Bone marrow & peripheral blood stem cell transplantation
Hematopoietic stem cell transplantation (HSCT) is the transplantation of multipotent hematopoietic stem cells, usually derived from bone marrow, peripheral blood, or umbilical cord blood. It is a medical procedure in the fields of hematology and oncology, most often performed for patients with certain cancers of the blood or bone marrow, such as multiple myeloma or leukemia.In these cases, the recipient's immune system is usually destroyed with radiation or chemotherapy before the transplantation.
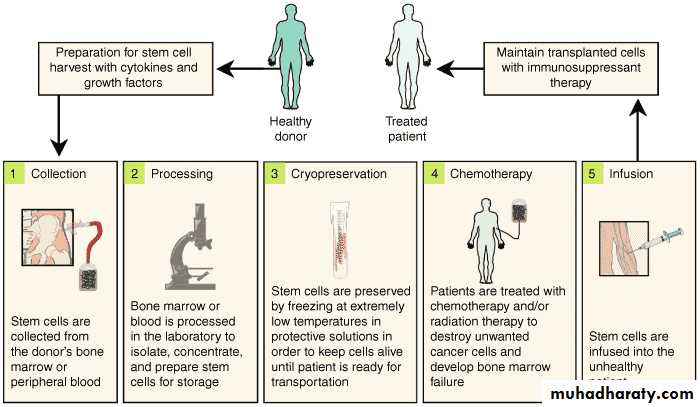
Hematopoitic stem cells can be obtained directly from the Bone marrow by multiple aspiration from the pelvic bones While the patient is under general anesthesia (BMT) Hematopoietic cells can be obtained from the peripheral Blood after stimulation with hematopoietic growth factor Such as (G-CSF), followed by leukopheresis (peripheral Stem cell transplantation
Allogeneic
Allogeneic HSCT involves two people: the (healthy) donor and the (patient) recipient. Allogeneic HSC donors must have a tissue (HLA) type that matches the recipient. Matching is performed on the basis of variability at three or more loci of the HLA gene, and a perfect match at these loci is preferred.Allogeneic BMT
Healthy marrow or stem cells from a donor are infused IV into the Recipient who has been suitably conditioned The conditioning treatment (chemotherapy with or without radiotherapy Destroy malignant cells and immunosuppresses the recipientAs well as ablating the recipients haematopoietic tissue the injected donor cells home to the marrow , engraft and Produce enough erythrocytes, granulocytes and platelets
For the patients needs after about 3-4 weeks During this period of aplasia patients are at risk of Infection and bleeding and require intensive supportive Care
It may take several years to regain normal Immunological function and patients remain at risk from apportunistic infections, in particular in first year.
An advantage of receiving donor stem cells is that the donor Immunological system can recognise residual malignant Recipient cells and destroy them. This immunological graft versus disease effect is a powerful Tool against many haematological tumours and can be Boosted in post –transplantation relapse by the infusion of T cells taken from the donor, so –called donor lymphocyte Infusion (DLI). The best results are obtained in patients with minimal Residual disease, and in those under 20 years of age Who have an HLA-identical sibling donor. Older patients are routinely transplanted but results become progressively worse with age and an upper age Limit of 55 years is usually applied.
Sources and storage of cells
To limit the risks of transplanted stem cell rejection or of severe gravt-versus- host diseas in allogeneic HSCT, the donor should preferably have the same human leukocyte antigens(HLA) as the recipient. About 25 to 30 percent of allogeneic HSCT recipients have an HLA-identical sibling. Even so-called "perfect matches" may have mismatched minor alleles that contribute to graft-versus-host disease
Bone marrow: in the case of a bone marrow transplant, the HSC are removed from a large bone of the donor, typically the pelvis , through a large needle that reaches the center of the bone. The technique is referred to as a bone marrow harvest and is performed under general anesthesia.
Peripheral blood stem cells: are now the most common source of stem cells for allogeneic HSCT. They are collected from the blood through a process known as apheresis. The donor's blood is withdrawn through a sterile needle in one arm and passed through a machine that removes white blood cells. The red blood cells are returned to the donor. The peripheral stem cell yield is boosted with daily subcutaneous injections of Granulocyte colony stimulating factor, serving to mobilize stem cells from the donor's bone marrow into the peripheral circulation.
Complications
These are outlined in Boxes 24.28 and 24.29.The risks and outcomes of transplant depend on several Patient and disease –related factors. In general 25% die from procedure –related complications Such as graft-versus host disease, and there remains. A significant risk of disease relapse The long term survival for patients undergoing allogeneic BMT in acute leukaemia is around 50%
Gravt-versus- host disease(GVHD)
This is due to the cytotoxic activity of donor T lymphocytes which become sensitized to their new host, regarding it as foreign. This may cause either an acute or chronic Form of GVHD.
Acute GVHD
This occur n the first 100 days after transplant in about One- third of patients ,manifested by symptoms in the Skin, GIT & liver. Skin manifestations range from a maculopapular rash to generalized erythroderma or desequamation. Liver manifestation in form of jaundice. GIT manifestation inform of diarrhoea.
Patients who receive transplant from unrelated donors are at increased risk , and the incidence and severity GVHD rise with age of the patient.
Prevention: 1-HLA-matching of the donor. 2-immunosuppressant drugs including methotrexate and cyclosporin, and antithymocyte globuline.
Treatment: 1-high-dose corticosteroids 2-antithymocyte globulin 3-or various monoclonal Abs
Chronic GVHD: May follow acute GVHD or arise independently. Occurs more than 100days after the transplant and is most likely to develop in older patients who also have acute GVHD. Symptoms include the sicca syndrome, chronic sinusitis Rashes, scleroderma –like skin thickening, diarrhea, wasting Syndrome and liver abnormalities.
Treatment with corticosteroids and immunosuppression e.g. cyclosporine
Reduced-intensity BMT :
Rather than use very intensive conditioning which causes Morbidity from organ damage, relatively low doses of Drugs such as fludarabine and cyclophosphamide are used Simply to immunosuppress the recipient and allow donor Stem cells to engraft.The emerging donor immune system then eliminates the Malignant cells via the graft versus disease effect, which May be boosted by the elective use of donor T-cells infusion Post transplant.
This type of transplant is less toxic and allows BMT to be offered to an older group of patients However, relapse and infection post transplant Remain a concern and the role of this type of Transplant is still under investigation.
Syngeneic BMT: Which occurs in about 1% of transplants, is the special Rare cases of donor and a recipient who are genetically Identical twins.
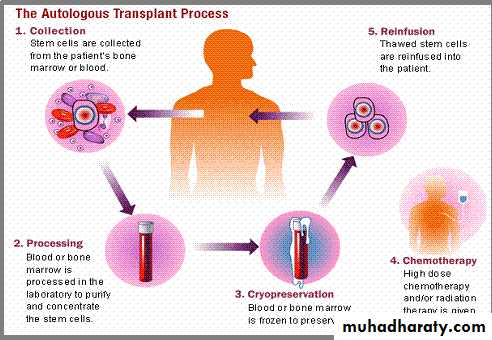
Autologous
Autologous HSCT requires the extraction (apheresis) of haematopoietic stem cells (HSC) from the patient and storage of the harvested cells in a freezer. The patient is then treated with high-dose chemotherapy with or without radiotherapy with the intention of eradicating the patient's malignant cell population at the cost of partial or complete bone marrow ablation (destruction of patient's bone marrow function to grow new blood cells)The patient's own stored stem cells are then transfused into his/her bloodstream, where they replace destroyed tissue and resume the patient's normal blood cell production.
Autologous transplants have the advantage of lower risk of infection during the immune-compromised portion of the treatment since the recovery of immune function is rapid. Also, the incidence of patients experiencing rejection (graft-versus-host disease) is very rare due to the donor and recipient being the same individual
The Transplant Procedure
Marrow is usually collected from the donor's posterior and sometimes anterior iliac crests, with the donor under general or spinal anesthesia. Typically, 10–15 mL/kg of marrow is aspirated, placed in heparinized media, and filtered through 0.3- and 0.2-mm screens to remove fat and bony spicules.The collected marrow may undergo further processing depending on the clinical situation, such as the:
1- removal of red cells to prevent hemolysis in ABO-incompatible transplants.
2- the removal of donor T cells to prevent GVHD. 3- attempts to remove possible contaminating tumor cells in autologous transplantation. Marrow donation is safe, with only very rare complications reported
Peripheral blood stem cells are collected by leukapheresis after the donor has been treated with hematopoietic growth factors or, in the setting of autologous transplantation, sometimes after treatment with a combination of chemotherapy& growth factors.
Stem cells for transplantation are generally infused through a large-bore central venous catheter. Such infusions are usually well tolerated, although occasionally patients develop fever, cough, or shortness of breath. These symptoms usually resolve with slowing of the infusion.
Engraftment
Peripheral blood counts usually reach their nadir several days to a week posttransplant as a consequence of the preparative regimen; then cells produced by the transplanted stem cells begin to appear in the peripheral blood. The rate of recovery depends on the source of stem cells, the use of posttransplant growth factors, and the form of GVHD prophylaxis employed. .
If marrow is the source of stem cells, recovery to 100 granulocytes/ L occurs by day 16 and to 500/ L by day 22. Use of G-CSF–mobilized peripheral blood stem cells speeds the rate of recovery by ~1 week when compared to marrow.
Storage of HSC: Unlike other organs, bone marrow cells can be frozen (cryopreserved) for prolonged periods without damaging too many cells.
This is a necessity with autologous HSC because the cells must be harvested from the recipient months in advance of the transplant treatment. In the case of allogeneic transplants, fresh HSC are preferred in order to avoid cell loss that might occur during the freezing and thawing process
Conditioning regimens: Myeloablative transplants: The chemotherapy or irradiation given immediately prior to a transplant is called the conditioning regimen, the purpose of which is to help eradicate the patient's disease prior to the infusion of HSC and to suppress immune reactions. The bone marrow can be ablated (destroyed) with dose-levels that cause minimal injury to other tissues. In allogeneic transplants a combination of cyclophosphamide with total body irradiation is conventionally employed.
Graft rejection
Occurs when immunologically competent cells of host origin destroy the transplanted cells of donor origin. This complication is rare after a fully matched, related donor transplant and occurs more commonly in patients who receive transplant from alternative donor or in T cell-depleted transplant. It is less likely in non-transfused patients with aplastic anemia.
Prognosis
Prognosis in HSCT varies widely dependent upon: disease type- stage- stem cell sourceHLA-matched status (for allogeneic HCST) and conditioning regimen.
A transplant offers a chance for cure or long-term remission if the inherent complications of graft versus host disease, immuno-suppressive treatments and the spectrum of opportunistic infections can be survived. In recent years, survival rates have been gradually improving across almost all populations and sub-populations receiving transplants.