1
Third stage
Surgery
Lec-3
.د
مدثر
1/1/2014
Hemorrhage and Blood Transfusion
Objectives
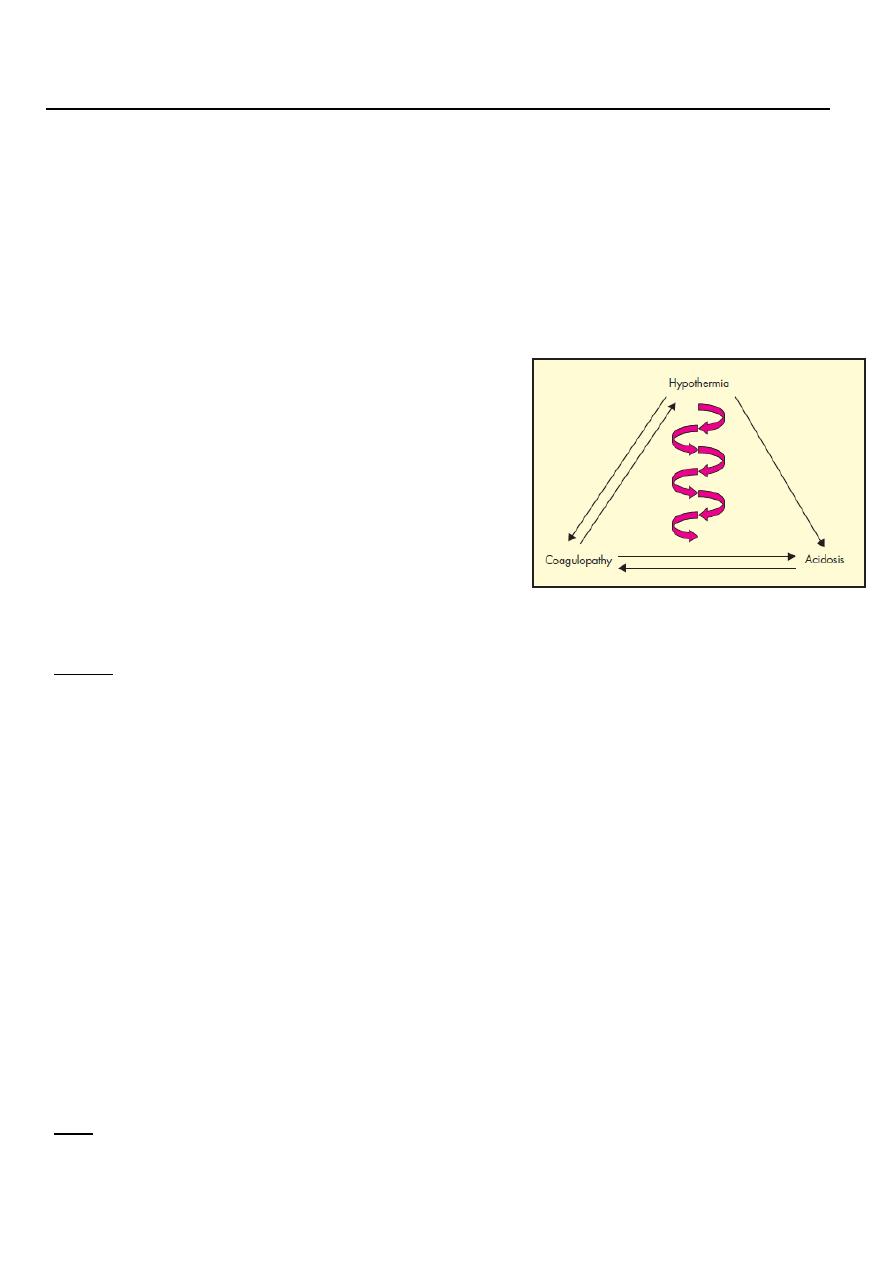
Define hemorrhage , triad of death
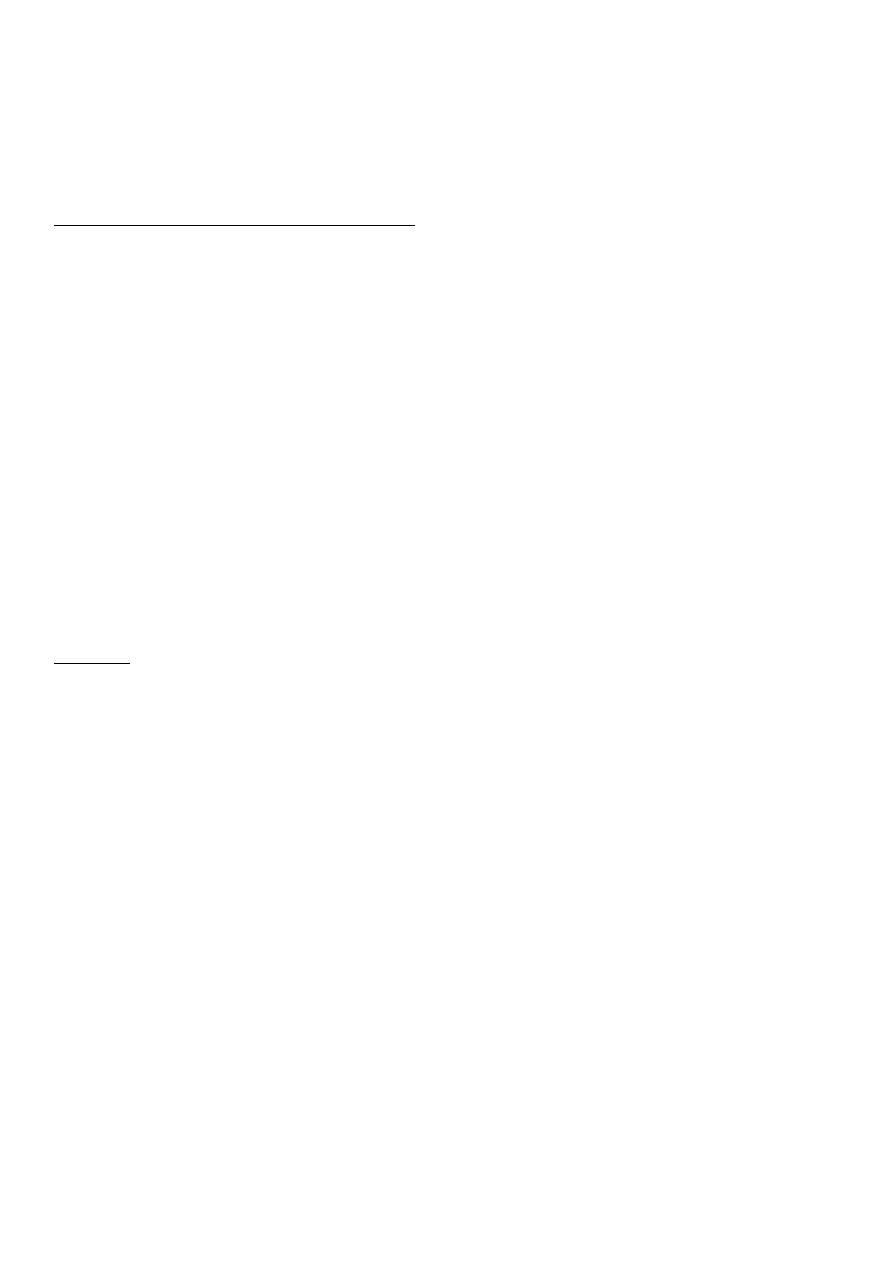
Know the classification of hemorrhage according to different criteria.
Understand the principles of management of blood loss.
Know the basic principles of blood groups
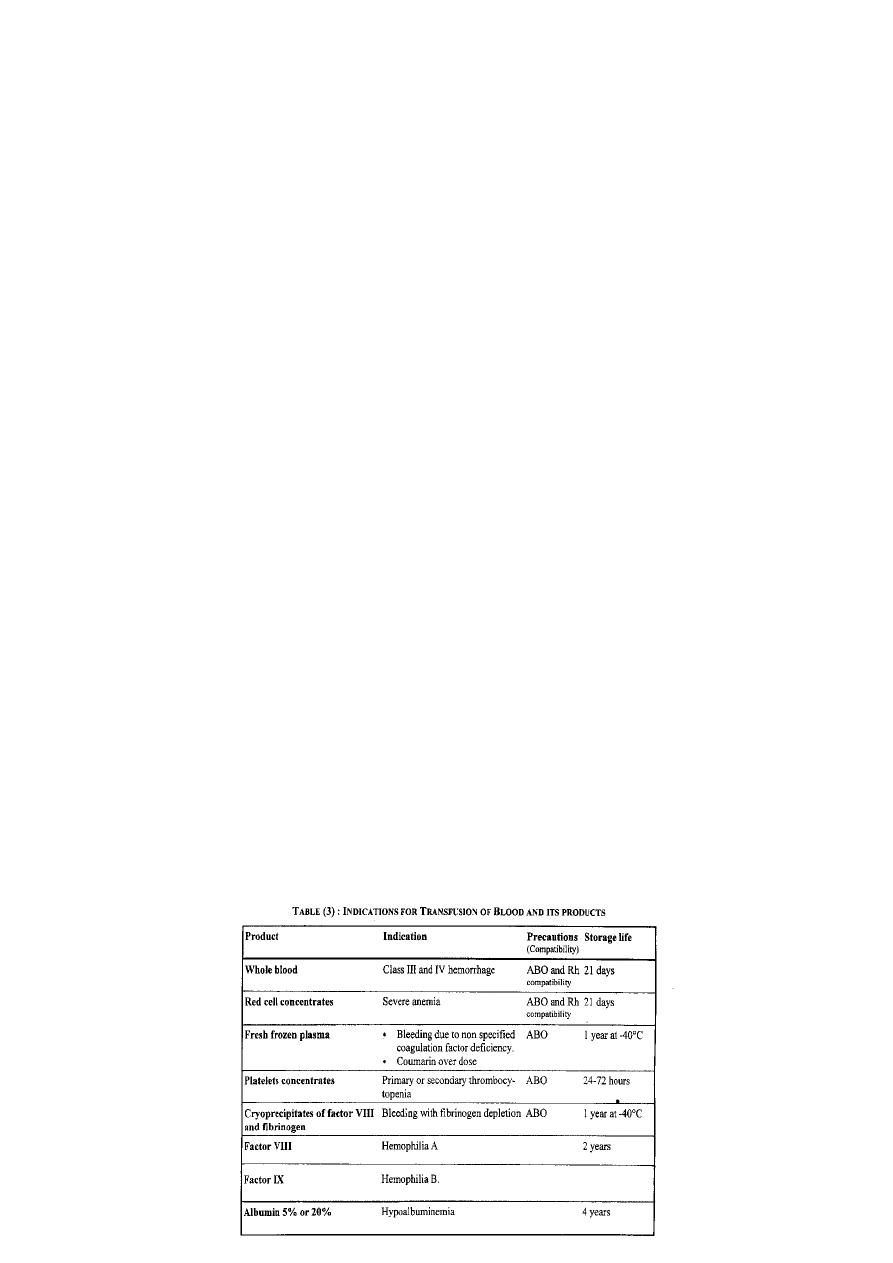
Know how to use blood and blood products
Understand the risks of blood transfusion
Hemorrhage
It is the escape of blood outside circulatory system
CLASSIFICATIONS
Origin:
1) Arterial:
The blood is bright red in color.
The blood comes in pulsatile jets (spurting).
The bleeding more from the proximal than the distal end.
2) Venous:
The blood is dark red in color.
The blood comes as a steady flow.
It is more from the distal than the proximal end.
EXCEPTIONS --- PULMONARY----COLOR
3) Capillary:
Bleeding occurs as diffuse ooze of bright red blood.
Site:
External: Bleeding is visible (revealed).
Internal: Bleeding is invisible(concealed)
2
o Could occur in body cavity e.g. peritoneal ,pleural,
o or it may occur into a tissue e.g. fracture hematoma (Interstitial hemorrhage)
o NOTE:
o A concealed hemorrhage may become revealed as in case of bleeding peptic
ulcer------ hematemesis or melaena.
Timing in relation to the onset of trauma:
Primary
o hemorrhage occurs at the time of trauma (injury or operation).
Reactionary
o Hemorrhage occurs within 24 hours after trauma usually (4-6 hours) .due to
o slipping of ligature, dislodgment of a clot or cessation of vasospasm.
o Precipitating factors are
1- rise in arterial blood pressure.
2-restlessness , cough and vomiting --- rise in venous pressure
Secondary
o Hemorrhage occurs one to two weeks after trauma due to infection and
sloughing of part of the wall of an artery .
o Predisposing factors:
1- drainage tube , fragment of bone or ligature in infected area or cancer.
2- More common in anorectal wounds e.g.hemorrhoidectomy
Etiology:
Traumatic: (surgical)
o Accidental
o Surgical operations
o Interventional procedures.
Pathological: (nonsurgical)
o Atherosclerotic (ruptured aortic aneurysm).
o Inflammatory (bleeding peptic ulcer).
o Neoplastic (hematuria in renal cancer).
o Bleeding diathesis can increase the amount of traumatic and pathological
bleeding,even can cause bleeding with little or no trauma (spontaneous
hemorrhage). Note anticoagulants and antiplatlets
Circulating blood volume
The adult human has approximately 5 litres of blood
(70 ml/ kg) children and adults
( 80 ml/ kg neonates).
3
Clinical Evaluation
Measuring blood loss (cont.)
Blood clot of clenched fist size= 500ml
Swelling of closed fracture e.g.
o Tibia= 500-1000ml
o Shaft of femur=500-2000ml
Swab weighing 1g=1ml after subtracting the dry weight. Note evaporation and other
fluid loss in operation.
Suction and drainage bottles
Central venous pressure measurement
Hemoglobin and packed cell volume level:
o Normal Hb ---12-16gm/100ml
o Normal pcv--- Hb x3 roughly
Poorly correlate with amount of blood loss in the immediate post hemorrhage period
TREATMENT OF HEMORRAHGE
Stop or Minimizing further blood loss
Pressure and packing .
Position and rest.
Intra –operative methods
VOLUME REPLACEMENT
Intravenous fluids
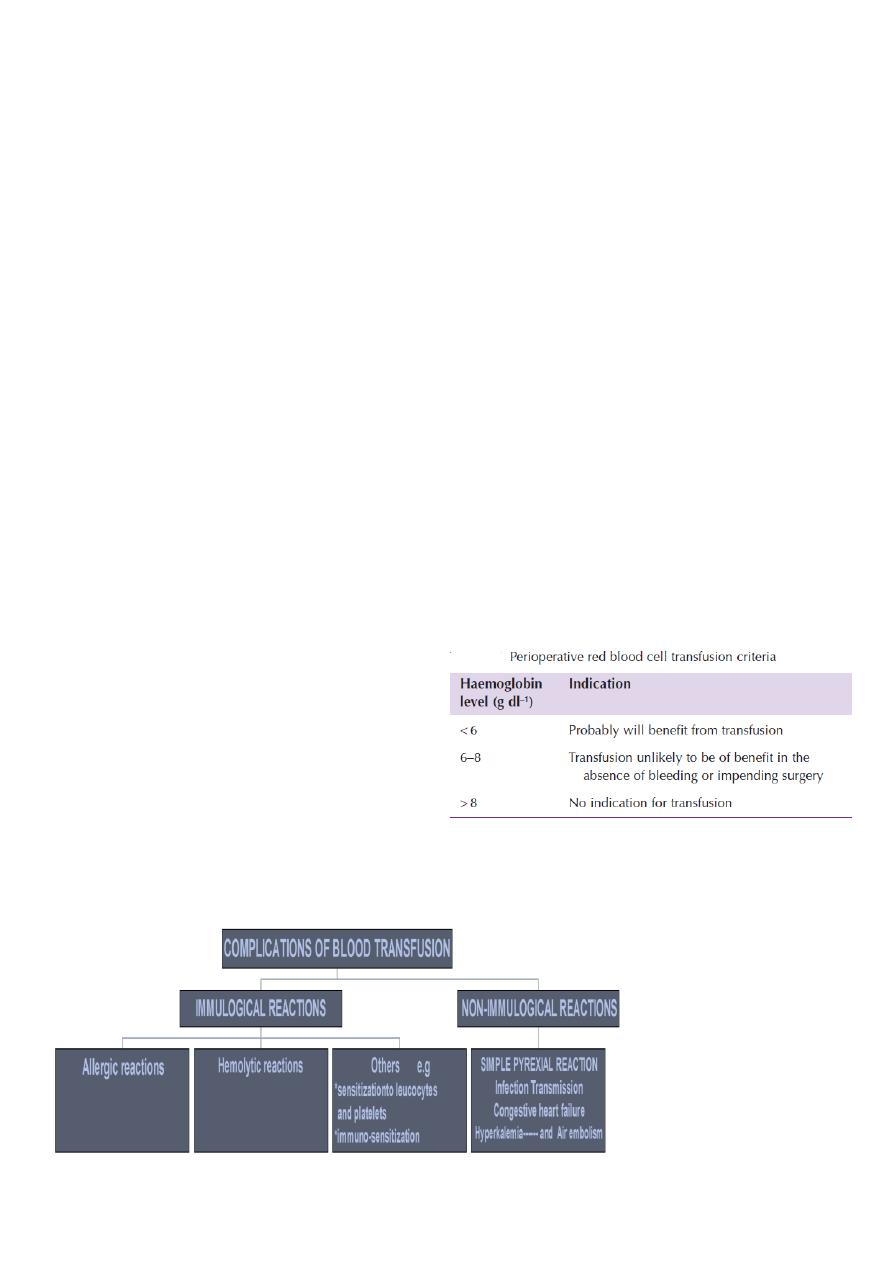
Blood transfusion
4
BLOOD TRANSFUSION
Blood grouping
Blood group antigens (sugars or proteins on red cell membranes)
ABO system
Group A have anti-B in their plasma
Group B have anti-A
Group O have anti-A and anti-B
Group AB have neither
Anti-A and B are naturally occurring IgM antibodies
Frequency of ABO Blood Groups
Group O 46%
Group A 42%
Group B 9%
Group AB 3%
The Rh Blood Group System
Described by Landsteiner in 1940
Antibodies produced as a result of pregnancy or transfusion
Immune antibodies - IgG
Can cause haemolytic disease of the newborn and transfusion reactions
First antigen discovered given the notation D
Other Blood Group Systems
Although ABO and Rh are the most important
Other systems are important if patient has the antibodies
Important systems are Kell, Duffy, Kidd and MNS
Antibodies can cause severe transfusion reactions
5
Procedure of blood transfusion
Donor selection.
Collecting blood from the donor.
Blood unit testing.
Blood storage.
o storage in blood bank.
o temp 4±2
O
C.
o Special bag containing 75ml anticoagulat solution --citrate phosphate dextrose
(CPD) or citrate phosphate dextrose +adenin.
o Note the temporary reduction in O
2
release.
Crossmatching/ Compatibility Testing
Patients plasma tested against donor red cells
Full procedure take one hour.
? Emergency .
Some blood banks are moving to computer crossmatching (electronic crossmatch)
Giving blood
Selection and preparation of the site .
Cannula insertion.
Check donor blood and patient I.D.
Detailed written instructions.
Note--- blood warming.
AUTO TRANSFUSION
Complications of Blood Transfusion

6
Complications Of Blood Transfusion
Simple pyrexial reaction, most common
o The patient develops chills, fever, headache, nausea and vomiting due to Some
pyrogens in the transfusion apparatus .
o Treatment : stop transfusion (Temporarily) and give antipyretics.
Congestive Cardiac failure,
o This is liable to occur in elderly persons especially if a large volume of blood is
administered too rapidly.
o It is recommended to transfuse packed red cells rather than whole blood to correct
anemia in elderly persons.
Allergic reactions.
o Range from mild itching and urticaria to a severe reaction with laryngeal edema
and collapse (anaphylaxis) .
o Etiology: due to the recipient's response to allergens in the donor's blood.
Blood transfusion should be stopped CHECK AND SEND FOR RECHECK
Treat shock if present ( adrenalin + crystalloids)
Antihistamin and corticosteroids
Hemolytic reactions.
o Etiology: due to:
The presence of antibodies in the recipient's blood against one or more of the
antigens of the donor's cells
Should be avoided by correct blood grouping ABO ,Rh and cross matching.
Nearly always due to human error.
o Clinical Picture of acute Hemolytic Reaction
Hemolytic reactions present after the transfusion of less than 50 ml by fever,
chills, flushing, constricting pain in the chest, dyspnea and pain in the flanks.
Examination reveals tachycardia and hypotension.
In anaesthetized patients the only manifestations of hemolytic reactions are
sudden tachycardia, hypotension and bleeding tendency.
A major hemolytic reactions will lead to hemoglobinuria, jaundice and acute
renal failure due to acute tubular necrosis.
o Management of acute hemolytic reaction:
Stop the infusion immediately Check patient and unit ID .
Send the donor's blood and a sample of the patient's blood for repeat typing
and cross matching in addition to Hb and bilirubin + patient urine shoul be send
for lab.
Correct the shock by infusion of crystalloid solution.
Insert a Foley's catheter and check that there is an adequate urine output. An
loop or osmotic diuretic as mannitol is given .
Keep an alkaline urine to protect against acute renal failure. IV infusion of
sodium bicarbonate is indicated.

7
Transmission of infection.
o Viral hepatitis (B or C). This is now the most feared complication. The virus can be
transmitted by whole blood or blood products. It is now obligatory to test the
donor for hepatitis viruses.
o AIDS: HIV infection can be transmitted by blood or by its products.
o Syphilis: This is now rare, Spirochetes cannot survive at the blood bank
temperature for more than 4 days.
o Malaria: The disease is transmitted only by red cells, not by blood components.
o Septicemia: Bacteria can survive, but they cannot multiply significantly in
refrigerated blood, However, if the blood is allowed to warm, bacteria can grow
and Gram-negative endotoxins can cause septicemic shock.
Massive blood transfusion
o Defined as the transfusion of blood that is greater in volume than a patient's
normal blood volume in less than 24 hours.
