
1
Fifth stage
Pediatric
Lec-3
.د
رواء
1/1/2014
Infant feeding-3
THE objectives
1.To know the proper method of sterilization of bottles
2. To know the proper method of preparation of formula
3.To know about the introduction of solid food
Preparing infant formula
Safe bottle-feeding depends on a safe water supply, sufficient family income,
effective refrigeration, clean surroundings and satisfactory arrangements for
sterilizing and storing equipment. tap water is preferred for preparing infant formula
All tap water used to prepare infant formulas should be boiled and cooled
1. Always wash hands before preparing formula and ensure that formula is prepared in a
clean area
2. Use sterilized bottles, teats,
3. Boil fresh water and allow it to cool until lukewarm – to cool to a safe temperature.
4. allow the water to sit for at least 30 minutes
5. Ideally prepare only one bottle of formula at a time, just before feeding
6. Add water to the bottle first, then powder
7. Always measure the amount of powder using the scoop provided in the can, as scoop
sizes vary between different formula(1scoop+1oz)
8. Keep the scoop in the can when not in use – do not wash the scoop as this can
introduce moisture into the tin if not dried adequately
9. Place the teat and cap on the bottle and shake it until the powder dissolves
10. Test the temperature of the milk with a few drops on the inside of your wrist
11. A feed should take no longer than 1 hour – any formula that has been at room
temperature for longer than 1 hour should be discarded
Sterilization methods
Sterilization by boiling
-1.-Wash bottles, teats and caps in hot soapy water with a bottle/ teat brush before
sterilization
2-Place utensils, including bottles, teats and caps in a large saucepan on the back
burner of the stove
3-Cover utensils with water, making sure to eliminate all air bubbles from the bottle
4-Bring water to the boil and boil for 5 minutes. Turn off – do not allow it to boil dry
5-Allow the equipment to cool in the saucepan until it is hand hot and then remove it
be very careful if children are present .
6-Store equipment that is not being used straight away in a clean container in the
fridge

2
Boil all equipment within 24 hours of use
7-No.of bottles should be =No. of feeds +1
Sterilizing using chemicals:
submersion in 50 ppm hypochlorite solution for 30 minutes, completely
eliminates bacterial contamination.
chemical sterilization is not as effective as boiling unless bottles and other utensils
are meticulously cleaned.
Steam sterilizers:
Risks associated with incorrect preparation of infant formula
Powdered infant formula is not a sterile product and there are occasional infections
of infants with Cronobacter sakazakii (enterobacter sacazakii) .
Infants are not at risk fromC. Sakazakii when formula is prepared with lukewarm
(body temperature), previously boiled water and fed within 1 hour.
Good bottle-feeding practice
good practice in bottle-feeding involves making feeding a comfortable experience for
parent and infant while
avoiding risks associated with incorrect bottle-feeding. this includes:
-always checking the temperature of the formula before feeding &the amount of milk
flow from the teat(it should be drop by drop).
-holding, cuddling and talking to (if it is not too distracting) the infant while feeding
and responding to infant cues .
-not leaving an infant to feed on their own (i.e. with the bottle propped) – the milk
may flow too quickly and cause the infant to splutter or chock.
-putting an infant to sleep while drinking from a bottle – as well as the risk of
choking this increases the risk
of ear infection and dental caries.
How much milk?
Bottle fed infants up to 6 months require about 150 ml/kg body weight each day to
meet their nutrient needs. some will
require more (up to 200 ml/kg), others less. It is important for parents to be aware
that there are many individual
variations in the amount of formula and the number of bottles consumed each 24
hours.
Plenty of wet nappies (six or more per day), consistent (but not excessive) weight
gain, and a thriving,
active infant indicate that all is well.

3
Fluoride in infant feeding
Fluoride is an essential nutrient, being part of the structure of bones and teeth. the
water supply in most developed countries is fortified with approximately 1 mg per
liter of fluoride
And it is assumed that this water will be used in preparing infant formula. However,
fluoridation policies and naturally
occurring fluoride levels vary by region. In areas where the water supply is not
fluoridated, an inadequate intake
of fluoride by infants and the general community poses a public health problem
however excessive exposure to fluoride results in dental fluorosis.
When should solid foods be introduced
Infancy is the period of most rapid growth in weight, height and all of the
developmental parameters. In round
figures, growth in the first 4 months of life is 150–200g per week and then 100–150 g
per week until 6 months.
In the first 6 months the average infant doubles his or her birth weight and by 1 year
typically weighs 2½ times the weight at birth.
continued growth and development through good nutrition is important to protect
the infant against morbidity &mortality
Appropriate growth during infancy protects against stunting at one extreme and
obesity at the other.
Appropriate early growth and development also protects against the development of
chronic illness in adulthood and influences future bone mass.
Introducing solid foods
the word ‘weaning’ is often used to describe the introduction of solid foods. this can
be confusing as this term
is also used to describe the introduction of non-milk drinks or even infant formula
that may be introduced .
As complete reliance upon breast milk ceases. due to this confusion, so the term
(‘introduction of solid foods )is used instead.
By around 6 months of age most infants are able to adapt to different foods, food
textures and modes of feeding .
this age has been identified as a time when :
appetite and nutritional requirements are no longer satisfied by breast milk or infant
formula alone
stores of several nutrients – for example, iron and zinc – are often falling in
exclusively milk-fed infants (both breast & formula )
feeding behaviour has progressed from sucking to biting (most infants are chewing by
7–9 months and can
manage finger foods at 8 months)
the tongue-extrusion reflex has disappeared and the infant’s increasing ability to sit
without support allows

4
greater manipulation of food before swallowing, so that thicker foods can be
managed
the digestive system has matured and the infant is able to digest starches
most infants have developed an interest in their environment, which prompts a
willingness to accept new
textures and flavours
Using a feeding cup
A feeding cup can be used instead of a bottle for feeding infant formula or expressed
breast milk.
The WHO states ‘If you live in an area where sanitation and clean water are a
problem, cup-feeding is a safer option than bottle feeding .
This is because the teats and screw tops of bottles are more difficult to clean and can
trap harmful bacteria.
Feeding cups containing formula or breast milk should continue to be sterilized up to
12 months
Problems associated with earlier introduction of solid food
Introducing solid foods too soon can lead to several problems:
1.if less time is spent on the breast, maternal milk production may decline because of
reduced stimulation and under- nutrition may result in extreme cases
2.If solid foods are introduced while the tongue-extrusion reflex is still strong, the
infant will reject the spoon (ahard object ) the mother
might then feel that the infant is rejecting the food, when in fact he or she is rejecting
the
object in the mouth
3.exposure to pathogens present in foods can cause increased rates of diarrheal
diseases.
Problems associated with later introduction of solid foods
1.growth can falter because breast milk or infant formula alone is insufficient after
6 months
2.immune protection can be compromised
3.micronutrient deficiencies, especially of iron and zinc, can develop – iron stores are
likely to become depleted
4.if a bioavailable source of iron from complementary foods is not provided
optimal development of motor skills such as chewing can be delayed and the infant
may be unwilling to accept new tastes & textures
5.There is an association with increased risk of developing allergic syndromes

5
First foods
the introduction of solid foods at around 6 months should start with iron-containing
foods, including iron-enriched
infant cereals, pureed meat, poultry and fish (all sources of haem iron), or cooked
tofu and legumes.
Food offered should be an appropriate texture and consistency for the infant’s
developmental stage:
from 6 months of age, infants should be offered purees and then mashed foods,
progressing to minced and
chopped foods
by 8 months most infants can manage ‘finger foods’
by 12 months, infants can have nutritious choices from the foods eaten by the rest of
the family and should be
consuming a wide variety of foods.
Vegetables,
fruits, and dairy products such as full-fat yoghurt, cheese and custard can then be
added.
Healthy food after 6 months
by 8 months most infants can manage ‘finger foods’
by 12 months, infants can have nutritious choices from the foods eaten by the rest of
the family and should be
consuming a wide variety of foods.
Vegetables,
fruits, and dairy products such as full-fat yoghurt, cheese and custard can then be
added.
small, hard pieces of food should be avoided as they can cause choking ,salt should
not be
added to food, as infant kidneys are immature and unable to excrete excess salt.
Frequent consumption of added
sugars is associated with increased risk of dental cariesInfants given salty or very
sweet foods may also acquire a taste for them, resulting in poor food choices later in
life
IMPORTANT PRINCIPLES FOR solid food introduction
Begin at 4-6 mo of age
At the proper age, encourage a cup rather than a bottle
Introduce 1 food at a time
Energy density should exceed that of breast milk
Iron-containing foods (meat, iron-supplemented cereals) are required
Zinc intake should be encouraged with foods such as meat, dairy products, wheat,
and rice
Phytate intake should be low to enhance mineral absorption
Breast milk should continue to 12 mo, formula or cow's milk is then substituted
6
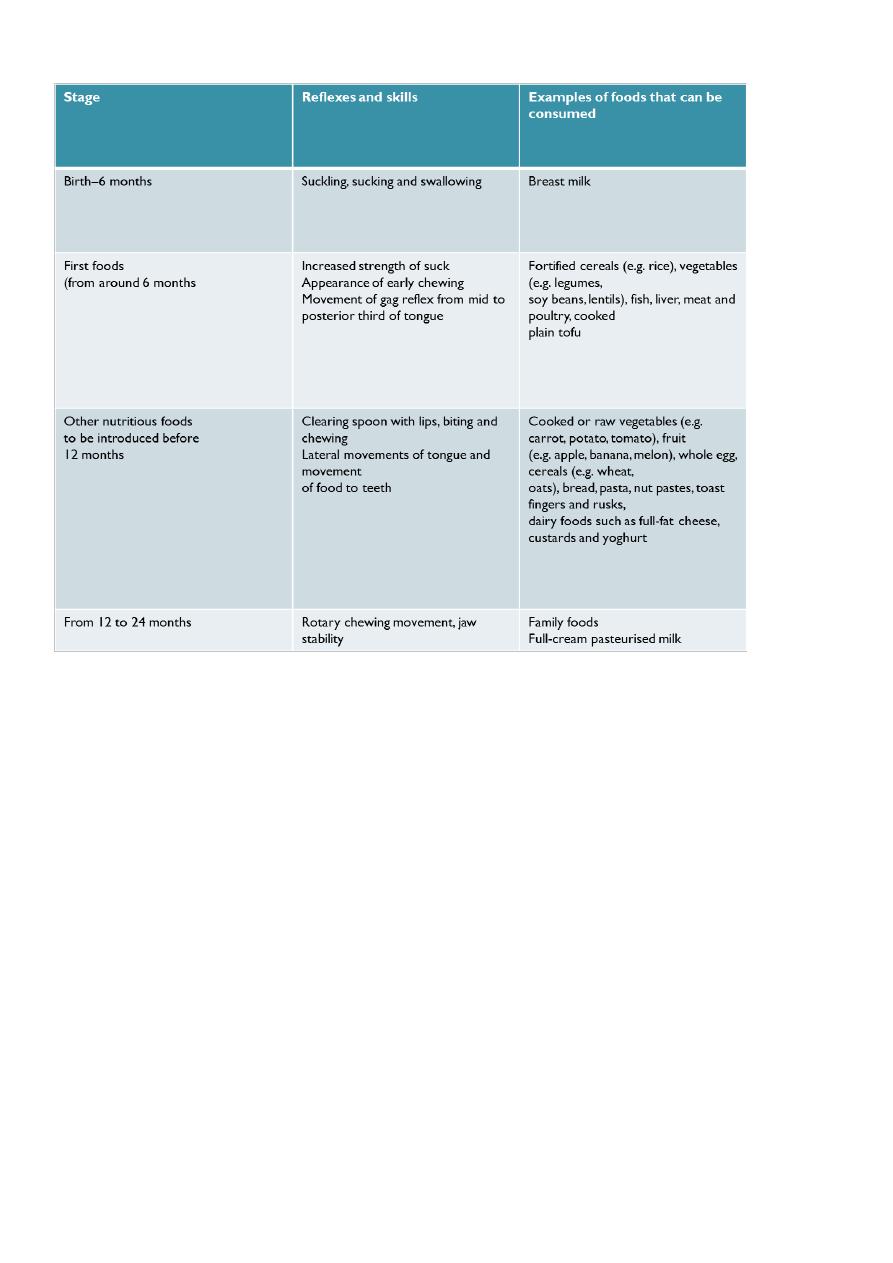
Developmental stages and examples of foods
Food safety
Attention to food hygiene is very important when preparing foods for infants and
children
1.To prevent salmonella poisoning, cook all eggs thoroughly (i.e. until the white is
completely set and yolk begins to thicken) and
2.do not use uncooked products containing raw eggs, such as home-made ice cream
or mayonnaise
3.Reduce the transfer of cariogenic bacteria from carer to infant by avoiding
inappropriate feeding practices such as sharing
spoons and other utensils, or tasting infant’s food with shared utensils.
4.consumption of nutrient-poor foods with high levels of fat/ saturated fat, sugar,
and/or salt
(e.g. cakes, biscuits, confectionery and potato chips) should be avoided or limited.
Infants with a family history of allergy
There is little evidence that delaying introducing solid foods beyond 6 months
reduces the risk of allergy.
some suggestion reveals that delaying introducing foods may increase (rather than
decrease) allergy.

7
So egg, peanuts, nuts, wheat, cow’s milk and fish should be avoided to prevent food
allergy or eczema in infants
(with siblings who already have allergies to these foods)
Treatment of proven food allergies involves avoiding foods known to cause
symptoms.
Foods and beverages not suitable for infants or that should be used with care
Nuts and other hard food
Foods with a high risk of choking such as whole nuts, seeds, raw carrot, and chunks of
apple should
be avoided for the first 3 years as their size and/or consistency increases the risk of
inhalation and choking.
However nut pastes and nut spreads can be offered to infants from around 6 months
of age.
Honey
Honey can contain the spores of Clostridium botulinum, and should not be given to
infants aged under 12 months
Non-milk beverages
Non-milk beverages
exclusively breastfed infants do not
require additional fluids up to 6 months of age. For formula-fed infants, cooled boiled
tap water may be used if
additional fluids are needed.
Fruit juice and fruit drink
fruit juice offers no nutritional benefit for infants younger than 6 months and no
nutritional benefits over breast milk or formula
100% fruit juice or reconstituted juice can be a healthy part of the diet when
consumed as part of a well-balanced
diet – fruit drinks often contain only a small quantity of fruit juice and are not
nutritionally equivalent to fruit juice or fruit
..
Fruit juice and fruit drink
-juice is not appropriate in treating dehydration or managing diarrhea
-excessive juice consumption may be associated with malnutrition (over nutrition and
under nutrition) and with
It can cause variety of gastrointestinal symptoms including diarrhea, flatulence,
abdominal distention, and dental caries.
-infants should not be given juice at bedtime
-fruit juice should be limited to 120–180 ml/per day for children aged over 12
months.
-children should be encouraged to eat whole fruits to meet their recommended daily
fruit intake
-fruit juice be limited to 120–180 ml/per day for children aged over 12 months.

8
Caffeinated and sugar-sweetened drinks
tea is the most widely used beverage in the world; it is of great cultural importance in
many societies and is
commonly given to infants, sometimes even as a prelacteal feed.
tea contains tannins and other compounds
that bind iron and other minerals, thereby reducing their bioavailability.
As well, sugar is often added to tea,
increasing the risk of dental caries. For these reasons, tea is not recommended as a
drink for infants – it is of no known benefit to infants and could possibly be harmful
