
1
Fifth stage
Pediatric
Lec-6
د.ندى العلي
26/10/2015
NEUROLOGY
Assessment
The process and interpretation of the neurologic examination vary with age. The
examination of a newborn is unique with transient and primitive reflex patterns. The
examination of an adolescent is similar to that of an adult.
NEUROLOGIC EXAMINATION OF A NEONATE
The neurologic examination of a neonate is used to assess the function of the basal ganglia,
brainstem, and more caudal structures. The results of the examination should be used
cautiously in predicting developmental outcome.
Neonatal reflexes
Numerous primitive reflexes, present at birth, assess the functional integrity of the
brainstem and basal ganglia . They are symmetric and disappear at 4 to 6 months of age,
indicating the normal maturation of descending inhibitory cerebral influences (Moro
reflex). The grasp and rooting reflexes are inhibited by maturation of frontal lobe structures
and may reappear later in life with frontal lobe lesions. The Landau and parachute reflexes
become apparent after the newborn period, indicating proper maturation of appropriate
brain structures. Asymmetry or persistence of the primitive reflexes may indicate focal
brain or peripheral nerve lesions.
Posture
Posture is the position that an infant naturally assumes when placed supine. An infant at 28
weeks of gestation shows an extended posture. By 32 weeks, there is a slight trend toward
increase in tone of the lower extremities with more lower extremity flexion. At 34 weeks,
the lower extremities are flexed, and the upper extremities are extended. At term, the
infant flexes lower and upper extremities. Recoil is defined as a liveliness with which an arm
or leg springs back to its original position after passive stretching and release. Recoil is
essentially absent in a small premature infant but is brisk at term.

2
NEUROLOGIC EXAMINATION OF A CHILD
The purpose of the neurologic examination is to "localize" or identify the region within the
neuraxis from which the symptoms are arising. The mental status examination assesses
various zones of the cerebral cortex. The cranial nerve examination evaluates the integrity
of the brainstem. The motor examination evaluates upper and lower motor neuron
function. The sensory examination assesses the peripheral sensory receptors and their
central reflections. The deep tendon reflexes assess the upper and lower motor
connections. The gait assessment puts the motor system into a dynamic state for better
functional assessment.
Mental Status Evaluation
Alertness is assessed in infants by observing spontaneous activities, feeding behavior, and
visual ability to fix and follow the movement of objects. Response to tactile, visual, and
auditory stimuli is noted. In circumstances of altered consciousness, the response to painful
stimuli is noted. Toddlers are expected to play at a level appropriate for their age. Older
children can be tested for orientation to time, place, person, and purpose.
The best way to assess intellectual abilities is through language skills. Language function is
receptive (understanding speech or gesture) and expressive (speech and the use of
gestures). Abnormalities of language resulting from disorders of the cerebral hemispheres
are referred to as dysphasia or aphasias. Anterior, expressive, or Broca aphasia is
characterized by sparse, nonfluent language. Posterior, receptive, or Wernicke aphasia is
characterized by an inability to understand language. Speech is fluent but nonsensical.
Global aphasia refers to impaired expressive and receptive language.
CRANIAL NERVE EVALUATION
MOTOR EXAMINATION (Power, Tone)
Gait:
The toddler gait is normally wide-based and unsteady. The base narrows with age. By 6
years old, a child is able to tandem walk and walk high on the toes and heels. Cerebellar
dysfunction results in a broad-based, unsteady gait accompanied by difficulty in executing
turns. Corticospinal tract dysfunction produces a stiff, scissoring gait and toe walking. Arm
swing is decreased, and the arm is flexed across the body. Extrapyramidal dysfunction
produces a slow, shuffling gait with dystonic postures. There also may be choreoathetotic
movements. Lower motor neuron disease results in either a waddling gait (if the proximal
muscles are weak) or a steppage gait (if the distal muscles are weak).

3
Reflexes
Deep tendon reflexes at the triceps, biceps, brachio-radialis, knee, and ankle are elicited by
sudden tendon stretch and can be obtained at any age. These reflexes are decreased in
lower motor neuron disease and increased with the development of clonus in chronic
upper motor neuron disease. The Babinski response or extensor plantar reflex with an
upward movement of the great toe and flaring of the toes on noxious stimulation of the
side of the foot is a sign of corticospinal tract dysfunction. This reflex is unreliable in the
neonates except when asymmetric because the "normal" response at this age varies. The
plantar response is consistently flexor (toes down) after 18 months of age.
Primary symptoms of neurological disease
Visual or hearing loss.
Impairment of swallowing or respiration.
Weakness.
Numbness or parasthesia.
Difficulty walking or talking.
Incontinence.
Deterioration in thinking.
Change in personality.
Seizures.
Headache and dizziness.
Congenital anomalies of the nervous system
Spina bifida:
It range in severity from simple defect at L5 or S1 vertebral arch, to major defect that
uncovered by skin or bone on baby's back(myelocele).or the defect involve the skull
(encephalocele).
Symptoms:
Total paralysis , loss of sensation in the legs , incontinence of bowel and bladder.
Meningocele :
The spinal canal and the cystic meninges are exposed but the spinal cord is functionally and
anatomically normal.
Prevention: folic acid

4
Macrocephaly: (large head )
1-Macrocrania-
2-Hydrocephalus-
3-Megalencephaly-
Microcephaly: (small head)
1-Crainocynostenosis:
2-Small brain:( infection, metabolic, toxic , vascular disorder)
Etiology of microcephaly
1-Chromosomal disorder: Trisomy 13 , trisomy 18
2-Genetic disorder: Microcephaly Vera ,sex linked microcephaly ,microcephaly with other
brain malformation.
3-Microcephaly with syndrome: Prader-willi syndrome ,angelman syndrome
4-Infection: TORCHS
5-Toxic: Radiation ,fetal alcohol syndrome,phenylketonuria ,hypoxic-ischemic injury.
CNS reflexes of infancy
Moro :start at birth disappear at 4 months
Grasp :
Rooting :
Placing :
Tonic neck:
Trunk incurvation:
Parachute: start at 6-8 months and never disappear.
Increased intracranial pressure (ICP)
A symptom of serious intracranial pathology and a cause of irreversible neurological injury.
The skull is rigid container ,brain accounts for 80-85% of volume,CSF 10-15%,blood 5-10%,

5
Brain herniation:
It occur when the brain shift in response to the continuing elevation of ICP
Etiology: mass lesion , hydrocephalus , brain swelling
Symptoms: headache ,vomiting , lethargy ,irritability ,6
th
nerve palsy , diplopia , papillodema
accept infant?
Sign: bulging fontanel , suture diastasis , distended scalp veins , sun set eyes , rapid growth
of OFC.
Cushing triad :↑ICP ,↓pulse , irregular respiration.
Brain abscess
It causes ↑ICP by:
1-large size 2-blockage of CSF 3- blockage of venous outflow
4-cerebral edema(vasogenic edema)
Etiology: chronic cardiac or pulmonary disease by embolization
Symptoms:
-focal neurological sign.
-↑ICP
-fever , malaise , anorexia , stiff neck.
Diagnosis : CT scan , (LP is contraindicated)
Treatment : surgery.
Hydrocephalus
Produces slowly evolving syndrome of ↑ICP extending over wks or ms.
Pressure is exerted by both enlarging ventricle & interstitial edema.
CSF:
Ultra filtration of plasma produced by choroids' plexus. Volume 50 ml in neonate ,150 ml in
adult
Flow from lateral v →3
rd
V through foramen of Monro then through cerebral aqueduct →4
th
V then through foramen of Magendie and Luschka to the subarachnoid space.
Absorption: by arachnoid villi.
6
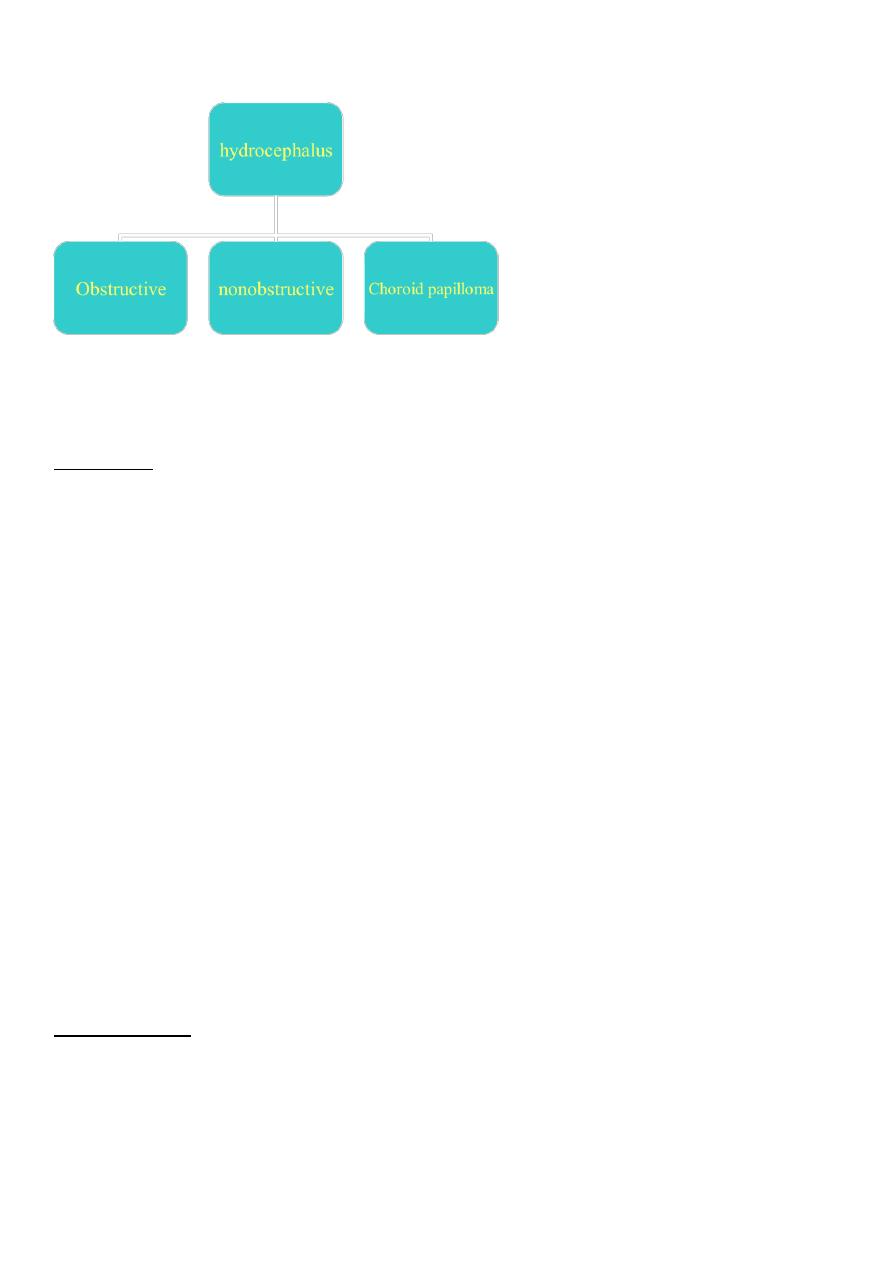
Types of hydrocephalus
Etiology
Obstructive
1-congenital
a- Arnold-Chiari malformation is characterized by progressive hydrocephalus with a
myelomeningocele. This lesion represents an anomaly of the hindbrain, probably due
to a failure of pontine flexure during embryogenesis, and results in elongation of the
4th ventricle and kinking of the brainstem, with displacement of the inferior vermis,
pons, and medulla into the cervical canalb
b- Dandy-Walker consists of a cystic expansion of the 4th ventricle in the posterior fossa
and midline cerebellar hypoplasia, which results from a developmental failure of the
roof of the 4th ventricle during embryogenesis
c- aqueduct stenosis) results from an abnormally narrow aqueduct of Sylvius that is
often associated with branching or forking
2-congenital infection. toxoplasmosis
2-post meningoencephalitis.
4-tumor( I V tumer ).
5-other(neurofibromatosis , AV malformation , achondroplasia ,rickets).
Non obstructive
1- congenital(arachnoid villi).
2-infection.
3-hemorrhage.

7
Clinical feature
1-symptoms&sign of ↑ICP.
2-ataxia&spasticity (lower limb)
3-endocrine dysfunction.
4-visual dysfunction.
5-˝sun set eyes˝.
6-dilated scalp veins.
7-widly opening fontanel.
8-rappid ↑in OFC by serial measures.
Diagnosis
1-clinically
2-imiging study(ultrasound).
3-radiological study(CT scan).
Treatment
Medical : (Meningitis, subarachnoid Hr) acetazolamide
Surgery : -(cyst ,tumer ,AVM) Removal. -shunt placing.
Floppy baby
Neonatal immobility:
The 1
st
step in evaluations of an infant who doesn't move spontaneously or in response to
stimuli is to determine whether awareness is intact ?
The cortical activity is intact if the baby is bright eyed able to follow and try to smile but is
unable to move .
If the face and eyes are immobile the problem is more difficult .
Clinical questions:
Does the infant response to :flashlight , bell , nasal cotton stimuli?
8
Does the eyes follow if the lids are lifted?
Are reflexes increase? UML
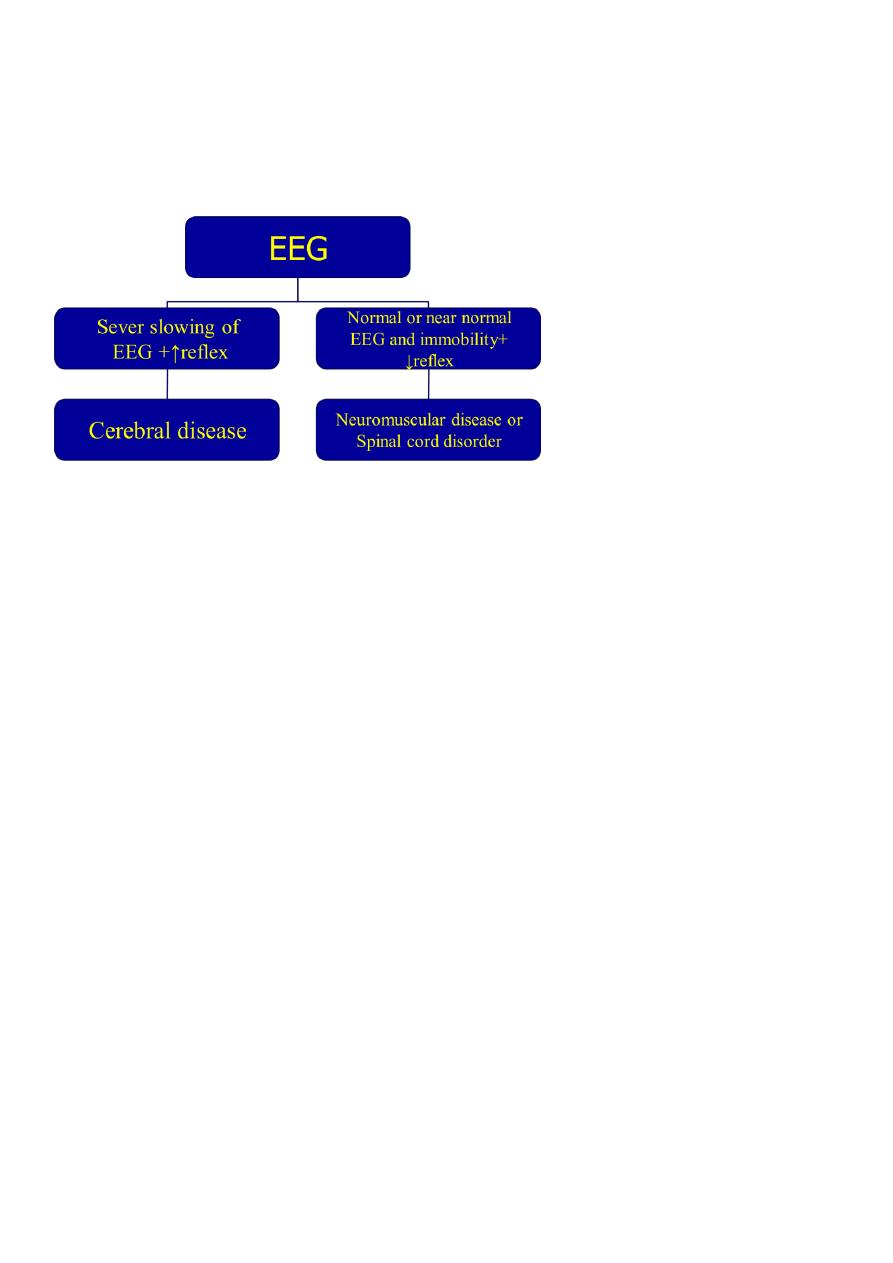
If the clinical exam. Doesn't settle the question then EEG will be helpful
Etiology of neonatal immobility
Sever hypoxic ischemic encephalopathy:
Flaccidity
Areflexia
Complete ptosis
Ophthalmoplegia
Absent corneal&gag reflex
Intoxication :
Mg sulfate
Barbiturate
Narcotics
Benzodiazepines
General anesthesia
Metabolic encephalopathy:
Hypoglycemia
Hyperbilirubinemia
Hypotonia without major weakness
acute systemic illness.
Mental retardation:

9
1. Specific syndromes
2. Down syndrome
3. Cerebrohepatorenal syndrome
4. Kinky hair syndrome
5. Prader-willi syndrome
6. Connective tissue disorder: Ehlers-Danlos syndrome, Marfan syndrome
Nutritional-metabolic disease:
1. Rickets
2. Renal tubular acidosis
3. Celiac disease
4. Biliary Artesia
5. Congenital heart disease
Benign congenital hypotonia:
• Exhibit the condition at 9-12 months.
• Delayed motor milestone.
• Normal social , intelligence , fine motor movement.
• Head lag , slip-through ventral suspension.
• Complete lab. Investigation are necessary.
• Most of children become normal by 3 yrs.
