Knee Disorders
Dr, Sadeq Al-MukhtarConsultant orthopedic surgeon
Clinical assessment:
Symptom:-Pain: The most common knee symptom. It may be diffuse with inflammatory degenerative disorders or localized with mechanical disorders. The patient must describe the mechanism of injury. Twisting injuries are more likely to cause a torn meniscus or a cruciate ligament rupture
Stiffness: Post-inactivity stiffness suggest arthritis.
Locking: The knee, quite suddenly, cannot be straightened fully although flexion is still possible; happens when a torn meniscus or loose body caught between the articular surfaces.Deformity; Knock knee especially if unilateral.
Swelling; may be localized or diffuse. Time of occurrence is important, if immediately after trauma, it suggest a haemoarthrosis , or only after some hours (typical of torn meniscus).Giving way; Suggest a mechanical disorder although it can result from muscle weakness; when it occurs particularly on stair, the patellofemoral joint defect is suspect.
Limp; may be due to either pain or instability.
Signs:
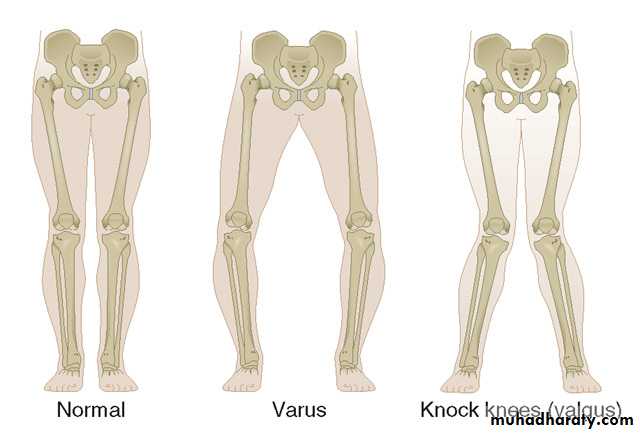
With patient upright;Look varus, valgus deformities.
On walking look for instability.
With the patient lying supine:
Look;for skin colour, sinuses, or scar.
Wasting of the quadriceps ( sign of joint disorder).
Measuring the girth of the thighs (at same level of both sides)..
Shape of patella compared with opposite side.
Position of the knee, varus or valgus, flexed or hyperextended position
Feel; of the patella.
Increased warmth (comparison), the temperature gradient.Feel, the joint line at 90 degrees of flexion.
Check intra-articular fluid.
Four useful tests:
Cross fluctuation test:
Patellar tap test:
Bulge test: Used when little fluid is present, medial side compression notice refilling again.
The patellar hollow test: Used when very little fluid is present. On flexion of knee, normally a hollow appears lateral to the patellar ligament and disappear with further flexion, if fluid present the hollow fills and disappear at a lesser angle of flexion.
Movement;
Flexion and extension: Normally the knee flexes until calf meet the ham. Crepitus during movement may be felt with the hand placed on the front of the knee.Varus and valgus stress during flexion ( pain here suggest articular cartilage softening in one or other compartment). Cartilage is insensitive and pain is due to pressure on subchondral bone.
Rotation: Flexion of hip and knee to 90 degrees. One hand rotate the foot, the other steadies and feel the knee (normal range for internal and external rotation is about 10 degrees
Tests for stability:
The collateral ligaments; varus and valgus stress in full extension ,and in 30 degrees flexion, normally there is some mediolateral movement, but if excessive (compared to the normal side), it suggest a torn collateral ligament.Sideway movement is always abnormal, may be due to:
Torn or stretched ligament and capsuleLoss of articular cartilage or bone.
The cruciate ligaments:
Flexion of both knees to 90 degrees, the feet resting on the couch, the upper tibia is inspected from the side, if the upper end has dropped back or can be gently pushed back, it indicate posterior cruciate ligameht injury (Sag sign) .
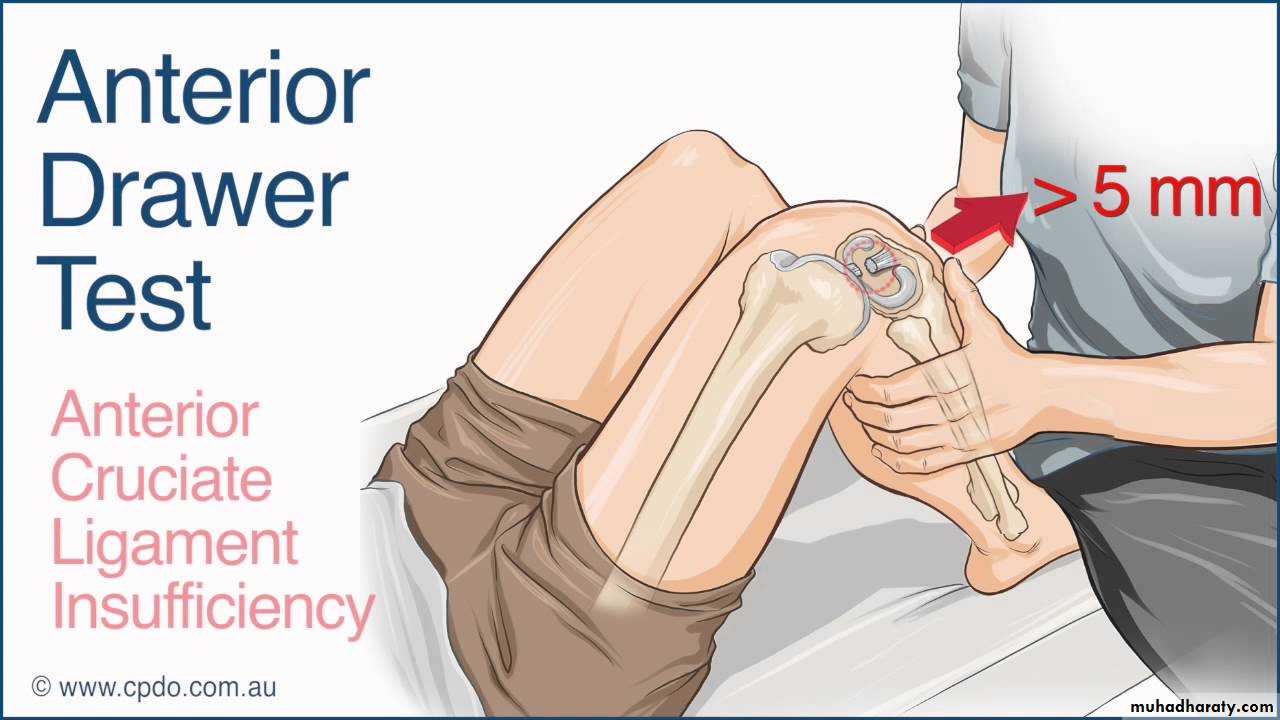
In the same position the foot anchored by the examiner sitting on it, using both hands the upper end of tibia is grasped firmly and rocked backward and forward to see if there is any glide ( Drawer test). Excessive anterior movement (positive anterior drawer test) denotes anterior cruciate ligament laxity . Excessive posterior movement (positive posterior drawer test), signifies posterior cruciate laxity
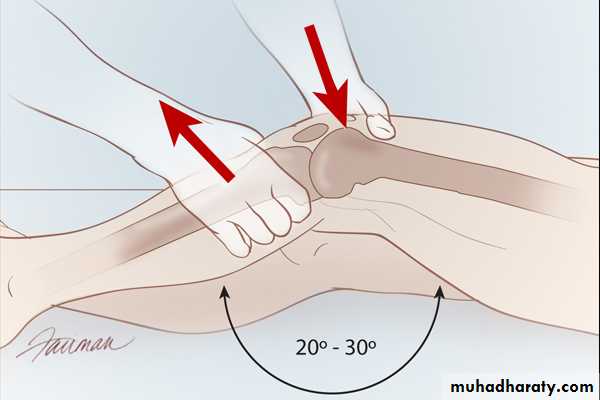
Lachman test:
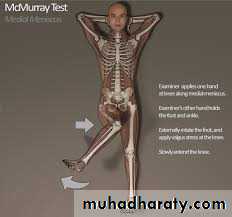
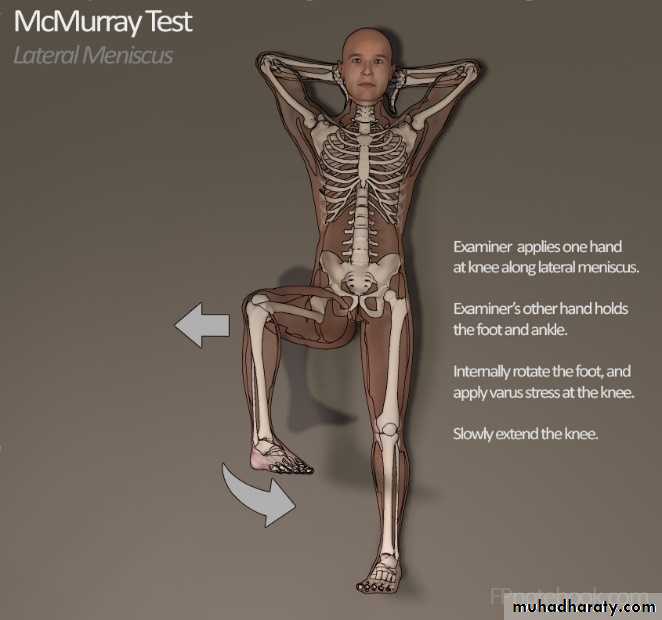
A more sensitive test. The patient’s knee is flexed to 20 degrees with one hand grasping the lower thigh and other, the upper part of the leg the joint surfaces are shifted backward and forward upon each other, if the knee is stable, there should be no glidingMcMurray’s test:
This is a classic test for a torn meniscus and is based on the fact that the loose tag can sometime trapped between articular surface and then induced to snap free with a palpable and audible click.The knee is flexed as far as possible , one hand steadies the joint and the other rotates the leg medially and laterally while the knee is slowly extended, the test is repeated several times with the knee stressed in valgus and varus, feeling and listening for the click.
A positive test is helpful but not pathognomonic; a negative test does not exclude a tear.
Signs with the patient lying prone:
See if there is any scar or lump in the popliteal fossa. If there is a swelling, is it in the midline (most likely a bulging capsule) or to one side (possibly a bursa). The popliteal fossa is carefully palpated. If there is a lump, where does it originate? Does it pulsate? Can it be emptied into the joint?Investigations:
X-ray:Anteroposterior and lateral (standing position),
skyline (patellofemoral),
tunnel views (intercondylar).
Both knees should be x-rayed to compare the abnormal with the normal side.
Radioscintigraphy: May show increased activity in the subarticular bone in early osteoarthritis, also in showing hot spots due to infection after joint replacement.
Computed-tomography C.T: Patellofemoral congruence at various angles of flexion.
MRI : for detection meniscal injuries or osteochondral lesions.
Knee arthroscopy:
A direct “look inside” is not a substitute for clinical examination; a detailed history and meticulous assessment of the physical signs are very important for diagnosis. Arthroscopy shows too much and the clinician will still have to decide which of the abnormalities detected are the cause of the patients complains. Depending on the patients age and the likely diagnosis, different aspects of the examination need to be emphasized.Adolescents with anterior knee pain are usually found to have chondromalacia patellae, patellar instability, osteochondritis or a plica syndrome. But remember –knee pain may be referred from the hip.
Young adults engaged in sports are the most victims of meniscal tears and ligament injuries.
Patients above middle age with chronic pain and stiffness probably have osteoarthritis.
Deformities of the knee:Genu valgum; Knock knee
Genu varum; Bow legs.
Genu recurvatum; Hyper-extended knee
Bow legs and knock knees in children:
Bilateral bow legs can be recorded by measuring the distance between the knees with the child standing and the heels touching. It should be less than 6 cm, similarly.knock knee can be estimated by measuring the distance between the medial malleoli when the knees are touching with the patellae facing forwards, it is usually less than 8 cm.
Bow legs in babies and knock knees in 4-years old are so common that they are considered to be normal. The parents should be reassured and the child should be seen at interval of 6 months to record progress.
By the age of 10 years, if the deformity is still marked (intercondylar distance more than 6 cm or intermalleolar distance more than 8 cm,
operative correction should be adviced and include:-
Stapling of the physes( the staples are removed once the knee has overcorrected slightly).Hemi-epiphysodesis: Fusion of one-half of the growth plate on the convex side of the deformity.
Encourage the child and the parents to put up with the deformity until growth is complete and then undergo a corrective osteotomy (supracondylar osteotomy for valgus and high tibial osteotomy for varus knees).
Pathological bow legs and knock knees
Disorders which causes distorted epiphyseal and/or physeal growth may give rise to these deformities:-Skeletal dysplasias.
Various types of rickets.
Injuries of epiphysis and physeal growth cartilage
Genu varum and valgum in adult:
It may be :
A sequel to childhood deformity.
Associated with joint instability, this can lead to osteoarthritis of medial compartment in varus and lateral compartment in valgus. Genu Valgum may cause abnormal tracking of patella and predispose to patellofemoral osteoarthritis.
The deformity may be secondary to arthritis, usually varus in osteoarthritis and valgus in rheumatoid arthritis.
Ligament injury,
malunited fracture,
and pagets disease
Genu recurvatum:
Congenital: Abnormal intrauterine posture, it usually recovere spontaneously. Gross genu recurvatum is the precursor of true congenital dislocation of the knee.Lax ligaments: Normal people with generalized joint laxity tends to stand with their knees back-set.., especially rheumatoid arthritis.
Prolonged traction.
Holding the knee hyperextension in plaster of paris. Following chronic or recurrent synovitis (Rheumatoid arthritis).
Hypotonic of rickets.
Poliomyelitis flailness.
Insensitivity of Charcots disease.
Growth plate injuries.
Malunited fractures.
MENISCUS LESIONS:
Function of meniscus:Improving articular congruency and increasing the stability of the knee
Controlling the complex rolling and gliding action of the joints.
Distributing load during movement during weight bearing.
The medial meniscus is much less mobile than the lateral. This may be why meniscal lesions are more common on the medial side than lateral. Even in the absence of injury, there is gradual stiffness and degeneration of the menisci with age, so splits and tears are more likely in later life.
Mechanisms of injury:
Usually young male presented at age of 14 years, or teenager foot-ball player. The criteria for injury is:Weight bearing.
Knee flexion.
Internal or external rotation.
Clinical features:
History of twisting trauma to the knee with severe pain, effusion after few hours (the content of the fluid is synovial not blood because the meniscus is avascular).The signs includes, effusion, localized tenderness at joint line, locked knee.Test:
McMurry test.Treatment
Conservative: In acute episode, the joint is held straight in a plaster backslab for 3-4 weeks; and quadriceps are encouraged.Operative: Surgery is indicated
If the joint cannot be unlocked.
if symptoms are recurrent.
Through diagnostic arthroscopy , tears closer to the periphery, which have the capacity to heal, can be sutured, the success rate for open and arthroscopic repairis almost 90%.
Tears other than those in the peripheral third are dealt with by excising the torn portion.
Total meniscetomy is thought to cause more instability and predispose to later osteoarthritis.
Recurrent dislocation of the patella
About 15-20% of cases of acute dislocation of patella is followed by recurrent dislocation or subluxation after minimal stress. It is now recognized that in all cases of recurrent ,one or more predisposing factors are often present:Generalized ligament laxity.
Underdevelopment of the lateral femoral condyle and flattening of the intercondylar groove.Maldevelopment of the patella, which may be too high or too small.
Valgus deformity of the knee.
External tibial torsion.
A primary muscle defect.
Repeated dislocation damages articular surfaces of the patella and femoral condyle.
Dislocation is almost always towards the lateral side
Clinical features:Girls are affected more commonly and the condition may be bilateral.
Dislocation occurs unexpectedly when the quadriceps muscle is contracted with the knee in flexion. There is acute pain, the knee is stuck in flexion and the patient may fall to the ground.
Tenderness and swelling may still be present and the apprehension test is positive ( if the patella is pushed laterally with the knee slightly flexed, the patient resists and becomes anxious, fearing another dislocation )
Investigations:
X-rays:
may reveal loose bodies.
Lateral view with slight flexion may show a high-riding patella,
and tunnel view can be used to measure the sulcus angle.
MRI : is helpful and may show signs of previous patellofemoral soft-tissue disruption.
Treatment:
If the patella is still dislocated, it is pushed back into place, while the knee is gently extended.The only indications for immediate surgery are:
inability to reduce the patella.the presence of a large , displaced osteochondral fragment.
A plaster cylinder is applid for 2-3 weeks.
Exercise should be continued for at least 3 months,
if recurrence are few and far between, conservative treatment may suffice; as the child grows older the patellar mechanism tends to stabilize.
If repeated episodes(15%), surgical reconstruction is indicated.
Anterior Knee Pain Syndrome AKPS
It is common among active adolescents and young adults. It is often associated with softening and fibrillation of the articular surface of patella “Chondromalacia patellae”.The basic disorder is mechanical overload of the patellofemoral joint, mostly due to repetitive overload due to either:
malcongruence of patellofemoral surfaces because of some abnormal shape of the patella or intercondylar groove,or
malalignment of the extensor mechanism, or relative weakness of vastus medialis, which causes the patella to tilt,or subluxate, or bear more heavily on one facet than the other during flexion and extension”overload”
Causes of AKP :
Patellofemoral overload (maltracking and overuse).Patellar instability (patellar subluxation and patellar tilt).
Intra-articular pathology (plica syndrome, meniscal disorders, osteochondritis dissecans, and patellofemoral arthritis).
Peri-patellar disorders (bursitis, tendinitis, and apophysitis).
Referred pain (hip disorders, e.g slipped femoral epiphysis).
Clinical features:
The patient, often a teenager girl or an athletic adult, complains of pain over the front of the knee or underneath the kneecap. Symptoms are aggravated by activity or climbing stairs, or standing up after prolonded sitting, wastig of quadriceps, knee effusion, and tenderness under the edge of the patella. The apprehension test is positive.Imaging:
X-ray examination should include skyline views of the patella, and lateral view with the knee half-flexed to see if the patella is high or small.C.T and MRI is very important in diagnosis.
Arthroscopy: It is useful in excluding other causes of AKPS. It can also serve to gauge patellofemoral congruence, alignment, and tracking.
Treatment:
Consevative: In the vast majority of cases the patient will be helped by adjustment of stressful activities and physiotherapy.
Surgery:
Indications ;
Failure of conservative treatment after 6 months.
There is a demonstrable abnormality that is correctable by operation.
Chondromalacia Patellae:
It is an erosion, of the hyaline articular cartilage undersurface of the patella and is characterized by a vague, aching pain under or around the knee-cap "patella". The patient may note a grinding or rubbing under the kneecap. Prolonged sitting with the knee flexed at 90 degrees, kneeling, squatting, and stair climbing accentuate the painLoose bodies:
These may be produced by:Osteochondritis dissecans, which may produce one or two fragments).
Osteoarthritis (piece of cartilage or osteophyte).
Injury (a chip of bone or cartilage).
Charcot s disease (a large osteocartilagnous bodies).
Synovial chondromatosis (cartilage metaplesia in the synovium, sometimes producing hundreds of loose bodies).
Clinical features:
May be asymptomatic.The usual complaint is attacks of sudden locking without injury.
The patient maybe aware of some thing ”popping in and out of the joint”.
In adolescents, loose body is usually due to osteochondritis dissecans, rarely to injury.
In adults, osteoarthritis is the most common cause.
X-ray: Most loose bodies are radio-opaque. The films also show an underlying joint abnormality.
The plica syndrome:
It is the remnant of an embryonic synovial partition which persists into adult life. It is present in over 20% of people, usually as a median infrapatellar fold. Patient usually complains of an ache in the front of the knee with intermittent episodes of clicking or giving way. The most characteristic feature is tenderness near the upper pole of patella and over the femoral condyle as a significant cause of anterior knee pain.Diagnosis by arthroscopy.
Swelling of the knee:-Acute swelling:Post-traumatic haemoarthrosis:
Immediately after injury.The knee is very painful.
It feels warm, tense and tender.
Later , there may be a dought feel.
Movement are restricted.
X-rays are essential to see if there is a fracture.
Treatment: The joint should be aspirated under aseptic condition. Treat the cause ”ligament injury”. In general crepe bandage is applied anduse back –splint, quadriceps exercises are practiced from the start.
Bleeding disorders;
Avoid aspiration if the clotting factor is not available, the knee is splinted in slight flexion until the swelling subsides.Acute septic arthritis.
Traumatic synovitis:
Typically the swelling appears only after some hours, and subsides over a period of days.Knee splint for several days.
Encourage movement and quadriceps exercise.
Treat internal knee injury.
.
Aseptic non-traumatic synovitis:
Acute swelling without a history of trauma or sign of infection.
Think of gout or pseudogout.
The synovial fluid look turbid, resembling pus, but it is sterile.
Microscopy reveals the crystals.
Treatment by anti-inflammatory drugs
Chronic swelling of the joint:
Arthritis: Osteoarthrits and rheumatoid arthritis.Synovial disorders; Like tuberculosis, synovial chondromatosis ,and pigmented villonodular synovitis
Swelling in front of the joint:
Prepatellar bursitis( housemaid s knee): treatment consist of firm bandaging, and kneeling is avoided. occasionally aspiration is needed. In chronic cases the lump is best excised.Infrapatellar bursitis; the swelling is bellow the patella and superficial to the patellar ligament, treatment same like above.
Other bursae
Swelling at the back of the knee:
Semimembranosus bursa.
Popliteal cyst.
Popliteal aneurysm.
Bony swelling around the knee:
Cartilage-capped exostosis ”osteochondromata”.Osgood-Schlatters disease ”apophysitis” of the tibial tubercle.A common disorder of adolescence, the tibial tubercle become painful and swollen, tender. Sometimes bilateral. X-ray reveal fragmentation of the apophysis
Rupture of the extensor apparatus:Resisted extension of the knee may tear the extensor mechanism:
Rupture above patella.
Rupture below patella.
Osgood Schlattrer disease.
Principles of knee operations:
Arthroscopy; UsesTo establish or refine the accuracy of diagnosis.
To help in deciding whether to operate.
To perform certain operative procedures.
Ligament reconstruction:
The collateral and cruciate ligaments and the knee capsule are important constrains which allow normal knee function; laxity or rupture of these structures either singly or in combination, is often the sourse of recurrent episodes of giving way. Although a significant proportion of such injuries are treated non-operatively, complete ruptures may require surgery in high-demand individuals.Repair.
Substitution; usually for anterior cruciate ruptures, the semitendonosus can be carefully anchored to the femur and tibia ensuring that stability is restored.
Tenodesis.
Arthrodesis
Knee replacement:
Indications: The main indication of knee replacement is pain associated with deformity and instability. Most replacements are performed ror rheumatoid and osteoarthritis.
Types:
Partial replacement.Total replacement:
Minimally constrained total replacement: used for prosthesis where some of the stability after replacement is provided by the prosthesis and some through preservation of the knee ligaments, you can sacrifice one or both cruciate ligaments.
Constrained joints: used when there is marked bone loss and severe instability. It provide mobile joint after resection of tumours at the bone ends.