Dr. Maitham F. Jalal
F.I.B.M.S F.E.B.NINFECTIONS OF THE CENTRAL NERVOUS SYSTEM
Meningitis
EncephalitisBrain abscess
MENINGITIS
A medical emergency!BACTERIAL
VIRALFUNGAL
TB
Other
BACTERIAL
Incidence:
Primary meningitis:
spread via the bloodstreamSecondary meningitis:
Ears, sinuses, trauma,Surgery
Main pathogens:
Neisseria meningitidisStrept. Pneumoniae
Haemophilus influenzaeHeadache
IrritableNeck stiffness
Photophobia
Fever
Vomiting
Varying levels of consciousness
Rash
Clinical features that suggest the diagnosis of acute meningitis
Neonates (first few weeks of life)
Elderly
Immunosuppressed
Groups in which clinical features are not so specific
The most common cause of acute bacterial meningitis
Most cases in children and young adultsGroup B serotype traditionally most frequent cause
Person to person transmission
Reservoir nasopharynx (2-25% carriage)
Respiratory droplet spread
Incubation period 1-3 days
N meningitidis (meningococcus) and meningococcal meningitis
Nasopharyngeal carriageBloodstream infection
Meningitis
May be sore throat
Progression from headache, drowsiness, signs of meningitisHaemorrhagic skin rash (non-blanching)
Sepsis complicated by intravascular coagulation, shock, acute renal failure
Bleeding into organs may occur eg, adrenal gland causing Waterhouse Friderichsen syndrome
Gangrene of peripheral limbs
CLINICAL FEATURES
Purpura fulminans
Clinical features
Clinical features
Tumbler (glass) test
If possible collect Cerebrospinal fluid (may not be, if raised intracranial pressure)
Blood culture, both before antibiotic therapySample from petechial skin lesion may yield meningococcus
CSF subjected to cell count, gram stain of deposit, and culture on chocolate agar in CO2 atmosphere
MICROBIOLOGICAL DIAGNOSIS
Diagnosis
LP
CSF Abnormalities in Meningitis
• Condition• Appearance
• Cells/cu mm
• Gram
• Protein
• Glucose
• Normal
• Clear, colourless
• 0-5 lymphocytes
• Bacterial
• Cloudy, turbid
• 100-2000 polymorphs
• Orgs
• High
• Low
• ‘Aseptic’ (viral)
• Clear, slightly cloudy
• 10-500 lymphocytes
• Normal
• Normal
• TB
• Clear, slightly cloudy
• 10-500 lymphocytes
• High
• Low
• Cryptococcal
• Clear
• 10-200 lymphocytes
• Normal, slightly elevated
• Normal, slightly reduced
Once the diagnosis is clinically suspected don’t delay treatment
If the causative agent is not clear eg, no rash, give ceftriaxone or cefotaxime plus vancomycin
This provides cover of the 3 main causes until a microbiological diagnosis is made
If meningococcal meningitis confirmed then a change to high doses of benzylpenicillin can be considered
Chloramphenicol can be an alternative if allergy to beta lactams
Steriod should be given prior to antimicrobial
Prophylaxis rafampicin 600mg twice for 2 days
TREATMENT OF ACUTE BACTERIAL MENINGITIS KEYPOINTS:
Strep pneumoniae is the cause, a capsulate gram positive coccus
Highest incidence in those at extremes of age, infants <3yrs and elderlyAlcoholism, debilitation, malnutrition, hyposplenism
May spread from middle ear or sinus infection
Or following trauma causing basal skull #
Pneumococcal meningitis
Acute onset with rapid development of loss of consciousness
Skin rash not a featureMay be a history of ear infection, splenectomy
Bacteraemia a feature
High incidence of complications in survivors
Pneumococcal meningitis: clinical features
High doses of penicillin eg, 1.2 g each 2 hourly
Note some strains have reduced susceptibility to penicillin, and some are resistant!
Need to review to find a potential underlying risk factor
Polyvalent vaccine for risk groups eg, before splenectomy
Treatment
Gram negative coccobacillus, capsulated strains (type b used predominate)
Peak incidence 2 years old, range 3 months to 5 yearsIncidence has declined greatly since the successful introduction of Hib vaccine
More insidious onset, no rash, lower mortality
Diagnostic approach as for other causes
Treament with cefotaxime or ceftriaxone
Haemophilus influenzae meningitis
Post trauma or surgery
Staph aureus, streps, anaerobes, coliforms, PseudomonasImmunocompromised
Listeria monocytogenesWe have to add ampicilline if suspected 2 g 4 hourly
Others
M tuberculosis, Leptospira, Borrelia burgdorferi
Other bacterial causes of meningitis in adults and children
Cerebral complications
Brain edema with the risk of herniationSeptic sinus/venous thrombosis
Hydrocephalus
Cerebritis
Subdural effusion (in in
Extracranial complications
myocarditis
Septic shock
Disseminated intravascular coagulation
Adult respiratory distress syndrome (ARDS)
Arthritis (septic or reactive)
(SIADH)
Complication of meningitis
low-grade fever, headache, and intermittent nausea and vomiting, followed by more severe headache, neck stiffness, altered mentation, and cranial (usually III, but also II, VII, and VIII) nerve palsiesmeningeal signs, seizures, and focal neurological deficits, including hemiparesis, increasing drowsiness, and signs of increased ICP
choroidal tubercles
Tuberculoma, or Tuberculous involvement of the spine with myelopathy (Pott's disease)
Tuberculous meningitis
CSF examination
polymerase chain reaction (PCR) technique has been applied and is now routinely available for the diagnosis of TB meningitis, with reported sensitivities of 70-75%.Tuberculomas : parenchymal form of TB, occur as single
or multiple brain or spinal cord lesions and present with signs and symptoms of space-occupying lesions.Diagnosis
CSF Abnormalities in Meningitis• Condition
• Appearance
• Cells/cu mm
• Gram
• Protein
• Glucose
• Normal
• Clear, colourless
• 0-5 lymphocytes
• Bacterial
• Cloudy, turbid
• 100-2000 polymorphs
• Orgs
• High
• Low
• ‘Aseptic’ (viral)
• Clear, slightly cloudy
• 10-500 lymphocytes
• Normal
• Normal
• TB
• Clear, slightly cloudy
• 10-500 lymphocytes
• High
• Low
• Cryptococcal
• Clear
• 10-200 lymphocytes
• Normal, slightly elevated
• Normal, slightly reduced
Complication of TB meningitis
• Progressive hydrocephalus
• damage to the optic nerves
• the syndrome of inappropriate secretion of antidiuretic hormone
• vasculitis; stroke;
• arachnoiditis; .
Isoniazid (INH) .5-10 (max 300 mg) PO, add pyridoxine to prevent
neuropathy (Child 25 mg/kg/day PO, Adult 50 /mg/kg/day PO)side effect Hepatitis (1-2%), neuropathy (5%), seizures
Rifampin (RIF) Child 15 PO, Adult 10 PO"
side effect Hepatitis (1-2%),
Pyrazinamide 25 (max 2.5 g/day) PO
Arthralgia (5%!, hepatitis (1-5%), hyperuricemia, gout, rash
Streptomycin Child 30 IM Adult 15 (max 1 g/day) IM Hearing loss, vestibular imbalance (1-5%)
Ethambutol 15-25 (max 2.5 g/day) PO Optic neuritis (3%), neuropathy (1-2%), rash
Most common infection of CNS especially in <1yr
Causes: enterovirus (commonest, meningitis occurring in 50% of children <3mth ) herpes, influenza, rubella, echo,coxsackie, EBV, adenovirusMild clinical feature
Symptomatic treatment. Complications associated with encephalitis and ICP
Viral meningitisExamination of CSF
Storage at -700C of CSF for subsequent virus isolationAdditionally throat swab, stool, paired sera
Diagnosis: viral meningitis
CSF Abnormalities in Meningitis
• Condition• Appearance
• Cells/cu mm
• Gram
• Protein
• Glucose
• Normal
• Clear, colourless
• 0-5 lymphocytes
• Bacterial
• Cloudy, turbid
• 100-2000 polymorphs
• Orgs
• High
• Low
• ‘Aseptic’ (viral)
• Clear, slightly cloudy
• 10-500 lymphocytes
• Normal or high
• Normal
• TB
• Clear, slightly cloudy
• 10-500 lymphocytes
• High
• Low
• Cryptococcal
• Clear
• 10-200 lymphocytes
• Normal, slightly elevated
• Normal, slightly reduced
Cryptococcus neoformans is main cause
HIV and immunosuppressed pts at risk
Insidious onset of headache, fever, neck stiffness
Diagnosis made on CSF examination
Shows raised lymphocyte count, protein, low sugar, capsulate yeasts, antigen
Treat with amphotericin B +flucytosine
Fungal meningitis
CSF Abnormalities in Meningitis
• Condition• Appearance
• Cells/cu mm
• Gram
• Protein
• Glucose
• Normal
• Clear, colourless
• 0-5 lymphocytes
• Bacterial
• Cloudy, turbid
• 100-2000 polymorphs
• Orgs
• High
• Low
• ‘Aseptic’ (viral)
• Clear, slightly cloudy
• 10-500 lymphocytes
• Normal
• Normal
• TB
• Clear, slightly cloudy
• 10-500 lymphocytes
• High
• Low
• Cryptococcal
• Clear
• 10-200 lymphocytes
• Normal, slightly elevated
• Normal, slightly reduced
Affects children and adults mostly
A variety of symptoms and signs
Drowsiness, confusion, coma, fits, nerve palsies, paresis focal sign
May have sequelae eg, memory loss, motor impairment, death
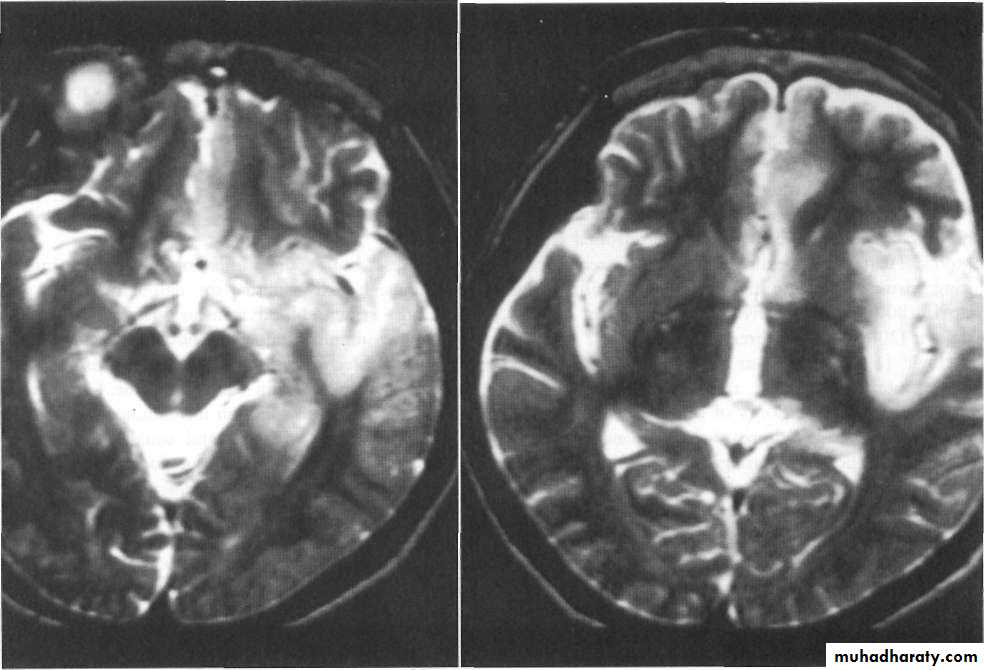
EEG, brain MRI, CSF exam
CSF : lymphocytic ,normal sugar
EEG : triphasic
MRI : temporal lobe
ENCEPHALITIS
Sporadic:Herpes simplex, mumps, VZV, EBV rabies
Post-infectious:
Measles, rubella, post-vaccinationDegenerative:
Measles (SSPE), vCJD, JC virus (PML)Causes of encephalitis
Most common cause of sporadic encephalitis in previously healthy
May be evidence of herpes infecion of skin, mucosae
Causes severe haemorrhagic encephalitis affecting temporal lobe,
Focal signs and epilepsy features
High mortality so treatment urgently needed with aciclovir
Herpes simplex encephalitis
Can arise from direct inoculation of infection following trauma, surgery; from spread of infection of ear or sinuses; or haematogenous spread from eg, lungs, heart (endocarditis)
May be non-specific signs, neurological symptoms
Needs urgent investigation by CT/MRI scan
Surgical treatment +antibiotics
Brain abscess
Ear: mixed anaerobes, coliforms
Sinus: pneumococci, streptococciTrauma/surgery: Staph aureus
Chest: strep, staph, pneumococci
Causes of brain abscess
Examination of pus aspirated from abscess
Blood cultures
Surgical drainage a priority
Antibiotics chosen with good penetration of CNS
Diagnosis and treatment