1
Third stage
Surgery
Lec-2
.د
سعدالله الزكو
1/1/2014
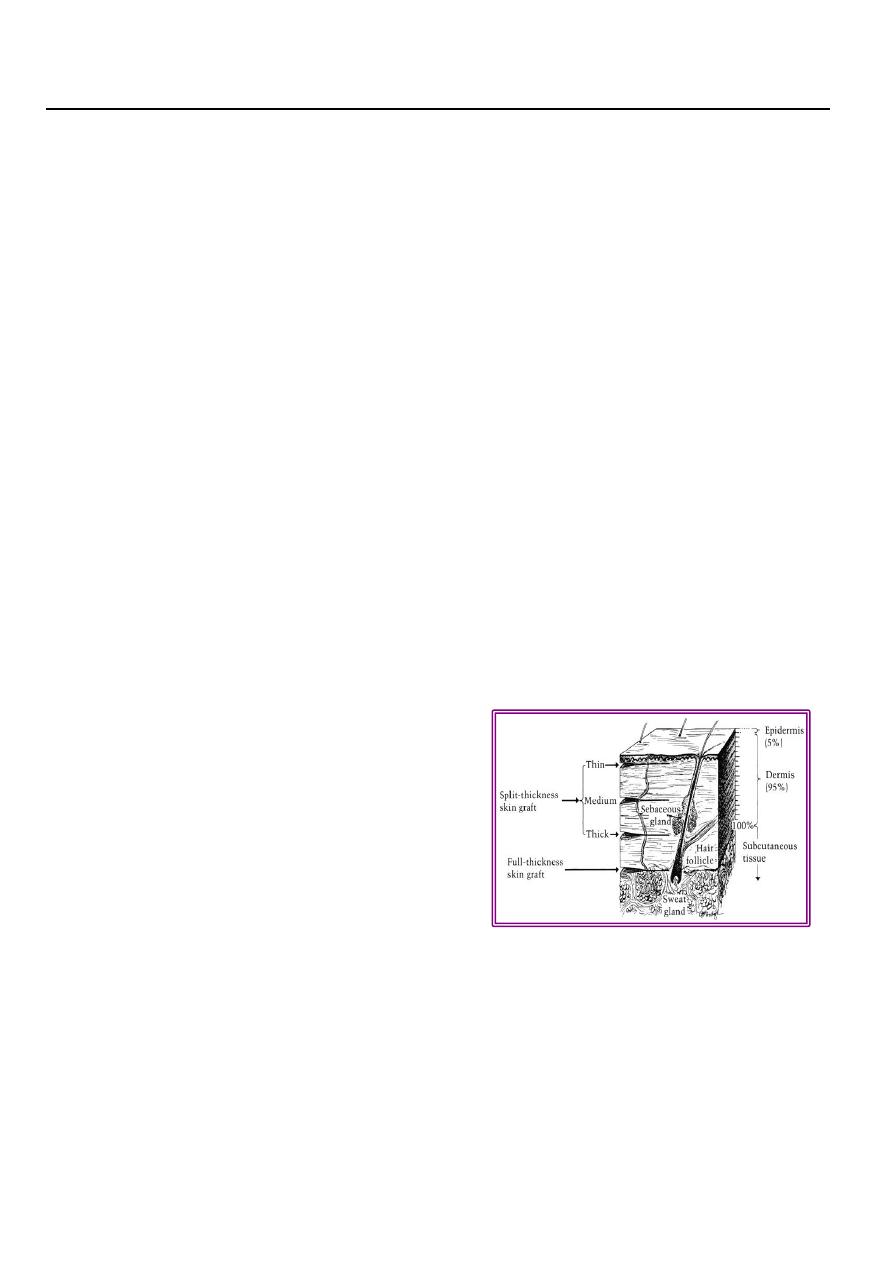
Skin graft
Definition: is a segment of epidermis and dermis that is removed from its blood supply at
donor site transferred into a recipient site.
Types:
1-Origin:
Autograft , allo-(homo)-, xeno(hetero).
2-Thickness:
Split (Thiersh ): thin ,intermediate, thick.
Full thickness (Wolfe).
Split skin graft (SSG)
Most useful and popular.
Contains epidermis and part of dermis.
Contract more postoperatively.
Survives more.
Full thickness graft:
Epidermis and entire dermis.
Normal color, texture, hair.
Not contract, less survive.
Donor site:
SSG :thigh buttock, abd. wall arm.
FSG: pre-, post-auricular, supraclav, upper eyelid.
Success of skin graft:
Vascular recipient bed.
Proper contact of graft with proper tension.
2
No fluid beneath.
No movement.
Free from infection.
Immunological.
Indications of skin graft
Skin loss: post traumatic, post surgical, result of pathology (venous ulcer).
Mucosa loss: leukoplakia, reconstruction of vagina.
Contraindications:
Avascular recipient bed.
Infection.
Flaps
“ part of tissue which retains its vascular attachment to body, transplanted to reconstruct a
defect.”
The flap donor site closed by suture or SSG.
Classification
1. Content:
A. Skin.
B. Fascio-cutaneous.
C. Myo-cutaneous.
D. Muscle.
E. Osteo-myo-cutaneous.
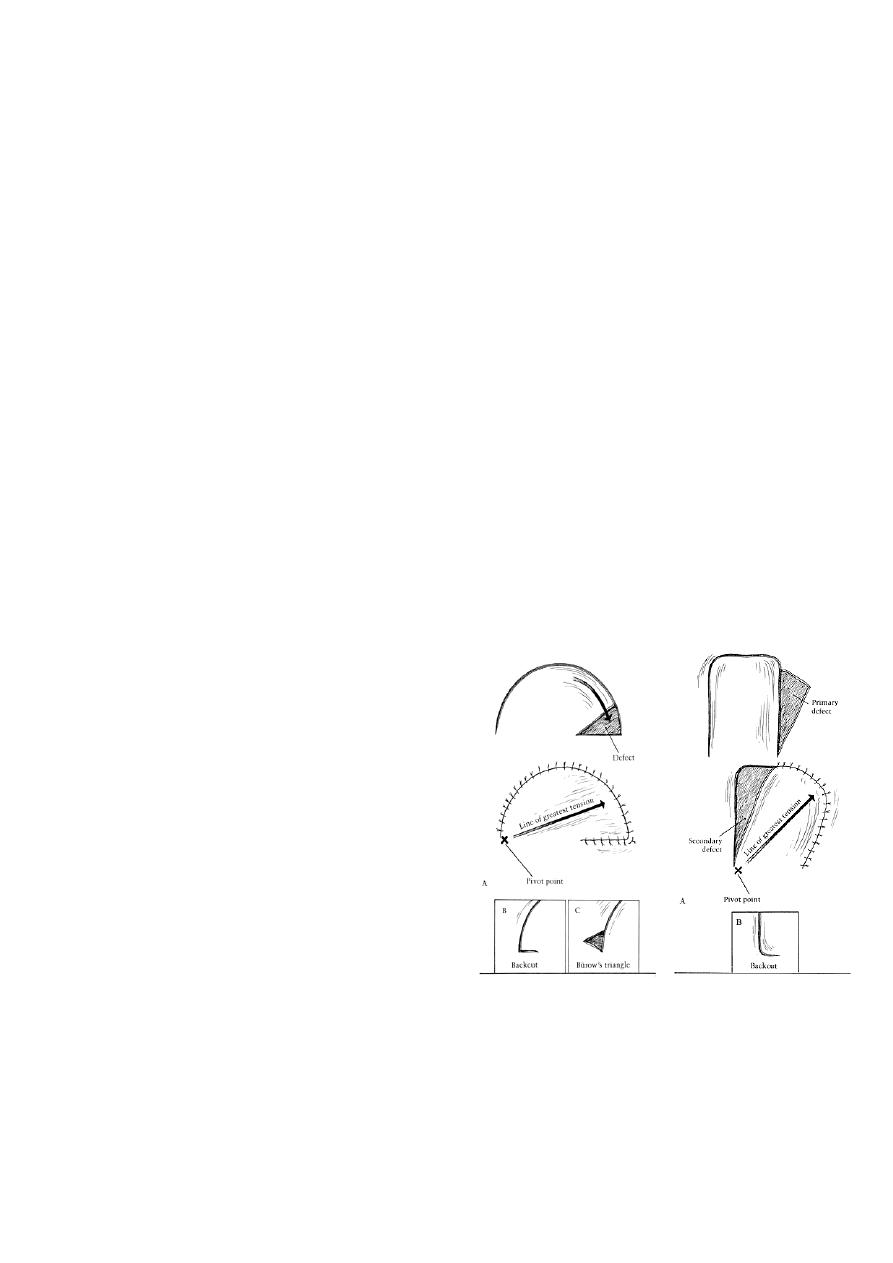
2. Site:
A. Local : where donor area near recipient site.
Rotation.
Transposition.
Advancement.
B. Distant flap :where donor area at a distance from recipient site.
Transposition
Rotation
3
C. Free flap: by using microsurgery.
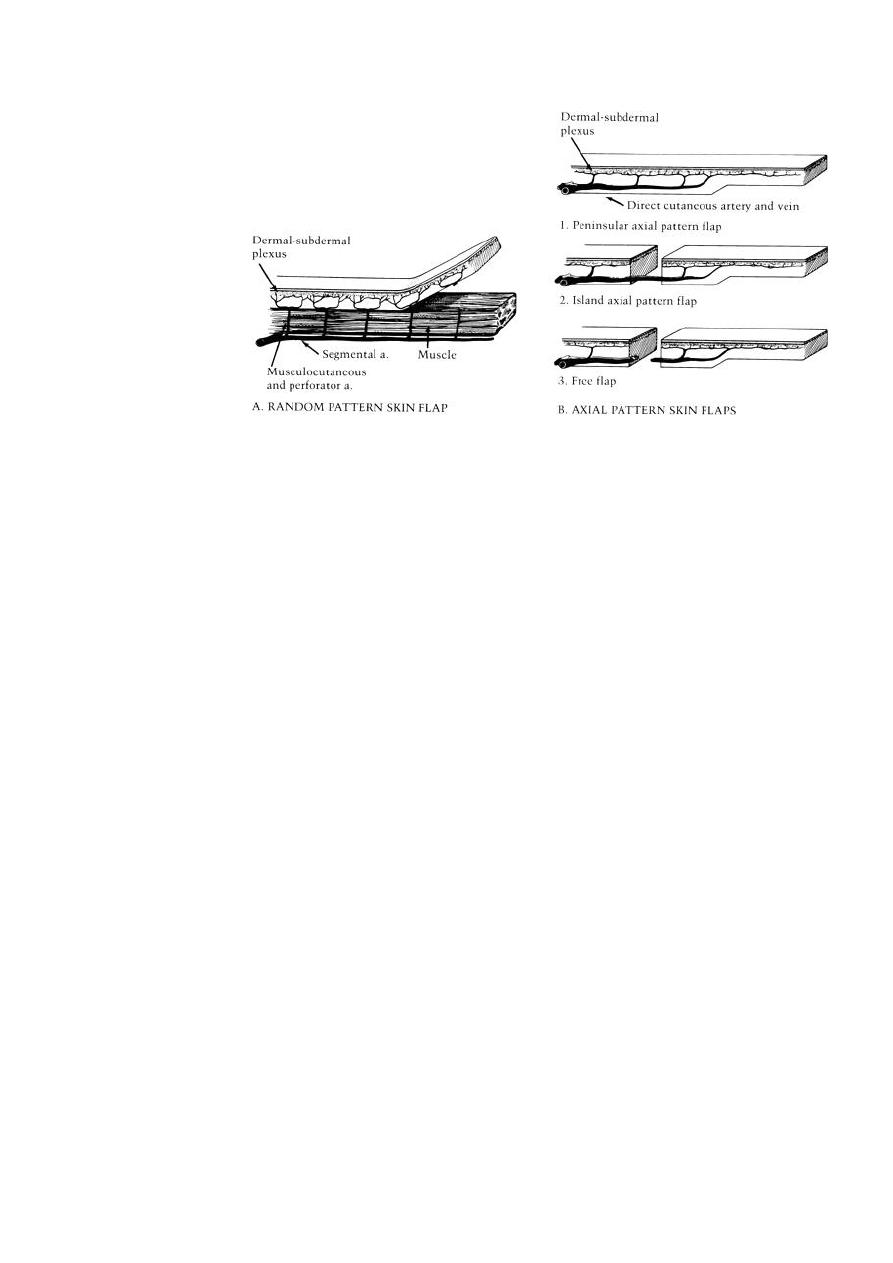
3. Vascular pattern ( skin flaps):
A. Axial pattern: longer, easier ,safer.
B. Random pattern.
Indications of flaps
1. Cover recipient bed with poor vascular supply.
2. Reconstruction full thickness eyelids, lip, nose, cheeck .
3. Padding bony prominences.
4. When operation through the wound at later date.
5. Muscle flap provides a functional unit.
6. Provide sensation.
Burns
Coagulative necrosis of tissue due to heat.
Causes:
1. Flame 45%.
2. Hot liquid (scald)30%
3. Hot object.
4. Electric.
5. Chemical.
6. Others : semi liquid, steam, UVL,XR.
4
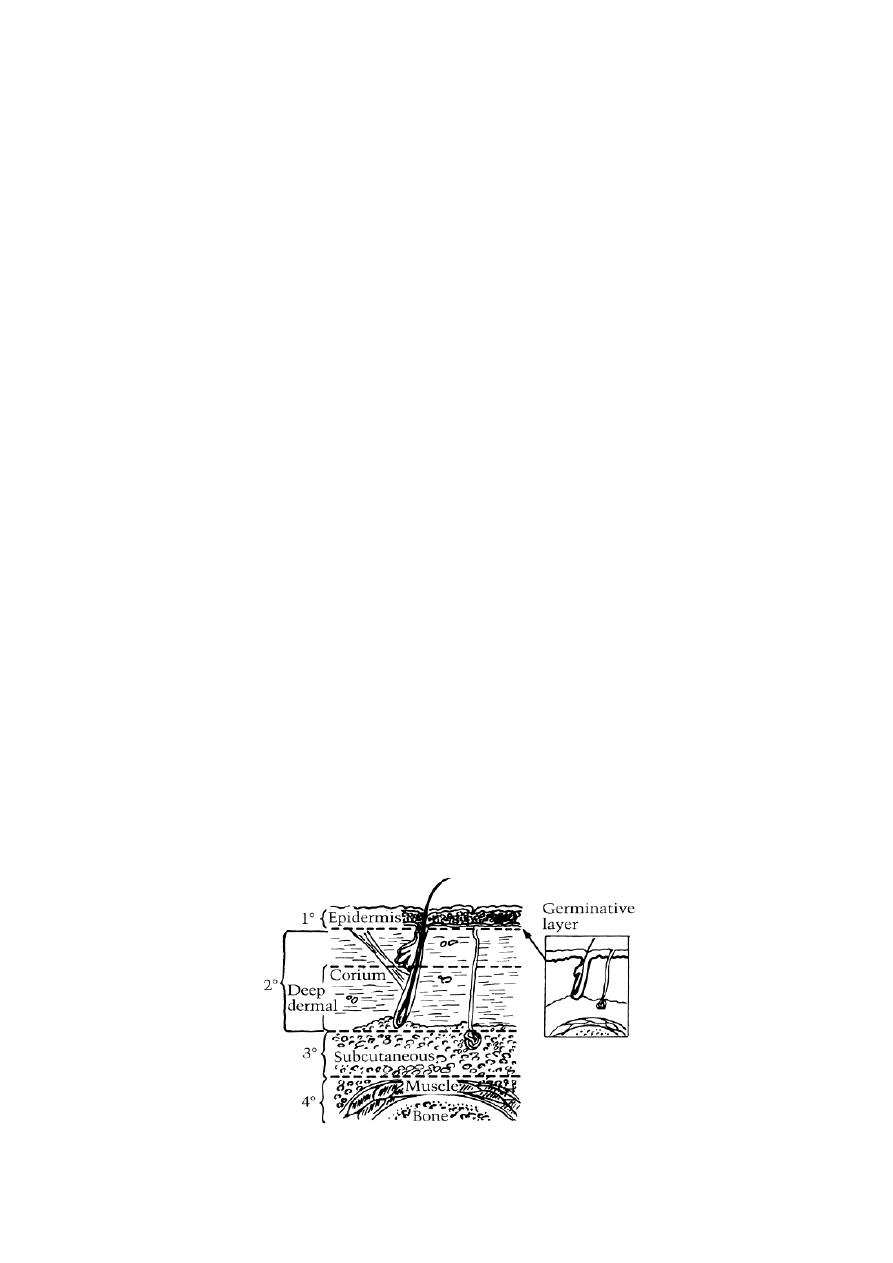
Depth of burn: 4 degrees:
1. First : epidermis.
A. Erythema, edema, scaling.
B. Analgesic, oint.
2. Second:
A. Superficial 2
nd
.
Epidermis and superf. dermis .
Blisters painful to light touch red blanch positive.
Dressing – 1w.
A. Deep 2
nd
( deep dermal )
Epidermis and most dermis.
Painful to pinprik, milky white blanch –ve.
Early excision + grafting.
3. Third:
1. Epidermis and whole dermis.
2. White, brown or black.
3. Painless thrombosed V.S.
4. Early excision and grafting or dressing and late graft.
4. Fourth : muscle and bone.
5
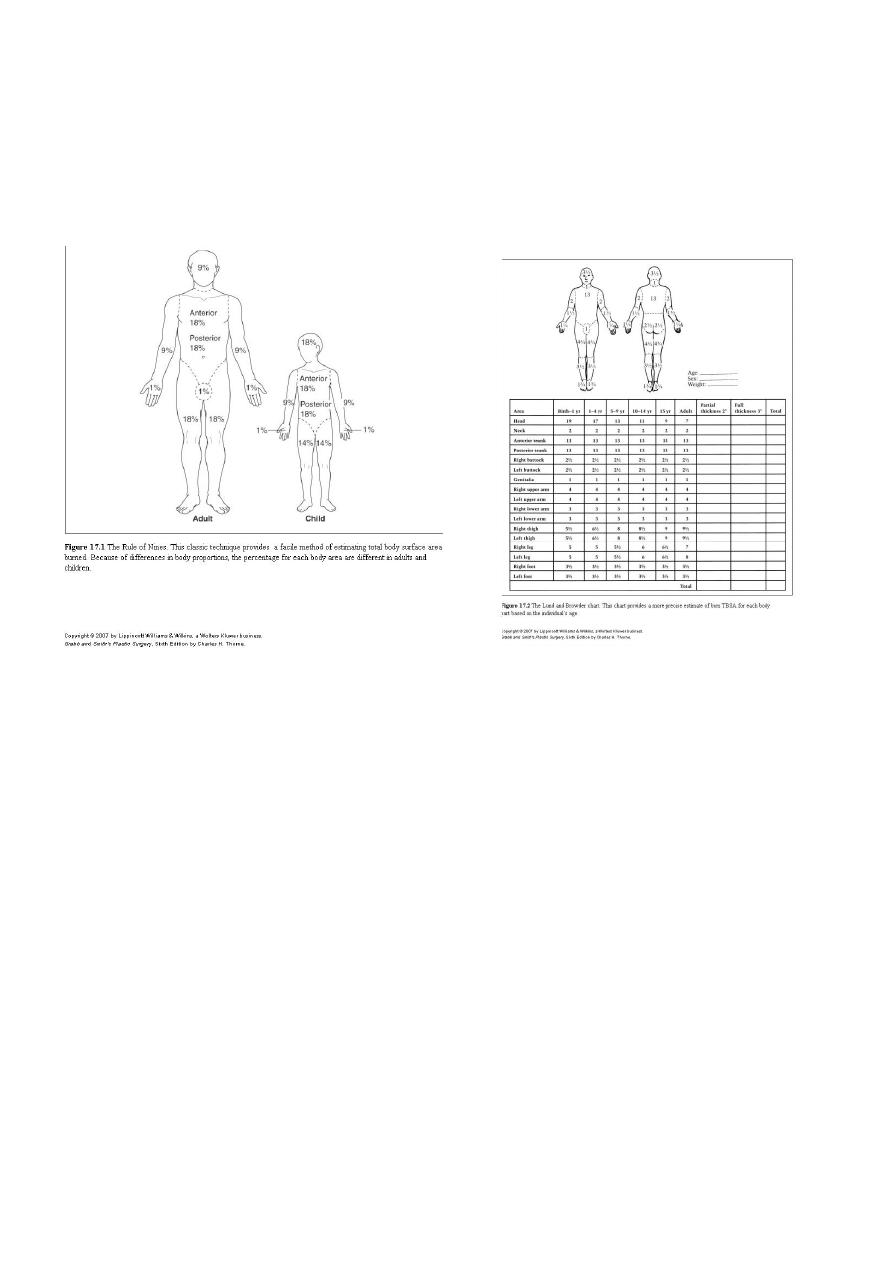
Extent :
1. Rule of nines.
2. Lund and Browder chart.
3. Palm method (1%).
Management of burns
1. ABC:
A. Airway clear.
B. Breathing humidified O2 , respirator.
C. Circulation cannula :
Blood sample (Hb., PCV, urea, electrolytes ).
Sedation.
IV Fluids.
2. Assessment :
A. History
B. Exam:
General
Local (depth, %).

6
2. Sedation: (i.v)
Morphine , pethidine, + largactil.
4. Iv :
A. Given in :
10% + in children.
15% + in adults.
B. ½ amount in 8 h,1/4 in 8h, 1/4 in 8h.
5. Investigations: Hb, PCV, bl. urea, s.elect. , blood group.
6. Urine:
A. Foly’s catheter.
B. Hourly output (0.5-1 ml/kg/h)
7. Tetanus toxoid 0.5 ml
or 250 mg human immunoglobulin + toxoid.
8. Antibiotic : pencilline 5 days.
9. Nothing by mouth, N.G. tube
10. Wound care:
A. Clean, ointment (Flamazine).
B. Dressing ( open, closed)
C. Operation (SSG ,flaps)
Complications
1. Shock: neurogenic, hypovolemic, septic
2. Infection: wound, resp., urinary, septicemia.
3. Renal failure.
4. Curling ulcer.
5. Deformity, scars, keloid.
6. Metabolic.
7. Psychological.
8. Marjolin (sq. cell carcinoma).
7
From other lecture
Severity of burn depend on:
1-Size.
2-Site.
3-Depth .
4-Age Increased mortality in less than two years of age because of
A-increase the surface area.
B-immature immune system.
C-immature kidneys.
Also increased mortality in patients over 50 years of age because of associated diseases.
5-Associated injury e.g. fractures, inhalation injury, head injury, internal bleeding
Indication for admission:
1-PTB > 15% in adult.
2-PTB > 10% in child.
3-FT B> 10% any age.
4-Burn in face , hand, foot , perineum ( except minor cases).
5-Inhalation injury.
6-Electrical burn.
7-Associated major medical illness e.g. DM.
8-Other considerations age, home situation and level of cooperation.
Burned skin after healing:
Hypo or hyper pigmentation.
Scar.
Susceptible for sun burn.
Dry.
Itching.

8
Effects of burn injury (complications)
1-Local effects:
1- Tissue damage (leakage of serous fluid)
2- Inflammation (erythema)
3- Infection
2-Regional effects :( circulatory problems: limb circulation may be compromised).
3-Systemic effects :
1-fluid loss either external or internal.
2-multiple organ failure.
4-Systemic complications:
Curling ulcer( gastric or duodenal ) leading to acute hematamesis.
Immune suppression which increase the rate of septic complications.
Weight loss due to catabolism (response to trauma
5- nonspecific complications:
- UTI from catheterization .
-DVT and
- pulmonary embolism
Clinical Picture of Burn Injuries
1- Pain:
2- Acute Anxiety:
3- Fluid loss and dehydration:
4- Local tissue edema:
Superficial burn: blister
Deep burn: edema formation in the subcutaneous spaces then may be marked in head and
neck, with sever swelling which may obstruct the airway.
Limb edema may compromise the circulation.
5- Special sites:
Burn of the eyes are uncommon in house fires, the eyes may be involved in explosion
9
injuries or chemical burns.
Burn in the nose, airway, mouth, and upper airway may occur in inhalation injuries.
6- Coma:
from carbon monoxide or cyanide poisoning.
Management of Burn
MINOR BURNS/OUT-PATIENT BURNS
Local burn wound care
Blisters.
Initial cleaning of the burn wound
Washing the burn wound with chlorhexidine solution is ideal for this purpose.
Topical agents
dressings with a non-adherent material such as Vaseline-impregnated gauze, 1% silver
sulphadiazin cream
1-AIRWAY: The first priority is the maintenance of the patient airway.
2-Breathing: Effective ventilation
3-Circulation
Put IV line and start I.V fluid
if burn is more than 15% (adult), and more than 10% (children) calculate the fluid
requirement by
Parkland formula.
Parkland formula = body wt. x % of TBSA x 4.
Type of fluid:
1-Crystalloid resuscitation.
Ringer’s lactate is the most commonly used crystalloid. Crystalloids

11
are said to be as effective as colloids for maintaining intravascular
volume. In children, maintenance fluid must also be given. This is
normally dextrose–saline given as follows:
• 111 ml kg–1 for 24 hours for the first 10 kg;
• 51 ml kg–1 for the next 10 kg;
• 21 ml kg–1 for 24 hours for each kilogram over 20 kg body
2-Colloid resuscitation
Plasma Proteins should be given after the first 12
hours of burn because,
4-Manage other complicating life threatening injuries .
5-Cold water application
a-decreased tissue damage.
b-Decreased pain.
C-Stabilizes mast cells (decreases edema).
Pain relief in second degree (not third degree) burn which is less than 15%TBS.
6-Evaluate the burn wound and look for the most two important conditions:
a- inhalation injury
b- release of constricting eschar (Escharatomy) which lead to
decrease chest wall movement (respiratory embarrassment)
Extremity constriction (compartment syndrome or distal ischemia and necrosis).
7- Folleys Urinary Catheter
done in burn more than 25% TBSA.
UOP should be not less than 30-50 ml/hr(adult) and 0.5-1ml/kg body wt/hr in children.

11
8- NGT
done in burn more than 25% TBSA. With suction for gastric decompression, because
there is chance of paralytic ileus.
9- Analgesic and Sedation
in major burn only IV not IM or SC morphine 0.2 mg/kg or into the drip.
10- Anti Ulcer Treatment
gastric or duodenal lesion occur within 48 hrs after burn, give prophylactic ranitidine
(H2 receptor antagonist) or give antiacids by NGT.
11-Tetanus Immunization
12-blood Transfusion
14- Oxygen Therapy
15- Careful monitoring
which includes
a-monitoring of the general condition or vital signs.
b-monitoring of the fluid resuscitation for adequate perfusion.
c- investigations for renal,metabolic and hematological condition.
16-Antibiotics (controversy)
sometime penicillin prophylaxis given in more than 10% burn to prevent hemolytic
streptococcal infection.
17- Physiotherapy and prevent bed sore.
