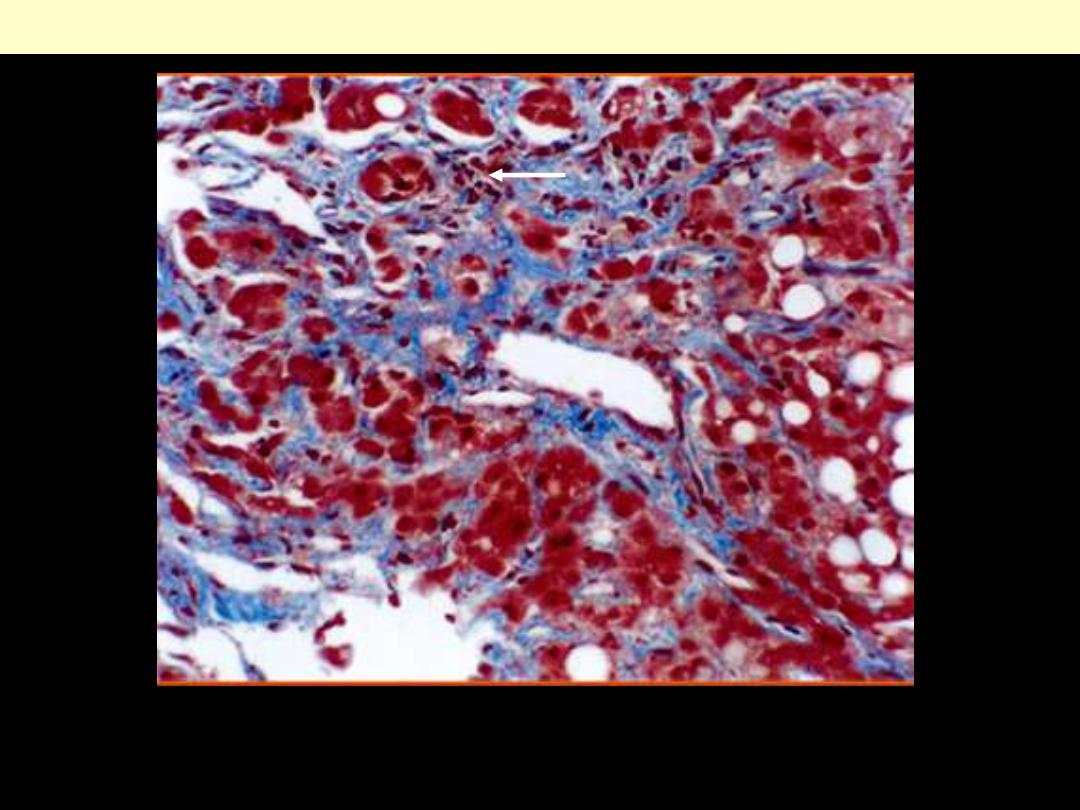
Pericentral (zone 3) sinusoidal fibrosis, typical of alcoholic steatohepatitis. Also note the presence of
patchy mixed inflammation (arrow) and mild microvesicular and macrovesicular steatosis (Masson
trichrome, magnification × 200).
Alcoholic hepatitis
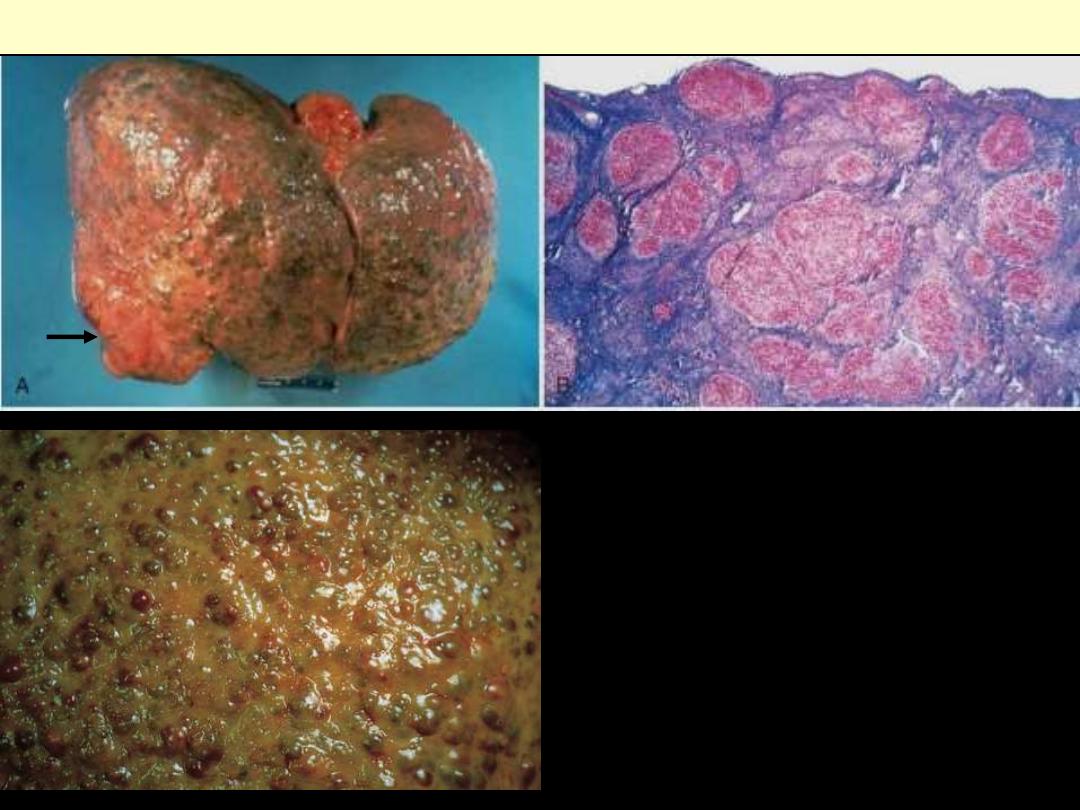
Alcoholic cirrhosis
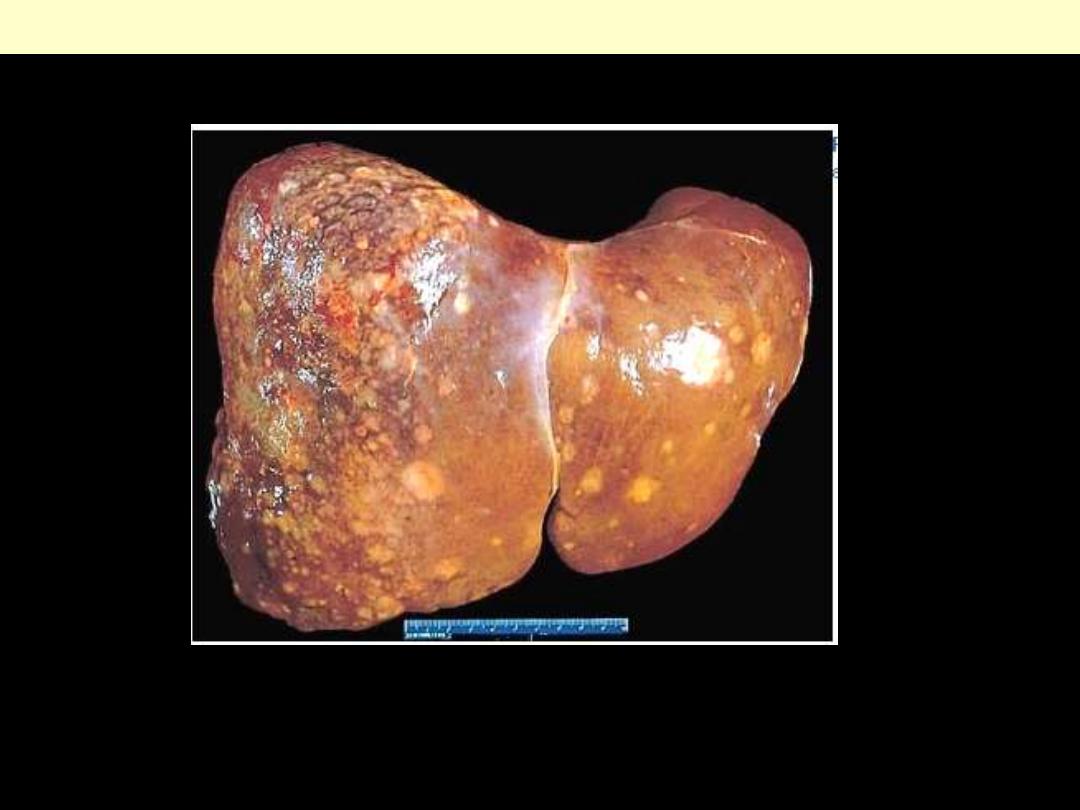
Alcoholic cirrhosis. A, The characteristic diffuse
nodularity of the surface reflects the interplay
between nodular regeneration and scarring. The
greenish tint of some nodules is due to bile stasis. A
hepatocellular carcinoma is present as a budding
mass at the lower edge of the right lobe (arrow). B,
The microscopic view shows nodules of varying
sizes entrapped in blue-staining fibrous tissue. The
liver capsule is at the top (Masson trichrome). C,
characteristic diffuse nodularity of the surface
induced by the underlying fibrous scarring. The
average nodule size is 3 mm in this close-up view.
The greenish tint is caused by bile stasis.
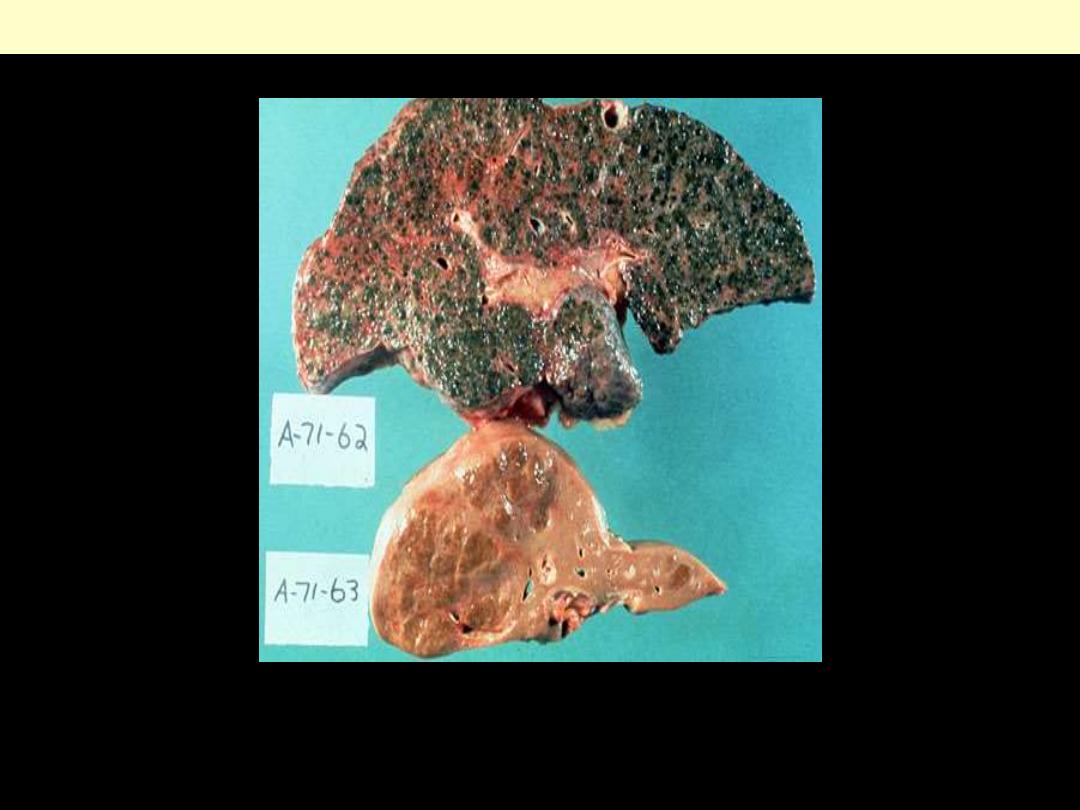
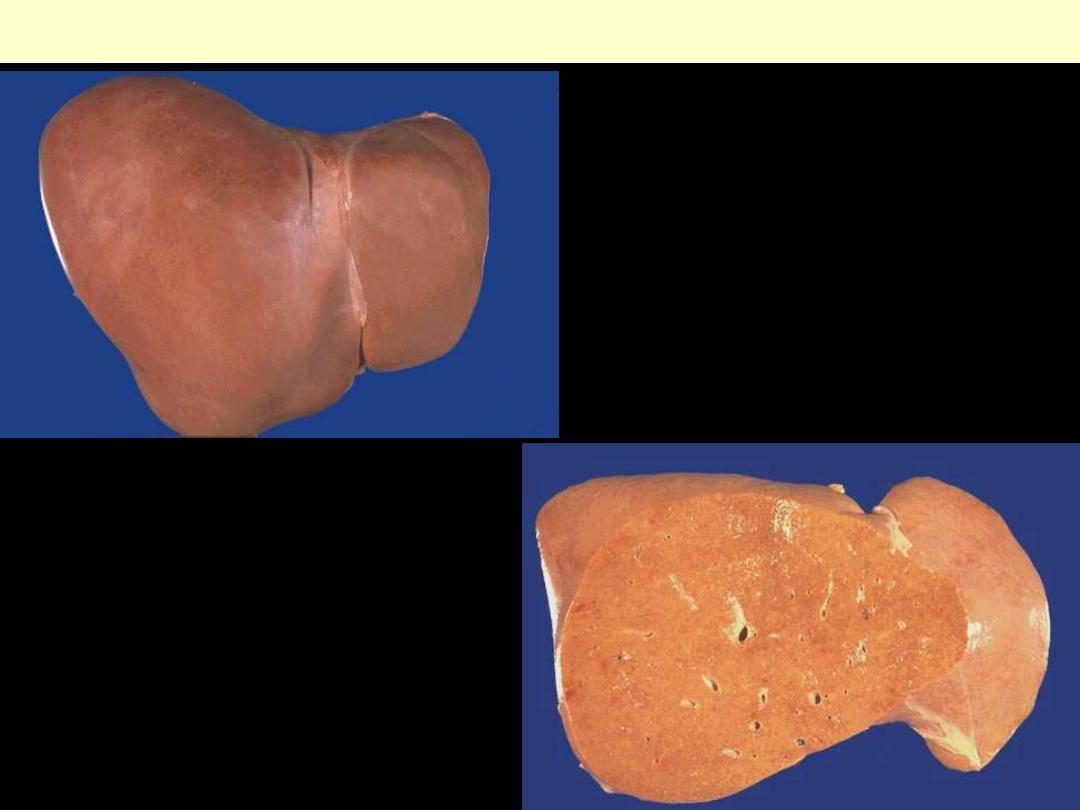
The disparity between the typical cirrhosis of chronic viral hepatitis (small liver, big nodules) and
alcoholic liver diseases (big liver, small nodules) is particularly evident here. The greenish discoloration
of the liver with alcoholic cirrhosis is due to bile stasis.
Alcoholic cirrhosis Vs cirrhosis of viral hepatitis
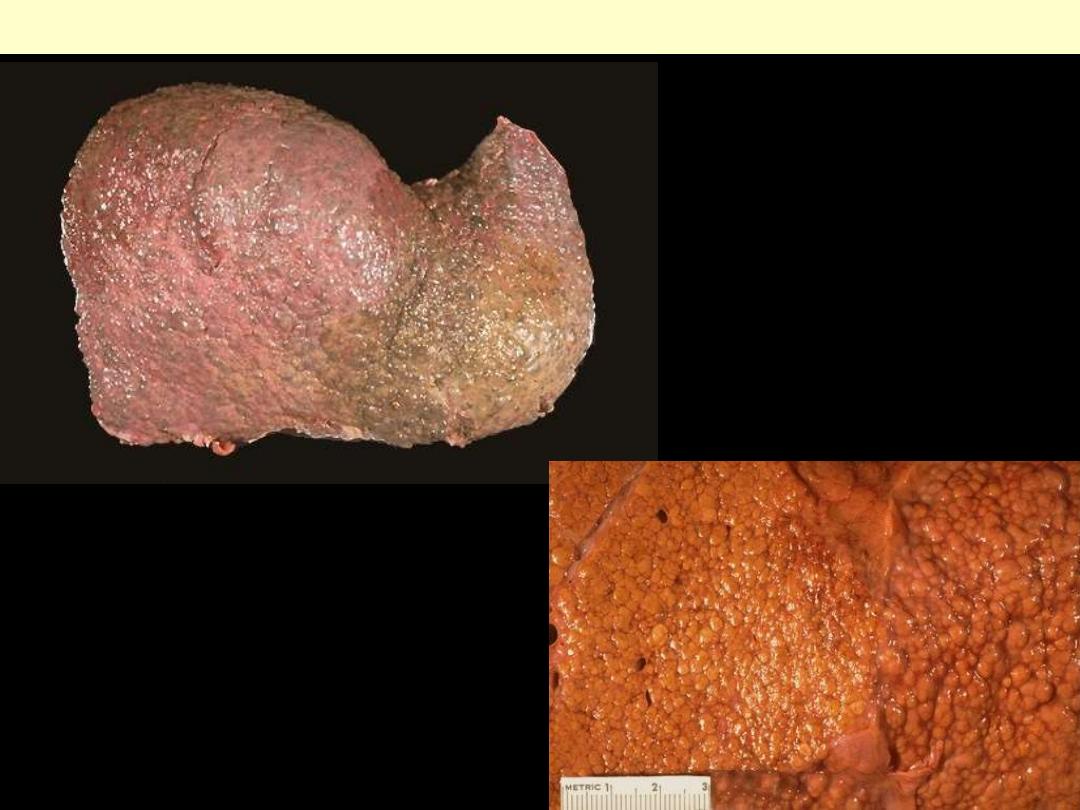
This is an example of a micronodular
cirrhosis. The regenerative nodules are
quite small, each averaging less than 3
mm in size.
Micronodular cirrhosis
The regenerative nodules of liver in this case of
micronodular cirrhosis are 3 mm in size or smaller.
The pale tan color is due to fatty change. The most
common cause of this form of cirrhosis is chronic
alcoholism.
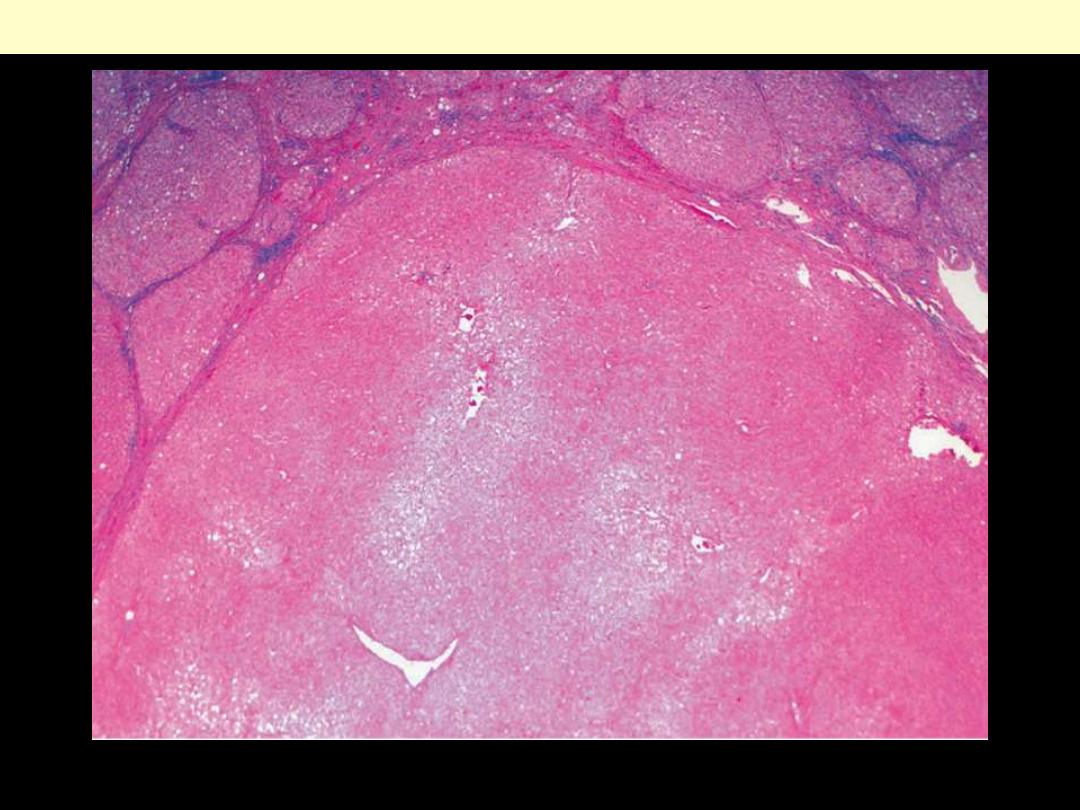
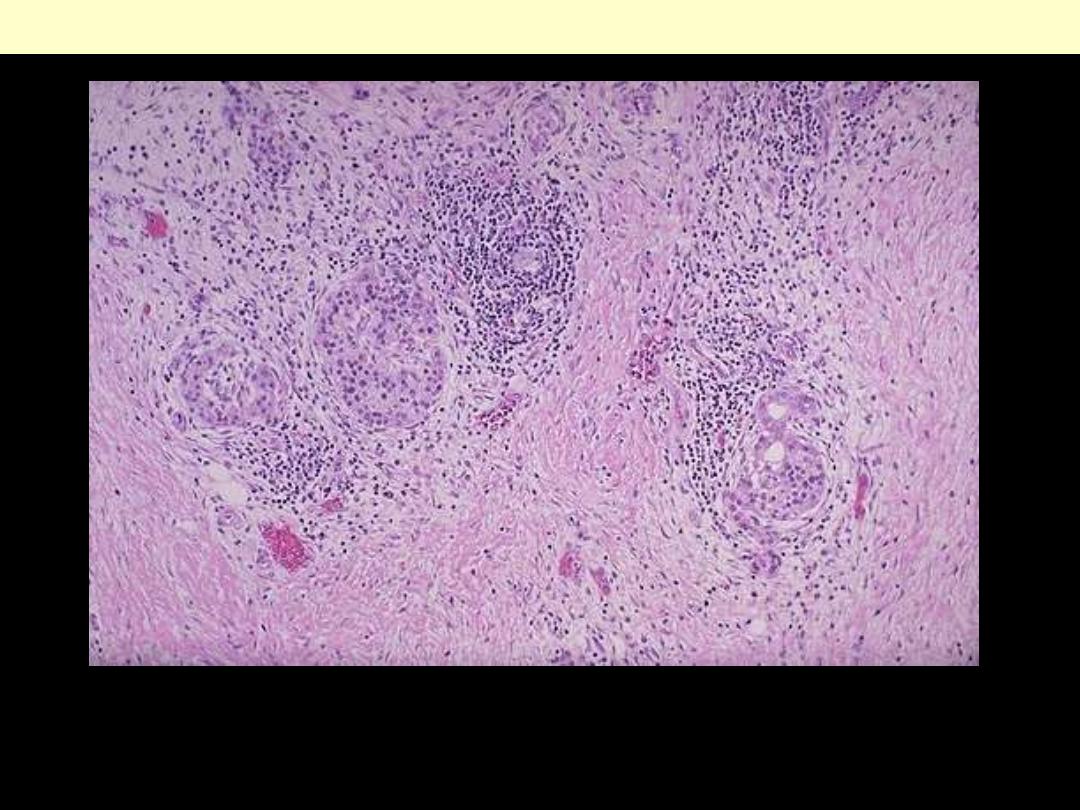
Primary biliary cirrhosis
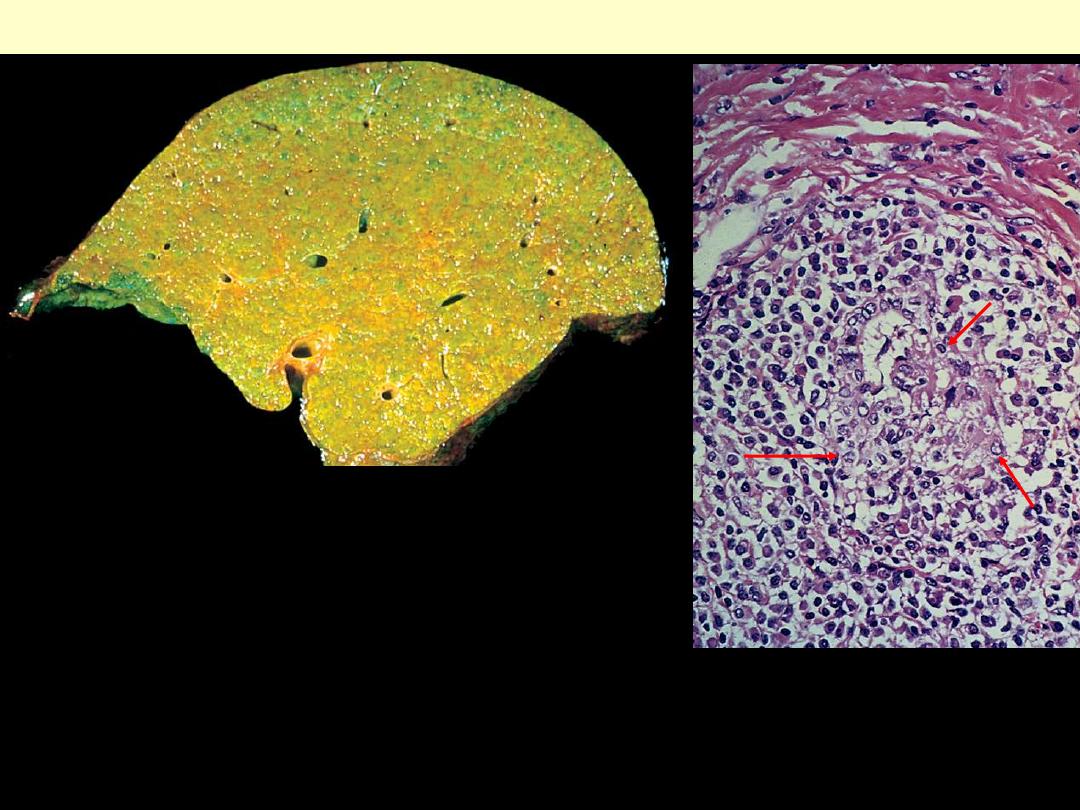
Primary biliarycirrhosis
A portal tract is markedly expanded by an
infiltrate of lymphocytes and plasma cells.
The granulomatous reaction to a bile duct
undergoing destruction (florid duct lesion)
is highlighted by the arrows.
This sagittal section through the liver
demonstrates the fine nodularity and bile
staining of end-stage primary biliary
cirrhosis.
Hepatitis – acute + chronic
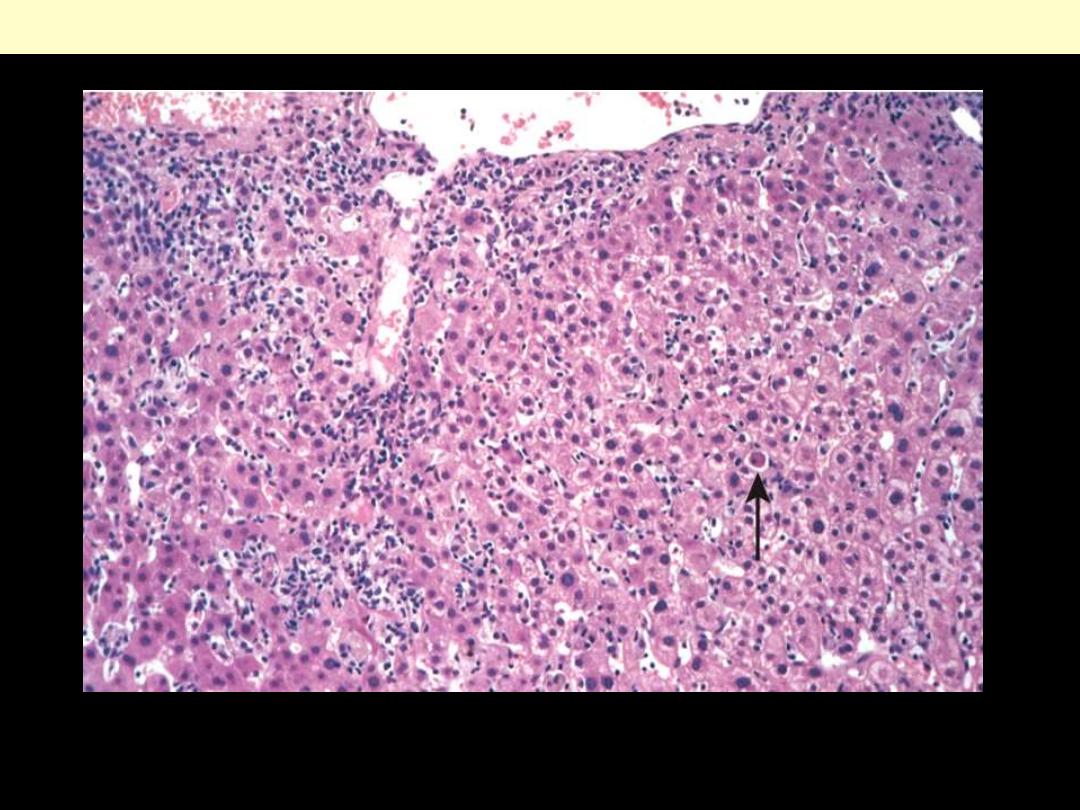
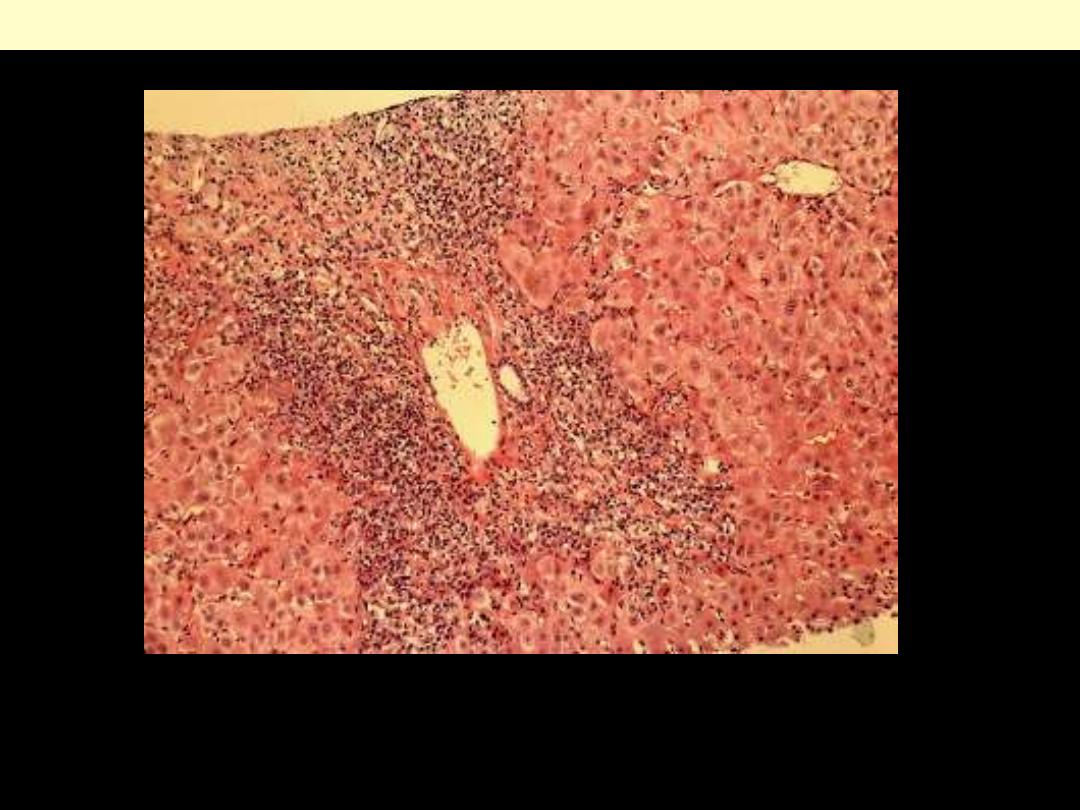
Acute viral hepatitis
There is disruption of lobular architecture, inflammatory cells in the portal tracts & sinusoids, and
hepatocellular apoptosis (arrow).
Acute viral hepatitis
Portal inflammation with interface hepatitis (arrow)
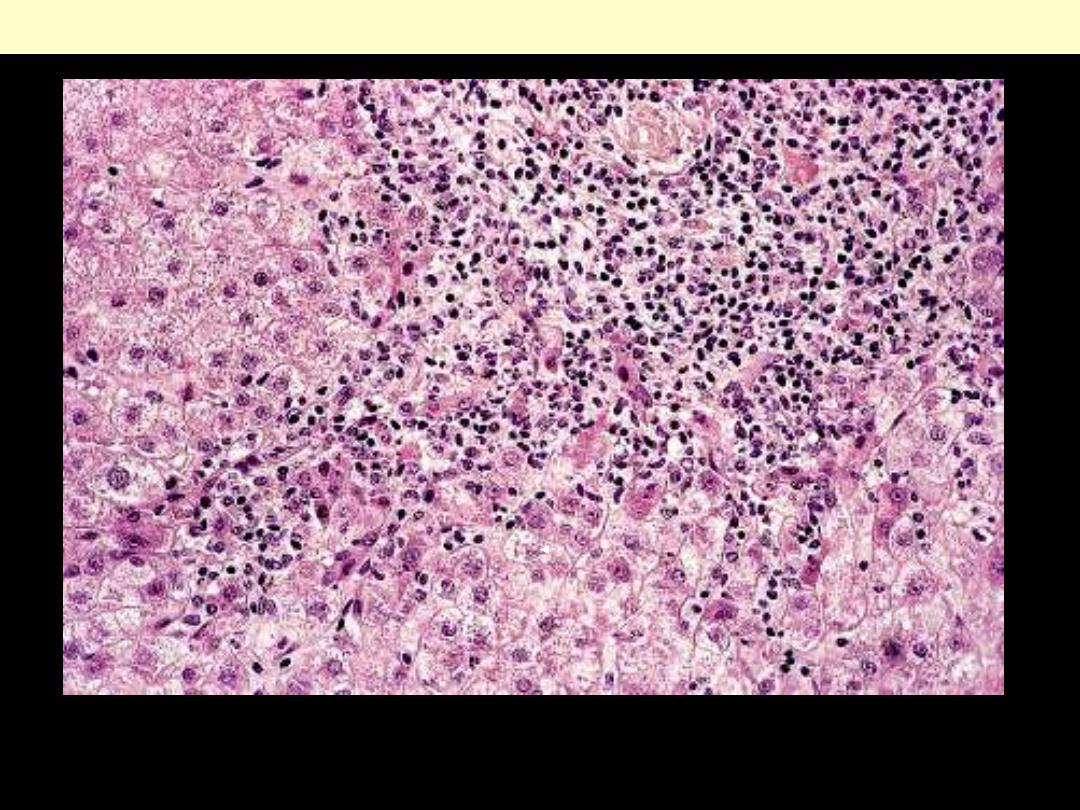
Acute viral hepatitis B
Acute viral hepatitis B. Centrolobular area of liver lobule, characterized by ballooning of hepatocytes, and
mononuclear (mainly lymphocytic) inflammatory infiltration. (H&E)
Hepatocytes shrink, become intensely
eosinophilic, and have fragmented or absent
nuclei. Apoptotic cells are phagocytosed within
hours by macrophages and hence may be difficult
to find despite extensive apoptosis.
Acute viral hepatitis: Acidophilic (apoptotic) bodies
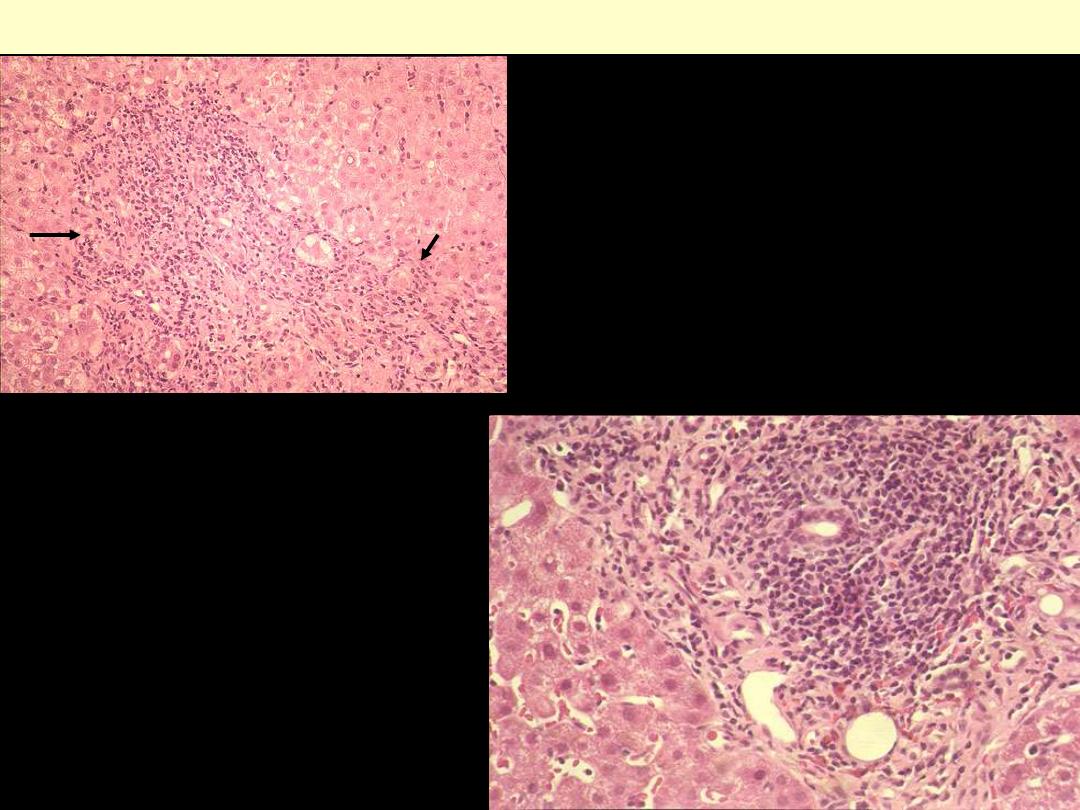
Acute viral hepatitis B with confluent necrosis
Severe necrotizing acute viral hepatitis B. Overview of liver lobule; mild to moderate mononuclear cell
infiltration in portal tracts (lower left, top, and lower right). Bridging portal-central confluent lytic
necrosis, creating a "star-shaped" area of necrosis with a centri-lobular vein at its center (arrow) and
peripheral points reaching portal tracts. Inflammatory cells are scattered throughout the lobule.
(H&E)
Interface hepatitis. Lymphocytic infiltrates extend from the portal tracts into acinar tissue with
destruction of the limiting plate. Findings are consistent with autoimmune hepatitis, drug reaction, or
viral infection.
Chronic hepatitis showing interface hepatitis (formerly piecemeal necrosis)
Note inflamed portal tract (upper right) and wedge-like extension of necro-inflammation (towards
lower left) and irregular interface between portal periphery and adjacent parenchyma.
Interface hepatitis (piecemeal necrosis)
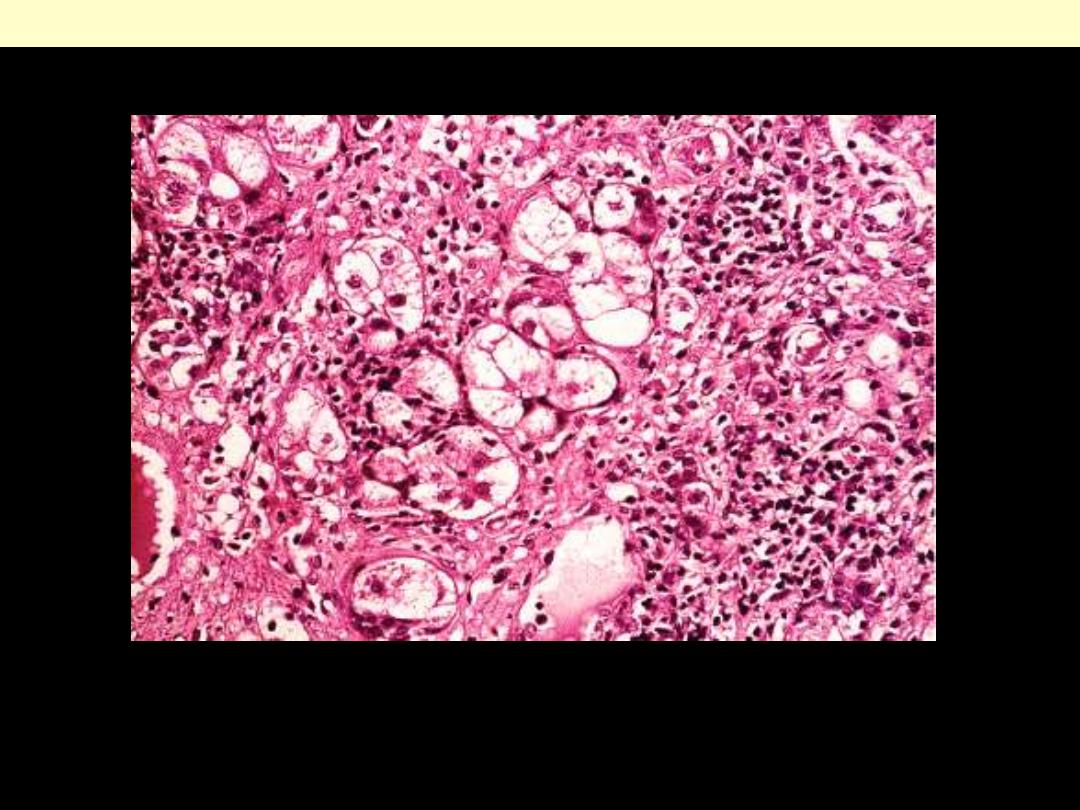
Severe chronic viral hepatitis B. Area of multilobular lytic necrosis in phase of postnecrotic collapse
and early fibrosis, with several small islands of surviving hepatocytes, appearing swollen and pale, and
sometimes arranged in tubular fashion (”hepatitic-type liver cell rosettes”). (H&E)
Chronic hepatitis with hepatocytes regeneration (hepatitic-type liver cell rosettes)
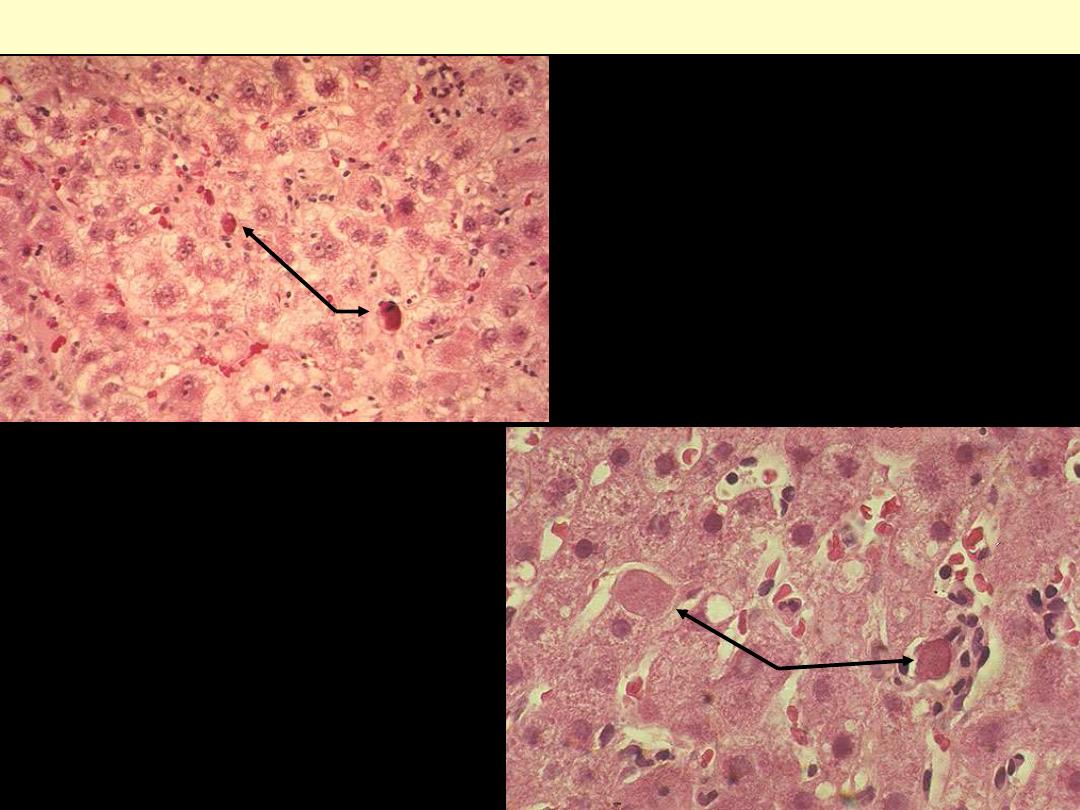
Ground glass hepatocytes, characterized by more pale, eosinophilic, and homogeneous cytoplasm than
surrounding normal (more granular) hepatocytes. Note (artifactual) cleft between "ground glass"
cytoplasm and hepatocellular cell membrane. The change corresponds to extensive endoplasmic
reticulum hyperplasia and massive accumulation of HBsAg. (H&E)
Chronic viral hepatitis B showing ground glass hepatocytes
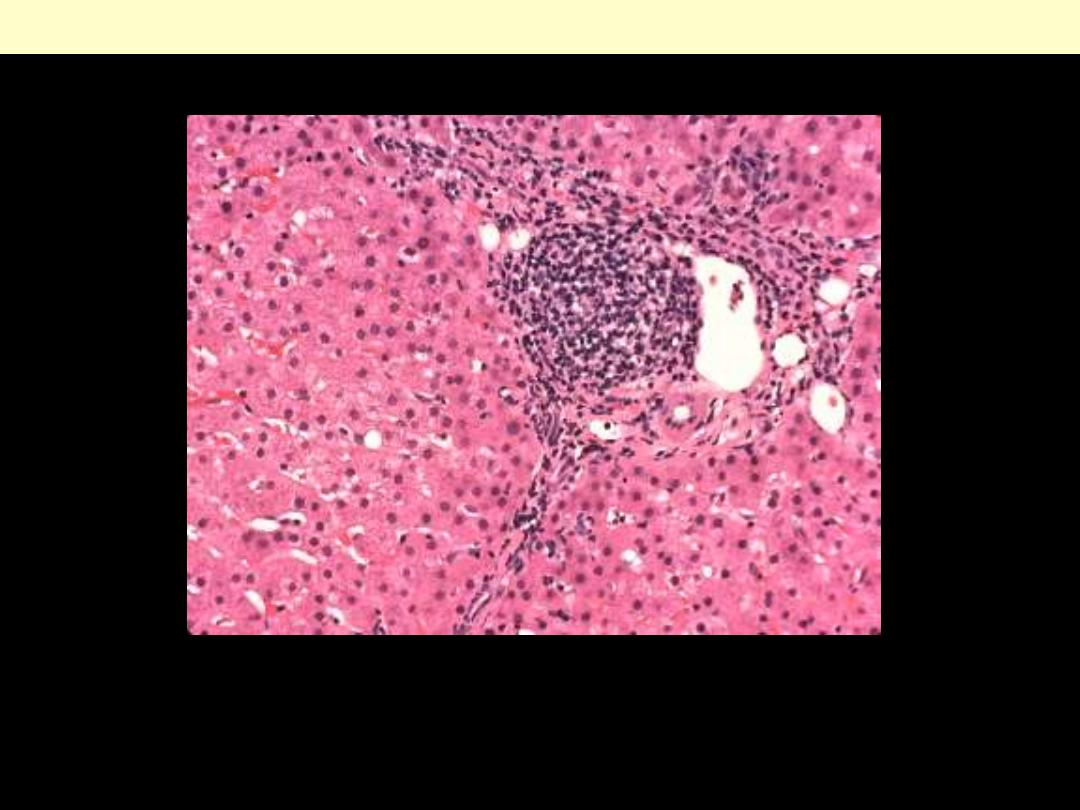
Portal lymphoid aggregates and minimal steatosis. The findings are consistent with a chronic hepatitis
C infection.
Chronic viral hepatitis C
This is a case of viral hepatitis C with extensive fibrosis and progression to macronodular cirrhosis, as
evidenced by the large regenerative nodule at the center right.
Chronic viral hepatitis C progressing to cirrhosis

Cirrhosis resulting from chronic viral hepatitis. Note the irregular nodularity of the liver surface
resulting in a macronodular pattern of cirrhosis.
Posthepatitic cirrhosis
Hydatid disease
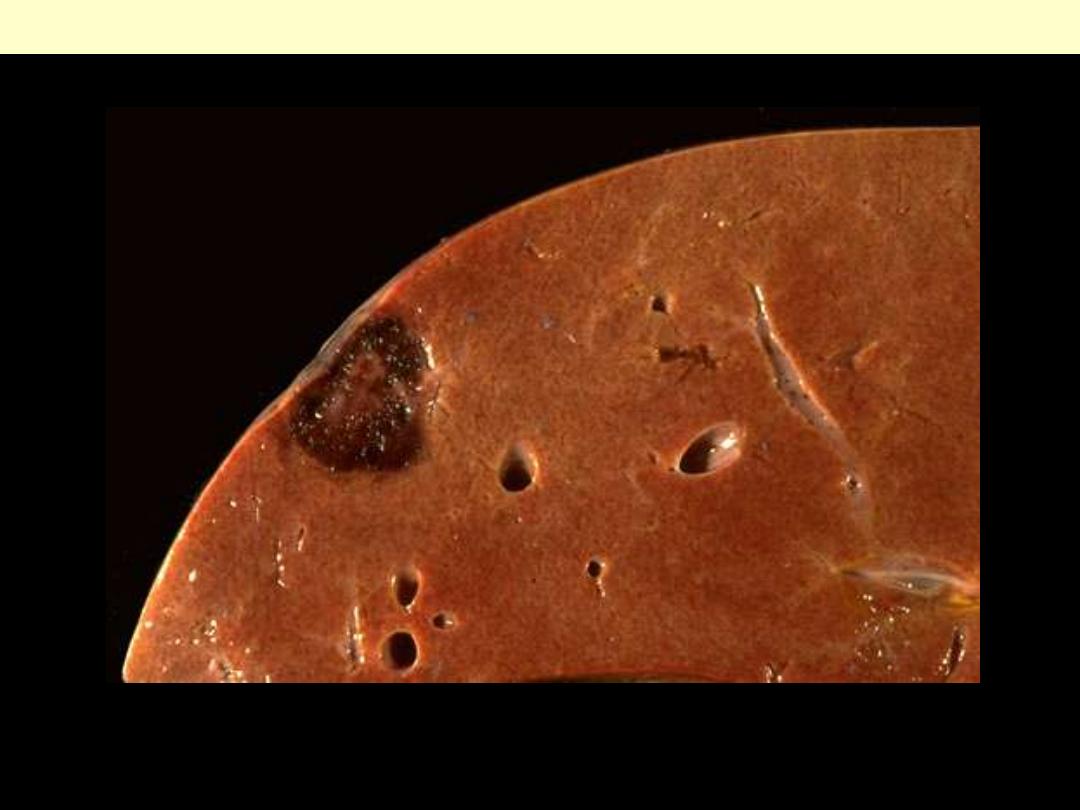
Hydatid cyst
The characteristic laminated membrane is bile stained due to communication of the cyst with the
biliary tree.
Massive necrosis
Massive hepatic necrosis
Figure 18-22 Massive necrosis. A, Cut section of liver. The liver is small (700 gm), bile-stained, and
soft. The capsule is wrinkled. B, Microscopic section. Portal tracts and terminal hepatic veins are closer
together than normal, owing to necrosis and collapse of the intervening parenchyma. An infiltrate of
mononuclear inflammatory cells is present.
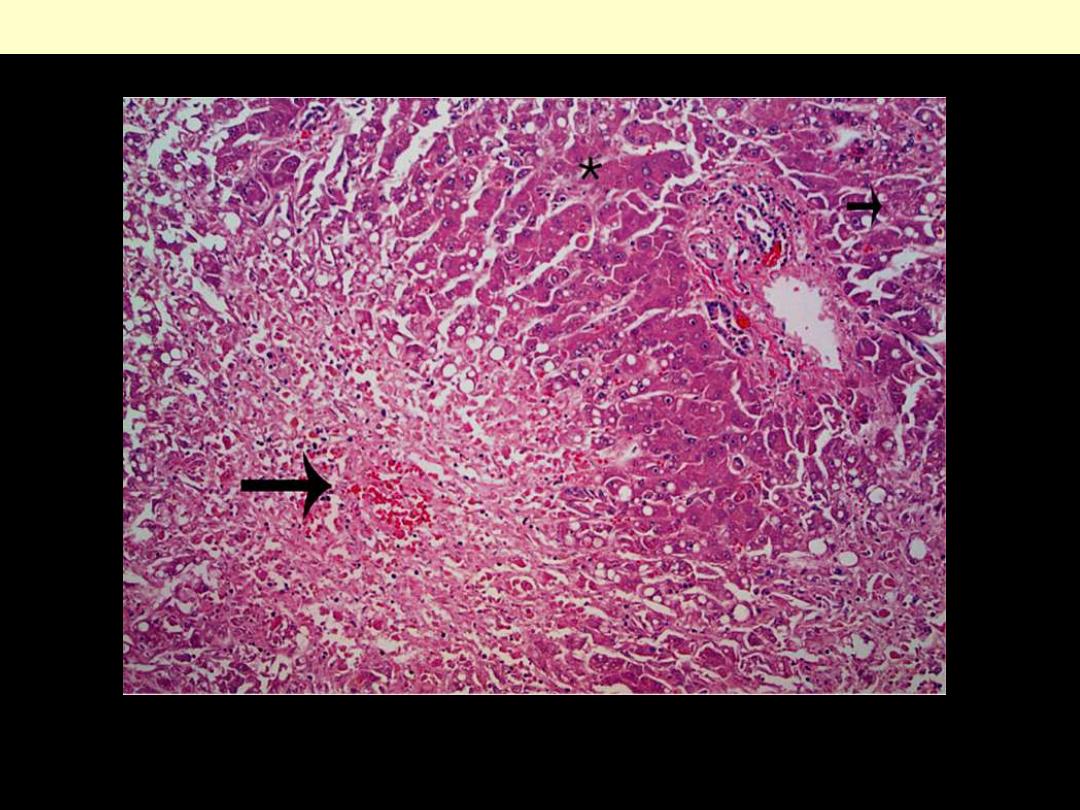
Confluent necrosis is seen in the perivenular region (zone 3; large arrow). There is little inflammation.
The residual normal tissue is indicated by the asterisk.
Acetaminophen overdose causing hepatocellular necrosis
Metabolic diseases
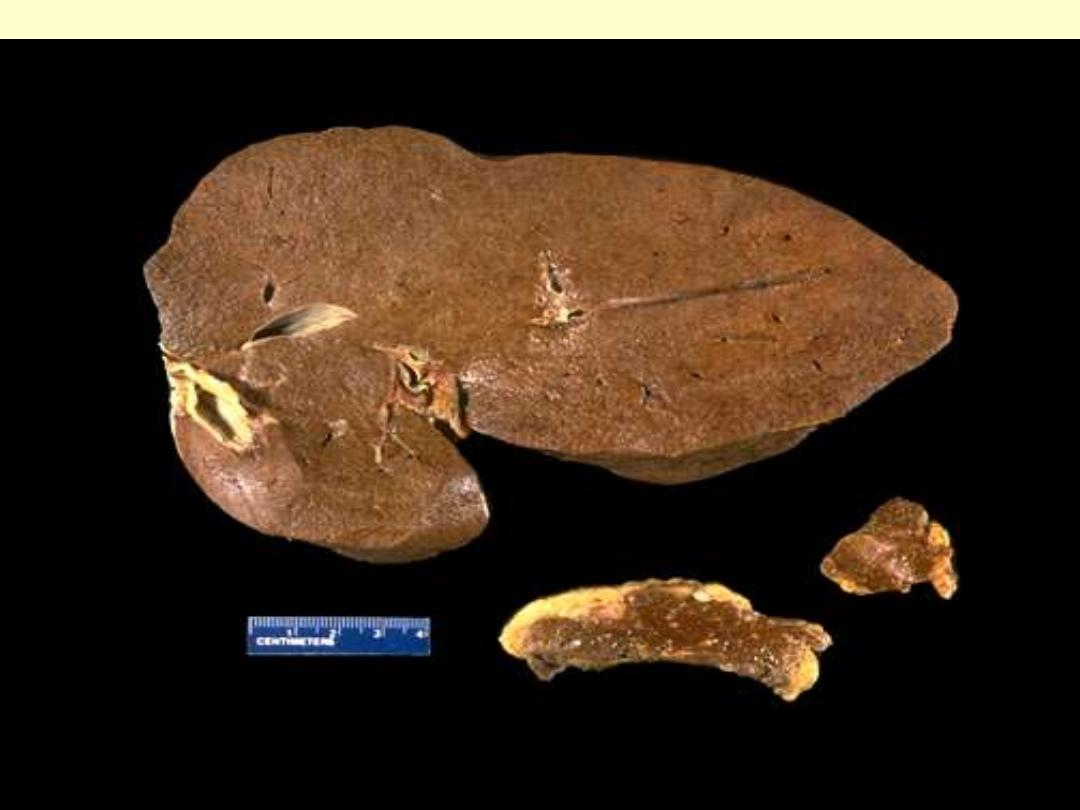
Hemochromatosis liver pancreas and lymph node
The dark brown color of the liver, as well as the pancreas (bottom center) and lymph nodes (bottom
right) on sectioning is due to extensive iron deposition in a middle-aged man with hereditary
hemochromatosis.
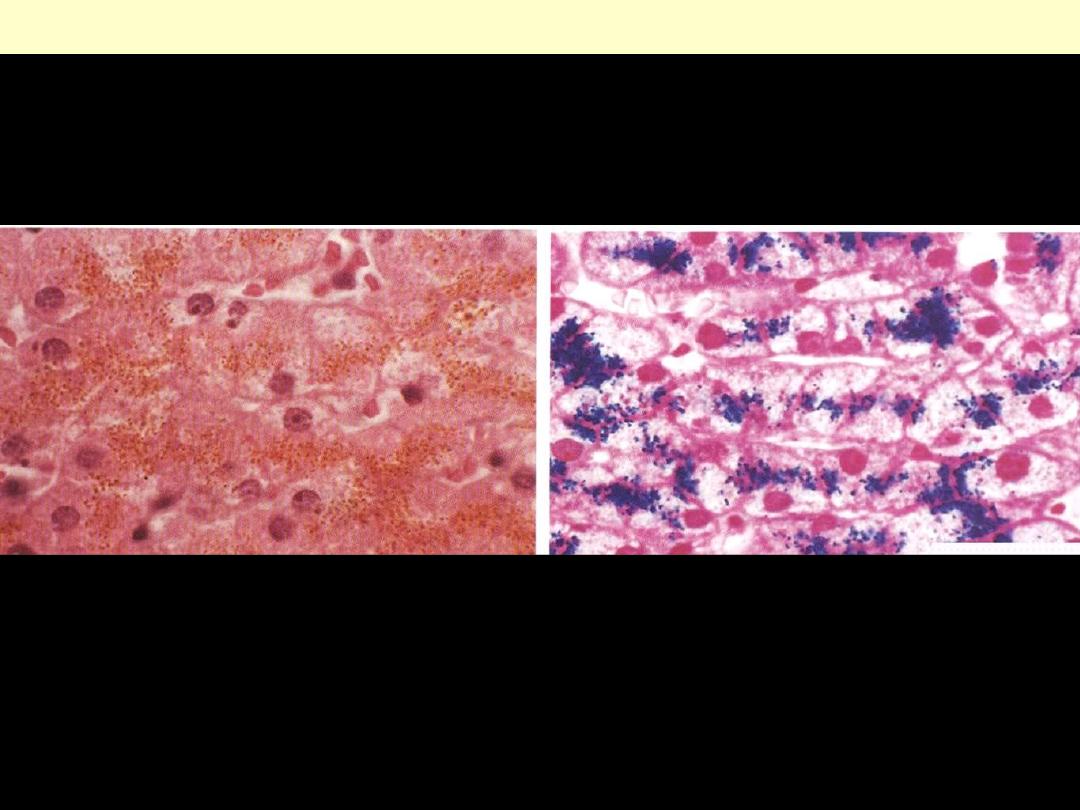
Rt: H&E stained section showing hemosiderin as yellow-brown finely granular pigment within
hepatocytes.
Lt.: same section stained with an iron stain (Prussian blue); the hemosiderin granules are deep blue.
Hemochromatosis liver
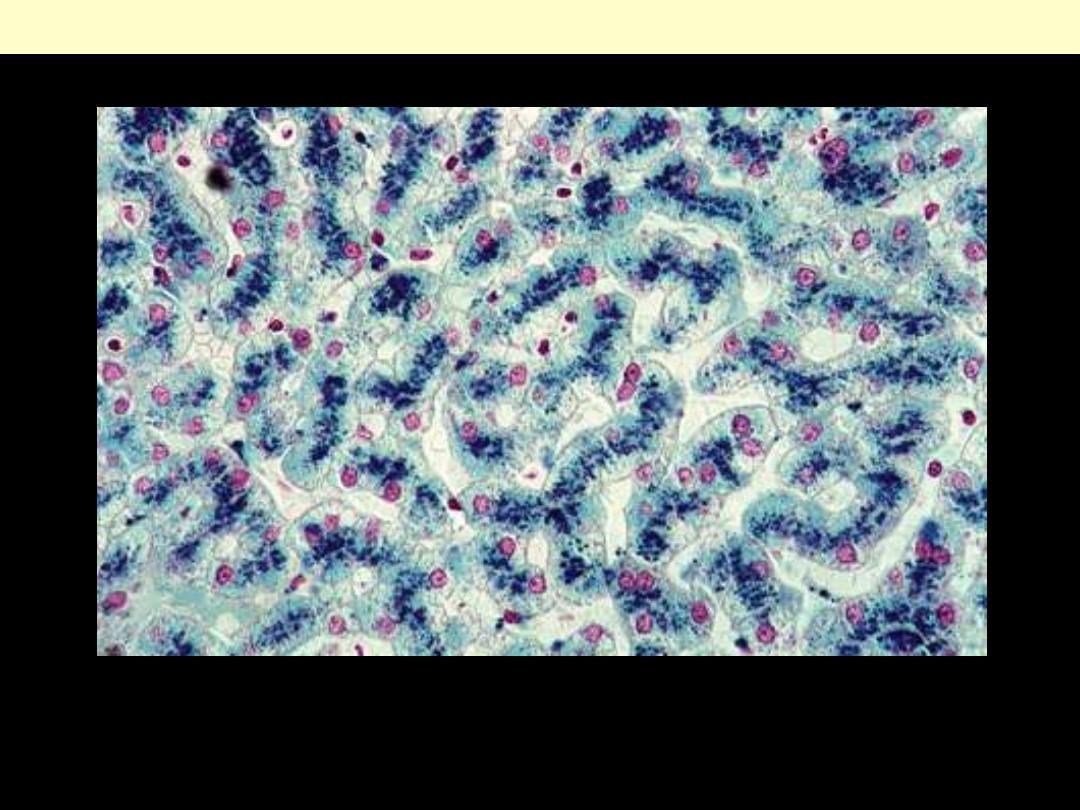
Hereditary hemochromatosis liver
Hereditary hemochromatosis. Hepatocellular iron deposition is blue in this Prussian blue-stained
section of an early stage of the disease, in which parenchymal architecture is normal.
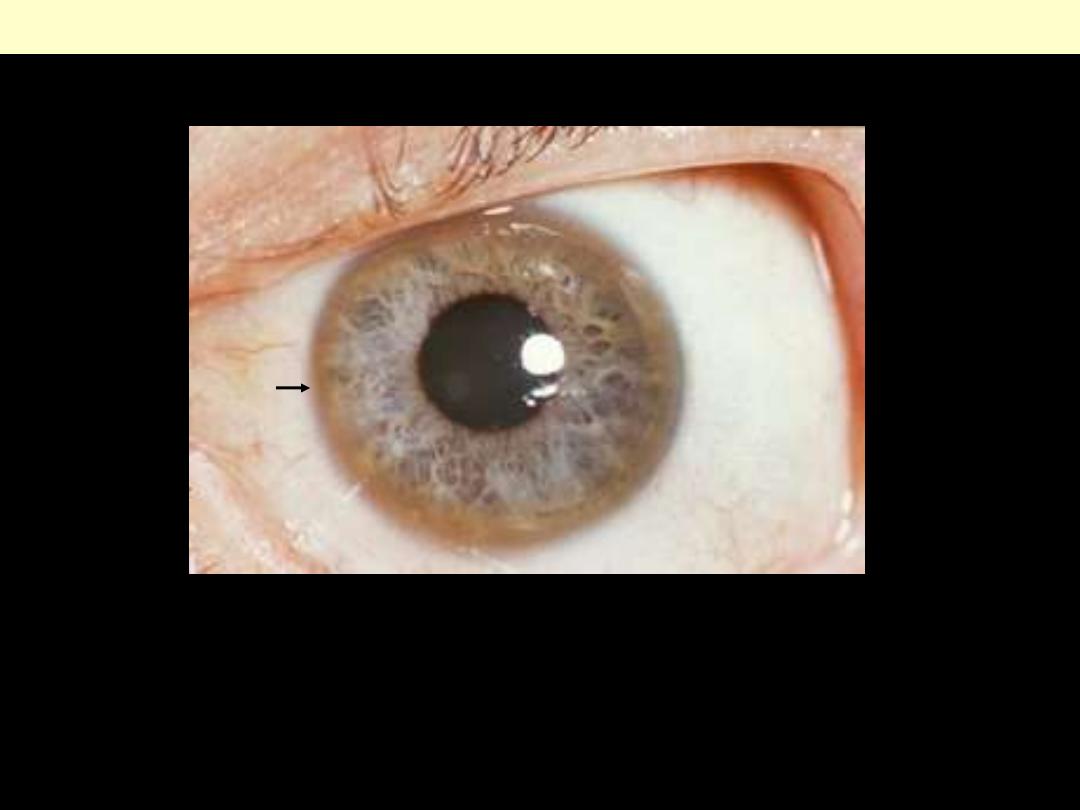
Copper deposition in Descemet’s membrane of the cornea. These rings can be either dark brown,
golden, or reddish-green, are 1 to 3 mm wide, and appear at the corneal limbus. With rare exceptions,
they are diagnostic of inherited hepatolenticular degeneration—Wilson’s disease. This 32-year-old
patient complained of longstanding difficulty speaking. He also had a tremor.
Kayser-Fleischer ring
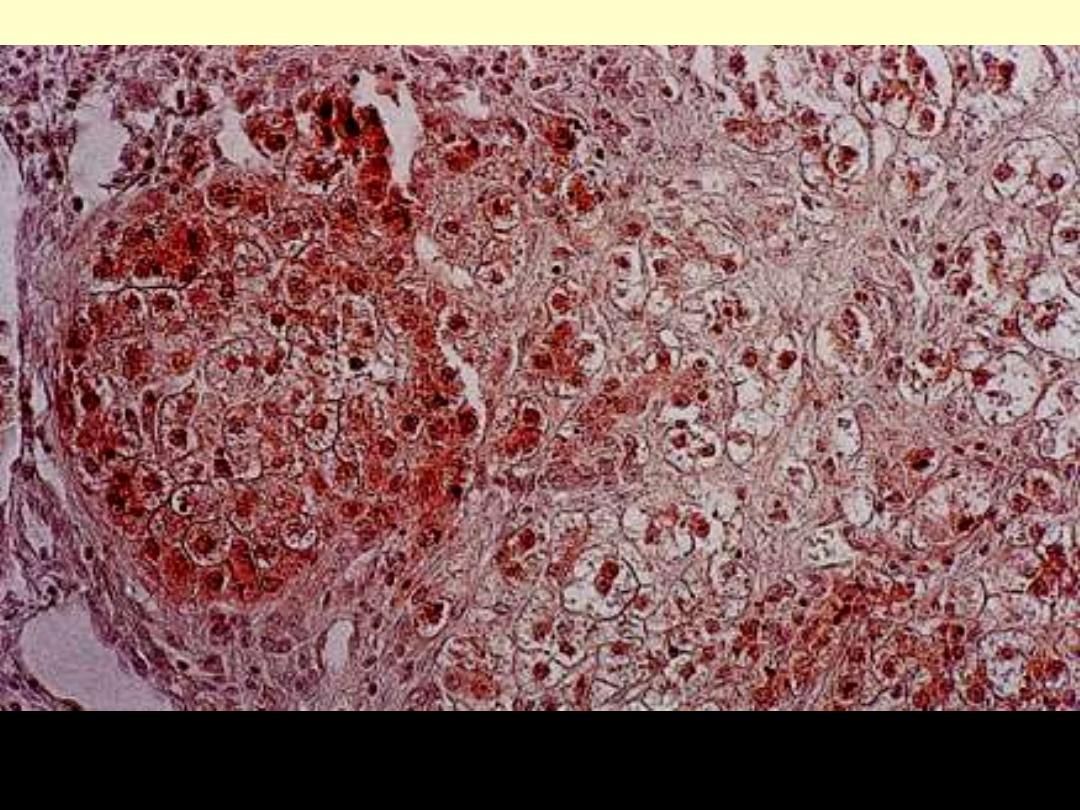
Wilson’s disease rhodanine stain
This is the cirrhotic stage. This reveals accumulation of copper (redgranules) in varying degree, most
pronounced in a nodular cluster of hepatocytes (left). (Rhodanine stain)
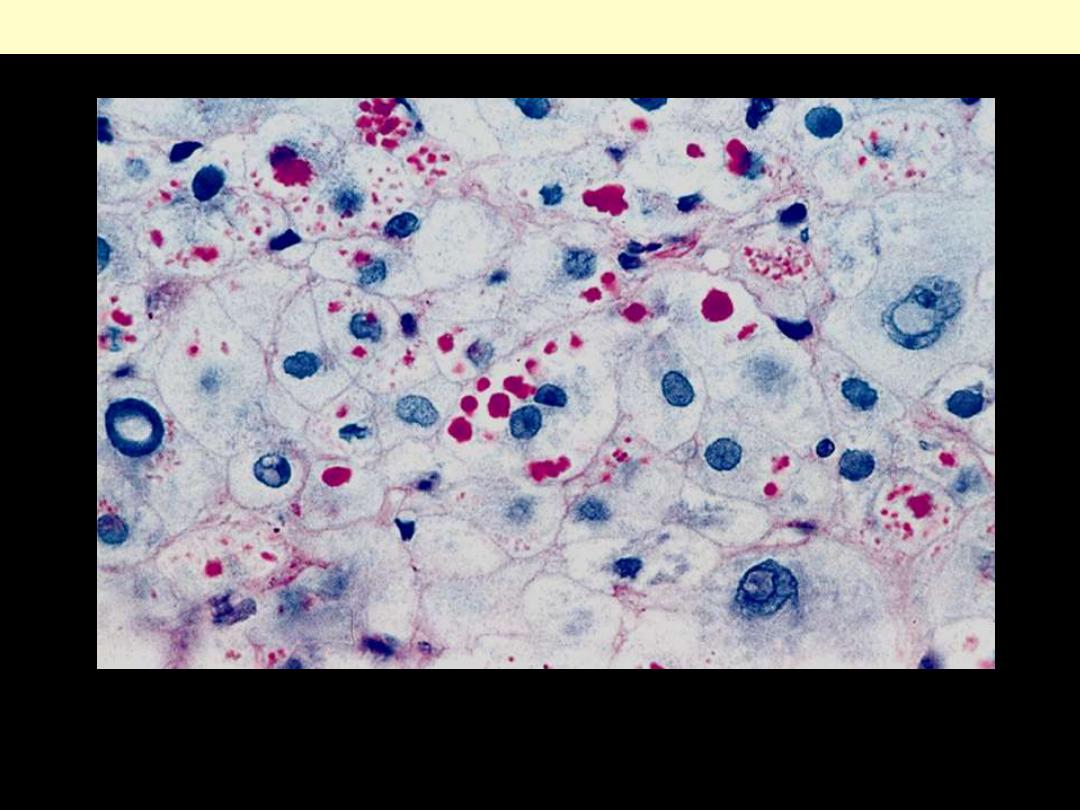
α1-AT deficiency
Periodic acid-Schiff stain of the liver, highlighting the characteristic red cytoplasmic granules
Tumors + nodules
Focal nodular hyperplasia
Gross appearances of focal nodular hyperplasia. The resemblance to cirrhosis is striking.
Typical star-shaped central scar of radial shape in nodular hyperplasia. The lesion has a brownish cast
Focal nodular hyperplasia
Central portion of nodular hyperplasia showing the interphase between the fibrous scar and the
hepatocytic nodules.
Focal nodular hyperplasia
It is larger than surrounding cirrhotic nodules but do not display atypical features.
Large macroregenerative nodule in a cirrhotic liver.
This is a benign hemangioma of the liver just beneath the capsule. Perhaps one person in 50 has such a
neoplasm, which is typically just an incidental finding, since most are 1 cm or less. They can sometimes
be multiple
Cavernous hemangioma liver
variably sized vascular spaces lined by flat endothelial cells and set within a fibrous stroma
Cavernous hemangioma liver
Liver cell adenoma
Resected specimen presenting as a pendulous
mass arising from the liver.
a
Surgically resected specimen showing a discrete
mass underneath the liver capsule
Gross appearance of liver cell adenoma. The tumor, which is well circumscribed, has a large, central
area of recent hemorrhage.
Liver
cell adenoma
Broad cords of liver cells with
prominent blood vessels (arrows)
Liver cell adenoma
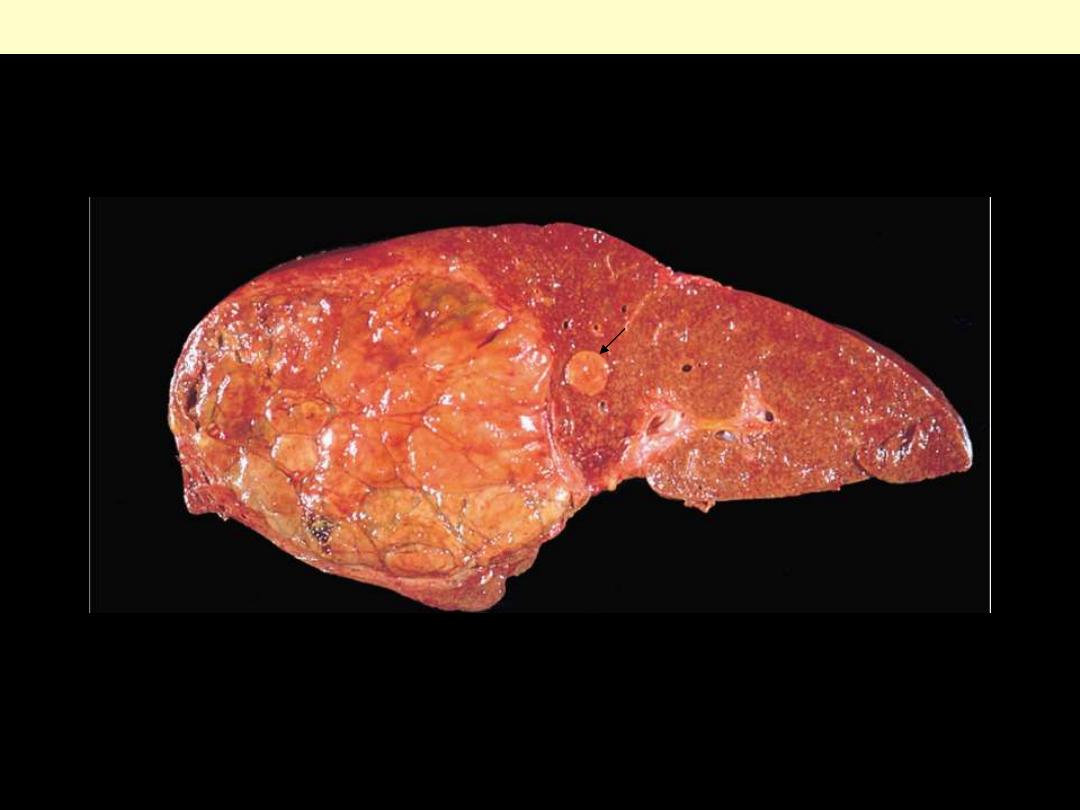
The cancer is unifocal, massive type. A large neoplasm has replaced most of the right hepatic lobe in
this noncirrhotic liver. A satellite nodule of cancer is seen in the vicinity of the main mass (arrow)
Hepatocellular carcinoma
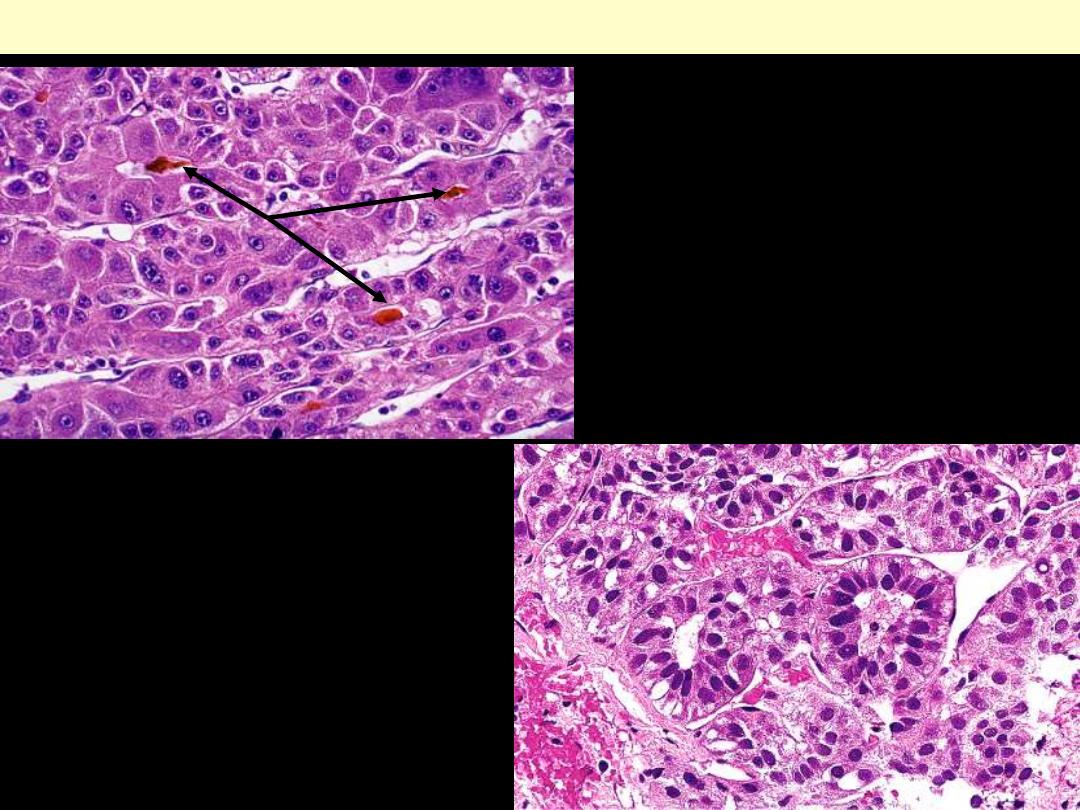
Note the trabecular pattern of growth, nuclear
atypicality, and bile production by tumor cells
(Arrows). The broad trabeculae are separated
by sinusoides
Hepatocellular carcinoma
Tubular formations in hepatocellular
carcinoma (pseudoglandular HCC). These
should not be interpreted as evidence of a
cholangiocarcinomatous component. Note the
separating sinusoids.
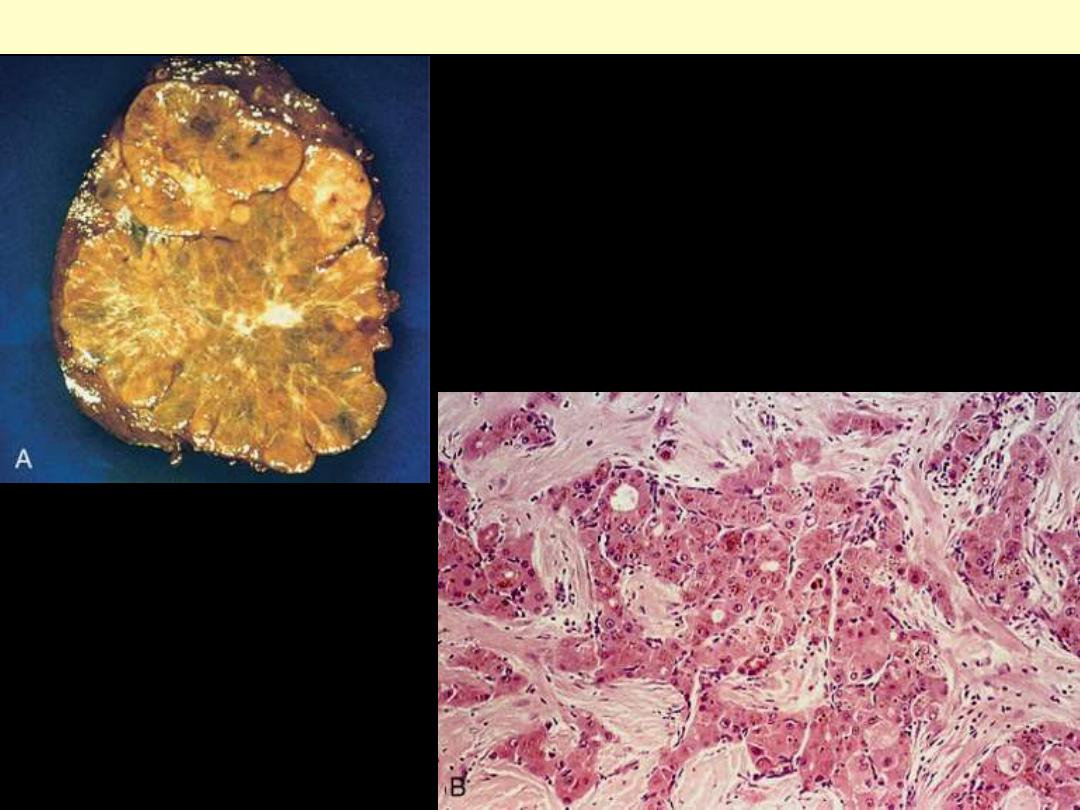
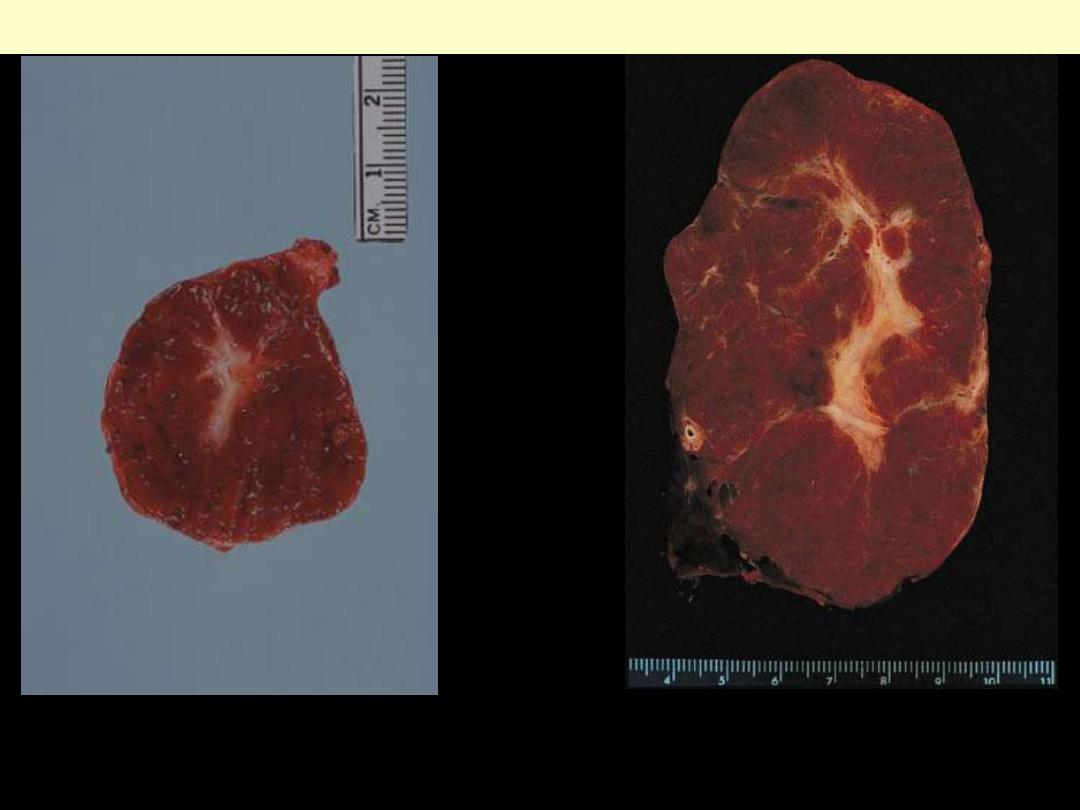
A, Resected specimen with an outer rim of normal liver. B,
Nests and cords of tumor cells separated by dense bundles of
collagen.
Fibrolamellar carcinoma
Hepatic metastases
Multiple hepatic metastases from a primary colon adenocarcinoma.
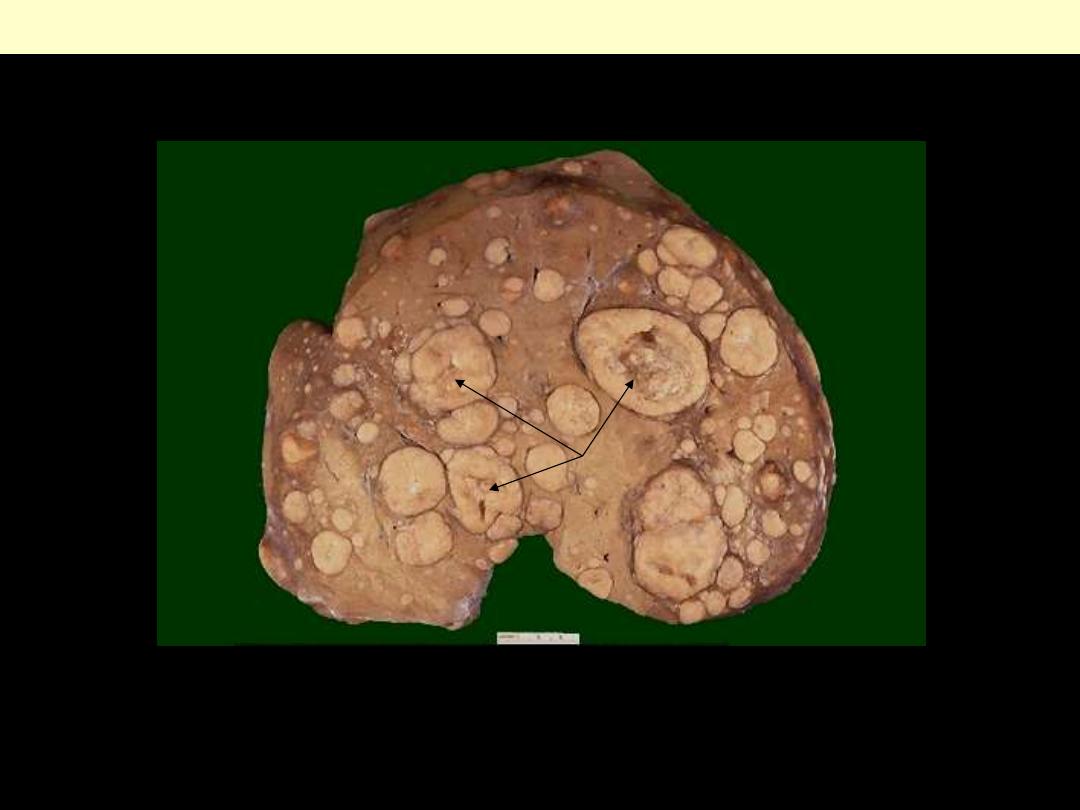
There are numerous variably sized whitish nodules. Some of the larger ones demonstrate central
necrosis (umblication) (arrows). The masses are metastases to the liver.
Metastases to the liver

Liver metastases from an adenocarcinoma primary in the colon, one of the most common primary sites
for metastatic adenocarcinoma in liver.
Liver metastases
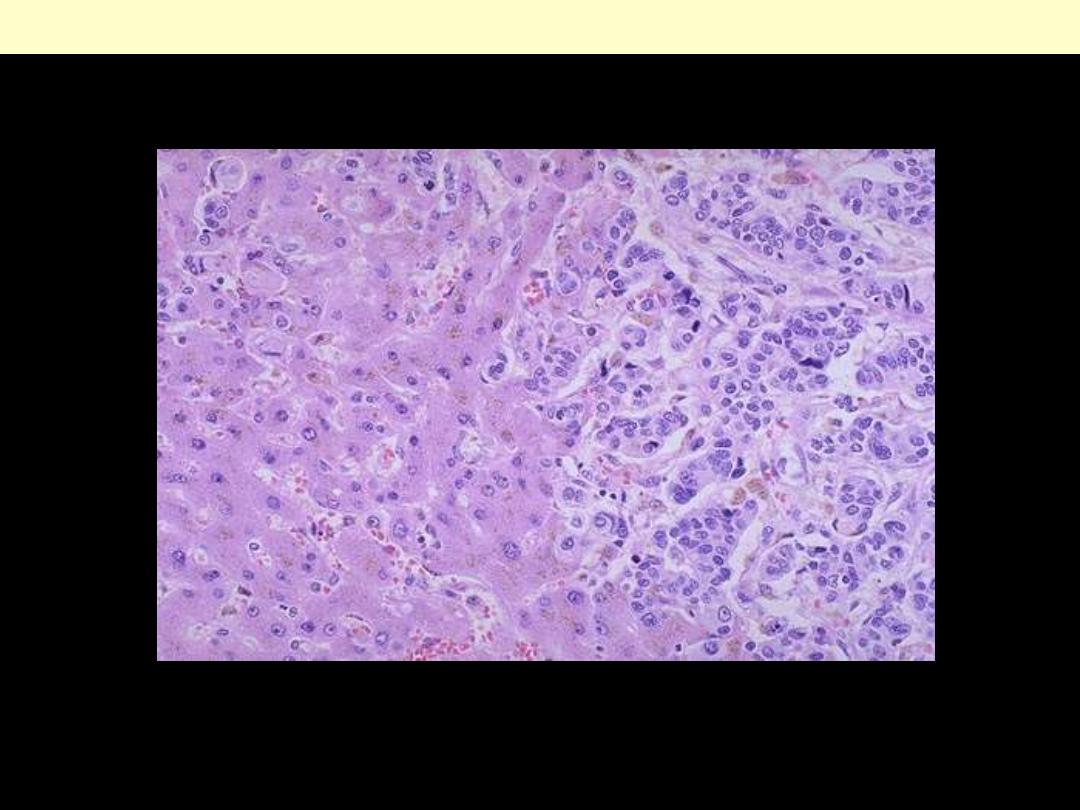
Metastatic infiltrating ductal carcinoma from breast is seen on the right, with normal liver
parenchyma on the left.
Liver metastases
Vascular disorders
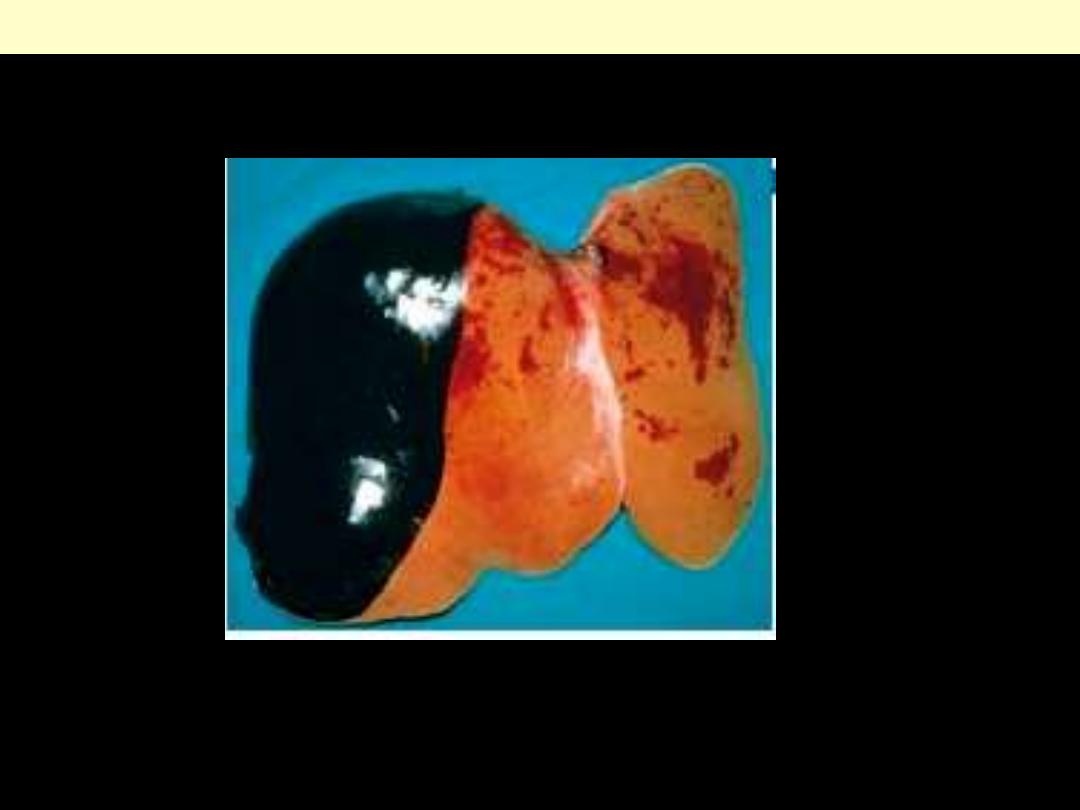
Eclampsia liver
Subcapsular hematoma dissecting under Glisson's capsule in a fatal case of eclampsia.
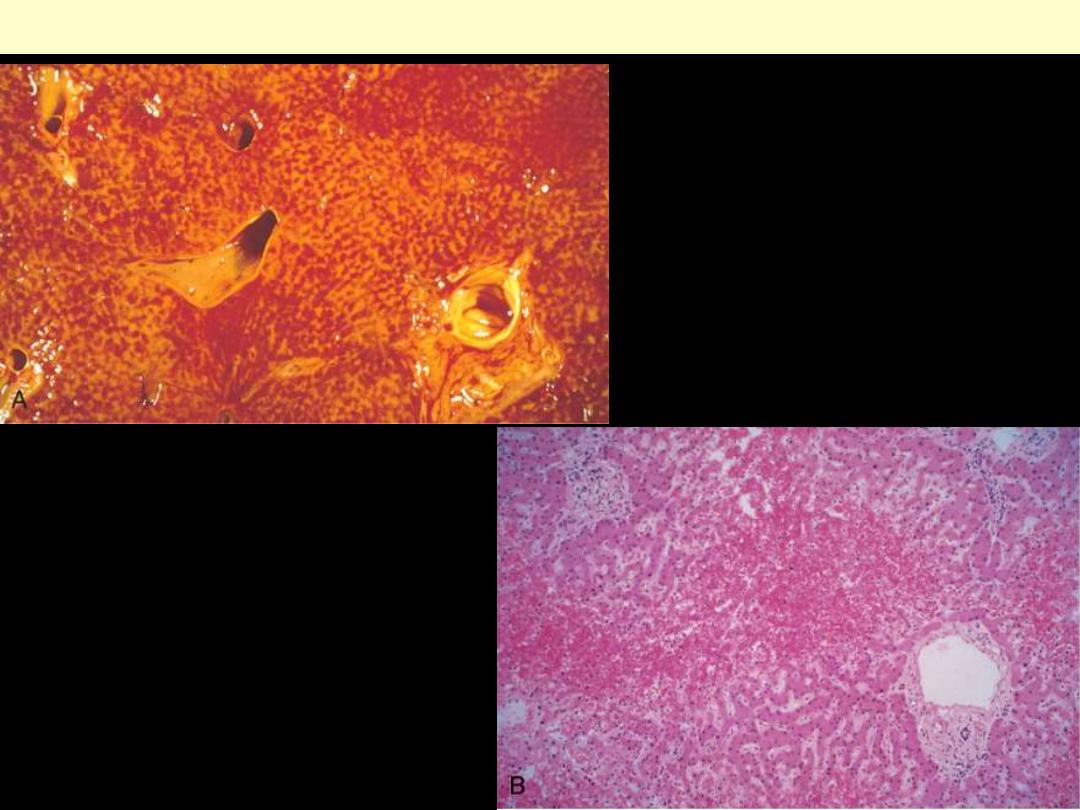
Centrilobular hemorrhagic necrosis liver
A, The cut liver section, in which major
blood vessels are visible, is notable for a
variegated mottled red appearance,
representing hemorrhage in the
centrilobular regions of the parenchyma
(nutmeg liver). B, Microscopically, the
centrilobular region is suffused with red
blood cells, and hepatocytes are not readily
visible. Portal tracts and the periportal
parenchyma are intact.
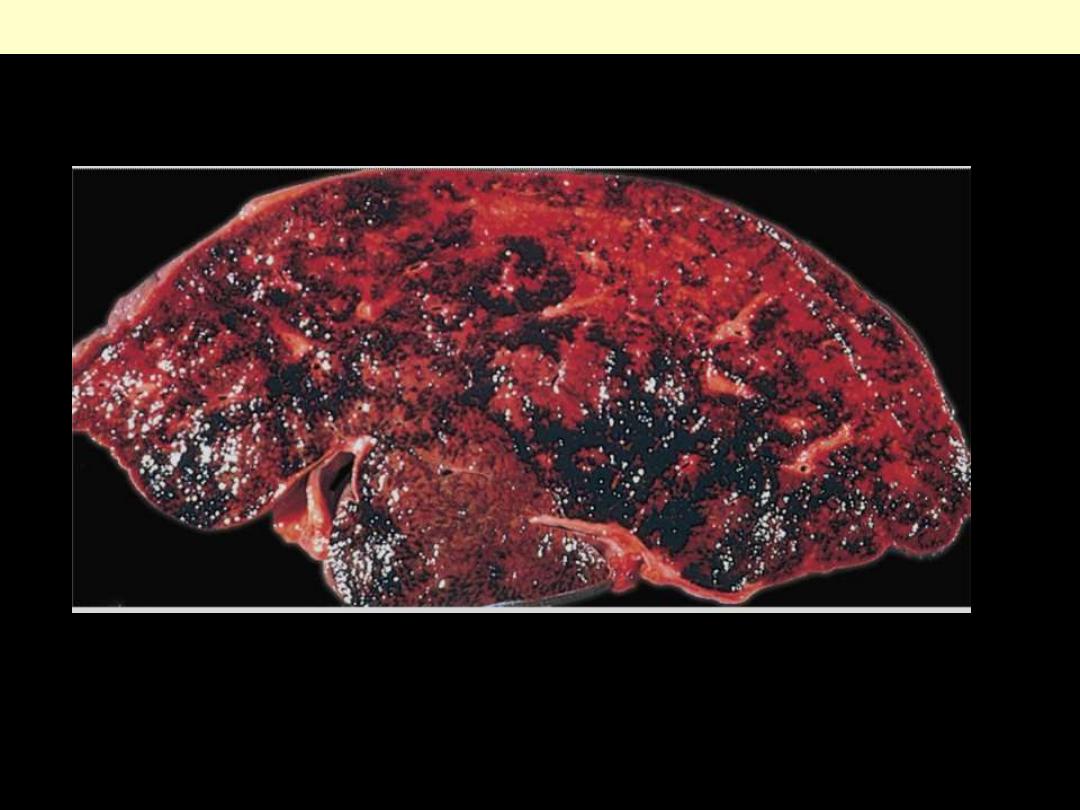
Thrombosis of the major hepatic veins has caused extreme blood retention in the liver.
Budd-Chiari syndrome
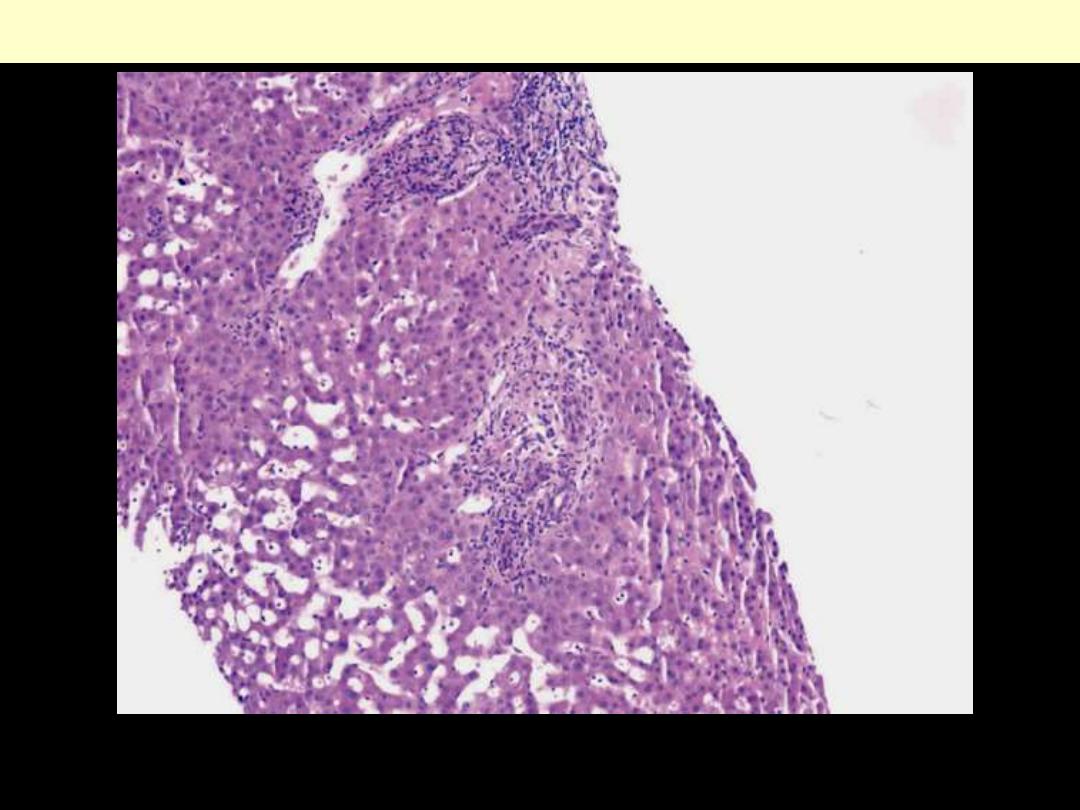
Venous outflow obstruction Budd-Chiari
Sinusoidal dilatation and congestion in zones 2 and 3. Portal tracts show mild bile ductular
proliferation and a mild lymphocytic infiltrate, hematoxylin and eosin, 100.
Pancreas
Pancreatitis – acute + chronic
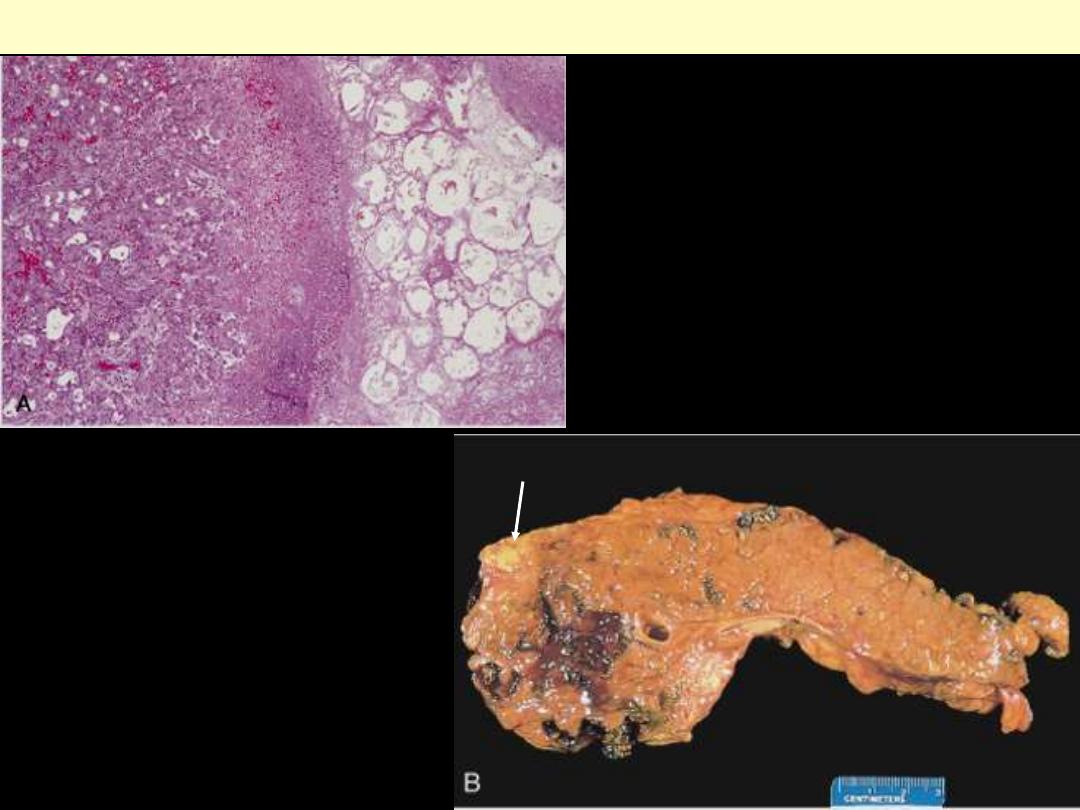
A, The microscopic field shows a region of fat
necrosis (right), and focal pancreatic
parenchymal necrosis (center). B, The pancreas
has been sectioned longitudinally to reveal dark
areas of hemorrhage in the pancreatic
substance and a focal area of pale fat necrosis in
the peripancreatic fat (arrow).
Acute pancreatitis

Yellow-tan foci of fat necrosis are visible throughout the hyperemic pancreas, which has been sectioned
in half. There is some edema, but no hemorrhage in this case of mild acute pancreatitis.
Acute pancreatitis
The fat necrosis consists of fat cells that have lost their nuclei and whose cytoplasm has a granular pink
appearance. Some hemorrhage is seen at the left in this case.
Acute pancreatitis
At high magnification, acute inflammation with necrosis and hemorrhage is seen with residual
pancreatic acini in a case of acute hemorrhagic pancreatitis.
Acute hemorrhagic pancreatitis
This is hardly recognizable as pancreas because a large pancreatic pseudocyst has formed. Seen here at
autopsy is the opened pseudocyst extending from hilum of liver to the right of the photograph. It has an
irregular red to brown to black inner surface.
Pancreatic pseudocyst
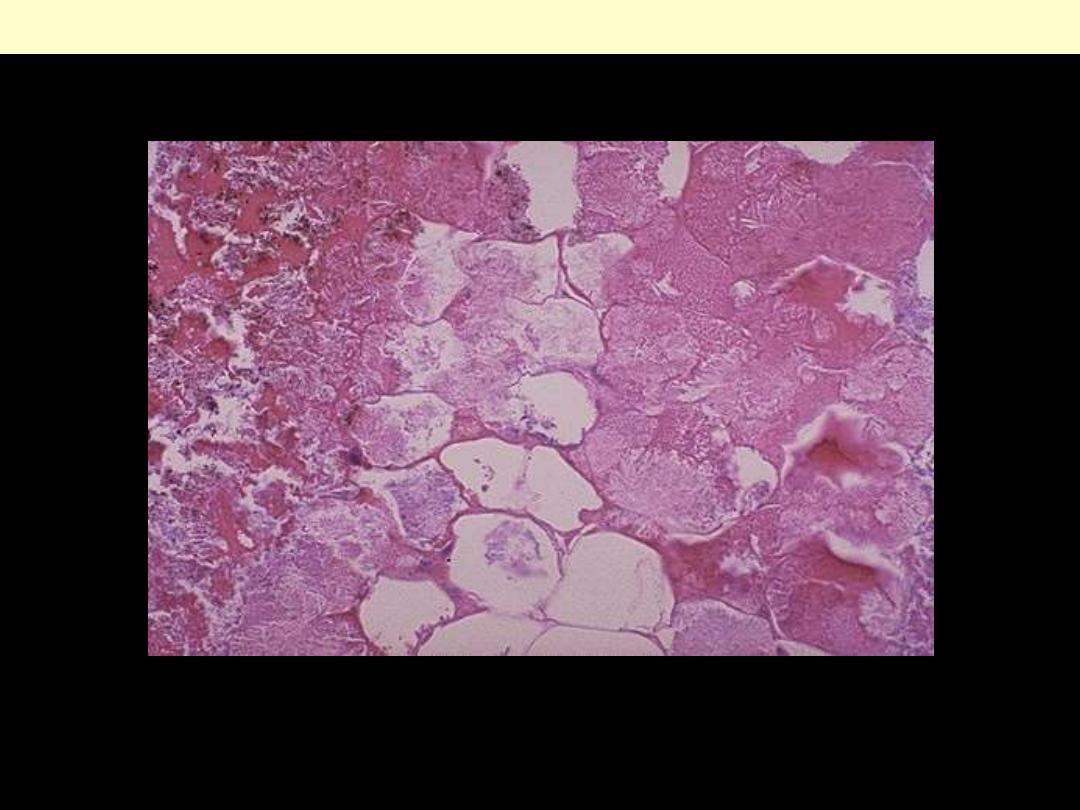
A, Cross-section revealing a poorly defined
cyst with a necrotic wall. B, Histologically
the cyst lacks a true epithelial lining and
instead is lined by fibrin, granulation tissue,
and chronic inflammation.
Pancreatic pseudocyst
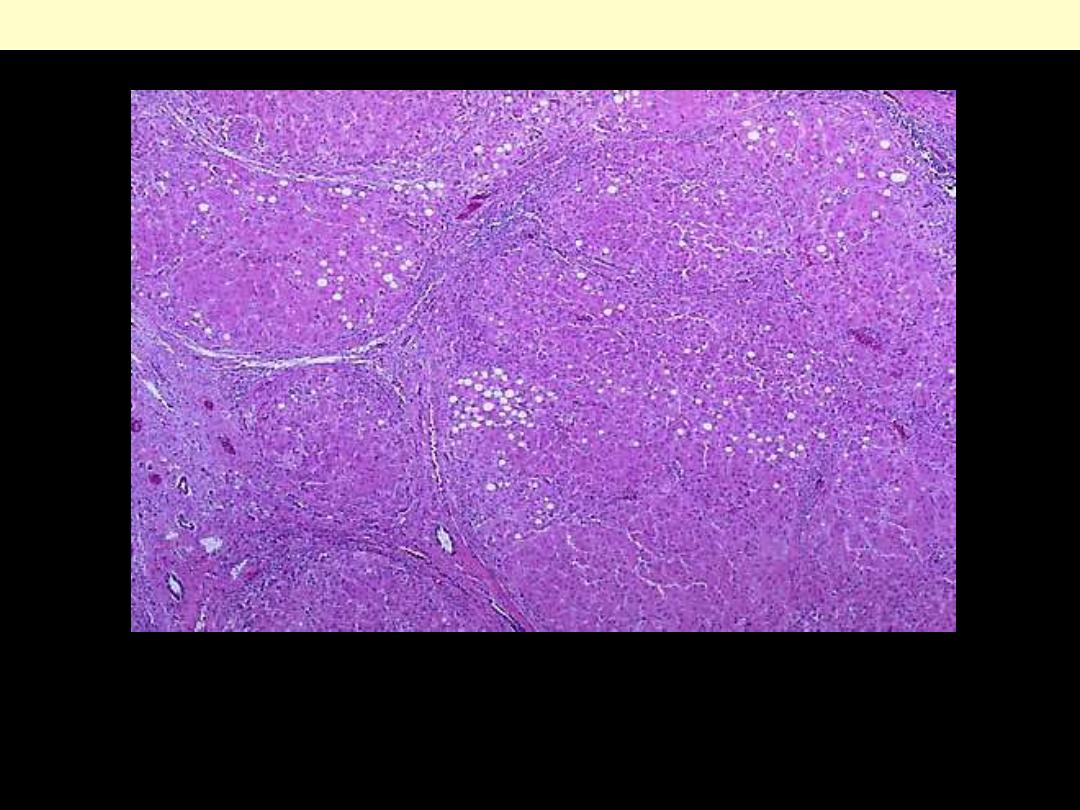
This low power photomicrograph demonstrates scattered chronic inflammatory cells in a collagenous
stroma with a few remaining islets of Langerhans in a case of chronic pancreatitis. Chronic alcoholism
is a common cause for this condition.
Chronic pancreatitis
A, Extensive fibrosis and atrophy has left only
residual islets (left) and ducts (right), with a
sprinkling of chronic inflammatory cells and
acinar tissue. B, A higher power view
demonstrating dilated ducts with inspissated
eosinophilic concretions in a patient with
alcoholic chronic pancreatitis.
Chronic pancreatitis
Tumors
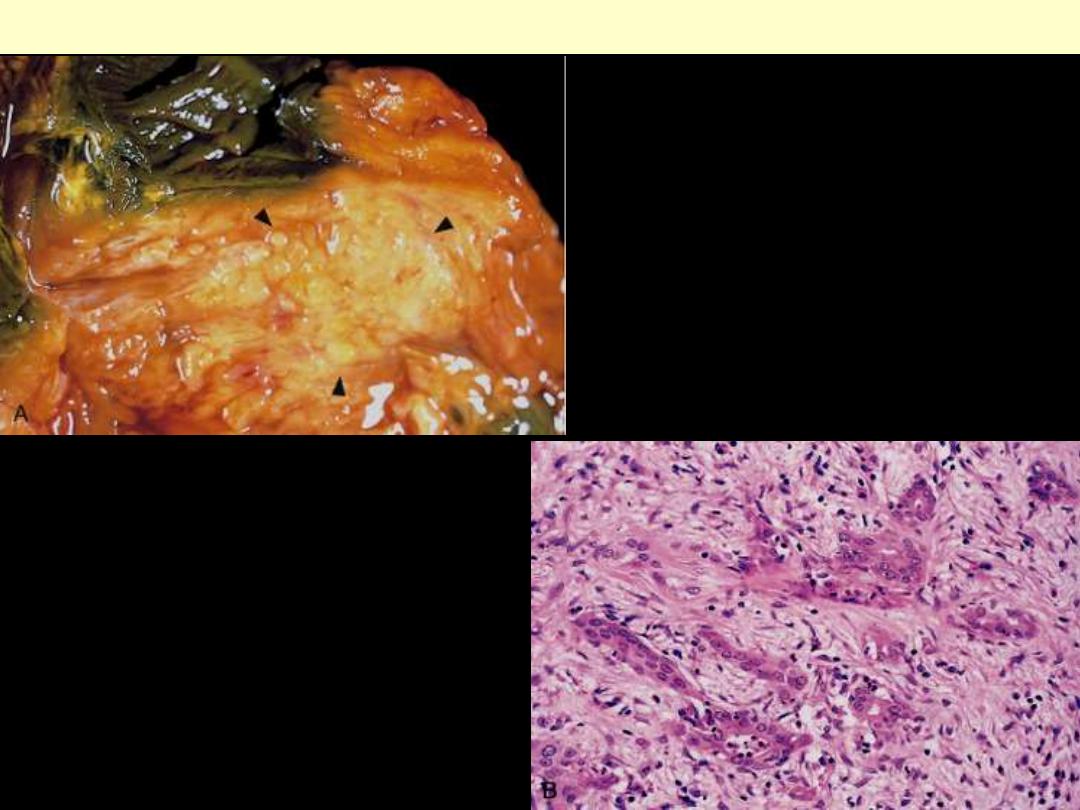
A, A cross-section through the head of the
pancreas and adjacent common bile duct
showing both an ill-defined mass in the
pancreatic substance (arrowheads) and the
green discoloration of the duct resulting from
total obstruction of bile flow. B, Poorly formed
glands are present in a densely fibrotic
(desmoplastic) stroma within the pancreatic
substance.
Carcinoma of the pancreas
