Prostatic Carcinoma
مكتب الجامعة للطباعة والاستنساخعدد : السعر:
مكتب الجامعة للطباعة والاستنساخ
عدد : السعر:
Carcinoma of the prostate {CAP}
One of the most common malignant tumor affecting males over the age of 65 years.The second leading cause of cancer death in men
Usually found in the peripheral zone of the prostate
Risk factors:
Family history: risk is higher if one or more first degree relative has the disease.The gene responsible for familial CAP resides on chromosome 1
Diet: dietary fat.
Race: African Americans have the highest incidence of the disease.
Age: incidence increase constantly over 50.
Cadmium : found in cigarette smoke, alkaline batteries, and in the welding industry.
Pathology
95% adenocarcinoma derived from acinar epithelium
5% include Transitional Cell Carcinoma (TCC) or sarcoma.
Grading: Gleason’s grade based on the degree of glandular differentiation and growth pattern
70%-75% of CAP arise from peripheral zone.
20% at the transition zone
5% at the central zone
Presentation
Accidental (DRE, PSA, TURP & Histopathology)Irritative & Obstructive symptoms.
Hematuria
Metastatic symptoms: bone pain, back ache, pelvic pain, lymph edema, dyspnoea, weight loss, or pathological fractures..
Cord compression: paraplegia, paresthesias and weakness of the lower extremities and urinary or fecal incontinence.
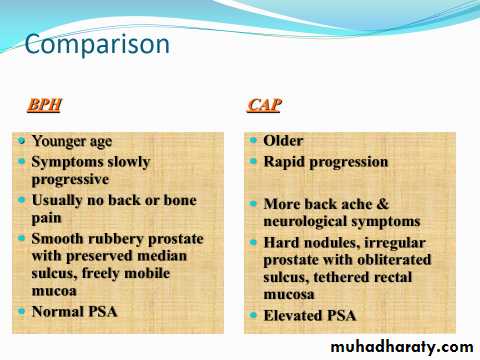
Rectal examination (DRE):
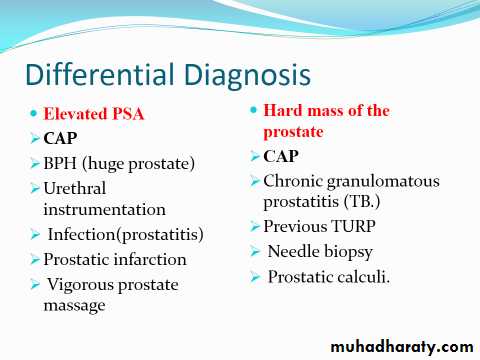
Stony hard irregular prostatic noduleIrregular surface
Obliterated median sulcus
Tethered mucosa (difficulty in moving the rectal mucosa over the prostate).
N.B.: -Normal DRE does not exclude CAP.
- There is no tenderness on DRE in BPH & CAP
Spread
Direct invasion: seminal vesicle, bladder neck & trigone,
ureteric obstruction in 15—30% .
Rectal involvement is rare, Denonvvilliar’s fascia act as barrier.
The external urinary sphincter
All indicates aggressive course
Lymphatic: obturator , internal, external & common iliac , hypogastric, mediastinal nodes and occasionally the supraclavicular nodes.
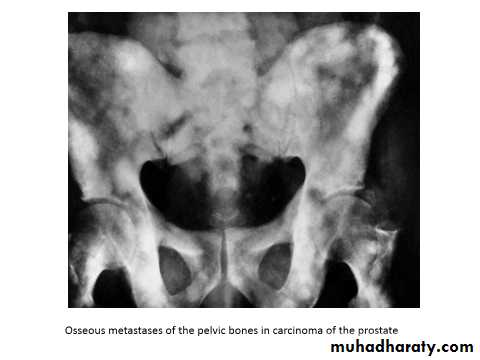
Blood: to the lower lumber vertebrae & pelvic bones due to reverse blood flow from vesicoprostatic plexus to the emissary veins of the bones (OSTEOBLASTIC changes)
Osteogenic : sclerotic in 65%, Osteolytic in 35%
Spread to lung, liver, adrenal
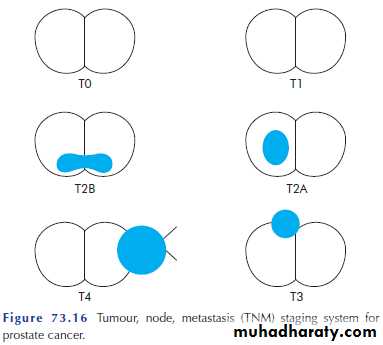
TNM Staging System for Prostate Cancer
T—Primary tumorTx Cannot be assessed
T0 No evidence of primary tumor
Tis Carcinoma in situ (PIN)
T1a 5% of tissue in resection for benign disease has cancer, normal DRE
T1b > 5% of tissue in resection for benign disease has cancer, normal DRE
T1c Detected from elevated PSA alone, normal DRE and TRUS (Trans Rectal Ultrasound).
T2a Tumor palpable by DRE or visible by TRUS on one side only, confined to prostate
T2b Tumor palpable by DRE or visible by TRUS on both sides, confined to prostate
T3a Extracapsular extension on one or both sides
T3b Seminal vesicle involvement
T4 Tumor directly extends into bladder neck, sphincter, rectum, levator muscles, or into pelvic sidewall
N—Regional lymph nodes (obturator, internal iliac, external iliac, presacral lymph nodes)
Nx Cannot be assessed
N0 No regional lymph node metastasis
N1 Metastasis in a regional lymph node or nodes
M—Distant metastasis
Mx Cannot be assessed
M0 No distant metastasis
M1a Distant metastasis in non regional lymph nodes
M1b Distant metastasis to bone
M1c Distant metastasis to other sites
Investigations
LABORATORYPSA (Prostatic Specific Antigen): prostatic tumor marker for diagnosis and follow up.
It may also increase in prostatitis, BPH, after DRE, urethral instrumentation or catheterization.
Up to 4 ng/ml is normal
PSA > 10 ng/mL is suggestive of CAP
PSA > 35 ng/mL is almost diagnostic of advanced CAP
GUE
FRT: Azotemia can result from bilateral ureteral obstruction
Hb: Anemia may be present in metastatic disease
Acid phosphatase: elevated with disease outside the confines of the prostate.
Alkaline phosphatase: elevated in bone metastasis.
Radiological investigations
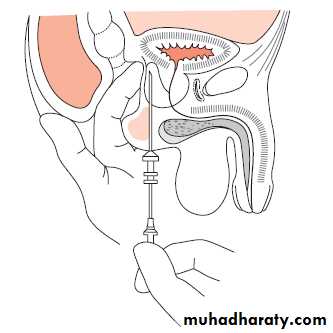
TRUS & biopsy (TRUS guided biopsy): 6 to 12 trucut biopsy.Endorectal MRI
Plain X ray: osteoblastic lesion.
Bone scan: hot areas (active).
CT scan.
MRI
CAP Diagnosis
Current detection strategies include the combination or triad of:
DRE
serum PSA
TRUS guided biopsy.
Treatment
Treatment options for prostate cancer depend on stage of disease, life expectancy of the patient and patient preference.Localised cancer can be treated by:
Radical prostatectomy
Radiation therapy
Cryosurgery
Active monitoring
Treatment of advanced disease is palliative, and hormone ablation remains the first-line therapy by complete androgen blockage.
Watchful waiting: elderly and have very small, well-differentiated cancers
Radical prostatectomy:
Enblock surgical removal of the entire prostate, seminal vesicles and pelvic lymph nodes. The bladder anastomosed to the urethra.
Indicated for early disease (T1 -T2)and healthy fit patient with a life expectancy of > 10 years..
(non metastatic, low stage , low grade)
Radiotherapy For the prostate & LN -External beam radiotherapy -Brachytherapy Interstitial implant of radioactive seeds that are permanently implanted into the prostate. N.B.: palliative DXT Effective for skeletal metastasis
Indication:
1- Locally advanced disease in combination with hormonal therapy.2- Unfit patient for surgery.
3-Symptomatic metastases to relieve pain.
Channeling TURP
To relieve bladder outlet obstruction for patients unfit for major surgery.Hormonal therapy
CAP is hormonal dependant (androgen), and about one third of tumors are hormone-sensitive.Methods of androgen ablation
Surgical : Castration (Bilateral orchiectomy)
Medical : - LHRH agonist: leoprolide, goserlin
- Anti androgen: cyproterone acetate, flutamide, Nilutemide, Stilbesterol.
Chemotherapy poor results
Taxine group