Myopathy
Dr. Maitham F. JalalF.I.B.M.S F.E.B.N
When you suspected myopathay
Proximal weaknessdifficulty in going upstairs
difficulty combing hair
No parasthesia and numbness
• The first goal in approaching a patient with a suspected muscle disease is to determine :
• The the cause of the myopathy.
• To determine whether a specific treatment is available and if not, to optimally manage the patient’s symptoms , functional abilities and enhance quality of life.
ETIOLOGY / CLASSIFICATION
Inherited myopathiesMuscular dystrophies
Congenital myopathies
Inherited metabolic myopathies
Acquired myopathies
Inflammatory myopathies
Acquired metabolic myopathies
Toxic myopathiesMyopathies Presenting in Adulthood
Inherited1 Muscular dystrophies
Limb-girdleFacioscapulohumeral FSHD
Becker , DMD
Myotonia dystrophica
2 Metabolic myopathies
Acid maltase deficiencyLipid storage diseases
Mitochondrial myopathies
3 Congenital myopathy
Nemaline myopathy
Acquired
1 Inflammatory myopathiesPolymyositis
Dermatomyositis
Inclusion body myositis
2 Endocrine( metabolic) myopathies
Thyroid3 Toxic myopathies
AlcoholCorticosteroids
Statin
What is Muscular Dystrophy?(MD)
• Muscular Dystrophy:• group of genetic disorders that are characterized by progressive loss of muscle integrity, wasting, and weakness. Characterized by degeneration and regeneration of muscle fibers (in contrast with static or structural myopathies)
• Muscular Dystrophy Association
• Multisystem diseases : cardiac , respiratory GIT and cognitive
• the two most common and severe dystrophies
Duchenne Muscular Dystrophy
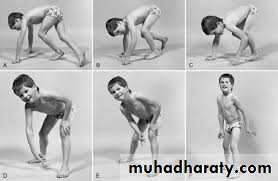
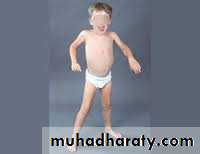
• Presentation: 3-5 y/o with pseudohypertrophy of calf muscles, frequent falls, tip toe walking , slow running, and waddling gait• Other organs affected
• Heart – cardiomyopathy
• Respiratory
• Intellect - 30 % with impairment IQ
• Very high CPK
Myotonia Dystrophica
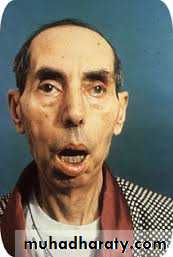
• Presentation – adult with multiple systems affected• Primarily distal and facial weakness
• Facial features: frontal balding in men, ptosis, hatchet face ^ shaped upper lip
• Myotonia: difficulty in relaxation after contraction
• In addition :
• Heart: conduction block – evaluate syncope
• Brain: learning disabilities
• Ophthalmology: cataracts
• Endocrine: insulin resistance, hypothyroidism, testicular atrophy
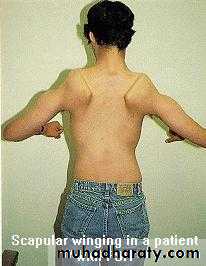
Facioscapulohumeral FSHD
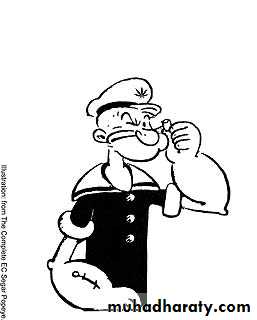
normal deltoidsbiceps, triceps commonly weak, forearm muscles are less involved resulting in a
popeye-like appearance
Scapular winging may be very asymmetric (misdiagnosed as long thoracic nerve of palsy)
General Diagnostic Testing
Creatine kinase :greatly elevated (50 times normal)
Increased in DMD
• nucleotide repeats …..dystrophen
• Steroids
• Briefly increase strength, slow progression in dystrophinopathy• Creatine and glutamine may help delay
• progression/improve energy in youngest with DMD
• Physiotherapy , contracture prevention and surgeory
• Treat respiratory , cardiac
Idiopathic inflammatory myopathies
Polymyositis
DermatomyositisInclusion body myositis
Clinical featuresProgressive painful weakness
Difficulty lifting above head/combing hair
Difficulty arising from a low chair or toiletNasal regurgitation or choking when eating
Hoarseness, change in voice
*Ocular/facial muscle involvement is very uncommon
Symmetric weakness of limb girdle muscles and anterior neck flexors.
Fatigue
Fever• Dermatologic features in dermatomyositis
Dermatologic manifestations
www.jfponline.com/Pages.asp?AID=2763&UID=
Inclusion body myositis
May differ from PM and DM :Occur in elderly
focal, distal UL and proximal LL weakness.Dyspagia is a late occurrence.
CK only slightly increased and can be normal in up to 25% of patients.
Multisystem disease
CardiacRespiratory involvement
fibrosis with anti –JO antibody
GIT
Autoantibody
Malignancy risk
Strong association between malignancy and dermatomyositis, but less clearly with polymyositis.
Ovarian, lung, pancreatic, stomach and colorectal and non-Hodgkin lymphoma
The overall risk is greatest in the first 3 years after diagnosis but is still increased through all years of follow-up.
Investigations
Muscle BiopsyNCS/EMG
Lab ( CK)
• Electromyographic (EMG)
•Corticosteroids is mainstay of treatment in most cases
Start 1-2 mg/kg/dayContinue until CPK returns to normal, then slow taper.
For severe acute disease, consider pulse dose steroids.
Other treatments
Steroid sparingMethotrexate
Imuran
Non-responders
Rituxan
IVIG
Cyclosporin
Cyclophosphamide
Plasmapheresis
Corticosteroid- Corticosteroid-Induced Myopathy
Steroid myopathy is usually an insidious disease process that causes weakness mainly to the proximal muscles of the upper and lower limbs and to the neck flexors.
An excess of either endogenous or exogenous corticosteroids is believed to cause the condition. Excess endogenous corticosteroid production can arise from adrenal tumors.
An excess of exogenous corticosteroid can result from steroid treatment for asthma, chronic obstructive pulmonary disease, and inflammatory processes, such as polymyositis, connective tissue disorders, and rheumatoid arthritis
Corticosteroid- Corticosteroid-Induced Myopathy
InvestigationSerum levels of creatine kinase typically are within the normal range.
Electromyography (EMG) and nerve conduction studies (NCSs)1. Motor and sensory NCS results typically are normal.
2. EMG studies reveal normal insertional without abnormal spontaneous activity (positivesharp waves and fibrillation potentials). Which is the main difference between inflammatory myopathy and myopathy result from steriod use in case of inflammatory myopathy
Corticosteroid- Corticosteroid-Induced Myopathy
TreatmentThe main treatment recommendations for steroid myopathy are a decrease in the dose of steroid to below a threshold level or the discontinuation of the corticosteroid's use.
Alternate-day dosing could also be considered.
Another recommendation is that the currently administered steroid be exchanged for one that is not fluorinated.
THANK YOU