
or
hysterosalpingography
Asherman`s syndrome) can be a cause and diagnosed by a
be the cause. Uterine synechiae
vical stenosis may
such as hymenal or cer
only spotting. An obstruction
Sometime
scanty menstruation.
rhoea:
Hypomenor
indication of malignant tumors or pregnancy complications.
lead to menometrorrhagia. Sudden onset of irregular bleeding episodes may be an
Any cause of intermenstrual bleeding can
amount and duration of bleeding also vary.
The
gular intervals.
eeding at irre
Prolonged or excessive b
Menometrorrhagia:
Exogenous estrogen may be a cause.
Endometrial polyps, endometrial and cervical carcinomas are pathological causes.
occurs at midcycle as spotting and can be documented with basal body temperatures
ying amounts but not excessive. Ovulatory bleeding
of var
regular menstruations
episodes of uterine bleeding between
ual bleeding
Intermenst
rhagia
Metror
may be the cause.
mors and dysfunctional bleeding
hyperplasias, malignant tu
IUCDs, endometrial
ions of pregnancy, adenomyosis
, complicat
fibroid
Submucous
coital bleeding.
over several consecutive cycles without any intermenstrual or post
ntervals
Excessive (>80 ml) & / or prolonged menstruation, at regular
Menorrhagia:
n the menstrual cycle.
luteal phase i
lation and rarely with a shortened
This is usually is associated with anov
intervals
regular
at
Described periods that occurs too frequently (<21 d)
Polymenorrhoea:
CLINICAL TYPES
80 ml
Volume: 30
Duration: 3
Frequency: 21
ENSES
NORMAL
and cervical cancer.
fibroid
uterine
eg.
than one entity may be present, such as
more
d, and always remember that
complication of pregnancy must always be considere
ina, urethra, or rectum. In child bearing women, a
of the bleeding from the vag
most difficult problems in gynecology. Patient may not be able to localize the source
ne bleeding present some of the
The diagnosis and management of abnormal uteri
reproductive age.
truation in women of
Any deviation in normal frequency, duration or amount of mens
DEFINITION:
general practitioner
Abnormal uterine bleeding is a common reason for women of all ages to consult their
the management options of AUB.
Analyze
g to specific age group.
Correlate the cause of bleedin
Determine the causes behind HMB (heavy menstrual blood loss).
Describe the causes of ABU.
List the clinical types of AUB.
Define AUB.
Learning objectives: By the end of this lect. You need to:
(AUB)
bnormal uterine bleeding
۱
A
1-
2-
3-
4-
5-
6-
•
.
•
•
M
:
•
-35 d
•
-7 d
•
-
:
.
u
I
,
(
r
):
.
l
(
Genital disease:
disease, placenta previa and abruptio placenta.
Abortion, Ectopic pregnancy, Trophoblastic
Pregnancy complications:
Dysfunctional uterine bleeding
of AUB:
USES
necessary.
invasive cancer, and colposcopy, biopsy, or both may be
not rule out
smear does
negative cytological
vaginal infection (eg, trichomonas), or atrophic vaginitis. A
her much common causes are cervical erosion, cervical polyp, cervical or
otherwise, ot
must be considered as a signs of cervical cancer until proved
Postcoital bleeding
causes, menopause) or systemic causes ( eg, excessive weight loss).
hypothalamic
, either from endocrine cause (eg, pregnancy, pituitary
novulation
iated with
assoc
. Usually
no menstrual period occurs for more than 6 months
is diagnosed if
amenorrhoea
(but
infrequent menstruation (>35 d)
Oligomenorrhea:
flow and can be reassured that this is not significant.
ral contraceptives occasionally complain of light
hysteroscope. Patients received o
۲
.
)
a
-
:
CA
1-
2-
3-
d), adenomyosis.
Benign: fibroid, polyps (cervical, endometrial, fibroi
Tumors:
.
secreting)
Malignant: cervical, endometrial, ovarian (estrogen
PID, cervicitis and endometritis.
Infection:
.
foreign
: laceration, abrasion
Trauma
.
,
body.
IUCD
.
genital:
Extra
4-
g's disease, Polycystic
mia, Cushin
thyroidism, Hyperprolactine
Endocrine
.
: hypo
Willebrand disease,
: Idiopathic thrombocytopenic purpura, Von
Haematological
syndrome, Adrenal dysfunction/tumor.
varia
O
n
.
-
: liver failure, renal failure, hypertension with uterine
Chronic systemic disease
.
therosclerosis.
artery a
( progestogen only contraception, IUCD)
: Sex hormones
Iatrogenic
.
,
anticoagulants.
: may be emotional as (change of country, climate & work; psychosomatic
Stress
.
disorders) or may be due to excessive exercise.
eripheral estrogen conversion]
: [increased p
Obesity
.
New classification of abnormal uterine bleeding:
dysfunctional uterine bleeding
Bleeding of endometrial origin (replace
eplace menorrhagia).
HMB
Heavy menstrual bleeding
1-
(r
2-
Prevalence and impact:
the leading indication for hysterectomy
and
system, being one of the most frequent indication for abstinence from work
complaint result in significant morbidity, has economical burden on the health
1/ 3 women of reproductive age. This
affects
HMB
ding
Heavy menstrual blee
(
)
۳
Causes of HMB :
usually associated with submucosal and intramural fibroids.
Fibroids:
1-
with
are common and sometime cause intermenstrual bleeding
Polyps:
2-
uterine fibroids.
polypoidal
increased volume of bleeding with
systemic
n with HMB will have
% of wome
: around 10
Coagulopathy
3-
-20
thrombocytopenia.
cquired condition as sever
ent. A
oung age or not respond to medical treatm
in 13% of women with HMB which should be considered in those present at
mild to moderate), especially von Willebrand’s which found
rder varies (
diso
disorder of haemostasis, which are inherited or acquired and the severity of
y
potential cause of
carcinomas are
Both endometrial and cervical
Malignancy
4-
:
bleeding.
abnormal
premalignant condition also may present with
hyperplasia which is
and rarely HMB. Endometrial
intermenstrual and postcoital bleeding
that typically
cause anovulation
idis
hypothyr
Untreated
Thyroid disease:
5-
o
m
present with amenorrhoea but sometime associated with HMB.
with abnormal
iate
assoc
chronic endometrial infection may
Pelvic infection:
6-
could be a cause of HMB
uterine bleeding both intermenstrual and heavy. Chlamydia Trachomatis
.
which are congenital or acquired
(AVM)
Arteriovenous malformation
7-
:
diagnosis.
curettage after pregnancy. Colour Doppler imaging may be helpful in the
Congenital AVM are rare but acquired type may follow uterine
bleeding.
occur in the uterus they have been associated with episodes of acute excessive
When they
veins
localized collection of abnormally connected arteries and
.
an with thromboembolic
ing anticoagulant drugs in wom
like us
Iatrogenic:
8-
inflammatory process).
he effect is through the local
cupper intrauterine contraceptive devices (t
ovarian axis) and
pituitary
hypothalamic
by prolactin related disruption of
disorder, tricyclic antidepressants and phenothiazines which affect ovulation
(
-
–
in the majority of the cases of HMB, it is
Bleeding of endometrial origin:
9-
prostaglandins, endothelins and nitric oxide.
and include
regulate vascular tone inside the uterus may play a role
by exclusion. The exact endometrial mechanism still unknown, factors which
which is diagnosed
previously called DUB (dysfunctional uterine bleeding
probable that the bleeding lies at the level of endometrium itself. This
)
50 %.
HMB and reduce blood loss by 40
fibrinolytic activity so antifibrinolytics commonly prescribed for complaint of
having increase
omen with HMB
lesser need for coagulation. W
e is
ther
so
Since menstrual loss is mainly controlled by vasoconstriction
HMB
inhibitors is the first line treatment during menses for women with
Cyclooxygenase
the endometrium of women with HMB so administration of
in
crease level of prostaglandins
arly researches in this field demonstrate in
E
(COX)
.
-
Summery for the causes of HMB
:
Don’t forget iatrogenic causes.
Malignancy should always be excluded.
20% of cases
athies may account for 10
Coagulop
In most women no cause will found.
1-
2-
-
.
3-
4-

al uterine bleeding in premenopausal women
of abnorm
Anovulation and its related progesterone deficiency is the leading cause
likely
most
bleeding of endometrial origin
f normal physical exam, anovulatory
Hematologic
PCOS
infection
Adenomyosis
Fibroids
Polyps
Pregnancy
Anovulation (90%)
Etiol
identifying the etiology of anovulation.
secondary to anovulation, and the diagnostic investigation is targeted at
origin
bleeding of endometrial
the most likely diagnosis is
ultrasound will be needed,
cytological examination and pelvic
ination,
normal findings on physical exam
with
the pathological causes are not common
In premenopausal women
menopausal AUB
Pre
performed to exclude pregnancy or pathological conditions
amination not possible in case she is unmarried, so pelvic ultrasound must be
and pelvic
Invasive diagnostic procedures are usually not necessary
needed.
be
treatment that is necessary. But if the bleeding is heavy then treatment will
s all the
, and explanation of the reason i
So the menses not unusually are irregular
Infection
Medical illnes
von Willebrand’s
, e.g.
menorrhagia have a bleeding disorder
Up to 20 % presenting with
Hematological
Pregnancy
Anovulation (90%)
Adolescents
Sexual abuse
Precocious puberty, neoplasm
Rare
rologic
Trauma, FB, vulvovaginitis, u
Most common :
Always abnorma
Menarchal
Pre
menopausal
Post
menopausal
Peri
Adolescence & later
menopausal
Pre
menarchal
Pre
Approach based on age
٤
AUB:
–
-
–
-
•
–
-
–
-
-
:
•
l
•
–
•
–
•
:
•
•
•
–
•
s
•
ex
-
•
•
ogy
–
–
–
–
–
–
–
–
– IUCD
• I
.
.
How:
4. Impact of the bleeding on the woman’s quality of life.
Ovulatory or anovulatory
Exclusion of organic causes
Nature & severity of bleeding
Aim:
of AUB
Diagnosis
( Hormone replacement therapy)
Fibroids
cervical c
hyperplasia
Endometrial
Atrophy of vagina, EM
carcinoma
Endometrial
Etiology
initial investigation.
group, endometrial biopsy or transvaginal ultrasonography is included in the
menopausal women with abnormal uterine bleeding. Thus, in this age
post
Uterine pathology, particularly endometrial carcinoma, is common in
menopausal AUB
Post
cancer
Endometrial
hyperplasia
Endometrial
Anatomic (fibroids, adenomyosis, polyps)
Anovulation
Etiology
therapy started.
hould be assured before hormonal
. And the cause of bleeding s
investigation
endometrial hyperplasia or carcinoma must be considered early in the
In perimenopausal patients, endometrial biopsy and other methods of detecting
menopausal AUB
Peri
٥
-
:
•
•
–
–
–
–
-
:
•
•
–
–
–
–
a
–
– HRT
1.
2.
3.
. History
I
:
Sexual history, contraceptive use and fertility wishes need to be determined.
r only a variation of normal.
her bleeding is abnormal o
determine whet
any change in general health. The patient must keep a record of bleeding patterns to
Note also the last normal menstrual period, age of menarche and the menopause, and
should raise the possibility of coagulation disorders.
story of bleeding
family hi
or
bleeding or bleeding associated with dental work, bruising, frequent epistaxis
Excessive bleeding since menarche, postpartum haemorrhage, surgery related
include bowel and urinary symptoms can indicate the presence of large fibroid
symptoms
anatomical causes, while pressur
usually suggest
or postcoital bleeding
ntermenstrual bleeding
. I
and the influence on the quality of life
amount of episodes
Note the amount of menstrual flow, the length of menstrual cycle, the length and
iated symptoms
assoc
relation to sexual intercourse and
smell,
, duration, color,
and clots indicate significant loss
(flooding
Present: amount
Past
Obstetric
to determine the amount and timing of the bleeding
calendar
Menstrual
al: age, wishes of the patient
Person
1.
2.
3.
4.
5.
)
.
ed
e
.
٦
Examination
II.
:
s).
give a symmetrically enlarged uteru
or endometrial carcinoma (where both can
, adenomyosis
irregular enlarged uterus)
fibroids
eveal enlargement from uterine
examination may r
uterine
imanual
can be seen, discharge can indicate infection.
of the cervix
invasive lesio
polyps and
visualized;
inflammatory vulvar and vaginal lesions can be
atrophic and
: lesions, lacerations,
rigin of the bleeding as Pelvic
To see the
Pelvic:
liver, spleen, pelvi abdominal mass
Abdominal:
, reflexes
and
largement, bruising
thyroid en
pallor, endocrinopathy, coagulopathy, pregnancy, hirsutism, acne, galactorrhea,
General:
1.
2.
3.
o
n
B
(
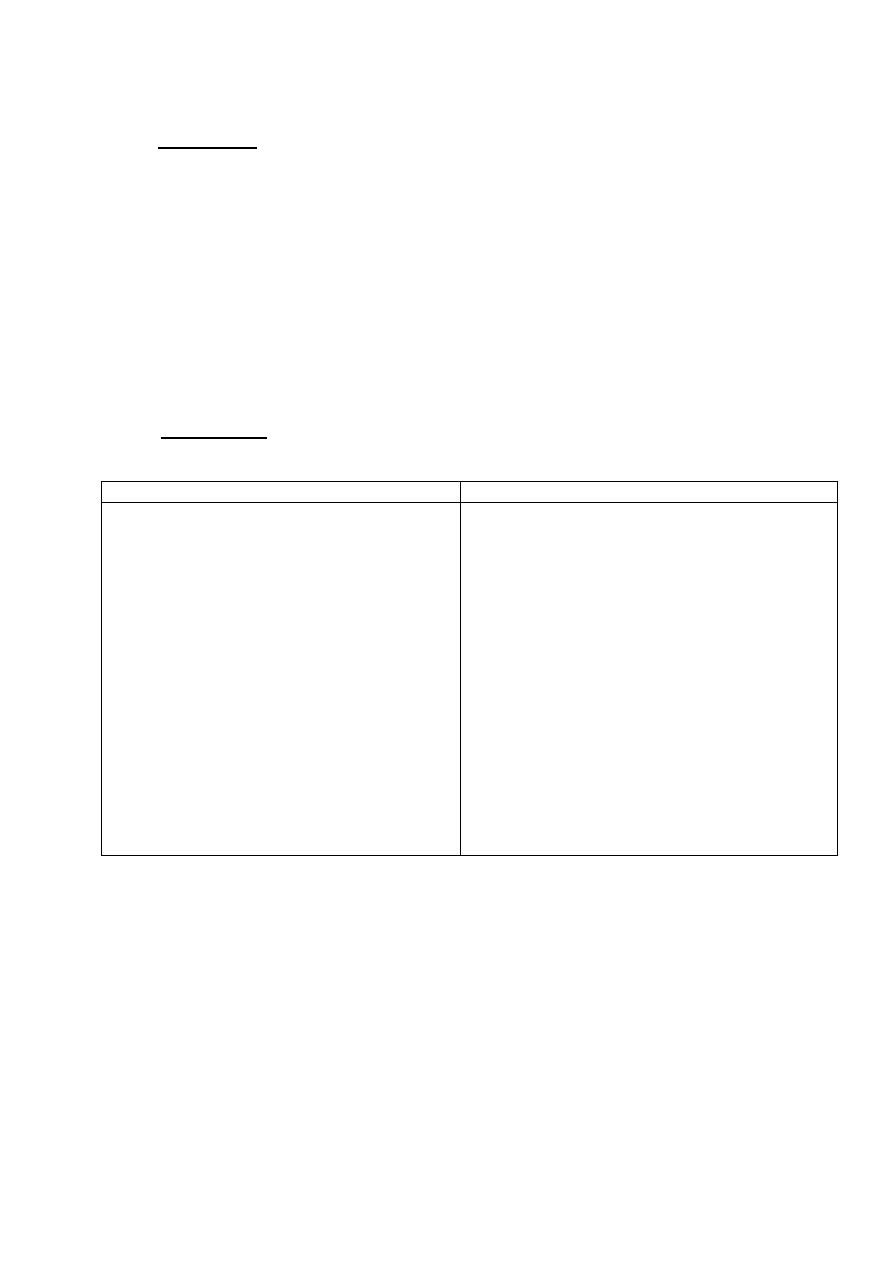
Investigations
III.
Systemic and local:
Investigation
Indication
-Full blood count
Histological assessment of the endometrium
Colposcopic examination
Endocervical / high vaginal swabs
Thyroid function tests
Coagulation n screening
-
-
-
-
-
(pelvic
valuation of the uterine cavity
-E
ultrasound, including saline infusion
sonography, and outpatient hysteroscopy).
- All women with HMB.
If history suggestive of coagulation disorder.
-
- Only from women with other symptoms of
thyroid disease.
intervention.
women prior to surgical
nd all
women when medical treatment has failed a
Symptomatic women ˃ 45 years old, younger
Suspicion of cervical malignancy.
history suggestive of risk of infection.
- If
-
-
-Intermenstrual or postcoital bleeding, irregular
HMB, suspected structural pathology or when
medical management has failed.
Semiobjective:
pads, do not reflect the actual blood loss
bjective methods: history of passage of clots, flooding, use of large number of
methods
50% of excessive menstruation have normal amount of blood loss by objective
Assessment of the amount of the bleeding
has failed, further investigations are needed.
women in whom medical treatment
n and in younger
tigations. In older wom
inves
45 years old, it is appropriate to implement first medical treatment without further
of pathology in a woman under
strongly suggest cyclical HMB without the presence
A full blood count is indicated in all women with HMB, if history and examination
e
:
1. Su
.
2.

and adnexal mass.
pregnancy complications
fibroids, intrauterine polyps,
intramural or submucous
: can exclude pelvic masses,
(transabdominal)
1. TAS
Ultrasonography:
2.Lack of availability or experience
he apparatus
1.Cost of t
Disadvantages:
pathology in the uterine cavity.
and currently is regarded as the gold standard evaluation of
Outpatient procedure
Biopsy of the suspected areas
hyperplasia.
& diagnosis of polyps, submucous fibroid,
Excellent view of the uterine cavity
: Advantage
3. Hysteroscopy
2. Dilatation and curettage ( D&C
general anesthesia.
) an outpatient procedure, without
(Pipelle or Sharman
. Aspiration curettage
Methods:
sonographic endometrial feature
uspicious
if abnormal bleeding or
PCOS
poly cystic ovarian syndrome (
4. In
treatment.
3. In younger women if abnormal bleeding not resolved with medical
carcinoma, tamoxifen Rx)
anovulation, nulliparity, infertility, family history of colonic and endometrial
nic
2. Those with ↑risk of endometrial malignancy ( obesity, DM, HT, chro
years
1. Age more than 4
Indications:
Diagnosis of organic disease e.g. endometritis, polyp, carcinoma, TB, fibroid
provides a guide to etiology & treatment)
dding, atrophic. This
hyperplastic, proliferative, secretory, irregular ripening, she
of the type of the bleeding (Diagnosis of the type of the endometrium:
Diagnosis
Aim:
assessment
Endometrial
based on cervical smear
cted
oestrogen. Tubal and ovarian cancer can suspe
abnormal unless she is receiving
abnormalities, the presence of endometrial cells in postmenopausal women is
s), although cytology is not reliable for the diagnosis of endometrial
lesi
endocervical
rs can help screening for invasive cervical ( especially
cytological smea
in diagnosis asymptomatic intraepithelial lesions of the cervix,
Although most useful
(Pap)
Cytological examination
v. Weighing technique: need further evaluation.
. Pictorial blood loss chart
asuring menstrual blood loss.
iii.Alkaline haematin method( gold standard) for me
ii.Menstrual calendar
i.Iron deficiency anemia
۷
iv
on
.
:
1-
2-
•
5
•
•
•
)
s
1
):
1.
2.
.
3.
Mirena
also named
IUS)
(LNG
releasing intrauterine system
Levonorgetrel
Progestogens:
Risks include thromboembolism and migrine
loss.
43% of blood
estradiol 30 mcg & levonorgetrel 150 mcg) causing reduction in
Using (ethinyl
fective in the managemnt of HMB.
considered ef
enerally
by endometrial suppression
t act
(COCP):
ombined oral contraceptive pills
II. Hormonal:
the cycle for 5 days.
Start on the first day of
menses.
acid 500 mg 3X/day during
Mefenamic
associated with gastrointestinal side effect
But they are
during menstruation and has advantage of analgesic properties.
used agent and reduces blood loss by approximately 25%. Taken
the most frequentl
leading to a reduction in menstrual blood loss. Mefenamic acid is
HMB, so they are
endometrium is a rich source of PGE2 & PGF2œ & its concentrations are greater i
the
etrial prostaglandin production as
lammatories (NSAIDs), inhibit endom
inf
steroidal anti
such as
Prostaglandin synthetase inhibitors (PSI)
Side effects are rare, include gastrointestinal symptoms.
defects.
with fibroid or coagulation
of HMB associated with IUCD,
effective in treating
is
It
ctivity is higher in HMB.
the fibrinolytic a
since
inhibiting endometrial fibrinolysis
: such as tranexamic acid, reduce blood loss by up to 50% by
Antifibrinolytics
interventions are unacceptable.
most surgical
woman is wishing to conceive, hormonal treatments and
: if a
rmonal
I. Non
B. Medical
of iron deficiency anemia
2. Treatment
calendar
1. Menstrual
A. General
most acute and chronic bleeding problems
endometrium corrects
Conversion of the endometrium from proliferative to secretory
irregular manner.
s sloughed in an
endometrium outgrows its blood supply, partially break down, and i
axis result in continuous oestrogen stimulation of the endometrium, so the
HPO
cause of bleeding is not well understood but probably result from dysfunction of the
re anovulatory, the exact
in which most of the patient a
bleeding of endometrial origin
ing, establish the diagnosis of
Exclusion of the pathological causes of abnormal bleed
Counsel the patient about treatment option.
to reassure them and make further treatment unnecessary.
sufficient
For some women, the demonstration that their blood loss is in fact ‘normal’ may be
hysterectomy to treat abnormal uterine bleeding.
result in decreased the use of
roved diagnostic technique and treatment
of AUB
Treatment
selected cases
sonography: an alternative to office hysteroscopy in
infusion
3. Saline
12 mm in follicular phase is suspicious
endometrial thickness 10
postmenopausal with endometrial thickness>4 mm and in premenopausal women
in
n TAS. All endometrial thickness
e tha
: More informativ
(transvaginal)
2. TVS
۸
-
.
.
Imp
-
-
-
.
–ho
1.
2.
:
non-
-
n
y
.
1- C
I
s
,
g
.
2-
-
-
-
:

tation and curretage (D&C) is no longer use as theraputic treatment.
modalities. D
leeding had been decrease with the introduction of new managemnt
uetrine b
for treatment of abnormal
The number of hysterectomies
is retained.
the fertility
with the exception of polypectomy and myomectomy where
complete their families
surgical treatment is considered in those who
Usually
treatment:
C. Surgical
the menstrual blood lo
effective in reducing
: still under trial as being
Selective progesterone receptore modulators (SPMR)
estrinone.
Ethamsylate
Danazol
are
because of its unacceptable side effect
Drugs that are no longer use nowaday
, for that it is not use usually more the 6 months.
after stopping treatment
ontinue
and since its effect dose not
Becuase of its adverse effect on bone density
ovarian suppression leading to amenorrhoea.
and induce
axis
HPO
nregulating the
ct by dow
failed.
are
If all other option
(GnRHa)
releasing hormone analogues
Gonadotrophin
of HMB.
ffective in the treatment
so may be
They are using as contraception and since they cause amenorrhea
gestogens
Injected/depot pro
are mainly weight gain, nausea, bloating.
Side effect
X /day) for 21 days
acetate (5mg, 3
northisterone
reproductive life
extremes of
at the
HMB
anovulatory)
with irregular (
for women
sefull
toges
Oral proges
years.
It require change every 5
related side effect are much less than oral.
progestogen
. Because of its local effect so
dometrial atrophy that it cause
because of en
no bleeding
. It associeted with little or
nd alternative to surgery
contraception a
long term
reversible
with HMB and seek reliable
Is very good choice for women
۹
-
-
:
U
, as
.
-
e
3-
-
:
s
It a
c
4-
;
,
:
-
-
-G
5-
ss.
ila
ulsed in the outpatient setting or
: Endocervical polyp can be av
Polypectomy
1-
anaesthesia or in the outpatient setting.
r by hysteroscopy resection under general
under general anaesthesia o
2-
me of the
Is the destruction of the endometrium and so
Endometrial ablation
:
hysterectomy.
. Some may need repeating the procedure or subsequent
contraception
g term effective
should advice to have lon
undergo this procedure
Women who
nd structural causes of HMB have been excluded.
and in whom all organic a
underlying myometrium. Suitable for woman who has complete her family
b. Resection
cal: a. Roller ball
2. Electrosurgi
1. Laser
I.Hysteroscopic:
Methods:
Gas embolism
due to absorption of distension media.
Fluid overload
is used to decrease that risk.
ntibiotics
3. Infection in the form of endometritis for that prophylactic a
Bleeding
Uterine perforation
Complications of hysteroscopic methods
3. Novasure.
2. Microwave.
1. Thermachoice
hysteroscopic:
II.Non
۰۱
-
1.
:
2. 2.
4.
5.
Is surgical removal of the fibroid from the uterus with
Myomectomy
3-
:
hysterectomy in case of intraoperative bleeding.
woman should be counseled before the procedure about the need for
on the location and size. Complications include bleeding and infection and the
oscopically depend
y or lapar
onservation of the uterus. Removed abdominall
c
AE) for the treatment of fibroid usually
Uterine artery embolization
4-
: (U
and shrinking.
results in fibroid become avascular
carried out by interventional radiologist. Blockage of both uterine artery
Hysterectomy:
5-
investigations will be performed looking to the cause.
clinically stable then
14 days and once the patient
of bleeding usually will occur within 10
ion
then 2X daily for 2 days then 1X daily for 3 weeks.
daily for 3 days
4X /day for 4 days then 3X
30 mcg / norgestrel 0.3 mg
Ethinyl oestradiol
is:
One of them
Several regimens had been described.
Resuscitation.
Management:
Anticoagulants.
AVMs.
Prolapsed fibroid.
Coagulopathy, most commonly is von Willebrand’s disease.
be due to the following causes:
This may
Sever acute heavy menstrual bleeding:
. Laparoscopic
history of previous caesarean section.
2. Abdominal: for large uterus, endometriosis or pelvic inflammatory disease or with
. Now is the preferred rout with small uterus.
Vaginal
Routes:
less invasive surgical options had failed.
2. Family is completed
1. Failure of medical treatment
Indications:
3.
1.
3
.
1-
2-
3-
4-
1-
2-
-(
)
Cessat
-
………………………………………………………………………………………..

1
Postmenopausal bleeding (PMB)
Learning objectives: By the end of this lecture, you need to:
1- Define PMB.
2- Explain why it does occur.
3- Discuss the causes behind PMB.
4- List the commonest health problems which contribute for this problem.
5- Analyze the investigations for this presentation.
6- Summarized the treatment options.
Definition
: is bleeding from the genital tract occurring after the menopause.
Its more critical than premenopausal bleeding. Any bleeding after 1 year of
menopause or menstruation that continue after the age of 55 years should be
investigated.
Pathophysiology:
• Once menopause occurs, estrogen and progesterone are no longer produced by
the ovaries; nor are they produced in any appreciable amounts by the liver and
fat. The endometrium regresses to some degree, and no further bleeding
should occur. When bleeding does resume, therefore, endometrium must be
evaluated.
■ Benign conditions is most frequent causes of PMB as the majority will have
atrophic vaginitis whereby the vaginal epithelium will thins and breaks down in
response to low oestrogen level which is easily treated with topical estrogen. But
endometrial cancer is the most serious potential underlying cause may be
responsible to 10% of cases and even more in developing countries. The
commonest cause in other countries is usually the use of hormonal replacement
therapy, otherwise in developing countries and in Iraq malignant disease is an
important cause.
Clinical features:
- If the women are not taking Hormone replacement therapy (HRT), then any
bleeding is abnormal.
- In women on combined cyclical HRT, bleeding in the progesterone free period
is normal.
- Unscheduled bleeding refers to bleeding at other times or abnormal in amount,
this should be investigated as abnormal bleeding.
Causes:
1-
Drugs
:
Tamoxifen: is associated with a two- to threefold increased risk of
endometrial cancer in postmenopausal women. TVUS of patients on this
therapy typically shows an increased endometrial thickness.

2
HRT: The occurrence of uterine bleeding or spotting after the initiation of
HRT is not unusual. More than half of HRT users will have some spotting or
bleeding at the beginning of therapy.
- Sequential (or cyclical) combined regimens cause scheduled bleeding
in most users. Continuous combined regimens are associated with a
reduced relative risk of endometrial cancer but may cause
unpredictable spotting or bleeding during initial use.
Anticoagulants: Overuse of anticoagulant medications such as aspirin,
heparin and warfarin- which are taken with greater frequency by patients in
this age group-may contribute to postmenopausal bleeding.
2-
Malignant neoplasms:
of the vulva, vagina, cervix, uterine body, fallopian
tubes.
3-
Benign neoplasms
of the vulva, vagina, cervix, uterine body, fallopian tubes.
4-
Ovarian tumours
: Oestrogen producing tumours
5-
Infections
:
- Vaginitis – Trichomonas, Candida, senile.
- Endometritis – tuberculous, senile
6-
Dysfunctional uterine haemorrhage
(Bleeeding of endometrial origin).
7-
Injuries
:
- Direct trauma
- Decubital ulceration
- Foreign bodies such supporting pessaries
- Postradiation ulceration
8-
Disease of the blood and the capillaries
: Abnormalities of the hematologic
system also must be considered as a possible cause of PMB. On rare
occasions, AUB will be the first sign of leukemia or a blood dyscrasia.
9-
Haemorrhage from other structures
:
- Urethral caruncle
- Papilloma and carcinoma of the bladder
- Haemorrhoids and fissure in ano
- Carcinoma of the rectum
10-
No cause could be found
.
Differential diagnosis
:
- Endometrial carcinoma.
- Endometrial hyperplasia.
- Endometrial polyp.
- Cervical carcinoma.
- Atrophic vaginitis.
Investigation:
1 -
Thorough history and examination
: PMB or discharge needs immediate
investigation even though there is only one episode.
2-
Blood test
to exclude blood disorders.
3-
Cervical smear and possibly biopsy
if any pathology detected.
4-
TVUS
( transvaginal ultrasonoraphy): Is a non invasive . It should be done for
all women with postmenopausal bleeding. Transvaginal ultrasound has a good

3
correlation with pathologic endometrial findings. Using an endometrial thickness of
(4) mm as upper normal level (or 5 mm if she is on HRT). If that is revealed thick
endometrium, then other tests for endometrial assessment are indicated as:
5-
Endometrial biopsy with or without hysteroscopy
.
6-
Dilation and curettage (D&C)
may be necessary for women with high risk of
endometrial carcinoma.
7-
Sonohysterography
: The introduction of intrauterine fluid (saline-infusion
sonography) during transvaginal ultrasound is one of the most significant advances in
ultrasonography.
Uterine fibroids and adenomyomas generally are apparent on ultrasound. Uterine
polyps may appear as a thickened endometrial stripe, but these and submucous
myomas can be clearly identified as filling defects when a sonohysterograyph is
performed
8-
Hysteroscopy
:
Hysteroscopic visualization has several advantages:
immediate out patient evaluation,
visualization of the endometrium and endocervix,
the ability to detect minute focal endometrial pathology and to perform
directed endometrial biopsies
Treatment:
1-If there is a cause then treating the cause.
2-When no cause in the genital tract and the haemorrhage is repeated its origin from
another site has to be excluded so full examination of the urinary system and the
lower bowel, including cystoscopy and sigmoidoscopy.
3- If bleeding persistent or recurrent with negative investigation so laparotomy is
needed with hysterectomy which may detect an early carcinoma of the uterus, of the
tube or the ovary.
4- Hypoestrogenic atrophic changes can be treated by HRT.
Always remember:
Endometrial carcinoma is one of the most important consideration in post
menopausal bleeding.
Atrophy is the most common cause of post menopausal bleeding.
Initial evaluation should include cervical cytology, transvaginal ultrasound
and / or endometrial sampling.
Findings should be further evaluated with saline sonography or hysteroscopy.
………………………………………………..
