1
Third stage
Medicine
Lec-2
د
.
بشار
1/1/2014
Coma
Definition
Is a sleeplike state in which the patient makes no purposeful response to the environment
and from which he or she cannot be aroused.
The eyes are closed and do not open spontaneously. The patient does not speak, and there
is no purposeful movement of the face or limbs. Verbal stimulation aproduces no response.
Mechanical (e.g. painful) stimulation may produce no response or may elicit nonpurposeful
reflex movements mediated through spinal cord or brainstem pathways.
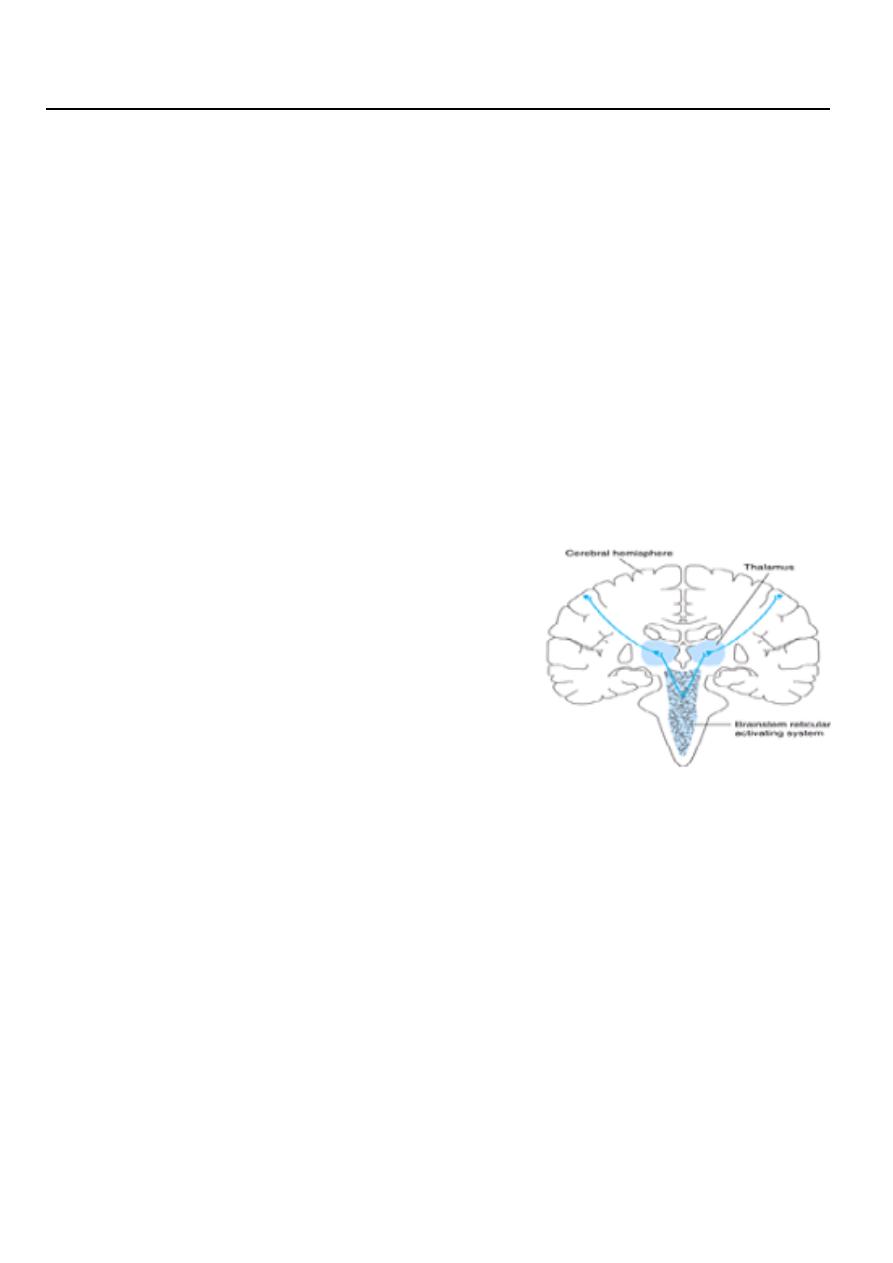
Anatomic basis of coma
Consciousness is maintained by the normal
functioning of the brainstem reticular activating
system above the mid pons and its bilateral
projections to the thalamus and cerebral
hemispheres.
Coma results from lesions that affect either the
reticular activating system or both hemispheres.
Pathophysiology
Coma results from a disturbance in the function of either the brainstem reticular activating
system above the midpons or both cerebral hemispheres since these are the brain regions
that maintain consciousness.
APPROACH TO MANAGEMENT
The approach to management of the comatose patient consists first of
emergency measures to stabilize the patient and treat certain life-threatening disorders,
followed by efforts to establish an etiologic diagnosis.
2
Ensure patency of the airway and adequacy of ventilation and circulation
If the airway is obstructed, the obstruction should be cleared and the patient intubated. If
there is evidence of trauma that may have affected the cervical spine, however, the neck
should not be moved until this possibility has been excluded by x-rays of the cervical spine.
In this case, if intubation is required, it should be performed by tracheostomy. Adequacy of
ventilation can be established by the absence of cyanosis, a respiratory rate greater than
8/min, the presence of breath sounds on auscultation of the chest, and the results of
arterial blood gas and pH studies . If any of these suggest inadequate ventilation, the
patient should be ventilated mechanically. Measurement of the pulse and blood pressure
provides a rapid assessment of the status of the circulation. Circulatory embarrassment
should be treated with intravenous fluid replacement, pressors, and antiarrhythmic drugs,
as indicated.
Insert an intravenous catheter and withdraw blood for laboratory studies
These studies should include measurement of serum glucose and electrolytes, hepatic and
renal function tests, prothrombin time, partial thromboplastin time, and a complete blood
count. Extra tubes of blood should also be obtained for additional studies that may be
useful in certain cases, such as drug screens, and for tests that become necessary as
diagnostic evaluation proceeds.
Begin an intravenous infusion and administer dextrose, thiamine, and naloxone
Every comatose patient should be given 25 g of dextrose intravenously, typically as 50 mL
of a 50% dextrose solution, to treat possible hypoglycemic coma. Since administration of
dextrose alone may precipitate or worsen Wernicke's encephalopathy in thiamine-deficient
patients, all comatose patients should also receive 100 mg of thiamine by the intravenous
route. To treat possible opiate overdose, the opiate antagonist naloxone, 0.4–1.2 mg
intravenously, should also be administered routinely to comatose patients.
Withdraw arterial blood for blood gas and pH determinations
In addition to assisting in the assessment of ventilatory status, these studies can provide
clues to metabolic causes of coma
Institute treatment for seizures, if present
Persistent or recurrent seizures in a comatose patient should be considered to represent
status epilepticus and treated accordingly
3
History
The most crucial aspect of the history is the time over which coma develops
1- A sudden onset of coma suggests a vascular origin, especially a brainstem stroke or
subarachnoid hemorrhage.
2- Rapid progression from hemispheric signs, such as hemiparesis, hemisensory deficit, or
aphasia, to coma within minutes to hours is characteristic of
intracerebral hemorrhage.
3- A more protracted course leading to coma (days to a week or more) is seen with tumor,
abscess, or chronic subdural hematoma.
4- Coma preceded by a confusional state or agitated delirium, without lateralizing signs or
symptoms, is probably due to a metabolic derangement.
Lateralizing (Focal) Signs
1- Assymmetry of pupils.
2- Squint
3- Assymmetry of the face
4- Gaze palsy
5- Assymmetry of motor response, reflexes & plantar response
Diseases that cause no focal or lateralizing neurologic signs
A. Intoxications: alcohol, barbiturates and other sedative drugs, opiates, etc.
B. Metabolic disturbances: anoxia, diabetic acidosis, uremia, hepatic failure, nonketotic
hyperosmolar hyperglycemia, hypo- and hypernatremia, hypoglycemia, addisonian crisis,
profound nutritional deficiency, carbon monoxide, thyroid states including Hashimoto
encephalopathy
C. Severe systemic infections: pneumonia, peritonitis, typhoid fever, malaria, septicemia,
WaterhouseFriderichsen syndrome.
D. Circulatory collapse (shock) from any cause.
E. Postseizure states and convulsive and nonconvulsive status epilepticus
F. Hypertensive encephalopathy and eclampsia
G. Hyperthermia and hypothermia. state,
H. Concussion
I. Acute hydrocephalus

4
Diseases that cause focal brainstem or lateralizing cerebral signs
A. Hemispheral hemorrhage or massive infarction
B. Brainstem infarction due to basilar artery thrombosis or embolism
C. Brain abscess, subdural empyema, Herpes encephalitis
D. Epidural and subdural hemorrhage and brain contusion
E. Brain tumor
F. Cerebellar and pontine hemorrhage.
G. Miscellaneous: cortical vein thrombosis, viral encephalitis (herpes), focal embolic
infarction due bacterial endocarditis,
A. Subarachnoid hemorrhage from ruptured aneurysm.
B. Acute bacterial meningitis
C. Some forms of viral encephalitis
General Physical Examination
A. SIGNS OF TRAUMA
1- Inspection of the head may reveal signs of basilar skull fracture, including the following:
a. Raccoon eyes—Periorbital ecchymoses.
b. Battle's sign—Swelling and discoloration overlying the mastoid bone behind the ear.
c. Hemotympanum—Blood behind the tympanic membrane.
d. Cerebrospinal fluid (CSF) rhinorrhea or otorrhea—Leakage of CSF from the nose or ear.
CSF rhinorrhea must be distinguished from other causes of rhinorrhea, such as allergic
rhinitis. It has been suggested that CSF can be distinguished from nasal mucus by the higher
glucose content of CSF, but this is not always the case.
The chloride level may be more useful, since CSF chloride concentrations are 15–20 meq/L
higher than those in mucus.
2- Palpation of the head may demonstrate a depressed skull fracture or swelling of soft
tissues at the site of trauma.
B. BLOOD PRESSURE
Elevation of blood pressure in a comatose patient may reflect long-standing hypertension,
which predisposes to intracerebral hemorrhage or stroke. In the rare condition of
5
hypertensive encephalopathy, the blood pressure is above 250/150 mm Hg in chronically
hypertensive patients.
Elevation of blood pressure may also be a consequence of the process causing the coma, as
in intracerebral or subarachnoid hemorrhage or, rarely, brainstem stroke.
C. TEMPERATURE
Hypothermia can occur in coma caused by ethanol or sedative drug intoxication,
hypoglycemia, Wernicke's encephalopathy, hepatic encephalopathy, and myxedema.
Coma with hyperthermia is seen in heat stroke, status epilepticus, malignant hyperthermia
related to inhalational anesthetics, anticholinergic drug intoxication, pontine hemorrhage,
and certain hypothalamic lesions.
D- Examination of skin
Pallor, Jaundice, Cyanosis, Purpura, Needle marks, Pigmentations…etc.
E- Breathing
1- Pattern : Air hunger
Cheyne- stokes
2- Smell : Drugs
Alcohol
Acetone smell
Fetor hepaticus
F. SIGNS OF MENINGEAL IRRITATION
Signs of meningeal irritation [eg, nuchal rigidity or the Brudzinski sign are of great
importance in leading to the prompt diagnosis of
meningitis or subarachnoid hemorrhage, but they are lost in deep coma.
G.PUPIL SIZE :
constricted; Pontine hemorrhage
Organophosphorous
poisioning
dilated; Anticholinergic drugs
H. OPTIC FUNDI
Examination of the optic fundi may reveal papilledema or retinal hemorrhages compatible
with chronic or acute hypertension or an elevation in intracranial pressure.
Subhyaloid (superficial retinal) hemorrhages in an adult strongly suggest subarachnoid
hemorrhage

6
DROWSINESS
STUPOR
CONFUSION
SEMICOSCIOUSNESS
Glasgow Coma Scale
