1
4
th
stage
Medicine
Lec-
.د
15/5/2016
LIVER CIRRHOSIS
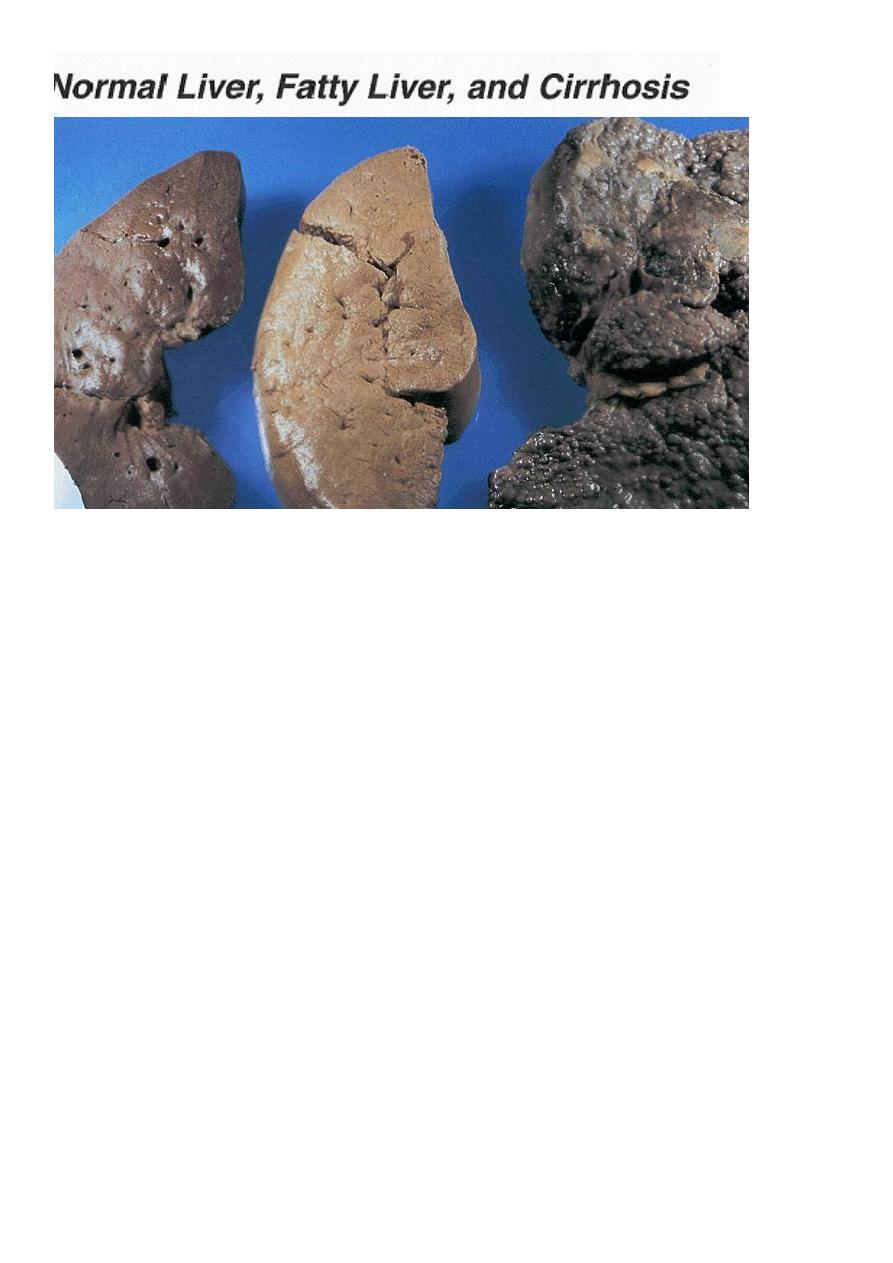
PATHOLOGY OF CIRRHOSIS
1. The changes in cirrhosis usually diffuse and involve the whole liver; except in biliary
cirrhosis they can be patchy .
2. They include progressive and widespread death of liver cells associated with
inflammation and fibrosis, leading to loss of the normal liver architecture.
3. Destruction of the liver architecture
4. development of portosystemic vascular shunts.
5. Formation of nodules rather than lobules due to the proliferation of surviving
hepatocytes.
6. The evolution of cirrhosis is gradual and progressive unless the aetiological agent is
withdrawn: for example, by abstinence from alcohol
.
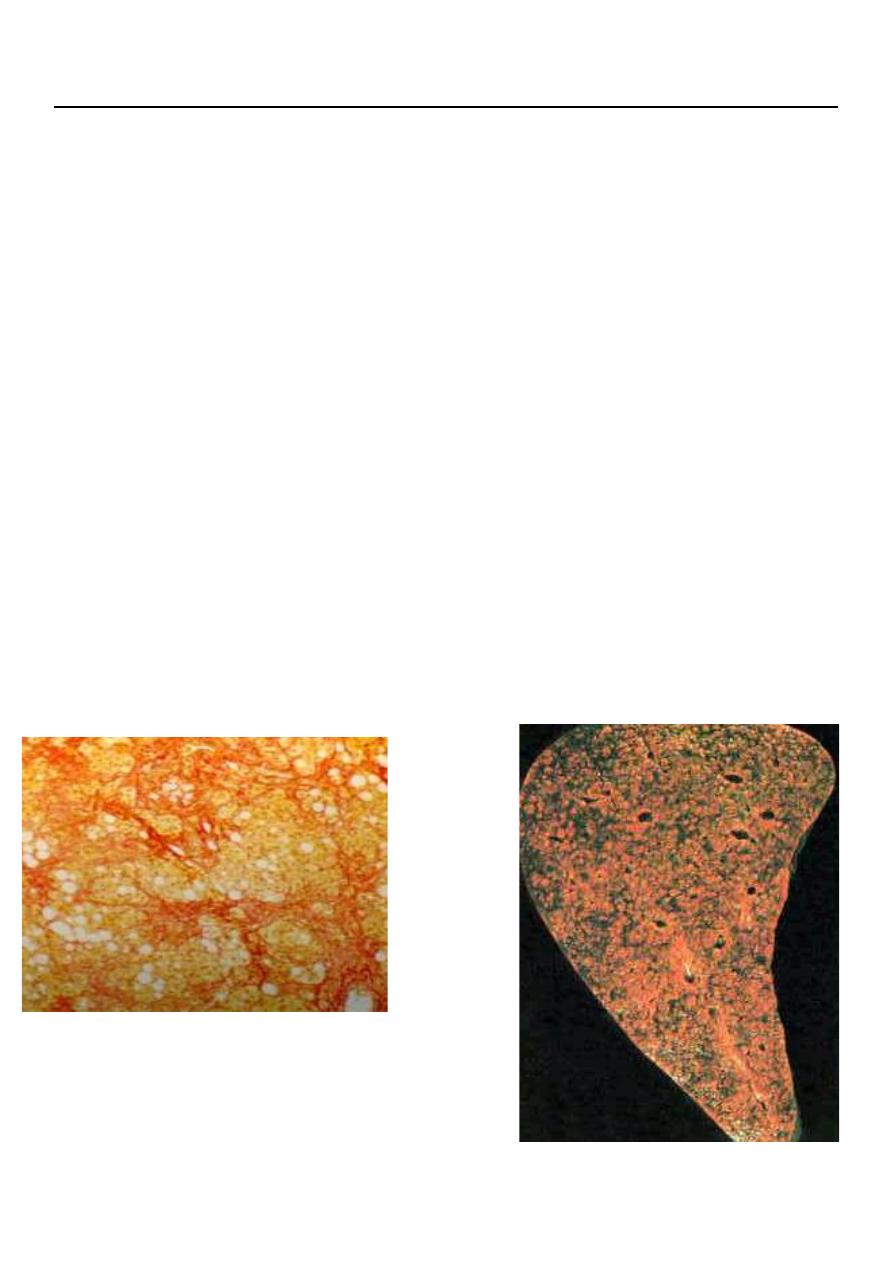
CIRRHOSIS - HISTOPATHOLOGY
AUTOPSY SECTION OF LIVER
2
Cirrhosis can be classified histologically into two types.
1. Micronodular cirrhosis: is characterised by small nodules about 1 mm in diameter and is
seen in alcoholic cirrhosis.
2. Macronodular cirrhosis: is characterised by larger nodules of various sizes. Areas of
previous collapse of the liver architecture are evidenced by large fibrous scars.
CAUSES OF CIRRHOSIS
1. Alcohol
2. Chronic viral hepatitis (B or C)
3. Non-alcoholic fatty liver disease
4. Immune
Primary sclerosing cholangitis
Autoimmune liver disease
5. Biliary
Primary biliary cirrhosis
Cystic fibrosis

3
6. Genetic
– Haemochromatosis
– α1-antitrypsin deficiency
– Wilson's disease
7. Cryptogenic (unknown
CLINICAL FEATURES OF LIVER CIRRHOSIS
SYMPTOMS:
1. Cirrhosis may be entirely asymptomatic in life and may be found incidentally at surgery
or may be associated with minimal features.
2. Frequent complaints include weakness, fatigue, muscle cramps, weight loss and non-
specific digestive symptoms such as anorexia, nausea, vomiting and upper abdominal
discomfort. irregular menses in female and Loss of libido and hair loss in male and female.
3. Other features are due mainly to hepatic insufficiency and portal hypertension.
PHYSICAL EXAMINATION
Hepatomegaly (although liver may also be small), Jaundice, Ascites, Circulatory changes
(Spider telangiectasia, palmar erythema, cyanosis) and Endocrine changes
(like,gynaecomastia, testicular atrophy, impotence in male, breast atrophy in women and
hair loss in both).
PALMER ERYTHEMA

4
LIVER EXAMINATION IN CIRRHOSIS:
Hepatomegaly is common in
A. Alcoholic liver disease .
B. haemochromatosis.
Progressive hepatocyte destruction and fibrosis gradually reduce liver size as the disease
progresses in other causes of cirrhosis. A reduction in liver size is especially common in:
A.viral hepatitis
B. autoimmune liver disease.
The liver is often hard, irregular and painless.
JAUNDICE IN CIRRHOSIS:
1. Jaundice is usually mild.
2. It is due primarily to a failure to excrete bilirubin.
3. Mild haemolysis may occur due to hypersplenism but is not a major contributor to the
jaundice.
Palmar erythema
can be seen early in the disease but is of limited diagnostic value as it occurs in many other
conditions associated with a hyperdynamic circulation including normal pregnancy, as well
as being found in some normal people
Spider telangiectasia
are due to associated arteriolar changes and consist of: a central arteriole (which
occasionally raises the skin surface) from which small vessels radiate.
Size: from 1-2 mm to 1-2 cm in diameter.
Usually they are found only above the nipples, and can occur early in the disease.
_ One or two small spider telangiectasia are found in about 2% of healthy people and can
occur transiently in greater numbers in the third trimester of pregnancy, but otherwise they
are a strong indicator of liver disease.
Florid spider telangiectasia, gynaecomastia and parotid enlargement
are most
common in alcoholic cirrhosis.
5
Pigmentation is most striking in haemochromatosis and in any cirrhosis associated with
prolonged cholestasis. Pulmonary arteriovenous shunts also develop, leading to
hypoxaemia and eventually to central cyanosis, but this is a late feature
Endocrine changes:
are noticed more readily in men, who show loss of male hair
distribution and testicular atrophy. Gynaecomastia is common and can be due to drugs
such as spironolactone.
Easy bruising:
becomes more frequent as cirrhosis advances.
Epistaxis:
is common and sometimes severe; it can mimic upper gastrointestinal bleeding
if the blood is swallowed.
Splenomegaly:
and collateral vessel formation are features of portal hypertension, which
occurs in more advanced disease .
Ascites
is due to a combination of liver failure and portal hypertension and signifies
advanced disease.
Evidence of
hepatic encephalopathy
also becomes increasingly common with advancing
disease.
Non-specific features of chronic liver disease include
clubbing of the fingers
and toes.
Dupuytren's contracture
is traditionally regarded as being associated with cirrhosis,
especially that due to alcohol, but the evidence for this association is weak.

6
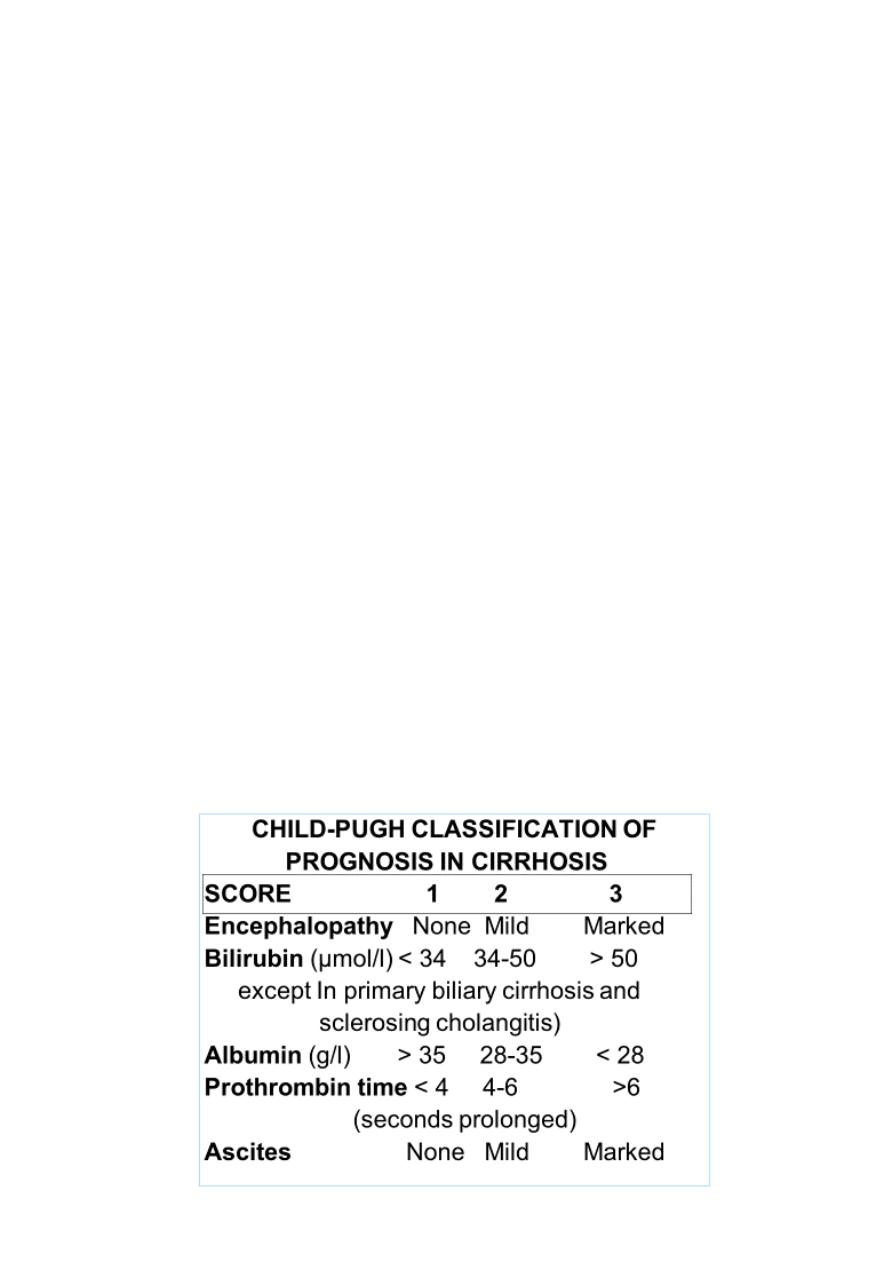
Add the individual scores:
< 7 = Child's A
7-9 = Child's B
> 9 = Child's C
PROGNOSIS IN LIVER CIRRHOSIS
The overall prognosis in cirrhosis is poor. 25% of patients survive 5 years from diagnosis
If liver function is good, 50% survive for 5 years and 25% for up to 10 years.
The prognosis is more favourable when the underlying cause of the cirrhosis can be
corrected, as in alcohol misuse, haemochromatosis and Wilson's disease.
The followings indicate a poor prognosis in cirrhosis
1. jaundice, ascites or encephalopathy,
2. Increasing plasma bilirubin.
3. falling plasma albumin or an albumin concentration < 30 g/l.
4. marked hyponatraemia (< 120 mmol/l, not due to diuretic therapy)
5. prolonged prothrombin time.
6. Poor renal function.
the Child’s Pugh and more recently, MELD
(Model for End-stage Liver Disease) scores can be used to assess prognosis.
Complications Of Chronic Liver Disease
1. Due to portal hypertension:
a. Splenomegaly and hypersplenism.
b. Ascites and spontanous bacterial
peritonitis.
c. Esophageal and fundal varices.
d. hepatic encephalopathy (porto- systemic shunt)
2. Due to impaired liver function:
a. hepatic encephalopathy.
b. coagulopathy and platelet
dysfunction

7
