1
Third stage
Medicine
Lec-1
د
.
ح
سين
1/1/2014
Toxoplasmosis
Toxoplasma gondii
Intracellular protozoan .The species designation originated from the name of the North
African rodent (Ctenodactylus gondi) from which this parasite was isolated.
The genus name is derived from the Greek word toxon, meaning "bow" crescent shape
of the organism.
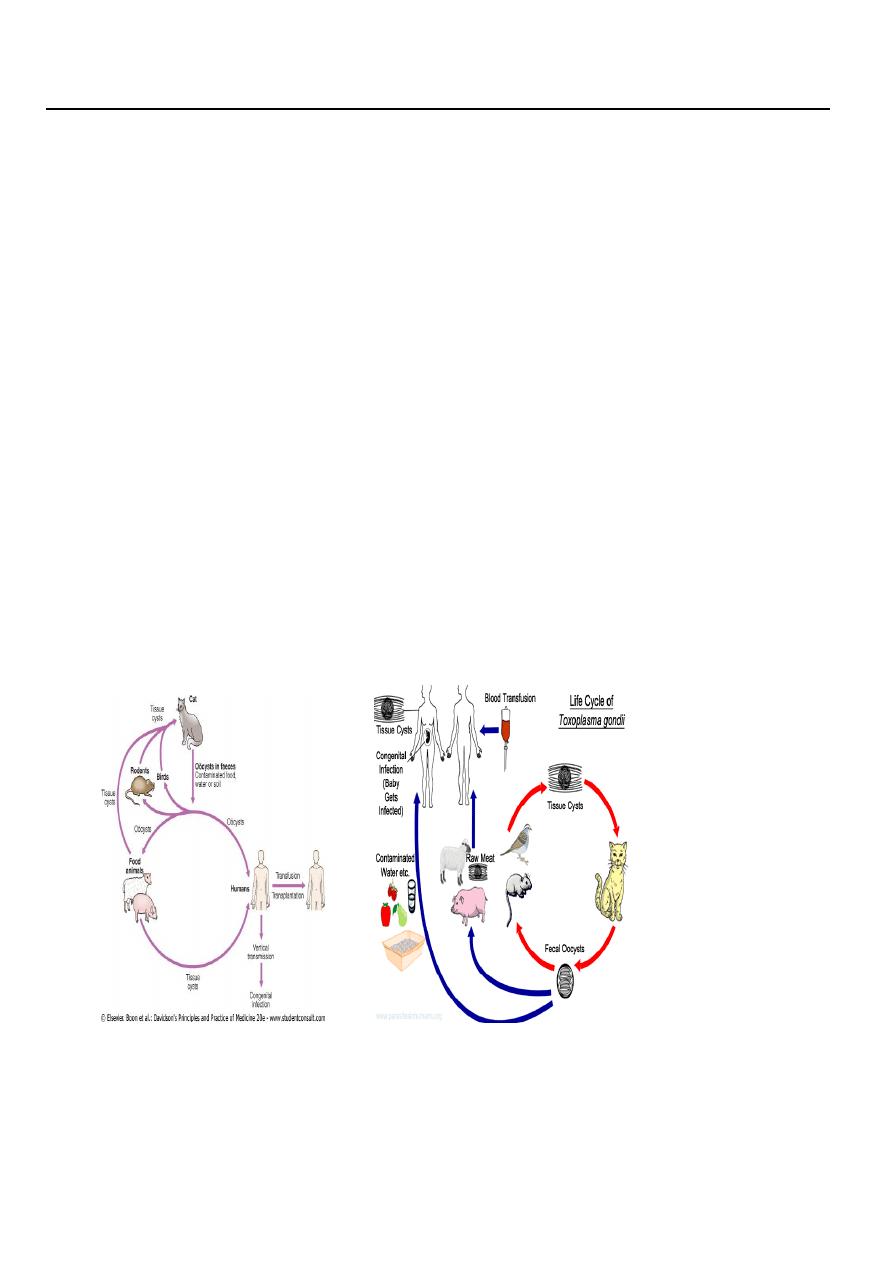
The sexual phase of the parasite's occurs in the small intestinal epithelium of the
domestic cat (definitive host).
Oöcysts are shed in cat faeces and are spread to intermediate hosts (pigs, sheep and
humans) through contamination of soil.
Oöcysts survive in moist conditions for weeks or months.
Once ingested by the intermediate hosts, the parasite transforms into rapidly dividing
Tachyzoites (asexual multiplication).
This leads to the formation of microscopic tissue cysts containing bradyzoites, which
persist for the lifetime of the host.
Cats become infected or Reinfected ((and shed oocysts))after ingesting any of the three
infectious stages of T. gondii ((in prey such as rodents and birds)) i.e., tachyzoites,
bradyzoites, and sporozoites.
Human acquisition of Infection occurs via
oöcyst-contaminated soil, salads and vegetables, water.
or by the ingestion or tasting raw or undercooked meats containing tissue cysts.
or blood transfusion and organ transplantation (very rare)

2
In developed countries, toxoplasmosis is the most common protozoal infection; around
22% of adults in the UK are seropositive. Account for about 15% of heterophile antibody-
negative glandular fever.
In India or Brazil, approximately 40-60% of pregnant females are seropositive .
In HIV infection, toxoplasmosis is an important opportunistic infection with considerable
morbidity and mortality.
Most primary infections are subclinical.
Clinical features
1- In most immunocompetent individuals, including children and pregnant women, the
infection goes unnoticed.
3- In approximately 10% of patients it causes a self-limiting illness. The most common
presenting feature is painless lymphadenopathy. In particular, the cervical nodes, but
mediastinal, mesenteric or retroperitoneal groups may be affected.
Most patients have no systemic symptoms, but Some complain of malaise, fever, fatigue,
muscle pain, sore throat and headache, resolution usually occurs within a few months,
although symptoms and lymphadenopathy tend to fluctuate and some do not recover
completely for ayear or more. The spleen is seldom palpable.
3- Very infrequently, patients may develop encephalitis, myocarditis, polymyositis,
pneumonitis or hepatitis.
Retinochoroiditis is nearly always the result of congenital infection but has also been
reported in acquired disease.
Congenital toxoplasmosis
Toxoplasmosis is once a lifetime infection.
Seropositive females infected 6 months before conception have no risk of fetal
transmission.
Acute toxoplasmosis, mostly subclinical, affects 0.3-1% of pregnant women, with an
approximately 60% transmission rate.
Congenital disease affects approximately 40% of infected fetuses. more severe with
infection early in gestation .
Many fetal infections are subclinical at birth but long-term sequelae include
1. Retinochoroiditis.
2. Microcephaly .
3. Hydrocephalus .
Investigations
1. In immunocompromised patients, the diagnosis often requires direct detection of
parasites.
2. Serology is often used in immunocompetent individuals.
a. The Sabin-Feldman dye test (indirect fluorescent antibody test), detects IgG antibody.
Recent infection is indicated by a fourfold increase in titre when paired sera are tested in
parallel. Peak titres of 1/1000 or more are reached within 1-2 months of the onset of
infection, the test then becomes an unreliable indicator of recent infection.

3
b. Toxoplasma-specific IgM antibody may be useful in confirming acute infection. False
positives or persistence of IgM antibodies for years after infection make interpretation
difficult.
Negative IgM antibodies virtually rule out acute infection .
3. During pregnancy, it is critical to differentiate between recent and past infection; IgG
avidity antibodies from infections older than four months bind tightly with the antigens,
while IgG avidity antibodies from infections acquired in the past four months form weaker
bonds , so the presence of high-avidity IgG antibodies excludes infection acquired in the
preceding 3-4 months .
4. The presence of organisms in a lymph node biopsy can be sought by staining sections
histochemically with T. gondii antiserum, or by the use of PCR to detect Toxoplasma-
specific DNA.
Management
In immunocompetent subjects uncomplicated toxoplasmosis is self-limiting and responds
poorly to antimicrobial therapy.
Treatment with pyrimethamine, sulfadiazine and folinic acid is therefore usually reserved
for rare cases of severe or progressive disease, and for infection in immunocompromised
patients .
In a pregnant woman
with an established recent infection, spiramycin (3 g daily in divided doses) should be given
until term.
Once fetal infection is established, treatment with sulfadiazine and pyrimethamine plus
calcium folinate is recommended (spiramycin does not cross the placental barrier).
There is insufficient evidence to determine the effects on mother or baby of current
antiparasitic treatment for women who seroconvert in pregnancy .
How likely is a baby to contract congenital toxoplasmosis?
1. Shortly before conception (within 2–3 months)
Infection shortly before conception carries a 1% or below risk of transmission to the
fetus, but a high risk of miscarriage if the fetus does become infected.
2.The first trimester
There is a 15% chance of the baby having congenital toxoplasmosis. consequences will be
severe in two thirds
3.The second trimester
The figure rises to a 25%. nearly 10 % will be severe
4.The third trimester
There is a 65% chance of the baby contracting congenital toxoplasmosis, , and none will
be severe .
To avoid toxoplasma during pregnancy?
In light of the severity of the potential consequences for the unborn child, it is imperative
that pregnant women who have never contracted toxoplasmosis, i.e. who are seronegative,
should not contract the disease during pregnancy.

4
Here are some tips can reduce the number of toxoplasmosis infections by two
thirds during pregnancy.
1. Do not allow your cat to go outside your home where it may come into contact with
toxoplasma. If possible, have someone else take care of your cat while you are pregnant.
2. Have another family member change the cat litter box and then disinfect it with boiling
water for 5 minutes.
3. Feces of cats should be removed daily before oocysts sporulate and become infective.
4. Use work gloves when gardening and wash your hands afterwards.
5. Avoid eating raw or undercooked meat and unwashed fruits and vegetables.
6. Wash your hands thoroughly before you eat and after handling raw meat, soil, sand or
cats. because water will kill the stages of T gondii that are found in meat.
7. Avoid rubbing your eyes or face when preparing food, and wipe the counter clean
afterwards.
8. Control flies and cockroaches as much as possible. They can spread contaminated soil or
cat feces onto food.
9. Avoid eating raw eggs and drinking unpasteurized milk. .
10. Meat should be cooked to 66℃ (152℉) or higher or frozen for a day in a household
freezer; both these measures are lethal to tachyzoites and bradyzoites.
Giardiasis
Infection with Giardia intestinalis, also known as G. lamblia, is found world-wide. It
particularly affects children, tourists and immunosuppressed individuals. The cysts remain
viable in water for up to 3 months.
Infection usually occurs by ingesting contaminated water.
The parasites attach to the duodenal and jejunal mucosa, causing inflammation.
Clinical features
After an incubation period of 1-3 weeks, there is diarrhoea, abdominal pain, weakness,
anorexia, nausea and vomiting.
On examination there may be abdominal distension and tenderness.
INVESTIGATIONS
1. Stools should be examined for cysts.
2. Duodenal or jejunal aspiration by endoscopy gives a higher diagnostic yield.
3. The 'string test' may be used, in which one end of a piece of string is passed into the
duodenum by swallowing, retrieved after an overnight fast, and expressed fluid
examined for the presence of G. lamblia trophozoites.
4. A number of stool antigen detection tests are available.
5. On jejunal biopsy fresh mucus examination may show Giardia on the epithelial
surface.
Management
Treatment is with a single dose of tinidazole 2 g.
or metronidazole 400 mg 8-hourly for 10 days.
