1
Third stage
Medicine
Lec-1
د
.ا
س
ما
ع
يل
1/1/2014
Presenting problems in GIT diseases (part 1)
1. Dysphagia
2. Dyspepsia
3. Vomiting
4. Gastrointestinal bleeding
5. Diarrhea
6. Malabsorption
7. Weight loss
8. Constipation
9. Abdominal pai
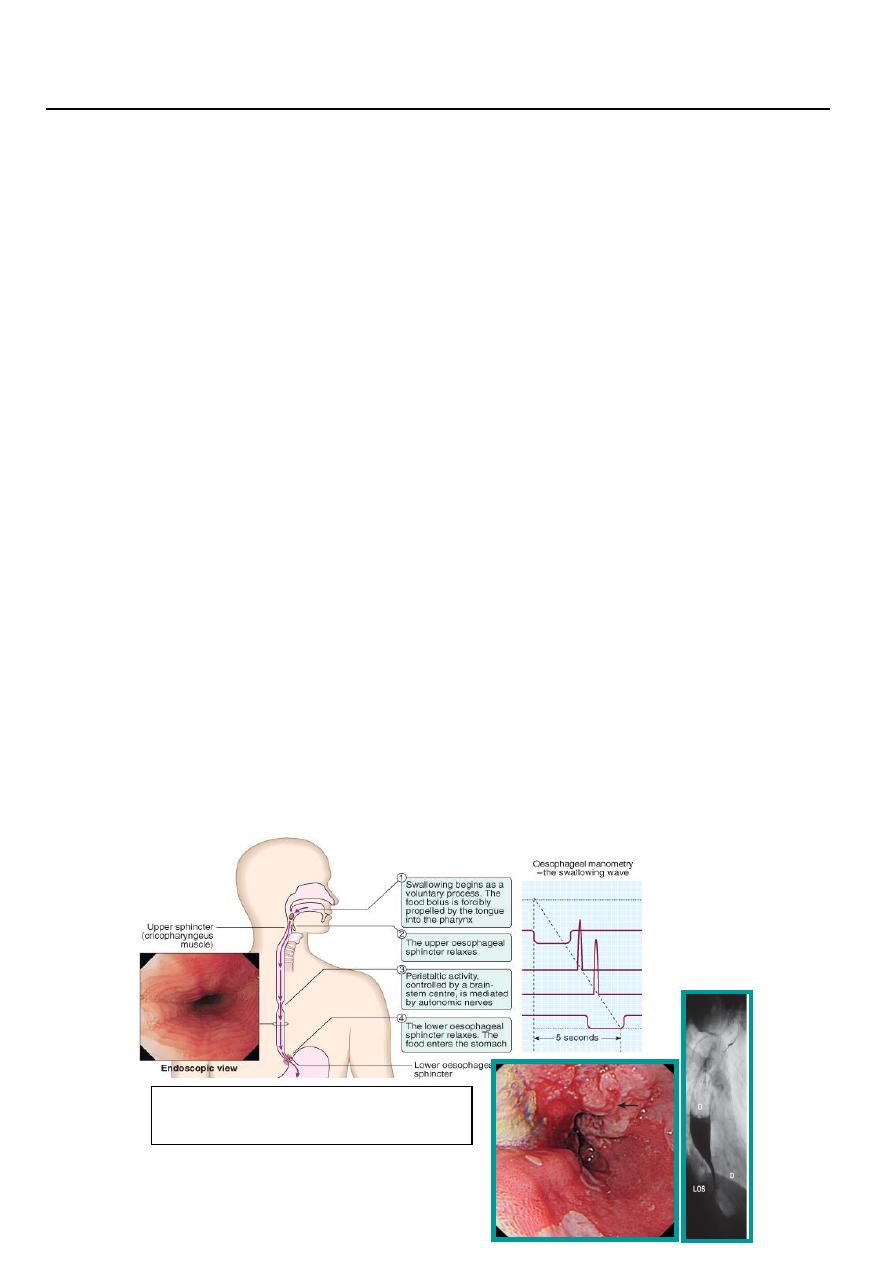
Dysphagia:
means difficulty in swallowing
Odynophagia: Painful swallowing usually due to GERD or Candidiasis.
Globus Hystericus: This is a condition in which anxious people feel a lump in the throat
Causes of dysphagia
1. Oropharyngeal: difficulty in initiation of act of swallowing, nasal regurgitation,
aspiration and chocking due to: e. g. Bulbar or pseudobulbar palsy and myasthenia
gravis.
2. Oesophageal causes: food sticking after swallowing but the level at which this is felt
correlates poorly with the true site of obstruction due to: e. g. structural diseases like
benign and malignant tumors, of oesophagus and strictures ( peptic ulcer, chemicals,..)
or it my be due to motility disorders like achalasia and oesophagitis (peptic or
candidiasis) or due to pressure from outside like lung tumour, cardiomegaly, aortic
aneurysm
Figure: Carcinoma of oesophgaus (left) and
barium swallowing showing achalasia (right)

2
Investigations
1. Endoscopy is the investigation of choice as biopsy can be taken and therapeutic
procedures like dilatation can be performed.
2. Barium swallow and Manometry for detection of motility disorders like achalasia.
Dyspepsia (indigestion)
Definition: dysphagia is chronic or recurrent pain or discomfort centered in the upper
abdomen.
Discomfort means:
• Bloating.
• Abdominal fullness.
• Early satiety, acidity, heartburn.
• Or nausea.
In dyspepsia:
• Detect symptoms suggest specific disorders like peptic ulcer.
• Detect “alarm features” (weight loss, anaemia, vomiting, haematemesis, dysphagia
and palpable abdominal mass) which need urgent endoscopy.
• Detect atypical symptoms more suggestive of other disorders like ischemic heart
disease.
Dyspepsia is an extremely common disorder in an otherwise healthy population. It has been
estimated that as many as 25% to 40% of adults will experience dyspepsia in a given year.
Although most individuals who experience dyspepsia symptoms do not seek medical
attention, approximately 25% do seek treatment, making the condition responsible for 4% to
5% of all primary care physician visits.
Due to the prevalence of the condition and the significant direct and indirect costs with which
it is associated, dyspepsia is a major healthcare concern all over the world.
Causes of dyspepsia
A. Common causes:
1.
Functional dyspepsia about 60% of cases.
2. Organic:
peptic ulcer diseases: 15-25%
.GERD: 5-15%
.Gastric or oesophageal cancer: 1-2%
3
B. Rare causes:
Pancreatic and hepato-biliary, colonic diseases, systemic diseases
like renal failure, hypercalcaemia, drugs (like NSAIDs, iron, digoxin) and alcohol
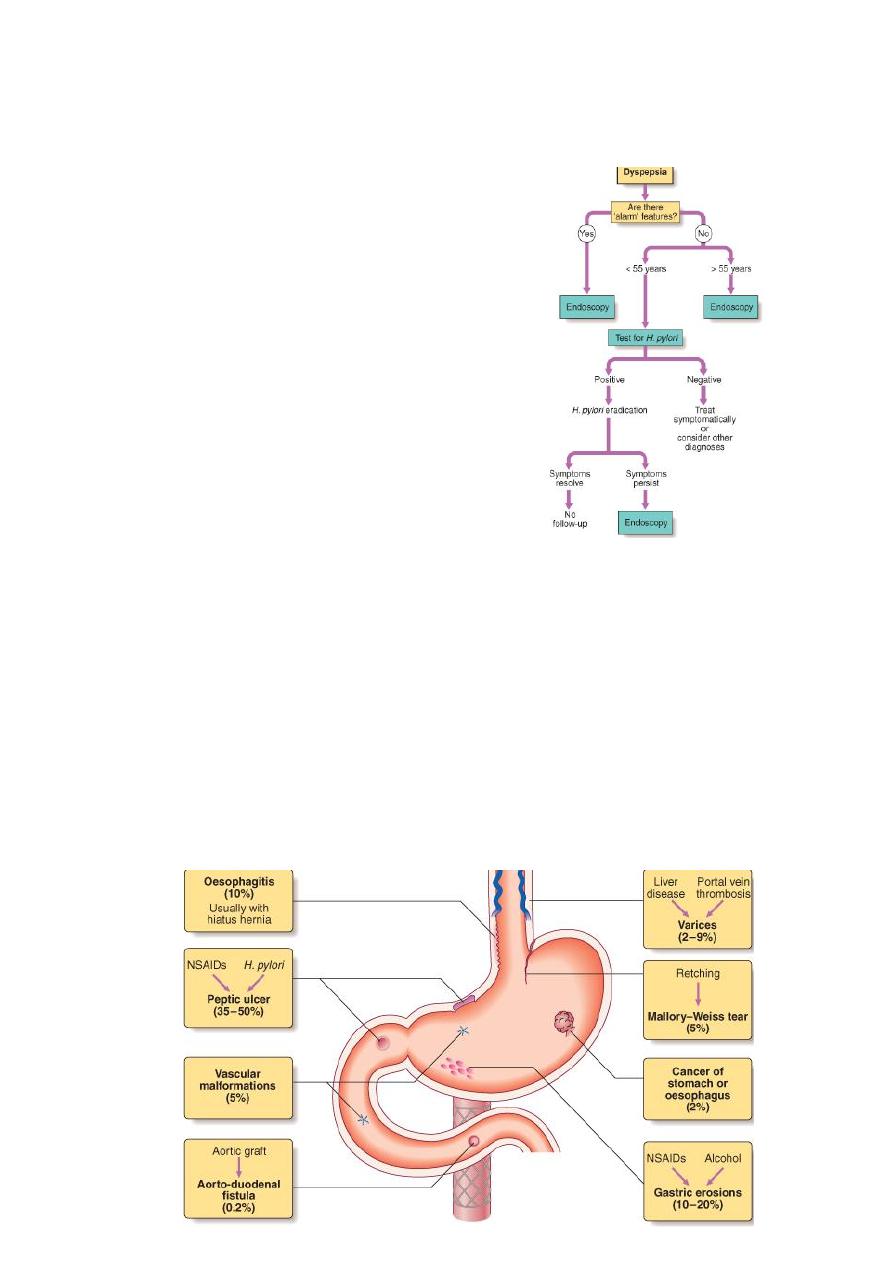
Investigation
1. Early endoscopy
If patient is above 55 years
Or alarm features are present
Or if patient (at any age) is not
responding to empiric therapy
for H. pylori
2. Test for H. pylori and Anti-
H. pylori (age below 55).
If it is positive
Or Symptomatic treatment if
Negative.
Upper GIT bleeding
• Haematemesis: Vomiting of blood, usually coffee ground materials due to partially
digested blood in stomach.
• Melena: Passage of tarry black stool per rectum. It also can be due to diseases of right
side of colon.
• It is an emergency condition and patient needs hospital admission.
• Upper GIT: areas proximal to ligament of Treitz ( usually oesophagus, stomach and
duodenum).
CAUSES

4
Management
1. Intravenous access using at least one large bore cannula.
2. Initial clinical assessment:
• Define circulatory status: severe bleeding causes tachycardia, hypotension, oliguria
and shock. The patient is cold and sweating and may be agitated.
• Seek evidence of chronic liver disease: Spider naevi, hepatosplenomegaly, jaundice
and ascites
• Define comorbidity: like heart, cerevascular diseases, renal diseases are important
because the risks of endoscopy and surgery are increased and also these conditions
become more worse after bleeding.
3. Blood tests:
• Full blood count: chronic or subacute bleeding leads to anaemia, but the haemoglobin
concentration may be normal after sudden major bleeding until haemodilution occurs.
• Urea and electrolytes: may show evidence of renal failure. Urea increases as absorbed
blood product from intestine metabolised by the liver.
• Liver function tests
• Prothrombin time: If there is evidence of liver disease or anticoagulant therapy.
• Cross-matching of at least 2 units of blood.
4. Resuscitation: Intravenous crystalloid fluids or colloid are given to restore the blood
pressure. Blood is transfused when the patient is shocked or when the haemoglobin
concentration is less than 100g/l.
Normal saline should be avoided in patient with chronic liver disease.
CVP (central venous pressure) monitoring is useful in severe bleeding especially if cardiac
disease is present to avoid fluid overload.
5. Oxygen: Given by face mask to all patients with shock.
6. endoscopy: This should be done after adequate resuscitation. A diagnosis will be achieved
in 80% of cases. Patients who are found to have major endoscopic stigmata of recent
haemorrhage can be treated endoscoply using heater probe, I njection of adrenaline (diluted)
into bleeding point and using of metalic clips. It can stop active bleeding and if IV proton
pump inhibitor is given in addition, it can prevent rebleeding and avoid need for surgery.
7. Monitoring: patient should be closely observed, with hourly pulse, BP and urine output
measurement.
8. Surgical operation: If bleeding not stopped or rebleeding occur in one occasion in elderly
or two occasions in young fit patient.
Prognosis
The mortality is about 10% after acute bleeding.
Risk factors:
1. Increasing age 2. Comorbidity 3. Shock 4. Diagnosis e. g. bleeding varices have worse
prognosis 5. Endoscopic finding of active bleeding and non-bleeding visible vessel associated
with high risk.5.Rebleeding: Associated with 10 fold rise in mortality.
Improved mortality can be achieved by specialised center and team work of physicians and
surgeons
