1
Neurology sessions
Part1: History
Symptoms ;suggesting or indicating a neurological problem ,that should be
thoroughly evaluated in "History of present illness" especially regarding their onset
and course are the followings:
Motor symptoms whether negative; weakness or paralysis or positive i.e. involuntary
movements.
Sensory symptoms; negative or positive. Disturbed level of consciousness or coma.
Pain like headache or neuropathic pain.
Episodic symptoms like vertigo, dizziness, fainting…etc.
Other symptoms which may or may not be neurological in origin; problems of
speech, swallowing, sphincter function, vision, hearing and smell.
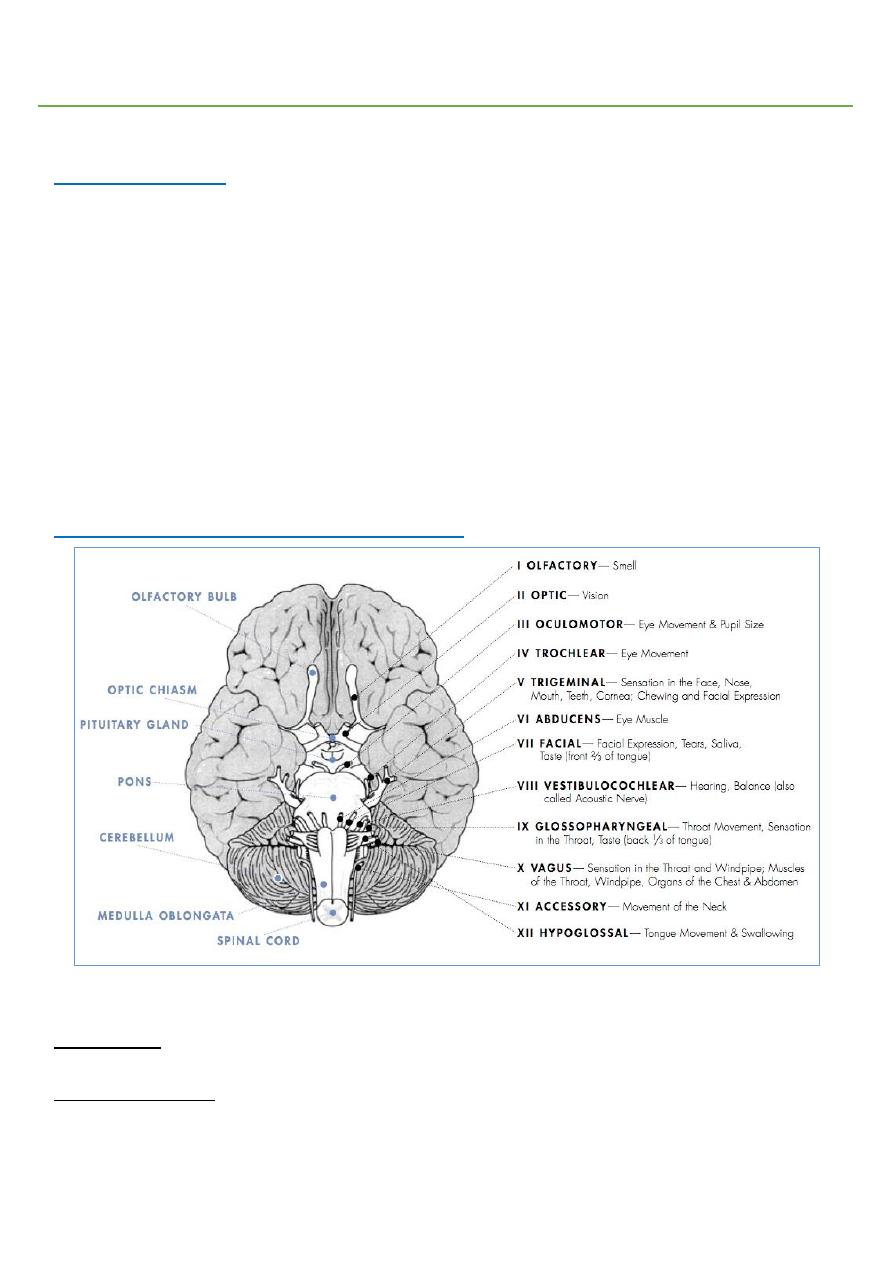
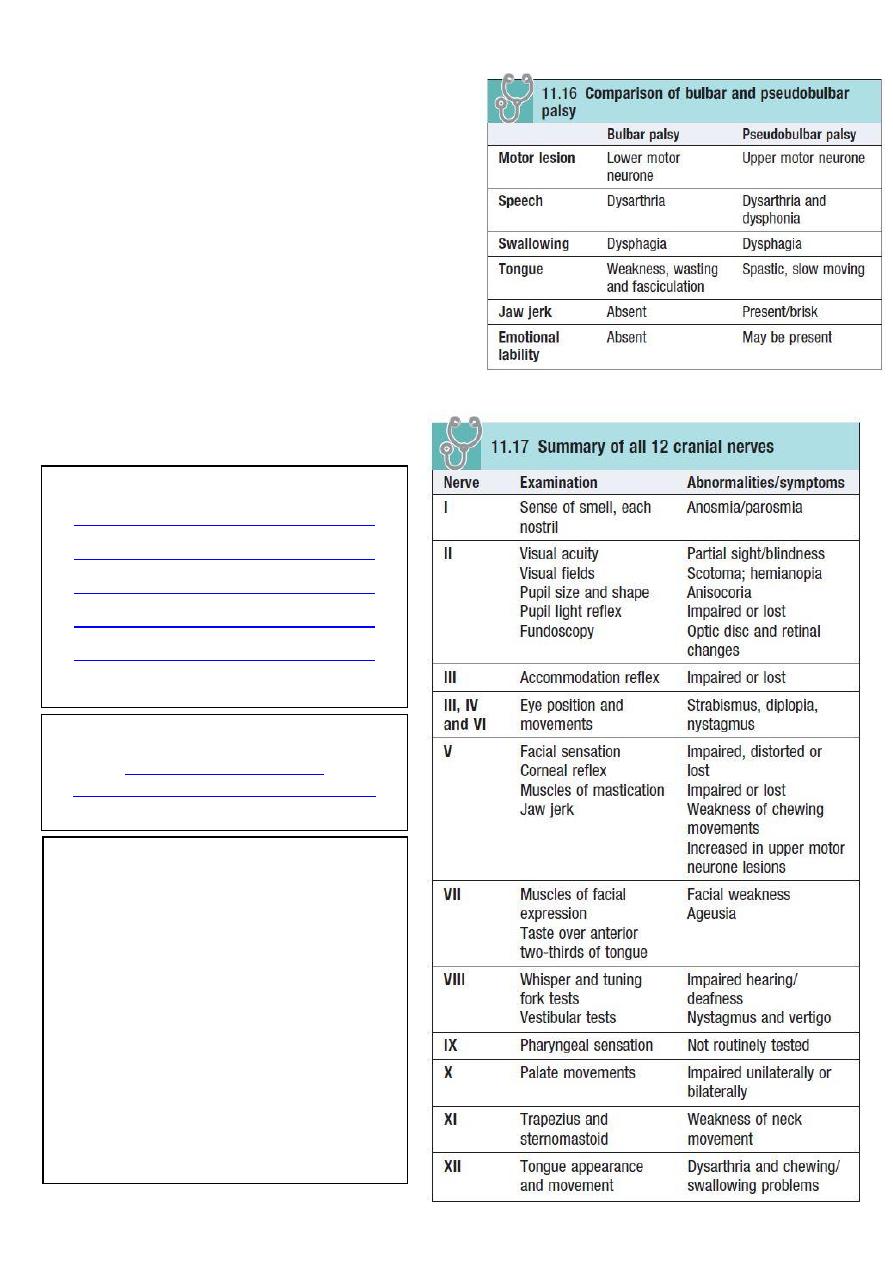
Part2: Cranial nerve examination
#Examination of olfactory nerve (1
st
CN):
Information:
It is pure sensory nerve.
Examination steps:
• Explain to patient, close eyes, examine each nostril alone, use familiar not irritating
odors.
2
• Smell is tested in each nostril separately by placing stimuli under one nostril and
occluding the opposing nostril. The stimuli used should be non-irritating and
identifiable. Some example stimuli include cinnamon, cloves, and toothpaste.
• Bedside testing of smell (limited clinical value).
• 'scratch and sniff' test cards.
• University of Pennsylvania Smell Identification Test (UPSIT).
Findings:
• Hyposmia or anosmia (reduction or loss of the sense of smell) may result from ear,
nose and throat disease, damage to the olfactory filaments after head injury or local
compression or invasion by basal skull tumors.
• Parosmia (is when pleasant odours are perceived as unpleasant) may occur with
head trauma, sinus infection or as an adverse effect of drugs.
• Olfactory hallucinations may occur in Alzheimer’s disease and temporal lobe
epilepsy and psychological problems.
• Bilateral loss can occur with rhinitis, smoking, or aging.
• Unilateral loss indicates a possible nerve lesion or deviated septum.
• Most common cause of anosmia is head injury which may lead to fracture of cribriform
plate and injury to the olfactory nerve.
#Examination of optic nerve (2
nd
CN):
Information:
It is pure sensory nerve.
The visual pathway:
• Consists of the retina, optic chiasm, optic tracts, lateral geniculate bodies, optic
radiations and visual cortex.
Examination steps:
• Examine each eye alone.
• Visual acuity: use Snellen chart, 6 meters from the patient.
• Visual field:
o Stand 50 cm in front of the patient and at the same level.
o Ask the patient to look directly and fix his eyes into your eyes.
o Cover non-tested eyes.
o Use small object (or index finger) and place it half distance between you and the
patient and beyond limits of field of vision.
o Advance the object (while moving) from outwards inwards.
o Test the four quadrants (upper nasal, lower nasal, upper temporal, and lower
temporal).
o Repeat for the other eye.
• Pupillary reflex:
o Shine a bright light obliquely into each pupil in turn.
o Look for the change of pupil size in the same eye (direct reflex).
o Record pupil size and any asymmetry or irregularity.
• The swinging flashlight test:
o Involves moving the light between the two pupils.
3
o Normally both direct and consensual responses are elicited when the light shines on
an eye, and some dilation will occur during the swing between.
• Color vision: is tested using Ishihara plates which identify patients who are color blind.
• Fundoscopy: should be performed on both eyes.
Findings:
• Peripheral retinal lesions spare central vision, causing localized scotomas.
• Optic nerve lesions central scotomas, blindness.
• Optic chiasm lesions bilateral temporal visual field defects (Bitemporal hemianopia).
• Optic tract lesions asymmetrical homonymous visual field defects.
• Optic radiations and occipital cortex lesions symmetrical visual field defects
(homonymous hemianopia).
Note:
• Scotoma is problem in the optic nerve, there is area of visual field defect surrounded
by normal visual field.
• Pupillary or light reflex afferent (optic nerve), efferent (oculomotor nerve).
• Normal size of pupil at rest is 3-5 mm.
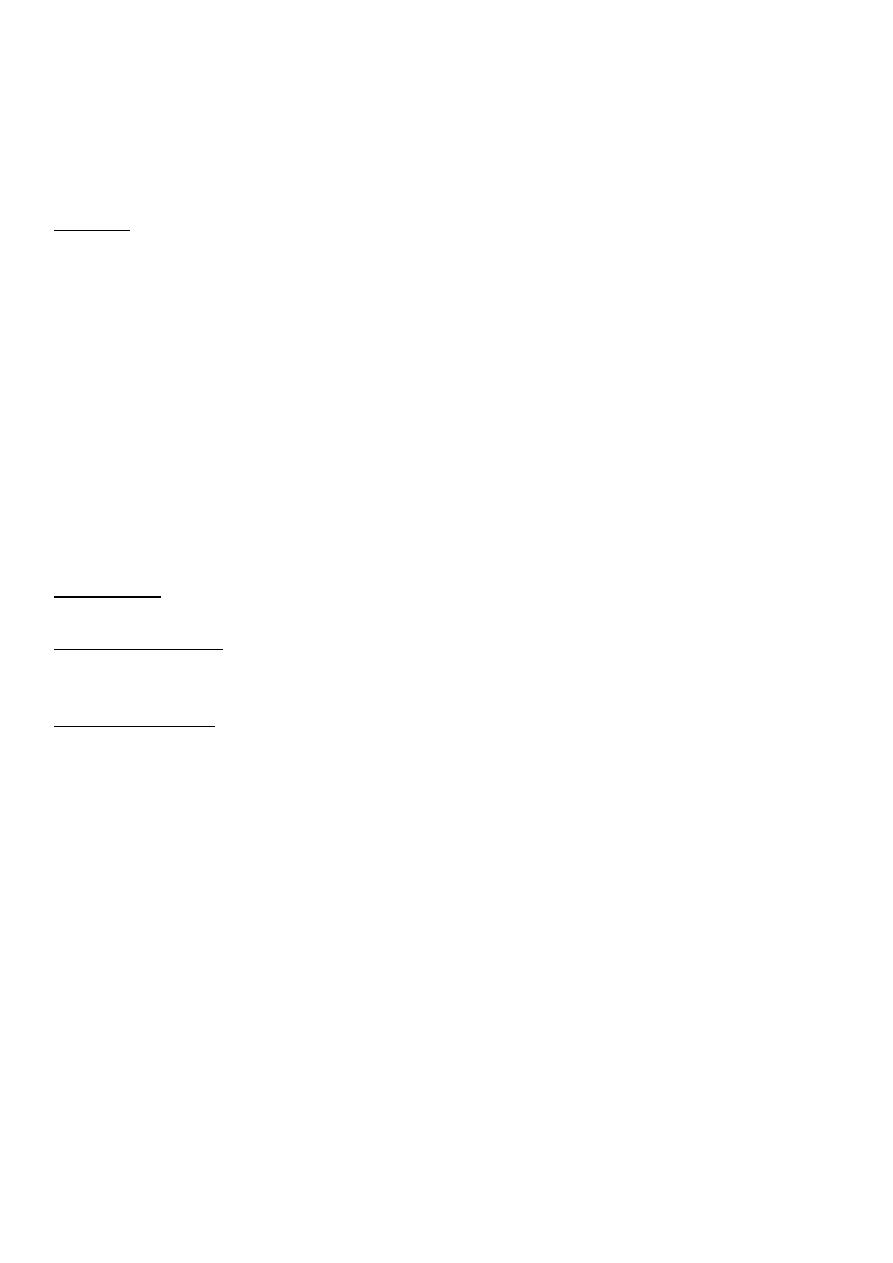
#Examination of Oculomotor, trochlear and abducent nerves (3, 4, 6
CN):
Movement of Eyeball controlled by 6 muscles:
• Superior rectus muscle moves eye upward innervated by 3 CN
• Inferior rectus muscle moves eye downward innervated by 3 CN
• Medial rectus muscle moves eye inward toward the nose innervated by 3 CN
• Lateral rectus muscle moves eye outward innervated by 6 CN
• Superior oblique muscle rotates the eye inward + move it downward innervated
by 4 CN
• Inferior oblique muscle rotates the eye outward + move it upward innervated by
3 CN
Function of 3rd CN:
• Elevation of eyelid (levator palpebrae superioris).
• Control eyeball movement.
• Control pupil by parasympathetic innervation.
• Provide preganglionic parasympathetics to the ciliary ganglion.
4
Examination steps:
• You should examine both eyes together.
• First, inspect for ptosis, eye position and nystagmus.
• The pupil size is measured, its shape and any asymmetry is tested.
• Examine the reflexes:
o Convergence reflex: far to near vision.
o Accommodation reflex: far and near and it is Convergence and slight constriction of
pupil.
o Light reflex: shine light, there is direct and indirect reflex, not put the torch in front
of patient eye.
• A commonly used abbreviation to describe normal pupils is PERRLA (pupils equal,
round and reactive to light and accommodation).
• The examiner tests ocular movements by standing one meter in front of the patient
and asking the patient to follow a target with eyes only, and not the head. The target is
moved in an "H" shape and the patient is asked to report any diplopia.
• Then, the target is held at the lateral ends of the patient's visual field. Nystagmus is
tested for. One or two beats is a normal finding.
• The accommodation reflex is tested by moving the target towards the patient's nose.
As the eyes converge, the pupils should constrict.
• The optokinetic nystagmus test is optional and involves asking the patient to look at a
moving strip of horizontal lines. Nystagmus is normally observed.
• Look for ptosis, Squint, Nystagmus, Pupillary reflex.
Findings:
• Ocuulomotor palsy: complete ptosis, divergent squint, normal or dilated pupil.
• Abducent palsy: convergent squint, diplopia. ((causes of palsy = D.M or trauma)).
• Trochlear palsy: diplopia when reading, writing, descending down stairs.
Note:
• Corneal touch afferent (trigeminal nerve), efferent (facial nerve).
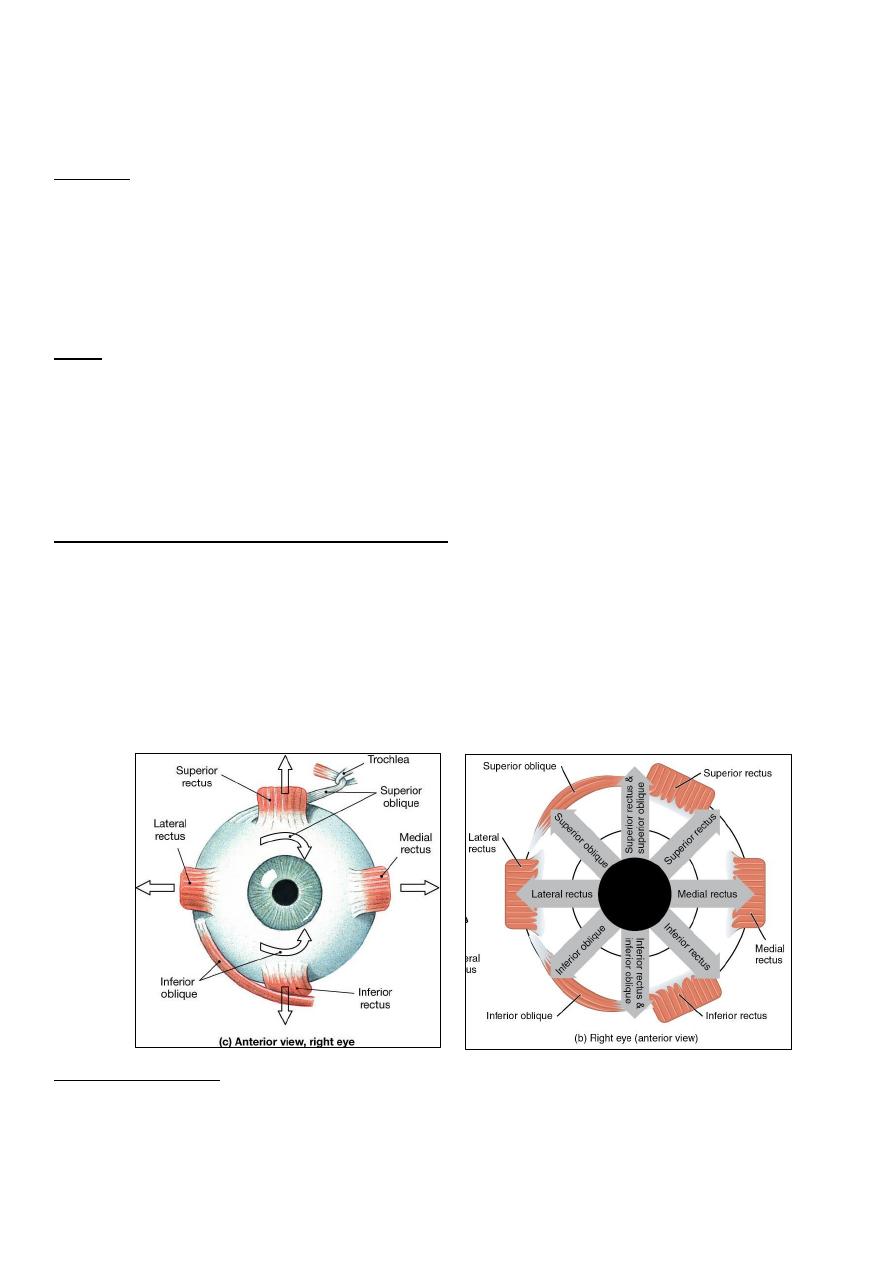
#Examination of Trigeminal nerve (5
th
CN):
Information:
• The V nerve provides sensation to the face, mouth
and part of the dura, and motor supply to the
muscles of mastication (temporalis, masseter, medial
and lateral pterygoid).
• There are three major branches of the nerve:
o Ophthalmic (V1): sensory.
o Maxillary (V2): sensory.
o Mandibular (V3): sensory and motor.
Examination steps:
• Sensory:
o Ask the patient to close his eyes and say 'yes' each time he feels you lightly touch
them using a cotton wool tip. Do this in the areas of V1, V2 and V3.
o Repeat using a fresh neurological pin, e.g. Neurotip, to test superficial pain.
5
o 'Nasal tickle' test: use a wisp of cotton wool to 'tickle' the inside of each nostril and
ask the patient to compare: it is an unpleasant sensation easily appreciated by the
patient.
• Motor:
o Inspect for wasting of the muscles of mastication (most apparent in temporalis).
o Ask the patient to clench his teeth; feel the masseters, estimating their bulk.
o Place your hand under the jaw to provide resistance; ask the patient to open his jaw.
Note any deviation of mandible.
• Corneal reflex:
o Explain to the patient what you are going to do, and ask him to remove contact
lenses, if relevant.
o Gently depress the lower eyelid while the patient looks upwards.
o Lightly touch the lateral edge of the cornea with a wisp of damp cotton wool.
o Look for both direct and consensual blinking.
o Ask the patient to let his mouth hang loosely open.
o Place your forefinger in the midline between lower lip and chin.
o Percuss your finger gently with the tendon hammer in a downwards direction,
noting any reflex closing of the jaw. An absent, or just present, reflex is normal.
Findings:
• Trigeminal neuralgia sensory symptoms include facial numbness and pain due to
neurovascular compression.
• Unilateral loss of sensation may result from direct injury in association with facial
fractures or local invasion by cancer.
• Lesions in the cavernous sinus cause loss of the corneal reflex and V1 or V2
cutaneous sensory loss.
• Reactivation of herpes varicella zoster virus (chickenpox) can affect any sensory
nerve, but typically either a thoracic dermatome or V1.
• Clinically significant weakness of the muscles of mastication may occur in
myasthenia, with fatigable chewing.
• Brisk jaw jerk occurs in pseudobulbar palsy.
#Examination of Facial nerve (7
th
CN):
Functions of facial nerve:
• Supply the muscles of facial expression (sensory and motor).
• Carry parasympathetic secretomotor fibers to the lacrimal, submandibular and
sublingual salivary glands (via nervus intermedius).
• Receive taste sensation from the anterior two-thirds of the tongue.
• Provides the efferent supply to several reflexes.
Examination steps:
• Motor function:
o Inspect the face for asymmetry or differences in blinking or eye closure on one side.
Note that minor facial asymmetry is common and rarely pathological.
6
o Raise both eyebrows ask the patient to raise the eyebrows and observe for
symmetrical wrinkling of the forehead. Then Frown.
o Test power by saying: 'Screw your eyes tightly shut and stop me from opening them,'
then 'Blow out your cheeks with your mouth closed'.
o Show both upper and lower teeth, Smile, Puff out both cheeks.
o Demonstrate baring your teeth and ask the patient to mimic you. Look for
asymmetry.
o Note any: lag, weakness, asymmetry, deviation, unilateral or bilateral, upper or
lower motor neuron lesion, emotional or voluntary problem.
• Sensory function: test for taste.
Steps from doctor:
• Ask the patient to elevate eyebrows (frontalis muscle).
• Orbicularis oculi exam.
• Nasolabial fold at rest.
• Nasolabial fold at contraction.
• Open mouth and protrude tongue.
• Close mouth and keep air (orbicularis oris) air leaking is due to weakness.
• Protrude the lips.
Steps form another doctor:
• Orbicularis oculi close eye forcefully.
• Orbicularis oris put pen between your upper lip and nose.
• Buccenator blow your check and keep air inside your mouth.
• Labial muscles show me your teeth.
• Frontalis muscle elevate your eyebrow (wrinkles of forehead appear).
Findings:
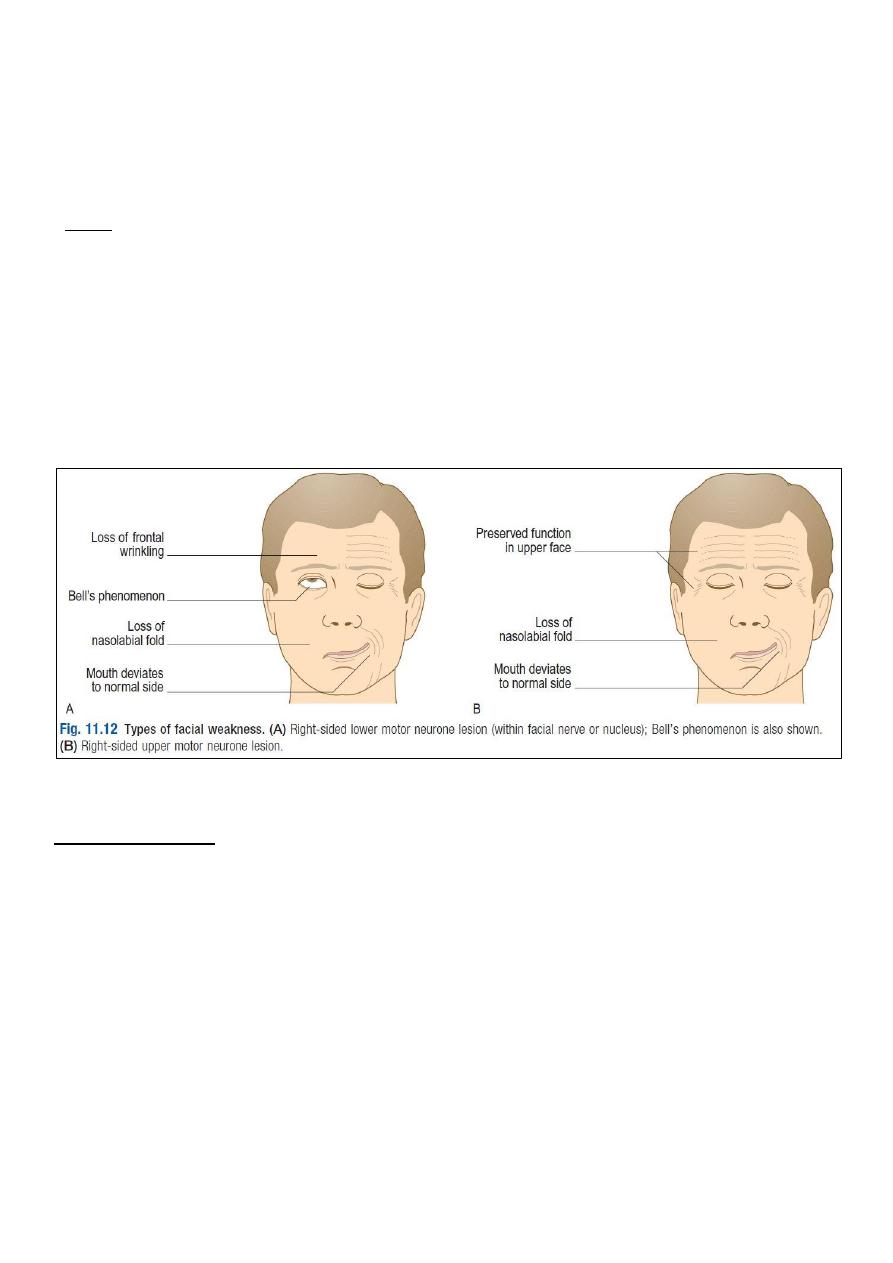
• Unilateral lower motor neuron VII nerve lesion there is weakness of both upper and
lower facial muscles.
• Bell’s palsy acute lower motor neuron VII nerve paralysis, preceded by mastoid pain,
impairment of taste and hyperacusis (high-pitched sounds appearing unpleasantly
louder than normal).
• Bell’s phenomenon occurs when the patient is unable to close his eye.
• Ramsay Hunt syndrome occurs in herpes zoster infection of the geniculate (facial)
ganglion, produces a severe lower motor neuron facial palsy, ipsilateral loss of taste
and buccal ulceration, and a painful vesicular eruption in the external auditory meatus.
• Other causes of a lower motor neuron VII lesion include cerebellopontine angle
tumors, e.g. acoustic neuroma, trauma and parotid tumors.
• Synkinesis most commonly twitching of the corner of the mouth on ipsilateral
blinking, may be seen in recovering lower motor neuron VII lesions.
• Unilateral VII nerve upper motor neuron lesions weakness is marked in the lower
facial muscles with relative sparing of the upper face, the Nasolabial fold may be
flattened and the corner of the mouth droop, but eye closure is usually preserved.
• Bilateral facial palsies occur in Guillain–Barré syndrome, sarcoidosis, Lyme disease
and HIV infection.
• Emotional facial nerve palsy deviation of mouth after smiling.
7
• Upper motor neuron lesion (above facial nerve nucleus) mild weakness, mild
deviation of the mouth, no Bell's phenomenon.
• Lower motor neuron lesion (below facial nerve nucleus) severe weakness, more
deviation of the mouth, there is Bell's phenomenon.
• Causes of bilateral facial nerve palsy: sarcoidosis, myasthenia gravis, leprosy, peripheral
neuropathy, guillian barre syndrome.
Note:
• The lower part of the face is affected by unilateral lesion of upper motor neuron of one
side only (not like other CN lesions).
• Any cranial nerve has 2 supply in upper motor neuron so any cranial nerve palsy is
definitely lower motor lesion, except for facial nerve.
• Upper motor neuron facial nerve palsy spares the upper part of face.
• Lower motor neuron facial nerve palsy affect upper and lower parts of face.
• 90% of stroke patients have hemiplasia with upper motor facial palsy in same side.
• Anterior 2/3 of tongue sensation by corda tendeni nerve which run with facial
nerve.
#Examination of vestibulocochlear nerve (8
th
CN):
Examination steps:
• Vestibular function:
o From history: vertigo.
o From exanimation: ataxic gait, nystagmus, dysarthria, tinnitus.
• Cochlear function (Hearing):
o Whisper numbers in one ear as patient covers the other and ask the patient to
repeat the numbers.
o Alternatively, have patient close their eyes and say "left" or "right" depending on the
side from which they hear the sound.
o Vigorously rub fingers together in one ear at a time to produce rustling sound.
o Conduct the Rinne test and Weber test.
• Weber’s test:
o Hit the prongs of the fork against a padded surface to make it vibrate.
o Place the base of the vibrating tuning fork in the middle of the patient's forehead.
8
o Ask: 'Where do you hear the sound?’
o Record which side Weber's test lateralizes to if not central.
• Rinne’s test:
o Place the vibrating prongs at the patient's external auditory meatus; ask if he can
hear it.
o Now place the still-vibrating base on the mastoid process.
o Ask: 'Is it louder in front, or behind your ear?’
Findings:
• Deafness :impairment of hearing is two type:
• Conductive deafness: impairment of the physical structures that conduct the sound
itself into cochlea is destroyed (external auditory meatus, tympanic membrane, middle
ear cavity, ossicles).
• Sensorineural deafness: impairment of cochlea or the auditory nerve (infection, toxin).
• If either the cochlea or the auditory nerve is completely destroyed, the person is
permanently deaf.
• Weber’s test:
o Normally Subject hears equally on both sides.
o In conductive deafness (one ear) the sound of the vibrating tuning fork is louder
in diseased ear because masking effect of environmental noise is absent on diseased
side.
o In nerve deafness (one ear) sound louder in normal ear.
• Rinne’s test:
o Normally The subject hears vibrating of the tuning fork in air after bone
conduction is over (air conduction > bone conduction).
o In conductive deafness (one ear) patient does not hear vibration in air after bone
conduction is over.
o In nerve deafness (one ear) patient hears vibration in air after bone conduction is
over.
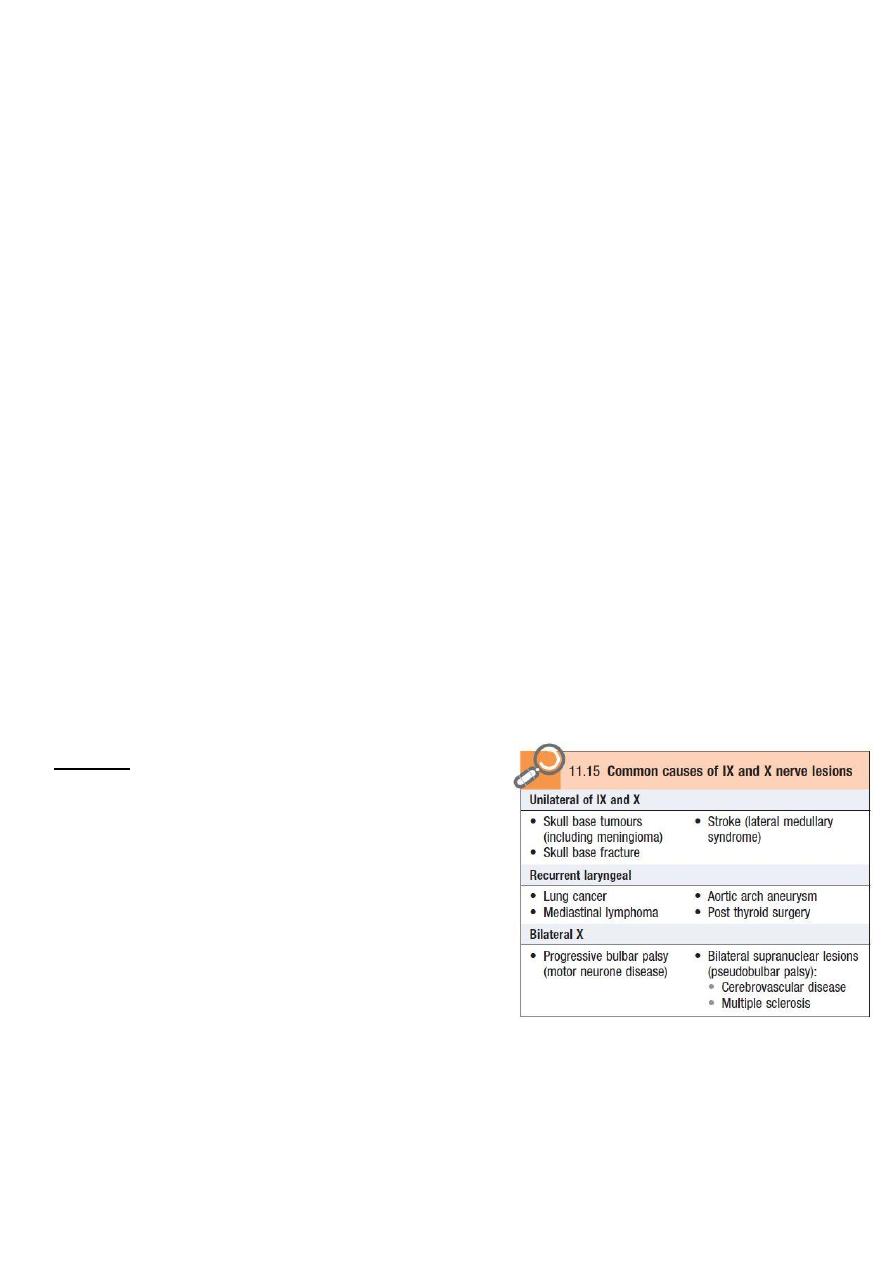
#Examination of Glossopharyngeal and vagus nerves (9, 10 CN):
Information:
• The glossopharyngeal (IX) nerve mainly carries sensation from the pharynx and
tonsils, and sensation and taste from the posterior one-third of the tongue.
• The vagus (X) nerve carries important sensory information but also innervates upper
pharyngeal and laryngeal muscles.
• The main functions of IX and X are swallowing, phonation/articulation and sensation
from the pharynx/larynx.
Examination steps:
• Speech examination:
o Exam for: comprehension, expression, reading, writing, repletion, naming.
o Look for: dysarthria or dysphonia
• Ala test (Visualizing uvula deviation):
9
o Ask him to say 'Ah'; look at the movements of the palate and uvula using a torch.
Normally, both sides of the palate elevate symmetrically and the uvula remains in
the midline.
o Uvula deviated to the right side left abnormality.
o Uvula deviated to the left side right abnormality.
o Uvula not elevated right and left abnormality.
• Swallowing:
o Administer 3 teaspoons of water and observe for absent swallow, cough or delayed
cough, or change in voice quality after each teaspoon.
o If there are no problems, watch for the same reactions while the patient swallows a
glass of water.
o In bulbar palsy there is dysphagia to fluids (more than solid).
• Air leaking:
o Ask the patient to puff out his cheeks with the lips tightly closed.
o Listen for air escaping from the nose.
o For the cheeks to puff out, the palate must elevate and occlude the nasopharynx.
o If palatal movement is weak, air will escape audibly through the nose.
• Cough: ask the patient to cough; assess the strength of the cough.
• Gag reflex:
o Is a reflex contraction of the back of the throat.
o Evoked by touching the roof of the mouth, the back of the tongue, the area around
the tonsils and the back of the throat.
o Touch lead t vomiting.
• Testing pharyngeal sensation:
o Divide the tongue depress into small and large halves, depress the tongue by the
large half, then touch the pharyngeal wall by the small half.
o Findings: hypoesthesia, loss of sensation.
Findings:
• Isolated unilateral IX nerve lesions are rare.
• Unilateral X nerve damage leads to
ipsilateral reduced elevation of the soft palate,
which may cause deviation of the uvula (away
from the side of the lesion) when the patient
says ‘Ah’.
• Damage to the recurrent laryngeal branch of
the X nerve due to lung cancer, thyroid surgery,
mediastinal tumors and aortic arch aneurysm
causes dysphonia and a ‘bovine’ cough.
• Bilateral X nerve lesions cause dysphagia and dysarthria.
• Less severe cases can result in nasal regurgitation of fluids and nasal air escape when
the cheeks are puffed out.
10
#Examination of Accessory nerves (11
th
CN):
Information:
• Provides fibers to the upper trapezius and the sternocleidomastoid muscles
responsible for elevating (shrugging) the shoulders, and head turning/flexing.
Examination steps:
• Face the patient and inspect the sternocleidomastoid muscles for wasting or
hypertrophy; palpate them to assess their bulk.
• Stand behind the patient to inspect the trapezius muscle for wasting or asymmetry.
• Ask the patient to shrug the shoulders, then apply downward pressure with your hands
to assess the power.
• Test power in the left sternocleidomastoid by asking the patient to turn the head to the
right while you provide resistance with your hand placed on the right side of the
patient's chin.
• Reverse the procedure to check the right sternocleidomastoid.
Findings:
• Isolated XI nerve lesions are uncommon but the nerve may be damaged during
surgery in the posterior triangle of the neck, penetrating injuries or local invasion by
tumor.
• Wasting of the upper fibers of trapezius may be associated with displacement of the
upper vertebral border of the scapula away from the spine, while the lower border is
displaced towards it.
• Wasting and weakness of the sternocleidomastoids are characteristic of myotonic
dystrophy, and head drop may be seen in myasthenia, motor neuron disease and some
myopathies.
#Examination of Hypoglossal (12
th
CN):
Examination steps:
• Ask the patient to open his mouth. Look at the tongue at rest for wasting, fasciculation
or involuntary movement.
• Ask the patient to put out his tongue. Look for deviation or involuntary movement.
• Ask the patient to move the tongue quickly from side to side.
• Test power by asking the patient to press the tongue against the inside of each cheek
in turn while you press from the outside with your finger.
• Assess speech by asking the patient to say 'yellow lorry'.
• Assess swallowing with a water swallow test.
Findings:
• Unilateral lower motor XII nerve lesions lead to tongue wasting on the affected side
and deviation to that side on protrusion.
• Bilateral lower motor neuron damage results in global wasting, the tongue lies thin
and shrunken and fasciculation may be evident.
• Unilateral upper motor XII nerve lesions are uncommon.
• Bilateral upper motor XII nerve lesions lead to a tongue with increased tone
(spastic), and the patient has difficulty flicking the tongue from side to side.
11
• Tremor of the resting or protruded tongue
may occur in Parkinson’s disease,
although jaw tremor is more common.
• Other orolingual dyskinesias are often
drug-induced, e.g. tardive dyskinesias due
to neuroleptics.
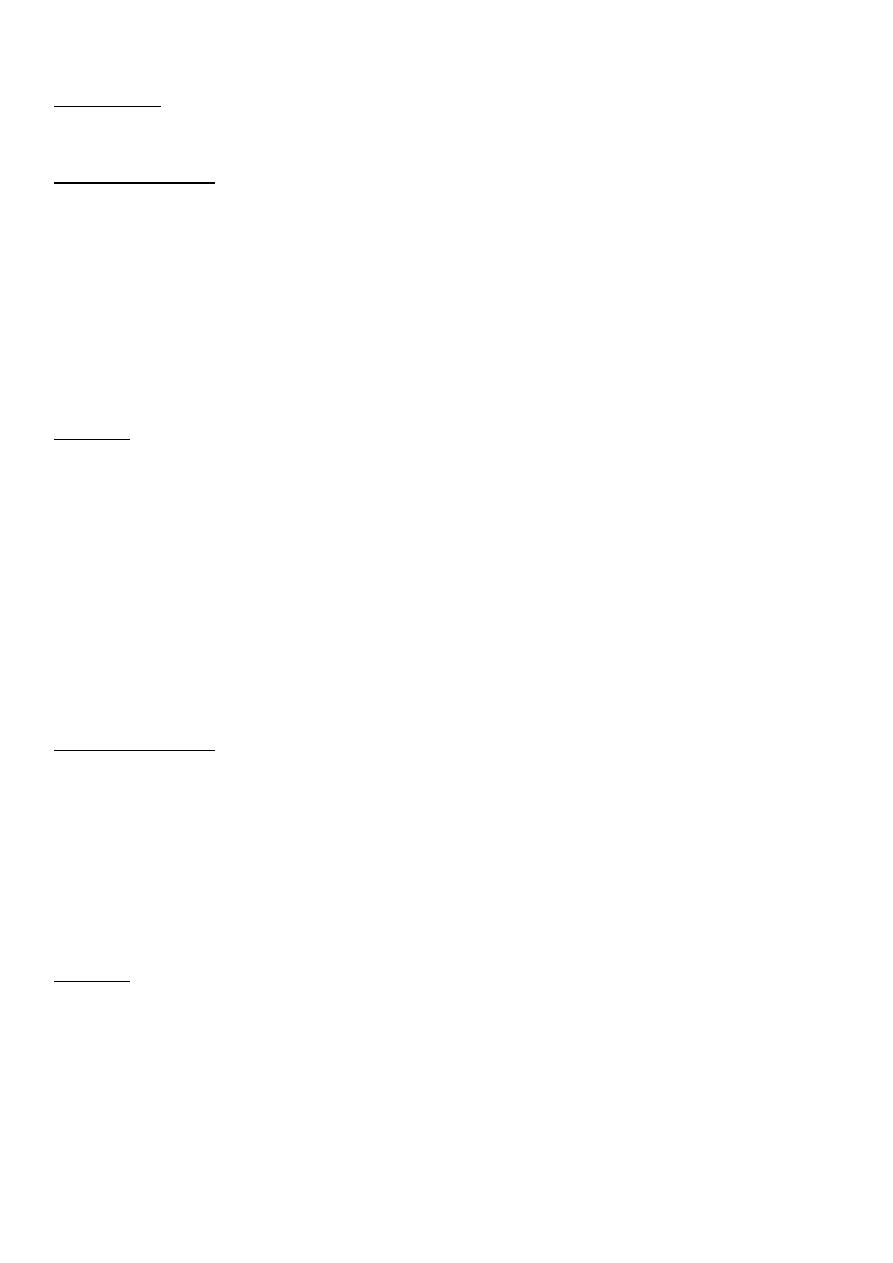
• Bilateral upper motor lesions of IX–XII
nerves may also affect the V and VII, and
are called pseudobulbar palsy (hot potato
speech, exaggerated gag reflex).
• Bilateral lower motor lesions of IX–XII
nerves are called bulbar palsy (nasal
speech, absent gag reflex).
Videos for cranial nerves examination:
http://www.muhadharaty.com/lecture/1178
http://www.muhadharaty.com/lecture/1180
http://www.muhadharaty.com/lecture/1182
http://www.muhadharaty.com/lecture/1183
OSCE steps of cranial nerves examination:
Notes:
First and second cranial nerves are not
peripheral nerves and they represent an
extension of white matter.
Upper motor lesion cause mild weakness
because the nucleus in the upper motor has
double innervation, so if one damage the
other is still work, so lead to mild weakness,
but in the lower motor there is only single
innervation so produce severe weakness.
IN motor part of trigeminal and in hypoglossal
nerve the affected part is deviated to the
abnormal side, but other cranial nerves lesions
are deviated to the normal side.
12
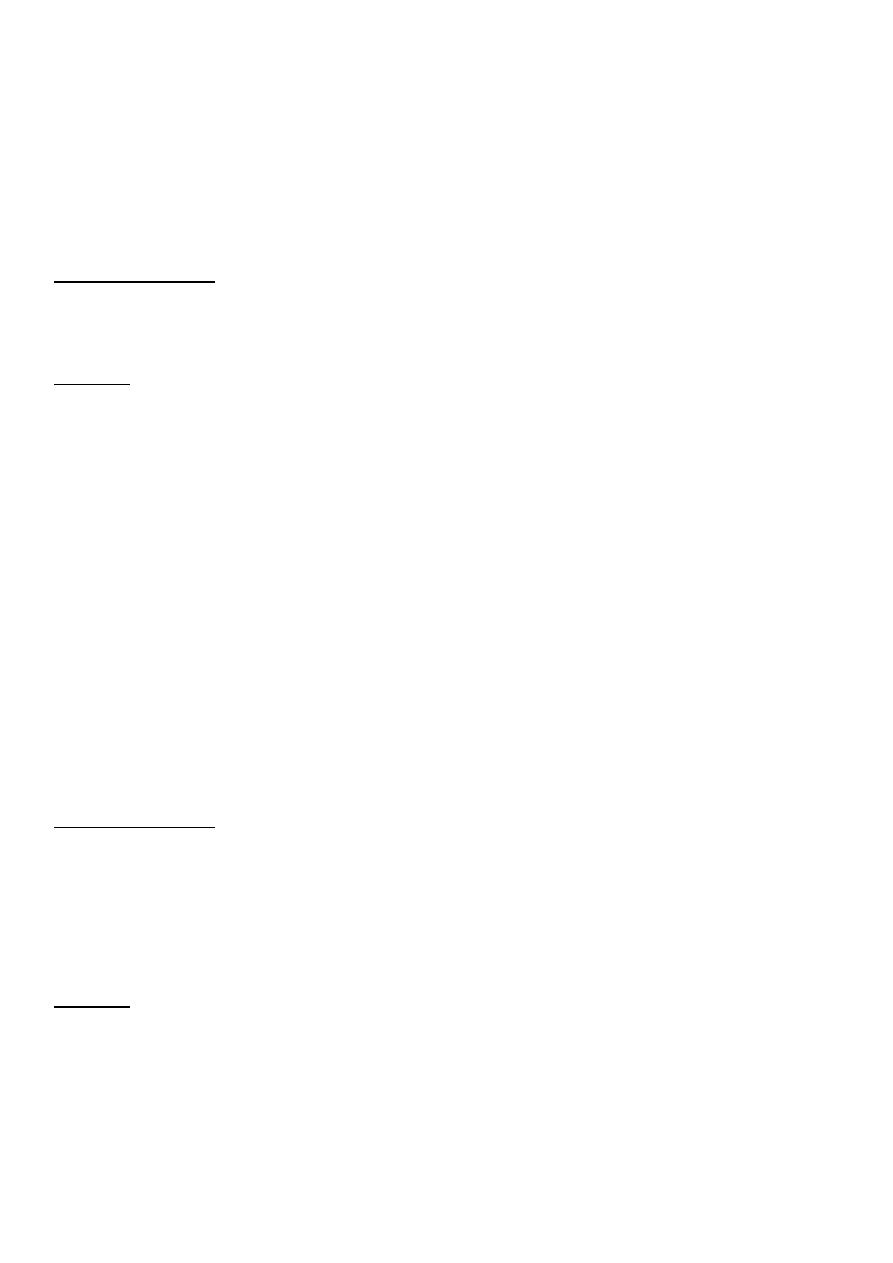
Part3: Motor system
• Inspection and palpation of muscles.
• Assessment of tone.
• Testing movement and power.
• Examination of reflexes.
• Testing coordination.
1- Inspection and palpation of the muscles:
Examination steps:
• Completely expose the patient while keeping the patient's comfort and dignity.
• Look for asymmetry, inspecting both proximally and distally.
• Note deformities, e.g. clawing of the hands or pes cavus.
• Examine for wasting or hypertrophy, fasciculation and involuntary movement.
• From video:
• http://www.muhadharaty.com/lecture/1193
• http://www.muhadharaty.com/lecture/1194
Findings:
• Muscle bulk:
o Distal atrophy in upper limbs small muscles of the hand, thinner, hypothinner.
o Proximal atrophy in upper limbs Biceps, triceps, shoulder.
o Distal atrophy in lower limbs Curve of foot exaggerated, atrophy of muscles of leg
and foot.
o Proximal atrophy in lower limbs gluteal, quadratus femoris, vastus medialis.
o Lower motor neuron lesions may cause muscle wasting.
o Disuse atrophy may develop with longstanding lesions.
o Pseudo-hypertrophy may occur in muscular dystrophy but the muscles are weak.
• Fasciculation:
o Fasciculation is irregular twitches under the skin overlying resting muscles (small
isolated muscle rippling.
o This occurs in lower motor neuron disease, usually in wasted muscles.
o Fasciculation is seen, not felt.
o Myokymia is rapid bursts of repetitive motor unit activity often occurring in an eyelid
or first dorsal interosseus, and is rarely pathological.
• Posture:
o Hemiplegic posture, spastic posture, frog like.
• Abnormal movements:
o Myoclonic jerks sudden shock-like contractions of one or more muscles, could be
normal or abnormal in epilepsy, diffuse brain damage, dementia.
o Tremor oscillatory movement about a joint or a group of joints, there are
Physiological tremor, Essential tremor, Rest tremor, Intention tremor, Isolated head
tremor, Functional tremor.
o Dystonia is caused by sustained muscle contractions, leading to twisting,
repetitive movements and sometimes tremor.
13
o Chorea describes brief, random, purposeless movements.
o Athetosis is a slower, writhing movement, more similar to dystonia than chorea.
o Ballism refers to violent flinging movements.
o Tics are repetitive, stereotyped movements.
• Contracture.
2- Assessment of tone:
Tone is resistance to passive movement around the joint when the patient is completely relaxed.
Examination steps:
• From video:
• http://www.muhadharaty.com/lecture/1193
• http://www.muhadharaty.com/lecture/1194
Findings:
• Hypotonia:
o Occur in lower motor neuron lesions and could occur in UMNL with neurogenic
shock which last from 2-6 months accourding to severity of disease (in brain last for
one week and in spinal cord last for 6 months).
o Associated with muscle wasting, weakness and hyporeflexia.
o Feature of cerebellar disease or in the early phases of cerebral or spinal shock.
• Hypertonia:
o Occur in upper motor neuron lesions, in pyramidal system diseases.
o Spasticity: Velocity-dependent resistance to passive movement. Accompanied by
weakness, hyperreflexia, an extensor plantar response, clonus.
o Rigidity: sustained resistance throughout the range of movement. It is extra-
pyramidal sign (Parkinson disease).
o Clonus: is a rhythmic series of contractions evoked by sudden stretch of the muscle
and tendon (more than 6 beats is abnormal.
3- Testing of power:
Examination steps:
• Exam distal and proximal in the upper and lower limbs.
• Exam these muscle: Deltoid, Biceps, Brachioradialis, Triceps, Gluteus maximus,
Hamstrings, Quadriceps, and other middle size muscles.
• From video:
• http://www.muhadharaty.com/lecture/1193
• http://www.muhadharaty.com/lecture/1194
Findings:
• Upper motor neuron lesions produce weakness of a relatively large group of
muscles, e.g. a limb or more than one limb.
• Lower motor neuron damage can cause paresis of an individual and specific muscle.
• Hoover’s sign is often present in functional leg weakness.
• Causes of muscle weakness:
o Lower motor neuron: Peripheral neuropathies, poliomyelitis, motor neuron disease.
o Upper motor neuron: Stroke, Spinal cord pathology, Multiple sclerosis, Brain tumor.
14
o Myopathies: Muscular dystrophies, inflammatory myopathies, Corticosteroids,
Alcohol.
o Functional weakness: Conversion disorders.
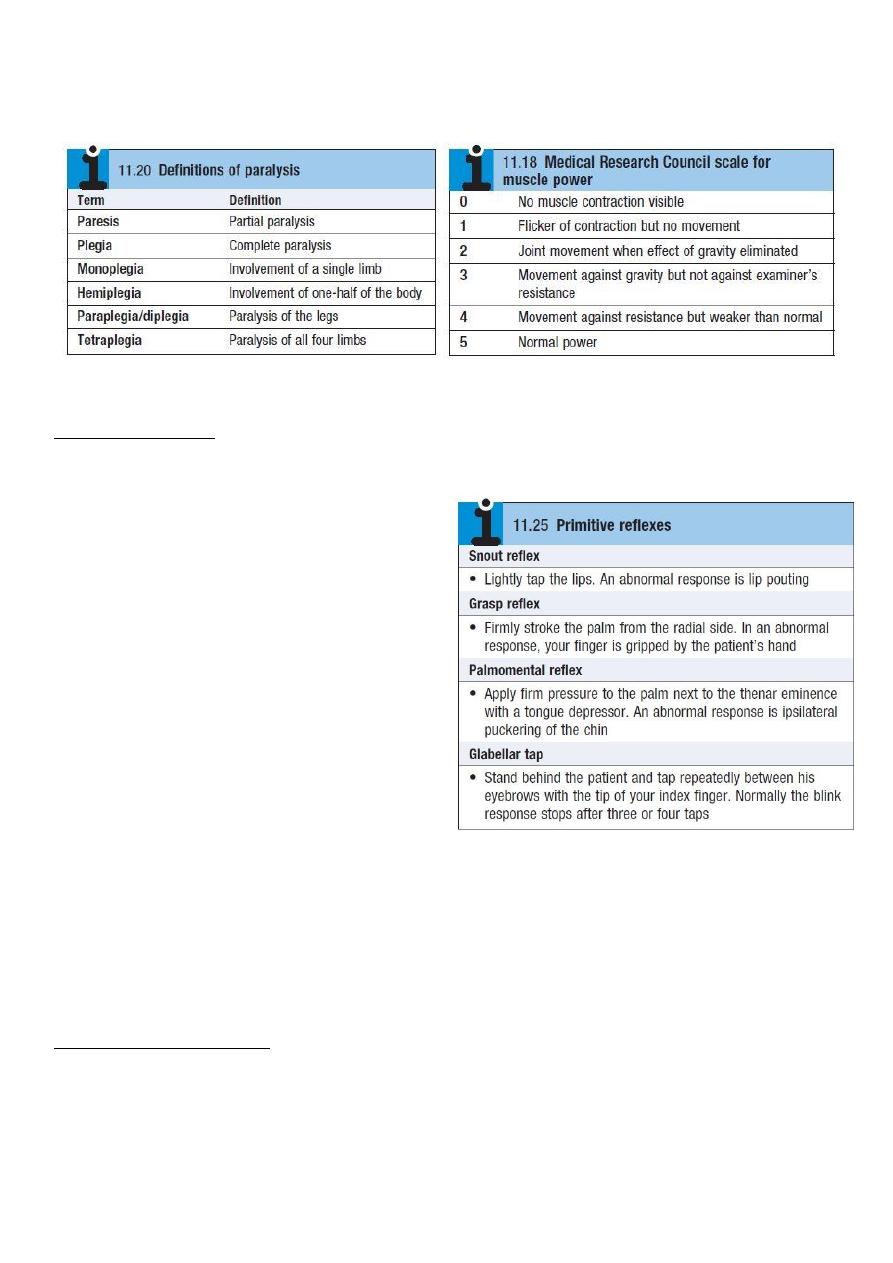
4- Examination of reflexes:
Examination steps:
• Record the response as: Increased (+++), Normal (++), Diminished (+), Present only with
reinforcement (+-), absent (-).
• Examine the following reflexes:
Deep reflexes:
o The brachioradialis reflex (C5,6)
o The triceps reflex (C6,7)
o The biceps reflex (C5,6)
o Hoffmann’s reflex
o Finger jerk
o The knee jerk reflex (L2, L3, L4)
o The ankle jerk reflex (S1, S2)
o The ankle clonus (S1, S2)
Superficial reflexes:
o Plantar response (S1–2)
o Abdominal reflexes (T8–12)
o Cremasteric reflex (L1–2): males only
Primitive reflexes:
o These are present in normal neonates and young infants but disappear as the
nervous system matures. People with congenital or hereditary cerebral lesions and a
few healthy individuals retain these reflexes.
• From video:
• http://www.muhadharaty.com/lecture/1193
• http://www.muhadharaty.com/lecture/1194
Information and findings:
• A tendon reflex is the involuntary contraction of a muscle in response to stretch.
• Hyperreflexia (abnormally brisk reflexes) (occur in anxiety) is a sign of upper motor
neuron damage.
• Diminished or absent (areflexia) jerks are most commonly due to lower motor neuron
lesions.
15
• Reflex patterns are helpful in localizing neurological lesions, but you should know the
nerve roots which serve the commonly tested reflexes Biceps (C5), Supinator
"brachioradialis" (C6), Triceps (C7), Knee "quadriceps" (L3, 4), Ankle "gastrocnemius,
soleus" (S1).
• An ‘inverted’ biceps reflex is caused by combined spinal cord and root pathology
localizing to a specific spinal level.
• Positive Hoffmann’s reflex (thumb flexion elicited by flicking the distal phalanx of the
middle finger) and finger jerks suggest hypertonia, but can occur in healthy individuals,
and are not useful signs in isolation.
• Extensor plantar or Babinski response is a sign of upper motor neuron damage.
• Superficial abdominal reflexes (T8–12) are lost in upper motor neuron lesions but are
also affected by lower motor neuron damage affecting T8–12. They are usually absent
in the obese, the elderly or after abdominal surgery.
• The cremasteric reflex in males (L1 and L2) is rarely elicited, but typically is lost in spinal
cord or root lesions.
• Jendrassik's maneuver: reinforcement when a reflex appears to be absent, for knee
and ankle reflexes.
5- Testing coordination:
Information:
• Performing complex movements smoothly and efficiently depends upon intact sensory
and motor function and an intact cerebellum.
• Right upper limb coordinate by right upper half of cerebellum.
• Left upper limb coordinate by left upper half of cerebellum.
• Right lower limb coordinate by right lower half of cerebellum.
• Left lower limb coordinate by left lower half of cerebellum.
• Trunk is coordinate by vermis. ((ataxic gait due to vermis lesion))
• Cerebellar lesion (at the same side) but cerebral lesion (at the opposite side).
• Function of cerebellum is coordination of movements and maintaining muscle tone.
Examination steps:
• Check coordination of upper limbs: by Finger-to-nose test.
• Check coordination of lower limbs: Heel-to-shin test.
• Check coordination of trunk: ataxic gait.
• Check coordination of the tongue: dysdiadochokinesis.
• Check coordination of the speech: slow slurred speech.
• Check coordination of the eye: nystagmus.
• Check Rebound phenomenon.
• Rapid alternating movements.
• Check the tone: hypotonia and hyporeflexia is abnormal.
• From video:
• http://www.muhadharaty.com/lecture/1193
• http://www.muhadharaty.com/lecture/1194
16
Findings:
• Dysmetria or past-pointing finger-to-nose test may reveal a tendency to fall short or
overshoot the examiner’s finger.
• intention tremor tremor of the finger as it approaches the target finger and the
patient’s own nose.
• Dyssynergia slow, disjointed and clumsy movement.
• Dysdiadochokinesis impairment of rapid alternating movements (slowness,
disorganization and irregularity of movement).
• Dysarthria and nystagmus also occur with cerebellar disease.
• Truncal ataxia in disorders predominantly affecting midline cerebellar structures,
e.g. tumors of the vermis and alcoholic cerebellar damage.
• Other signs of cerebellar disease rebound phenomenon, pendular reflexes,
hypotonia, Tandem gait (heel–toe walking).
• Dyspraxia or apraxia is difficulty or inability to perform a task, despite no
impairment of the necessary individual functions (higher cortical dysfunction).
• Weakness may produce false positive finger-to-nose or heel-to-shin tests, so
demonstrate that power is normal first.
Acquired and genetic causes of ataxia:
• Toxic: phenytoin, alcohol, heavy metals.
• Vascular: Stroke (ischemic or hemorrhagic).
• Neoplastic: Metastases, Primary brain tumors.
• Inflammatory: multiple sclerosis, Sarcoidosis.
• Infective/transmissible: mumps, herpes zoster, HIV, syphilis.
• Degenerative: Multiple system atrophy.
• Structural and traumatic: Traumatic brain injury.
• Metabolic, nutritional: Hypothyroidism, Vitamin B1, B12 or E deficiency.
• Genetic: Friedreich’s ataxia, Spinocerebellar ataxias, Episodic ataxias.
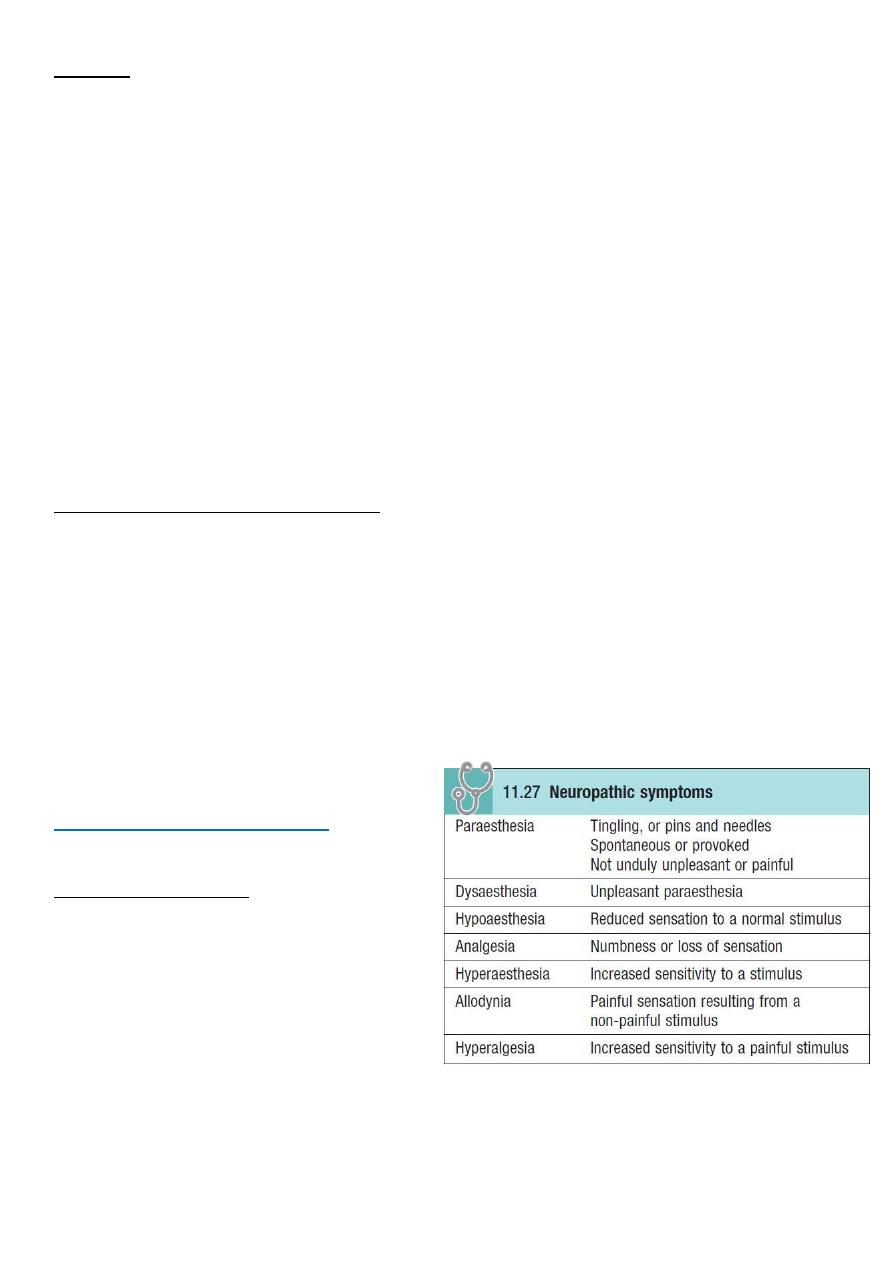
Part4: Sensory system
Examine the following:
• Light touch
• Superficial pain
• Temperature
• Vibration
• Joint position sense
• Stereognosis and graphaesthesia
• Sensory inattention (only test if
sensory pathways are otherwise intact)
• Test: Median, radial, ulnar, common peroneal never, lateral cutaneous nerve of thigh.
• See video: http://www.muhadharaty.com/lecture/1195
• Cortical sensations stereogensis, graphesthesia, localization of touch point, two-
point discrimination.

17
Findings:
• Carpal tunnel syndrome this may be compressed as median nerve passes between
the flexor retinaculum and the carpal bones at the wrist.
• Wrist drop this may be compressed as radial nerve runs through the axilla, or
injured in fractures of the humerus.
• Ulnar nerve this is most often affected at the elbow by external compression or
injury, e.g. dislocation.
• Foot drop Common peroneal nerve may be damaged in fibular head fractures, or
compressed.
• Meralgia paraesthetica it is paresthesia in the lateral thigh, caused by compress of
Lateral cutaneous nerve of thigh as it passes under the inguinal ligament.
• From doctor:
o Problem in cerebral cortex Hemi-sensory impairment.
o Problem in brain stem crossed sensory loss.
o Stoke and gloves sensory loss brain stem problem.
o Any cross sensory or motor brain stem lesion.
o Problem in spinal cord sensory level (below level of pathology).
o Root affected like in cord compression, dermatome sensory loss.
o Generalized advanced peripheral neuropathy generalized sensory loss.
o Kadle sensory loss in serangomalia.
o Saddle sensory loss intra-medullary spinal cord lesion.
Common features of carpal tunnel syndrome:
• More common in women.
• Unpleasant tingling in the hand.
• May not observe anatomical boundaries, radiating up the arm to the shoulder.
• Weakness uncommon, but affects thumb abduction if occurs.
• Symptoms commonly occur at night, wakening patient from sleep.
• The patient may hang the hand and arm out of the bed for relief.
• Thenar muscle wasting (in longstanding cases).
• Associated with pregnancy, diabetes and hypothyroidism.
18
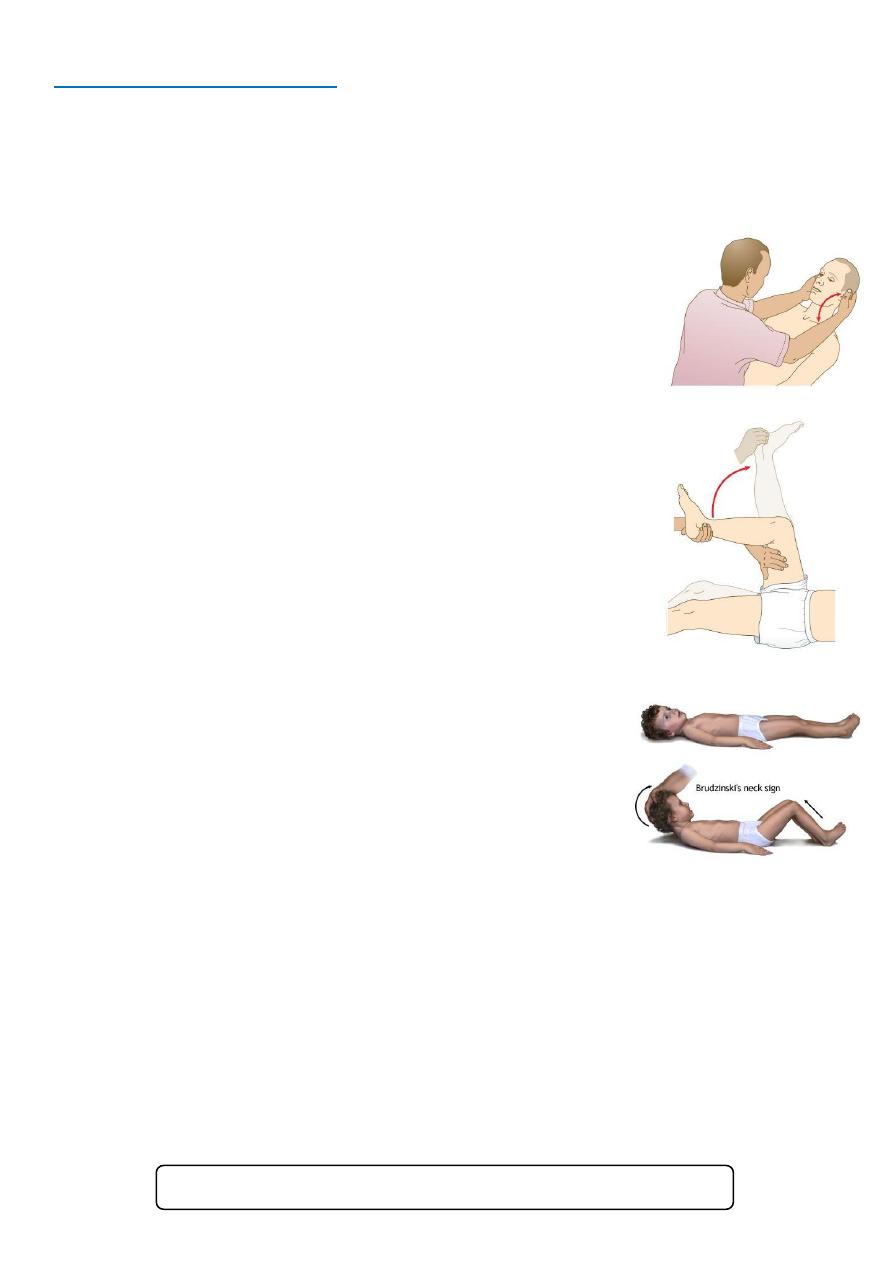
Part5: Meningeal signs
• Causes of meningism:
o Infection meningitis.
o Blood within the subarachnoid space subarachnoid hemorrhage.
o Non-neurological infections urinary tract infection.
• Examination steps:
o Position the patient supine with no pillow.
o Expose and fully extend both the patient's legs.
Neck stiffness:
o Support the patient's head with the fingers of your hands at
the occiput and the ulnar border of your hands against the
paraspinal muscles of the patient's neck.
o Flex the patient's head gently until his chin touches his chest.
o Ask the patient to hold that position for 10 seconds. If neck
stiffness is present, the neck cannot be passively flexed and
you may feel spasm in the neck muscles.
o Flexion of the knees in response to neck flexion is Brudzinski's
sign.
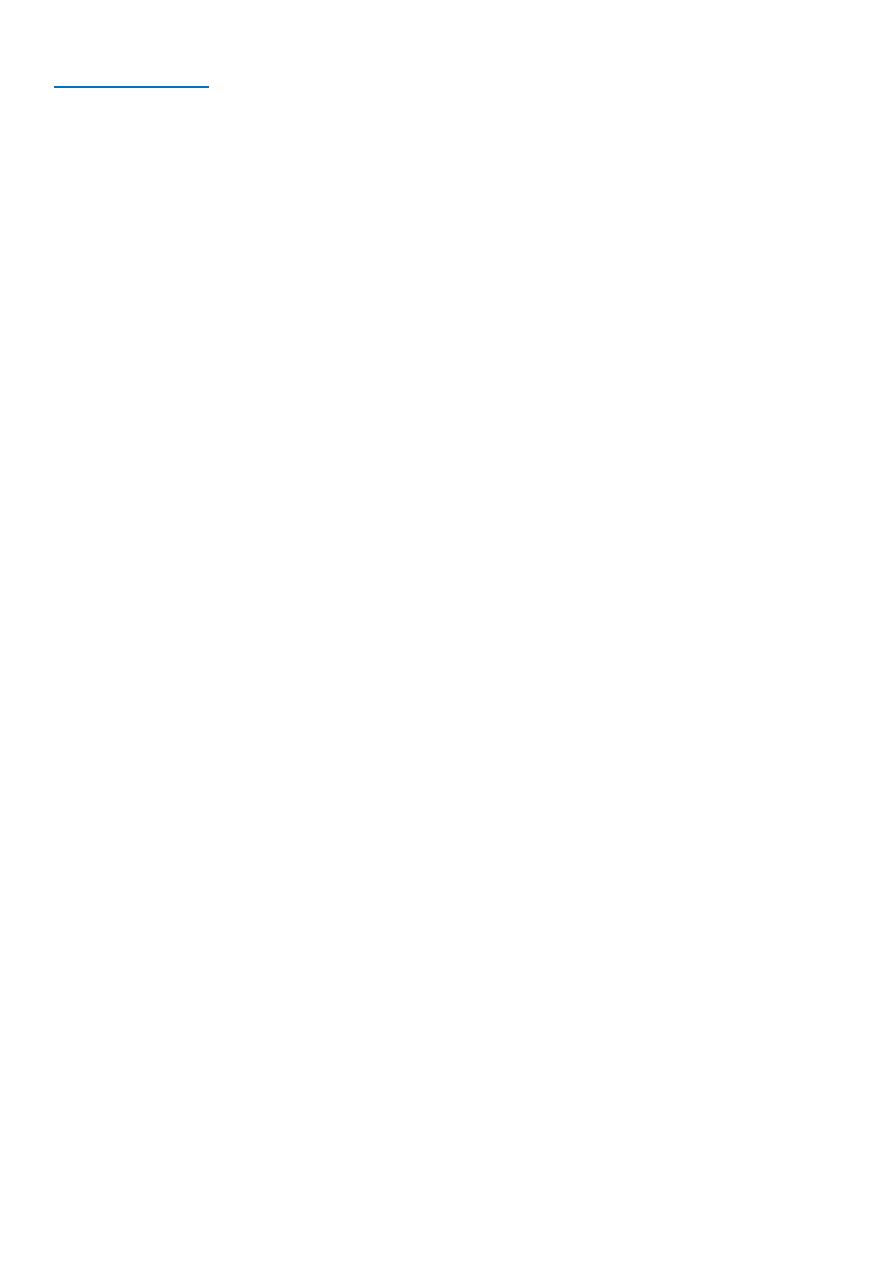
Kernig’s sign:
o Flex one of the patient's legs at the hip and knee, with your
left hand placed over the medial hamstrings.
o Use your right hand to extend the knee while the hip is
maintained in flexion. Look at the other leg for any reflex
flexion. Kernig's sign is positive when extension is resisted
by spasm in the hamstrings. The other limb may flex at
the hip and knee. Kernig's sign is absent in local causes of
neck stiffness, e.g. cervical spine disease or raised
intracranial pressure.
Brudzinski's sign:
o One of the physically demonstrable symptoms of
meningitis is Brudzinski's sign. Severe neck stiffness
causes a patient's hips and knees to flex when the neck is flexed.
• Notes:
o Neck stiffness occur in: meningitis, tumor in meninges, tumor in posterior fossa,
subarachnoid hemorrhage.
o There is no neck stiffness in: coma, old age, low immunity.
o Neck rigidity occur in: muscle spasm, cervical spondylosis.
o Kernig's sign:
Normally 180 degree.
Limited in old age 170 -\+ 5 degree.
Bilateral limitation: in severe disease, it is important in prognosis.
See this video http://www.muhadharaty.com/lecture/1196
19
Part6: Notes
• Nucleus of cranial nerves:
o 3 – 4 mid brain.
o 5 – 6 – 7 – 8 pons.
o 9 – 10 – 11 – 12 medulla.
• Tongue:
o General sensation: anteriorly (trigeminal), posteriorly (glossopharyngeal).
o Taste sensation: anteriorly (facial), posteriorly (glossopharyngeal).
o Motor: hypoglossal nerve.
• Pseudobulbar palsy: upper motor neuron lesion of any 2 nerves of the lower 4 crainal
nerves.
• Bulbar palsy: lower motor neuron lesion of any 2 nerves of the lower 4 crainal nerves.
• Fasciculation: it is a sign of bulbar palsy.
• Spasticity: it is a sign of pseudobulbar palsy.
• Spasticity: lead to small raised conceal tongue.
• Pronator sign: sign of mild upper motor neuron lesion.
• Unilateral muscle wasting due to poliomyelitis, disc prolapse.
• Bilateral proximal muscle wasting due to osteomalacia, muscle diseases.
• Bilateral distal muscle wasting due to peripheral neuropathy.
• Clonus:
o Sudden and sustained stretch of the tendon lead to contraction and relaxation of
muscles.
o Examine when suspect upper motor neuron lesion.
o So first examine for tone (hypertonia) then reflex (exaggerated reflex) then clonus
(+ve) this is occur in upper motor neuron lesion.
• Primary sensations (touch, pain, position, vibration) go to thalamus then post
central gyrus.
• Cortical sensations (Sterognosis, Graphesthesia, Tactile Extinction, look for sensory
inattention) not examine them if the primary sensations are normal.
