PLAIN ABDOMINAL RADIOGRAPH
Dr. Abdullateef AlbayatiRole of plain abdominal x-ray
1. baseline for surgical preparation2. for detection of air under the diaphragm
3. for patients with acute abdomen
4. for patients with chest conditions that may present with abdominal complaint
1
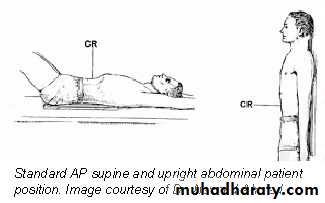
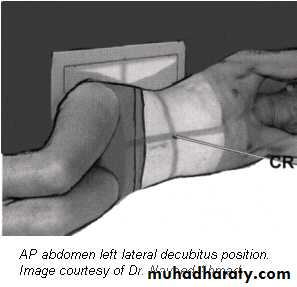
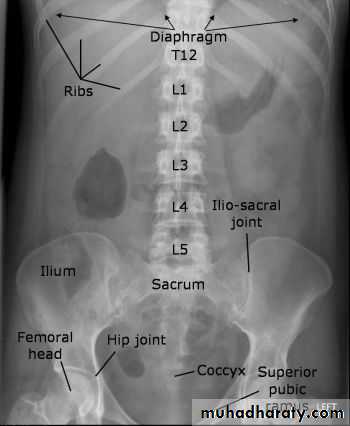
POSITIONING
• Supine AP• Erect AP
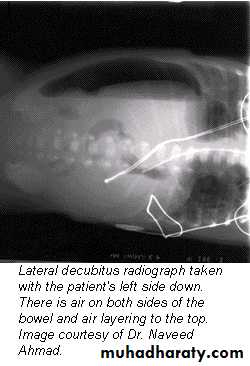
• Lateral decubitus
The main purpose of horizontal beam films is to detect air-fluid levels and free intraperitoneal air
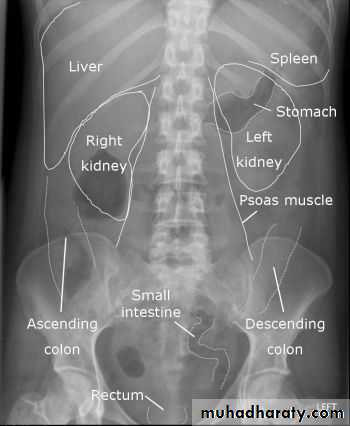
How to look at a plain abdominal film :
• Analyze the intestinal gas pattern and identify any dilated portion of the gastrointestinal tract
• Look for gas outside the lumen of the bowel
• Look for ascites and soft tissue masses in the abdomen and pelvis
• If there are any calcifications, try to locate exactly where they lie
• Assess the size of the liver and spleen
2
Intestinal gas pattern
Relatively large amounts of gas are usually present in the stomach and colon in a normal patient.The stomach can be readily identified by it's location, gastric rugae in the supine view , and by the air fluid level beneath the left hemidiaphragm in the erect view
The duodenum often contains air and show a fluid level
Short fluid levels in the small and large bowel are normal.
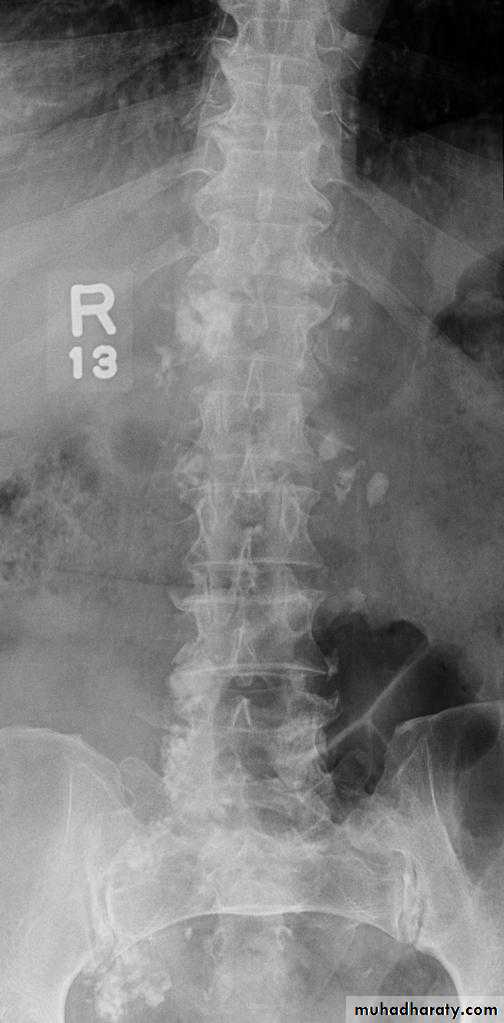
Dilatation of the bowel
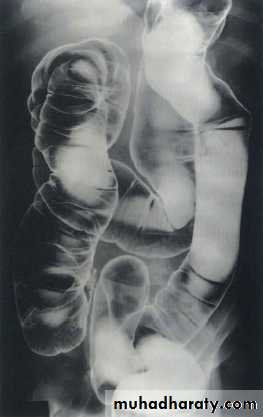
Dilatation of the bowel is the cardinal plain film sign of intestinal obstruction
If the bowel is dilated it is important to try and decide which portion is involved
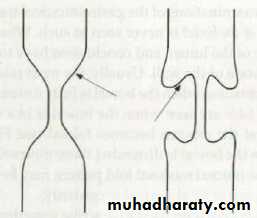
The valvulae conniventes (seen in proximal and mid small bowel) are always closer together than the colonic haustra and cross the width of the bowel , often giving "stack of coins" appearance
The colonic haustra ,which usually form incomplete bands across the colonic gas shadows, are always present in the ascending and transverse colon, but may be absent distal to the splenic flexure
3
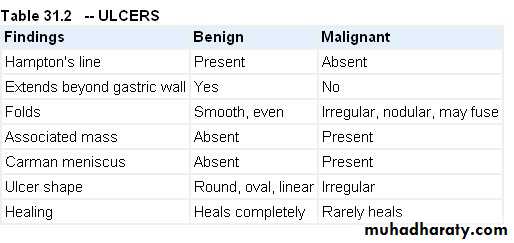
Small bowel obstruction
Large bowel obstruction
Valvulae conniventes
Present
Absent
Number of loops
Many
Few
Distribution of loops
Central
Peripheral
Haustra
Absent
Present
Diameter
3 – 5 cm
More than 5 cm
Radius of curvature
Small
Large
Fecal material
Absent
Present
4
Causes of bowel dilatation
• Mechanical SB obstruction : small bowel dilation with normal or reduced caliber of colon• Mechanical LB obstruction: dilated colon down to the point of obstruction. May be accompanied by small bowel dilation if the ileocecal valve becomes incompetent
• Generalized paralytic ileus: SB and LB dilatation, gas may be present in the rectum
• Localized peritonitis: dilatation of loops adjacent to inflammatory process (sentinel loops)
• SB infarction : mimic obstruction of SB or LB depending on distribution of ischemia
• Closed loop obstruction : e.g. cecal and sigmoid volvulus
• Toxic dilatation of the colon: the dilatation is maximal in transverse colon more than 6 cm The haustra are lost or grossly abnormal . Ulcerative colitis is the commonest cause
5
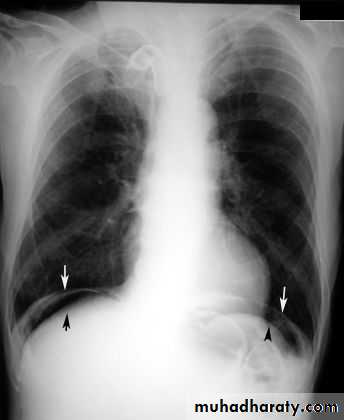
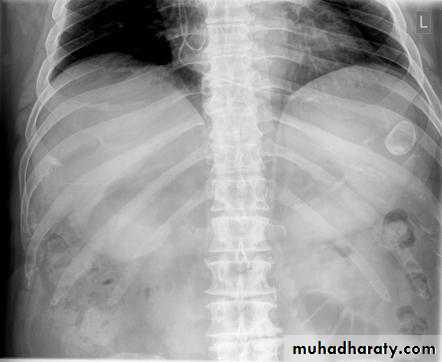
Pneumoperitoneum
Defined as free gas in the peritoneal cavityThe commonest cause is perforated peptic ulcer and two-thirds of such cases are recognizable radiologically
Free intraperitoneal air is a normal finding after a laparotomy or laparoscopy.
In adults, the air is usually absorbed within 7 days .
In children, the air absorbs much faster ,usually within 24 hours.
An increase in the amount of air on successive films indicates continuing leakage of air.
Pneumoperitoneum under the right hemidiaphragm is usually easy to recognize, but free gas under the left hemidiaphragm is difficult to recognize because of the overlapping gas shadows of the stomach and splenic flexure.
Gas under the diaphragm is much easier to diagnose on an erect chest film than on an upright abdominal film
6
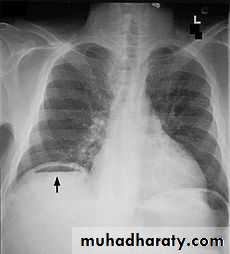
Gas in an abscess
It may form either small bubbles or larger collections of air , both of which could be confused with gas within the bowel.Fluid levels in abscesses may be seen on a horizontal x-ray film.
Subphrenic abscess cause elevation of the diaphragm, pleural effusion and pulmonary collapse/consolidation
Ultrasound and CT are extensively used to evaluate abdominal abscesses
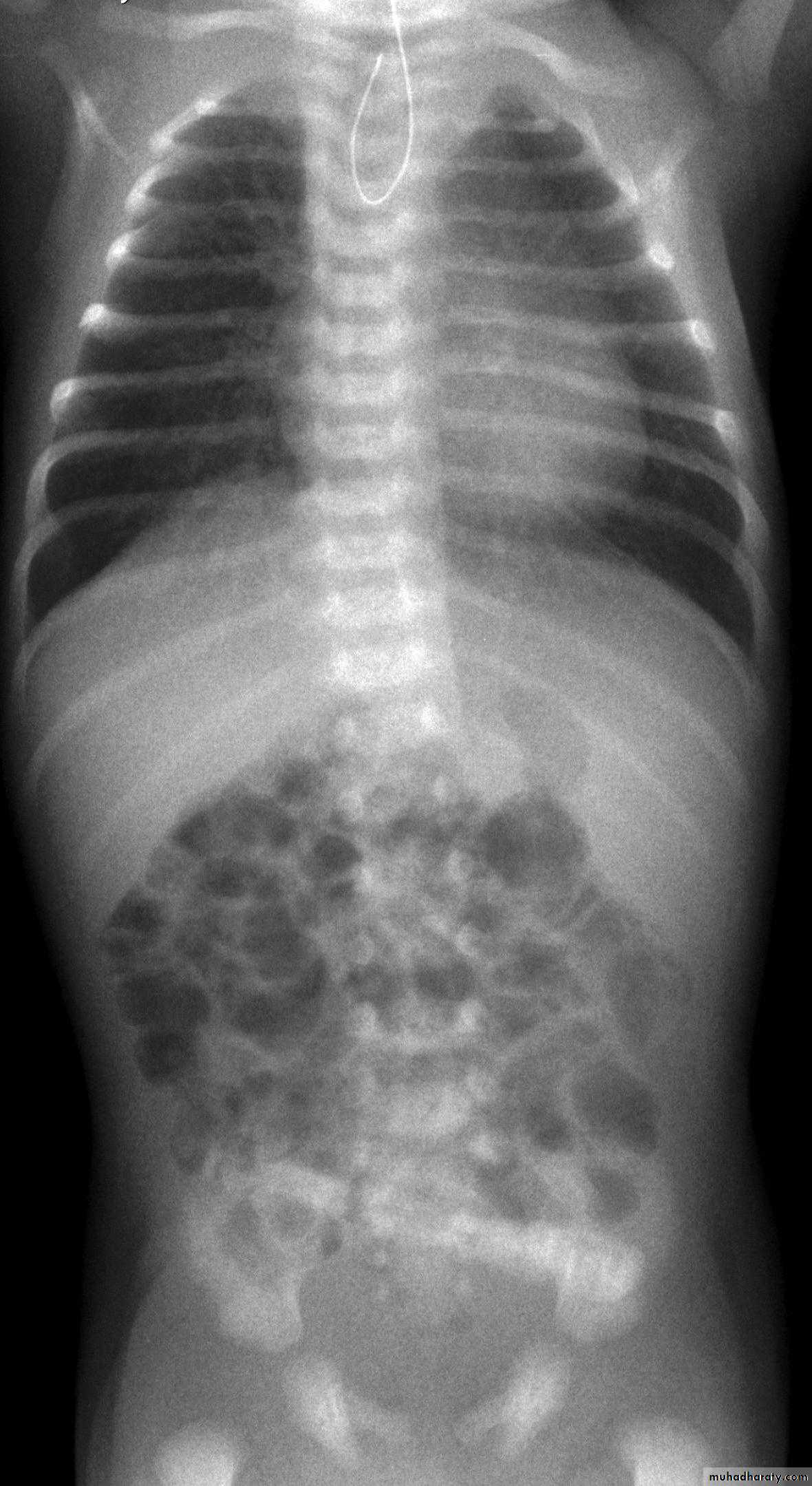
Gas in the wall of the bowel
Spherical or oval bubbles of gas are seen in wall of LB in adults in pneumatosis coli
Linear streaks of intramural gas usually indicate infarction of the bowel wall
Gas in the wall of bowel in neonates, whatever its shape, is diagnostic of necrotizing enterocolitis
7
Gas in the biliary system
Commonly seen following sphincterotomy or anastomosis of the CBD to the bowelIt is also seen with a fistula from erosion of a gall stone into the duodenum or colon, or following penetration of a duodenal ulcer into the CBD
Occasionally, gas may be seen in the wall or lumen of GB in acute cholecystitis from gas-forming organisms
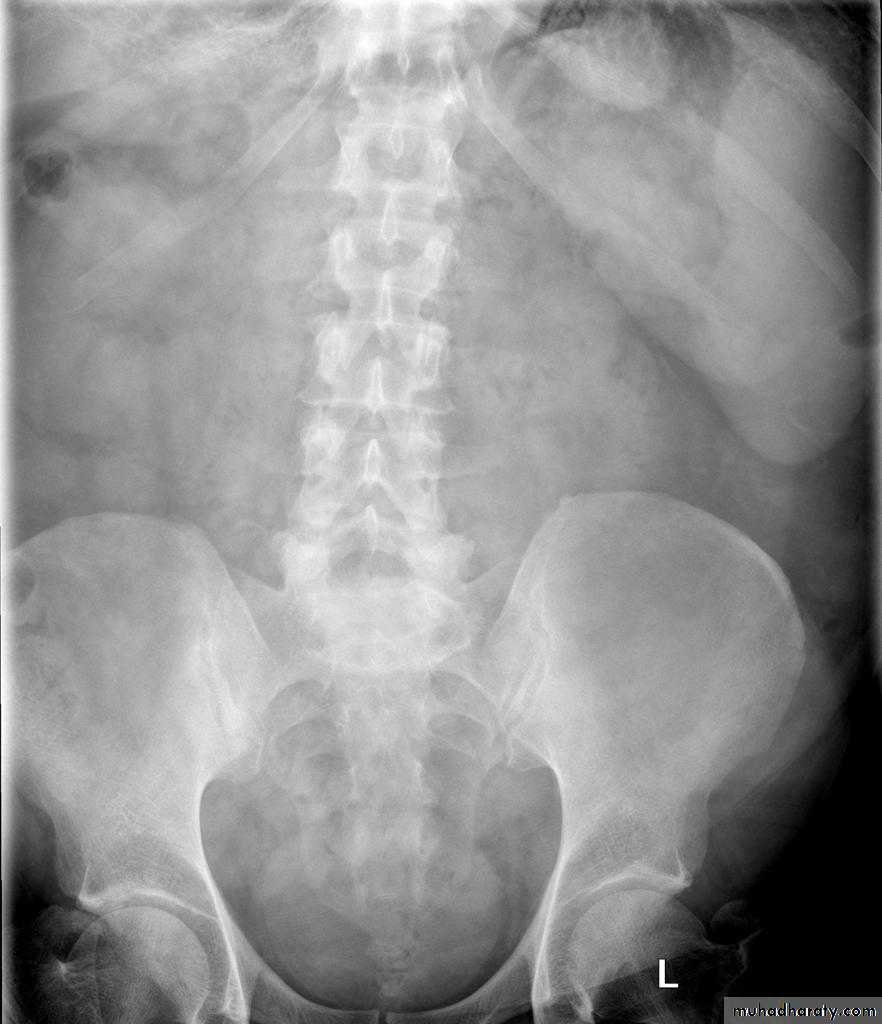
Ascites
Plain films are of very limited value in the diagnosis of ascites
Small amounts of ascites cannot be detected on plain films.
Larger quantities separate the loops of bowel and displace the ascending and descending colon from fat stripes. SB loops float to the center of abdomen
Ascites is more readily recognized with ultrasound or CT
8
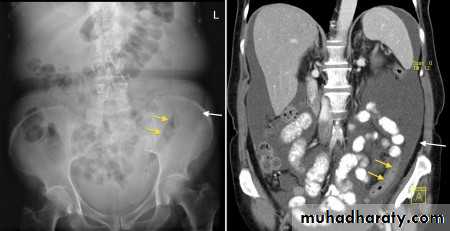
Abdominal calcifications
Assessment of the shape and pattern of abdominal calcification will usually limit the diagnosis to one or two choices. Calcification in the abdomen are likely to be :1. Pelvic vein phleboliths: very common, may be mistaken for urinary stones & fecoliths
2. Calcified mesenteric LN: caused by old TB. They are irregular, very dense and mobile
3. Vascular calcification: e.g. aortic aneurysm which best assessed on lateral film
4. Uterine fibroids: irregular shaped well-defined calcifications conforming to the spherical outline of fibroids
5. Soft tissue calcification in buttocks following injection of certain medicines
6. Ovarian masses may contain calcification. Dermoid cyst may contain teeth
7. Adrenal calcification after adrenal haemorrhage & TB, also in tumor & Addison disease
8. Liver calcification: occur in hepatoma, hydatid cyst, abscess and TB
9. Gall stones
10. Splenic calcifications in cysts, infarcts, old hematomas and TB
11. Pancreatic calcification: occur in chronic pancreatitis & diagnosed from it's position
12. Faecoliths seen in colonic diverticulae or in the appendix. The presence of appendicolith is a strong indicator of acute appendicitis, often with perforation.
13. Renal stones and other calcifications of the urinary tract
9
Plain films of the liver and spleen
Substantial enlargement of the liver has to occur before it can be recognized on a plain abdominal film. As the liver enlarges it extended well below the costal margin displacing the hepatic flexure, transverse colon and right kidney downwards and displacing the stomach to the left .The diaphragm may also be elevatedOccasionly, there is a tongue-like extension of the right lobe into the right iliac fossa, this is a normal variant known as a "Reidl's lobe" and should not be confused with generalized liver enlargement.
As the spleen enlarges, the tip become visible in the left upper quadrant below the lower ribs. Eventually, it may fill the left side of the abdomen and even extend across the midline into the right lower quadrant. The splenic flexure and the left kidney are displaced downwards and medially , and the stomach is displaced to the right.
10
GASTROINTESTINAL TRACT
Dr. Abdullateef AlbayatiImaging techniques – general principles
Contrast examinationsBarium sulphate
It produces excellent opacification, good coating of the mucosa & is completely inert.Its disadvantages are that the barium may solidify and impact proximal to a colonic or rectal stricture.
It may cause a severe inflammatory peritonitis if there is a barium leak from the bowel.
A water-soluble contrast medium, such as Gastrografin is predominantly used when perforations or anastmotic leaks are suspected , in cases where SB obstruction is suspected & in specific circumstances in paediatric patients.
It have several disadvantages: it is hypertonic & soon become diluted ; it is an irritant if enter the lungs; and it is less radio-opaque than barium.
Most barium and Gastrografin examinations are carried out under fluoroscopic control.
Barium examinations of stomach & colon (and in some cases small bowel) are usually undertaken using a double contrast techniques: the mucosa is initially coated with barium and the lumen is distended by introducing air, often in combination with an injection of a short-acting smooth muscle relaxant.Computed tomography
CT can show the full width of the wall and lumen of GIT using either Gastrografin as the contrast agent or air as in CT pneumocolon and virtual colonoscopyCT used for diagnosing and staging of GI tumors
CT can be used to diagnose acute appendicitis & bowel obstruction and in bowel trauma
Ultrasound
US can be used for detecting ascites and assess the bowel wall
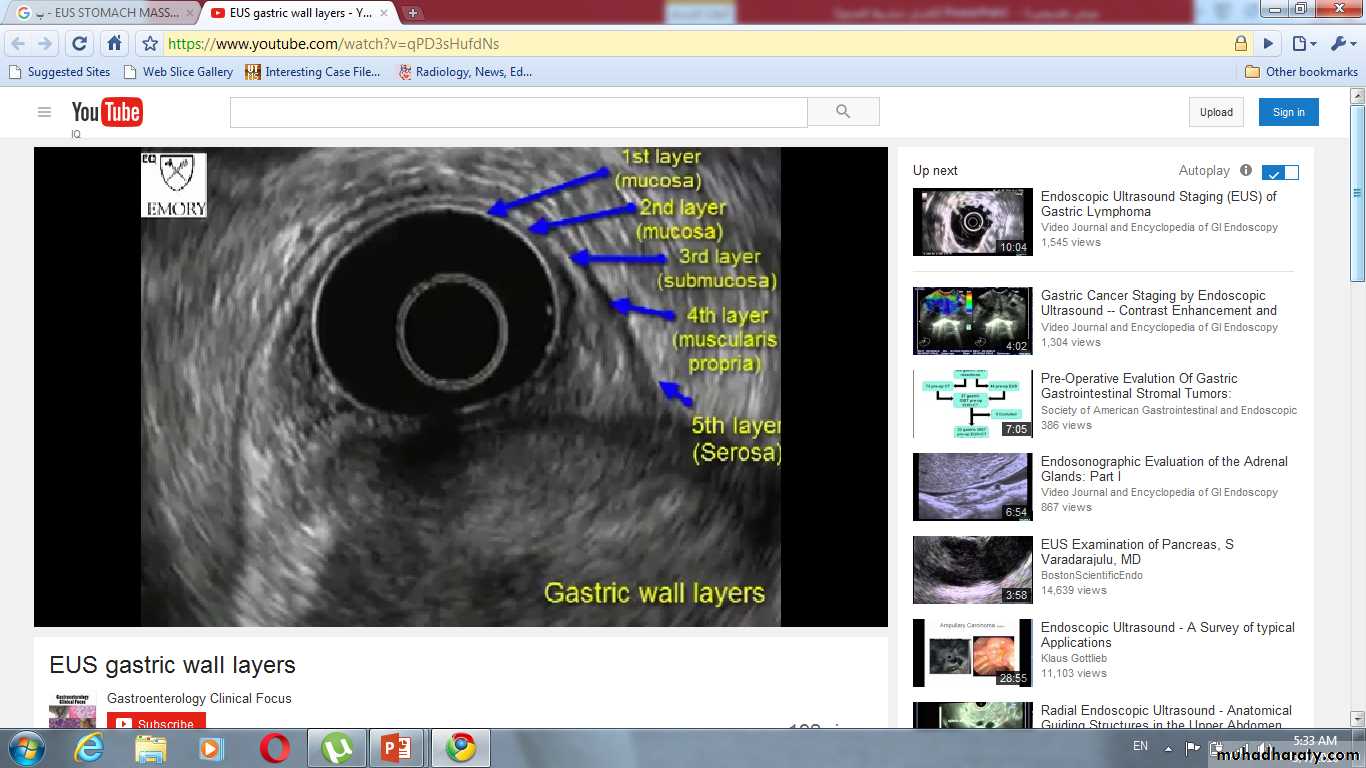
US used for diagnosis of infantile pyloric stenosis, intussusception & in cases of suspected appendicitis. Endoscopic US is used to assess the depth of invasion of tumors in bowel loops and in diagnosing small tumors of pancreas.
MRI
Has a limited role in GIT diseases, due to artefacts caused by peristalsis of the bowel. It's major use is for assessing the local spread of rectal carcinoma and for assessing perianal fistula and abscess formation.
Basic descriptive terms used in reporting contrast examinations
Mucosal pattern : the normal mucosa of stomach and SB is thrown into folds, whereas mucosa of colon and rectum is smooth. Diseased mucosa may be abnormally smooth or abnormally irregular
Ulceration: an ulcer is a breach of a mucosal surface that becomes visible when the crater contains barium.
Filling defect: is a term used to describe any process which prevents the normal filling of the lumen.
Intraluminal filling defect e.g. food is surrounded by barium
Intramural filling defect e.g. carcinoma caused indentation on the lumen
Extramural filling defect compressing the lumen from outside e.g. enlarged LN
Stricture: is a circumferential narrowing. It may have tapering ends or it may end abruptly and have overhanging edges (shouldering) which indicate malignancy
Esophagus
Plain filmsDo not normally show the esophagus unless it is very dilated (achalasia)
Used to check the position of nasogastric tube
Used to demonstrating an opaque forgein body such as bone lodged in the esophagus
Barium examination
The patient swallows a gas-producing agent to distend the esophagus, followed by barium.
Films are taken with esophagus both full of barium to show the outline, and following the passage of the barium to show the mucosal pattern. The esophagus has a smooth outline when full of barium. When empty and contracted, barium normally lies in between the folds of mucosa, which appear as three or four long, straight parallel lines.
Aortic arch cause impression on the left side of the esophagus while the left main bronchus cause smaller impression below the esophagus. Peristaltic waves are observed during fluoroscopic control. Sometimes the contraction waves may not occur in an orderly fashion but are pronounced and prolonged giving the esophagus an undulated appearance (tertiary contractions)
Endoscopy is the primary investigation in patients with dysphagia.
The indications for barium or Gastrografin swallows are:1. swallowing disorders, including confirming or excluding a pharyngeal pouch
2. determining the length of esophageal strictures3. assessing possible mild gastro-esophageal reflux
4. assessing the integrity of an esophageal anastomosis
5. following obesity reduction surgery and anti-reflux surgery
Esophageal carcinoma
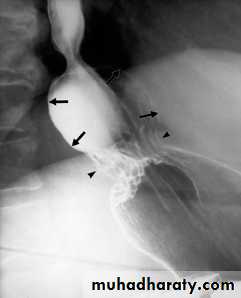
Carcinoma of the esophagus usually involve the full circumference of the wall to form a stricture which can readily demonstrated at barium swallow examination. It may occur anywhere in the esophagus, shows an irregular lumen with shouldering edges and is often several centimeters in length. A soft tissue mass may be visible.Assessing the extent of the tumor is carried out by endoscopic ultrasound (EUS) and CT examination
EUS is able to demonstrate the layers of the esophageal wall and the surrounding LN
EUS is highly accurate in local staging of early cancers
CT is performed following an intravenous smooth muscle relaxant while swallowing water. The tumor is seen as a thickening of the esophageal wall. CT may also show invasion of the mediastinum or adjacent structures, evidence of metastatic spread to LN, liver or lungs.
Peptic stricture
Found in the lower end of esophagus , almost invariably associated with a hiatus hernia and gastro-esophageal reflux. Peptic strictures are characteristically short and have smooth outlines with tapering ends. Ulcer may be seen nearby.
Achalasia
It is a neuromuscular abnormality result from failure of relaxation of the cardiac sphincter, which present at barium examination as a smooth , tapered narrowing always at the lower end of esophagus (bird beak or rat-tail appearance).There is associated dilatation of the esophagus, which often shows absent peristalsis. The dilated esophagus usually contains food residues and may be visible on CXR. The lungs may show consolidation and bronchiectasis from aspiration of the esophageal contents. The stomach gas bubble is usually absent.
Corrosive stricture
It result from swallowing corrosives such as acids or alkalis. It is long stricture begin at level of the aortic arch, usually smooth with tapering ends, but may be irregularLeiomyoma
It is the commonest benign tumor of esophagus. It cause a smooth rounded indentation into the lumen of the esophagus.
Dilatation of esophagus
There are two main types:
Dilatation due to obstruction: associated with visible stricture e.g. carcinoma & achalsia
Dilatation without obstruction: occur in scleroderma. This disease involve the esophageal muscle resulting in dilatation of the esophagus, which resembles an inert tube with no peristaltic movements so that the barium does not flow from the esophagus into the stomach unless the patient stands upright.
Esophageal web
It is a thin, shelf-like projection arising from the anterior wall of the cervical portion of the esophagus. To demonstrate it, that part of the esophagus must be full of barium. A web may be an isolated finding, but the combination of a web, dysphagia and iron-deficiency anemia is known as Plummer-vinson syndrome.
Esophageal varices
Appears as lucent, tortous, wormlike filling defects on barium swallow which distort the mucosal pattern
Esophageal diverticulae
Are saccular outpouchings, which are often seen as chance findings.
Zenker's diverticulum arise from congenital weakness in the inferior constrictor muscle of the pharynx and comes to lie behind the esophagus near the midline. It may reach very large size and can cause displacement and compression of esophagus
Esophageal atresia
The esophagus end as a blind pouch in the upper mediastinum. Diagnosis is made by passing a soft tube into the esophagus and showing that the tube holds up in the blind-ending pouch. The use of contrast agents is potentially dangerous because the contrast may cause respiratory problems if it spills over into the trachea.Stomach and duodenum
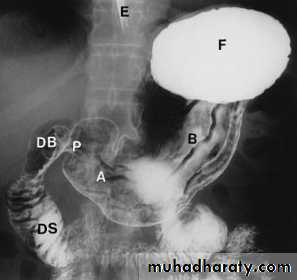
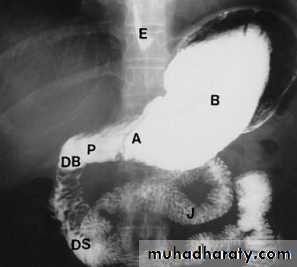
Barium meal examination (the patient instruct to fast at least 6 hours then drinks about 200 cc of barium) is now rarely performed.Upper GI endoscopy is widely used as the initial investigation in patients with possible disease of the stomach and duodenum. It enables the mucosa of the stomach and duodenum to be directly inspected and biopsied.
The main indications for its use :
1. demonstrating mucosal lesions such as gastritis, ulceration or carcinoma2. investigating persistent dyspepsia
3. detecting H. pylori infection
4. assessing healing of ulcer
5. examining patients after gastric surgery
6. diagnosing the cause of bleeding from the upper GIT
7. making a histological diagnosis of an abnormality shown on a barium meal
Indications for contrast radiography(barium or Gastrografin meal):
1. failed gastroscopy
2. assessment of duodenal stricture
3. assessment of functional patency/gastric emptying following gastroenetrostomy
4. to confirm or rule out anastomotic leak following gastric surgery
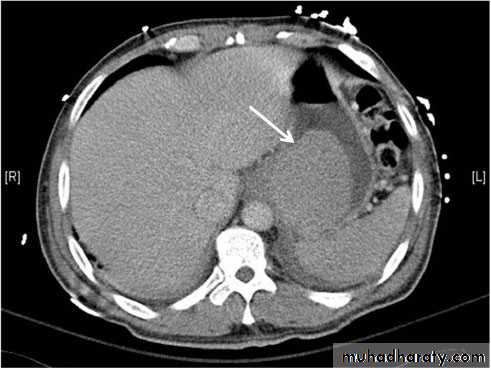
Indications for CT:
1. stage the extraluminal extent of any disease, notably carcinoma, discovered at endoscopy
2. further evaluate the stomach if there is a suspicious of an external mass compressing the stomach.
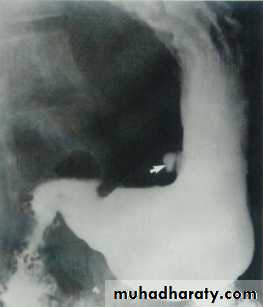
• Peptic ulcer
• Gastric ulcers may be benign or malignant so confirmation at gastroscopy is routinely• Undertaken, whereas duodenal ulcers are almost invariably benign
•
Gastric carcinoma
At barium examination, gastric cancer typically produce an irregular filling defectLinitis plastica is a severe diffused carcinoma resulting in narrowed rigid stomach.
EUS used for in some cases for local staging of early carcinoma.
CT is the main imaging modality for the pre-operative staging as it can show the extent of the tumor, presence of LN and liver metastases
Leiomyoma
Is the commonest benign tumor , produce a smooth round filling defect. It may ulcerateGastric polyps
May be single or multiple, sessile or with stalk. Imaging cannot differentiate between benign and malignant , so gastroscopy with biopsy is carried outLymphoma
The stomach is the most frequent site of lymphoma involving the GIT.Typically produce diffuse thickening of the gastric wall. There may be extensive, bulky LAP.
Gastric outlet obstruction
Gastric outlet obstruction result in gastric dilatation .The causes are:
1. chronic duodenal ulceration
2. carcinoma of antrum3. duodenal, ampullary and pancreatic carcinoma
4. acute or chronic pancreatitis including pseudocyst formation
5. poor functional patency of a gastroeneterostomy
6. pyloric stenosis in infants (US shows a thickened, elongated pyloric canal)
Hiatus hernia
A hiatus hernia is a herniation of the stomach into the mediastinum through the esophageal hiatus in the diaphragm. Two main types: sliding and rollingSliding hiatus hernia: is the commoner type. The gastroesophageal junction and a portion of stomach are situated above the diaphragm. The cardiac sphincter is usually incompetent, so reflux from the stomach to the esophagus occurs readily and this may cause esophagitis, ulceration or peptic stricture
Rolling or para-esophageal hernia: the fundus of the stomach herniates through the diaphragm, but the gastroesophageal junction often remains competent below the diaphragm.
In large hernia, CXR may demonstrates a rounded mass with an air-fluid level projected behind the heart shadow.
Small intestine
Barium follow through : is the standard contrast examination that involves drinking 200 – 300 ml then taking films at regular intervals until the barium reaches the colon. It may take 2-3 hours.The indications are:
1.inflammatory bowel disease (crhon's)
2.suspected stricture
3.malabsorption
4.enterocutaneous fistula
5.malrotation
6.post-small bowel resection
Enteroclysis (small bowel enema) is an alternative contrast procedure that distends the bowel with excellent mucosal detail, but it involves intubation with a nasoduodenal tube through which barium is injected and followed by water or methyl cellulose to propel barium through the bowel
CT scan using oral Gastrografin or water after 4-6 hours fasting can show thickening of bowel wall, irregularity of mucosa and SB tumors
US and MRI has a limited role
Normal appearance of the small bowel
The normal SB occupies the central lower abdomen.
The terminal ileum enters the medial aspect of the cecum through the ileocecal valve.
Normal mucosa exhibit a feathery appearance.
The diameter of SB loop should not exceeds 3 cm .
Signs of disease of the small intestine
Dilatation: more than 3 cm e.g. paralytic ileus, malabsorption and SB obstruction
Thickened mucosal folds: e.g. edema, hemorrhage & inflammation
Stricture : e.g. Crohn's, TB and lymphoma
Ulceration: e.g. Crohn's, TB and lymphoma
Filling defect: tumor, polyp
Diverticulum:
Malrotation:
Crohn's disease
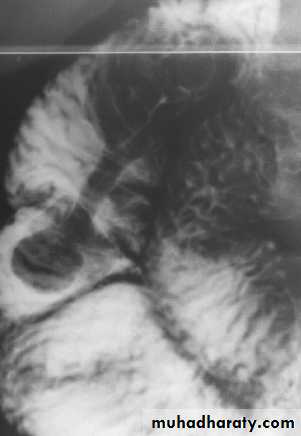
It is non-specific granulomatous inflammatory disease of unknown etiology, it nearly always affect the terminal ileum or other several parts of the small and large intestine, leaving normal intervening bowel, forming the skip lesions.The major radiological signs on barium examinations are :
1.strictures(string sign) are variable in length2.contraction of the cecum, this is seen with a diseased terminal ileum
3.dilatation of the bowel may be seen proximal to narrowed areas
4.ulcers :are quite deep. Fine ulceration + mucosal edema=cobblestone appearance
5.thickening,distortion and effacement of mucosal folds
6.separation of loops of bowel due to bowel wall thickening or an inflammatory mass
7.fistula to other loops of SB, colon, bladder or vagina
8.signs of malabsorption
Small bowel ischemia
A life threatening condition with thrombosis or embolus occlusion of the SMA producing thickening and mucosal edema, may extend to perforate into the peritoneal cavity. The features are best demonstrated by CT scan.Tuberculosis
Affects the ileocecal region indistinguishable from crohns, but sometimes with other associated features e.g. LAP and peritoneal ascites
Lymphoma
Extremely difficult to differentiate from crohns , but other findings associated include: hepatosplenomegaly, enlarged mesenteric LN, marked thickening of bowel loops and lymphomatous deposits in the liver and spleen .
Malabsorption
Definitive diagnosis is done by jejunal biopsy
The imaging signs include:
1.small bowel dilatation
2.thickening of mucosal folds
3.the barium may be diluted
Large intestine
Colonoscopy is now the gold standard for examining the colonic mucosa.If the colonoscopist fails to reach the cecum, the large bowel may be investigated by performing either a barium enema or a CT pneumocolon
Barium enema: bowel preparation is important to get rid of the fecal material, barium is run into the colon under gravity, air is then blown in, to push the barium around the colon to give the double contrast effect. Barium enema is helpful in extensive diverticular disease being prepared for resection, colonic carcinoma, stricture, filling defect and ulceration.
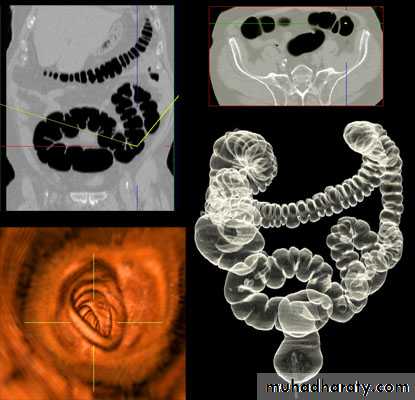
CT pneumocolon: useful to identifying malignant tumors of the colon. A rectal tube is inserted and the colon is distended with gas(CO2 or air). IV contrast agent is given to enhance any tumors that may be present. Neither barium nor Gastrografin is used. CT pneumocolon images can be reconstructed to a three-dimentional display and viewed as "virtual colonoscopy"
MRI has limited role in investigation of the colon due to movements artefacts from bowel peristalsis. MRI is mainly used to evaluate the rectum and anal canal, where movement artefacts are minimal.
Imaging signs of disease of the large intestine
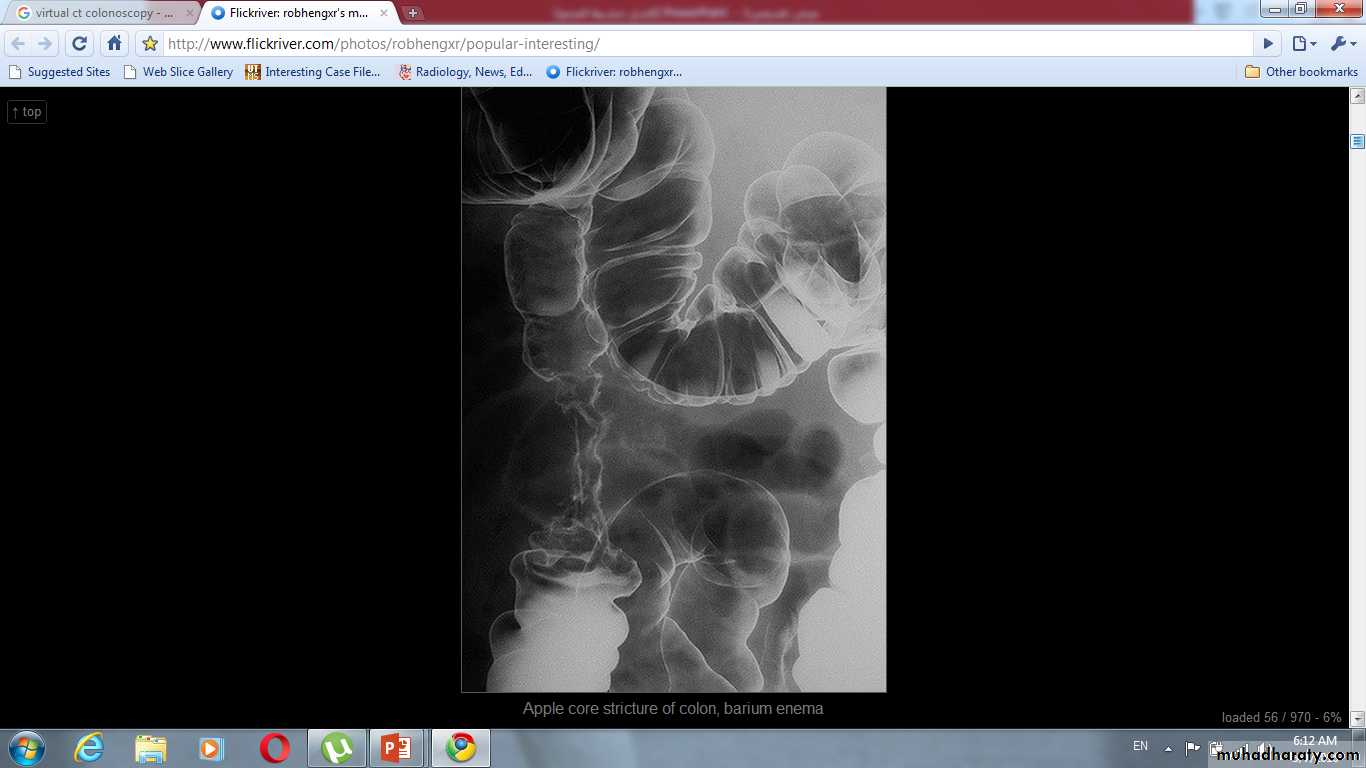
Narrowing of the lumen: may be due to spasm, stricture formation or compression by an extrinsic mass. Common causes for stricture include: carcinoma, diverticular disease, crohn's disease and ischemic colitisThe following points should be assessed to diagnose the nature of stricture:
1.neoplastic strictures have shouldered edges, irregular lumen, are rarely> 6 cm
whereas benign strictures classically have tapered ends, a relatively smooth outline and may be of any length.
2.ulceration may be seen in strictures due to crohn's disease, and sacculation of the colon is a feature of ischemic strictures
3.narrowing in diverticular disease is accompanied by other signs of diverticular disease and may appear similar to neoplastic stricture
4.site of the stricture can help in diagnosis. Diverticular disease is usually confined to sigmoid. Ischemic strictures are usually centered between the splenic flexure and sigmoid . Crohn's disease and TB have a predilection for the cecum
5.extrinsic compression cause a smooth narrowing of the colon frequently from one side only and often displaces the colon.
Dilatation: caused by obstruction, paralytic ileus, volvulus, ulcerative colitis with toxic megacolon and Hirschprung's disease & megacolon
Filling defect: may be intraluminal, mural or extrinsic. In clean colon, a filling defect is likely to be a polyp or an neoplasm. Feces may cause filling defect with no attachment to the wall and completely surrounded by barium and freely mobile. Intramural hemorrhage, edema or air in wall all cause multiple smooth defects arising from bowel wall. Intussusception causes a unique filling defect
Diverticula and muscle hypertrophy: are seen in diverticular disease
Ulceration: recognized as small projections from the lumen into the wall of the bowel in a fuzzy or shaggy appearance. Caused mainly by ulcerative colitis & crohn's disease
Ulcerative colitis
Always involve the rectum, sometimes extends to involve the whole colonRadiological signs:
1.widespread shallow ulcer is the cardinal sign. Ulcers may be deep in severe cases2. widening of the presacral space due to peri-rectal edema
3. loss of the normal colonic haustra in the affected portions of the colon
4.narrowing and shorting of the colon giving the appearance of rigid tube
5.pseudopolyps ( swollen mucosa between ulcers) seen as filling defects
6.strictures are rare and likely to be due to carcinoma in longstanding disease
7.abnormal dilated ileum due to reflux through an incompetent ileocecal valve
8.toxic megacolon is a serious complication diagnosed by plain abdominal film or native CT. Due to the risk of perforation, barium enema, colonoscopy and CT pneumocolon should be avoided
Crohn's disease of the colon
The colon may be the only part of the alimentary tract to be involved, but usually the disease affects the small bowel if the colon is involvedRadiological signs of early stage of the disease are :
1.loss of haustration
2.narrowing of the lumen
3.shallow ulceration
4.cobblestone appearance, combination of mucosal edema and criss-crossing ulceration
Radiological signs of late stage of the disease are:
1.deep ulcers penetrating muscular layer (rose-thorn ulcers or deep fissures)
2.more extensive deep ulceration produce fistulae and abscess formation
3.strictures are common , smooth tapered ends
4.when involved the cecum is usually contracted
5.the disease may involve one portion of the circumference of the bowel
6.skip lesions are diagnostic feature
7.the rectum is often spared
8.ileocecal valve is normal or narrowed; terminal ileum stenosed
Diverticular disease:
Out-pouching of the mucosa through the muscular layer of the bowel wall
Very common particularly in adults, commonest in the sigmoid.
The diverticulae when filled with barium produce a spherical out-pouching with an narrowed neck (diverticulosis), some pouches do not fill with barium when inflamed (diverticulitis) causing symptoms such as sepsis, diarrhea or obstruction.
The colon may show "saw tooth serrated" appearance from muscle hypertrophy.
More extensive lesions produce perforation with fistulae into the bladder, SI or vagina,Pericolic abscess and sometimes pneumoperitoneum.
A stricture may occur in an area of recognizable diverticular disease otherwise canot be differentiated from carcinoma.
Ischemic colitis
Mucosal hemorrhage & edema cause indentations into the lumen of bowel (thumb prints)A long smooth tapered ends stricture involving the splenic flexure with sacculations
Colorectal tumors
Polyps
Best investigated by endoscopy. May be sessile or on a stalk, single or multiple.
Features suggest malignancy are: size>2 cm, short thick stalk, irregular surface & rapid rate of growth.
Carcinoma
May arise anywhere in colon but commonest in rectosigmoid and cecum.
In rectosigmoid, it is often annular obstructing stricture whereas cecal carcinoma can become large without obstruction.
A barium enema shows annular carcinomas as an irregular stricture with shouldered edges (apple-core appearance), usually < 6 cm in length. The polypoid or fungating carcinoma causes an irregular filling defect projecting into the lumen of the bowel.
Volvulus
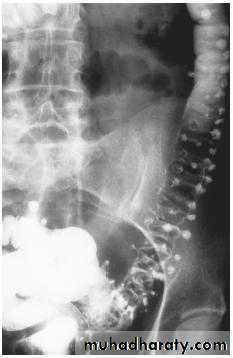
Frequently seen in sigmoid and less often in cecumThe twisted loop becomes greatly distended and proximal bowel dilatation is noted
The diagnosis can be made from plain film
Ba enema will show smooth tapered narrowing with marked dilatation of proximal bowel
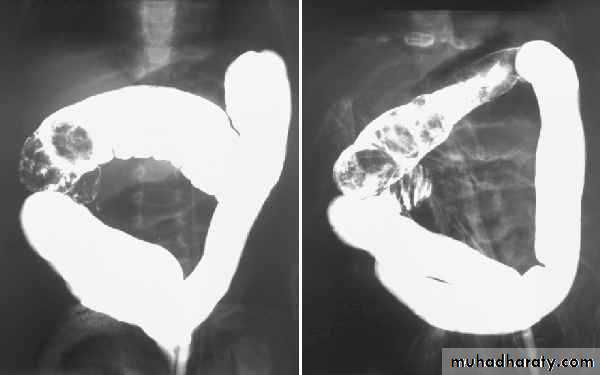
Intussusception
It is the invagination of one segment of the bowel into another. Infants and young children are much more liable than adults. The commonest type is ileocolic. The diagnosis in children is often made by US. In adults, it is almost always due to the presence of a neoplasm.
Hepatobiliary system, spleen & pancreas
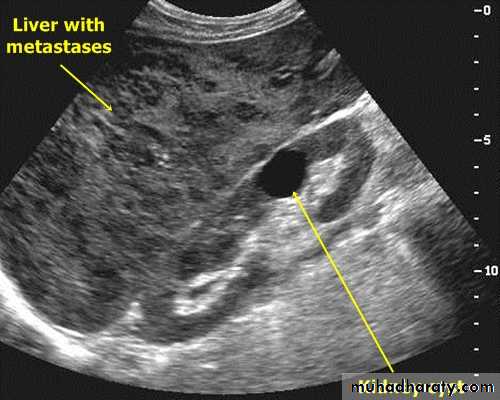
LiverUltrasound : The normal liver parenchyma is of uniform echotexture with portal and hepatic vessels. The normal liver size and shape is variable. Focal masses are noted as alteration of normal echo pattern. They can be divided into cysts, solid or complex masses.
In practice, it is difficult to distinguish benign and malignant lesions unless the mass is clearly a simple cyst.
When multiple masses are seen, metastatic disease is the likely diagnosis. Other differential diagnosis include multiple abscesses and multiple hemangiomas.
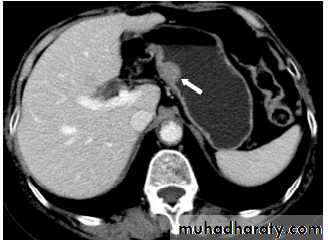
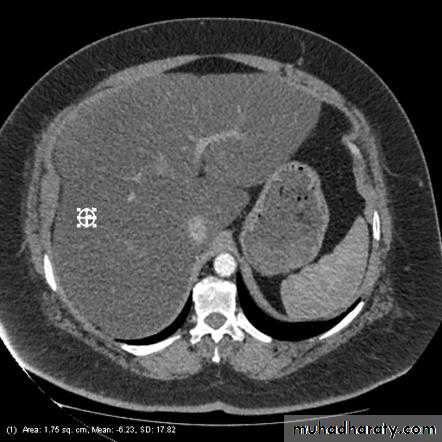
CT : IV contrast is usually given to emphasize the density between normal parenchyma and pathological lesions. The liver has dual blood supply from hepatic artery and portal vein. The liver is divided into 8 segments determined by hepatic and portal veins. The normal liver is higher or equal in density to the spleen. The normal intrahepatic bile ducts are not visible.
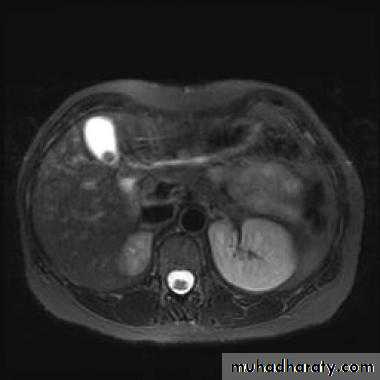
MRI : It is used as a problem-solving technique to give additional information to US and CT scan. It is a good technique for demonstrating primary and secondary tumors and is often used when surgery is contemplated. IV contrast is used to improve visualization and help characterize lesions.
Malignant liver neoplasms
Metastases, notably from carcinoma of stomach, colon, pancreas, lung and breast are much more common than primary tumors.Metastases are often multiple, situated peripherally and of variable size.
At US, they may show increased echogenicity or, more usually, decreased echogenicity compared with the surrounding parenchyma. At times, they show a complex echo pattern and when they undergo central necrosis they may even resemble cysts.
A metastases may have an echogenic center giving an appearance of "target lesion".
At CT, metastases are seen as rounded areas, usually lower in density than normal liver parenchyma with intense enhancement seen after IV contrast.
At MRI, metastases typically have a signal lower than normal liver on T1 and a high signal intensity on T2.
Primary carcinoma (hepatoma) is usually solitary , but may be multifocal. Its CT,US and MRI features are similar to metastatic neoplasms.
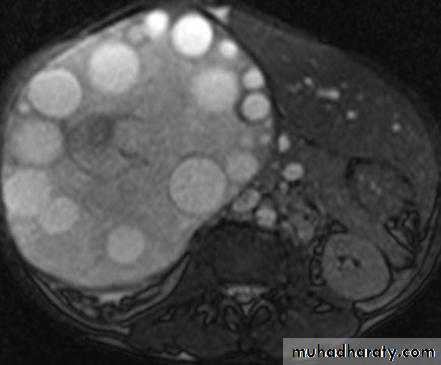
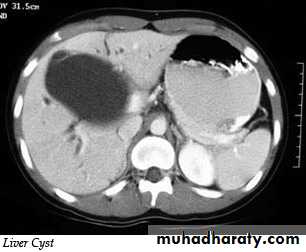
Liver cysts
Simple cysts: may be single or multiple, usually congenital , some are due to infectionMultiple hepatic cysts occur in adult polycystic disease
US features of simple cyst: sharp margin, echofree, with acoustic enhancement
CT features of simple cyst: very well defined margin with water density(HU=0 – 20).
MRI features of simple cyst: low signal on T1 and high signal on T2.
Simple cyst do not show enhancement after IV contrast in CT and MRI
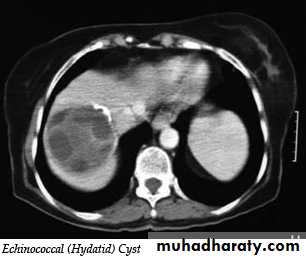
Hydatid cysts may be single or multiple; a few show calcified walls. Daughter cysts may be seen within a main cyst at both US and CT.
Occasionally, metastases can have a cystic appearance.
Hemangiomas of the liver
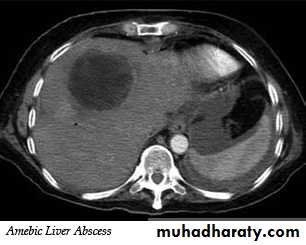
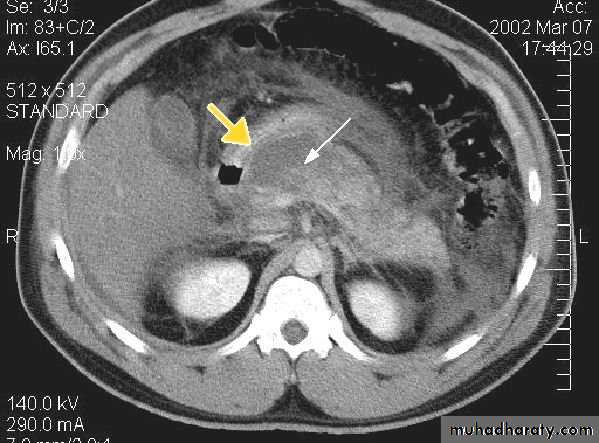
They are the commonest benign tumors in liver. They are common incidental finding and rarely requires treatment. It may cause significant hemorrhage, especially after trauma ,so percutaneous biopsy should be avoided. Hemangiomas are typically well-defined, peripheral echogenic masses at US. At CT, there is usually a characteristic peripheral, nodular and centripetal enhancement after IV contrast. MRI shows uniform very high signal intensity on T2 images.Liver abscess
It appears similar to cysts but have a thick irregular wall with fluid center.
Occasionally chronic abscess calcify.
It cannot be distinguished from necrotic tumor , but the clinical events should aid in the diagnosis. Aspiration under US guidance is invariably undertaken.
Cirrhosis of the liver and portal hypertension
In portal hypertension, the pressure in the portal venous system is elevated due to obstruction of the blood flow in the portal or hepatic venous system. Cirrhosis is the commonest cause. Other causes include the occlusion of the hepatic veins (Budd-chiari syndrome) and thrombosis of the portal vein following infection of the umbilical vein in neonates or secondary to acute pancreatitisThe signs of liver cirrhosis at CT and US are :
1.reduction in size of the right lobe of the liver2.irregularity of the surface of the liver
3.splenomegaly
4.ascites
5.coarse abnormal liver texture at US while at CT, the parenchyma appears normal until late in the disease.
Patency of the splenic, portal & hepatic veins can be assessed with Doppler US,CT&MRI
Liver trauma
Trauma to the liver is the commonest abdominal injury that leads to death, with parenchymal lacerations are the most frequent injury, often accompanied by subcapsular and intrahepatic hematoma.US has become part of the standard assessment. Focused Assessment with Sonography for Trauma "(FAST scan) is a rapid bedside examination which examines four areas for free fluid:
1.perihepatic and hepatorenal space
2.perisplenic
3.pelvis
4.pericardium
CT is more sensitive and specific. Lacerations and hematomas are recognized as low density areas relative to the normal intact, enhanced parenchyma. Leakage of contrast indicate active bleeding
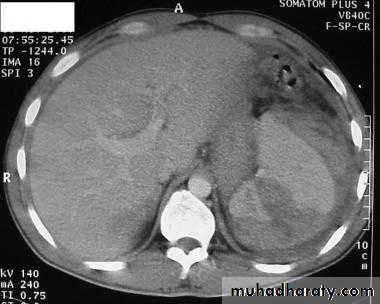
Fatty infiltration of the liver
It is a frequent finding, particularly in those with hypercholesterolaemia, obesity, diabetes or those who take alcohol to excess. It may involve the whole liver or it may just involve individual subsections
At CT, liver density is less than splenic density
At US, increased liver echogenicity (bright liver)MRI useful in problem cases because fat gives a characteristic set of signals
The biliary system
US: is the best method for investigation.The patient is asked to fasting 6 hours to prevent GB contraction.
The normal GB has a thin wall< 3 mm, and thickening of wall suggest either acute or chronic cholecystitis. Stones > 2 mm can be identified.
The normal CBD can be visualized in all patients and should not measure>7 mm unless the patient done cholecystectomy when it may be larger.
The lower end of CBD is obscured by bowel gases.
The normal intrahepatic tree is of such smaller caliber to be visualized by US.
Magnetic resonance cholangiopancreaticography (MRCP)
MRCP technique use heavily T2-weighted sequences where bile and pancreatic ducts have high signal intensity. Unlike ERCP, it is non-invasive, does not require sedation and bowel intubation & no contrast agent used , although ERCP is necessary for any endoscopic biopsy or treatment
Gall stones
Gall stones are more frequent in middle age females. 20% of gall stones are visible on plain film. On US, stones are strongly echogenic with acoustic shadow(which is not seen with polyps). US is not reliable for detecting stones in CBD which are better demonstrated by MRCP
Cholecystitis
US features of early or uncomplicated acute cholecystitis:1.gall stones (which may be impacted in the GB neck or cystic duct)
2.gall bladder wall thickening
3.gall bladder distension
4.positive sonographic Murphy's sign (focal tenderness over the GB when compressed by the US transducer)
US features of advanced or complicated acute cholecystitis:
1.pericholecystic fluid collection
2.striated appearance of the thickened GB wall
3.intraluminal membranes caused by sloughed GB mucosa
4.gas in GB wall or lumen resulting in emphysematous cholecystitis
US features of chronic cholecystitis are thick wall and GB contraction
Biliary obstruction
Common causes of biliary obstruction are :1.impacted stone in CBD
2.carcinoma of the head of pancreas
3.carcinoma of the ampulla of vater
4.cholangiocarcinoma
US is the first test to be performed in obstructive jaundice. US can show dilated ducts& can demonstrate the level of obstruction & sometimes the specific cause of biliary obstruction e.g. stone or pancreatic head tumor.
MRCP is often more helpful than CT in cases of suspected CBD stones or biliary stricture.
Pancreas
CT is the main stay for imaging of the pancreas, it can image the pancreas regardless of the amount of bowel adjacent to it, whereas the US beam is absorbed by the gas in the GIT.The normal pancreas is an elongated retroperitoneal organ surrounded by a variable amount of fat.
The head is visualized to best advantage when the duodenum is opacified with oral contrast. The body of the pancreas lies in front of the SMA and V.
The tail situated near the hilum of the spleen. The splenic vein lies behind the body, it join the SMV at the neck of the pancreas to form the portal vein.
Pancreatic adenocarcinoma
It locate in head of pancreas in 2/3 cases.It obstruct CBD even with small lesions giving rise to jaundice.
Tumors in the body or tail become large until giving rise to symptoms.
The important sign of carcinoma at both CT and US is a focal mass within or deforming the outline of the gland.
On contrast-enhanced CT, the tumor appears of lower density compared to the normal pancreatic tissue. The main pancreatic duct may be dilated distal to an obstructing mass . Most tumors are irresectable at time of diagnosis because of involvement of regional LAP, liver metastases and regional vascular encasement.
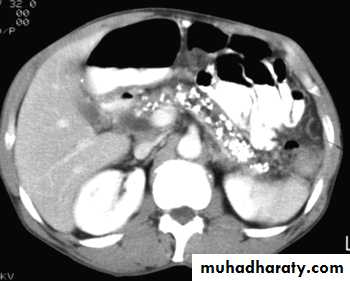
Acute pancreatitis
The pancreas is usually enlarged, often diffusely with irregular outlines due to extension of inflammatory process into the surrounding fat. There may be low density areas at CT or echo-poor areas at US (edema and necrosis)
The diagnosis is usually made on clinical and biochemical grounds, the purpose of CT is to assess the severity and complications:
1.pancreatic necrosis (areas with no enhancement)
2.abscess appear as fluid collection which may contain gas
3.vascular complications e.g. splenic vein thrombosis, arterial erosion & pseudoaneurysm
4.pseudocysts occur as a result of leak of pancreatic secretions that are contained in a cyst like manner within and adjacent to the pancreas.
They can be demonstrated with CT or US as thick or thin walled cysts of variable sizes.
Many pseudocysts resolve in the weeks following an attack of acute pancreatitis, some persist and may need surgical or percutaneous drainage.
Chronic pancreatitis
It result in fibrosis, calcifications, and ductal stenosis and dilatation.Pseudocysts are seen.
The calcification often recognizable on plain x ray film, but more obvious on CT.
The gland may enlarge focally or generally. The gland may atrophied. The pancreatic duct may be enlarged and irregular.
Spleen
The commonly encountered splenic masses are cysts, including hydatid cysts, abscesses, and tumors; lymphoma is much commoner than metastases, which are rare in the spleen.Causes of splenomegaly include lymphoma, portal hypertension, chronic infection and various blood disorders.
Splenic infarction occur secondary to severe pancreatitis, pancreatic carcinoma, sickle cell and trauma. It show focal or complete loss of normal enhancement following IV contrast
The spleen is the most commonly injured organ in blunt trauma. CT is the superior method of investigation.
END