Introduction:
Greet the doctor & introduce yourselfStand to the right side of the patient.
Greet the patient, introduce yourself & get permission.
Close the curtain around the patient’s bed (privacy is important)
When finished, thank the patient and cover his body.
During cold weather, warm your hands and instruments (stethoscope) are warm.
History Taking:
-Introductory questions:Name: full name including grandfather or surname.
(Sex + Religion)
Age
Occupation
Residency
Marital status and number of children.
-Date of admission
-Date of examination-Chief complaint and its duration before admission.
-History of the present illness: (Let the patient tell the story, avoid leading questions).
Acute condition: Talk about the current problem only.
Chronic problem: Start by brief describing overall course, admissions, diagnosis given, & medications.
Description:
The condition started (gradually, suddenly)
One system only, with all its cardinal symptoms arranged chronologically
Fever, sweating, weakness, weight loss, & anorexia could be a part of any system.
-Review of other systems: CVS, respiratory, GIT, GUT, nervous, musculoskeletal.
In surgery:
-History of the present illness & review of other systems
-Pre-operative: What investigations were done? Number of blood pints prepared?
-Operative: what procedures were done? Duration of surgery? Type of anesthesia? Fluids, blood, & drugs given during surgery? Intraoperative complications?
-Post-operative (Day 0, 1, 2...): Recovery from anesthesia. IV fluids, blood, drugs. Time of eating. Time of urination, time of passing stool, time of moving after surgery. Fever, cough, dyspnea, vomiting. Wound complications, surgical complications.
In surgery:
-History of the present illness & review of other systems
-Pre-operative: What investigations were done? Number of blood pints prepared?
-Operative: what procedures were done? Duration of surgery? Type of anesthesia? Fluids, blood, & drugs given during surgery? Intraoperative complications?
-Post-operative (Day 0, 1, 2...): Recovery from anesthesia. IV fluids, blood, drugs. Time of eating. Time of urination, time of passing stool, time of moving after surgery. Fever, cough, dyspnea, vomiting. Wound complications, surgical complications.
Past History:
Medical: Acute or chronic diseases (diabetes mellitus, hypertension, rheumatoid arthritis)Surgical interventions.
Drug History:
Any drugs received recently or chronicallyDrugs allergy: penicillin, methoprim
Blood transfusion
Personal History:
Smoking: how many packs per day and for how long? Date of cessation?Alcohol: amount and duration
Family History:
Similar problems in familyHereditary diseases
Multifactorial diseases (DM, HTN, RA)
Cause of death of siblings
Infectious diseases
Social History: SNM
Socioeconomic & housing
Nutrition and nutritional diseases.
Marital harmony
Menstrual History:
Age of menarcheDuration of menstrual cycle
Amount and duration of bleeding.
In menopause: duration, and symptoms (hot flushes)
Cardinal symptoms:
Cardiovascular system• Dyspnea: Lying flat (orthopnoea)
At night (paroxysmal nocturnal dyspnoea)
• Chest pain: On exertion (angina) On minimal exertion – record how much
• Palpitation
• Syncope
• Ankle swelling
• Pain in legs on walking (claudication)
Respiratory system
• Cough
• Sputum (amount, colour, consistency, presence of blood)
• Haemoptysis (Blood in sputum or pure)
• Wheeze
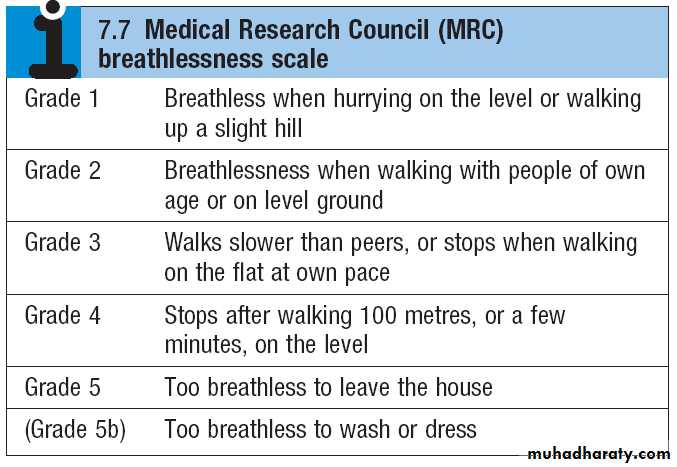
• Dyspnea (at exercise, at rest)
• Chest pain (due to inspiration or coughing)
Note: CVS and respiratory systems are taken together in some patients with overlapping cardiac and respiratory system.
Gastrointestinal system
• Mouth (oral ulcers, dental problems)• Dysphagia: Difficulty swallowing, distinguish from pain on swallowing (odynophagia)
• Nausea, vomiting and vomiting of blood (haematemesis)
• Regurgitation
• Heartburn
• Abdominal pain
• Change in bowel habit: constipation, or diarrhea (amount, color, consistency, frequency, presence of blood or mucous or pus, presence of tenesmus or abdominal pain, presence of fever or vomiting)
• Change in color of stools (pale, dark, tarry black, fresh blood)
• Jaundice: itching (obstructive jaundice), upper abdominal pain (hepatitis and cholangitis), color of urine and stool (dark urine and pale stool in obstructive jaundice).
• Appetite
• Weight loss (>3 kg over 6 months is significant)
Genitourinary system
A-Local:
• Pain: renal (loin pain), bladder (suprapubic_.
• Urination (amount, color, frequency)
• Dysuria (pain when passing urine)
• Nocturia (frequently passing urine at night)
• Haematuria (blood in the urine)
• Passing renal stones
• Incontinence (stress and urge)
• Libido
B-General:
• Puffiness of face and leg swelling (glomerulonephritis and fluid retention)• Uremia (Anorexia & fatigue, headache, nausea, vomiting, disturbed consciousness)
Nervous system
• Headaches• Dizziness (vertigo or lightheaded)
• Loss of consciousness (faints and fits)
• Visual disturbance
• Hearing problems (deafness, tinnitus)
• Limb Weakness
• Paresthesia (pins and needles)
• Altered sensation
• Incontinence (stress and urge)
Musculoskeletal system
• Joint: pain, swelling, stiffness, or deformity.
• Backache • Mobility
Hematological:
1-Anemia: dizziness, fatigue, fainting, dyspnea, palpitation2-Leukopenia: fever, sore throat.
3-Thrombocytopenia: bleeding, bruises.
4-Lymph nodes: Lumps and swellings
5-Bone pain.
Symptom Analysis:
Pain:Site
Duration
Radiation
Character
Severity (interfere with normal activity, wakes the patient up from sleep)
Time of occurrence
Frequency
Relieving factors (rest, medication)
Aggravation factors (exercise, special food)
Associated symptoms.
Shortness of breath (SOB) AAA
At lying or at nightAt exertion or at rest (at what degree of exertion)Associated symptoms (cough, wheeze, allergy to dust, palpitation)
Fever:
Continuous or intermittent?Presence of chills, shivering, rigors?
Associated symptoms (sweating, loss of appetite, fatigue, aches)
Note: when presenting the history, avoid Latin words. In other words, use the words of the patient.e.g.: shortness of breath (dyspnea), vomiting of blood (hematemesis), fainting (syncope).
The General Examination
1-General Description2-Head
3-Neck
4-Hands
5-Leg
6-Vital signs
1-General Description
Age, Sex, Appearance, Position, Conscious state (drowsy, stuporous, comatose), Build (thin, obese, average build), Additional (cannula, AV shunt, O2 mask), Dyspnea.
E.g.: A young lady who looks ill, she is lying down, fully conscious, and of average build.There are cannula in her left hand, O2 mask, and a blood unit.
She looks dyspnic at rest.
2-Head
Hair:Coarse dry lusterless: hypothyroidism
Alopecia :localized; skin disease, Generalized; SLE
Face:
Facial expression: sad, angry, anxiousSpecial faces: cushing, acromegaly, thyrotoxicosis, myxedema, butterfly rash of SLE
Skin Color:
Pallor: anxiety, anemia, shock, hypopituitarism, nephrotic syndromeJaundice: under natural light
Yellow-brownish “earthy pale”: chronic kidney disease
Pleothoric: polycythemia
Pigmentation: addisions, haemochromatosis, cloasma.
Malar flush: mitral stenosis
Eye:
Puffiness: nephrotic syndrome, myxedema, allergy
Xanthelasma: soft yellowish plaques periorbitally and on the medial aspect of the eyelids associated with hyperlipidaemia
Conjunctiva: slightly push the lower eyelid
pallor, congestion “polycythemia or conjunctivitis”, jaundice.
Sclera: Ask the patient to look downward
subconjunctival haemorrhage “ in bleeding tendency, conjunctivitis, severe cough
Cornea : corneal arcus “arcus senilis” due to hyperlipidaemia
Lens: cataract
Lips:
Angular cheilitis and cheilosisColor: tattooing, cyanosis
Ulcer: herpis labialis
Gums: Gingivitis (red and swollen), hypertrophy (scurvy, leukemia, phenytoin)
Teeth: Caries, loss, denture.Tounge: Ask the patient to put out his tongue.
Size: large in Acromegaly.Shape : geographical tongue
Surface:
furred (heavy smokers)
oral thrush,
Leukoplakia (thickened white patch that cannot be scraped off the tongue. It may be premalignant)
Colour: red in glossitis, pale in severe anemia.
Movements :
Tremor “can be due to anxiety, thyrotoxicosis”
Fasciculation: irregular ripples or twitching of the tongue occurs in lower motor neurone disease”.
Frenulum (cyanosis, jaundice)
Buccal Mucosa: using tongue depressor and light
Pigmentation: Addison’s disease
Petechia: bleeding, infectious mononucleosis
Lesion: thrush, aphthous
Tonsils (say Ahhh, with tongue depressor and light): enlarged with whitish discharge in tonsillitis
Pharynx: redness and post nasal discharge.
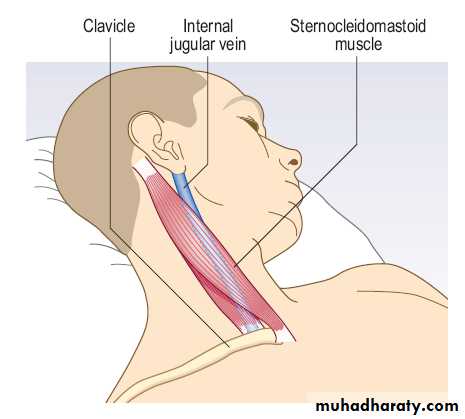
3-Neck1-Pulsations: Carotid, JVP
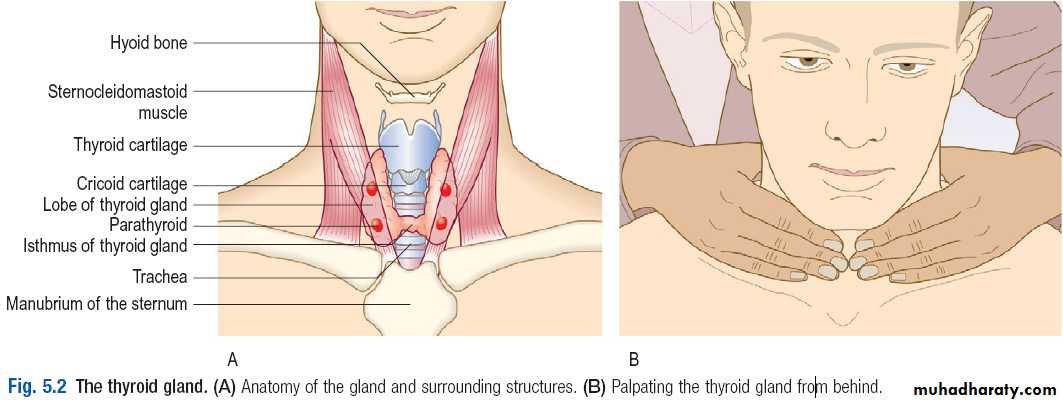
2-Thyroid:General
Overall:Agitation, restlessness or apathy and lethargy
The facial appearance and expression.
Signs of weight loss or gain
Eyes:
Exophthalmos: best seen from above
Diplopia, conjunctival oedema or conjunctivitis, corneal ulceration.
Lid retraction: this is present if the sclera is visible above the iris.
Lid lag: ask the patient to follow your index finger as you move it from the upper to the lower part of his visual field. Delay between the descent of the upper eyelid in relation to that of the eyeball is lid lag.
Listen to voice because it may be characteristic in sever hypothyroidism
Hands:Fine tremor and sweating (in hyperthyroidism)
Carpal tunnel syndrome may complicate myxedema
Hand changes in thyroid acropathy
Pulse: tachycardia and AF can occur in thyrotoxicosis.
Legs: pretibial myxedema
Inspection:Inspect the neck from the front. Give the patient a glass of water and ask him to take a sip. Look for a swelling while he swallows.
Palpation:
Ask the patient to sit with the neck muscles relaxed and stand behind him. Feel the gland.Place your hands gently on the front of the neck, with your index fingers just touching. Ask him to swallow a sip of water and feel the gland as it moves upwards.
Some patients find neck palpation uncomfortable, so be alert for any signs of distress.
Note the size, shape and consistency of any goitre and feel for any thrill.
Measure any discrete nodules with callipers.
Record the maximum neck circumference of a large goiter using a tape measure (objective measurements are useful for long-term follow-up).
Percussion:
In the prescence of retrosternal extension, the trachea is implapable below the thyroid, percussion note is dull in upper sternum, and when the patient is asked to elevate his arm above his head he will suffocate.
Auscultate:
Auscultate with your stethoscope for a thyroid bruit. A thyroid bruit may be confused with other sounds: bruits from the carotid artery or transmitted from the aorta are louder along the line of the artery.Transient gentle pressure over the root of the neck will interrupt a venous hum from the internal jugular vein.
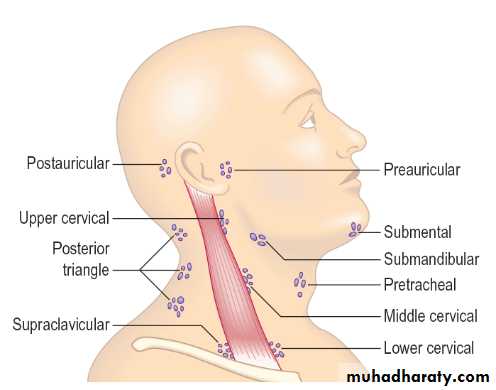
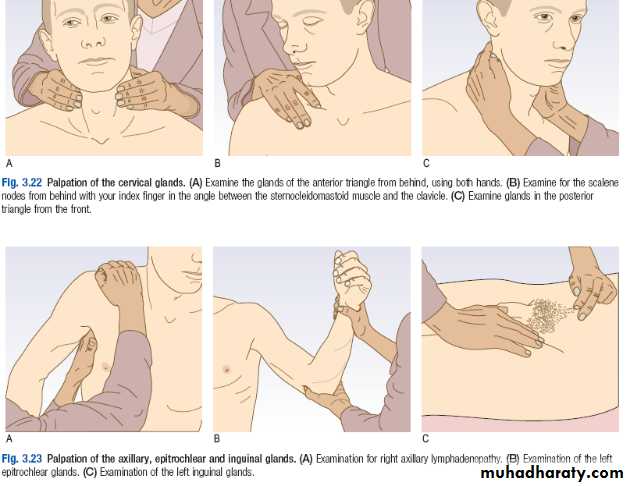
3-Lymph nodes:
Inspect for visible lymphadenopathy.
Palpate one side at a time using the fingers of each hand in turn.Compare with the nodes on the contralateral side.
Assess:
site
size.
consistency.
tenderness.
determine whether the node is fixed to deep structures, or skin.
E.g.: anterior cervical lymph node is enlarged “about 1 cm in diameter” discrete rubbery, not tender and immobile.
Cervical nodes
Examine the cervical and axillary nodes with the patient sitting.From behind, examine the submental, submandibular, preauricular, tonsillar, supraclavicular and deep cervical nodes in the anterior triangle of the neck
Palpate for the scalene nodes by placing your index finger between the sternocleidomastoid muscle and clavicle. Ask the patient to tilt his head to the same side and press firmly down towards the first rib
From the front of the patient, palpate the posterior triangles, up the back of the neck and the posterior auricular and occipital nodes.
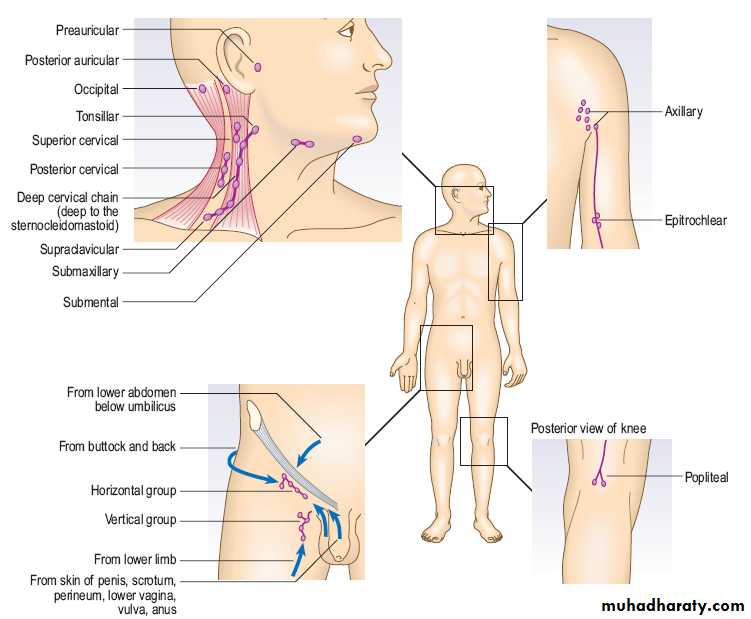
Axillary nodes
From the patient’s front or side, palpate the right axilla with your left hand and vice versa.Gently place your fingertips into the apex of the axilla and then draw them downwards, feeling the medial, anterior and posterior axillary walls in turn.
Epitrochlear nodes
Support the patient’s right wrist with your left hand, hold his partially flexed elbow with your right hand and use your thumb to feel for the epitrochlear node. Examine the left epitrochlear node with your left thumb.Inguinal nodes
Examine for the inguinal and popliteal nodes with the patient lying down.Palpate over the horizontal chain, which lies just below the inguinal ligament, and then over the vertical chain along the line of the saphenous vein.
Popletial nodes
4- Hand (compare both hands)
Joint: swelling, stiffness, deformity.
Muscle wasting: bilateral (systemic), Unilateral (neurologic or myopathic)Skin color:
Pallor: compare with your hand
Cyanosis: central (warm) , peripheral (cold)
Palmar erythema.
Nail:
Leukonychia: White nail in hypoalbumenemia.
Koilonychia: Flat or spoon shaped
Onycholysis: detachment of the nail from the nail bed.
Clubbing:
Look across the nail bed from the side of each finger. Observe the distal phalanges, nail and nail bed.
Measure the nail bed angle.
Place the nails of corresponding fingers back to back and look for a visible gap between the nail beds – Schamroth’s window sign.
Place your thumbs under the pulp of the distal phalanx and use your index fingers alternately to see if you can feel movement of the nail on the nail bed. This is fluctuation.
Abnormal movement:
Rest tremor in Parkinsonism.Tremor of outstretched hands: fine tremor in anxiety and thyrotoxicosis, coarse tremor in essential and senile tremor.
Flapping tremor (asterixis) of outstretched arms and dorsiflexed hands. Occurs in liver failure, renal failure, respiratory failure type II (CO2 retention)
Intention tremor: occurs during movement, in cerebellar disease.
5-Leg (compare both legs)
Inspect for:
Limb ischemia (6P)
Deformity or amputation (Count the toes)
Check:
Temperature
Edema (unilateral or bilateral): Apply firm pressure with your fingers or thumb for at least 15 seconds. Pitting may persist for several minutes until it is obliterated by the slow return of the displaced fluid.
6-Vital signs
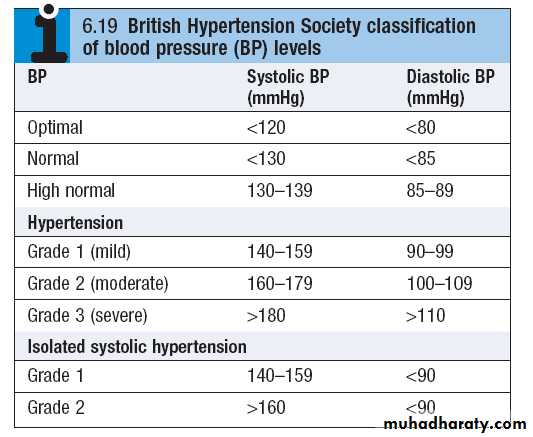
1-Pulse: 60-90bpm2-Blood pressure: 120/80 mmHg
3-Temperature: 37 ℃ ± 0.2: sublingually, armpit, rectal (core) 4-Respiratory rate (14/min): distract patient’s activity by pretending to examine the pulse.
CVS examination
General:Hands and skin
1-Dorsal aspect of the hands:
Tobacco “tar” staining
Peripheral cyanosis.
Temperature.
Clubbing
Splinter haemorrhages (linear, reddishbrown marks along the axis of the finger and toenails, thought to be due to circulating immune complexes).
2-Palmar aspect of the hands:
Janeway lesions – painless red spots, which blanch on pressure, on the thenar/hypothenar eminences of the Palms, and soles of the feet.
Osler’s nodes – painful raised erythematous lesions which are rare but found most often on the pads of the fingers And toes.
3-Palmar and extensor surfaces of the hands: xanthomata (yellow skin or tendon nodules from lipid deposits).
4-Entire skin surface: petechiae.
The face and eyesCentral cyanosis.
Xanthelasmata
Corneal arcus (iris).
Conjunctival petechiae.
Fundi: features of hypertension, diabetes and roth’s spots (flame-shaped retinal haemorrhages with a ‘cotton-wool’ centre).
Measuring blood pressure
Rest the patient for 5 minutes.With the patient seated or lying down, support the patient’s arm comfortably at about heart level, with no tight clothing constricting the upper arm.
You can measure over thin clothing, as it makes no difference to the result.
Always measure BP in both arms (brachial arteries); the higher of the two is closest to central aortic pressure and should be used to determine treatment.
The usual sphygmomanometer cuff has a bladder width of 12.5 cm and length of 30–35 cm. Apply the cuff to the upper arm, with the centre of the bladder over the brachial artery. Palpate the brachial pulse.
Inflate the cuff until the pulse is impalpable. Note the pressure on the manometer; this is a rough estimate of systolic pressure.
Inflate the cuff another 30 mmHg and listen through the diaphragm of the stethoscope placed over the brachial artery.
Deflate the cuff slowly (2–3 mmHg/s) until you hear a regular tapping sound (phase 1 Korotkoff sounds). Record the reading to the nearest 2 mmHg. This is the systolic pressure.
Continue to deflate the cuff slowly until the sounds disappear.
Record the pressure at which the sounds completely disappear as the diastolic pressure (phase 5). If muffled sounds persist (phase 4) and do not disappear, use the point of muffling as the diastolic pressure
E.g.: The blood pressure is 146/92 mmHg, right arm, supine.
Assess any hypertensive patient for:
Underlying cause.
End-organ damage:
Heart (HF)
Kidney (chronic kidney disease)
Retina (hypertensive retinopathy)
Overall risk of vascular disease: stroke, MI.
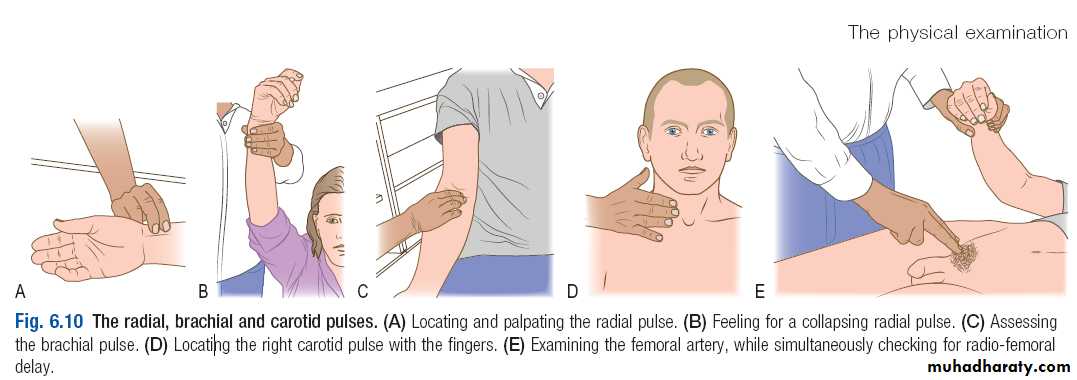
Pulse
Radial Pulse:1-Using the pads of your index and middle fingers over the right radial artery. Count the pulse rate over 30 seconds; multiply by 2 to obtain the beats per minute (bpm).
2-Examine vessel wall: after obstructing the brachial artery by the other hand.
3-Collapsing pulse: check that the patient has no shoulder or arm pain. Feel the pulse with the base of your fingers, then raise the patient’s arm vertically above the patient’s head.
4-Palpate both radial pulses simultaneously (then radial and femoral), assessing any delay between the two, and any difference in pulse volume.
Brachial pulse
With the patient’s hand extended, use your index and middle fingers to palpate this over the lower end of the humerus just above the elbow joint. Assess the character and volume.
Carotid pulse
1-Gently place the tips of your fingers between the larynx and the anterior border of the sternocleidomastoid muscle and feel the pulse2-Listen for bruits over both carotid arteries, using the diaphragm of your stethoscope during held inspiration.
Note: Lie the patient semirecumbent in case you induce a reflex bradycardia.
Femoral pulse
1-Place your index and middle fingers over the femoral artery, which is just inferior to the midpoint between the anterior superior iliac spine and the pubis.2-check for radiofemoral delay (coarctation of the aorta) by simultaneously feeling the radial pulse.
3-Listen for bruits over both femoral arteries, using the diaphragm of the stethoscope.
Popliteal pulse
The patient is lying down, flex the patient’s knee to 30°.With your thumbs in front of the knee and your fingers behind, press firmly in the midline over the popliteal artery.
Then slide your fingers 2–3 cm below the knee crease and try to compress the artery against the back of the tibia as it passes under the soleal arch.
Posterior tibial pulse: Feel 2 cm below and 2 cm behind the medial malleolus, using the pads of your middle three fingers.
Dorsalis pedis pulse: Using the pads of your middle three fingers, feel in the middle of the dorsum of the foot just lateral to the tendon of extensor hallucis longus.
Findings:
1-Radial artery:Rate: normal 60-90, tachycardia >100, bradycardia >60
Rhythm: Regular-sinus rythm, regular irregularity-ectopic at regular interval or 2nd degree atrioventricular block, irregular irregularity- atrial fibrillation, atrial flutter, multiple ectopics (differentiated from AF: it subsides with exercise, no pulse deficit).
Volume: large, small volume
Character: collapsing pulse, slow-rising pulse, pulsus bisferiens, pulsus alternans, pulsus paradoxus.
Vessel wall: Just palpable, thickened in atherosclerosis
Present bilaterally
Radioradial and radiofemoral delay (considered a volume abnormality).
2-Brachial artery: Volume and character.
3-Carotid: auscultate for bruit (carotid artery stenosis or radiation of aortic stenosis) while the patient is holding his breath in.
4-Femoral: auscultate for bruit.
5-Popletial
6-Posterior tibial
7-Dorsalis pedis
E.g.: The pulse is 80 bpm of regular rhythm and normal volume.
There is collapsing pulse, the vessel wall is just palpable, & the pulse is present bilaterally.No radioradial delay, no radiofemoral delay.
The other arterial pulses are present without bruit in carotid or femoral.
Artery Surface marking
Radial: lateral to the flexor carpi radialis tendon
Brachial: In the antecubital fossa, medial to the bicepstendon
Carotid: At the angle of the jaw, between the larynx and the anterior border of sternocleidomastoid muscle
Femoral: Just below the inguinal ligament (the mid inguinal point). It is immediately lateral to the femoral vein and medial to the femoral nerve
Popliteal: Lies posteriorly in relation to the knee joint, at the level of the knee crease, deep in the popliteal fossa.
Posterior tibial: Located 2 cm below and posterior to the medial malleolus, where it passes beneath the flexor retinaculum between flexor digitorum longus and flexor hallucis longus
Dorsalis pedis: Passes lateral to the tendon of extensor hallucis longus and is best felt at the proximal extent of the groove between the first and second metatarsals.
Pulsus paradoxicus
Place a BP cuff and inflate until no sounds are heard.Decrease the cuff pressure until sounds are heard only on expiration. Note the reading.
Decrease the cuff pressure again until sounds are heard throughout the respiratory cycle; again note the reading.
A difference >10 mmHg on inspiration is pulsus paradoxus.
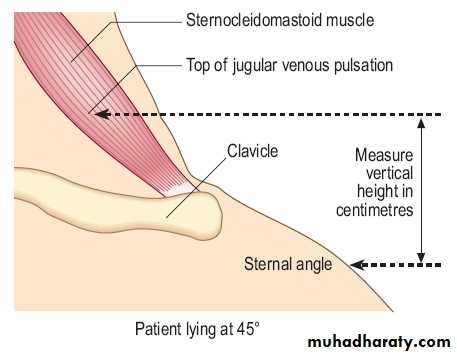
Jugular Venous Pressure JVP
The JVP is best seen on the patient’s right side when the patient is supine, reclined at 45°, with the head on a pillow to relax the sternocleidomastoid muscles.Use oblique lighting if the JVP is difficult to see. The jugular vein pulsation in the suprasternal notch or behind the sternocleidomastoid muscle.
Identify: the timing and waveform of the pulsation and note any abnormality.
If not certain, Use the abdomino-jugular test or occlusion to confirm it is the JVP.
Measure: JVP is the vertical height in centimetres between the upper limit of the venous pulsation and the sternal angle (junction of the manubrium and sternum at the level of the second costal cartilages) by using a pen and a tape measure.Normally it is ≤4 cm from sternal angle, when the patient lies at 45°.
E.g.: The patient is examined while lying at 45°.
There is pulsation in the lateral side of the neck, wavy and visible, not palpable, with upper limit & 2 distinct peaks.
It decreases with inspiration, increases with abdominojugular reflux, and wave form is obliterated by occluding the base of neck.
The Precordium
Inspection:Remove all clothing above the waist to inspect the precordium with the patient sitting at a 45° angle with shoulders horizontal.
Visible pulsation
Deformity: funnel chest, pigeon chest)
Scar:
Midline sternectomy (Coronary artery bypass grafting CABG, Aortic valve replacement)
Left submammary (mitral valvatomy)
Infraclavicular (pacemaker, defibrillator)
Palpation:
Place your right hand flat over the precordium to obtain a general impression of the cardiac impulse.Apex position & character: by lying your fingers on the chest parallel to the rib spaces. If not palpable, roll the patient to his left side. Detect the position by counting the ribs starting from sternal angle (2nd intercostal space).Normal apex is in the 5th intercostal space, at or medial to mid-clavicular line.
Heave: Have the patient held his breath on expiration, note the heave by pressing the heel of your right hand firmly on left parasternal area.
Thrills : using the flat of your fingers palpate the apex and both sides of the sternum.
Percussion is not usually done, but is useful in pericardial effusion.
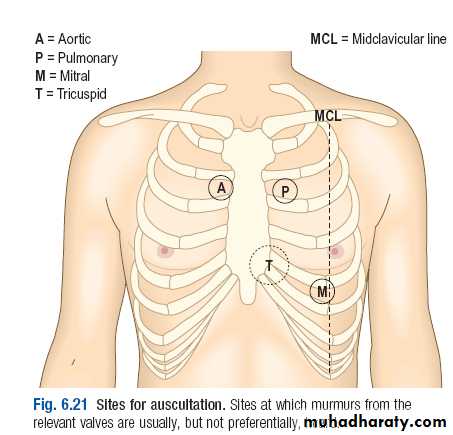
Auscultation:
Make sure the room is quiet when you auscultate. Your stethoscope should fit comfortably with the earpieces angled slightly forward. Listen with your stethoscope diaphragm at the:apex
lower left sternal border
upper right and left sternal borders.
Listen with your stethoscope bell at the:
apexlower left sternal border.
Listen over the carotid arteries (radiation of ejection systolic murmur of aortic stenosis) and in the left axilla (radiation of pansystolic murmur of mitral regurgitation).
Listen for murmurs (examine the carotid artery to time any murmur)
Mitral Stenosis: roll the patient on to his left side then listen at the apex using light pressure with the bell.Aortic regurgitation: ask the patient to sit up and lean forwards, then to breathe out fully and hold his breath. Listen over the right second intercostal space and over the left sternal edge with the diaphragm.
Findings:
Heart Sounds: S1: Apex
S2: upper left sternum
S3 & S4: Apex
Murmurs:
1-Location: the site(s) where you hear the murmur best. This helps to differentiate diastolic murmurs (mitral stenosis at the apex, aortic regurgitation at the left sternal edge), but is less helpful with systolic murmurs, which are often loud over all the precordium.
2-Timing: palpate the patient’s carotid pulse while listening to the precordium. S1 barely precedes the upstroke of the carotid pulsation while the S2 is clearly out of phase with it.
Systole: begins with the S1.
Diastole: is the interval between S2 and S1.
3-Duration
Systolic: ejection systolic or pansystolicDiastolic: Early diastolic or mid diastolic.
The ejection systolic murmur of aortic or pulmonary stenosis begins after S1 reaches maximal intensity in mid-systole, then fades, stopping before S2.
4-Character and pitch: The quality of a murmur is subjective, but terms such as harsh, blowing, musical, rumbling, high- or low-pitched can help.
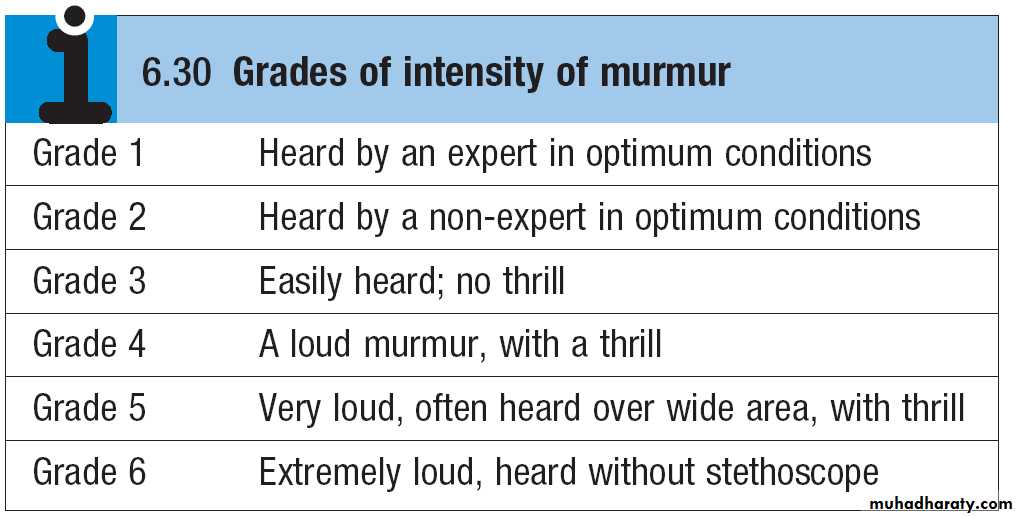
5-Intensity
Describe any murmur according to its grade of intensity. Diastolic murmurs are rarely louder than grade 3.6-Radiation
The pansystolic murmur of mitral regurgitation towards the left axilla
ventricular septal defect murmur radiates towards the right sternal edge
Aortic stenosis murmur radiates the carotid arteries.
Added sounds:
Opening snapsEjection clicks
Pericardial rub (friction rub) is a coarse scratching sound, often with systolic and diastolic components. It is best heard using the diaphragm with the patient holding his breath in expiration. It is heard over the precordium, but often localized.
Pleuropericardial rub ‘crunching’ noise.
E.g.: On auscultation of the precordium, there were normal heart sounds.
A pansystolic murmur is heard is heard on the aortic area, with radiation to the carotid arteries. It is a grade 3 murmur.No added sounds.
Notes:
The most common murmurs are:Mitral stenosis & mitral regurgitation.Aortic stenosis & aortic regurgitation
The common diastolic murmurs (mitral stenosis, aortic regurgitation) need a maneuver to hear, localized, and rarely more than grade 3.
The remaining common systolic murmurs (mitral regurgitation, aortic stenosis) are easily heard, not localized, and sometimes with radiation.
Respiratory examination
General
General inspection from end of the bed with the patient lying on one pillow and shoulders are out of the pillow (for orthopnea).
Generally, Look for:
Respiratory distress
Respiratory symptoms
Fever
Weight loss
Face: SACH
Special faces (cushing due to steroids)Anemia
Central cyanosis
Horner syndrome (apical lung cancer)
Neck
Pulsation (elevated JVP in cor pulmonale or superior vena cava obstruction by lung cancer)Thyroid (goiter causes tracheal obstruction)
Lymph node
Hands
Radial pulse :Tachycardia: B agonists or respiratory difficulty
AF: lung Cancer
Pulsus paradoxicus: large pneumothorax or tension pneumothorax.
Blood pressure
Tobacoo “tar” staining
Cyanosis, clubbing, pulmonary osteoarthropathy
Asterixes (respiratory failure II)
Leg: Edema (DVT, cor pulmonale).
Chest
Inspection:Respiratory rate (14/min) and rhythm (Cheyne stokes in head injury & high altitude & CO poisoning , Kussmauls breathing in metabolic acidosis)
Inspect for:
Chest deformity (Kyphosis, scoliosis, funnel chest)
Scar
Gynecomastia, mass, dilated veins.
Intercostal recession
Paradoxical chest movement (flail chest), or paradoxical inward movement of the abdomen during inspiration
Chest diameter (hyperinflation in COPD and asthma)
look from the end of the bed for Asymmetry: (pneumothorax, collapse, consolidation, asthma)
Listen to: hoarsness of voice recurrent laryngeal nerve damage
Palpation
Trachea:With the patient looking directly forwards, look for any deviation of the trachea. Gently place the tip of your right index finger into the suprasternal notch and palpate the trachea. This can be uncomfortable; be gentle and explain what you are doing. Slight displacement to the right is common in healthy people.
Measure the distance between the suprasternal notch and cricoid cartilage, normally 3–4 finger breadths; any less suggests lung hyperinflation.
Tracheal tug: with fingers resting on patient trachea, they move inferiorly with inspiration.
Cardiac apex beat (“with the trachea“ to determine the position of mediastinum).
Impalpable.
Deviated
Also examine the heave of right ventricle.
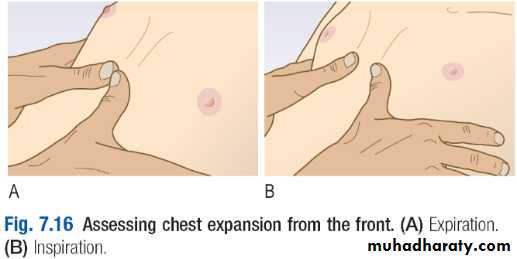
Chest expansion
Upper lobes: Stand behind the patient and assess expansion of the upper lobes by watching the clavicles during tidal breathing.
Lower lobes: Assess expansion of the lower lobes by placing your hands firmly on the chest wall (below nipples) . Extend your fingers around the sides of the patient’s chest. Your thumbs should almost meet in the midline and hover just off the chest so they can move freely with respiration. Ask the patient to take a deep breath. Your thumbs should move symmetrically apart by at least 5 cm.
Tactile vocal fremitus: by using the ulnar side of heel of hand. Ask the patient to say one one one.
Percussion
1-Clavicle: directly over the medial third, as percussing laterally is dull over the shoulder muscles.
2-Intercostal spaces: anteriorly and laterally, by placing the palm of your left hand on the chest, with your fingers slightly separated, press the middle finger of your left hand firmly against the chest, aligned with the underlying ribs over the area to be percussed. Strike the centre of the middle phalanx of your left middle finger with the tip of your right middle finger, using a loose swinging movement of the wrist and not the forearm.
Remove the percussing finger quickly so the note generated is not dampened. Percuss the lung apices by placing the palmar surface of your left middle finger across the anterior border of the trapezius muscle, overlapping the supraclavicular fossa and percussing downwards. Map out abnormal areas by percussing from resonant to dull. Percuss each side alternately and compare the note.
3-Back: Ask the patient to fold the arms across the front of the chest, moving the scapulae laterally and percuss the upper posterior chest. Do not percuss near the midline, as solid structures of the thoracic spine and paravertebral musculature produce a dull note.
E.g.: on percussion the chest was resonant anteriorly. Cardiac and liver dullness were present (or impaired, absent)
Auscultation
Ask the patient to relax, breath deeply through his open mouth.
Describe:
Normal (vesicular sound)
Added sounds
Ronchi wheeze
Rales (Crackles, Crepitation): Ask the patient to cough, to clear the normal secretions that may cause crackles.
Pleural rub: creaking sound produced by stiff pleura ( due to pleurisy)
Vocal resonance: Ask the patient to say ‘one, one, one’ while you auscultate to assess the quality and amplitude of vocal resonance. Ask the patient to whisper ‘one, one, one’ while you continue to listen.
Stridor: Harsh inspiratory sound produced by partial obstruction of large airways. Ask the patient to cough and then breathe deeply in and out with the mouth wide open. Listen closely to the patient’s mouth, for stridor.
Avoid asking him to breathe deeply for prolonged periods, as this causes giddiness and even tetany. Auscultate each side alternately, comparing findings over a large number of equivalent positions to ensure that you do not miss localised abnormalities.
Anteriorly from above the clavicle down to the sixth rib
Laterally from the axilla to the eighth rib
Posteriorly down to the level of the 11th rib.
E.g.:
There is bronchial breathing in upper anteriolateral chest.There is diminished vesicular breathing
There is vesicular breathing with prolonged expiratory phase (normally expiration is barely heard). This is a typical presentation of COPD “barrel chest, audible wheeze”
Abdomen
General:
Record Height, weight, and BMI.Muscle wasting.
Hydration
Pain: colicky (writhing patient), peritonitis (still patient)
Purpura: Hypersplenism, impaired clotting in liver disease.
Respiration rate (increase in metabolic acidosis) and smell ( fetor hepaticus, alcohol, ketone, uremia)
Hand:
ClubbingKoilonychia: spoon shaped
Leukonychia : hypoalbuminemia
Asterixis: Liver failure
Palmar erythema: chronic liver disease
Head and neck:
PallorJaundice
Kayser-Fleischer rings: Wilsons disease
Spider nevi: Chronic liver disease
Parotid swelling: Mumps
Ulcers
Angular stomatitis: iron deficiency
Atrophic glossitis (pale, smooth) in iron deficiency. B12, folate deficiency causes the tounge to be beefy raw in appearance.
Troisier sign: enlarged left supraclavicular (left Virchow) lymph node in metastatic gastric and pancreatic cancer.A more widespread lymphadenopathy with hepatosplenomagly indicates lymphoma,
In surgery: from nipples to knees.
In surgery: from nipples to knees.
Inspection
Expose the abdomen from the xiphisternum to the symphysis pubis. Position the patient supine with the head resting on only one or two pillows to relax the abdominal wall muscles
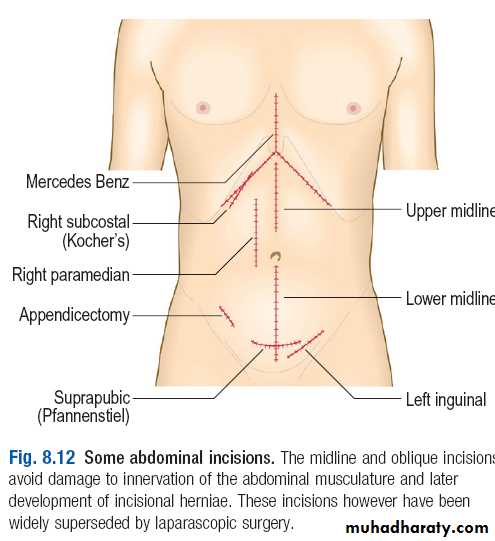
Scar
Swelling:look from foot of bed for any asymmetry.
Generalized or localized
Obesity (umbilicus is usually sunken)
Ascites (umbilicus is flat or everted)
Straie
Dilated veins portal hypertension
Inferior vena caval obstruction
Rarely superior vena caval obstruction
Is the patient in pain ?
Writhing movement due to colic
Still in peritonitis
Does abdomen move with respiration ( Still in peritonitis)
Umbilicus
Superficial Palpation
-Ask the patient to place the arms by the sides, one pillow under the head and another one under the knee to help relax the abdominal wall.
-If the bed is low, kneel beside it. Ask the patient to show you where any pain is and to report any tenderness elicited during palpation.
-Use your right hand, keeping it flat and in contact with the abdominal wall.
Tenderness: Ask the patient about tenderness. Begin with light superficial palpation away from any site of pain. Observe the patient’s face for any sign of discomfort throughout the examination.
Soft or hard abdomen? Hard abdomen in:
peritonitis (generalized)
appendicitis (localized)
Mass:
Describe any mass using the basic principles. To determine if a mass is superficial and in the abdominal wall rather than within the abdominal cavity, ask the patient to tense the abdominal muscles by lifting his head. An abdominal wall mass will still be palpable, whereas an intra-abdominal mass will not.
Decide whether the mass is an enlarged abdominal organ or separate from the solid organs.
Note: If you suspect ascites, postpone deep palpation until you conform ascites. In this case the deep palpation will be by dipping method.
Ascites
-Shifting dullnessWith the patient supine, percuss from the midline out to the flanks. Note any change from resonant to dull, along with areas of dullness and resonance.
Keep your finger on the site of dullness in the flank and ask the patient to turn on to his opposite side.
Pause for 10 seconds to allow any ascites to gravitate, then percuss again. If the area of dullness is now resonant, shifting dullness is present, indicating ascites.
-Fluid thrill (only detected in gross ascites).
Place the palm of your left hand flat against the left side of the patient’s abdomen and flick a finger of your right hand against the right side of the abdomen.
If you feel a ripple against your left hand, ask an assistant or the patient to place the edge of his hand on the midline of the abdomen. This prevents transmission of the impulse via the skin rather than through the ascites. If you still feel a ripple against your left hand, a fluid thrill is present.
Deep palpation:
In surgery: hand is horizontal on the abdomenIn surgery: hand is horizontal on the abdomen
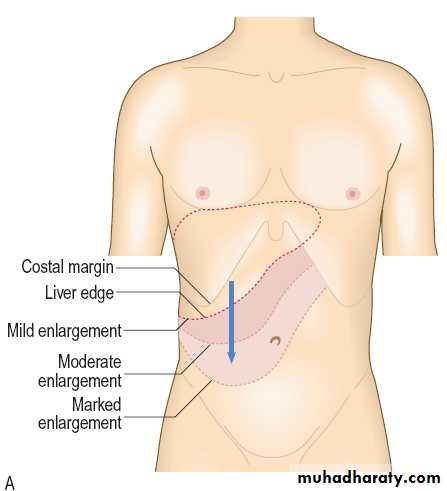
1-Hepatomegaly
1-Place your hand flat on the skin of the right iliac fossa. Point your fingers upwards and your index and middle fingers lateral to the rectus muscle, so that your fingertips lie parallel to the rectus sheath. Keep your hand stationary. Ask the patient to breathe in deeply through the mouth. Feel for the liver edge as it descends on inspiration. Move your hand progressively up the abdomen, 1 cm at a time, between each breath the patient takes, until you reach the costal margin or detect the liver edge. The liver may be enlarged or displaced downwards by hyperinflated lungs.2- Ask the patient to hold his breath in full expiration. Percuss downwards to the right fifth intercostal space in the mid-clavicular line, listening for the dullness that indicates the upper border of the liver.
3-Measure the distance in centimetres below the costal margin in the mid-clavicular line or from the upper border of dullness to the palpable liver edge.
If you feel a liver edge, describe:
Size (normal span is 6-12 cm)Surface: smooth or irregular
Edge: smooth or irregular
Consistency: soft , firm, hard
Tenderness
Whether it is pulsatile: tricuspid regurgitation
Bruits : hepatocellular ca, alcoholic hepatitis
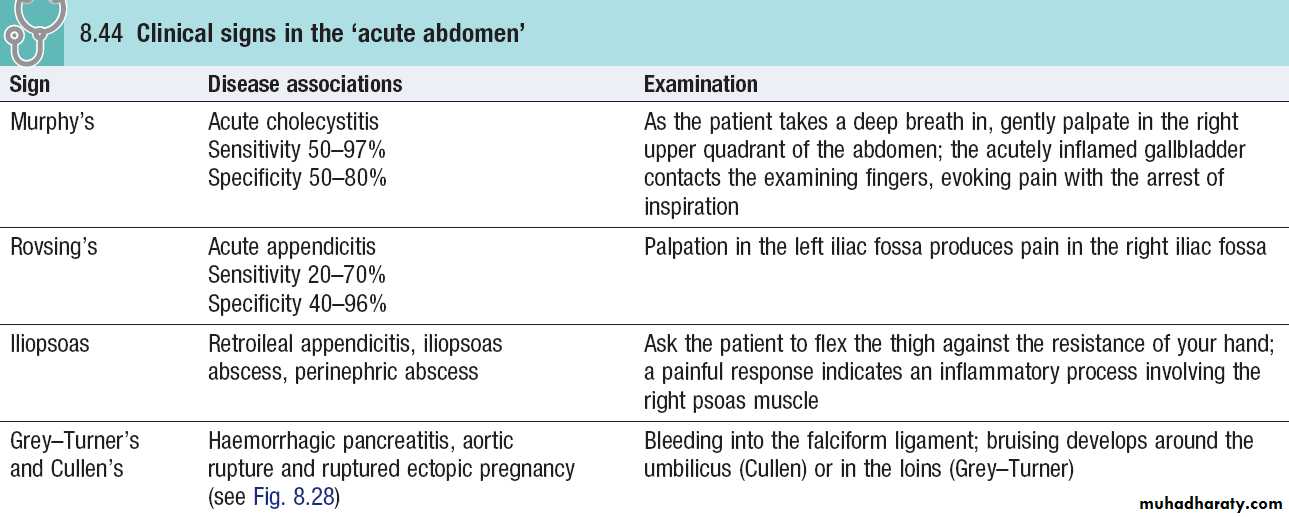
2-To feel for gallbladder tenderness (in cholecystitis):
Ask the patient to breathe in deeply and gently palpate the right upper quadrant of the abdomen in the mid-clavicular line. As the liver descends, the inflamed gallbladder contacts the fingertips, causing pain and the sudden arrest of inspiration (Murphy’s sign).
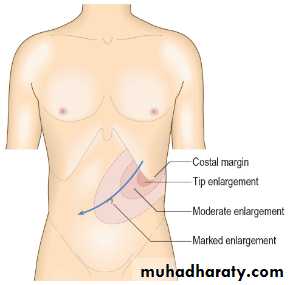
3-Splenomegaly
1-Place your hand over the umbilicus. Keep your hand stationary and ask the patient to breathe in deeply through the mouth. Feel for the splenic edge as it descends on inspiration.Move your hand diagonally upwards towards the left hypochondrium 1 cm at a time between each breath the patient takes.
Feel the costal margin along its length, as the position of the spleen tip is variable.
2-If you cannot feel the splenic edge, ask the patient to roll towards you and on to his right side, placing your left hand behind the patient’s left lower ribs, pulling the ribcage forward and repeat the above (Palpate with your right hand).
3-Feel along the left costal margin and percuss over the lateral chest wall to confirm or exclude the presence of splenic dullness. (usually on 9th, 10th, & 11th rib)
4-Kidney
1-Palpate in the right and left lower quadrant
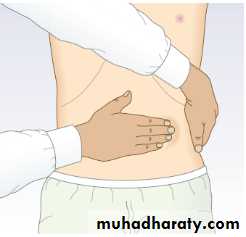
2-To detect lesser degrees of kidney enlargement; place your left hand behind the patient’s back below the lower ribs and your right hand anteriorly over the upper quadrant just lateral to the rectus muscle
Ask the patient to breathe in deeply; feel for the lower pole of the kidney moving down between your hands.
Push your hands together as the patient breathes out. If this happens, gently push the kidney back and forwards between your two hands to demonstrate its mobility. This is ballotting, and confirms that this structure is the kidney.
If the kidney is palpable, assess its size, surface and consistency.
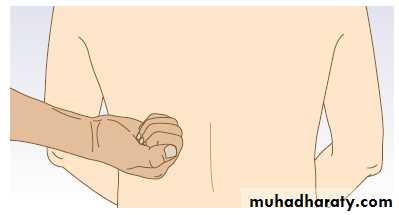
4-Ask the patient to sit up. Palpate the renal angle (between the spine and 12th rib posteriorly) firmly but gently. If this does not cause the patient discomfort, firmly (but with moderate force only) strike the renal angle once with the ulnar aspect of your closed fist after warning the patient what to expect and note any discomfort.
5-Bladder: Percuss for the bladder over a resonant area in the upper abdomen in the midline and then down towards the symphysis pubis. A change to a dull percussion note indicates the upper border of the bladder.
Auscultation
Bowel sounds: With the patient supine, place your stethoscope diaphragm to the right of the umbilicus and do not move it. Listen for up to 2 minutes before concluding that bowel sounds are absent.Arterial bruits: Listen above the umbilicus over the aorta for arterial bruits.
Renal artery stenosis bruit : 2–3 cm above and lateral to the umbilicus
Liver
Bruit: hepatocellular carcinoma, alcoholic hepatitis
Friction rub: perihepatitis
Spleen: Friction rub of perisplenitis
A succussion splash: It is a sound like a half-filled water bottle being shaken. Explain the procedure to the patient, then shake the patient’s abdomen by lifting him with both hands under his pelvis.If positive 4 hours after drinking or eating indicates delayed empying.
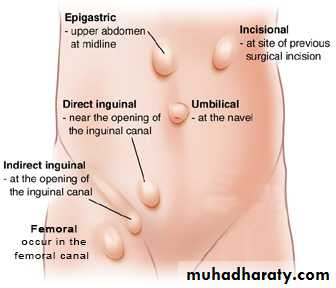
Hernias
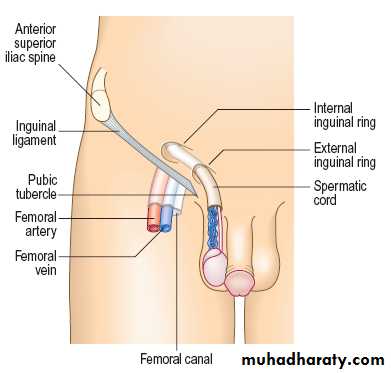
Examine the groin with the patient standing upright.Inspect the inguinal and femoral canals and the scrotum for any lumps or bulges.
■ Ask the patient to cough; look for an impulse over the femoral or inguinal canals and scrotum.
■ Identify the anatomical relationships between the bulge, the pubic tubercle and the inguinal ligament to distinguish a femoral from an inguinal hernia.
■ Palpate the external inguinal ring and along the inguinal canal for possible muscle defects. Ask the patient to cough and feel for a cough impulse.
■ now ask the patient to lie down and establish whether the hernia reduces spontaneously.
■If so, press two fingers over the internal inguinal ring at the mid-inguinal point and ask the patient to cough or stand up while you maintain pressure over the internal inguinal ring. If
the hernia reappears, it is a direct hernia. If it can be prevented from reappearing, it is an indirect inguinal hernia.
■ Examine the opposite side to exclude the possibility of asymptomatic hernias.