1
Fifth stage
Pediatric
Lec-5
.د
رواء
1/1/2014
Hypothermia, Hypoglycemia, Hypocalcemia, Seizures
Objectives
• To recognize the ways of heat loss in newborn baby, and etiology, clinical features
and management of hypothermia in newborn baby
• To list the risk factors, clinical features, differential diagnosis, and management of
hypoglycemia in neonate
• To understand the pathophysiology ,clinical manifestations, complications, and
management of infant of diabetic mothers
• To recognize the definition, etiology, clinical manifestations of hypocalcemia in
neonate
• To understand the etiology, types, and management of neonatal seizures
HYPOTHERMIA
Heat balance: heat production= heat loss
Heat is produced as product of cell metabolism by non-shivering thermo genesis from
chemical reactions of [ATP] hydrolysis in specialized areas of tissue containing brown
adipose tissue.
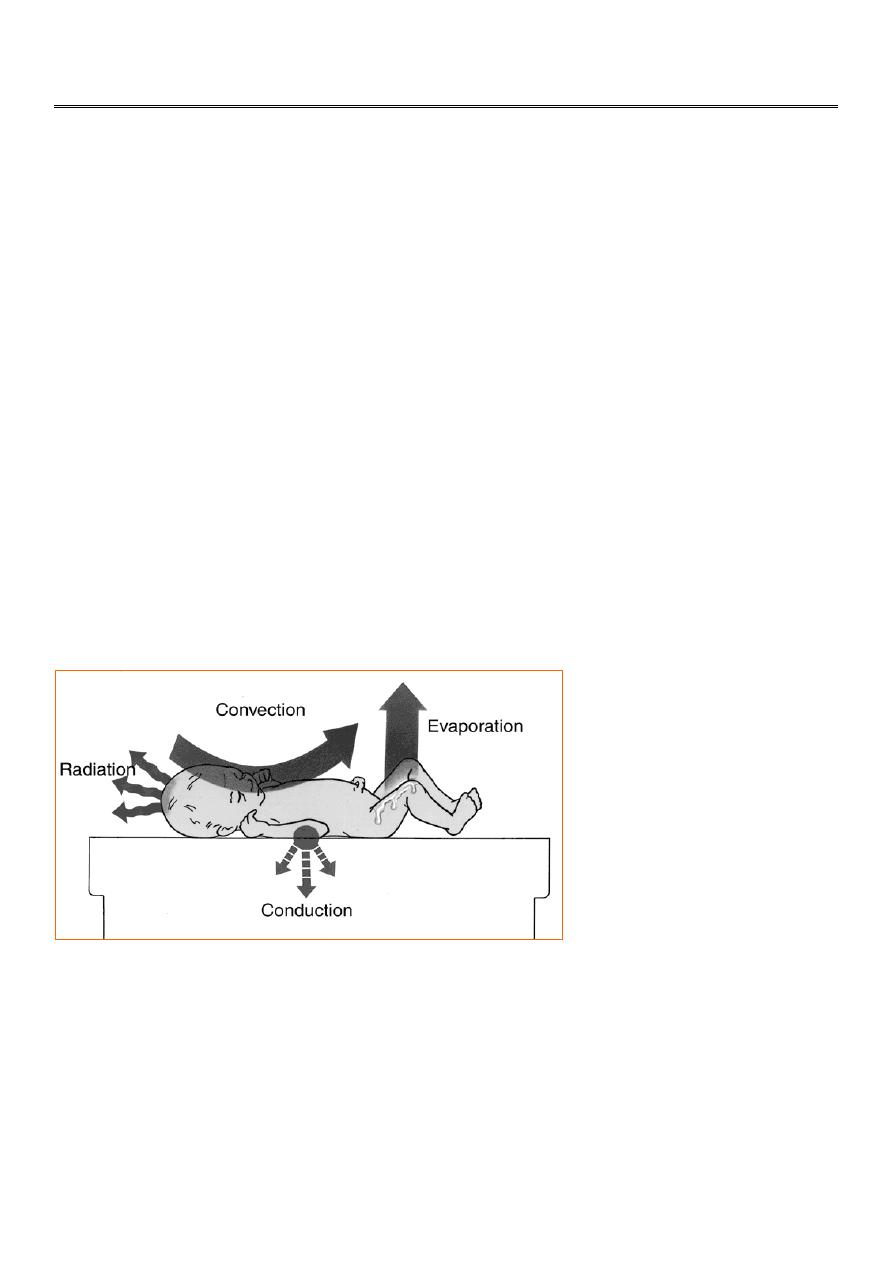
Four ways a newborn may lose heat to the environment
Heat loss in newborn infant is by:
1-Convection: heat is lost from skin surface to the surrounding air by convection[ loss is
high if the air is cold]
2-Radiation: heat is lost from skin surface to the nearest surface which faces the skin by
means of radiation.
3-Evaporation: heat is lost as water evaporates from the surface of the skin[ loss is high in
preterm infant who have high transepidermal water loss due to passive diffusion of water
vapor through the thin poorly keratinzed immature epidermis.
4-Conduction: heat loss from skin surface to the cold structure in direct contact with it.

2
Low body temperature is below 36° c
1- Mild [ rectal temp. 34-36°c]
2- Moderate [ rectal temp.30-34°c]
3- Severe [ rectal temp.below 30°c]
Etiology:
1-Accidental hypothermia: due to cold exposure in hospital or at home specially in low birth
weight baby due to inadequate clothing or cold thermal environment.
2- Other causes:
- sepsis
- severe heart failure or with marked cyanosis
- malnutrition
- hypothyroidism
Clinical features:
Symptoms develop when temp. falls below 34°c.
Early features: baby lethargic,feed poorly,week cry,&reduced movement.
Late features: peripheral edema, sclerema, marked facial erythema with striking cold skin.
In severe hypothermia: profound bradycardia, slow shallow
respiration,apnea,hypoglycemia, acidosis,& infant appear to be dead.
Diagnosis: is by recording temp. by low reading rectal temp. to 30° c.
Treatment:
Is by reworming and if there is underlying cause should be treated.
In mild hypothermia rewarming takes place rapidly.
In moderate or severe cases rewarming takes place slowly.
Rewarming is by using radiant warmer or incubator or heated cot. Use plasma expander
during rewarming has been advocated.
Hypoglycemia may occur during rewarming. It should be treated or prevented by slow I.V
infusion of 10% dextrose water.
Complications:
Abdominal distension & ileus
NEC &hemorrhagic pulmonary edema.
In severe hypothermia mortality 25-50%.
Hypoglycemia
Is common during the neonatal period.
Definition: Blood glucose level below 40 mg/dl
Risk factors for neonatal hypoglycemia
Common
1-Prematurity
2-Infant of diabetic mother
3-IUGR
4-Asphyxia-perinatal stress
5-Hypothermia
6-Large for gestational age

3
7-Maternal medication
[tocolytics,propranolol,chloropropamide,high glucose infusion in labor]
Uncommon causes
1-Erythyroblastosis fetalis
2-Beckwith-Wiedman syndrome
3-Islet cell adenoma
4-Familial and non familial hyperinsulinism
5-Polycythemia
6-Sepsis
7-Inborn error of metabolism
7-Growth hormone deficency
8-Adrenal insufficiency
Clinical manifestations:
Hypoglycemia usually noted on first or second day of life,could be assymptomatic,to central
nervous system,and cardiopulmonary disturbances.
Hypotonia, lethargy,apathy,poor feeding,jitteriness,and seizure are common.
Congestive heart failure,tachycardia,cyanosis,pallor, diaphoresis,apnea,and hypothermia.
Differential diagnosis:
1-Congenital heart disease
2-Sepsis
3-IVH
4-Hypocalcemia
5-Hypomagnesemia
6-Inborn error of metabolism
7-Narcotic withdrawal
Prevention:
All newborn infant at risk for hypoglycemia should be monitored with serial capillary blood
glucose levels measured during first day of life.
Newborn at risk for hypoglycemia should be breast feed or given formula within the first
few hours of birth.
If oral feeding not possible because of cardiopulmonary disease 10% dextrose water should
be given intravenously.
4
Treatment:
Requires initial intravenous bolus infusion of 200mg/kg [2ml/kg] 10%glucose, this should be
followed immediately by continuous infusion of 6-8mg/kg/min of glucose.
In resistant cases can use hydrocortisone intravenously.
Other drugs can be used diazoxide, nifidipine, or somatostatin.
Surgery:
Indicated in adenoma of pancreas, or diffuse hyperplasia of pancreas.
Prognosis:
In symptomatic neonatal hypoglycemia with seizure is poor, and is associated with
abnormal neurointellectual development.
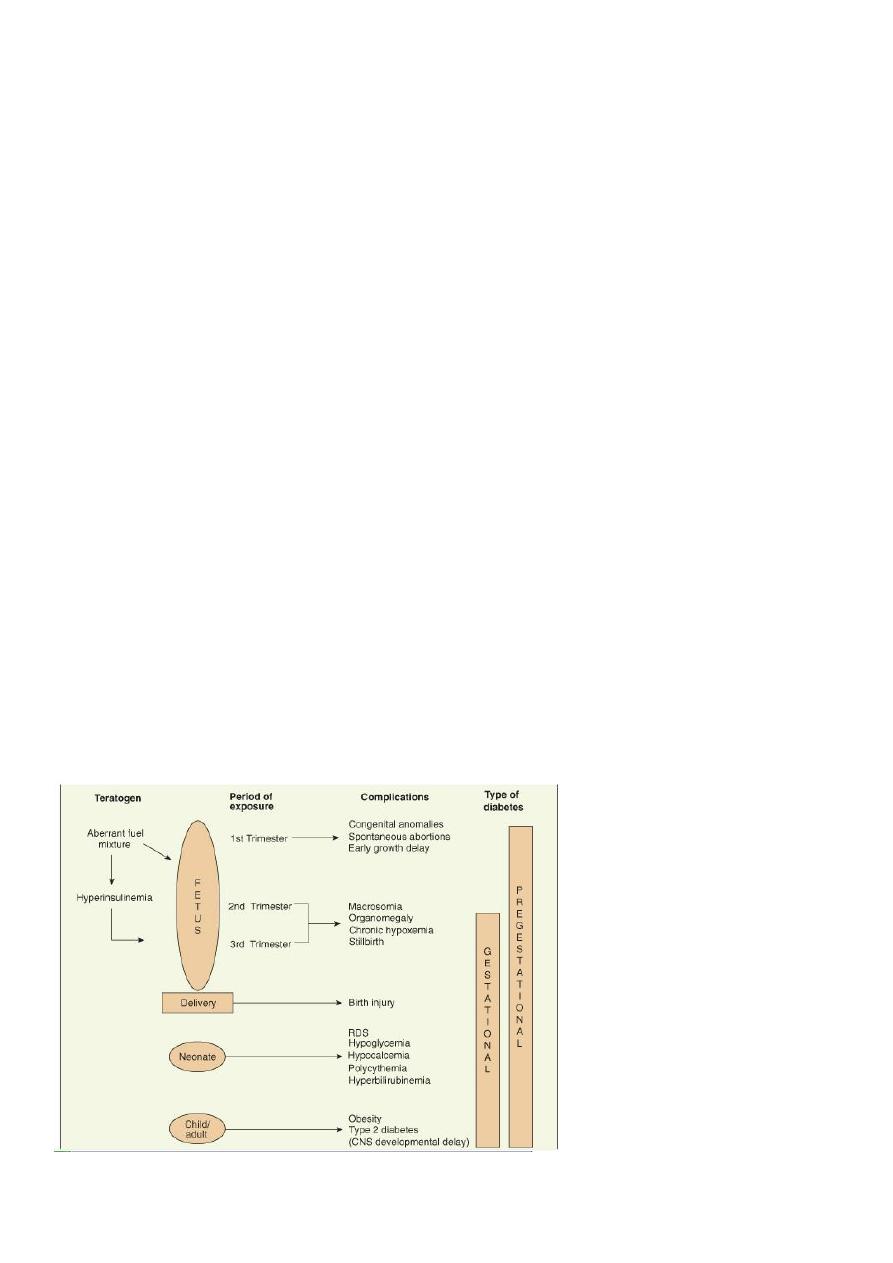
Infant of Diabetic Mother
DM present before pregnancy or develop during pregnancy[gestational diabetes is noted in
about 5% of women] adversely influences fetal and neonatal well being.
Pathophysiology
Poorly controlled maternal diabetes leads to maternal hyperglycemia, this produce fetal
hyperglycemia that stimulate fetal pancreas results in hyperplasia of islets of langerhans
leads to hyperinsulinism.
1-Fetal hyperinsulinism acts as a fetal growth hormone ,in last trimester results in increased
fat& protein synthesis& fetal macrosomia with organomegally [all organs enlarge except
the brain], fetus large for gestational age.
2-Fetal acidosis which may result in increased rate of still birth.
3-Increased extramedullary erythropoiesis results in polycythemia.
4-The separation of placenta suddenly interrupts glucose infusion in to the neonate without
proportional effect on hyperinsulinism, resulting in hypoglycemia in the first hours after
birth.
5
Clinical manifestations:
Baby tend to be large and plump,puffy plethoric facies.
The baby tend to be jumpy,tremulous,and hyperexitable.
Complications:
Maternal:
ketoacidosis
hypoglycemia
preeclampsia
polyhydromnias
retinopathy
Neonatal:
-Prematurity
-Macrosomia
-Birth trauma&birth asphyxia
-RDS, TTN
-Hypoglycemia ,nadir of blood glucose level at 1-3 hours
-Hypocalcemia,polycythemia,unconjugated hyperbilirubinemia
-Congenital malformation
hear t[cardiomegally& asymmetric septal hypertrophy]
lumbosacral agenesis,small left colon syndrome.
-Renal vein thrombosis
-Intrauterine fetal death
-Neurodevelopental delays
Treatment:
Management of these infants should be initiated before birth [during pregnancy].
After birth infant should receive intensive observation and care.
Asymptomatic infant should have a blood sugar determination hourly for first 6hours.
If baby clinically well and normoglycemic, oral feeding initially with 5%glucose water
followed by milk.
If baby can not take orally give I.V fluid 10%glucose.
If baby hypoglycemic treat by 2-4ml/kg 10% glucose water I.V.
HYPOCALCEMIA
Definition:Total serum calcium of less than7mg/dl, and ionized calcium levels of less than3-
3.5mg/dl
Etiology:
1-Early neonatal hypocalcemia: occurs in first 3days of life and is often asymptomatic.
A-Transient hypoparathyroidism especially in premature infant and infant of diabetic
mother.

6
B-Congenital absence of parathyroid gland and DiGeorge syndrome.
C-Hypomagnessemia[<1.5mg/dl] may be associated with hypocalcemia.
2-Late neonatal hypocalcemia or neonatal tetany:
A-Ingestion of high-phosphate containing milk and is associated with
hyperphosphatemia[>8mg/dl].
B-Vit D deficency and malabsorption
Clinical Manifestations:
Apnea, muscle twiching, seizures, laryngospasm, [chvostek sign&Trosseau sign are rare in
newborn period].
Treatment:
Symptomatic hypocalcemia treated by 2-4ml/kg of 10%calcium gluconate given I.V slowly
over10-15min then continous infusion of 75mg/kg/24hr of calcium.
If hypomagnesemia is associated with hypocalcemia magnesium sulfate 0.1ml/kg I.M&
repeated every 8-12hr.
Late hypocalcemia: include immediate management as early hypocalcemia,and giving
formula of low phosphate level.
Neonatal Seizures
Etiology:
1-Hypoxic-ischemic encephaolopathy: usually occur 12-24hours after birth.There is history
of birth asphyxia,also may be associated with metabolic disorder such as
hypoglycemia&hypocalcemia.
2-IVH: is common cause of seizure in premature infants and occur between 1-3 days of
age.Usually there is bulging fontanel,hemorrhagic spinal fluid,anemia,lethargy,coma.
3-Hypoglycemia: occur in at risk patients.
4-Hypocalcemia& hypomagnesemia.
5-Seizure in delivery room may be due to:
A- Injection of local anesthetic agents in fetal scalp.
B- Severe anoxia.
C- Congenital brain malformation.
6-Infection: bacterial or viral infection of brain usually occur after 5days.
7-Drug withdrawal: like methadone or heroin usually occur after 5days.
8-Inborn error of metabolism: usually there is lethargy,acidosis,and family history of infant
death
9-Other causes
-subarachnoid hemorrhage
-benign familial seizure
-vit B6 deficency or dependency

7
Types of Neonatal Seizures:
1-Subtle: most common type occur in more than 75% of cases
-Eye signs:eyelid fluttering,eye deviation,fixed open stare,blinking.
-Apnea,cycling,boxing,stepping,swimming movement of limbs.
-Mouthing,chewing,lip smacking,smiling.
2-Tonic:stiffening,decerebrate posture.
3-Clonic:repetitive jerking.
4-Myoclonic: arrhythmic contraction of muscle groups of the limb,face,or trunk.
Differential diagnosis:
Jitteriness&tremor: fine and rapid movement are sensory dependent elicited by stimuli,and
interrupted by holding the extremity and not associated with abnormal eye movements.
Investigations:
1- immediate determination of capillary blood glucose with chemstrip.
2-blood glucose,calcium,sodium,&bilirubin determination.
3-when infection suspected cerebrospinal fluid and blood culture.
Other investigations done in selected cases:
-MRI,C.T scan,or ultrasound of brain.
-Test for inborn error of metabolism
-EEG: often demonstrates seizure activity when clinical diagnosis is uncertain especially in
subtle seizure.
Treatment:
1-Specific: such as treatment of meningitis, hypoglycemia,hypocalcemia,hypomagnesemia,
hyponatremia, or vit B6 deficency or dependency.
2-Treatment of seizure:
A-Phenobarbital 20-40mg/kg I.V
B-Phenytoin 10-20mg/kg I.V infusion
C-Diazepam 0.1-0.3mg/kg I.V.
