1
Third stage
Surgery
Lec-2
.د
مدثر
1/1/2014
The metabolic response to injury
LEARNING OBJECTIVES
• Classical concepts of homeostasis
• Mediators of the metabolic response to injury
• Physiochemical and biochemical changes that occur during injury and recovery
• Changes in body composition that accompany surgical injury
• Avoidable factors that compound the metabolic response to injury
• Concepts behind optimal perioperative care
Basic concepts
Homeostasis is the foundation of normal physiology
‘Stress-free’ perioperative care helps to restore homeostasis following elective surgery
Resuscitation, surgical intervention and critical care can return the severely injured
patient to a situation in which homeostasis becomes possible once again
BASIC CONCEPTS IN HOMEOSTASIS
‘Homeostasis: the co-ordinated physiological
process which maintains most of the steady
states of the organism.’ (Walter Cannon)
Responses to injury are, in general, beneficial
to the host and allow healing/survival. (John
Hunter).
It is important to recognise that the response
to injury is graded ,the more severe the injury,
the greater the response .
This concept not only applies to physiological/metabolic changes but also to
immunological changes/sequelae.
2
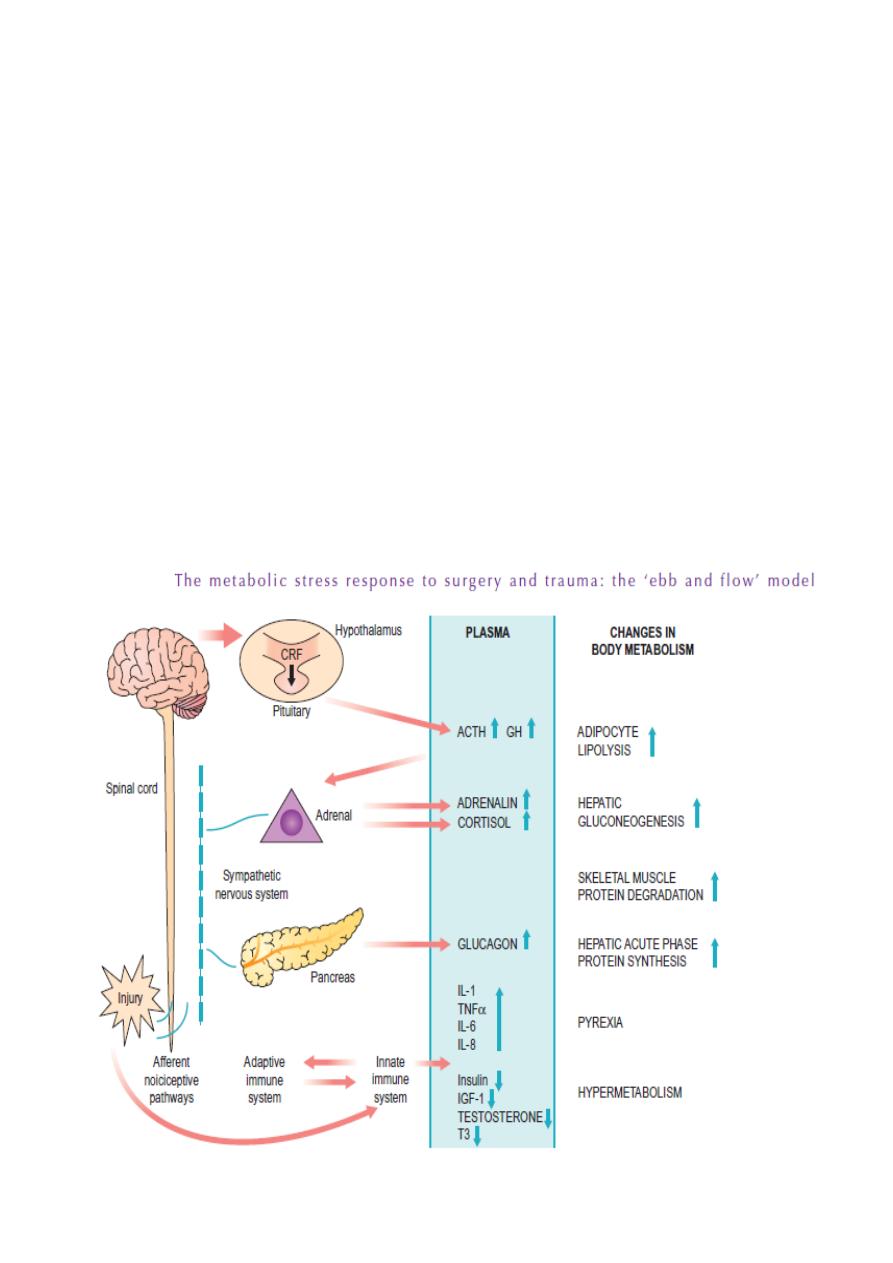
THE METABOLIC STRESS RESPONSE TO SURGERY AND TRAUMA :
The physiological natural response to injury includes:
Immobility/rest
Anorexia
Catabolism
The changes are designed to aid survival of moderate injury in the absence of medical
intervention
The neuroendocrine response to severe injury/critical illness is biphasic:
Acute phase characterised by an actively secreting
pituitary and elevated counter-regulatory hormones
(cortisol, glucagon, adrenaline). Changes are thought to be beneficial for short-term
survival
Chronic phase associated with hypothalamic suppression and low serum levels of the
respective target organ hormones. Changes contribute to chronic wasting
3
Systemic inflammatory response syndrome (SIRS) following major injury:
■ Is driven initially by pro-inflammatory cytokines
(e.g. IL-1,IL-6 and TNFα)
■ Is followed rapidly by increased plasma levels of cytokine antagonists and soluble
receptors (e.g. IL-1Ra, TNF-sR)
■ If prolonged or excessive may evolve into a counterinflammatory response syndrome
(CARS)
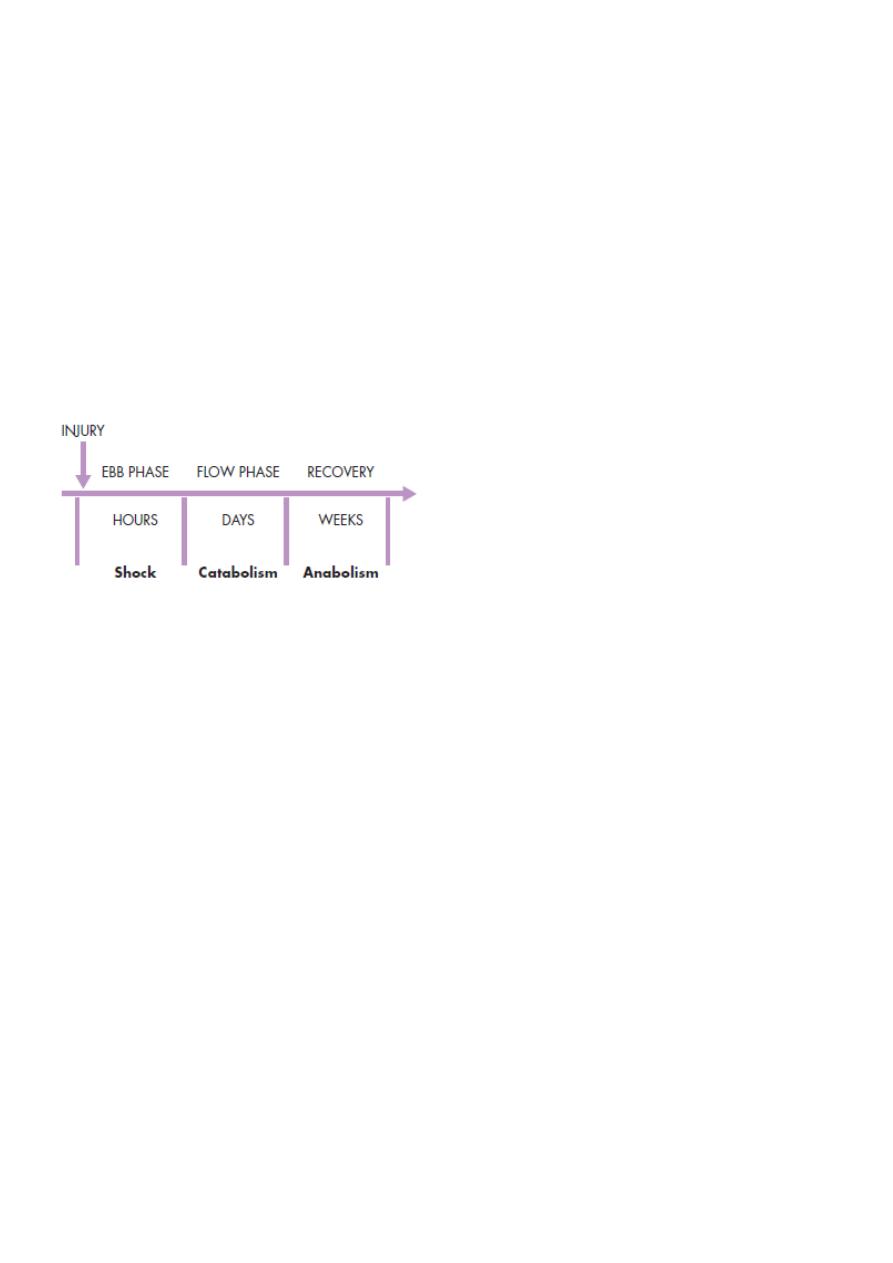
In 1930, Sir David Cuthbertson divided the metabolic response to injury in humans into
‘ebb’ and ‘flow’ phases :
Ebb phase begins at the time of injury and lasts for approximately 24–48 hours. It may
be attenuated by proper resuscitation, but not completely abolished.
The ebb phase is characterised by:
hypovolaemia, decreased basal metabolic rate, reduced cardiac output, hypothermia
and lactic acidosis.
The predominant hormones regulating the ebb phase are:
catecholamines, cortisol and aldosterone (following activation of the renin–angiotensin
system).
The flow phase may be subdivided into an initial catabolic phase, lasting approximately 3–
10 days,
followed by an anabolic phase, which may last for weeks if extensive recovery and repair
are required following serious injury
Purpose of neuroendocrine changes following injury is to:
Provide essential substrates for survival
Postpone anabolism
Optimise host defence
These changes may be helpful in the short term, but may be harmful in the long term,
especially to the severely injured patient who would otherwise not have survived without
medical intervention.
4
KEY CATABOLIC ELEMENTS OF THE FLOW PHASE OF
THE METABOLIC STRESS RESPONSE
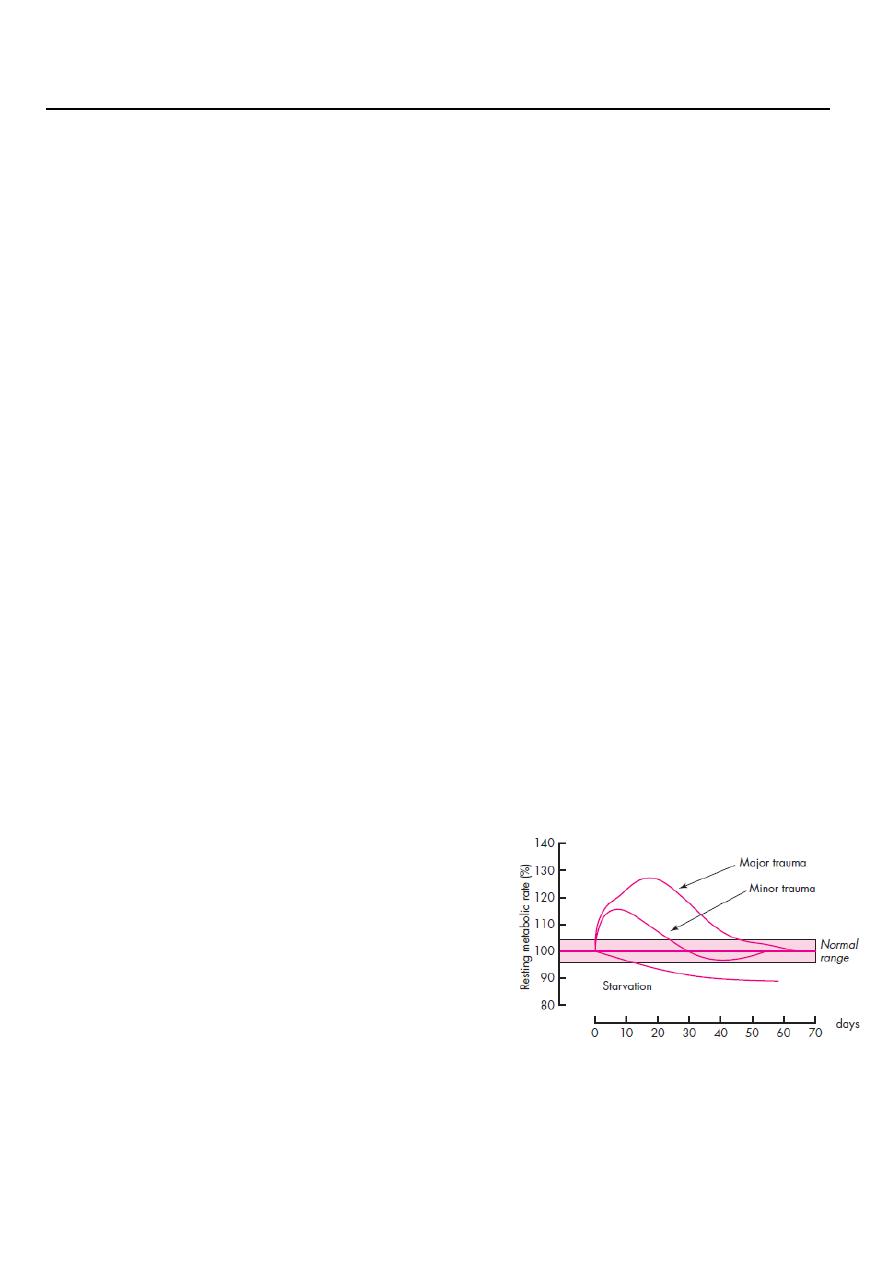
Hypermetabolism following injury:
Is mainly caused by an acceleration of futile metabolic
cycles
Is limited in modern practice by elements of routine critical
care
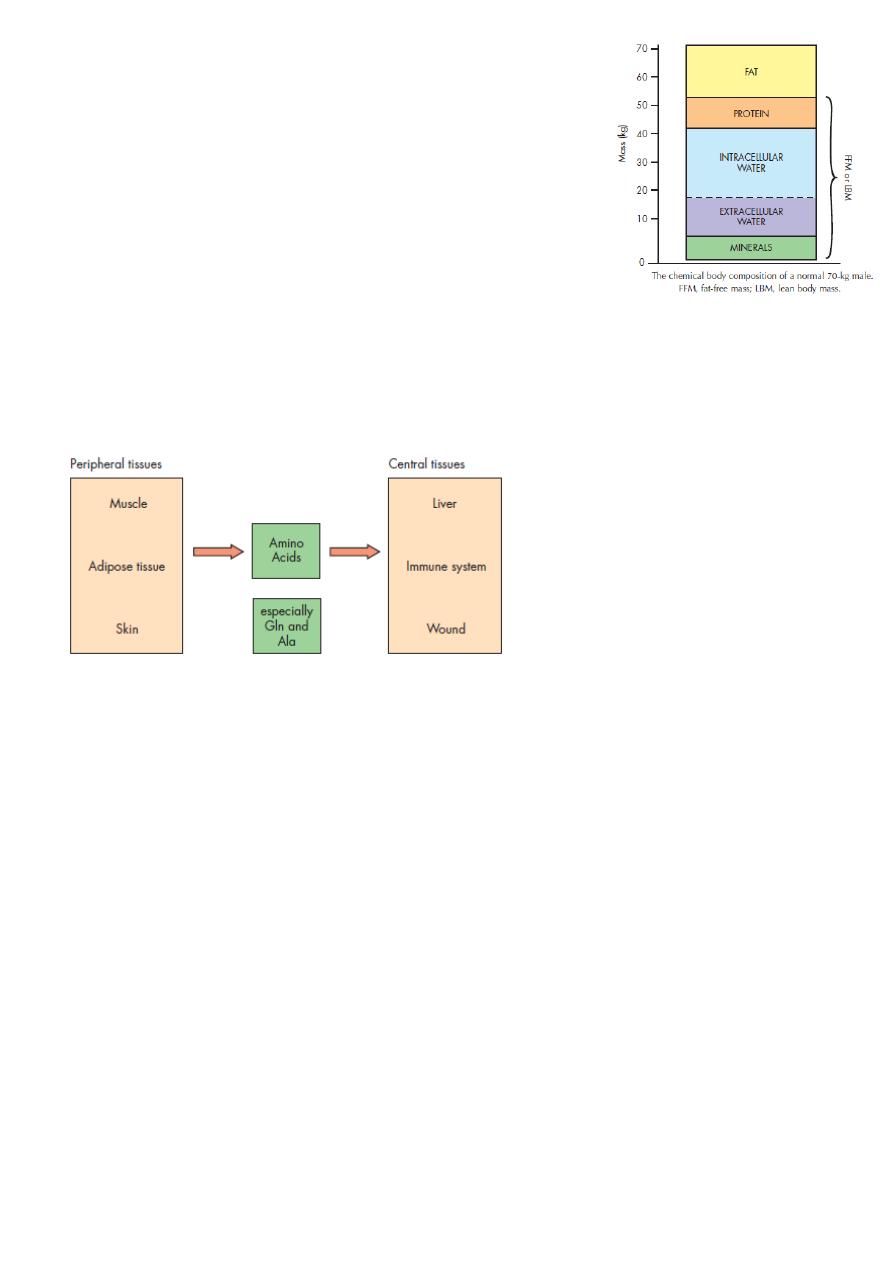
During the metabolic response to injury, the body reprioritises protein metabolism away
from peripheral
tissues and towards key central tissues such as the liver, immune system and wound.
Changes in body composition following major surgery/critical illness
Catabolism leads to a decrease in fat mass and skeletal muscle mass
Body weight may paradoxically increase because of increase in the extracellular fluid
space
Alterations in hepatic protein metabolism:
the acute phase protein response (APPR)
The hepatic acute phase response represents a reprioritisation of body protein
metabolism towards the liver and is
characterised by:
Positive reactants (e.g. CRP): plasma concentration
Negative reactants (e.g. albumin): plasma concentration

5
Insulin resistance
*Following surgery or trauma, postoperative hyperglycaemia develops as a result of
increased glucose production combined with decreased glucose uptake in peripheral
tissues.
*Decreased glucose uptake is a result of insulin resistance which is transiently induced
within the stressed patient.
Suggested mechanisms for this phenomenon include the action of pro-inflammatory
cytokines and the decreased responsiveness of insulin-regulated glucose transporter
proteins. The degree of insulin resistance is proportional to the magnitude of the injurious
process. Following routine upper abdominal surgery, insulin resistance may persist for
approximately 2 weeks.
Avoidable factors that compound the response to Injury
Continuing haemorrhage
Hypothermia
Tissue oedema
Tissue underperfusion
Starvation
Immobility
A proactive approach to prevent unnecessary aspects of the surgical stress
response:
Minimal access techniques
Blockade of afferent painful stimuli (e.g. epidural analgesia)
Minimal periods of starvation
Early mobilisation

6
From other lecture
Body response to trauma
Trauma in general initiate a series of biochemical and physiological reactions created by
secretion of hormones and mediators (neuro - endocrine) as an adaptive mechanism for
restoration of hemostasis and promote tissue healing.
The intensity of the reaction is proportional to the severity of the injury.
It is also affected by the age, pre trauma health state and accompanied disease.
The main stimulus of the neuro endocrine reaction are
1- Changes in the effective circulatory volume like hemorrhage, burn, diarrhea or
vomiting.
2- Changes in the concentration of Oxygen or Carbon dioxide like in asphyxia, chest
trauma or head injury.
3- Pain and noxious stimuli.
4- Sepsis like sever infection, peritonitis.
The neuro-endocrine response characterized by secretion of hormones that control and
maintain the reaction These Hormones called the stress hormones which include:
1- catcholamin.
2- corticosteroid.
3- glucagons.
4- renin - angiotonsen
5- aldosteron
6- vasopressin
7- growth hormone
Caticholamine:
Secreted from the adrenal medulla in form of adrenalin and nor adrenalin, there actions
are:
1- Increase sympathetic tone result in vasoconstriction and increase cardiac rate and
contractility.
2- Glycogenolysis, gluconeogenesis, (hyperglysemia)
3- ketolysis (break down of protein into AA)

7
4- lipolysis (break down of lipid into FA)
Corticosteroid:
Secreted from the adrenal cortex its actions are:
1- glycogenolysis, gluconeogenesis,
2- ketolysis.
3- lipolysis.
4- stabilize cell membrane and lysosoms.
5- Anti inflammatory action.
6- increase intravascular volume.
7- permissive effect to catecholamine
Renin angiotensin system:
Secreted from the distal convoluted tubule its actions are:
1- Vasoconstriction
2- Increase cardiac rate and contractility
3- Increase vascular permeability.
4- Stimulate aldosteron and vassopressin secretion.
Glucagon:
Secreted from the pancreas its actions are:
1- glycogenolysis, gluconeogenesis
2-lipolysis
3-ketogenesis.
4- inhibit insulin secretion
5- increase cardiac rate and contractility
Aldosteron:
from adrenal cortex, it increase water and sodium retention from the kidney.
Vassopressin:
from posterior pituitary gland its actions are:

8
1-Vasoconstriction
2-Increase cardiac rate and contractility.
Growth hormone:
from anterior pituitary gland its actions are:
1-Glycogenolysis, gluconeogenesis
2-Lipolysis
3-Ketogenesis
4-Promote action of caticholamine.
The aim of the neuro endocrine response are:
1- Hyper glycemia.
2- Production of amino acid(AA).
3- Production of fatty acid (FA).
4- Restore fluid and electrolyte.
5- Support cardiac function.
6-mentain vascular resistance.
The body response pass into 3 phases
1- The ebb phase:
it’s the first 24 to 48 hours after injury the aim is to restore circulation and prepare fuel for
the next phase. The metabolic changes are :
1- Glycogenolysis
2- Gluconeogenesis
3- Increase secretion of stress hormones.
4- Decrease secretion of insulin
The result of this changes are:
Hyperglysemia, water and sodium retention, increase vascular resistance, decrease urine
output and elevation of blood pressure.

9
2- The flow ( catabolic) phase:
Its started after 48 hours and may last several weeks depending on the severity of the
injury.
The metabolic changes are :
1- Increase in resting energy expenditure which is due to catecholamine, this results in
hypermetabolic state.
2- Increase oxygen consumption by tissue.
3- Increase secretion of stress hormones.
4- Hyperglycemia: which is needed for
A- CNS metabolism.
B- WBC and RBC nutrition.
C- Wound healing
D- Immune system function.
5- ketolysis ( protein break down) to AA which is used for
A- intermediates to gluconeogensis
B-provide AA for the syntheses of leukocytes and cellular proliferation.
6- lypolysis: degradation of fat to FA which is used for:
A- intermediates to gluconeogensis
B- energy substrate for muscles specially of respiration, heart and kidneys (non glucose
depended tissue)
3- anabolic phase:
It’s the last phase started after abolishing of infection and disappearance of pain and
subsiding of inflammation.
The body start to build its self again and return the functional capacity of the organ, it
needs along time to restore body protein and fat.
Its characterized by
1- increase body Wight
2- stabilization of cardiac output
3-returne of blood sugar to normal.
11
In summary the response to injury result in
1- Hyper metabolism
2- Hyperglycemia.
3- Hyper catabolism
The aim is to provide high circulating substrate (glucose, AA, FA)
but
On the expense of body tissue stores.
If the body support fail to meet the body requirement during the hyper metabolic phase,
the cellular energy level well decrease and result in
MULTIPLE ORGAN DYSFUNCTION SYNDROMAND MULTIPLE ORGAN FAILURE
