
1
Fifth stage
Gynecology
Lec-5
د.سراب
2/3/2015
Gestational trophoblastic disease
It is uncommon complication of pregnancy.
Could be changed to malignancy but it is treatable malignancy.
Occur only in married women (sexually active).
Classification:
o Premalignant: partial mole and H.mole.
o Malignant: invasive mole and choriocarcinoma.
Association:
Younger age group less than 16 years and more than 40 years.
Areas: Asians.
History of previous mole.
Nutritional factors: carotene deficiency.
Partial mole:
Triploid (3 sets of chromosome = 69).
Due to fertilization of 2 sperms to one ovum or fertilization of one divided sperm to one
ovum.
Fetal vessels and placenta present.
There is focal hydropic degeneration in placenta.
Presentation: abortion.
Diagnosed by histopathological study.
Need for chemotherapy (0.5%).
H.mole:
46 chromosome.
Only paternal chromosome (2 sperms or one divided sperm).
Usually xx.
2
No feral vessels.
Presence of villi with hydropic degeneration.
Presentation: excessive symptoms of pregnancy like pre-eclampsia, thyroid
enlargement, large uterus.
50% need chemotherapy.
Diagnosed by US snow storm appearance due to excessive cystic lesions.
Management of partial mole and H.mole:
Evacuation:
Preparation: prepare blood, investigation (CBC, Hb, blood group, cross match, B-hCG).
General ansthesia.
Suction method if evacuation.
If bleeding occur not use oxytocin but use ergometrine at the end of evacuation.
Follow up:
Twice weekly for 6 months.
Avoid pregnancy to avoid confusion.
Better not use COCP cause slower lowering of B-hCG.
Better not use IUCD or progesterone they lead to bleeding and confusion.
Best method is condom.
Contraception for 6 months if not use chemotherapy.
Contraception for 1 year if use chemotherapy.
Chemotherapy:
Indications of chemotherapy:
Biochemical:
o If B-hCG above 20000 IU after 4 weeks of evacuation.
o If increased in 2 readings.
o If plateau for 3 measures or readings.
o If decreased at beginning then increased.
Histopathology: choriocarcinoma.
Clinically:
B-hCG is tumor marker

3
o Bleeding: hematuria, vaginal bleeding, hemoptysis, peritoneal bleeding all with
elevated B-hCG.
o Focal symptoms.
Choice of chemotherapy:
High risk patient (more than 6 score) multiple therapy (EMA-CO).
Low risk (less than 6 score) single chemotherapy:
o Give intensive dose every 2 weeks.
o Methotrexate is the drug.
o Give folinic acid after methotrexate by 30 hours.
o Give every 48 hours I.M.
o Side effects of methotrexate:
GIT problems.
Bone marrow (anemia, thrombocytopenia, low WBC lead to infections).
Loss of hair.
Dermatological problem.
Pleurisy.
o Do follow up by B-hCG.
o Give contraception for one year to avoid malformation in baby.
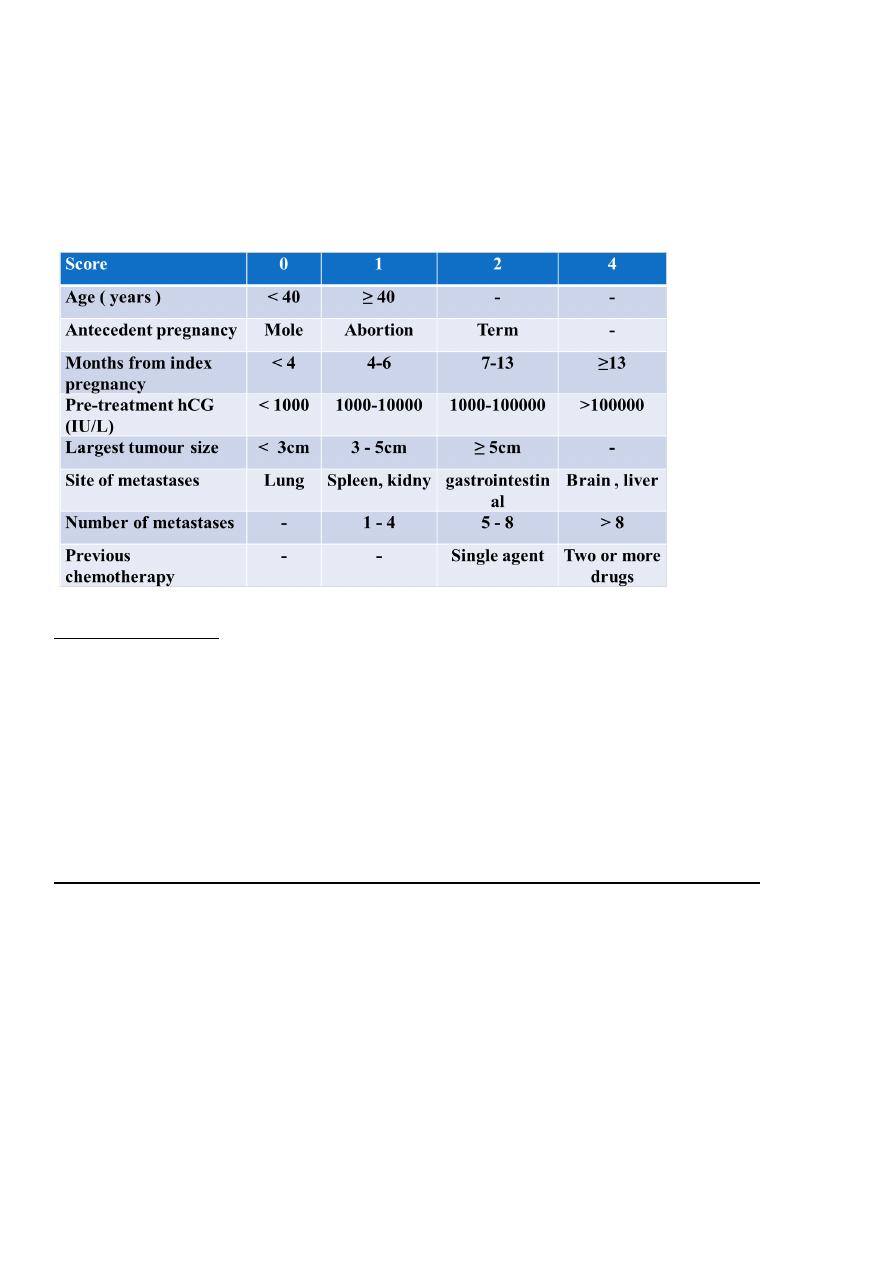
Figo scoring or staging:
Age of patient less than 40 years is low risk, more than 40 years is high risk.
Previous pregnancy before the mole H.mole (low risk), abortion (moderate risk),
normal pregnancy (high risk).
Duration between H.mole and pregnancy less than 3 months (low risk), more than 1
year (high risk).
Level of B-hCG 1000 (low risk), 1000000 (high risk).
Site of metastasis lung (low risk), brain (high risk).
Number of metastasis large number (high risk), low number (low risk).
Size of metastasis small size (low risk), large size (high risk).
Previous chemotherapy if not take (low risk), if take (high risk).
=== Figo scoring: less than 6 (give one chemotherapy), more than 6 (give multiple
chemotherapy).

4
From other lecture
Gestational Trophoblastic Disease GTD
Is defined as a spectrum of disorder resulting from an abnormal placental (
trophoblast ) growth and invasion, it is ranged from the benign condition (
hydatiform mole ) to the malignant ( gestational trophoblastic neoplasia GTN ).
These disease retain certain characteristic of the normal placenta such as
invasive tendencies and the ability to make hCG hormone.
Clinical classification
Benign = 80% (HM)
Partial HM .
Complete HM .
Malignant=20% (GTN) include
Persistant or invasive mole =12-15% of cases.
Choriocarcenoma=5-8% of cases .
Placental site trophoblastic tumor (rare).
Epidemiology
Less than 1 in 1000 pregnancies in most of the world, 2 in 1000 in Asia .
Risk of recurrence is 1 % (previous one mole).
25% (previous two moles).
Risk factors
Extremes of maternal age < 15 years or > 40 years of age.
Patients with previous history of molar pregnancy.
Possible other factors: deficiency of animal fat and carotene , history of prior
spontaneous abortion .
The incidence is in excess in maternal blood group A, and deficit in group O.
Low socioeconomic state .
Using of oral contraceptive pills
5
Hydatidiform mole (HM)
Complete mole
Partial mole
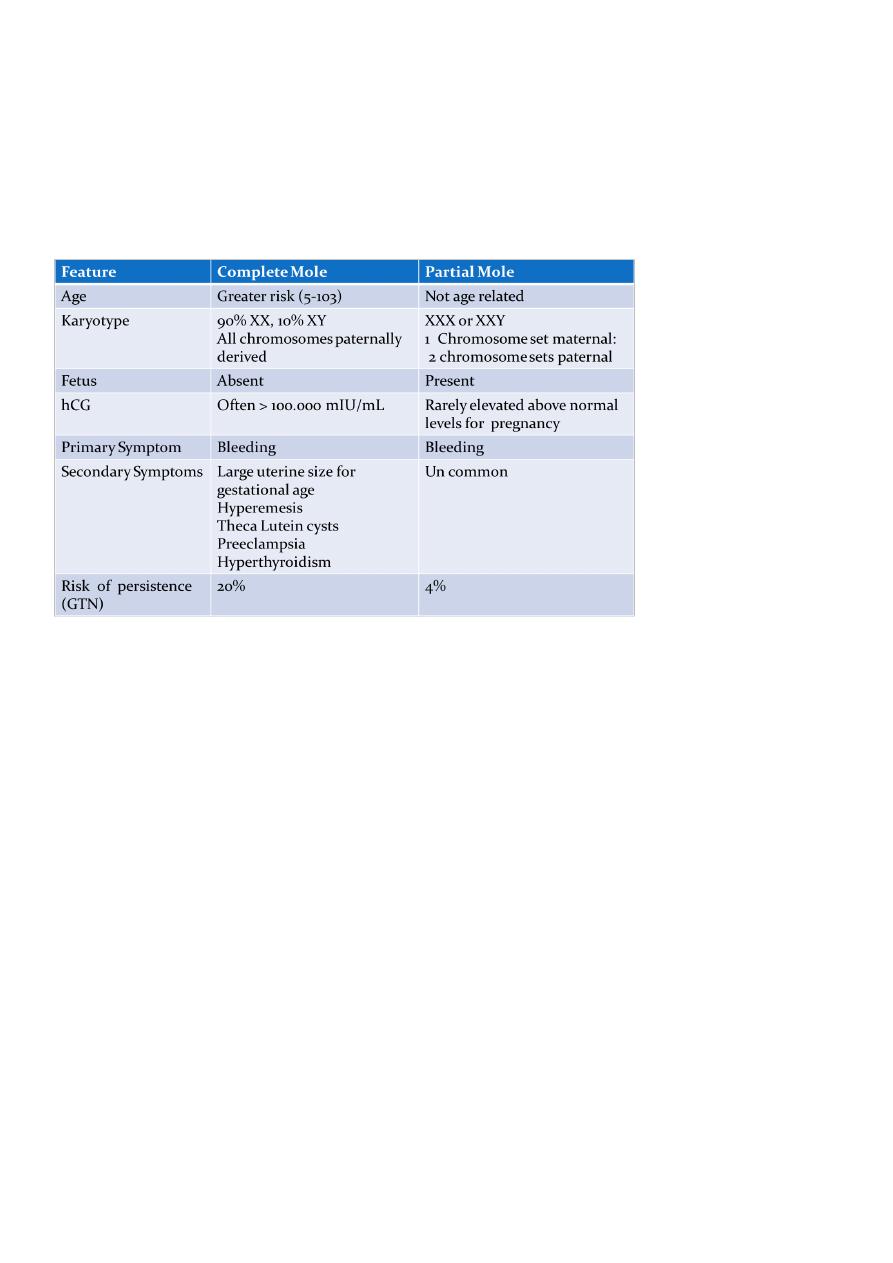
Comparison of Complete and partial moles
Management of HM
In general , the more active trophoblastic appearance the greater the risk of
malignancy.
Patients with hydatidiform mole are curative over 80% by treatment of evacuation.
(suction curettage)
About 90% of cases ,the trophoblastic tissue die out completely.
About 10% of cases the trophoblastic tissue does not die out completely and may
persist or recur as invasive mole or choriocarcinoma.
The follow-up after moler evacuation :
The follow - up after evacuation is key necessary to ensure early recognition of
persistent trophoblastic tissue and the development of GTN, this includes :
Clinically ( uterine involution , ovarian cyst regression and cessation of bleeding )
Serial quantitative measurement of serum hCG level 48 hours after evacuation of
the mole then at weekly intervals till the hCG become normal for three
consecutive reading .Then monthly for 6 months then yearly .

6
To achieve effective follow - up , the pregnancy should be avoided to avoid the
overlap of raising HCG level due to recent pregnancy , the use of mechanical or oral
contraceptive pills until the hCG levels returns to normal after the evacuation of the
mole.
Indication of chemotherapy after the evacuation of the hydatidiform mole :
Serum hCG >20000 i.u/L , at any time after evacuation of mole.
Raised hCG at 4 to 6 weeks after evacuation of mole.
Evidence of metastases ,hepatic ,brain and pulmonary.
Persistent uterine hemorrhage after evacuation of mole with raised hCG levels.
Early diagnosis of persistent trophoblastic disease ensures a good prognosis and an
effective system of follow-up.
A rising or persistently elevated serum hCG concentration is diagnostic of GTN after a
new pregnancy is ruled out.
Approximately 75 percent of these cases represent invasive mole , and 25
percent are choriocarcinomas ; placental site trophoblast tumors are rare.
High-risk postmolar trophoblastic tumor:
Pre - evacuation uterine size larger than expected for gestational duration.
Bilateral ovarian enlargement (> 9 cm theca lutein cysts)
Age greater than 40 years.
Very high hCG levels(>100,000 m IU/ml).
Medical complications of molar pregnancy such as toxemia ,
hyperthyrodism and trophoblastic embolization (villi come out of placenta ).
Repeated hydatidiform mole .
Gestational trophoblastic neoplasia (GTN)
Invasive mole
Choriocarcinoma
Placental site trophoblastic tumor
Gestational trophoblastic neoplasia (GTN)
GTN defines a heterogeneous group of lesions that represent an aberrant
fertilization event.

7
The pathogenesis is unique because the maternal tumor arises from fetal tissue.
It is the most curable gynecologic malignancy.
Malignant trophoblastic disease can exist in:
1. Invasive mole ( = non – metastatic form).
2. Choriocarcinoma = metastatic form
3. (Both are treated with chemotherapy and follow up by serum BHCG).
4. Placental site trophoblastic tumor (PSTT).
Invasive mole
The diagnosis of invasive moles or “chorioadenoma destruens” is applied to the
moles characterized by :
o Abnormal peneterativeness
o Extensive local invasion
o Excessive trophoblastic proliferation
o With preserved villous pattern.
The proliferative villi may invade the myomatrum , paramatrum ,broad ligament
, or the vaginal wall , although there is rarely evidence of metastasis.
The morbidity and mortality (10%) of this disease results from the penetration of
the tumor through the myomatrum and to the pelvic vessels with the resultant
hemorrhage
Clinical Manifestation
irregular vaginal bleeding.
uterine subinvolution.
theca lutein cyst does not disappear after emptying uterus.
abdominal pain.
metastatic focus manifestation.
Diagnosis
history and clinical manifestation.
successive measurement of HCG.
ultrasound examination.
X-ray and CT.
histologic diagnosis obtained after hysterectomy .
8
Choriocarcinoma (metastatic GTN)
Choriocarcinoma subdivide into:
o good-prognosis (low risk).
o Poor- Prognosis (High risk).
Epidemiology
The incidence of choriocarcinoma in the West: 1 :10000 and 1 : 70000 pregnancies; and
,in Asia 1:6000 pregnancies.
The antecedent pregnancy is :
o Hydatidiform mole in about 5o% of cases.
o Normal pregnancy in about 25% of cases.
o Abortion and ectopic pregnancy in about 25 % of cases.
Choriocarcinoma is more likely to occur after complete mole .
Pathological features
Site :
o In the uterus 90 % of cases; 10 % of cases in the , vagina, lung, liver, and brain.
Macroscopically:
o Uterus : It may be localized in the form of hemorrhagic polyp or multiple
hemorrhagic ,necrotic masses in the cavity.
o Some times it is present in the uterine wall ( intramural ) and the cavity is empty.
Microscopically:
o Malignant hyperplasia of both cytotrophoblasts , and syncytiotrophoblasts.
o Extensive hemorrhage.
o Absence of villi.
o Destruction of the surrounding myomatrum.
Spread
Direct : Through the myomatrum and may end in uterine perforation , internal
hemorrhage, and peritonitis .
Blood : The main method of spread ,and occurs to;
o Genital : Vagina ( 30% ).
o Extra genital : Lung ( 80% ) , ( the commonest site liver , brain (10%) and bones
especially skull and spine.(10%).
Causes of death in choriocarcinoma :
Vaginal bleeding.
9
Haemoptysis.
Intraperitoneal hemorrhage.
Peritonitis.
Metastasis to the vaital organs e.g ,brain.
Pulmonary complications.
Clinical feathers
Symptoms :
o Recent history of expulsion of vesicular mole , or abortion , or full term pregnancy.
o Persistent vaginal bleeding is the commonest presentation.
o Haemoptysis.
o Abdominal pain.
o Palpable abdominal mass ( enlarge uterus or parauterine metastasis ).
o neurological symptoms.
Signs:
o Marked deterioration of the general condition.
o An abdominal swelling may be felt.
o The uterus symmetrically enlarged.
o Hemorrhagic secondaries may be seen in the vagina.
Investigations:
Serum hCG.
CBC
L.F.T .
U/S for abdomen and pelvis.
Chest X-ray for pulmonary metastasis.
Liver scan
CT scan for the secondaries.
EEG .
Clinical classification of GTN
According to the FIGO system , patients who score 6 and below receive low-risk
treatment while patients scoring 7 are given high-risk treatment (chemotherapy )
According to the presence of metastasis
o Non metastatic trophblastic disease(Disease is limited to the uterus)
o Metastatic either :
Good Prognosis Metastatic Trophoblastic neoplasia
11
Poor Prognosis Metastatic Trophoblastic neoplasia
o Drug-resistant disease
The international federation of gynaecology and obstetrics(FIGO) prognostic scoring system
employed for assessing the intensity of the initial chemotherapy treatment.
Treatment of GTN :
Chemotherapy (single agent ,multi agent).
Surgery.
Radiotherapy .
Medical (chemotherapy)
I. Non metastatic and good prognosis GTN we use the Single agent chemotherapy .
Methotrexate ( antimetabolite ) + folinic acid . Is the treatment of choice given
on alternate days followed by six rest days . The cytotoxic therapy is controlled by
doing CB , platelet count and LFT.
After the hCG level gets normal ; stop the therapy and follow - up by weekly
estimation of hCG levels . Physical examination, chest x-ray, and LFT.
Actinomycin D ,if there is resistance .
Treatment is 100 % successful.
11
II. Poor Prognosis metastatic trophoblastic neoplasia and drug resistant tumor we use
Multiple agent chemotherapy is recommended in this disease.
EMA - CO is considered the regimen of choice in most high–risk patients (Etoposide
, Methotrexate, Actinomycin D , Cyclophosphamide, Vincristin ).
The overall survival rate for these patients is 80 – 85 %.
Patients with cerebral or hepatic metastases are treated concurrently with
radiotherapy for the whole brain or liver (for hemostasis).
Surgery:
Total abdominal hysterectomy may be done in patients not desirous of further
reproduction , and in old age woman.
Surgical excision of isolated metastases e.g. pulmonary if resistant to chemotherapy.
operation is also important in controlling bleeding , infection, complication.
in removing remained or drug-resistant foci.
Irradiation
Whole brain irradiation for cerebral metastases , and the whole organ irradiation
for hepatic metastases
Follow-up
After successful therapy , physical examination , and chest x-ray follow - up
together with the hCG levels are obtained for serial interval measurement .
If at any time hCG levels rises , repeat the evaluation , staging ,and chemotherapy.
Women who undergo chemotherapy are advised not to conceive for one year after
completion of treatment.
Placental Site Trophoblastic Tumor .
Rare tumors (account for 0.23% cases of GTD).
It has a variety of clinical features and its course is unpredictable.
Can appear shortly after termination of pregnancy or years later.
Hysterectomy is considered optimal therapy and is usually adequate in most situations.

12
It has normal HCG level but high human placental lactogen level so used as a
tumor marker.
It is chemoresistant and radioresistant.
Future Childbearing
After treatment of GTN, molar pregnancies occur in only about 1-2 % of subsequent
pregnancies.
These patients should be evaluated with a first trimester ultrasonography.
Fertility rates and pregnancy outcomes are similar in patients treated for GTD
compared with the general population .
Standard chemotherapy protocols have minimal impact on the subsequent ability to
reproduce.
Patients treated with EMA/CO regimens have an increased rate of second malignancies,
particularly hematologic.
