
1
Fifth stage
Gynecology
Lec-3
.د
احمد جاسم
4/11/2015
Abnormal Uterine Bleeding
It is a descriptive term applied to any alteration in the normal pattern of menstrual flow and
it is the uterine bleeding that is abnormal in amount, duration or timing. The abnormalities
of menstruation are only symptoms and do not describe pathological entities.
<21d 21-35d >35d ≥6 m
Polymenorrhoea Normal Oligomenorrhoea Amenorrhoea
Amenorrhoea: absence of menstruation for ≥6 months.
Oligomenorrhoea: menses at interval of >35 days is usually caused by a prolonged follicular
phase.
Polymenorrhoea: is a frequent menstruation as menses occurring at < 21 days interval
associated with a shortened follicular phase or inadequate luteal phase.
Menorrhagia > 80ml blood loss: heavy, regular blood loss occurring over several consecutive
cycles. More than 80 ml per period. Because of the practical difficulties of measuring
menstrual blood loss, subjective diagnosis based on the history is generally accepted as the
basis of management.
Metrorrhagia: irregular intervals with excessive flow and duration.
Intermenstrual bleeding: Uterine bleeding of variable amounts occurring between regular
menstrual periods.
Midcycle spotting: is scanty intermenstrual discharge occurring just before ovulation that is
associated with a decrease in estrogen at midcycle.
Postcoital bleeding: is non-menstrual bleeding that occurs immediately after sexual
intercourse.
Withdrawal bleeding: bleeding occurred after stopping oestrogen and progesterone use or
progesterone use.
Postmenopausal bleeding - Recurrence of bleeding in a menopausal woman at least 6
months to 1 year after cessation of cycles.

2
Aetiology of abnormal uterine bleeding:
A. Organic causes:
1. Local disorders:
Uterine fibroids.
Endometrial/ Endocervical polyp.
Adenomyosis.
Pelvic endometriosis.
Intrauterine device (IUD).
Pelvic inflammatory disease (PID).
Cervicitis.
Polycystic ovary disease
Oestrogen-secreting ovarian tumour. (Granulosa or theca cell tumour).
Cervical carcinoma.
Uterine body carcinoma.
Trauma of lower genital tract.
Urethral caruncle.
2. Systemic disorders:
Pregnancy: Should be considered in women of reproductive life in any patient
presenting with abnormal uterine bleeding.
Endocrine disorders may interfere with normal feedback mechanisms that
regulate
secretion
of
gonadotrophin-releasing
hormone
(GnRH),
gonadotrophin, and sex steroid.
A. Thyroid disorder (Hypothyroidism or hyperthyroidism).
B. Diabetes mellitus.
C. Adrenal disease.
D. Cushing disease
E. Prolactin disorders.
Haemostasis disorder:
A. Willebrand's disease.
B. Idiopathic Thrombocytopenic purpura (ITP).
C. Deficiencies of factors 11, V, VII, X1.
D. Myeloproliferative disorders.
Liver disorder (may interfere with metabolism of oestrogen, reduced
coagulation factors).
Renal disease (alter excretion of oestrogen and progesterone).
Medications as steroid hormones, neuroleptics, anticoagulants and cytotoxic
agents, contraceptive method.

3
Contraceptive method:
Oral contraceptives method: Breakthrough bleeding may occur in patients taking oral
contraceptives that have low doses of estrogen and progestin. Intermenstrual bleeding may
occur secondary to missed pills, varied ingestion times, and drug interactions.
Progesterone-only compounds
An iatrogenic cause of DUB is the use of progestin-only compounds for birth control.
Medroxyprogesterone acetate (Depo-Provera), a long-acting injection given every 3 months,
inhibits ovulation. An adverse effect of this drug is prolonged uterine breakthrough bleeding;
this may continue after discontinuation of the drug because of persistent anovulation.
The Norplant system (surgically implanted levonorgestrel), which acts to block some but not
all ovulatory cycles, has the same adverse effects as Depo-Provera.
Intrauterine device (IUD): Can cause menorrhagia.
Psychological and emotional cause, Excessive exercise, stress, and weight loss.
All these can cause hypothalamic suppression leading to abnormal uterine
bleeding due to disruption along the hypothalamus-pituitary-ovarian pathway.
B. Non –organic cause (Dysfunctional uterine bleeding (DUB) no specific organic cause can
be found.
Dysfunctional uterine bleeding
Is defined as abnormal uterine bleeding in the absence of organic disease.
It is the most common cause of abnormal vaginal bleeding during a woman's
reproductive years.
Bleeding is most common at the extreme ages of a woman's reproductive years, either
at the beginning or near the end, but it may occur at any time during her reproductive
life.
It is a diagnosis of exclusion.
Types of dysfunctional uterine bleeding:
Anovulatory DUB (90%).
Ovulatory DUB regular cyclicity) 10% of cases
4
Anovulatory dysfunctional uterine bleeding
All causes of anovulation represent a progesterone-deficient state results from a disturbance
of the normal hypothalamic-pituitary-ovarian axis and is particularly seen at extreme of
reproductive life (i.e. post menarchal (due to immature hypothalamic-pituitary axis) and
perimenopausally in patients who are 40 years or older (where the number and quality of
ovarian follicles decrease and altered).
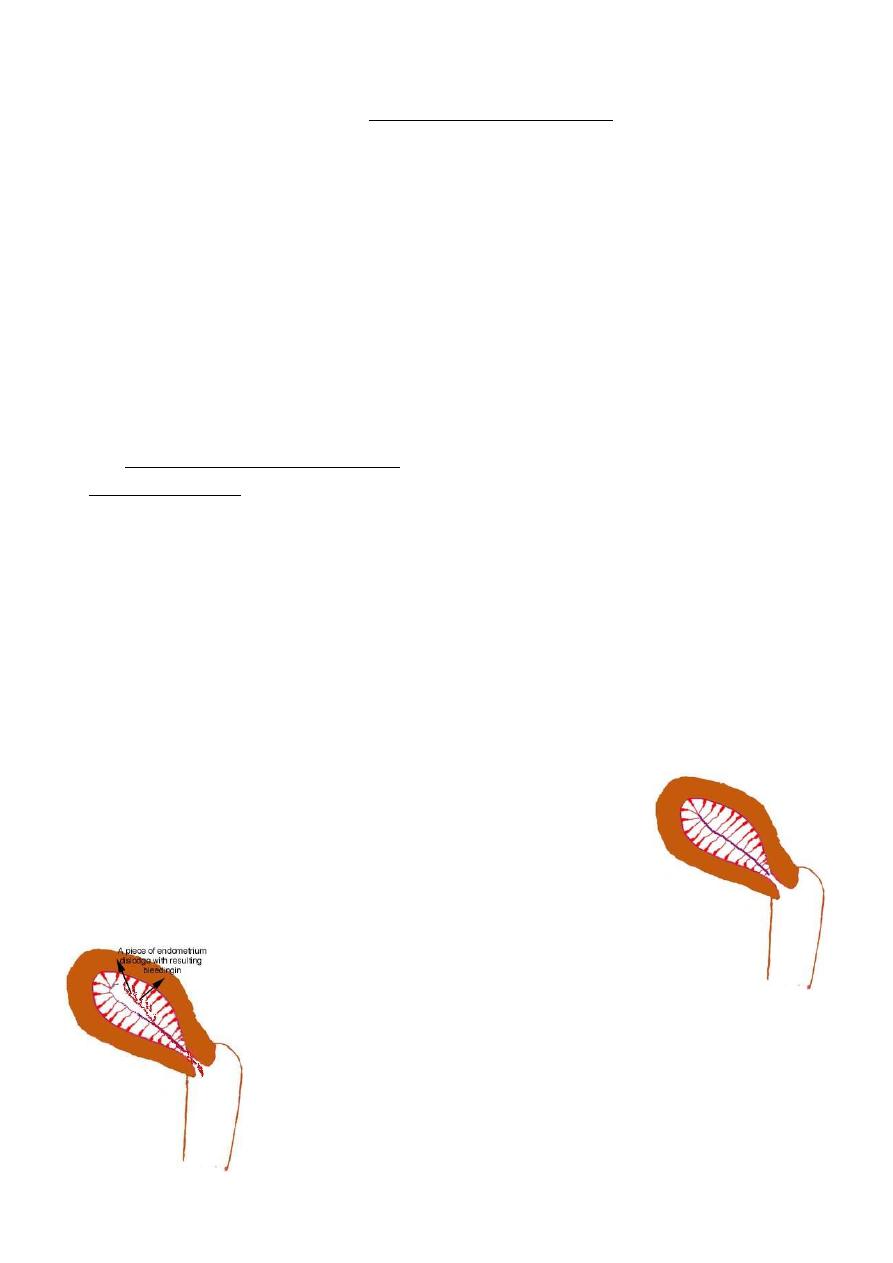
Pathophysiology in anovulatory DUB are:
Estrogen breakthrough bleeding. Persistant ovarian follicle
Prolonged cycle, period of amenorrhoea followed by excessive bleeding)
Estrogen breakthrough bleeding. Persistant ovarian follicle
There is adequate secretions of estrogen but ovulation does not occur and no corpus luteum
so no progesterone thus the endometrium will not stabilized; thus, proliferative
endometrium persists and the endometrium is thick, very vascular, very fragile and
spontaneously bleeds at various sites and bleeding is random (not universal) one site heals
the other breakdown and bleeding is continuous, as no progesterone so there is no self-limit
of bleeding. All this make bleeding episodes become prolonged, irregular, and sometimes
heavy bleeding and amenorrhea are common.
Unopposed estrogen may continue to secreted and result in continuing proliferation of
endometrium. If high level maintained could cause endometrial hyperplasia and eventually
endometrial carcinoma. For that reason endometrial sampling is mandatory in all cases of
DUB particularly in older premenopausal women.
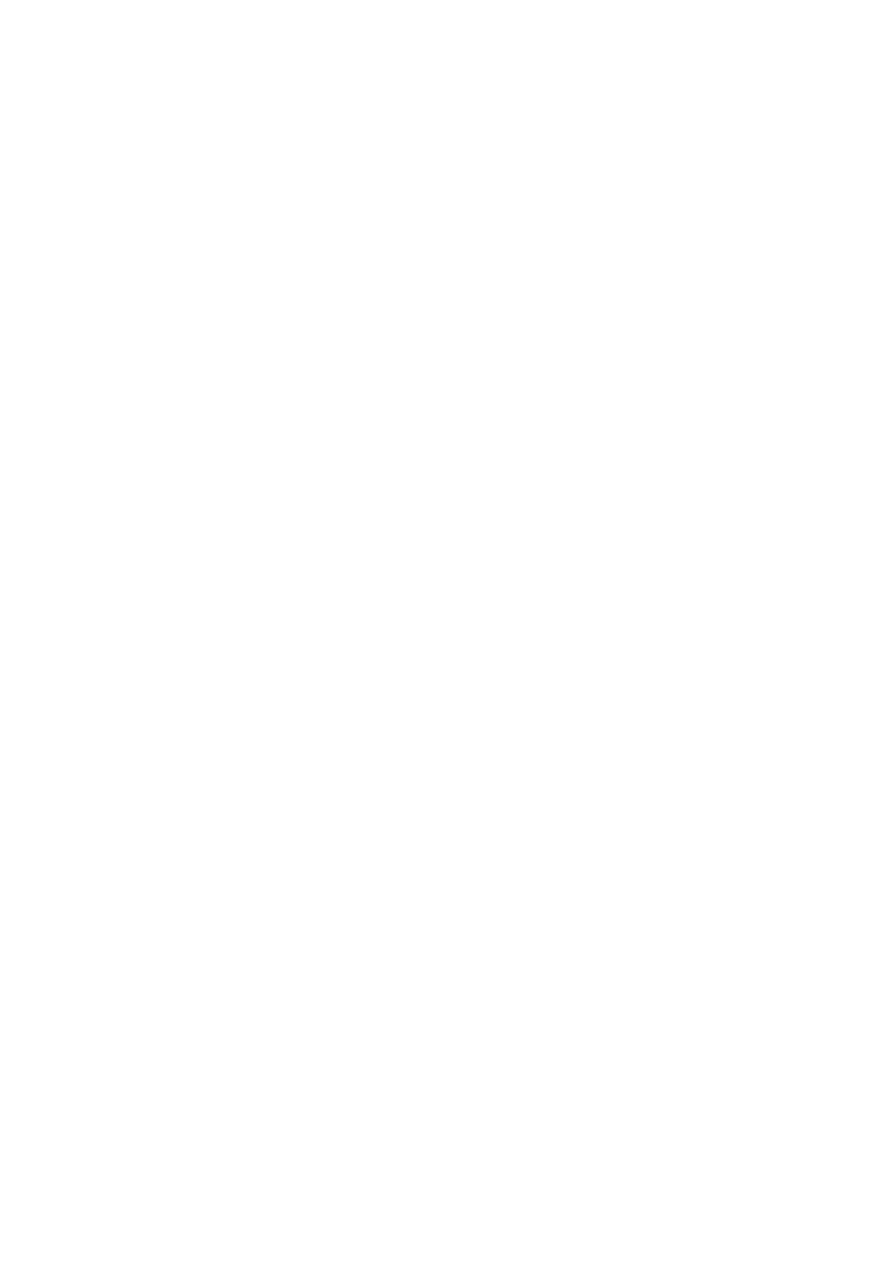
Thick endometrium seen in continuous estrogen stimulation.
The follicles might developed but they do not rupture. Estrogen
is produced but it is not opposed by progesterone and the
endometrium becomes thick. In the latter case there is usually
one or many estrogen producing follicles present.
Prolonged bleeding in a case of an overstimulated endometrium.
5
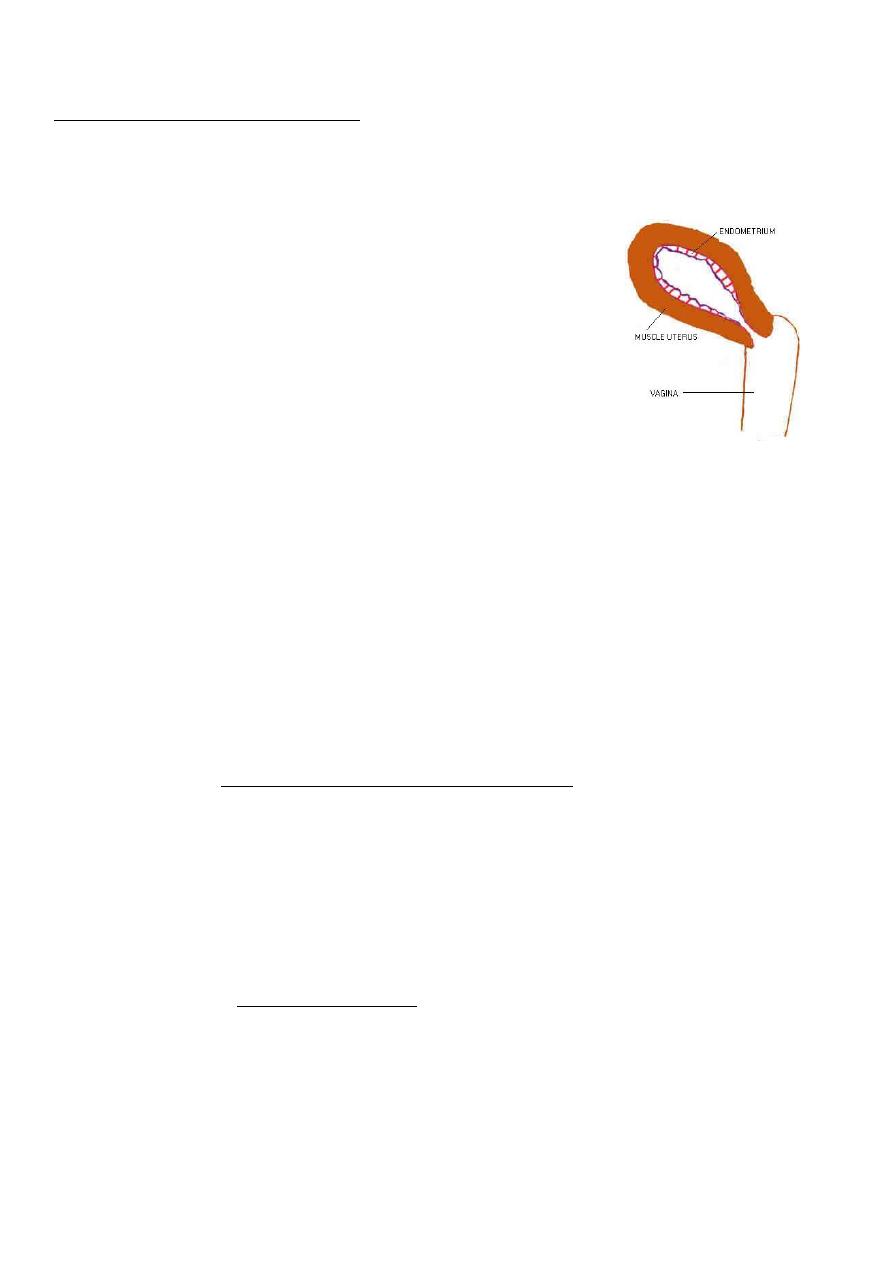
Insufficient follicular development:
Inadequate production of estrogen and inadequate proliferation of endometrium without
any secretary change result in deficient or atrophic endometrium. Large venules situated
superficially under thin endometrium which may ruptured and may be the commonest cause
of post-menopausal bleeding (PMB) and most common in premenopausal women.
Thin endometrium seen in the absence of estrogen.
The follicles do not develop and no estrogen are produced.
In this case the endometrium will be thin.
Ovulatory dysfunctional uterine bleeding
More common in women aged 35-45 years and is typified by regular heavy and painful
menstrual periods (menorragia, dysmenorrhoea).
Pathophysiology of ovulatory DUB:
Corpus luteum insuffiency: luteal phase deficiency
menorhgia, premenstrual spotting and/or shortening of menstrual cycle, prolongation
of menstrual bleeding)
May cause insufficient production of progestrone and prematurely decreased
progestrone levels and insufficient secretory changes in endometrium and
menorrhagia. Histologically show irregular ripinnig of endometrium in second half of
cycle.
Persistant corpus luteum: prolonged corpus luteum activity
Abnormal prolongation of menstruation, resulting in prolonged cycle or protracted
menstrual bleeding).
May result in Persistant continued secretion of estrogen and progestrone (in the
absence of pregnancy) and absence of the normally sharp fall in estrogen and
progestrone secretion which precede menstruation which may lead to irregular
shedding of the endometrium.

6
Evaluation and diagnosis of abnormal uterine bleeding:
History:
Age, parity, marital status (single, married, widow, divorced).
Description of the pattern of abnormal menstrual bleeding and its severity and its
duration and amount of blood loss.
Presence of other cyclical symptoms as dysmenorrhoea, breast tenderness,
psychological disturbance, fatigue, dizziness, and syncope.
The patient should be questioned about the possibility of pregnancy.
Menstrual history:
Last menstrual period (LMP), Age of menarche, and regularity including flow, duration,
and presence of dysmenorrhea, Postcoital bleeding or intermenstrual bleeding.
Past obstetric history: Gravida and para & Previous abortion or recent termination of
pregnancy.
Contraceptive history: Contraceptive method used, use of barrier protection.
Past gynecological history:
o History of sexually transmitted diseases (STDs) or ectopic pregnancy.
o Cervical smear and its result history.
o Sexual history:
o Ask about dyspareunia, postcoital bleeding.
Ask about: Recent illness, psychological stress, excessive exercise, or weight change
Past medical history: Diabetes mellitus, Thyroid disease, Endocrine problems, pituitary
tumors, Liver disease.
Past surgical history.
Drug history: Medication usage, including exogenous hormones, anticoagulants,
aspirin, anticonvulsants, and antibiotics.
Clinical examination:
Look for:
Height and weight and body mass index (BMI).
Signs of anemia or hypovolemia, vital signs.
General looking for stigmata of underlying systemic disease is important. hirsutism,
striae, thyroid enlargement or nodularity, skin pigment changes.
Assessment for secondary sexual characteristic.
ecchymoses or petechiae (suggest coagulopathy).
Abdominal examination:
Liver enlargement.
Pelvic masses.
Regional lymph nodes palpation.

7
Pelvic examination:
Inspection of vulva for any external evidence of bleeding or sign of local infections.
Speculum examination: for cervix and vagina
Bimanual palpation to assess for uterine or adenexal enlargement or tenderness.
Rectal examination: if bleeding from bowel is suspected.
Laboratory investigations:
The patient's history and examination will guide the selection of various tests.
A complete blood count is essential investigation.
If there is suspicion of organic disease, it is mandatory to undertake the fullest
investigation necessary to reach a precise diagnosis.
Young women presenting with intermenstrual or postcoital bleeding should be tested
for Chlamydia.
Hormonal assay:
B-hCG if any possibility of pregnancy exists.
In patients with suspected endocrine disorders, laboratory studies such as thyroid
function tests and prolactin levels may be helpful
A mid-luteal progestrone level in regular cycle only (done in day 21 in 28 day cycle).
Level >30nmol/L is indicative of ovulation.
Serum androgen in some cases as it is elevated in poly cystic ovary syndrome (PCO),
androgen producing tumour, adrenal condition.
Prolactin.
Coagulation screen and bleeding time is important to request if bleeding disorder is
suspected.
Renal function tests and liver function tests should be requested if systemic condition
or malignancy is suspected.
Imaging Studies
Pelvic ultrasound.
It is useful to determine shape and size of uterus and adnexal structures.
It may determine the etiology of the bleeding such as a fibroid, endometrial thickening,
poly cystic ovary, adenomyosis.
Computed tomography (CT scan) / Magnetic resonance imaging (MRI)
Is used in cases needed greater level of detail of pelvic structures and abnormalities
and for cancer staging.

8
Endometrial sampling:
Endometrial biopsy is important step in evaluation abnormal uterine bleeding. It is indicated
for the following patients with abnormal uterine bleeding:
1. Women older than 35 years.
2. Those with abnormal endometrial thickness (>12mm in perimenopausal women and
>4mm in postmenopausal women).
3. Obese patients.
4. Women who have prolonged periods of unopposed estrogen stimulation
5. Women with chronic anovulation.
Endometrial biopsy can be done by:
1- Hysteroscopically directed biopsy: is the gold slandered procedure as it provides direct
visualization of uterine cavity and allows to take biopsy from specific lesion. It is ideally
done in proliferative phase of menstrual cycle when the endometrium is at its thinnest.
2- Aspiration technique.
3- Curettage.
Treatment of abnormal uterine bleeding:
In treatment of abnormal uterine bleeding, Consider:
Age group.
Amount and pattern of bleeding.
Menstrual calendar day to day report of amount of blood loss for 2-3 months is helpful.
Oral iron should be given to patient with menorrhagia routinely.
Treatment of secondary disease if present.
Medical therapy:
Non hormonal therapy:
Prostaglandin synthetase inhibitor: antiprostaglandins (non-steroidal anti-inflammatory
drugs, NSAIDS): e.g. Mefenamic acid (ponstan). Great benefit to use in ovulatory DUB and in
menorrhagia associated with dysmenorrhoea.

9
NSAIDS
It acts by inhibiting the enzyme cyclo-oxygenase and reduce local prostaglandin level. This
leads to vasoconstriction and increased platelet aggregation. These medications may reduce
blood loss by 20-50%. It is used only during menstruation as it is used with the onset of
menses or just prior to its onset and continued throughout its duration. It is generally well
tolerated.
Note: Although aspirin is included in this category of drugs, women with heavy menstrual
bleeding should not use aspirin.
Antifibrinolytic agents
As tranexamic acid, it is potent inhbitor of fibrinolysis so decrease menorrhagia and
also in menorrhagia related to IUD.
Given orally at time of menstruation.
Side effects: nausea, dizziness, diarrohea, intracranial arterial thrombosis.
It is contraindicated in patients with history of thromboembolism. Used alone or in
combination.
Hormone therapy
There is some help obtained from endometrial histology in the second half of cycle to decide
treatment. The aim of treatment is to maintain or restore the normal endocrine cycle.
First-line drugs:
Cyclical Combined oral contraceptive pills (OCPs)
Are effective in reducing menstrual bleeding, controlling cycle irregularities and relieving
menstrual pain giving for women requiring contraception or for women whom hormonal
agents are acceptable. It helps to prevent the risks associated with prolonged unopposed
estrogen stimulation of the endometrium. It effectively manage anovulatory bleeding in
premenopausal and perimenopausal women.
Progestogen therapy:
Treatment with cyclic progestins is preferred when COCP use is contraindicated, such
as in smokers over age 35 and women at risk for thromboembolism.
Cyclical progestogens are effective for menorrhagia when given for 21days out of 28
and first choice for control of anovulatory dysfunctional bleeding.

11
Withdrawal bleeding occured 3-5 days after completion of the course.
Method of administration:
Arrest bleeding.
Norethisterone acetate (primolut-N) 20-30 mg daily until bleeding stops usually in 24-
48 hours and for not more than 3days and may continue in lower dose for up to 21
days.
Once she stopped, withdrawal bleeding will occur in a few days later.
Cyclical:
Luteal phase treatment in second half of cycle (from 15th to 26th day) indicated when
corpus luteum insufficiency has been diagnosed particularly in premenstrual spotting.
Treatment continued for 6-9 months.
Norethisterone acetate (primolut-N) 5mg tid (three times a day) Or Medroxy progesterone
acetate (Provera) 10 mg tid
Whole cycle treatment: Throughout menstrual cycle (5th to 26th day)
Effective treatment for menorrhagia when given at high doses between days 5 and 26
of cycle. As luteal phase treatment is not so effective in treating menorrhagia.
Treatment can be continued for 6-9 months.
Norethisterone acetate (primolut-N ) 5mg tid for 21days out of 28 Or Medroxy
progestrone acetate (Provera) 10 mg tid
Side effects include weight gain, headache and bloatedness.
Long acting high dose progestogens (e.g. Depo-Provera) may be used to induce Amenorrhoea
but limited by side effects.
Progestogen-releasing intrauterine system:
Levonorgestrel-releasing intrauterine system (LNG-IUS) used to relief Menorrhagia as it
induce progressive endometrial atrophy.
Oestrogen therapy:
Alone used rarely in DUB treatment. Used in atrophic endometrium and in cases of DUB
secondary to depot progestogen.

11
Second-line drugs:
Used in:
When Simple measure have failed.
Management of severe anemia prior to surgery.
When Surgery is contraindicated.
Danazol
Danazol creates a hypoestrogenic and hyperandrogenic environment, (as it is
progestogen but it is converted into testosterone peripherally and acts as androgen
which induces endometrial atrophy resulting in reduced menstrual loss).
200mg is effective to decrease menorrhagia continuous for 12 weeks.
Side effects: Androgenic Side effect (breast atrophy, hirsutism, voice changes, weight
gain, oily skin, and acne), musculoskeletal pain and skin rash. Because of the significant
androgenic side effects, this drug is usually reserved as a second-line treatment for
short-term use prior to surgery.
Gestrinone
Gestrinone is a 19-testosterone derivative which has anti-progestogenic, anti-oestrogenic
and androgenic activity.it reduce menstrual blood loss in menorrhagia. However, it also has
androgenic side effects.
Gonadotropin-releasing hormone agonists (GnRH analogue) such as buserelin, goserelin.
They produce a profound hypoestrogenic state similar to menopause (They induce medical
menopause by suppressing gonadotrophions). Side effects include menopausal symptoms
and bone loss with long-term use so it should not prescribed for longer than 6 months
because the risk of osteoporosis. They are also of value as endometrial-thinning agents prior
to hystroscopic surgery. In cases of severe menorrhagia in which simple measure have failed,
long term therapy with a GnRH agonist plus hormonal add-back can be considered if there
are contraindications to surgery.
Golden rule
Note: no hormone treatment should be given unless malignant disease has first been
excluded in women with abnormal uterine bleeding around the menopause.

12
Surgical management:
It is reserved for patients in whom medical treatments have failed.
In acute situation (occasionally). As dilatation and curettage in acute situation with severe
blood loss can reduce hemorrhage.
Surgical method:
Dilatation and curettage (D&C)
Endometrial resection and ablation.
Hysterectomy
Dilatation and curettage (D&C):
A D&C may be done for a woman with heavy bleeding used in acute situation (for diagnostic
and therapeutic purpose).
Endometrial resection and ablation:
This procedure removes or destroys layers of the endometrium down to myometrium
including basal layer so no regeneration of endometrium and layers of fibrous tissue replace
it (theraputic asherman’s syndrome). It can be done as an office procedure in several
technique. It usually reduces the amount of bleeding.
This procedure is only appropriate for
1- women with refractory dysfunctional bleeding who do not want to have more or any
children
2- Patients with submucous fibroid.
Endometrial histology should be evaluated prior to surgery in order to exclude carcinoma
and endometrial hyperplasia.
Amenorrhea is seen in approximately 35% of women treated, and decreased flow is seen in
another 45%. A substantial number of patients receiving endometrial ablation require re-
operation.
Hysterectomy
It is the most effective treatment for bleeding and indicted for patients who have not respond
to medical or conservative therapy.
13
However, it is associated with more frequent and severe adverse events compared with
either conservative medical or ablation procedures. Operating time, hospitalization, recovery
times, and costs are also greater.
No need for removal of ovaries unless there is indication as abnormal ovaries.
Emergency Department Care:
Treatment in cases with severe uterine bleeding and hemodynamically unstable patients
after resuscitation, consider treatment by:
Administration of IV conjugated estrogen (Premarin) 25 mg IV every 4-6 hours until the
bleeding stops.
An oral contraceptive with 35 mcg of ethinyl estradiol can be taken twice a day until
the bleeding stops for up to 7 days, at which time the dose is decreased to once a day
until the pack is completed.
In women with severe, persistent uterine bleeding, an immediate dilation and
curettage (D&C) procedure may be necessary.
Abnormal uterine bleeding according to age:
Abnormal uterine bleeding in Adolescent and teenager girl (discussed in puberty lecture).
Abnormal uterine bleeding in Adult 20-39 years:
It most commonly due to:
Benign disease of genital tract including pelvic inflammatory disease (PID), uterine
fibroid or some complication of pregnancy.
DUB is also common.
Organic disease must therefore always be excluded before a diagnosis of DUB is made which
is most commonly ovulatory, though anovulatory bleeding seen in 20% of cases.
Most cases resolve spontaneously in ovulatory but in anovulatory is less good and
endometrial hyperplasia may be the cause which tend to recur.
Conservative therapy is usually indicated.
Hysterectomy may be indicated if bleeding is severe or recurrent and patient has completed
her family.

14
Abnormal uterine bleeding in Perimenopausal women (40 years and more):
Most commonly dysfunctional, though organic cause also common as malignancy
increase with age so it is important to exclude these condition so curettage is
mandatory.
Conservative therapy.
Hysterectomy is often indicated.
Abnormal uterine bleeding by bleeding pattern:
Regular cyclical bleeding: menorrhagia
Frequently due to:
Benign organic disease of genital tract.
DUB-ovulatory.
Rarely due to malignancy.
Considered relatively favorable.
In younger women with menorrhagia of short duration, investigation may be referred as
spontaneous remission frequently occur.
Irregular bleeding:
Frequently due to:
It is characteristic of organic disease of genital tract and in particular carcinoma of
cervix or endometrium.
Anovulatoiry DUB.
So it is regarded unfavorable particularly in perimenopausal women, and promote
investigation is mandatory.
Intermenstrual bleeding:
Frequently due to:
Dysfunctional due to fall in estrogen following ovulation.
Cervical and endometrial polyp.
Submucous uterine fibroid.
Cervical carcinoma.
It is essential to regard all cases of intermenstrual bleeding as abnormal until proved
otherwise.
