مكتب المنتظر للحاسباتًف ةعابطلا تمت
–
البصرة
–
مٌلس نٌدلا زع دٌهشلا ةٌحان
-
السوق
Some
Information
About Common
Pediatric Cases
أنور قيس سعدون
2
5
6
6
7
8
11
13
14
23
24
25
28
31
32
33
34
36
37
38
39
40
41
42
44
46
47
48
"
ًم ساعة بقّلعتلا ِّلذ ىلع ربصٌ مل نم
اًادب لهللا ِّلذ ًف
"
الرسول
األكرم
(
ص
)
Index
The Subject Page number
o
Preface
o
History
1) Identity, chief complaint,
history of present illness
2) Review of systems
3) Past history
4) Feeding history
5) Vaccination history
6) Developmental history
7) Family history
8) Social history, Drug history
History of special cases
1) Convulsion
2) Diabetes mellitus and DKA
3) Diarrhea and vomiting
4) Jaundice
5) Neonatal jaundice
6) Bleeding tendency
7) Haematuria
8) Skin rash
9) Poor weight gain
10) Cough
11) Dyspnea
12) Stridor
13) Pallor
14) Fever
15) Joint pain
16) Oedema
17) Other important symptoms
3
"
بَبولقلا ذذ ن
لُّلمت
ّكما تمل
األبدان فابتغوا لها طرائف الحكمة
"
اإلمام
ًعل
(
ع
)
The Subject Page number
o
Examination
1) General examination
2) Nutritional status assessment
3) Vital signs
4) Growth measures
5) Cardiovascular examination
6) Respiratory examination
7) Abdominal examination
8) Reticuloendothelial examination
9) Examination of male genitalia
10) Neurological examination of the child
11) Neurological examination of the infant
12) Musculoskeletal examination
13) Head, eyes , ears, nose, throat examination
14) Newborn examination
o
Management
1) Status epilepticus
2) Status Asthmaticus
3) Acute bronchiolitis
4) Pneumonia
5) Croup
6) Acute epiglottitis
7) Bacterial meningitis
8) Heart failure
9) SVT
10) Tet spell
11) Shock
12) Dehydration
No dehydration
Some dehydration
Severe dehydration
13) Poisoning
Salicylate poisoning
49
49
51
52
52
53
55
57
60
61
62
65
66
69
71
73
74
75
76
77
78
79
80
81
82
83
84
85
85
87
89
91
92
4
The Subject Page number
Acetaminophen poisoning
Petroleum compounds poisoning
Organic phosphorus poisoning
Iron poisoning
14) Snake bite
15) Acute renal failure
16) Diabetes Mellitus
17) Diabetic ketoacidosis (DKA)
18) Painful crisis of SCA
19) Blood transfusion reactions
20) Infant of diabetic mother
21) Infant with hypoglycemia
22) ITP
23) Severe malnutrition
24) Rickets
o
Primary health care
1) ARI program
2) CDD
3) Vaccination schedule in Iraq
o
Clinical skills
1) Basic life support
2) Chocking
3) Intraosseouss line
4) Measurement of blood pressure
o
Procedures
Phototherapy
Exchange transfusion
Ventolin nebulizer
Blood transfusion
o
Family counseling
1) Febrile convulsion
2) DKA
3) Nephrotic syndrome
4) Asthma
5) Breast feeding
o
Appendices
93
93
94
95
96
97
99
100
102
104
106
107
108
109
111
112
112
114
115
116
116
117
118
120
121
121
122
123
124
125
125
127
129
131
133
135
"
تسعٌ هنإف ملعلا ءاعو لا هٌف عضو امب قٌضٌ ءاعو لك
"
ًاإلمام عل
(
ه السالمٌلع
)
ًوالت دزن
5
بسم اهلل الرمحن الرحيم
ًاحٌخأً ًحٌخإ ىكن بهقنا ٍي تٍتح
ت انطبٍهك تبهط
جايعت انبصزة
ٌَّإ
هتٍصح ًى تيزهلدا هذى في ثايٌهعلدا
يا
ٍمتكنج ي
ج
ىـ
عو
خالل
فرتة
زي يف ادلزحهت انسادستٌزسنا بٌردخنا
ادًخعلاا عي
زيٌزسنا صحفنا عٍضاٌي في لافطلأا عزف تزيهي ىهع
باإلضافت إىل
سعفينٌ لم ٍكنً ثلاالحا ضعب جلاع في لافطلأا بخك ضعب
حيا نذنك أضعيا بنيٍقنخن جقٌنا
كىٌدٌأ
ًا ىًك
ً
أ
عخذر نكى
أيٍع
أخطاء
و
ًت أٍعبط
تًٍهع
.
ًسائال
اهلل
حعاىل
فقناٌٌ ٌا
اكىٌإً
إ
ٌأً تعفنلداً يرلخا وٍف اي مك لى
بٍمج عٍسم وَا تٍفاعناً تحصناب ىكٍهعً انٍهع ٍيم
اندعاء
.
سٍق رٌَأ
12
/
12
/
2012
"
ل تبد بخطوةٌم فللأا ةلحر
"
ةٌنٌص ةمكح
ًوالت دزن
6
"
العطر
ظلٌ
اًامئاد
ًف
دٌلا
ًالت
ًتعط
الز رة
"
ادا
لارٌب
History
Identity
1- Name
2- Age (Date of birth)
3- Sex
4- Address
5-Source of information - next of kin
6- Date of admission & Time
7-Source of referral
Chief complaint:
Symptom & duration
History of Present illness
Try to use open questions and use direct questions if necessary
For most symptoms ask about:
1. Onset
2. Duration
3. Course
4. Frequency, pattern
5. Analysis of the symptom
6. Aggravating and relieving factors, and severity
7. Associated symptoms
8. Review the involved system & exclude other differential diagnoses and
ask about risk factors
9. Family reaction , hospitalization
10. Patient condition now
7
Table 1 :
Review of systems
CNS
CVS:
Respiratory system:
1-
Headache
2-
Dizziness
3-
Vertigo
4-
Visual disturbance
5-
Syncope
6-
Loss of consciousness
7-
Limb weakness
8-
convulsion
9-
Tremor
10-Paresthesia
11- funny turns
1-
Chest pain
2-
Dyspnea
3-
Claudication
4-
Orthopnea
5-
PND
6-
Palpitation
7-
faints
8-
Fatigue
9-
cyanosis
10-
Ankle edema
1-
Chest pain
2-
Dyspnea
3-
Cough
4-
Sputum
5-
Haemoptysis
6-
Wheeze
7-
Stridor
GUT:
GIT:
1-
Dysuria
2-
Enuresis
3-
Frequency
4-
Nacturia
5-
Urgency
6-
Urine retention
7-
Polyuria
8-
Haematuria
9-
Incontinence
10-
Loin pain
11-Intermittent stream
12-Post micturition dripping
13- age of menarche
14-dysmenorrhea
1-
Appetite
2-
Abdominal pain
3-
Altered bowel motion (diarrhea or constipation)
4-
Flatulence
5-
Nausea & vomiting
6-
Haematemesis
7-
Jaundice
8-
Dysphgia
9-
Melaena
10-
Bleeding per rectum
ENT
Locomotor system:
development
1-
Earache
2-
Hearing impairment
3-
Recurrent sore
throat
4-
Enlarged glands
1-
Joint pain
2-
Joint swelling
3-
Joint Stiffness
4-
Joint locking
5-
Muscle weakness
6-
Deformity
7-
Myalgia
1-
Gross motor
2-
Fine motor
3-
Language and speech
4-
social
General
Skin:
Note:
1-
Activity
2-
Sleep
3-
School absence
4-
Weight loss
5-
Fever
1-
pallor
2-
Echymosis or any lesions
3-
Itching
4-
Skin rash
Some of these symptoms are not
suitable for certain age groups
"
رزٛلغ يْا ه١ٍؼف ًغؼٌا ٓػ شؾجٌٍ ذج٘ر ارا
عؼبد
ًؾٌٕا
"
ذأٚبو ش١ٕ١و
8
Past history
Prenatal, natal and post natal
1- Maternal age during pregnancy, G… P…
+…
2- Any problem during pregnancy (at which trimester)
3- Maternal diseases
4- Exposure to radiation
5- Drug use during pregnancy
6- Anemia, tetanus vaccination , trauma , infection, ANC, chronic
diseases like diabetes mellitus, hypertension
7- Fate of previous pregnancies
8- Normal vaginal delivery or caesarian
9- Instrumental delivery
10- Term or preterm
11- Place of delivery at home or at hospital
12- Prolong labor
13- Presentation (breach, vertex ,face )
14- Birth trauma
15- Complication during delivery
16- Birth weight
17- neonatal progress
18- Cry immediately or not
19- Cyanosis
20- Asphyxia
21- Meconium aspiration
"
ول
العلم
الصمت
،
و
ًالثان
االستماع
،
و
الثالث
الحفظ
،
و
الرابع
ا
،لعمل
والخامس
نشرذ
"
ًاألصمع
9
22- Admission to NCU
23- Pass Meconium
24- Voiding urine
25- Early feeding practice
26- Vitamin k prophylaxis
27- Receiving Drug or oxygen
28- Jaundice at which day how long it last
29- Tetanus or neonatal convulsion
Past medical and surgical History
1- Pervious same symptoms or similar attack
2- Previous hospitalization (when, why)
3- Previous operation(when ,why name of the hospital)
4- Previous blood transfusion(NO. of units ,reason,
complications)
5- Previous investigations and screening tests
6- childhood Illnesses ( measles , whooping cough , mumps)
7- Chronic illnesses should be listed in chronological order
"
فغهٔ ٟف دشىف بِّٙ
،
ذٔأف
ألٜٛ
ًب رزخ١ِّ
"
بدٚٔ ظغ٠س
"
ه رب٠غشٔاشف
ٟٔصد ذٌاٚ
10
If there is chronic illness
Ask about:
1- Age of diagnosis.
2- Initial clinical features and investigations
3- Initial hospitalization : cause, duration, name of the hospital,
progression in the hospital)
4- Frequency of hospitalization => severity
5- Period between the attacks or hospitalizations
6- Drugs details : name , type, dose, rout of administration ,who
responsible for administration, any side effect ,any change in the
drug or it's dose. follow up, special investigations
7- Other measures they did (according to the disease)
a. Blood transfusion
b. Dialysis
c. B.M biopsy or Aspiration
d. CSF analysis
8- Hx of last attacks
9- Progression of the symptoms
Example about chronic diseases that frequently repeated in OSCE
1- Thalassemia
2- Bronchial asthma
"
ًفؼٌا ٟف شضى٠ٚ ِٗلاو ٟف غماٛز٠ ِٟبغٌا ًعشٌا
"
فٛؽ١ٛطٕو
ٟٔصد ذٌاٚ
11
Feeding History
In most OSCE stations Ask about name , age , sex of the child
Introduce yourself
Explain to the mother what you are going to ask
Ask about type of feeding
1f :
Breast feeding:
1- Duration of exclusive breast feeding
2- On demand or on schedule
3- How often he/she feed
4- night feeding
5- Duration of each feeding
6- Whether she use one or both breasts
7- Proper feeding technique
8- Satisfaction of mother and baby
9- Breast engorgement , oozing of milk from other breast during the
feeding
10- Sleeping after feeding, weight gain and how often he wet his napkin
11- If there is excessive crying
12-
Were there any problems
13- Was she complement breast milk with any food (semisolid or solid)
14-
Whether she Washes her hand before and after each feeding?
15-
Medication that took by the mother
"
اًبّابف دبِ ومف ًِاا ٍٝػ ػبػ ِٓ
"
ٓ١ٍىٔاشف
ٟٔصد ذٌاٚ
12
Bottle feeding
1- Whether preceded by breast feeding (for how long?)
2- When she start bottle feeding
3- Formula or unmodified cow's milk or medical formula
4- Type of the formula that the child is receiving now
5- How was it prepared
6- Type of water that the mother uses
7- How long that the milk can take to be over
8- How often the child feed
9- On demand or on schedule
10- The amount of milk that the child consumes in each feeding
(how many ounce and how many scopes per ounce ?)
11- Volume of the residual milk
12- Average duration of each feeding
13- Sleeping pattern and sleeping after feeding ,weight gain & how
often he wet his napkin
14- Satisfaction of mother & baby
15- Number of bottles that the mother has
16- Method of sterilization
17- If there is any allergy or problems associated with feeding
(diarrhea, colic)
18- Is the mother complement bottle feeding by any food , type of that
food
"
ٍُؼٌا
ة
ٓذ٠ٌا ْٚد
أػشط
ّٝػأ ٍُؼٌا ْٚذث ٓ٠ذٌاٚ
"
ٓؾزب٠ٕ٠آ
ٟٔصد ذٌاٚ
13
Dietary History:
1) Number of meals
2) Content of meals ( Animal or plant)
3) Number of snacks
4) Favorite food
5) Food that the child forbidden from it ( why?)
6) Allergy to food
7) Weight gain, sleeping , activity
8) Whether the child has a tendency or craving to eat substances other
than normal food ? (Pica)
Weaning :
1. When it start
2. Type of weaning foods
3. By spoon or by bottles
Vaccination History
1. Is the mother herself responsible for taking the child for vaccination
2. Whether the child has vaccination card? And whether the mother is
bringing it with her now ?
3. Whether the child completed his vaccinations or not?
4. was there missed vaccine? Why ?
5. was there delayed vaccine ? why ?
6. Rout of administration of each received vaccine
7. Is there allergy to any vaccine ?
8. Ask in detail about complications of each vaccine ( fever, convulsion...)
9. Ask about BCG scar
10. Ask about additional vaccines? And why?
11. Chronic diseases: SCA, recurrent chest infection
"
ٙذفٌا ٍٝػ دبجضٌا ٛ٘ ػبغٌٕا شع
"
ٍٟ١ااسصد ٓ١ِب١ٕث
"
فرانك تايجر
والت دزني
14
Developmental History
Table 2 : Developmental Milestones in the First 2 Yr of Life
MILESTONE
AVERAGE AGE OF
ATTAINMENT (MO)
DEVELOPMENTAL IMPLICATIONS
GROSS MOTOR
Holds head steady while
sitting
2
Allows more visual interaction
Pulls to sit, with no head lag
3
Muscle tone
Brings hands together in
midline
3
Self-disCovery of hands
Asymmetric tonic neck reflex
gone
4
Can inspect hands in midline
Sits without support
6
Increasing exploration
Rolls back to stomach
6.5
Truncal flexion, risk of falls
Walks alone
12
Exploration, control of proximity to
parents
Runs
16
Supervision more difficult
FINE MOTOR
Grasps rattle
3.5
Object use
Reaches for objects
4
Visuomotor coordination
Palmar grasp gone
4
Voluntary release
Transfers object hand to hand
5.5
Comparison of objects
Thumb-finger grasp
8
Able to explore small objects
Turns pages of book
12
Increasing autonomy during book time
Scribbles
13
Visuomotor coordination
Builds tower of 2 cubes
15
Uses objects in combination
Builds tower of 6 cubes
22
Requires visual, gross, and fine motor
coordination
COMMUNICATION AND LANGUAGE
Smiles in response to face,
voice
1.5
More active social participant
Monosyllabic babble
6
Experimentation with sound, tactile sense
Inhibits to ―no‖
7
Response to tone (nonverbal)
Follows one-step command
with gesture
7
Nonverbal communication
Follows one-step command
without gesture
10
Verbal receptive language (e.g., "Give it to
me‖)
"
ٌُؼبٌا
خٌآ
رقٛ٠ش
:
هٍنف ِٓ ُغزثا
"
خٌٛمِ
ش٠ىِٟأ
ح
15
MILESTONE
AVERAGE AGE OF
ATTAINMENT (MO)
DEVELOPMENTAL IMPLICATIONS
Says ―mama‖ or ―dada‖
10
Expressive language
Points to objects
10
Interactive communication
Speaks first real word
12
Beginning of labeling
Speaks 4–6 words
15
Acquisition of object and personal names
Speaks 10–15 words
18
Acquisition of object and personal names
Speaks 2-word sentences (e.g.,
"Mommy shoe‖)
19
Beginning grammaticization, corresponds
with 50+ word vocabulary
COGNITIVE
Stares momentarily at spot
where object disappeared
2
Lack of object permanence (out of sight,
out of mind) [e.g., yarn ball dropped]
Stares at own hand
4
Self-disCovery, cause and effect
Bangs 2 cubes
8
Active comparison of objects
UnCovers toy (after seeing it
hidden)
8
Object permanence
Egocentric symbolic play (e.g.,
pretends to drink from cup)
12
Beginning symbolic thought
Uses stick to reach toy
17
Able to link actions to solve problems
Pretend play with doll (e.g.,
gives doll bottle)
17
Symbolic thought
Table 3 : Rules of Thumb for Speech
Screening
Age
(yr) Speech Production
Articulation (Amount of Speech
Understood by a Stranger)
Following
Commands
1
1-3 words
One-step
commands
2
2- to 3-word phrases
½
Two-step
commands
3
Routine use of sentences
¾
4
Routine use of sentence sequences;
conversational give-and-take
Almost all
5
Complex sentences; extensive use of
modifiers, pronouns, and prepositions
Almost all
"
سل١كَبمزٔا ٛ٘ حءبعلإا ٓػ ٛفؼٌا
"
خّىؽ
ذٕ٘
٠خ
16
Table 4: Emerging Patterns of Behavior During the 1st Year of Life
[*]
NEONATAL PERIOD (1ST 4 WK)
Prone:
Lies in flexed attitude; turns head from side to side; head sags on ventral suspension
Supine:
Generally flexed and a little stiff
Visual:
May fixate face on light in line of vision;―doll's-eye‖ movement of eyes on turning of the
body
Reflex:
Moro response active; stepping and placing reflexes; grasp reflex active
Social:
Visual preference for human face
AT 1 MO
Prone:
Legs more extended; holds chin up; turns head; head lifted momentarily to plane of body on
ventral suspension
Supine:
Tonic neck posture predominates; supple and relaxed; head lags when pulled to sitting
position
Visual:
Watches person; follows moving object
Social:
Body movements in cadence with voice of other in social contact; beginning to smile
AT 2 MO
Prone:
Raises head slightly farther; head sustained in plane of body on ventral suspension
Supine:
Tonic neck posture predominates; head lags when pulled to sitting position
Visual:
Follows moving object 180 degrees
Social:
Smiles on social contact; listens to voice and coos
AT 3 MO
Prone:
Lifts head and chest with arms extended; head above plane of body on ventral suspension
Supine:
Tonic neck posture predominates; reaches toward and misses objects; waves at toy
Sitting:
Head lag partially compensated when pulled to sitting position; early head control with
bobbing motion; back rounded
Reflex:
Typical Moro response has not persisted; makes defensive movements or selective
withdrawal reactions
Social:
Sustained social contact; listens to music; says ―aah, ngah‖
AT 4 MO
Prone:
Lifts head and chest, with head in approximately vertical axis; legs extended
Supine:
Symmetric posture predominates, hands in midline; reaches and grasps objects and brings
them to mouth
Sitting:
No head lag when pulled to sitting position; head steady, tipped forward; enjoys sitting with
full truncal support
Standing: When held erect, pushes with feet
Adaptive: Sees pellet, but makes no move to reach for it
Social:
Laughs out loud; may show displeasure if social contact is broken; excited at sight of food
"
ٛأبو ُ٘ ُو ٛاوسذ٠ ٌُ ؿبخؽا ذٔبو حب١ؾٌا ٟف ًؾفٌا دلابؽ ِٓ ش١ضو
َٝ االعزغالٍػ اٍٛجلا بِذٕػ ػبغٌٕا ِٓ ٓ١ج٠شل
"
ْبط أد٠غِٛٛر
17
AT 7 MO
Prone:
Rolls over; pivots; crawls or creep-crawls (Knobloch)
Supine:
Lifts head; rolls over; squirms
Sitting:
Sits briefly, with support of pelvis; leans forward on hands; back rounded
Standing: May support most of weight; bounces actively
Adaptive: Reaches out for and grasps large object; transfers objects from hand to hand; grasp uses
radial palm; rakes at pellet
Language: Forms polysyllabic vowel sounds
Social:
Prefers mother; babbles;enjoys mirror; responds to changes in emotional content of social
contact
AT 10 MO
Sitting:
Sits up alone and indefinitely without support, with back straight
Standing: Pulls to standing position;―cruises‖ or walks holding on to furniture
Motor:
Creeps or crawls
Adaptive: Grasps objects with thumb and forefinger; pokes at things with forefinger; picks up pellet
with assisted pincer movement; unCovers hidden toy; attempts to retrieve dropped object;
releases object grasped by other person
Language: Repetitive consonant sounds (―mama,‖ ―dada‖)
Social:
Responds to sound of name; plays peek-a-boo or pat-a-cake;waves bye-bye
AT 1 YR
Motor:
Walks with one hand held (48 wk); rises independently, takes several steps (Knobloch)
Adaptive: Picks up pellet with unassisted pincer movement of forefinger and thumb; releases object to
other person on request or gesture
Language: Says a few words besides ―mama,‖ ―dada‖
Social:
Plays simple ball game; makes postural adjustment to dressing
*
Data are derived from those of Gesell (as revised by Knobloch), Shirley, Provence, Wolf, Bailey, and others. Knobloch H, Stev ens F,
Malone AF: Manual of Developmental Diagnosis. Hagerstown, MD, Harper + Row, 1980.
"
لب ن تثق بنفسك و ذا لمٌ
؟ثق بكٌس يذلا اذ نمف كسفنب قثت
"
رسطو
18
Assessment of development
*(Means examination as well as the history)
(Examine according to the child's age and the information that you get from the developmental history )
Gross motor
Put the child in prone position : look for creeping, crawling,
raising of his head and chest
Put the child in Supine: rolling, looking, movement of extremities
Pull him to sit and see the head lag
Standing
Do axillary suspension
Do ventral suspension
Fine motor
Hold a toy in front of him and see whether he follow it
Put the toy in front of him see whether reach to it or not
Or give him the toy
Examine for pincer grip :
put a small thing in front of the child
Give him a cup and see what he will do
Give him a pen and paper
Speech and hearing:
See whether the child obey commands
Hearing assessment:
do distraction test
( according to child's age)
Social :
Type of playing
Respond to his name or not
Others : wave bye-bye
Assess the vision of the child
For more details see table 4 ( Pages 16-17)
"
من حاسب نفسه ربح ومن غفل عنها خسر ومن خاف امن ومن اعتبر
مِلبَع مهف نمو مهف رصب نمو رصب
"
نٌنمؤملا رٌم
(
ع
ه السالمٌل
)
19
Newborn
*for more accurate details see table 2 (Pages 14-15)
Gross motor
1- limbs flexed
2- symmetrical postures
3- Marked head lag on pulling up
Fine motor & vision
Follows face in midline
Speech language & learning
Straddles to laud noises
Social & emotional & behavioral
Eye contact with the mother
Responds to parents
1-3 months
Gross motor
1- Holds head up to 45
o
, holds head steady while sitting (2 months)
2- Push up on arms to sit (3monthes)
3- No head lag (3 months)
4- Bring hand together in midline (3 months)
Fine motor & vision
1- Follows moving object or face by turning the head
Speech language & learning
1- Hearing loud noises
2- Different small sounds
Social & emotional & behavioral
Smile responsively
"
دٍذ٠ خؾفبقِ هٕىّ٠ لا
مجٛمخِ
"
ذٞٔبغ اش٠ذٔا
20
4-6 months
Gross motor
1- Sits with support
Round back on sitting
2- Hold head up
3- extend & roll
Fine motor & vision
1- Reaches out for toys and catch
2- Transfer toys from one hand to another
Speech language & learning
1- Vocalizes alone or when spoken to
2- Coos
Social & emotional & behavioral
laughs
7-8 months
Gross motor
1- sits without support with straight back
2- crawling
Fine motor & vision
1- arm face to each
2- grasp pick
Speech language & learning
1- turn to soft sound
2- out of sight used indiscriminately
Social & emotional & behavioral
1-
Put food in mouth
2-
Fear from stranger
"
فت غصانهُثك ذدوع نلا ْنبَم
"
طالبًب نبا ًلع
(
ع
ه السالمٌل
)
21
9-11 months
Gross motor
1- Pull to stand
2- Walks around the furniture
Fine motor & vision
1- Mature pincer grip
Speech language & learning
1-Use sound discriminately to parents
Social & emotional & behavioral
1- Wave bye-bye
2- Play peek a poo
One year
Gross motor
1- Independent standing
2- Walking unsteadily with broad gait hand apart
Fine motor & vision
1- Pincer grip
2- catch a cup
Speech language & learning
2 to 3 wards other than dada mama
Social & emotional & behavioral
Drink from a cup
"
مٌظع و ام لك قٌقحت مهناكمإب عٌرذلا لشفلا ىلع نوؤرلٌ نم
"
ديٌنك نول
22
2 years
Gross motor
1- Walks alone steadily
2- Two feet step
3- Climbs stairs
Fine motor & vision
1- Scribbles with a pencil ( may be able since 13
th
month)
2- Builds tower of 3 or 6
Speech language & learning
1- 10 words
2- Obey commands
3- Identifying different parts of the body(nose, ear, eye, moths)
4- Use 3 or more words to make simple phrases
Social & emotional & behavioral
1- Holds food by spoon and get safely to mouth
2- Symbolic play
3- Dry by day
4- Pulls off some clothing
3 years
Gross motor
1- One foot step
2- Playing
Fine motor & vision
Draw a circle without seeing how to do
Speech language & learning
Talk constantly in 3-4 ward sentences more clear
Social & emotional & behavioral
1- Inter active playing
2- Know colors
"
اإلنسان
العاقل
و
الذي
غلقٌ
فمه
قبل
ان
غلقٌ
الناس
آذانهم
"
كٌردٌرف
تشهٌن
23
"
ّسم
ا
رةٌشع
،
و
صلة
قرابة
،
و
سرة
..
سمها
ما
شئت
،
فمهما
كنت
ستحتاج
واحدة
"
نٌال
وارد
4 years
Gross motor:
Jump
Fine motor & vision
1- Able to draw across(4 yrs. ) or square (4.5 yrs.)
2- Build tower of 8
3- Trains with 4 bricks
4- Bridge and steps
5- Catches ball
Speech language & learning
Tall long story
Social & emotional & behavioral
Play with other children
0lder children
1- Relation with family
2- Activity and hobbies
3- School performance (Stage , missing days, attendance, grades,
relation with friends & teacher )
Family history
1-
Father : name ,age, occupation
2-
Mother : name ,age, occupation
3-
Consanguinity: relative or not degree of consanguinity
4-
Brothers & sisters(age ,sex, illnesses)
5-
Order of the child in the familly
6-
Same symptoms in the family
7-
History of death in the family :cause ,date
8-
Diseases affect more than one member of the family
9-
Chronic diseases in the family
24
"
بدٌ
بٌبطلا
اتهٌح
ةٌنهملا
بأن
صفٌ
نٌرشع
اًءاود
لكل
مرض
،
و
بعد
سنوات
من
الخبرة
ًنتهٌ
الى
ان
صفٌ
دواء
اًادحاو
نٌرشعل
اًاضرم
"
امٌلو
وسلر
Social history
1-Parents smoking
2- Living conditions
Own or rented house
Water and electrical supply
Number of rooms
Sanitary condition
Safety measures
3- Animal relationship & Pet rearing
4-Hobbies
5-Traveling or contact with patient with same symptoms
6-Worris or stresses
Drug history
:
1- Chronic drug use: steroid and others
2- Allergy to drug & food and previous significant drug side effect
3- Over the counter medicines and herbal preparations
4- Hx of specific drug use according to the condition like
Warfarin or Heparin in bleeding tendency
5-others : radiotherapy , psychotherapy
6- If there is a chronic disease controlled by special drug ask about:
Name of the drug that the patient use
Dose of the drug
Duration of thereby
Form of the drug
Freq. of administration
Rout of administration
Who responsible for administration of the drug
Any side effect
Any new adjustment to the dose or type of the drug
Storage of the drug
Is the disease well controlled by this drug ?
25
"
دٍعاٚ ٍُؼزِٚ كهبٔ ٌُبػ ٓ١ٍُعشٌ لائ ؼ١ػ لا
"
جٛٞ ؽش٠فٔ ش٠ذؽ
ًاإلمام عل
(
ع
)
History of common symptoms
1- Convulsion
Name, Age, sex
1)
Onset
2)
Timing( day , night)
3)
Duration
4)
Frequency
Whether the mother notice the attack
5)
Pre ictal
1. What precede the attack:
a. Nervousness
b. Excessive crying
c. Shortness of breath
d. abdominal pain
2. What was the child do at time of the attack
6)
ictal description
1. facial changes
a. eye ( flickering, blinking , rolling, upward movement, staring)
b. oropharyngeal : excessive salivation , lip smacking
c. twitching of the face
2. limb changes : jerky limb movement ( which limb involved , unilateral
or bilateral , coming regularly or not)
3. sphincter control
4. associated symptoms
a. loss of consciousness
b. circumoral pallor
c. cyanosis
d. tongue biting
5. Resolve spontaneously or by medication
7)
post ictal phase
1. pass in deep sleeping
2. limb weakness
3. period between the attack (if frequent) is the child well
8)
precipitating conditions
1. Fever, skin rash
2. vomiting and diarrhea (bloody or watery)
3. symptoms of UTI
4. chest infection (cough , SOB)
5. Headache with vomiting (Brain tumor)
6. Drug intake
7. Withdrawal from antiepileptic drug
8. Stressful condition
9. Recent vaccination
9)family history of convulsion
10) family action, investigation & medication that the pt. received & pt. condition
now
26
"
لو
اعتقدت
انك
قادر
على
فعل
شئ
ما
،
و
اعتقدت
نك
رٌغ
قادر
على
فعل
ءًش
ما
،
ًفف
كلتا
نٌتلاحلا
نت
على
صواب
"
شٞ فٛسدٕ٘
ًاإلمام عل
(
ع
)
Past Hx of epileptic patient
1) Prenatal
a. Any drug intake during pregnancy
b. Fever , rubella infection
c. DM , hypertension , ANC
2) Natal:
a. Term or not
b. Mode of delivery, Instrumental delivery
c. Prolong labor , any other complication during labor
d. Birth trauma
3) Post natal
Develop jaundice, asphyxia , admitted to NCU
If there were recurrent attacks:
1. Age of first attack
2. Initial manifestations
3. Initial investigations
4. Initial hospitalization (cause, duration, name of hospital ,
progression of the condition)
5. Freq. of hospitalization (severity)
6. Reason for each hospitalization
7. Patient condition between the attacks
8. Is the patient on antiepileptic drug? When he start?
9. Antiepileptic therapy:
Name of the drug that the patient use
Form of the drug
Dose of the drug
Freq. of administration
Rout of administration
Who responsible for administration of the drug
Any side effect
Any new adjustment to the drug dose or type
Storage of the drug
Is the disease well control on this drug ?
10. Last attack (details)
11. Progression of the condition
12. Freq. of child follow up & EEG
4) Other points in past medical and surgical history (blood transfusion,
chronic diseases, childhood diseases (mumps , measles))
27
"
بيِ٢ا
خّ١ظؼٌا
غٕقر
ااؽخبؿ
بءّظؼٌا
"
ْبط أد٠غِٛٛر
ٍٟػ َبِلإا
(
ع
)
Examination of a patient with seizure
Physical Examination General Appearance: Post-ictal
lethargy. Note whether the patient looks well or ill. Observe the
patient performing tasks (tying shoes, walking).
Vital Signs: Growth percentiles, BP (hypertension), pulse,
respiratory rate, temperature (hyperpyrexia).
Skin: Café-au-lait spots, neurofibromas (Von Recklinghausen's
disease). Unilateral port-wine facial nevus (Sturge-Weber
syndrome); facial angiofibromas (adenoma sebaceum),
hypopigmented ash leaf spots (tuberous sclerosis).
HEENT: Head trauma, pupil reactivity and equality, extraocular
movements; papilledema, gum hyperplasia (phenytoin); tongue
or buccal lacerations; neck rigidity.
Chest: Rhonchi, wheeze (aspiration).
Heart: Rhythm, murmurs.
Extremities: Cyanosis, fractures, trauma.
Perianal: Incontinence of urine or feces.
Neuro: Dysarthria, visual field deficits, cranial nerve palsies,
sensory deficits, focal weakness (Todd's paralysis), Babinski's
sign, developmental delay.
28
"
"
ال
،ر١أط
فؼبدح
بِ
ْ٠ىٛ
آخش
فزبػِ
فٟ
ٛػخّغِ
فبر١ؼٌّا
٘ٛ
بعتٌّٕا
فزؼٌ
جبةٌا
"
نورمان
فنسنت
لٌب
ًاإلمام عل
(
ع
)
2- Diabetes Mellitus & DKA
ID:
Name, age, sex
CC:
1. Hyperglycemia, DKA: vomiting , abdominal pain
2. Hypoglycemia : drowsiness ,sweating, loss of consciousness ,
convulsion)
3. Infection : UTI, Chest infection, diarrhea, vomiting and fever)
4. Classical symptoms of DM (Polyuria, polyphagia polydipsia ,
nocturnal enuresis, weight loss).
HPI
1. analysis of presented symptom
2. review of the system involved
3. ask about other symptoms of DM (as above)
4. ask about the precipitating factors for DKA:
1) fever and skin rash
2) stress : trauma , surgery, psychological stress, exercise
3) take insulin , usual dose or less
5. other symptoms of DKA if the family notice :
a. acetonic smell
b. change in pattern and depth of breathing
c. decrease urine output (dehydration)
d. convulsion
8. family action
9. hospitalization ( investigations and medications in details and
whether the patient improved in the emergency department or not?)
Past Hx of DKA Patient
1) Prenatal
a. Any drug intake during pregnancy
b. Fever , rubella infection
c. DM , hypertension , ANC
2) Natal:
a. Term or not
b. Mode of delivery, Instrumental delivery
c. Prolong labor , any other complication during labor
d. Birth weight
e. Birth trauma
f. Birth asphyxia
29
"
ع
بِذٔ
ال
رزفبءي
،
٠زغٛط
زوبٌا
ء
"
فىزٛس ٘١غٛ
ٍٟػ َبِلإا
(
ع
)
3) Post natal
like the other diseases.
4)
If there were recurrent attacks:
1. Age of diagnosis of DM
2. Initial manifestations
3. Initial investigations
4. Initial hospitalization (when, cause, duration, name of
hospital , progression of the condition)
5. Freq. of hospitalization (severity)
6. Reason for each hospitalization
7. Patient condition between the attacks
8. Insulin therapy:
1) When he start to take insulin
2) Type of insulin
3) Dose of the insulin
4) Freq. of administration
5) Rout and sites of administration
6) Who responsible for administration of the insulin
7) Any local or systemic side effect
8) adjustment to dose or type of insulin
9) Storage of the insulin
10) Is the disease well control on this regimen
9. Last attack (details)
10. Progression of the condition
11. Whether the family has glucometer at home
12. Freq. of follow up
5) Other points in the past medical and surgical history (blood
transfusion, chronic diseases (celiac disease, Vitiligo, autoimmune
thyroiditis ) childhood diseases (mumps, measles)
Family Hx.
1. DM
2. Auto immune diseases :
a. Autoimmune thyroiditis
b. Celiac disease
c. Addison disease
d. Vitiligo
e. Other autoimmune diseases
3. Other points in family history like any dz.
30
"
فشقٌا
ٓث١
ٛالغٌا
ٚ
ٍُؾٌا
٘ٛ
خٍّو
ِٓ
صالصخ
أ
ؽشف
(
ًّػ
" )
رولر
تسٌرف
Dietary Hx.:
Number of meals & Snacks
Type of food ,and preferred food
Forbidden from any food or restricted food e.g food contain sugar
Social Hx.:
Living conditions
Income of family
Drug Hx.:
Details of insulin therapy
Any recent drug ingestion chronic drug use
Examination of a child with DKA
1- General look:
1. Age
2. Look ill, or well
3. Built
4. Conscious level
5. Pattern of breathing
6. Dyspneic or not
7. Acetonic smell (musty, apple odor),
8. Capillary refilling
9. Clubbing of finger (celiac dz. may associated with DM)
2- Vital signs
3- Hydration status
4- Growth measures
5- Chest : rales, rhonchi
6- Examination of the skin:
1. Sites of insulin injection
2. Hypo/hyper pigmentation (signs of other autoimmune diseases)
3. Examination of tips of the fingers for pin prick (site of blood investigation)
4. Any skin changes (ulceration , thickening( autoimmune thyroiditis))
5. Skin infection
31
"
بءٕجغٌا
ْ٠ٙشثٛ
ِٓ
خطشٌا
،
ٚ
خطشٌا
٠ٙشة
ِٓ
ؾغؼبٌا
ْ
"
توٌدود
ً ػَبِلإا
3- Diarrhea ( Frequent bowel motion) and vomiting
ID:
name, age , and other information
HPI
1- onset
2- duration
3- frequency per day
4- related to eating or not?
5- Amount, color, odor , consistency : watery , semisolid
6- Associated with mucus or blood ( fresh blood, streak , mixed
with the stool)
7- Associated with :
1) Pain or crying on defecation (tenesmus)
2) Protrusion of a lump (rectal prolapse)
3) Napkin rash, skin rash
4) Fever
5) Vomiting : onset, which start first vomiting or diarrhea , freq. relation
to feeding , vomiting of everything, projectile or effortless, amount ,
color, consistency, aggravating or reliving factors, contain blood or
not)
6) Abdominal distension
7) Urine output, irritability, disturbed conscious level, sunken eyes
8) convulsion
8- Effect on feeding, sleeping, activity, weight gain
Past Hx: Previous same attack, chronic diseases, celiac dz. ,
IBD, Abdominal surgery, recurrent chest infection
Feeding Hx:
type of feeding breast or bottle feeding,
sterilization, No. of bottle that the mother has , source
of water, Any weaning food
Family Hx.
Of IBD, celiac dz., same condition other family
members affected or not
Drug Hx
.
Antibiotics
32
"
ٓزىٌ
فبرؾب
ألثٛاةٌ
ٌّٓ
ْ٠أرٛ
ثؼذن
"
رالف
والدو
امرسون
4- Jaundice:
ID
1) name
2) Age
HPI
1- Duration
2- Onset
3- Progressive or fluctuant
4- Associated with:
1) Abdominal pain
2) Itching
5- Color of urine
6- Color of the stool
7- Bleeding from any where
8- Review of GIT
1- Anorexia
2- Nausea & vomiting
3- Flatulence
4- Altered bowel motion (diarrhea or constipation)
5- Poor wt, gain
6- Haematemesis
7- Melaena
8- Bleeding per rectum
9- Constitutional symptoms
Fever & rigor
Malaise
Precipitating factors : food , stress, hunger
1-
Past Hx
Blood transfusion
Previous jaundice (neonatal)
Haematemesis and malena
Previous biliary surgery
SCA, G6PD, thalassemia, chronic liver dz
2- Social Hx
Contact with jaundice pt.
Hx of traveling
3- Family Hx:
Hemolytic dz
Liver dz,
History of perinatal infant death (metabolic disorders).
Other member of family Affected
4- Developmental Hx.
5- Vaccination history : hepatitis B vaccine
6- Feeding Hx breast feeding or bottle feeding ,serialization
7- Drug Hx
Acetaminophen, isoniazid, phenytoin.
33
"
ا تصعدًاملس اهب ًنباو اهعملا لب ،اهب رثعتت لاف ةرالحلاب ةئٌلم ةاٌحلا
به نحو النلاح
"
نجٌك رثول نترام
5- Neonatal Jaundice:
ID
1) Name
2) Age
HPI
1- Age of onset (in days)
2- Duration
3- Progression of jaundice
4- Color of urine
5- Color of the stool
6- Bleeding from any where
7- Ask about these symptoms
Fever
Skin rash
Convulsion
Sleepiness, decrease activity
Poor feeding
Vomiting
8- Ask about blood group of the child and the parents
Past history
Perinatal history:
o Any complication during the pregnancy, whether the mother developed
jaundice
o Term or preterm ?
o Birth trauma, cephalhematoma
o Birth weight
o Previous child with neonatal jaundice
Family Hx:
Whether the parents relatives
Hemolytic dz
Liver dz
Vaccination history : hepatitis B vaccine
Feeding Hx. breast feeding or bottle feeding ,serialization
Drug Hx
Icterogenic drugs
Any addition , Thank you
34
"
٠غت
ىٌٟ
غؼٕر
ْأ
ْرىٛ
سغجزه
فٟ
غبػٌٕا
أوجش
ِٓ
خٛفه
ِٓ
ًفؾٌا
"
ًث١
وٛعجٟ
6-Bleeding tendency
ID:
Name, age , and other information
HPI
1- onset
2- duration
3- site the bleeding ( if rash ask about distribution)
4- bleeding from other sites (Haematuria ,malena , epistaxis, haematemesis)
5- spontaneous or there are precipitating factors ( like trauma , ask about degree of trauma and
after how long after trauma) (factor XIII delayed )
6- frequency of the bleeding ,color of the bleeding , amount , contain clot
7- if there is bruising ask about color of bruising and how long stays before fading
8- joint pain , joint swelling , menorrhagia (in older female child)
9- any skin other lesions?
10- Preceded by ( respiratory tract infection , Diarrhea)
11- associated symptoms:
pallor
fever
syncope
decrease activity
palpitation (in older child)
jaundice
dyspnea ( bleeding in the soft tissue of the neck)
abdominal pain ( iliopsoas bleeding), distention, diarrhea
headache , convulsion , vomiting, change in the mood
12- how the bleeding stopped (spontaneously or not)
13- general condition of the child ( feeding , sleeping , weight gain)
14- family action
15- management received
16- the pt. condition now
Past history
any similar attack of bleeding
age of onset of first attack
Hx of hepatitis
Hx of previous blood transfusion
Chronic dz. Chronic liver dz. , chronic renal failure
Hematoma at site of vaccine or injection
Hx of bleeding after cutting of umbilical cord or after or minor operation like tooth
extraction , circumcision or after tonsillectomy
Family Hx
Any similar condition in the family
Drug Hx
Aspirin
NSAID's
Heparin
Warfarin
Other parts of the history
35
"
الوزغبة
ؼشفخٌّا
ٍٝػ
شءٌّا
ْا
٠ذسط
،
ٚ
الوزغبة
خّىؾٌا
١ٍٗػ
ْأ
٠الؽع
"
نٌلرام
فوس
سافانت
Examination of a child with bruising or skin rash
Goals:
1- to exclude dangerous site of bleeding (CNS, Neck, iliopsoas muscle)
2- to exclude other DDX
General look
Ask about the name and take a permission
1-
age of the pt. (e.g ITP in toddlers )
2-
sex
3-
conscious level
4-
look well or ill
5-
dyspneic
6-
pallor
7-
jaundice
local examination
inspection
1- site of the bruise, affect which part of the body, on flexors or extensors
2- bilateral or unilateral
3- symmetrical OR asymmetrical distribution
4- color
5- size in mm
6- shape
7- numbers
8- type of bruising (Petechiae, purpura, ecchymosis )
palpation
1- palpable or not
2- blenching or not (Differ from rash, bruise is not fade by blenching)
3- tender or not
other sites to be examined
1- bleeding from mouth mucous membrane
2- epistaxis
3- neck muscle for swelling (hematoma)
4- joint swelling
5- reticuloendothelial system ( spleen , LN)
6- abdominal examination for hepatosplenomegaly
7- signs of chronic liver dz.
36
"
فشلٌ
الناس
راٌثك
،
سٌل
بسبب
نقص
القدرات
،
و نما
بسبب
نقص
ًف
االلتزام
"
زج زللر
7-Red color urine (Haematuria)
ID:
name ,age , and other related information
1- duration
2- onset
3- Timing(terminal, whole stream, only beginning of micturition)
4- pattern ( intermittent , continuous)
5- severity
1) Associated with clot
2) Amount
3) palpitation , Dyspnea, headache, decrease urine output, fainting
attack
6- Bleeding between voiding
7- Bleeding from other sites
8- Has :
1) Hx of passing stone
2) Hx of trauma or Exercise
3) Hx of foley catheter insertion
4) Hx of URTI
9- Abdominal mass
10-
Review of GUT
1) Dysurea
2) Frequency
3) Nacturia
4) Urgency
5) Urge incontinence
6) Polyuria
7) Hesitancy
8) Intermittency
9) Loin pain
10) Poor stream
11) Post micturition dribbling & Terminal dribbling
11-
Other symptoms
1) Poor weight gain
2) Poor feeding
3) Fever
4) skin rash
5) convulsion
6) bloody diarrhea, vomiting (HUS)
7) hemoptysis (good pasture syndrome)
8) joint pain (SLE)
12-family history of deafness(Alport syndrome), congenital kidney
anomalies (polycystic kidney)
13- Menstrual Hx (in older female)
14-
Hx of drug ingestion
(like rifampicin)
15-
Food ingestion (beet root
)
16-
Ask about child Abuse
37
"
لذ
غٕٝر
زٌٞا
مؾىذ
ؼِٗ
،
ٚ
ٓىٌ
ٌٓ
غٕٝر
زٌٞا
ثى١ذ
ؼِٗ
"
ط
ْثشا
ً١ٍخ
ْعجشا
8-Skin rash
ID:
name, age , and other information
HPI
1- onset
2- duration
3- site of start
4- distribution
5- Any other sites of rash
6- color of the rash
7- itchy?, tender?
8- Unilateral or bilateral
9- occurs spontaneous or there are precipitating factors ( like trauma , ask about degree of
trauma and how long after trauma it appeared) (factor XIII delayed )
10- progression
11- whether it disappear or not, after how long
12- type of rash ( popular, maculopapular, macular, vesicular)
13- bleeding from any site (Haematuria ,malena, epistaxis)
14- joint pain , joint swelling , menorrhagia (in older female child)
15- Preceded by ( Respiratory tract infection , Diarrhea, Tonsillitis)
16- associated symptoms:
pallor
fever
sore throat
syncope
decrease activity, irritability
palpitation (in older child)
jaundice
dyspnea ( bleeding in the soft tissue of the neck muscles)
abdominal pain, distention, diarrhea
Haematuria and other urinary complains
headache , convulsion , vomiting, change in the mood
17- general condition of the child ( feeding , sleeping , weight gain)
18- family action
19- management received
20- the pt. condition now
Past history
any similar attack of rash or bleeding
age of onset of first attack
Hx of hepatitis
Hx of previous blood transfusion
Chronic dz. Chronic liver dz. , chronic renal failure
Hematoma at site of vaccine or injection
Hx of bleeding after cutting of umbilical cord or after or minor operation like tooth extraction ,
circumcision or after tonsillectomy
Family Hx
Any similar condition in the family
Drug Hx
Aspirin. Penicillin , NSAID's , Heparin, Warfarin
Other parts of the history
38
"
نا
حتفظ
بستة
من
نٌنواعملا
،
تعلمت
منهم
كل
ما
عرف
...
و
م
:
ماذ
ا
لماذا،
،
متى
،
فٌك
،
نٌ
،
من
"
اردٌدور
بلنغٌك
9-Poor weight gain
ID: Name ,age , and other related information
1- onset
2- duration
3- was the condition started since birth or newly developed
4- is the child has any medical condition
5- Review of GIT
1) appetite
2) frequent bowel motion, frequent vomiting
6- symptoms of hyperthyroidism
7- history of head trauma
8- Review urinary system
9- Review respiratory systems , chronic chest infection (CF)
10- fever , leg swelling, diarrhea, colic, vomiting, irritability, fatigue or chronic
cough
Past Hx
1) Prenatal
IUGR
congenital infection and prenatal problems
2) Natal
a. Birth asphyxia
b. Birth trauma
c. Low birth weight
3) Post natal: prematurity , jaundice
4) Past medical
Hx of meningitis, any chronic illnesses , may jeopardize growth potential.
Recurrent or chronic illness may affect growth, congenital heart diseases
Feeding history: Take a dietary history (a food diary can be helpful).
Ask about feeding difficulties: did they start at birth, weaning or as
a toddler? Consider whether they are a result or cause of FTT
Developmental Hx : Are there neurodevelopmental problems? Has FTT
affected the baby's developmental progress?
Family Hx: history of same condition in the family Is there a family history
of FTT or genetic problems? Are there psychosocial problems?
Social Hx :concentrate on social class and income , parents education
Drug Hx : steroid use
Family reaction
Ix which was done and the medication that the child received
39
"
ربما
تفشل
اذا
خاطرت
،
لكن
من
المؤكد
انك
ستفشل
اذا
لم
تخاطر
"
روبرت
تاٌفرول
10-Cough
ID:
Name ,age , sex and other related information
1- Duration
2- Onset
3- Time of occurrence ( night , morning)
4- Frequency
5- Short or Paroxysmal
6- Character : barking , whooping
7- Dry or productive : if there is sputum : color , amount , with blood , smell
8- Description of the attacks and what the child was doing at that time
9- Aggravating factors relieving factors
10- Associated symptoms( fever, dyspnea, vomiting , convulsion, cyanosis ,
noisy breathing, hoarse voice, sore throat, preceded by choking)
11- Effect on feeding , sleeping , activity
12- Past history
1- Prenatal: mother fever , rubella
2- Natal : premature , post term difficult labor, birth asphyxia , Meconium aspiration
3- Cyanosis at birth
4- Admission to NCU the cause
5- any similar attack in the past
6- age of onset of first attack
7- allergy , eczema
13- Feeding Hx .
type of feeding
14-Family Hx
1- Any Hx of asthma or allergy in the family
2- Dermatitis , atopy , sinusitis , cystic fibrosis
3- Immune deficiency , child death, hx of congenital heart diseases , heart failure ,
cardiomyopathy , any chronic respiratory problems
15-
Social Hx :
1- Occupation of mother and father
2- Smoking
3- Pet owner
4- overcrowded
16-
Developmental Hx:
Effect on development
17-
Vaccination Hx:
DTP, BCG
18-
Drug Hx
1- Aspirin
2- ACE inhibitors
3- Allergy to food or drug
40
"
كم فال تملوا النعمٌلع للو زع الله معن نم مكٌل سانلا جئاوح نا اوملع
اًامقن مكٌلع دوعتف
"
نٌسحلا ماملإا
(
ه السالمٌلع
)
11-dyspnea
ID:
Name ,age , and other related information
HPI
1- Onset (sudden or gradual)
2- Duration
3- Timing (at night or day time)
4- precipitating factors: exercise , perfume , dust, dandruff
5- what the child was doing when the attack occurred
6- preceded symptoms : fever , cough , chocking
7- Ass. symptoms : cyanosis, runny nose, noisy breathing, chest pain , sore throat ,
sputum , hemoptysis
8- aggravating factors & relieving factors: certain position
9- frequency of the attacks
10- wt. gain , sleeping pattern , interfere with the activity
11- associated with eczema , allergy
12- associated with:
1) pallor
2) syncope
3) leg edema
4) convulsion , vomiting of every thing
5) abdominal distention
6) diarrhea ( cystic fibrosis)
13- family action
14- management received
15- the pt. condition now
Past history
Prenatal: mother fever , rubella
Natal : premature , post term difficult labor birth asphyxia , Meconium aspiration
Cyanosis at birth
Admission to NCU the cause
any similar attack in the past if the condition recurrent take a history of chronic diseases
age of onset of first attack…
history of eczema, allergy
history of chocking
Feeding Hx .
type of feeding, method of sterilization
Family Hx
Any Hx of asthma or allergy in the family
Dermatitis , atopy , sinusitis , cystic fibrosis
Immune deficiency , child death, hx of congenital heart diseases , heart failure ,
cardiomyopathy , any chronic respiratory problems
Social Hx :
Occupation of mother and father, Smoking
Pet in the house
overcrowded
Developmental Hx:
Effect on development
Drug Hx
Aspirin ,NSAID's, Allergy to food or drug
41
"
ٓو
اًبّااد
اإلفذاس
ااٚي
ِٓ
فغهٔ
،
ٚ
ال
ٓرى
اإلفذاس
ٟٔبضٌا
ِٓ
اؽذ
آخش
"
لودي
لارالند
12-Stridor
ID:
Name ,age , and other related information
HPI
1- Onset (sudden or gradual)
2- Duration
3- Timing (at night or day time)
4- Is the stridor exertional, biphasic, continuous
5- what the child was do when the attack occurred
6- preceded symptoms : fever , cough , chocking, runny nose, sore throat
7- relieving & aggravating factors (exertion, certain position)
8- associated symptoms:
1) high grade fever
2) Dysphagia, drooling
3) dyspnea and respiratory distress
4) cyanosis
5) any change in the voice
6) convulsion , vomiting, chest pain , sputum , hemoptysis
9- whether the child take special posture
10- wt. gain , sleeping pattern , interfere with child's activity
11- family action
12- management received
13- pt. condition now
Past history
Premature , post term difficult labor, birth asphyxia , Meconium aspiration
Cyanosis at birth
History of choking
any similar attack in the past
age of onset of first attack
Feeding Hx .
type of feeding…
Family Hx
Same condition in the family
chronic respiratory problems
Drug Hx
History of drug exposure
42
"
ُاا٘
ِٓ
ْا
َرزمذ
ثغشػخ
٘ٛ
ْا
َرزمذ
فٟ
االرغبٖ
قؾ١ؼٌا
"
ْبط أد٠غِٛٛر
13-Pallor:
ID: Name, age, sex
HPI
1- onset
2- duration
3- external bleeding (hx: of trauma)
4- color of stool , urine
5- associated with :
jaundice
bleeding from any where
fever
skin rash
bone pain
abdominal pain
diarrhea (bloody, offensive , difficult to Wash "malabsorption")
headache fatigue , dizziness , poor concentration, convulsion
syncope
pica
child activity , sleeping pattern, weight gain
menorrhagia (in older female)
6- Past Hx:
Hemoglobinopathies,G6PD
Neonatal jaundice
Previous attacks of pallor or jaundice
Hx of blood transfusion
7- Family Hx:
Of hemolytic anemia : Hemoglobinopathies , G6PD , spherocytosis
8- Feeding Hx:
Type of feeding
No. and content of meals
Beans and other foods that cause hemolysis in
G6PD
9- drug Hx:
Trimethoprim
Ciprofloxacin … and other drugs that cause hemolysis in G6PD
43
"
ىٌٟ
ْرىٛ
اًبِب٘
،
ٓو
اًبّزِٙ
"
ضٌسبؾر
َٛسربٔ
Examination of a patient with pallor
1) General look
1- Conscious level
2- Dysmorphic features (e.g thalassemic face )
3- Café au lait (fancony anemia)
4- Erythematous rash, Butterfly rash
5- Microcephaly , microphthalmia or bony abnormalities
(fancony anemia)
2) examination for anemia
i. Lower Conjunctiva for pallor
ii. Mouth signs :mucus membrane, loss of tongue papillae ,
angular stomatitis
iii. hand signs: palmar creases (compare with the other
hand) , capillary refilling, Clubbing of fingers,
koilonychia, white nail bed
3) Other important signs
1- Jaundice
2- LAP
3- Petechiae or bleeding from any site
4- Features of malabsorption
5- Cleft lip, Lip pigmentations
6- Also examine for organomegaly
44
"
١هٍػ
ْأ
ًرفؼ
ااؽ١بء
زٌٟا
رؼزمذ
ٗٔا
١ظٌ
ثبعزطبػزه
ْأ
ٙبٍؼفر
"
انورٌلا
روزفلت
14-Fever
ID: Name , age ,sex
HPI:
1- Duration
2- Onset
3- Height
4- When increase (night or day)
5- Pattern of fever (intermittent , remittent , sustaining , relapsing….)
6- How does the fever assessed by (touch, thermometer)
7- low grade or high grade (associated with sweating, rigor , chill , shivering)
8- aggravating and relieving factors (medication , cold sponges)
9- how quickly the fever responds to antipyretics drugs
10- Hx of recent vaccination
11- associated with:
a) red eyes
b) nasal discharge
c) recurrent pharyngitis with ulceration
d) abnormal body movement
e) headache in older children
f) skin rash
g) limbs or bones pain, joint swelling
h) ear pain
12- Review of:
o Respiratory (cough , SOB ,runny nose, sore throat )
o GIT: ( diarrhea , abdominal pain , vomiting, poor appetite )
o GUT: (dysurea or cry during micturition , loin pain
13- If it affects feeding , sleeping , activity of the child
14- Whether there is weight loss, night sweating
15- Family action, investigation which was done for the child
16- Consumption of unpasteurized milk (brucellosis)
Past hx
.
o Previous same illness, recent surgery (abdominal…)
o Previous infectious dz. ( measles, mumps , chicken box , whooping cough )
o History of congenital heart disease
Vaccination
Complete or not, BCG, Recent vaccination
Family Hx.
Any similar condition in the family
Social Hx.
o Sanitation & water supply,
o Hx. Of exposure to wild or domestic animals
,
tick bite or
o travel to tick- or parasite-infested areas
o Contact with infected or ill person
Feeding history :
o
Hx. of pica (is a particularly important clue to infection with Toxocara)
o
Bottle feeding , sterilization , type of water
Developmental Hx
Drug Hx
Iodides , atropine
45
"
لٌلق
من
اإلدراك
مٌلسلا
،
و
لٌلق
من
التسامح
،
و
لٌلق
من
المرح
..
و
سوف
تند ش
عندما
ترى
فٌك
استطعت
ان
حٌرت
نفسك
على
سطح
ذا
الكوكب
"
سومرست
موم
Examination of a child with Fever
WIPE
Ask about name ,age , sex
1.General Appearance: Lethargy, toxic appearance. Note whether the
patient looks ―ill‖ or well. Dysmorphic features
2.Vital Signs: Temperature (fever curve), respiratory rate (tachypnea),
pulse (tachycardia). Hypotension (sepsis), hypertension (neuroblastoma,
pheochromocytoma). Growth and weight percentiles.
3.Skin: Rashes, nodules, skin breaks, bruises, pallor. Icterus, splinter
hemorrhages; delayed capillary refill, petechia (septic emboli,
meningococcemia), ecthyma gangrenosum (purpuric plaque of
Pseudomonas). Pustules,cellulitis, furuncles, abscesses.
4.Lymph Nodes: Cervical, supraclavicular, axillary, inguinal adenopathy.
5.Eyes: Conjunctival erythema, retinal hemorrhages, papilledema.
6.Ears: Tympanic membrane inflammation, decreased mobility.
7.Mouth: Periodontitis, sinus tenderness; pharyngeal erythema, exudate.
8.Neck: Lymphadenopathy, neck rigidity.
9.Breast: Tenderness, masses, discharge.
10.Chest: Dullness to percussion, rhonchi, crackles.
11.Heart: Murmurs (rheumatic fever, endocarditis, myocarditis).
12.Abdomen: Masses, liver tenderness, hepatomegaly, splenomegaly; right
lower quadrant tenderness (appendicitis). Costovertebral angle tenderness,
suprapubic tenderness (urinary tract infection).
13.Extremities: Wounds; IV catheter tenderness (phlebitis) joint or bone
tenderness (septic arthritis). Osler's nodes, Janeway's lesions (endocarditis).
Clubbing, vertebral tenderness.
14.Rectal: Perianal skin tags, fissures, anal ulcers (Crohn disease), rectal
flocculence, fissures, masses, occult blood.
15.Pelvic/Genitourinary: Cervical discharge, cervical motion tenderness,
adnexal tenderness, adnexal masses, genital herpes lesions.
46
"
لو
ن
اًائٌش
اًارٌغص
له
القدرة
على
ن
لعلكٌ
،تغضب
ال
رٌشٌ
ذا
لى
حلمك
؟
"
ًدنٌس
سٌرا
15-Joint pain
ID: Name , age , sex
HPI:
1- Onset
2- Duration
3- Increased at (night or day)
4- Number of involved joints (poly /
oligoarthritis)
5- Pattern of distribution
6- progression
7- aggravating and relieving factors (medication , certain position)
8- effect of the pain on joint movement… and walking (limping)
9- is there joint swelling, early morning stiffness?
10-
associated with:
a)
fever
b)
skin rash( on the trunk "erythema marginatum", on the extensors )
c)
abnormal limb movements ( chorea )
d)
pallor
e)
diarrhea, Melaena, Haematuria
f)
bleeding from any site
g)
development of nodules over bony prominences
11- Preceded by tonsillitis , sore throat
12- History of trauma
13- Hx of recent vaccination
14- If it affect feeding , sleeping , activity of the child
15- If there is weight loss, night sweating
16- Family action
17- Pt. condition now
Past hx
.
Birth trauma, instrumental delevery
Previous same illness , Previous trauma, rheumatic fever, joint diseases
Sickle cell anemia, tonsillitis, hemophilia
Vaccination : MMR
Family Hx.
Of SCA, hemophilia
Any similar condition in the family
Developmental Hx
Drug Hx
47
"
رٌكفتلا
ًالسلب
منعٌ
اإلنسان
من
ةٌؤر
الطرق
ئةٌضملا
و
لعلهٌ
سلكٌ
الطرق
المظلمة
ًالت
ال
لدٌ
ًف
اتهاٌاهن
مخرلا
"
نوٌز
16-
Oedema (body swelling)
ID: Name, age, sex
HPI
1- Duration
2- Onset
3- Timing (night, daytime)
4- Generalize or localize
5- Distribution, Periorbital ,ankle swelling
6- Bilateral, unilateral
7- Progression of edema
8- Intermittent or persistent
9- Pain , redness
10- Hx of trauma, insect bite (if localize)
11- Associated symptoms:
1) SOB, Orthopnea, Cough
2) Abdominal distention, Chronic diarrhea, steatorrhoea and abdominal pain,
uremic symptoms such as nausea, vomiting
3) Jaundice
4) Haematuria ,Anuria ,oliguria ,Polyuria, , frothy urine
5) Skin rash
6) Convulsion
7) pallor
8) Poor feeding
9) Fatigue
12- Weight gain and physical activity
13-
Past Hx:
Nephrotic syndrome
Liver dz. Heart dz.
Chronic Gastrointestinal dz.
Hx of renal biopsy
Previous surgery
14- Feeding Hx. Type of feeding , protein diet
15- Family History: Lupus erythematosus, cystic fibrosis, renal disease,
cardiac problem Alport syndrome, hereditary angioedema, deafness.
16- Drug Hx.
Steroid, diuretics, allergies to food, animal dander
48
"
شعبيٌا
أسثؼخ
:
ًسع
٠ذسٞ
ٚ
٠ذسٞ
ٗٔا
٠ذسٞ
،
هٌزف
ُؽى١
فبرجؼٖٛ
..
ٚ
ًسع
٠ذسٞ
ٚ
ال
٠ذسٞ
ٗٔا
٠ذسٞ
،
هٌزف
ًغبف
جٖٕٙٛف
..
ٚ
ًسع
ال
٠ذسٞ
ٚ
٠ذسٞ
ٗٔا
ال ٠ذسٞ
،
هٌزف
ًعب٘
ٍّٖٛؼف
..
ٚ
ًسع
ال
٠ذسٞ
ٚ
ال
٠ذسٞ
ٗٔا
ال
،٠ذسٞ
هٌزف
كّؽأ
جٖٕٛزعبف
"
لٌلخلا
بن
احمد
ديٌ ارفلا
Symptoms you need to read about its History
1- Chronic constipation
2- Acute paralysis
3- Abdominal pain
4- Loss of consciousness
5-Hadache
Note:
Not all previously mentioned questions
Are needed in OSCE examination and on the
other hand may be there are some missed
points but that is what I can collect it so you
should keep that in your mind and please
excuse me.
49
"
ال
ًرم
ٗٔئ
١ظٌ
ذ٠هٌ
ٛلذٌا
،
ذ٠هٍف
ًو
َ٠ٛ
فظٔ
ػذد
غبػبدٌا
زٌٞا
ْوب
ذٌٜ
ٓ١ٍ١٘
ًو١
س
ٚثبعزٛس
ًب٠ىِٚ
ٍٛغٔأ
بسدٚٔٛ١ٌٚ
ؾٟٕ١فاد
ٚ
بطِٛر
ْع١فشعٛ
ٚ
جشدٌأ
ٓؾزب٠ٕ٠آ
"
ْعبوغٛ
ْثشاٚ
Examination
(Note: Most of these information are taken from the booklet of the pediatrics department)
In most OSCE stations
Ask about patient's name, age and sex
Explain what you are going to do
The hand must be Washed before and after the examination
Warm smile, warm hand and a warm stethoscope all help
Undressing better to do by the child himself or his parent
General examination
Ask about patient's name, age and sex
Explain what you are going to do
1- WIPE
1) Wash your hand
2) Introduce your self
3) Take permission, put the pt. in the suitable position
4) Expose the patient and examine from right side
2-General observations:
1) Dysmorphic feature: like face of down syndrome (Mongolian face ),
Buffy face , moon face
2) Look for the child: well , ill, in pain, irritable
3) Hygiene : good, poor
4) Child activity
5) Behavior
6) Child parents interaction
50
"
القوة
ال
ًتأت
من
مقدرة
ةٌنامسل
،
بل
ًتأت
بها
رادة
ال
تقهر
"
المهاتما غاندي
Others
(not listed in the pediatric department's booklet)
7) Age: infant , toddler, preschool, school, adolescent
8) Built:
thin (built , average built , obese built if >5yrs
well nourished or mal nourished for <5 yrs (see below)
9) Conscious level: full conscious, lethargic, unconscious
10) Position: lying ,sitting in his mother lab , standing
11) Posture : flexed ,extended
12) Dyspneic or signs of distress
13) Crying
14) Surroundings ( O
2
bottle , nebulizer, iv fluid)
3-
Look for general signs
Jaundice
Anemia
Cyanosis
Clubbing
Oedema
LAP (lymph adenopathy )
Skin rash
4- Assessment hydration status:
Note: this assessment is not according to the new CDD (see page
114 for CDD program)
General state:
Well , alert
restless or irritable
lethargic or unconscious
Eyes: not sunken, Sunken, very Sunken
Tear: present , absent , absent
Tongue: moist , dry , very dry
Thirst: drink normally, thirsty drink eagerly, drink poorly
Skin turgor : goes back immediately, goes back slowly, goes back very
slowly >2 sec.
Pulse: normal ,fast, very fast
Fontanels (infant) : normal sunken ,very sunken
Decide : no dehydration , some dehydration , severe dehydration
51
"
قةٌقحلا
مثل
النحلة
تحمل
ًف
لوفها
العسل
ًوف
ذنبها
اإلبرة
"
ةٌنامل ةلوقم
4-Nutritional status assessment
1)
WIPE
2)
Ask about name and age of the child
3)
General look:
1. facial appearance : old man face , miserable , puffy face
2. hair (discolored , brittle)
3. photophobia
4. avoid eye contact or not
4)
examination:
1) for wasting ( loose skin and creasing):
1. axillae
2. abdomen
3. thighs (medial aspects)
Other regions
4. gluteal region : flat buttocks
5. intercostal muscles
6. prominent vertebrae
2) palpate for peripheral edema
>5 years
10 cm above the medial malleolus on the shin of
tibia for 1 min
Also don’t forget to examine for sacral edema ,
periorbital , pulmonary edema and for ascites
Infant :At the dorsum of the foot for 30
seconds
3) Eye signs of malnutrition : ulceration , bitot spots,
conjunctivitis
4) Skin (smooth, shiny ,blistered, burned,
pigmentation, cracked)
5) Mouth for angular stomatitis , smooth tongue ,
dentition status
5)
Check for growth measures : height , weight, OFC, and plot them on
growth chart and Z score ,also measure mid upper arm circumference
(MUAC) if >6 months
6)
Decide : well nourished , malnourished (mild, moderate, severe,
malnutrition)
52
"
ارا
ذٕو
خالي
ٛادٕغٌا
بم١خٌّا
ٌُ
ٓرزج
اًاسبىفأ
ٚ
سؤٜ
عذ٠ذح
١هٍؼف
ْا
رم١ظ
جنهٔ
،
بّثشف
ْرىٛ
ّاًبز١ِ
"
فرانك
تٌلٌل
6-Vital signs
* for normal values according to the age see table 14 (page 148)
a.
Pulse: Rate (
beat/minute), rhythm, volume, character, radio-radial or
radio-femoral delay
b. Temperature: normal core temperature is 36.5-37.5
Can be measured (sublingual, rectal, axillae, tympanic)
c. Respiratory rate: calculate it in full minute while your hand on the radial pulse to
draw patient attention (cycle/minute), depth , pattern of respiration
d. Blood pressure ( see page 120)
7-
Growth measures:
*see
appendices (pages 135-145) for more details
Weight :
Scales must be calibrated accurately
Weigh the child naked
Weigh the older children with light clothes or only underwear
Length or Height :
Length:
Use a measuring frame or mat
Measure the child lying down until 2 years old
Ask the helper to hold baby head against the head board
Make sure the legs are straight and the feet at 90 degrees before reading of the
length
Height :
For children > 2yrs
Use a properly calibrated standing frame.
Check the feet are bare, against the wall and flat on the floor with knee
straight
Gently extend the neck and ensure the eyes are level with the external
auditory meatus
Head circumference :
Use flexible non stretchable tape measure
Measure the occipito-frontal circumference three times and take the largest
diameter.
53
"
ؼجمش٠خٌا
١
%
ٙبِٕ
ئ
َٙبٌ
،
ٚ
٩٩
%
عٙذ
ٚ
رؼت
"
ْبط أد٠غِٛٛر
ًاإلمام عل
(
ع
)
Cardiovascular system examination
Ask about patient's name, age and sex
Explain what you are going to do
1- WIPE
1) Wash your hand
2) Introduce your self
3) Take permission, put the pt. in the suitable position
4) Expose the pt. and examine from right side
2- General observations:
1) Pallor
2) Cyanosis
3) Respiratory distress
4) Ankle edema
5) Finger clubbing
6) Capillary refilling
7) Pulse: radial, brachial, carotid, femoral describe:
Rate
Rhythm: regular or irregular
Character: collapsing, slow raising
Volume
3- Inspection of precordium:
For any thoracotomy scar may be hidden under the arm or
in the back
others
visible apex beat
4- Palpation:
1- Parasternal heave in lower half of the sternum heave indicate
right ventricular hypertrophy
54
"
اًلاو
تلا لونكٌ
..
ثم
سخرونٌ
منك
..
ثم
قاتلونكٌ
..
ثم
تفوز
"
المهاتما
غاندي
2- Thrill : palpable murmur over the four valve areas and in
suprasternal notch
3- Apex beat normally in 5
th
intercostal space or 4
th
in children less
than 5 years in mid clavicular line
4- Liver : palpate and percuss over the liver, hepatomegaly suggest
heart failure
5- Auscultation:
1- Auscultate carefully use both bell and diaphragm of stethoscope
2- listen over the four valve areas and over the back
3- look for:
First and second heart sounds
Murmurs: if you heard murmur describe:
Systolic or diastolic
Character (blowing or harsh)
Grade (I-VI)
Site of maximum intensity
Radiation
And recognize whether it's innocent or pathological
Note : diastolic murmurs always pathological
Added sound such as gallop rhythm in heart failure and ejection
click in aortic stenosis
6- Measure the blood pressure:
7- Measure growth parameters and plot on percentile charts
poor growth suggest congenital heart diseases
Cover the patient
Wash your hand
Thank the child and the mother
55
"
بط صالسٌٕا
ةٌح
ةٌٍُؼزِٚ ٟٔبثس ٌُبؼف
ٍٝػ
ًعج١
دٍحبغٔ
ةٌظّ٘ٚ
دٍعبػس
ُأرجبع
س٠ؼًو غِ ٍْٛ١ّ٠ كػبٔ ًو
٠غزنٌُٟ
اٛ
ٌُٞٚ ٍُؼٌا سٕٛث ا
غئٛاٌ
دٍٓوس ٌٝا
دٍك١صٚ
"
ٓ١ِٕإٌّا ش١ِأ
(
َغالٌا ٗ١ٍػ
)
Respiratory system examination:
Ask about patient's name, age and sex
Explain what you are going to do
1- WIPE
1) Wash your hand
2) Introduce your self
3) Take permission, put the pt. in the suitable position
4) Expose the pt. and examine from right side
2- General observation
1- Restlessness, drowsiness
2- any audible sound: stridor , wheezes, grunting
3- signs of respiratory distress
1. flaring of alae nasi
2. indrowing of the chest ,recession
3. use of accessory muscles
4- count respiratory rate (tachypnea)
5- cyanosis
6- pallor
7- finger clubbing
others
notice cough character
notice the surrounding
3-examination of the chest
1) exposure
2) inspection
1. signs of respiratory distress
2. shape of the chest
others
3. any scar
4. movement with respiration
5. depth of respiration
6. mode of respiration
56
"
ُت
قدر
مةٌقلا
ةٌقٌقحلا
لإلنسان
بدرلة
طرتهٌس
على
ذاته
"
البرت
نٌاتشنٌا
3) palpation
1. tracheal deviation (position of trachea )
2. localize the apex beat
3. chest expansion (it is normally 1 cm in a 5 years child)
4. tactile vocal fremitus: ask the child to say (44 in Arabic) while you palpate
the chest it will increase over an area of consolidation
others
5. palpate the chest wall for any:
a. tenderness
b. mass
6. palpate the liver (palpable in bronchiolitis)
4) Percussion:
In systematic way including the clavicles and axillae
o From anterior compare side to side
o From mid axillary line
o From back
5)Auscultation:
Ask the pt. to breath in & out though the mouth
ask the child to Cough
Auscultate from anterior & from posterior and compare side to side
During the auscultation notice :
breathing sound :vesicular or bronchial breathing
additional sounds : crepitation, rhonchi
using diaphragm of the stethoscope start at the top of the chest and
compare side to side
describe your findings according to their location in the chest
o infraclavicular area, mammary area, inframammary area
o axillary area, infra-axillary area
o suprascapular area, interscapular area, infrascapular area
vocal resonance : ask the child to say (44 in Arabic) it will increase over an
area of consolidation
Cover the patient
Wash your hand
Thank the child and the mother
57
"
رقشف
اًبّااد
ًضِ
جطخٌا
..
ؽ١ش
رجذٚ
اًبادب٘
ٚ
اًبٕ١ىزغِ
ٍٝػ
غطؼٌا
،
ٚ
رغذف
ثمٛح
فٟ
بٌّا
ء
"
لاكوب
برود
Abdominal examination
Ask about patient's name, age and sex
Explain what you are going to do
1- WIPE
1) Wash your hand
2) Introduce your self
3) Take permission, put the pt. in the suitable position
4) Expose the pt. and examine from right side
2- General look:
1) General appearance does the child look : ill, well
2) Jaundice
3) Pallor
4) Mouth: check for state of teeth and abnormal smell
5) Skin lesions: spider nevi
6) Palmar erythema
7) Finger clubbing
8) Wasted buttocks suggest recent weight loss
9) Edema
4- Inspection of the abdomen :
1-From the foot of the bed
Symmetry
Shape
Distension (generalize or localize)
2- kneeling from side of the bed
Movements
Movement with respiration
Visible pulsation
Visible Peristalsis
58
"
اذا
تعلمت
الهروب
اًاموٌ
،
فسوف
صبحٌ
عادة
"
نسٌف
لومباردي
Others
3- from the side of the bed look for :
1)
Skin
Dilated veins
Scars (site, describe it)
Any discoloration , pigmentation
Signs of liver diseases
stria
2)
Umbilicus: position, shape ,discharge (amount, color, type)
3)
Ask the pt. to cough to examine hernial orifice
4- Palpation:
Before palpation warm your hand and ask the child if there is tenderness
Get down the child's level and watch his face
Do superficial and deep palpation for tenderness or masses
use two or more fingers depending on child's size
All four quadrants should be palpated in turn
palpation for organomegaly
liver:
o normally palpable 1-2 cm below right costal margin in children under 2
years
o
Palpate from right iliac fossa using tip of the fingers
o
You can confirm liver size by percussing upper and lower borders
Spleen:
o ask the patient to take deep breath and palpate from right iliac
fossa
o you can turn the child to toward you
kidneys : examine the kidneys by bimanual palpation
Other masses: also check for constipation in the left iliac fossa
( for any organomegaly look for span, edge , surface , consistency)

59
"
اذا
ردت
ن
تتخلص
من
عادة
ئةٌس
فال
تلق
بها
من
النافذة
،
و
لكن
انزل
معها
السلم
درلة
درلة
"
لٌما
كراي
5- Percussion:
Percuss the entire abdomen
Ascites is suspected if you found dullness in the flanks and a resonant note
in the mid line
Confirm that by shifting dullness and fluid thrill
6- Auscultation:
Bowel sound , renal artery bruit on renal angle
7- Rectal examination:
Not routinely performed
If needed left it until last
Use your little finger in infant
Cover the child
Wash your hand
Thank the child and the mother
60
"
اثذأ
نشٚسٌٞبث
،
ُص
ًزمٔا
ٌٝا
ٓىٌّّا
،
رغذ
فغهٔ
فغأح
ًرفؼ
ًغزؾ١ٌّا
"
سٌسنارف
كونٌب
Reticuloendothelial system examination
Ask about patient's name, age and sex
Explain what you are going to do
1- WIPE
2- General look:
1) jaundice
2) pallor
3- Examine the neck:
1)
examine the lymph node in anterior and posterior triangles
2)
stand in front of the child and feel the pre and post auricular ,occipital nodes
and those along the anterior cervical chain
3)
stand behind the child and feel the submental ,submandibular , posterior
cervical nodes
4)
examine the throat if you find cervical LAP
4- Examine the axillae:
1) While the child sitting facing you
2) Support the flexed arm at the elbow with your left hand holding the left arm
3) Place your right hand in the left axilla
4) Feel for the enlarge nodes against the chest wall.
5) Reverse the process for the other side
6) If there is LAP check the hands and arms for a focus of infection
5- Examine the Groin:
1) Lie the child down and gently palpate the groin for enlarge nodes
2) If there is LAP check the feet and legs for a focus of infection
If you find a large node describe it in term of:
o Size
o Position
o Texture: hard, rubbery
o Mobility
6- Examine for hepatosplenomegaly
61
"
ال
عٌطتسٌ
اإلنسان
رٌٌغت
نفسه
بدون
لم
،
فهو
الرخام
و
و
نفسه
النحات
"
سٌسكل
لٌلراك
Examination of male genitalia
Ask about patient's name, age and sex
Explain what you are going to do
1- WIPE
2-inspection :
1) Under developed scrotum
2) Enlarge scrotum
3) Groin swelling
4) Hypospadias
3-palpation :
1) Warm your hand
2) If can't feel the testis may be retracted or undescended
3) Milk it down from the groin
4) If you failed, examine the child in squatting or sitting cross-legged position
If you find a swelling in the groin it may be enlarge lymph node, hernia or gonad
Do transillumination test to distinguish a hydrocele from hernia
Cover the child
Wash your hand
Thank the child and the mother
62
"
حرسك و نت تحرس المال والمال تنقصه النفقة والعلمٌ ملعلاف لاملا نم رٌخ ملعلا
زكوا عٌ
لى
زول بزوالهٌ لاملا عٌنصو قافنلإا
"
ًاإلمام عل
(
ه السالمٌلع
)
Neurological examination of the child
Ask about patient's name, age and sex
Explain what you are going to do
1) WIPE
2) General look
1) conscious level
2) dysmorphic features
3) observe the child's posture and look for evidence of contractures
4) abnormal movements
5) observe the child gait
6) Gower's sign
7) Muscle bulk
3) Motor examination
1)
Tone
Tone is assessed by the resistance to passive movement of the
limbs. In infants, tone and strength may be judged by
observing the posture. Predominantly flexor tone is normal,
whereas a frog-leg position suggests hypotonia.
Spasticity
2)
Power:
Upper limbs
Lower limbs
3)
Reflexes:
Tendon reflexes:
The symmetry and magnitude of muscle stretch reflexes
are evaluated. The joint under consideration should be at
approximately 90 degrees and fully relaxed. It is often
helpful for the examiner to cradle the joint in his or her
own arm to support it. The end of the hammer should be
held with the other hand and the head of the hammer
63
"
ْا
َم١بٌا
ثخطٛح
عذ٠ذح
أٚ
فعٍزٌا
خٍّىث
عذ٠ذح
٘ٛ
أوضش
بِ
٠خؾبٖ
بطٌٕا
"
ًفسكٌوتسود
allowed to drop like a pendulum so that it strikes the
tendon. Reflexes usually tested are:
Biceps: C5
Triceps : C6
Supinator: C5
Knee: L3,4 S1
Ankle: L5
Planter reflex
4)
Clonus
5)
Coordination (see Cerebellar signs)
4) Sensory examination
1. light touch: using cotton wool
2. pain: with blunt needle
3. temperature
4. proprioception (position sense)
5) Cerebellar signs and coordination (very important)
1. Speech
2. tremor
3. nystagmus
4. nose finger test
5. dysdiadokokinesis
6. heel-shin test
7. Gait
A wide-based, unsteady gait is characteristic of cerebellar
dysfunction.
Circumduction and toe-dragging often occur with
spasticity.
A high-stepping, slapping gait often is seen with peripheral
neuromuscular disease.
A waddling gait occurs with pelvic girdle weakness (eg,
myopathies and muscular dystrophies).
Asymmetries of gait, or decreased arm swing or abnormal
arm posturing are often present in hemiparesis
8. Romberg's sign (read about it)
64
"
ىٌٟ
رخزشع
ذٔا
ثؾبعخ
ٌٝا
خٍ١خِ
ع١ذح
ٚ
خِٛو
خشدح
"
توماس
سونٌدا
6) Cranial nerves:
I: Olfactory nerve : Ask the child if he has a sense of smell and test with a familiar
non irritant substance.
II. Optic nerve: examine fundi , and vision
III. Occulomotor, IV.Trochlear &VI. Abducent nerves : Examine eye
movements
V. Trigeminal nerve: the motor component of the fifth nerve supplies the jaw
muscles. Ask the child to
open his mouth and bite hard . palpate the masseter muscle . the 5
th
nerve also
provides sensation to much of the face and is divided into the ophthalmic,
maxillary and mandibular divisions test sensation to light touch in each of these
areas , the corneal reflex is not routinely examined in children.
VII. Facial nerve : Ask the child to screw up his eyes as tightly as possible and
show his teeth . in ability to bury the eyelashes on one side or close the eye , and
drooping of the corner of the mouth may indicate facial nerve pulsy.
VIII. Auditory nerve: Ask about hearing . if there is any doubt, or speech delay
you should obtain a hearing test.
IX. Glossopharyngeal nerve, X . vagus nerve, XII. Hypoglossal nerves: ask the
child to stick out his tongue, look for tongue and uvula deviation. The gag reflex
is not routinely examined in children.
XI. Accessory nerve : Ask the child to turn his head to the sides against the
resistance of your hand, and to shrug his shoulderd
Cover the child
Wash your hand
Thank the child and the mother
65
"
مذسحٌا
ٍٝػ
سثو
ٛسِاا
ثطش٠مخ
غش٠جخ
ٟ٘
ؾٛسِ
االثذاع
ٟٕ٘زٌا
ثغل
ظشٌٕا
ٓػ
غبٌّا
ي
"
لورج
دلٌس
Neurological examination of the infant
Ask about patient's name, age and sex
Explain what you are going to do
1. WIPE
2. General look :
1) Irritability
2) Position at rest
3) Spontaneous movement
4) Look for base of the spine for any tuft of hair
3. Regional examination :
1) Fontanelle
2) Head circumference
3) Tone
Prone position
Supine position
Pull to sit to see head lag
Axillary suspension
Ventral suspension
Passive movement
4) Reflexes
Deep tendon reflexes
Primitive reflexes:
o Moro reflex :disappears by three months of age
o Grasp reflexes (palmar and plantar): disappear by three months
of age
o Sucking and rooting reflexes
o Extensor plantar response :variably present in normal newborns;
disappears by 8 to 12 months of age
o Stepping reflex: disappears by one to two months of age
o Asymmetrical tonic neck reflex: variably present in normal
newborns; disappears by six months of age
o Parchute reflex: develops from 9 months and persist
5) Vision : check that the baby can fix and follow a silent moving object
6) Hearing consider doing distraction test
66
"
الحالة
م
االختراع
"
افالطون
Musculoskeletal system examination
Ask about patient's name, age and sex
Explain what you are going to do
1) WIPE
2) Look :
Look for gait of the child for limp and rhythm and symmetry of movements
Look for any gross abnormalities of the muscles, bones and joint
1. Redness
2. Swelling
3. Deformity
4. Wasting
5. Function: gait, hold a pencil, do up buttons
3)
Feel
for:
1. Tenderness
2. Temperature
3. Effusion : for the knee joint
look for bulge sign by milking fluid in the medial aspect of the knee in
the lateral side
then firmly stroke the lateral aspect of the knee downwards to push the
fluid back in to the medial compartment , you will see a "bulge" of
fluid.
4. Limb length and muscle bulk
Leg length is measured from anterior superior iliac spine to the
medial malleolus
Muscle bulk is measured at a fixed distance from the tibial
tuberosity
You should compare side to side
67
"
لو
ان
الحالة
ً
م
االختراع
،
فان
عدم
الرضا
و
بو
التقدم
"
دٌفٌد
روكفلر
4) Move
Range of movement
Check for active movement by asking the child to mimic your movement
Check passive movement and notice any limitation or contractures
Observe child's face for any signs of pain
Compare the limbs on each side
Examine for scoliosis
Ask the child to stand erect with feet together and examine the child from
behind
1. look for asymmetry of the shoulders
2. then ask the child to bend forward at the waist and straightening up
slowly
3. examine the spine and thorax for symmetry and prominence of the
scapulae
Examine the following:
Thoraco-lumbar spine:
flexion
extension
rotation
lateral flexion
Cervical spine:
flexion
extension
rotation
lateral flexion
Shoulder joint:
abduction
adduction
flexion
extension
rotation
Elbow and wrist joints:
flexion
extension
pronation
supination
rotation of the wrist
68
"
ٓذ٠ٌا
لٛح
ّٝظػ
..
ٗٔا
مٛحٌا
ذافؼخٌا
ؾم١م١خٌا
ٛؽ١ذحٌا
فٟ
ٌُؼبٌا
"
لورج
برناردشو
Hand:
fingers movement
open and closing the fist
Hip joint:
flexion
extension internal and external rotation
abduction
adduction
Knee joint:
flexion
extension
Ankle joint:
flexion
extension
rotation
Feet:
inspect the arches
flexion and extension of the toes
Cover the child
Wash your hand
Thank the child and the mother
Note:
Examination of knee joint is frequently coming in
OSCE
69
"
لقد
شكل
القرآن
خالق
نٌملسملا
،
و
حضهم
على
االعتدال
لدرلة
ال
ولدٌ
لها
رٌظن
ًف
ي
بقعة
سكنهاٌ
الرلل
ضٌبلأا
...
و
علمهم
موالهة
اةٌحلا
دون
شكوى
و
دموع
"
لٌو
ورانتٌد
Head, ear, eye, nose, throat examination
Ask about patient's name, age and sex
Explain what you are going to do
WIPE
Head
1) Inspection:
1)
Shape of the head
2)
dysmorphic features
3)
Size of the head (measure OFC)
4)
Fontanelle
:
bulged , depressed
2) palpation:
1)
Anterior Fontanelle: closed, measure its diameter
2)
posterior fontanelle
3)
suture lines
4)
skull bones for any swelling , craniotabes
5)
palpate the scalp, hair ( texture, pattern)
Ear
1. inspection:
site : low seated ?
size
discharge: color of the discharge
swelling
patency
2. Palpation
for tenderness
ear cartilage
swelling
3. Examine the ear by auriscope
4.Do distraction hearing test
70
"
السبب
ًف
انتشار
اللهل
ن
من
ملكونهٌ
متحمسون
لدا
لنشرذ
"
فرانك
كالرك
Eye examination
1. inspection:
shape
orientation: slanted or not
size
distance between the eyes : telecanthus
epicanthal fold
look for any obvious abnormality like squint
examine the cornea (hazy) , conjunctiva, iris
eye lid: ptosis
2.
Examine for visual acuity
3.
Examine for eye movements
4.
Visual field: "wiggy finger test"
5.
Reflexes
corneal reflex
red reflex
6. Fundoscopy
7. Cover test
Examination for squint:
1.corneal light reflex
2.occular movement
3.visual acuity
4.Cover test
5.fundoscopy
Nose examination:
sit the child
examine the nostrils for inflammation , obstruction, polyp
look for any abnormality
look for nasal discharge
Throat examination:
sit the child
examine the mucosa of the mouth , teeth, tongue, palate, tonsils using tongue
depressor
look for any abnormality
examine for cervical LAP
71
"
حالة
اإلنكار
تصل
ببعض
الناس
الى
درلة
نهم
على
استعداد
لتلا ل
ولود
لٌف
معهم
ًف
نفس
الغرفة
"
بوب
ودورد
Newborn examination
Ask about patient's name, age and sex
Explain to mother what you are going to do
1) WIPE
2) General appearance:
1. Posture
2. Dysmorphic features
3. Activity
4. Lethargy
5. Irritability
6. Quality of crying
7. Describe any abnormality: phocomelia, spina bifida
3) Gestational age
1. Skin color, gelatinous , sticky, cracking
2. Lanugo hair, none , abundant
3. Planter surface for creases
4. Breast: subcutaneous tissue
5. Eye, ear : lids of eyes and cartilage of the ears
6. Genitals (male): scrotum rugae , testes presence
7. Genitals (female): labia and clitoris
4) Examine the skin
1) Color: jaundice, pale , plethoric
2) Texture: dry ,wrinkled, vernix – Covered
3) Look for : milia , erythema toxicum, hemangiomas (capillary, strawberry),
mongolian blue spots, fat necrosis
5) Examine the head
1) Shape e.g rounded in premature baby
2) Measure OFC usually 35 cm
3) Fontanels: size, bulging , depressed
4) Suture lines
5) Feel skull bones for craniotabes, moulding , cuput succedaneum
Cephalhematoma
72
"
ر المنظمٌكفتلا مول ةهلاوم عٌطتست ةلكشم دلوت لا
"
رٌتلوف
ًاإلمام عل
(
ع
)
6)Examine the eyes
Look for :
1) Discharge
2) Cataract
3) Increase size and haziness of cornea suggest congenital glaucoma
4) Look for presence of red reflex
7) Examine the ears
For shape, patency
8) Examine the mouth
For:
Thrush on the tongue or buccal mucosa
Movement of oropharynx and epithelial pearls
Hard palate ( high, normal , flat) , cleft palate , ranula
For systemic examination of newborn see the booklet of pediatric
department
73
"
الو م
نصف
،الداء
و
االطمئنان
نصف
،الدواء
و
الصبر
ول
خطوات
الشفاء
"
ناٌس نبا
Management
The following pages contain information about
management of about 24 Cases but of course
that's not enough and further reading is required,
so at least you need to read about the following
subjects which are frequently coming in OSCE
like:
1- Management of spherocytosis
2-Mangemant of hemorrhagic disease of newborn
3- Tb and it's Management
4- Management of Iron deficiency anaemia
5-Management of Thalassemia
6- Management of pyelonephritis
7-Management of Nephrotic syndrome
8-Managemnt of Haemophilia and Haemarthrosis
Also there are some stations of data interpretation
like chest X-ray, complete blood count and ECG
you must know something about them
74
"
من
وثق
بنفسه
ال
حتاجٌ
الى
مدح
الناس
اذٌ
،
و
من
طلب
الثناء
فقد
ّدل
على
ابهٌترا
ًف
مةٌق
نفسه
"
غوستاف
لوبون
Management of special cases
1. Status epilepticus:
mortality 4-5%
1)
ABC
2)
Put the patient in left lateral position
3)
Control fit and stabilize the patient
4)
ECG , Respiratory function should be monitored
5)
Put i.v. cannula
6)
At the same time take short history and do brief examination and check the
temperature and blood pressure
7)
Draw blood sample and do important diagnostic Investigations:
Blood sugar
S. electrolyte(sodium , calcium, phosphate, magnesium)
Lumbar puncture, anticonvulsant drug level , urine study for
toxicology screen and arterial blood gases if indicated
EEG if indicated
8)
Start glucose-containing IV
fluid
9)
Give 50% glucose if serum glucose low (1–2 mL/kg
)
10)
Diazepam 0.3mg/kg i.v to control convulsion
11)
If I.v line is not available give 0.5mg/kg of Diazepam rectally
12)
Buccal and nasal midazolam is another option
13)
If you find correctable cause treat it.(like hypoglycemia <3mmol treat it
with 5ml /kg of 10% dextrose by rapid infusion
14)
Reassess the patient for response within 5-10 min
15) Other Pharmacological therapy:
1. If no response use Fosphynitoin 15-20 mg /kg as second line treatment
2. I.v Phenobarbital at loading dose of 15-20 mg /kg is third line drug if
seizure persist intravenous sodium valproate can be use
3. If no response use one of the following:
1) Diazepam infusion
2) Constant infusion of medazolam or propofol
3) Barbiturate coma use thiopental in an ICU use ventilator and
continuous EEG monitoring
4) Paraldehyde i.v or rectal
5) General anesthesia use halothane or isoflurane
16) correct the precipitated factors
75
2. Status Asthmaticus:
1)
ABC
2)
Close monitoring of clinical status, O
2
saturation
3)
O
2
by a mask or nasal prongs
4)
Weigh the child rapidly
5)
place i.v. cannula
6)
At the same time take a short history and do a brief examination and check the
temperature and respiratory rate and look for signs of respiratory distress and
auscultate the chest rapidly
7)
Draw blood sample and do important Investigations
8)
Inhaled short acting B- agonist like salbutamol every 20 min for one hour
9)
Systemic glucocorticoid (methylprednisolone 1mg/kg 6hourly or hydrocortisone
i.v or orally)
10)
nenulized ipratopium may added to B- agonist
11)
Reassess the patient (calculate respiratory rate , look for signs of respiratory
distress and auscultate the chest for wheeze and air entry )
12)
If improved discharge him on inhaled B-agonist and oral steroid (like
prednisolone for 5 days)
13)
Admit the child to the hospital if:
1. No improvement after 1-2 hrs of initial treatment
2. No improvement in peak expiratory flow (PEF) (less than 70%)
3. O
2
saturation less than 92%
4. Prolong symptoms before emergency visit
14)
Hospital management :
1. O
2
2. Inhaled short acting B- agonist and Systemic glucocorticoid iv or orally
3. Iv fluid
If no response give:
4. Iv theophylline 5-10mg/kg i.v over 1 hr followed by infusion 1.1 mg /kg
per hr (age 1-9 yrs) or 0.7 mg/kg per hr (10 yrs to adult)
5. Inhaled heliox: 70% hhelium- 30% O
2
improvement within 20 min
6. Iv. magnesium sulfate 25-40 mg /kg over 30 min (monitor B. pr every 15
min. during infusion)
7. Mechanical ventilation if impending respiratory failure
8. Halothane inhalation during mechanical ventilation
9. Reassess the patient for response
"
ذٍّؼر
ذّقٌا
ِٓ
ضشصبسٌا
،
ٚ
االعزٙبد
ِٓ
ْىغالٌا
،
ٚ
زٛامغٌا
ِٓ
زىجشٌّا
،
ٚ
غش٠تٌا
ٟٔأ
ال
الش
ًثفن
٘إالء
ٓ١ٍّؼٌّا
"
لبران
لٌلخ
لبران
"
ه رب٠غشٔاشف
ٟٔصد ذٌاٚ
76
"
١ظٌ
ِٓ
قؼتٌا
ْأ
رؼضش
ٍٝػ
،ؾم١مخٌا
ٚ
ٓىٌ
خٍىؾٌّا
ىجشٌٜا
ٟ٘
أال
رؾبٚي
ٙشٚةٌا
ٙبِٕ
ئرا
ٚعذرٙب
"
انٌت
للسوت
3. Acute bronchiolitis:
1)
Give cool humidified O
2
by head box or O
2
tent
2)
elevates head and chest put the child in 30 degree with neck
extended
3)
assess the child condition (respiratory rate, signs of respiratory
distress, pulse oximetry for O
2
saturation) may need for admission
4)
May need to NG tube to avoid aspiration
5)
Keep the child nil by mouth
6)
Maintain with iv fluid give 75% of maintenance
7)
Endotracheal intubation if there is risk of further respiratory
decompensation
8)
Adjuvant treatment :
1. Bronchodilators: short acting β-agonist
2. Nebulized epinephrine
has same effect of short acting β-agonist
3. Corticosteroids : methylprednisolone 1mg/kg
4. Ribavirin: for CHD or Chronic lung dz.
5. Antibiotics if there is secondary bacterial pneumonia
11) Avoid sedative it may depress respiratory derive
Prevention :
1. I.V immunoglobulin (RSV-IVIG, RespiGam)
2. Palivizumab monoclonal Antibody for:
Child <2 yrs with:
Chronic lung dz.
Prematurity
3. Hand Washing
77
"
لقد
اخترعنا
الفن
ًلك
ال
نموت
من
قةٌقحلا
"
كٌردٌرف
تشهٌن
4. Pneumonia :
Note: this management is not according to the ARI program (see page 113)
1-
Send chest X-ray to confirm the diagnosis and detect complications
2-
Put iv line and Draw blood sample and do important Investigations(WBC, blood
culture, cold agglutination, isolation of the Bacteria or the virus.
3-
Treatment of suspected bacterial pneumonia is based on the presumptive cause and
the clinical appearance of the child. For mildly ill children who do not require
hospitalization, amoxicillin is recommended. In communities with a high percentage
of penicillin-resistant pneumococci, high doses of amoxicillin (80–90 mg/kg/24 hr)
should be prescribed. Therapeutic alternatives include cefuroxime axetil or
amoxicillin/clavulanate. For school-aged children and in those in whom infection with
M. pneumoniae or C. pneumoniae (atypical pneumonias) is suggested, a macrolide
antibiotic such as azithromycin is an appropriate choice. In adolescents, a respiratory
fluoroquinolone (levofloxacin, gatifloxacin, moxifloxacin, gemifloxacin) may be
considered for atypical pneumonias.
4-
The empirical treatment of suspected bacterial pneumonia in a hospitalized child
requires an approach based on the clinical manifestations at the time of presentation.
Parenteral cefuroxime (150 mg/kg/24 hr), cefotaxime, or ceftriaxone is the mainstay
of therapy when bacterial pneumonia is suggested. If clinical features suggest
staphylococcal pneumonia (pneumatoceles, empyema), initial antimicrobial therapy
should also include vancomycin or clindamycin.
5-
If viral pneumonia is suspected, it is reasonable to withhold antibiotic therapy,
especially for those patients who are mildly ill, have clinical evidence suggesting viral
infection, and are in no respiratory distress. Up to 30% of patients with known viral
infection may have coexisting bacterial pathogens. Therefore, if the decision is made
to withhold antibiotic therapy based on presumptive diagnosis of a viral infection,
deterioration in clinical status should signal the possibility of superimposed bacterial
infection and antibiotic therapy should be initiated.
6-
Admit the child if:
Age < 6 months
Sickle cell anemia with acute chest syndrome
Multiple lobe involvement
Immunocompromised state
Toxic appearance
Severe respiratory distress
Requirement for supplemental oxygen
Dehydration
Vomiting
No response to appropriate oral antibiotic therapy
Noncompliant parents
Supportive care
O
2
if needed
If the child has fever (≥39 °C or ≥102.2 °F) which appears to be causing distress, give
paracetamol.
Encourage the child to eat and drink. oral zinc (20 mg/day) helps accelerate recovery
from severe pneumonia
IV fluid if needed, Avoid frequent examinations or disturbing the child unnecessarily
If there is difficulty in swallowing, nasogastric feeding is required.
78
"
ً لْا
وضٍُٟؼٌا غِ ًّؼٌا ً٠
س
ً١ٍل ًٙغٌا غِ ٖش١ضو ْا بّو ،
"
ؽذ٠ش ؽش٠ف
5. Croup :
1)
Ask about patient's name ,age
2)
You should know the weight of the child
3)
Use cool mist by tent or face mask
4)
Nebulized epinephrine or Racemic epinephrine decrease
laryngeal and mucosal edema
Indications are:
1-
Moderate to severe stridor at rest
2-
The need for intubation
3-
Respiratory distress and hypoxia
4-
No response to cool mist
5)
Corticosteroid decrease edema use Iv or I.m dexamethasone
0.6 mg/kg or single dose of prednisolone 1mg/kg
6)
Heliox have same effect of neubulized epinephrine
7)
May need for endotracheal intubation
8)
There is no indication for antibiotics and sedative
9)
Ensure adequate fluid intake
Indication for hospitalization
1- Progressive stridor
2- Sever stridor at rest
3- Respiratory distress, hypoxia, cyanosis
4- Depress mental status
79
"
بعض
الحقائق
ائلة
ًف
حلمها
،
لدرلة
ان
كٌلع
ن
تلتهد
ًف
طالع
نٌرخلآا
هاٌلع
جٌردتلاب
"
من كتاب حدائق الحكمة
–
ل احمدٌبن
6. Acute epiglottitis
,
:
Is a medical emergency and warrants immediate treatment
1-
Keep the child in a sitting position
2-
Give cool humidified O
2
by mask
3-
Summon immediate help from anaesthetist or intensivist
4-
Don’t examine the larynx unless an anesthetist is present
and able to intubate
5-
Endotracheal intubation must be performed immediately
for all patients
6-
If intubation is difficult ventilate the child with bag-valve-
mask
7-
If ventilation is impossible perform cricothyrotomy or
tracheostomy
8-
Blood culture and epiglottis swab should be obtained
9-
Start with appropriate intravenous antibiotics to cover
H influenzae and Streptococcus species (parenteral
ceftriaxone sodium initial dose 100 mg /kg with a second
dose 50mg/kg after 24 hrs)
10-
Intravenous antibiotics should be continued for 2–3
days, followed by oral antibiotics to complete a 10-day
course.
11-
I.v fluid 60% of the maintenance
12-
Extubation can usually be accomplished in 2–3 days
13-
Corticosteroid and neubulized epinephrine are in
effective
80
"
ذّقٌا
...
ٓف
ُػظ١
ِٓ
ْٕٛف
َىالٌا
"
امٌلو
تٌرن
7. Bacterial meningitis :
* for CSF finding see table 12 (page 147)
1-
Control seizure if present use phenytoin
2-
Confirm the diagnosis by LP and CSF Analysis and culture
3-
Dexamethasone 0.6 mg/kg/day (0.15 mg/kg/dose given every 6
hr) for 2 days give it before the antibiotics by 1-2 hrs .
corticosteroid recipients have a shorter duration of fever, lower
CSF protein and lactate levels, and a reduction in sensorineural
hearing loss.
4-
Antibiotics therapy: *For more details see table 13 (page 148)
Vancomycin 60 mg /kg/24hr given every 6 hrs
In combination with
Cefotaxime 200 mg /kg/24hr given every 6 hrs
or
Ceftriaxone 100 mg /kg/24hr once per day or in divided doses
If the pt. is allergic to β-lactam use:
Chloramphenicol 100 mg /kg/24hr given every 6 hrs
5-
Duration of therapy is 7 days for meningococcal infections, 10
days for Haemophilus influenza or pneumococcal infection, and
14–21 days for other organisms.
Supportive care :
Treat shock if present
Treat DIC if present
Treat anemia if present
Give antipyretics for fever
Treat dehydration with I.v fluid 50% of the maintenance
Treat raise intracranial pressure if present
6-
All patient required hearing assessment 6-8 wks after discharge
For viral meningitis :
Use supportive treatment with 30 mg/kg /day of acyclovir for 14
days if HSV infection
81
"
تٍمٌٍ
ْػ١ٛ
ال
٠ذسوٙب
ًؼمٌا
"
تشارلز
بارخرست
8. Heart failure:
1-
Ask about patient's name ,age, sex
2-
You should know the weight of the child
3-
Support the child in a semi-seated position with head and shoulders elevated and
lower limbs dependent.
4-
Give cool humidified O
2
by nasal prongs or mask if the child has a respiratory rate
of
70cycle/min, shows signs of respiratory distress, or has central cyanosis.
5-
Do important investigations: Chest X-ray ,ECG, Echocardiography
6-
Reduction of preload
diuretics : furosemide 1mg/kg/dose PO or I.V up to qid
Add hydrochlorthiazide 2mg/kg/day bid
7-
Inotropic drugs:
Digoxin : rapid digitization 0.04 mg/kg
Maintenance(slow digitization 0.01 mg/kg /day)
Give half dose in preterm baby or patient with myocarditis
75% of this dose if given I.V
Dopamine or dobutamine 5-28 mcg/kg /min
8-
After load reduction
ACE inhibitors
Captopril 0.1 mg /kg/d PO q8h
Enalapril 0.1 mg/kg/d PO bid
9-
Sedative like chloral hydrate 20mg/kg/dose
10-
Morphine 0.1mg/kg/dose
11-
Sodium bicarbonate may use to correct sever acidosis
12-
Antibiotics if there is chest infection
13-
Packed blood cell are given in severe anemia
14-
Improve nutrition
Supportive care
• Avoid the use of IV fluids, where possible.
• Relieve any fever with paracetamol to reduce the cardiac workload.
Monitoring
The child should be checked by nurses every 6 hours (3-hourly whilst on oxygen
therapy) and by doctors once a day. Monitor both respiratory and pulse rates, liver
size, and body weight to assess the response to treatment. Continue treatment until
the respiratory and pulse rates are normal and the liver is no longer enlarged.
82
"
ال
رخف
ِٓ
ْأ
رخطٛ
خطٛح
وج١شح
بِذٕػ
رنطش
هٌزٌ
..
ئر
ال
هٕىّ٠
ْأ
رؼجش
فغٛح
ٓثمفضر١
ٓفغ١شر١
"
دٌفٌد
دٌول
لورج
9. SVT
1)
Vagal stimulation by submersion of the face in iced saline (in older children) or by
placing an ice bag over the face (in infants) may abort the attack. To abolish the
paroxysm, older children may be taught vagotonic maneuvers such as the Valsalva
maneuver, straining, breath holding, drinking ice water, or adopting a particular
posture.
2)
When these measures fail, several pharmacologic alternatives are available:
In stable patients, adenosine (0.1mg/kg diluted by normal saline )by rapid
intravenous push is the treatment of choice because of its rapid onset of action and
minimal effects on cardiac contractility. The dose may need to be repeated rapidly
(given at 2 min. intervals, increase the dose by 0.05 mg /kg up to 0.3 mg/kg (max 18
mg).
Other drugs that have been used for initial treatment of SVT include infusions of
phenylephrine (Neo-Synephrine) or edrophonium (Tensilon), which increase vagal
tone through the baroreflex, as well as the antiarrhythmic agents quinidine,
procainamide, and propranolol. Calcium channel blockers such as verapamil have
also been used in the initial treatment of SVT in older children. Verapamil may
reduce cardiac output and produce hypotension and cardiac arrest in infants
younger than 1 yr; it is therefore contraindicated in this age group.
3)
In urgent situations when symptoms of severe heart failure have already occurred,
synchronized DC cardioversion 0.5–2 W-sec/kg (average 1J/kg) is recommended as the
initial management .
4)
Once the patient has been converted to sinus rhythm, a longer acting agent is selected
for maintenance therapy. In patients without an antegrade accessory pathway, digoxin
or propranolol is the mainstay of therapy. In children with evidence of pre-excitation
(WPW syndrome), digoxin or calcium channel blockers may increase the rate of
anterograde conduction of impulses through the bypass tract and should be avoided.
These patients are usually managed in the long term with propranolol. In patients with
resistant tachycardias, procainamide, quinidine, flecainide, propafenone, sotalol, and
amiodarone have all been used. It should be recognized that most antiarrhythmic agents
could have proarrhythmic and negative inotropic effects. Flecainide in particular should
be limited to use in patients with otherwise normal hearts. If cardiac failure occurs
because of prolonged tachycardia in an infant with a normal heart, cardiac function
usually returns to normal after sinus rhythm is reinstituted, although it may take days
to weeks.
5)
Twenty-four hour electrocardiographic (Holter) recordings are useful in monitoring the
course of therapy and in detecting brief runs of asymptomatic tachycardia. A brief
assessment of arrhythmia control can be made at the bedside with transesophageal
pacing. More detailed electrophysiologic studies performed in the cardiac
catheterization laboratory are often indicated in patients with refractory SVTs.These
studies are necessary prerequisites to radiofrequency ablation.
6)
Radiofrequency ablation of an accessory pathway is another treatment option
commonly used in patients with re-entrant rhythms. It is often used electively in
children and teenagers, as well as in patients who require multiple agents or find drug
side effects intolerable or for whom arrhythmia control is poor.
83
"
زٌمتٌ
اللراح
المشهور
نٌعب
صقر
و
قلب
سد
و
دٌ
دةٌس
"
وناردٌل
تٌار
10. Hypercyanotic (tet) spells
1-
You should know the weight of the child
2-
Put an I.v cannula and draw blood for important
investigation ( Hb%, PCV, Blood sugar, blood
gas analysis, U&E)
3-
Place the child on his back or over the mother's
shoulder in knee-chest position
4-
Give O
2
by mask or nasal prongs
5-
Give morphine
0.2 mg/kg i.m
6-
Na-bicarbonate in sever acidosis
7-
β- blockers like propranolol 0.2-0.5 mg/kg/12hr
8-
in extreme cases child may need i.v fluid
replacement , intubation and positive pressure
ventilation
9-
phenylephrine may be of benefit in extreme cases
10-
Stabilize general condition of the patient correct
hypoglycemia, Acidosis, electrolyte changes
11-
Monitor child's condition
12-
definitive treatment is surgical correction by total
correction (usually performed in the first 2 yrs of
life)
or palliative surgery (Blalock-Taussing operation)
84
"
ؽبٚي
أال
رغشق
فٟ
بدٍِٛؼٌّا
ٚ
ذٔأ
رجؾش
ٓػ
ؼشفخٌّا
"
ًانطون
لوٌلناد
11. Shock
Hemorrhagic shock
1) Control external bleeding
2) O
2
by mask
3) Insert 2large bore cannulae
4) With draw blood for blood group and cross match
5) Rapidly infuse 20 ml/kg of crystalloid or colloid solution
6) Infuse blood if available
7) Insert foley catheter
8) Monitor blood pressure, heart rate , oxygenation, urine out put
9) Calcium and fresh frozen plasma are needed if 1-2 blood volumes
have been transfused
Septicaemic shock
1) O
2
by mask
2) Insert 2large bore cannulae
3) With draw blood for blood group and cross match
4) Collect blood for culture
5) Rapidly infuse 20 ml/kg of crystalloid or colloid solution
6) Give empirical antibiotics I.v like cefotaxime 50mg/kg 4 hourly max 2g
7) Dopamine 5-20 mcg /kg may be needed
8) Monitor blood gases
9) Mechanical ventilation may required
10)
Defer Lumpar puncture till the child has been stabilized
85
"
رذ واحتج الىٌظن نكت تئش نمع نغتساو ذرٌم نكت تئش نم ىلا نسح
رذٌس نكت تئش نم
"
نٌنمؤملا رٌم
(
ه السالمٌلع
)
12. Dehydration
No dehydration:
Plan A
➤Treat the child as an outpatient.
➤Counsel the mother on the 4 rules of home treatment:
1)
give extra fluid
2)
give zinc supplements
3)
continue feeding
4)
give advice on when to return.
1) Give extra fluid, as follows:
— If the child is being breastfed, advise the mother to breastfeed frequently and for
longer at each feed. If the child is exclusively breastfed, give ORS solution or clean
water in addition to breast milk. After the diarrhea stops, exclusive breastfeeding
should be resumed, if appropriate to the child’s age.
— In non-exclusively breastfed children, give one or more of the following:
• ORS solution
• food-based fluids (such as soup, rice water and yoghurt drinks)
• clean water. To prevent dehydration from developing, advise the mother to give
extra fluids—as much as the child will take:
• for children <2 years, about 50–100 ml after each loose stool
• for children 2 years or over, about 100–200 ml after each loose stool.
Tell the mother to give small sips from a cup. If the child vomits, wait 10 minutes
and then give more slowly. She should continue giving extra fluid until the
diarrhoea stops. Teach the mother how to mix and give ORS solution and give her
two packets of ORS to take home.
2)Give zinc supplements
— Tell the mother how much zinc to give:
Up to 6 months 1/2 tablet (10 mg) per day 6 months and more 1 tablet (20 mg) per
day for 10–14 days
— Show the mother how to give the zinc supplements:
• Infants, dissolve the tablet in a small amount of clean water, expressed
milk or ORS.
• Older children, tablet can be chewed or dissolved
— Remind the mother to give the zinc supplements for the full 10–14 days.
3)Continue feeding
4)Advise the mother on when to return
Follow-up
➤Advise the mother to return immediately to the clinic if the child becomes more sick, or
is unable to drink or breastfeed, or drinks poorly, or develops a fever, or shows blood in
the stool. If the child shows none of these signs but is still not improving, advise the
mother to return for follow-up at 5 days.
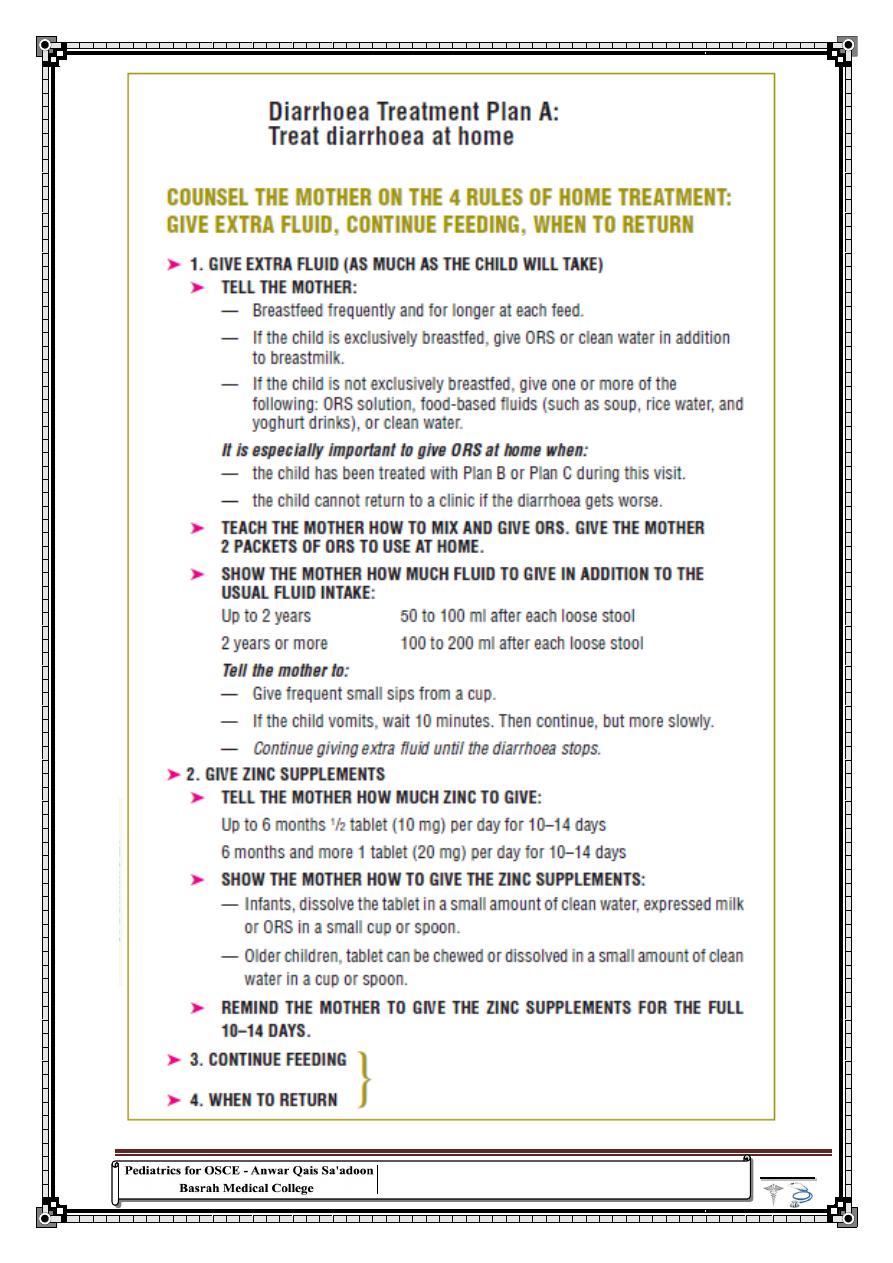
86
"
نت اآل
هٌلع نوكتس امم ةٌم لقاو هٌلع تنك امم ةٌم رثك ن
"
ه رب٠غشٔاشف
ًوالت دزن
87
"
١ظٌ
ٍُزؼٌا
ْا
رؾفع
ؾمباكٌا
ٓػ
ظٙش
تٍل
ًث
ْأ
رؼشف
براِ
ًرفؼ
ثٙب
"
رولر
تسٌرف
Some dehydration:
Plan B
➤In the first 4 hours, give the child the following approximate amounts
of ORS solution, according to the child’s weight (or age if the weight is
not known) However, if the child wants more to drink, give more.
➤Show the mother how to give the child ORS solution, a teaspoonful
every 1–2 minutes if the child is under 2 years; frequent sips from a cup
for an older child.
➤Check regularly to see if there are problems.
• If the child vomits, wait 10 minutes; then, resume giving ORS solution
more slowly (e.g. a spoonful every 2–3 minutes).
• If the child’s eyelids become puffy, stop ORS solution and give plain
water or breast milk.
➤Advise breastfeeding mothers to continue to breastfeed whenever the
child wants.
➤If the mother cannot stay for 4 hours, show her how to prepare ORS
solution and give her enough ORS packets to complete the rehydration at
home plus enough for 2 more days.
➤Reassess the child after 4 hours, checking for signs of dehydration
(Note: Reassess the child before 4 hours if the child is not taking the ORS
solution or seems to be getting worse.)
If there is no dehydration, teach the mother the four rules of home
treatment:
(i) give extra fluid
(ii) give zinc supplements for 10–14 days
(iii) continue feeding
(iv) return if the child develops any of the following signs:
1) drinking poorly or unable to drink or breastfeed
2) becomes more sick
3) develops a fever
4) has blood in the stool.
If the child still has some dehydration, repeat treatment for another
4 hours with ORS solution, as above, and start to offer food, milk or
juice and breastfeed frequently.
If signs of severe dehydration have developed for treatment.
Give zinc supplements
➤Tell the mother how much zinc to give Up to 6 months 1/2 tablet (10
mg) per day 6 months and more 1 tablet (20 mg) per day for 10–14 days
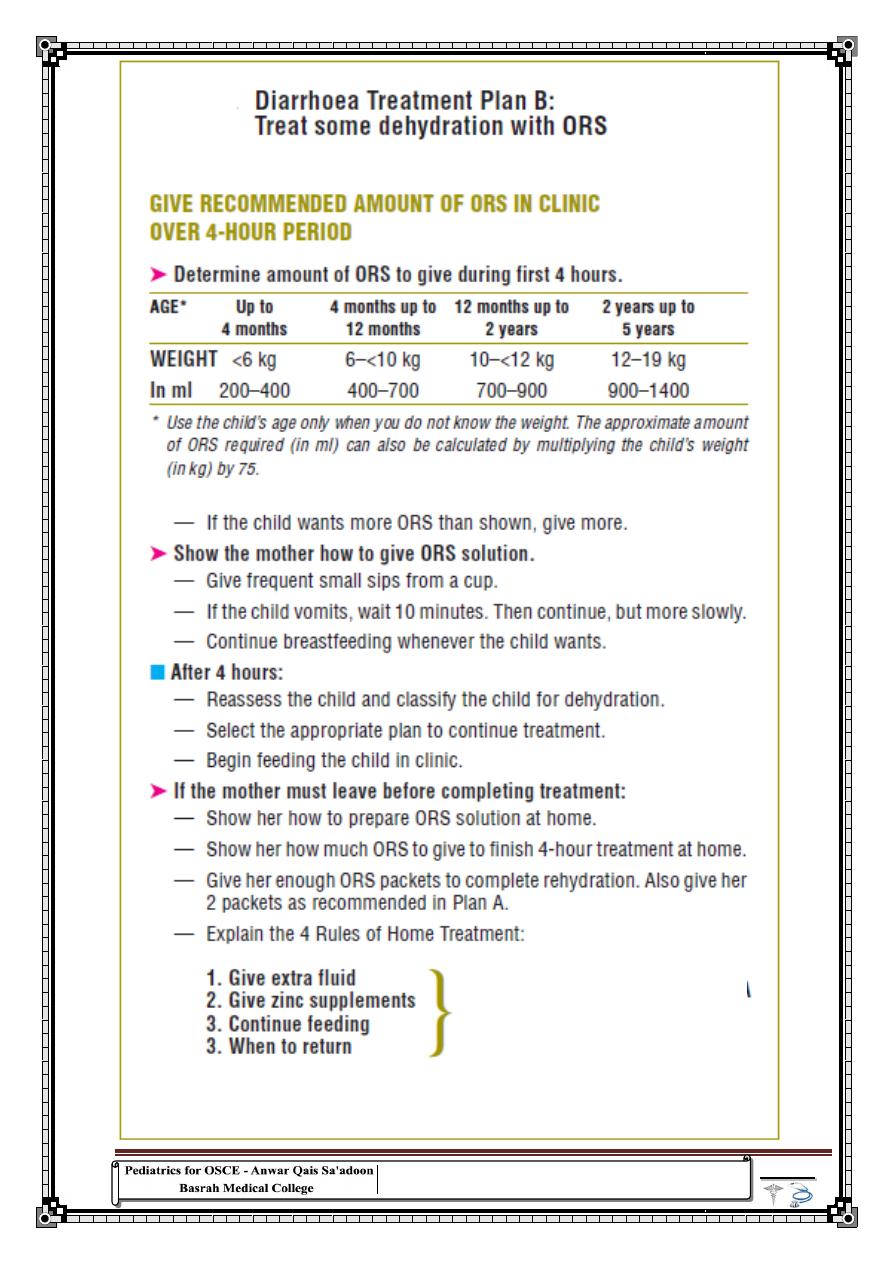
88
"
دراك
لهلك
خطوة
رةٌبك
ًف
اتلاذ
المعرفة
"
نٌماٌنب
ًلٌئارزد
89
"
العلم
كبر
من
ن
حاطٌ
به
،
فخذوا
من
كل
ش
يء
حسنه
"
نٌرٌس نبا
Severe dehydration:
Plan C
Children with severe dehydration should be given rapid IV rehydration followed by
oral rehydration therapy.
➤Start IV fluids immediately. While the drip is being set up, give ORS solution if
the child can drink. Note: The best IV fluid solution is Ringer's lactate Solution
(also called Hartmann’s Solution for Injection). If Ringer's lactate is not available,
normal saline solution (0.9% NaCl) can be used. 5% glucose (dextrose) solution on
its own is not effective and should not be used.
➤Give 100 ml/kg of the chosen solution divided
First, give 30 ml/kg in: Then, give 70 ml/kg in:
<12 months old 1 hour 5 hours
≥12 months old 30 minute 2and half hours
Repeat again if the radial pulse is still very weak or not detectable.
Monitoring
Reassess the child every 15–30 minutes until a strong radial pulse is present. If
hydration is not improving, give the IV solution more rapidly. Thereafter, reassess
the child by checking skin pinch, level of consciousness, and ability to drink, at least
every hour, in order to confirm that hydration is improving. Sunken eyes recover
more slowly than other signs and are less useful for monitoring. When the full
amount of IV fluid has been given, reassess the child’s hydration status fully
• If signs of severe dehydration are still present, repeat the IV fluid
infusion as outlined earlier. Persistent severe dehydration after IV rehydration is
unusual; it usually occurs only in children who pass large watery stools frequently
during the rehydration period.
• If the child is improving but still shows signs of some dehydration,
discontinue IV treatment and give ORS solution for 4 hours
If the child is normally breastfed, encourage the mother to continue breastfeeding
frequently. Where appropriate, encourage the mother to continue breastfeeding
frequently. Observe the child for at least 6 hours before discharge, to confirm that
the mother is able to maintain the child’s hydration by giving ORS solution. All
children should start to receive some ORS solution (about 5ml/kg/hour) by cup
when they can drink without difficulty (usually within 3–4 hours for infants, or 1–2
hours for older children). This provides additional base and potassium, which may
not be adequately supplied by the IV fluid. When severe dehydration is corrected,
prescribe zinc
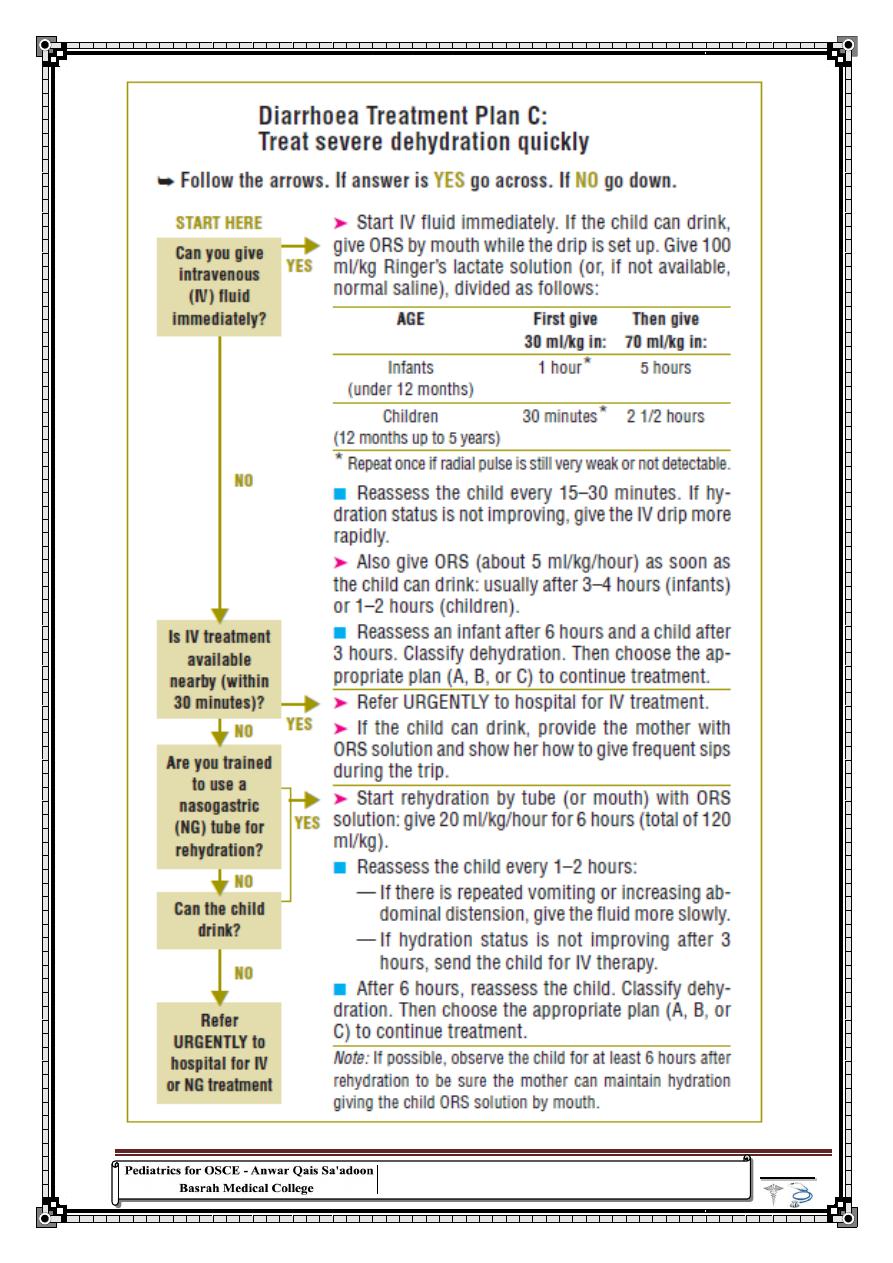
90
"
نماٌب
سعىٌ
اإلنسان
ًالذك
طٌسبتل
ما
و
معقد
،
سعىٌ
األحمق
دٌقعتل
ما
و
طٌسب
"
رالدٌل
لرومت
91
"
ٍُؼٌا
٘ٛ
زش٠بقٌا
نبدٌّا
ُّزغٌٍ
ًغٌٙبث
ٚ
خشافبدٌا
"
"
آدم
ثٌمس
13. Poisoning
Initial medical care
A- Prevention of Absorption
1. Emesis:
use syrup of ipcac 15-30 ml followed by liquid such as water .
its contraindicated in comatose patient, ingestion strong acid or base
2. Lavage:
should be done within one hour
3. Charcoal:
most effective and safe procedure give as s water slurry with a minimum
dose of 15-30 g , 2-6 hrs
.
The dose of charcoal is 1–2 g/kg (maximum, 100 g) per
dose. Repeating the dose of activated charcoal may be useful for those
agents that slow passage through the gastrointestinal (GI) tract. When
multiple doses of activated charcoal are given, Charcoal dosing is
repeated every 2–6 hours until charcoal is passed through the rectum.
4. Cathartic
s
Like sorbet (max 1g/kg) magnesium sulfate, sod citrate. despite their
widespread use, cathartics do not improve outcome. The use of cathartics
should therefore be avoided.
5. Whole Gut Lavage
Whole bowel lavage uses an orally administered, non absorbable
hypertonic solution such as CoLyte. The use of this procedure in
poisoned patients remains controversial. Preliminary recommendations
for use of whole bowel irrigation include poisoning with sustained-
release preparations, mechanical movement of items through the bowel
(eg, cocaine packets, iron tablets), and poisoning with substances that are
poorly absorbed by charcoal (eg, lithium, iron). Underlying bowel
pathology and intestinal obstruction are relative contraindications to its
use. Consultation with a certified regional poison center is recommended.
Enhancement of Excretion
1. Forced diuresis
: helpful in salicylate ingestion
2. Dialysis
92
"
من
ال
تفوقٌ
على
معلمه
كنٌ
اًاذٌملت
اًاهفات
"
وناردوٌل
ًدافنش
Hemodialysis (or peritoneal dialysis if hemodialysis is unavailable) is
useful in the poisonings listed below and in the general management of a
critically ill patient. dialysis is useful for thiophylline, Digoxin and
refractory salicylate intoxication.
3. Hemoperfusion over activated charcoal or resin helpful in:
thiophylline
,
salicylate intoxication
contraindicated in Digoxin, acetaminopgin
Aspirin and other salicylates poisoning
This can be very serious in young children because they rapidly become
acidotic and are consequently more likely to suffer the severe CNS
effects of toxicity. Salicylate overdose can be complex to manage.
■ These cause acidotic-like breathing, vomiting and tinnitus.
1)
Give activated charcoal if available 1-2 g/kg.
Note: that salicylate tablets tend to form a concretion in the stomach
leading to delayed absorption, so it is worthwhile giving several doses
of charcoal. If charcoal is not available and a severely toxic dose has
been given, then perform gastric lavage or induce vomiting.
2)
Give IV sodium bicarbonate 1 mmol/kg over 4 hours to correct
acidosis and to raise the pH of the urine to above 7.5 so that salicylate
excretion is increased.
3)
Give supplemental potassium
(20-40 ml/L)
even the serum K
+
is normal
4)
Monitor urine and plasma PH hourly.
5)
do important other investigations like:
S. K
+
, PT, S.GPT, S.GOT, TSB, Measure level of Salicylate
6)
Give IV fluids at maintenance requirements unless child shows signs of
dehydration in which case give adequate rehydration.
7)
Monitor blood glucose every 6 hours and correct as necessary
8)
Give vitamin K 10mg IM or IV.
9)
Refractory salicylate intoxication may benefit from dialysis.
10)
Charcoal hemoperfusion
93
"
ال
ولدٌ
شئ
صعب
اًاٌلمع
اذا
قمت
مهٌسقتب
الى
عمال
رةٌغص
"
نري
فورد
Paracetamol poisoning
Table 5 -- Classic Stages in the Clinical Course of Acetaminophen Toxicity
STAGE TIME AFTER
INGESTION
CHARACTERISTICS
I
0.5–24 hr
Anorexia, nausea, vomiting, malaise, pallor, diaphoresis
II
24–48 hr
Resolution of earlier symptoms; right upper quadrant abdominal pain
and tenderness; elevated bilirubin, prothrombin time, hepatic enzymes;
oliguria
III
72–96 hr
Peak liver function abnormalities; anorexia, nausea, vomiting, and
malaise may reappear
IV
4 days–2 wk
Resolution of hepatic dysfunction or complete liver failure
1)
If within 1 hour of ingestion give activated charcoal, if available, or induce vomiting UNLESS
an oral antidote may be required.
2)
Decide if antidote is required to prevent liver damage: ingestions of 150 mg/kg or more, or toxic
4 hour paracetamol level where this is available. Antidote is more often required for older children
who deliberately ingest paracetamol or when parents overdose children by mistake.
3)
If within 8 hours of ingestion give oral methionine or IV acetylcysteine. Methionine can be
used if the child is conscious and not vomiting (<6 years: 1 gram every 4 hours for 4 doses; 6
years or older: 2.5 grams every 4 hours for 4 doses).
4)
If more than 8 hours after ingestion, or the child cannot take oral treatment, give IV
acetylcysteine.
Petroleum compounds poisoning
Examples: kerosene, turpentine substitutes, petrol
1)
Do not induce vomiting or give activated charcoal as inhalation can
cause respiratory distress with hypoxaemia due to pulmonary oedema
and lipoid pneumonia. Ingestion can cause encephalopathy.
2)
chest x-ray may show infiltrates by 2-3hr after ingestion, and after
2-3wk may show pneumatocele
3)
Specific treatment includes:
oxygen therapy if respiratory distress
put the patient in left lateral position
observation
94
"
ْٕٛغٌا
٘ٛ
ْأ
ًرفؼ
ؾٟءٌا
شحِ
ثؼذ
شحِ
ٚ
رزٛلغ
ز١غخٔ
فخٍزخِ
"
البرت
نٌاتشنٌا
Organo-phosphorus and carbamate
compounds poisoning
Examples: organophosphorus – malathion, parathion, TEPP,
mevinphos (Phosdrin); and carbamates – methiocarb, carbaryl
These can be absorbed through the skin, ingested or inhaled.
The child may complain of vomiting, diarrhoea, blurred vision or
weakness. Signs are those of excess parasympathetic activation:
salivation, sweating, lacrimation, slow pulse, small pupils, convulsions,
muscle weakness/twitching, then paralysis and loss of bladder control,
pulmonary oedema, respiratory depression.
Treatment involves:
1)
Remove poison by irrigating eye or Washing skin (if in eye or on skin).
2)
Give activated charcoal if ingested and within 1 hour of the ingestion.
3)
Do not induce vomiting because most pesticides are in petrol-based
solvents.
4)
In a serious ingestion where activated charcoal cannot be given,
consider careful aspiration of stomach contents by NG tube (the airway
should be protected).
5)
If the child has signs of excess parasympathetic activation, then give
atropine 15–50 micrograms/kg IM (i.e. 0.015–0.05mg/kg) or by
intravenous infusion over 15 minutes. The main aim is to reduce
bronchial secretions whilst avoiding atropine toxicity. Auscultate the
chest for signs of respiratory secretions and monitor respiratory rate, heart
rate and coma score (if appropriate). Repeat atropine dose every 15
minutes until no chest signs of secretions, and pulse and respiratory rate
returns to normal.
95
"
اافذلبء
ُ٘
ئهٌٚا
ْبدسٌٕٚا
ٓز٠ٌا
بٌٕٔٛأغ٠
و١ف
ٓؾٔ
ُص
ْزظشٕٚ٠
بعّغٌ
غٛاةٌا
"
د
كاننغام
6)
Check for hypoxaemia with pulse oximetry, if possible, if giving
atropine as it can cause heart irregularities (ventricular arrythmias) in
hypoxic children.
7)
Give oxygen if oxygen saturation is less that 90%.
8)
If muscle weakness, give pralidoxime (cholinesterase reactivator)
25–50mg/ kg diluted with 15 ml water by IV infusion over 30 minutes
repeated once or twice, or followed by an intravenous infusion of 10 to 20
mg/kg/hour, as necessary.
Iron poisoning
(you need to read more than this)
Check for clinical features of iron poisoning: nausea, vomiting,
abdominal pain and diarrhoea. The vomit and stools are often grey or
black. In severe poisoning there may be gastrointestinal hemorrhage,
hypotension, drowsiness, convulsions and metabolic acidosis.
Gastrointestinal features usually appear in the first 6 hours and a child
who has remained asymptomatic for this time probably does not require
antidote treatment.
1)
Activated charcoal does not bind to iron salts, therefore consider giving
a gastric lavage if potentially toxic amounts of iron were taken.
2)
Decide whether to give antidote treatment. Since this can have side-
effects it should only be used if there is clinical evidence of poisoning.
3)
If you decide to give antidote treatment, give deferoxamine (50 mg/kg
IM up to a maximum of 1 g) by deep IM injection repeated every 12
hours;
4)
if very ill, give IV infusion 15 mg/kg/hour to a maximum of 80 mg/kg
in 24 hours.
96
"
ال
رغأي
بّػ
ٓىّ٠
الاهِضٌ
فٟ
فش٠كٌا
ّٗ٠ذمر
هٌ
..
اعأي
فغهٔ
بِ
ثٛعؼه
ّٗ٠ذمر
الاهِضٌ
"
كٌلام
لونسون
14.Snake bite
First aid
1)
Splint the limb to reduce movement and absorption of venom. If the
bite was likely to have come from a snake with a neurotoxic venom
2)
Apply proximal tourniquet loose enough to insert 2 fingers and allow
arterial blood flow.
3)
Clean the wound.
4)
Transport to hospital which has antivenom as soon as possible. If
snake has already been killed, take this with child to hospital.
5)
Avoid cutting the wound or applying ice to bite site.
Hospital care
1)
Insert large iv cannula and draw blood for investigations :
CBC, PT, PTT, Blood group, fibrinogen and FDP, RFT
2)
Give tetanus toxoid
3)
Treat shock, if present.
4)
Paralysis of respiratory muscles can last for days and requires
intubation and mechanical ventilation or manual ventilation (with a mask
or endotracheal tube and bag) by relays of staff and/or relatives until
respiratory function returns. Attention to careful securing of endotracheal
tube is important. An alternative is to perform an elective tracheostomy.
5)Antivenom
■ If there are systemic signs or severe local signs (swelling of more than
half of the limb or severe necrosis), give antivenom, if available
➤
Give monovalent antivenom if the species of snake is known. Give
polyvalent antivenom if the species is not known. Follow the directions
given on the antivenom preparation. The dose for children is the same as
for adults.
Deliver it with in 4 hrs (5 vials and repeated every 2 hrs) Give it more
slowly initially and monitor closely for anaphylaxis or other serious
adverse reactions.
Prepare IM epinephrine and chlorpheniramine and be ready if allergic
reaction occurs.
97
"
الكذبة
تسافر
حول
نصف
الكرة
ةٌضرلأا
قبل
ن
ترتدي
قةٌقحلا
حذائها
"
مارك
نٌوت
15. Acute renal failure:
1-
Ask about patient's name ,age
2-
You should know the weight of the child
3-
treat dehydration or shock by i.v crystalloid 20 ml/kg or by blood
if there is blood loss pt. should void with in 2hrs if fail indicate
intrinsic or post renal ARF
4-
diuretics therapy considered after adequacy of circulation
established
use furosemide 1-4 mg /kg /dose as single dose
if urine output isn’t improved use continuous infusion of
furosemide
5-
to increase renal blood flow use dopamine 3 ug/kg/min
6-
if no response diuretics is should stopped and fluid restriction
consider as the following 400ml/m
2
/day + urine output
Treatment of complication of ARF
Hyperkalemia (very important)
S.K
+
> 6 mEq/L
1- eliminate exogenous source of K
+
2- continuous ECG monitoring (wide QRS ,Tall T wave)
3- sodium bicarbonate 1mmol/kg I.v over 30 min
4- Na-polystyrene resine 1g/kg given orally or rectal may repeated
every 2 hrs
5-
Ca-gluconate 0.5-1 ml/kg I.v over 5-10 min
6-
Regular insulin 0.1 U/kg with 50% glucose 1g/kg over 1hr
7-
Persistent Hyperkalemia should managed by dialysis
98
"
ًتنته
تكٌرح
ثٌح
تبد
ةٌرح
نٌرخلآا
"
سكوٌتنوم
Metabolic acidosis
If severe give Na-bicarbonate I.V then orally
Hypocalcaemia
1- Low phosphate diet
2- Oral phosphate binder ( Ca-carbonate , Ca-acetate)
Hyponatremia
1- Fluid restriction
2- Hypertonic saline 3% for
Symptomatic hyponatremia (seizure ,lethargy)
S.Na < 120 mEq/L
Hypertension
1- Salt and water restriction
2- diuretics
3- antihypertensive agents
β- blockers like propranolol 0.5 mg/kg/12hr
menoxidil 0.5 mg/kg/12hr
nifedipine 0.5 mg/kg/dose bid
Anemia
if Hb% <7 g/dl use packed RBC slowly over 4-6 hrs
Indication of dialysis:
1- Volume overload with HT or pulmonary edema refractory to
diuretics therapy
2- Persistent Hyperkalemia
3- Sever metabolic acidosis unresponsive to treatment
4- Neurological symptoms (seizure, altered mental status)
5- B . urea > 100-150 mg/dl
6- Calcium/phosphorus imbalance with hypocalcemic tetany
99
"
التقدم
..
و
قدرة
اإلنسان
على
دٌقعت
البساطة
"
ثور
ردا لٌ
16. Diabetes Mellitus:
If pt. firstly present with hyperglycemia
1)
Admission of the pt. to the ward for DM control
2)
Apply sliding scale:
Date time RBS Urine sugar Insulin U note
Measure RBS every 6 hrs and see the reading if:
<90 mg/dl no need for insulin
90-180 mg/dl give 0.1 U/kg of insulin
180-270 mg/dl give 0.2 U/kg
270-360 mg/dl give 0.3 U/kg
>360 mg/dl give 0.4 U/kg
Notes:
1- The insulin used in this scale is soluble Insulin only
2- Night dose is 0.1 U/kg
3- The pt. must stay on this scale for 3 days
4- After 3 days count the total amount of insulin used and
divided it on 3 to calculate the maintenance dose of insulin
that the pt. will need after discharge
5- Use mixtard insulin after discharge
6- Give the dose half hr. before the meal
7- Give the pt 2/3 of this dose at morning and 1/3 at night
3- Educate the family about DM , complication , Insulin, diet.
patient may be firstly presented with DKA:
(See next page)
20% of diabetic pt. firstly present with DKA
Dx:
Clinical features( vomiting , abdominal pain,…)
RBS > 300
Ketonaemia, ketonuria
Low bicarbonate
Low PH
100
"
ضمفٌّا
...
٘ٛ
ِٓ
٠غزط١غ
ٍٗمػ
شالجخِ
فغٗٔ
"
رٌبلا
كامو
17. Diabetic Ketoacidosis (DKA)
1-
Ask about patient's name ,age, weight
2-
You must arrange a observation chart
3-
Confirm the diagnosis by RBS & urine for ketone bodies and sugar
4-
Admission to ICU
5-
Initial treatment
Successful therapy consistently includes the following:
Stabilization of the airway, respiration, restoration of circulatory
volume
Institution of insulin therapy to correct hyperglycemia and clear
ketoacidosis
Correction of fluid and metabolic abnormalities
Determination of the cause of diabetic ketoacidosis; rule out infection
Avoidance of complications of therapy, including cerebral edema,
hypokalemia, and hypoglycemia
6-
Rehydration is the main step of treatment The initial goal of fluid
resuscitation is to restore circulation, usually with a 10-20mL/kg bolus of
isotonic saline solution or Ringer lactate over 30 to 60 minutes then slow
rehydration from the 2
nd
hour until reduce the risk of cerebral edema using
0.45% NaCl the amount of which is calculated according to the following
formula: IV rate = 85ml/kg + maintenance - bolus divided by 23 hours to
replace the deficit
Maintenance (24 hr) = 100 ml/kg (for the 1st 10 kg) + 50 ml/kg (for the 2nd
10 kg) + 25 mL/kg (for all remaining kg)
7-
Insulin therapy
We begin with by infusion of 0.1 U/kg until blood sugar is less than 250
mg/dL (14 mmol/L) then we give 5% glucose water
8-
Potassium therapy
During therapy for diabetic ketoacidosis, serum level of potassium can
decrease as insulin therapy facilitates intracellular glucose uptake and with
potassium shift back into the intracellular compartment as acidosis resolves.
In anticipation of these shifts, one must begin potassium replacement early
in the course of therapy for diabetic ketoacidosis.
a-If the patient is urinating
101
"
ذّقٌا
...
٘ٛ
قذ٠كٌا
ا
ٛؽ١ذٌ
زٌٞا
ٌٓ
هٔٛخ٠
اًاذثأ
"
فٛؽ١ٛطٔٛو
b- potassium level is 5 mEq/L or less, potassium replacement is initiated
with up to 40 mEq/L added to the maintenance fluids. The goal is to
provide 2 to 5 mEq/kg/d. Patients with more marked deficits may need
potassium replacement at up to 0.5 mEq/kg/h. Potassium replacement
should be given as 50% potassium chloride and 50% potassium phosphate
9-
Bicarbonate therapy should be avoided unless severe acidosis (pH
<7.0) results in hemodynamic instability, or symptomatic hyperkalemia is
present
10-
Subsequent treatment
when diabetic ketoacidosis has been successfully controlled that’s to say
pH is greater than 7.3, bicarbonate level is greater than 15 mEq/L, glucose
less than 300 mg/dl, and the patient is ready to resume enteral intake The
insulin infusion can be discontinued this transition ideally occurs during the
day and before a meal. The insulin infusion must be continued for 30 to 60
minutes after the first subcutaneous dose is administered to allow for
delayed onset of action of the injected insulin. Calculation of an appropriate
subcutaneous dose is based on sliding scale in which insulin dose is divided
into 4 daily doses continued for 2-3 days as follows
Blood glucose level
Dose of insulin(soluble)
More than 360mg/dl
0.4u/kg
270-360mg/dl
0.3u/kg
180-270mg/dl
0.2u/kg
90-180mg/dl
0.1u/kg
90mg/dl
Not give insulin
11-
After that the patient should be shifted Outpatient Management
The dose should be divided into two daily injections, with two thirds of the
total daily dose given in the morning, 30 minutes before breakfast if using
regular insulin or at breakfast if using lispro or aspart, and one third given
in the evening, likewise 30 minutes before dinner if using regular or at
dinner if using lispro or aspart The ratio of insulin in the morning dose
should be two-thirds intermediate-acting insulin (NPH or Lente), and one-
third short-acting or fast-acting insulin, In the evening, one half of the
evening insulin dose should be given as intermediate-acting insulin (NPH or
Lente), and one half should be given as short-acting or fast-acting insulin
102
18.
Painful crisis of SCA
Specific therapies for pain vary, but generally include the use of
acetaminophen or a nonsteroidal agent early in the course of pain,
followed by acetaminophen with codeine and short- or long-acting oral
opioids, or hospitalization with IV administration of morphine or
morphine derivatives . The incremental increase and decrease in the use
of medication to relieve pain roughly parallels the 8 phases associated
with a chronology of pain and comfort In phase 1 (baseline), the patient is
free of pain. Phase 2 involves no pain, but the child may show prodromal
signs and symptoms of painful episodes, such as scleral icterus or fatigue.
During this phase, comfort measures can be used. Phases 3–7 involve
increasing and then decreasing levels of pain, including the pain start
point, phase 3, when acetaminophen with codeine or nonsteroidal
inflammatory agents may be used. Pain acceleration, phase 4, is often
associated with administering short- or long-acting morphine derivatives.
Peak pain experience, phase 5, is the point at which IV morphine may be
started and the patient is often admitted to the hospital. The average
hospital stay for children admitted for pain is 3–5 days. The pain starts to
decrease during phases 6 and 7, and the pain medication is slowly
decreased. In general, decreasing the opioid medication by 20% of the
starting dose should occur during the early morning hours, when the
caretaker, physician, or house staff is available to assess the effect of the
change in dose. Decreasing opioid administration in the afternoon or late
at night is not advisable because pain is often worse at night and the
primary health care provider is often not available to assess the effect of
the change in dose administration. In phase 8, pain resolution, the pain
decreases to a manageable level so that the child can be discharged from
the hospital.
Several myths exist about the treatment of pain in sickle cell anemia. The
concept that painful episodes in children should be managed without
opioids is without foundation and results in unwarranted suffering on the
part of the patient. There is no evidence that blood transfusion therapy
during an existing painful episode decreases the intensity or duration of
the episode. Blood transfusion should be reserved for patients who have a
decrease in hemoglobin, resulting in hemodynamic compromise, and for
patients with respiratory distress or a dropping hemoglobin concentration
with no expectation that a safe nadir will be reached.
"
من
خافٌ
من
األلم
،
تألمٌ
من
الخوف
"
لٌشٌم
مٌكٌا
دي
ًمونتان
103
"
ًؼمٌا
...
قجبػِ
ٛيّؾِ
ٍٝػ
شأطٌا
،
جؼلٌا
ٍّٗؾ٠
اًبئ١نِ
ٚ
جؼلٌا
ا٢خش
٠زشوٗ
طفأِ
"
ً هف١ٓثا
IV hydration does not relieve or prevent pain and is appropriate when the
patient is dehydrated or is unable to drink as a result of severe pain.
Concern about opioid dependency in children with sickle cell anemia
must never be used as a reason not to treat a child in pain. Patients with
multiple painful episodes requiring hospitalization within 1 yr or those
whose pain episodes require hospital stays of longer than 7 days should
be evaluated for comorbidities and psychosocial stressors that may
contribute to the frequency or duration of pain.
Hydroxyurea, a myelosuppressive agent, is the only effective drug proven
to reduce the frequency of painful episodes. Hydroxyurea raises the level
of Hb F and the hemoglobin level. Hydroxyurea usually decreases the
rate of painful episodes by 50%; it also decreases the rate of ACS
episodes and blood transfusions by approximately 50% in adults. In
children with sickle cell anemia, only a safety and feasibility trial of
hydroxyurea has been conducted. This study demonstrated that
hydroxyurea was safe and well tolerated in children older than 5 yr of
age. No clinical adverse events were identified. The primary laboratory
toxicities were limited to myelosuppression, which was reversed on
cessation of the drug. Given the short-term safety profile of hydroxyurea
in children and its established efficacy in adults, hydroxyurea is
commonly used in children with multiple painful episodes. Hydroxyurea
treatment begun in infancy may preserve splenic function, improve
growth, and reduce the incidence of ACS. The long-term toxicity
associated with hydroxyurea in children has not been established, and
there are theoretical concerns about the potential risk of leukemia and
unknown complications. The typical starting dose of hydroxyurea is 15–
20 mg/kg daily, with an increase in dose every 8 wk of 2.5–5.0 mg/kg, if
no toxicities occur, up to a maximum dose of 35 mg/kg. The therapeutic
effect of hydroxyurea may require several mo of treatment. Monitoring
children who are receiving hydroxyurea is labor-intensive, with initial
visits every 2 wk and then monthly, after a therapeutic dose has been
identified. Close monitoring of the patient requires a commitment by the
parents and the patient as well as diligence by a physician to monitor
toxicity.
104
"
غبػٌٕا
..
ٍُع
ال
رغزط١غ
مٍٗغر
ٚ
٠ذان
فٟ
ع١جه
"
لورج
وتٌلا
19. Management of transfusion reactions
If a transfusion reaction occurs, first check the blood pack labels and
patient’s identity. If there is any discrepancy, stop the transfusion
immediately and notify the blood bank.
Mild reactions (due to mild hypersensitivity)
Signs and symptoms:
■ itchy rash
Management:
➤slow the transfusion
➤give chlorphenamine 0.1 mg/kg IM, if available
➤continue the transfusion at the normal rate if there is no
progression of symptoms after 30 minutes
➤if symptoms persist, treat as moderate reaction .
Moderately severe reactions
(due to moderate hypersensitivity, nonhaemolytic reactions, pyrogens
or bacterial contamination
Signs and symptoms:
■ severe itchy rash ( urticaria )
■ flushing
■ fever >38 °C or >100.4 °F (Note: fever may have been present
before the transfusion)
■ rigors
■ restlessness
■ raised heart rate.
Management:
➤stop the transfusion, but keep the IV line open with normal saline
➤give IV 200 mg hydrocortisone, or chlorphenamine 0.25 mg/kg IM,
if available
➤give a bronchodilator, if wheezing
105
"
١خٌبضٌّا
..
ٟ٘
ْا
٠الؽع
ـؽخ
ْأ
سااؾخ
ٛسدٌا
ًأفن
ِٓ
ُبهّطٌا
زظٕزغ١ف
ْأ
ؽغبء
ٛسدٌا
ْع١ىٛ
ًأفن
"
نري
لوبس
مانكن
➤send the following to the Blood Bank: the blood-giving set that was
used, blood sample from another site, and urine samples collected
over 24 hours.
➤if there is improvement, restart the transfusion slowly with new
blood and observe carefully
➤if no improvement in 15 minutes, treat as life-threatening reaction,
and report to doctor in charge and to the Blood Bank.
Life-threatening reactions
(due to hemolysis, bacterial contamination and septic shock, fluid
overload or
anaphylaxis)
Signs and symptoms:
■ fever >38 °C or >100.4 °F (note: fever may have been present
before the transfusion)
■ rigors, restlessness
■ raised heart rate, fast breathing
■ black or dark red urine (haemoglobinuria)
■ unexplained bleeding, pallor, jaundice
■ confusion
■ collapse.
Note that in an unconscious child, uncontrolled bleeding or shock
may be the only signs of a life-threatening reaction.
Management:
➤stop the transfusion, but keep the IV line open with normal saline
➤maintain airway and give oxygen
➤give epinephrine (adrenaline) 0.01 mg/kg body weight (equal to 0.1
ml of 1 in 10 000 solution
➤treat shock
➤give IV 200 mg hydrocortisone, or chlorpheniramine 0.1 mg/kg
IM, if available
➤give a bronchodilator, if wheezing
➤report to doctor in charge and to blood laboratory as soon as
possible
➤maintain renal blood flow with IV furosemide 1 mg/kg
➤give antibiotic as for septicaemia.
106
"
ٍُؼٌّا
...
٘ٛ
ـؾخٌا
زٌٞا
هٍؼغ٠
ال
رؾزبط
١ٌٗا
اًب١غ٠سذر
"
توماس
كاروترس
20.Management infant of diabetic mother
Treatment of infants of diabetic mothers should be initiated before birth by frequent
prenatal evaluation of all pregnant women with overt or gestational diabetes, by
evaluation of fetal maturity, by biophysical profile, by Doppler velocimetry, and by
planning the delivery of these infants in hospitals where expert obstetric and
pediatric care is continuously available. Periconception glucose control reduces the
risk of anomalies and other adverse outcomes, and glucose control during labor
reduces the incidence of neonatal hypoglycemia. Women with Type 1 diabetes who
have tight glucose control during pregnancy (average daily glucose levels <95
mg/dL) deliver infants with birthweights and anthropomorphic features that are
similar to those of infants of nondiabetic mothers. Treatment of gestational diabetes
also reduces complications; dietary advice, glucose monitoring, and insulin therapy
as needed decrease the rate of serious perinatal outcomes (death, shoulder dystocia,
bone fracture, or nerve palsy). Women with gestational diabetes may also be treated
successfully with glyburide, which may not cross the placenta. In these mothers, the
incidence of macrosomia and neonatal hypo glycemia is similar to that in mothers
with insulin-treated gestational diabetes. Regardless of size, all infants of diabetic
mothers should initially receive intensive observation and care.
Asymptomatic infants should have a blood glucose determination within 1 hr
of birth and then every hour for the next 6–8 hr
if clinically well and normoglycemic, oral or gavage feeding with breast milk
or formula should be started as soon as possible and continued at 3 hr
intervals.
If any question arises about an infant's ability to tolerate oral feeding, the
feeding should be discontinued and glucose given by peripheral intravenous
infusion at a rate of 4–8 mg/kg/min.
Hypoglycemia should be treated, even in asymptomatic infants, by frequent
feeding and/or intravenous infusion of glucose.
Bolus injections of hypertonic glucose should be avoided because they may cause
further hyperinsulinemia and potentially produce rebound hypoglycemia.
Managing
Hypoglycemia
Hypomagnesemia
respiratory distress syndrome
polycythemia
107
"
جذعٌّا
..
٘ٛ
ًسع
أوضش
ثذاا١خ
،
أوضش
اًاشنؾر
،
أوضش
اًاش١ِذر
،
اوضش
اًبٕٔٛع
،
ٚ
أوضش
١خٔلامػ
ِٓ
أٞ
ًسع
ػبد
ٞ
"
فرانك
براون
21. Management infant with hypoglycemia
1) When symptoms other than seizures are present, an intravenous bolus of
200 mg/kg (2 mL/kg) of 10% glucose is effective in elevating the blood
glucose concentration.
2) In the presence of convulsions, 4 mL/kg of 10% glucose as a bolus injection
is indicated.
3) After initial therapy, a glucose infusion should be given at 8 mg/kg/min.
4) If hypoglycemia recurs, the infusion rate and concentration should be
increased until 15–20% glucose is used.
5) If intravenous infusions of 20% glucose are inadequate to eliminate
symptoms and maintain constant normal serum glucose concentrations,
hyperinsulinemia is probably present and diazoxide should be
administered.
6) If the diazoxide is unsuccessful, octreotide may be useful
7) infants with severe persistent hyperinsulinemic hypoglycemia may
eventually need to undergo subtotal pancreatectomy .
8) The serum glucose level should be measured every 2 hr after initiating
therapy until several determinations are above 40 mg/dL.
9) Subsequently, levels should be measured every 4–6 hr
10) the treatment gradually reduced and finally discontinued when
the serum glucose value has been in the normal range
the baby asymptomatic for 24–48 hr.
11) Treatment is usually necessary for a few days to a week, rarely for several
weeks.
12) Infants at increased risk for hypoglycemia should have their serum glucose
measured within 1 hr of birth, every 1–2 hr for the 1st 6–8 hr, and then
every 4–6 hr until 24 hr of life.
13) Normoglycemic high-risk infants should receive oral or gavage feeding
with human milk or formula started at 1–3 hr of age and continued at 2–3
hr intervals for 24–48 hr.
14) An intravenous infusion of glucose at 4 mg/kg/min should be provided if
oral feedings are poorly tolerated or if asymptomatic transient neonatal
hypoglycemia develops.
108
"
االثطبي
ال
ْؼٕٛق٠
فٝ
فبالد
زذس٠تٌا
..
االثطبي
ْؼٕٛق٠
ِٓ
اؽ١بء
١مخّػ
فٟ
ٍُٙخاد
،
ٟ٘
االسادح
ٚ
ٍُؾٌا
ٚ
شؤ٠خٌا
"
محمد
ًعل
كالي
22.Management of ITP
platelet transfusion in ITP is usually contraindicated unless life-threatening bleeding is
present. Initial approaches to the management of ITP include the following:
1. No therapy other than education and counseling of the family and patient for patients
with minimal, mild, and moderate symptoms, as defined earlier. This approach
emphasizes the usually benign nature of ITP and avoids the therapeutic roller coaster
that ensues once interventional therapy is begun. This approach is far less costly, and
side effects are minimal.
2. Intravenous immunoglobulin (IVIG). IVIG at a dose of 0.8–1.0 g/kg/day for 1–2 days
induces a rapid rise in platelet count (usually>20× 10
9
/L) in 95% of patients within 48
hr. IVIG appears to induce a response by downregulating Fc-mediated phagocytosis
of antibody-coated platelets. IVIG therapy is both expensive and time-consuming to
administer. Additionally, after infusion, there is a high frequency of headaches and
vomiting, suggestive of IVIG-induced aseptic meningitis.
3. Intravenous anti-D therapy. For Rh positive patients, IV anti-D at a dose of 50–
75μg/kg causes a rise in platelet count to>20× 10
9
/L in 80–90% of patients within 48–
72 hr. When given to Rh positive individuals, IV anti-D induces mild hemolytic
anemia. RBC-antibody complexes bind to macrophage Fc receptors and interfere
with platelet destruction, thereby causing a rise in platelet count. IV anti-D is
ineffective in Rh negative patients.
4. Prednisone. Corticosteroid therapy has been used for many years to treat acute and
chronic ITP in adults and children. Doses of prednisone of 1–4 mg/kg/24 hr appear to
induce a more rapid rise in platelet count than in untreated patients with ITP.
Whether bone marrow examination should be performed to rule out other causes of
thrombocytopenia, especially acute lymphoblastic leukemia, before institution of
prednisone therapy in acute ITP is controversial. Corticosteroid therapy is usually
continued for 2–3 wk or until a rise in platelet count to>20× 10
9
/L has been achieved,
with a rapid taper to avoid the long-term side effects of corticosteroid therapy,
especially growth failure, diabetes mellitus, and osteoporosis.
Each of these medications may be used to treat exacerbations of ITP, which commonly occur
several wk after an initial course of therapy.
In the special case of intracranial hemorrhage, multiple modalities should be used, including
platelet transfusion, IVIG, high-dose corticosteroids, and prompt surgical consultation, with
plans for emergency splenectomy.
patients who are bleeding significantly should be treated, and these may represent only 5%
of children with ITP. Intracranial hemorrhage remains rare, and there are no data showing
that treatment actually reduces its incidence.
The role of splenectomy in ITP should be reserved for 1 of 2 circumstances. The older child
(> 4 yr) with severe ITP that has lasted >1 yr (chronic ITP) and whose symptoms are not
easily controlled with therapy is a candidate for splenectomy. Splenectomy must also be
considered when life-threatening hemorrhage (intracranial hemorrhage) complicates acute
ITP, if the platelet count cannot be corrected rapidly with transfusion of platelets and
administration of IVIG and corticosteroids. Splenectomy is associated with a lifelong risk of
overwhelming postsplenectomy infection caused by encapsulated organisms.
109
"
ال
ً٠ق
بطٌٕا
ٌٝا
ؽذ٠مخ
غبػٌٕا
،
ْدٚ
ْا
شٚاّ٠
ؾطبدّث
زؼتٌا
ٚ
ًفؾٌا
١أطٌاٚ
ٚفبؽت
اإلسادح
مٛ٠خٌا
ال
ً٠ط١
ٛلٛفٌا
فٟ
٘زٖ
ؾطبدٌّا
"
لون
تشارلز
ساالك
23.Management of severe malnutrition
Treat the following conditions
1)
Hypoglycaemia
➤Give the first feed of F-75 if it is quickly available and then continue with 2–3 hourly
feeds.
➤If the first feed is not quickly available give 50 ml of 10% glucose or sucrose
solution (1 rounded teaspoon of sugar in 31/2 tablespoons of water) orally or by
nasogastric tube, followed by the first feed as soon as possible.
➤Give 2–3-hourly feeds, day and night, at least for the first day.
➤Give appropriate antibiotics.
➤If the child is unconscious, treat with IV 10% glucose 5 ml/kg or, if unavailable, 10%
glucose or sucrose solution by nasogastric tube
Monitoring
If the initial blood glucose was low, repeat the measurement (using fingerprick
or heelprick blood and dextrostix, where available) after 30 minutes.
• If blood glucose falls <3 mmol/1 (<54 mg/dl), repeat the 10% glucose or sugar solution.
• If the rectal temperature falls <35.5 °C or if there is deterioration in the level
of consciousness, repeat the dextrostix measurement and treat accordingly.
Prevention
➤Feed 2 hourly, starting immediately or, if necessary, rehydrate first. Continue feeding
throughout the night.
2)
Hypothermia
➤Feed the child immediately (if necessary, rehydrate first).
➤Make sure the child is clothed (including the head), Cover with a warmed
blanket and place a heater (not pointing directly at the child) or lamp nearby,
or put the child on the mother’s bare chest or abdomen (skin-to-skin) and
Cover them with a warmed blanket and/or warm clothing.
➤Give appropriate antibiotics.
Monitoring
• Take the child’s rectal temperature 2-hourly until it rises to
more than 36.5 °C. Take it half-hourly if a heater is being used.
• Ensure that the child is Covered at all times, especially at night.
Keep the head Covered, preferably with a warm bonnet to reduce heat loss.
• Check for hypoglycaemia whenever hypothermia is found.
Prevention
➤Feed the child 2-hourly, starting immediately
➤Always give feeds through the night.
➤Place the bed in a warm, draught-free part of the ward and keep the child Covered.
➤Change wet nappies, clothes and bedding to keep the child and the bed dry.
➤Avoid exposing the child to cold (e.g. after bathing, or during medical examinations).
➤Let the child sleep with the mother for warmth in the night.
Position for kangaroo mother
care of young infant. Note:
after wrapping the child, the
head needs to be covered
with a cap or bonnet to
prevent heat loss.
110
"
رادة
النلاح
مهمة
،
لكن
األ م
منها
ارادة
رٌضحتلا
للنلاح
"
ًبوب
تٌان
3)
Dehydration:
Treatment
Do not use the IV route for rehydration except in cases of shock .
Standard WHO-ORS solution for general use has a high sodium and low
potassium content, which is not suitable for severely malnourished children.
Instead, give special rehydration solution for malnutrition, ReSoMal (see recipe
below, or use commercially available ReSoMal).
➤Give the ReSoMal rehydration fluid, orally or by nasogastric tube, much
more slowly than you would when rehydrating a well-nourished child:
— give 5 ml/kg every 30 minutes for the first 2 hours
— then give 5–10 ml/kg/hour for the next 4–10 hours.
The exact amount depends on how much the child wants, volume of stool
loss, and whether the child is vomiting.
➤If rehydration is still occurring at 6 hours and 10 hours, give starter F-75
instead of ReSoMal at these times. Use the same
volume of starter F-75 as for ReSoMal.
Monitoring
During rehydration, respiration and pulse rate should fall and urine start to be
passed. The return of tears, a moist mouth, less sunken eyes and fontanelle,
and improved skin turgor are also signs that rehydration is proceeding, but
many severely malnourished children will not show these changes even when
fully rehydrated. Monitor weight gain.
Monitor the progress of rehydration half-hourly for 2 hours, then hourly for
the next 4–10 hours. Be alert for signs of overhydration, which is very
dangerous and may lead to heart failure. Check:
• respiratory rate
• pulse rate
• urine frequency
• frequency of stools and vomit.
If you find signs of overhydration (increasing respiratory rate by 5/min and
pulse rate by 15/min), stop ReSoMal immediately and reassess after 1 hour.
Prevention
Measures to prevent dehydration from continuing watery diarrhoea are similar
to those for well-nourished children, except
that ReSoMal fluid is used instead of standard ORS.
➤If the child is breastfed, continue breastfeeding.
➤Initiate refeeding with starter F-75.
➤Give ReSoMal between feeds to replace stool losses. As a guide, give 50–
100 ml after each watery stool.
4)
Electrolytes
5)
Infection
6)
Micronutrients
7)
Initiate feeding
8)
Catch-up growth
9)
Sensory stimulation
10)
Prepare for follow-up
For further information see the lecture ( Management of severe malnutrition )
111
"
نحن
ًنبن
رٌثكلا
من
اللدران
و
لٌلقلا
من
اللسور
"
وتنٌن
24. Rickets :
Children with nutritional vitamin D deficiency should receive vitamin D
and adequate nutritional intake of calcium and phosphorus.
There are 2 strategies for administration of vitamin D. With stoss therapy,
300,000–600,000 IU of vitamin D are administered orally or
intramuscularly as 2–4 doses over 1 day. Because the doses are observed,
stoss therapy is ideal in situations where adherence to therapy is
questionable.
The alternative is daily, high-dose vitamin D, with doses ranging from
2,000–5,000 IU/day over 4–6 wk. Either strategy should be followed by
daily vitamin D intake of 400 IU/day, typically given as a multivitamin.
It is important to ensure that children receive adequate dietary calcium
and phosphorus; this is usually provided by milk, formula, and other
dairy products.
Children who have symptomatic hypocalcemia may need intravenous
calcium acutely, followed by oral calcium supplements, which typically
can be tapered over 2–6 wk in children who receive adequate dietary
calcium. Transient use of intravenous or oral 1,25-D (calcitriol) is often
helpful in reversing hypocalcemia in the acute phase by providing active
vitamin D during the delay as supplemental vitamin D is converted to
active vitamin D. Calcitriol doses are typically 0.05 μmg/kg/day.
Intravenous calcium is initially given as an acute bolus for symptomatic
hypocalcemia (20 mg/kg of calcium chloride or 100 mg/kg of calcium
gluconate).
Some patients require a continuous intravenous calcium drip, titrated to
maintain the desired serum calcium level. These patients should transition
to enteral calcium, with most infants requiring approximately 1,000 mg of
elemental calcium.
Wrist x-rays in a
normal child (A)
and a child with
rickets (B). The child
with rickets has
metaphyseal
fraying and cupping
of the distal radius
and ulna.
Rachitic rosary
in a young
infant
112
"
من
دٌفملا
ن
نضع
عالمات
استفهام
نٌب
نٌحلا
واألخر
على
األمور
مّلسملا
بها
"
برتراند
راسل
Primary health care
ARI Program
1- WIPE
2- Ask about :
1- Name, age, sex of the patient
2- Ask about danger signs : convulsion, vomiting of
everything , inability to drink or breastfeed
3- Does the child have cough or difficult breathing?
4- Duration (For how long)?
3-look and listen
1. Count the breaths in one minute fast if:
i. >2mon <1yr = 50 breath /min or more
ii. >12mon <5 yr= 40 breath /min or more
2. Look for chest in drawing
3. Listen for stridor
4. Listen for wheeze
5. Look for danger signs
i. Lethargic or unconscious
ii. Is the child convulsing now
The child must be calm
Classify cough or difficult breathing:
1.Sever pneumonia or Very sever disease
1- any general danger signs
or
2- stridor in calm child
or
3- chest indrawing
(If also wheeze go to treat wheeze and reassess)
113
"
ال
رؾشػ
بطٌٍٕ
هٍوبؾِ
قؾ١خٌا
،
ٌُٙٛمف
و١ف
هٌبؽ
؟
غشدِ
رؾ١خ
ٚ
١غذٌ
اًلااإع
"
آرثر
ترمانٌل
Treatment of Sever pneumonia or Very sever disease
:
1- Give first dose of an appropriate antibiotic
2- Treat wheeze if present
3- Prevent low blood sugar
4- Refer urgently to hospital
2.Pneumonia
( fast breathing If also wheeze go to treat wheeze
and reassess)
Treatment of pneumonia
1- Give an appropriate antibiotic for 5 days
2- Treat wheeze if present
3- Soothe the throat and relieve the cough with a safe remedy
4- Follow up in 2 days
5- Advice the mother when to return immediately
3.No pneumonia
( cough or cold)
( no signs of pneumonia or very sever disease, if also wheeze go to
treat wheeze and reassess)
Treatment of cough or cold
1-
Treat wheeze if present
2-
If coughing more than 30 days refer for assessment
3-
Soothe the throat and relieve the cough with a safe remedy
4-
Advice the mother when to return immediately
5-
Follow up in 2 days
6-
Follow up in 5 days if not improving
114
"
عأي
ٓىٌّّا
ًغزؾ١ٌّا
ٓأ٠
ُرم١
،
فأعبة
:
فٟ
َأؽال
ؼبعضٌا
"
هبغٛس
Assessment hydration status according to CDD
program:
1)
WIPE
2)
Ask about name , age
3)
Ask about danger signs, convulsion, vomiting of everything,
poor feeding
4)
Ask whether the child has diarrhea, duration, whether
bloody , fever
5)
General look:
General condition:
* Well , alert
# restless or irritable
$ lethargic or unconscious
Thirst: *drink normally, #thirsty drink eagerly , $ unable
to drink
Eyes: *not Sunken, #sunken, $very sunken
Skin turgor : *return immediately, #slow return, $delay
return >2 sec.
6)
See whether the child lethargic, has abnormal movement
(Danger signs) , has fever
7)
Decide : Patient with diarrhea can be classified as :
No dehydration = * * => Management plan A
Some dehydration = # # => Management plan B
Severe dehydration = $ $ => Management plan C
(for management of these cases see pages 85 - 90 )
115
على
قدر
ا ل
العزم
ًتأت
العزائم
...
و
ًتأت
على
قدر
الكرام
المكارم
و
تعظم
ًف
نٌع
رٌغصلا
صغار ا
...
وتصغر
ًف
نٌع
مٌظعلا
العظائم
(
ًالمتنب
)
Vaccinations
Table 6: Vaccination Schedule In Iraq
Birth
2 mon. 4 mon.
6 mon.
9 mon.
15 mon. 18 mon. 4-6 yrs
OPV
0D
OPV
1
st
D
OPV
2
nd
D
OPV
3
rd
D
Measles
V.
MMR OPV
1
st
BD
OPV
2
nd
BD
BCG
DPT
1
st
D
Hep. B
2
nd
D
Hi b
(
بعّٟخٌا ػبمٌٍا
)
1
st
D
DPT
2
nd
D
Hi b
(
شثبػٌٟا ػبمٌٍا
)
1
st
D
DPT
3
rd
D
Hep. B
3
rd
D
Hi b
(
بعّٟخٌا ػبمٌٍا
)
2
nd
D
Vitamin
A
100 U
DPT
Hi b
(
شثبػٌٟا ػبمٌٍا
)
1
st
BD
DPT
2
nd
BD
Hep. B
1
st
D
MMR
Booster
Vitamin
A
200 U
Rota virus
1
st
D
Rota virus
2
nd
D
Rota virus
3
rd
D
Notes:
OPV = Oral polio vaccine
BCG = Bacillus Calmette-Guerin
َخ ػذٌبؽ ٟف ٝزؽ شّؼٌا ِٓ ٌٝٚاا خٕغٌا ٌٗبّوئ ذؼث ًفطٌٍ ػبمٌٍا از٘ ٝطؼ٠ لا
غشػخ عبثمخٌ ِٗلازعا
ــٌمبػ اٍث ؼ١مٍزٌا دبؼ٠
BCG
ٓنٟ ؽٙش٠ِ ذؼث خثذٌٕا سٛٙظ َذػ خٌبؽ ٟف خ١ٔبص حشِ
م١ؼٍزٌا ٍٝػ
Hep. B = Hepatitis B
DPT = Diphtheria , Pertussis, Tetanus= ضالصٌٟا ػبمٌٍا
Rota virus:
ٍٟغؼٌا ٟعٚش٠بفٌا ػبمٌٍا
(
ذٚاسٌا
)
م١ؼٍزٌبث شؽبج٠ ٌُٚ شٙؽا خصلاص ٖشّػ صٚبغر ارا ًفطٌٍ ٍٟغؼٌا ػبمٌٍا ٝطؼ٠ لا
ْ١خ اؽٙش ؽزٝ ٚأبّص ٖشّػ صٚبغر ارا ًفطٌٍ ػبمٌٍا ٝطؼ٠ لا هٌزو
غشعٌا ًّى٠ ٌُ
مشسحٌّا
MMR = Mump, Measles, Rubella= طخٍزخٌّا خجقؾٌا ػبمٌ
Hi b = H. Influenza type B = خ١ٌضٌٕا خ١ِذزغٌّا ػبمٌ
DPT +Hi b = ٟػبثشٌا ػبمٌٍا
DPT +Hi b+ Hep. B = ٟعبّخٌا ػبمٌٍا
D = Dose
BD= Booster dose
١خٕ١رٚشٌا دبؾ١مٍزٌا ٓػ لا٠ذث ١خٕهٌٛا دلاّؾٌا َب٠أ ٟف ؼ١مٍزٌا شجزؼ٠ لا
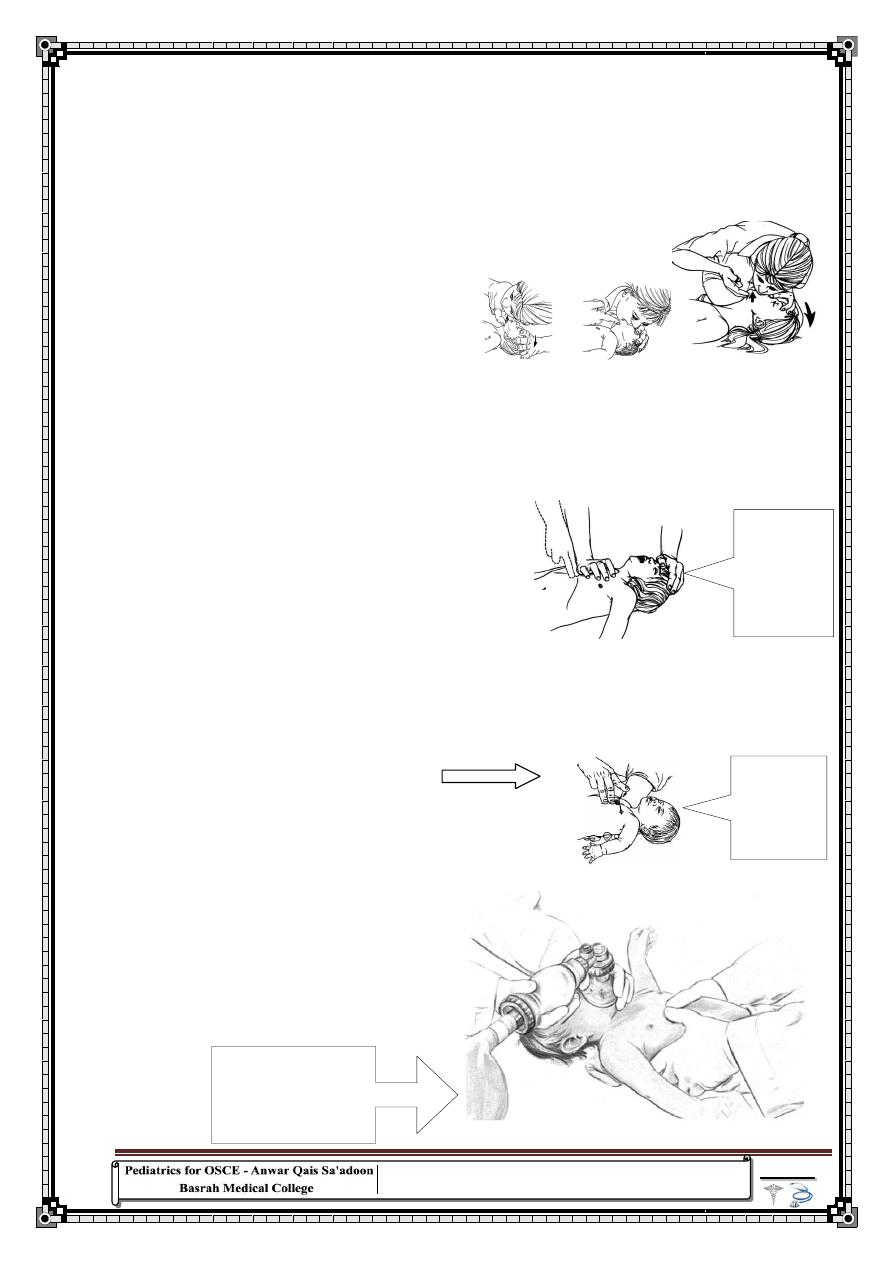
116
Locating the
hand
position for
chest
compression
in a child
The infant is
supine on the
palm of the
rescuer's
hand.
"
ِٓ
ًاافن
ْئ
ؾّٝر
ثجوء
ٌٝئ
َبِاا
ٍٝػ
ْئ
ؾّٝر
اًبػشغِ
ٌٝئ
فٍخٌا
"
ٌٓىٌٕٛ َب٘اشثا
Clinical Skills
Basic life support
(Management of a child with sudden collapse)
:
1- Ensure safety of the environment
2- Check for response: by gentile stimulation or by loud verbal stimuli
3- If no response shout for help
4- Open the air way by head tilt and chin lift or jaw thrust
Look for chest movement
Listen for abnormal sound
Feel for respiration by putting your cheek near the patient's mouth
5- If no response deliver 5 rescue breathings:
In infant : no neck extension, breathing from mouth and nose
In older children : do neck extension and close the nose
6- Check pulse for response (brachial in infant and carotid in older children )
in ten second multiply x 6
7- If bradycardia or no response start CPR
8- CPR 15:2
in infant : by two methods
1) Two thumb-encircling hands used to perform chest compression in
an infant (2 rescuers). (See below)
2) By two fingers above the lower third of the sternum about 1 finger
above xiphisternum and press up to one third of AP diameter of the
chest wall (see the figure )
for older child use heel of your hand
9- If there is response put the child in recovery position (left lateral position)
10- Stop CPR If:
Response
No improvement for > 20 min.
Exhaustion of rescuer
Availability of ALS and help
Two thumb-encircling
hands used to perform
chest compression in an
infant (2 rescuers).
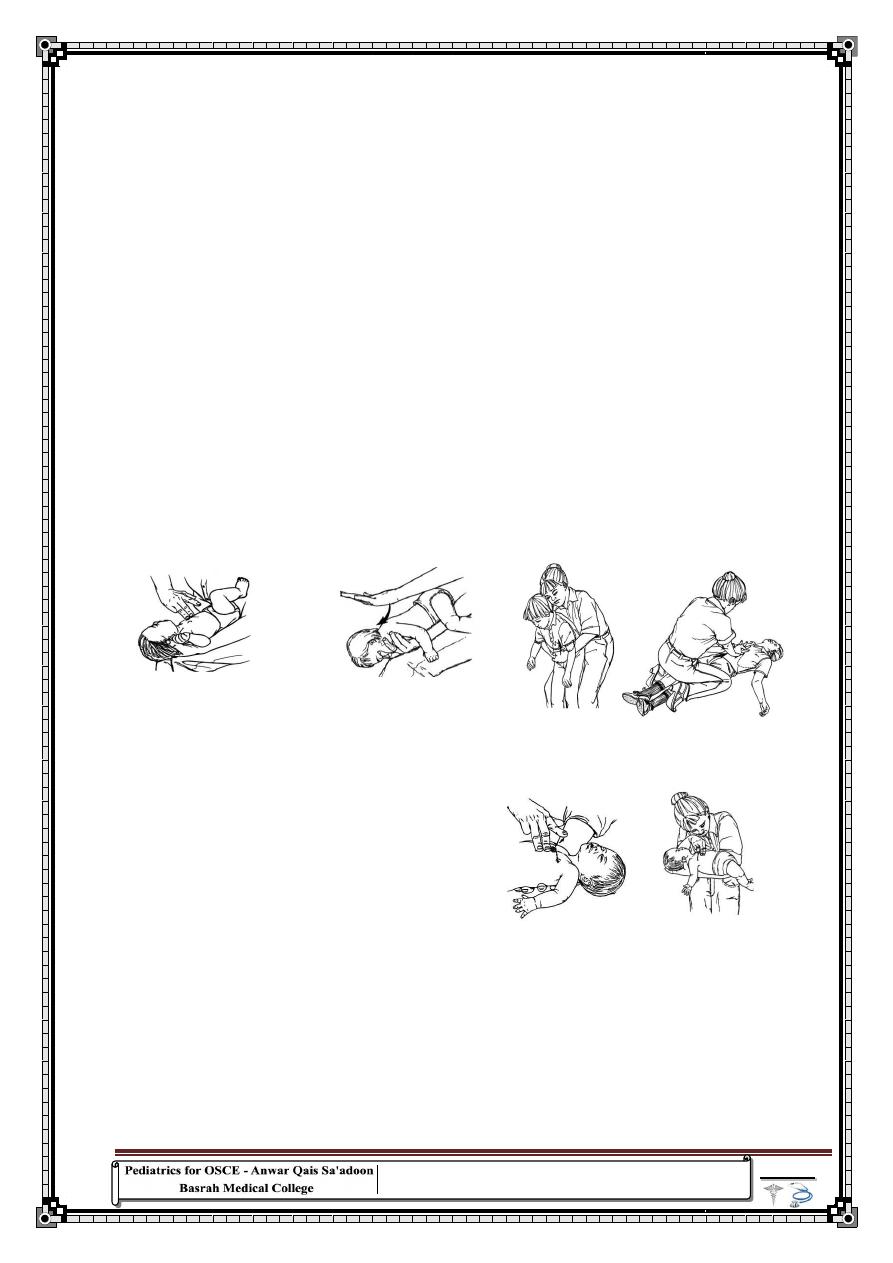
117
"
نشثبدٌا
مٛ٠خٌا
ُرٙؾ
ضعبطٌا
ٙبٕىٌ
ًرقم
ؾذ٠ذٌا
"
ٓثٛؽى١
Chocking:
1- Ensure safety of the environment
2- Check for response: by gentile stimulation or by loud verbal stimuli
3- If no response shout for help
4- Open the air way by head tilt and chin lift or jaw thrust
5- Check for response :
Look for chest movement
Listen for abnormal sound
Feel for respiration by putting your cheek near the patient's mouth
6- Hold the infant in prone position over your hand and deliver five back blows
between the scapulae (Use the upright position in older children)
7- If no response place the infant in a supine position. Give up to five thrusts to the
sternum by two fingers vertically about one finger above the xiphisternum ( In
children over one year deliver up to five abdominal thrusts ).
8-
If no response also hold the infant in prone position over your hand and deliver
5 back blows between the scapulae
(Use the upright position in older children)
11- If no response deliver 5 rescue breathings :
In infant : no neck extension breathing from mouth and nose
In older children : do neck extension and close the nose
12- Check pulse for response (brachial in infant and carotid in older children ) for
10 second multiply x 6
13- If bradycardia or no response do CPR
14- CPR 15:2
In infant : by two methods
1) By two thumbs above lower third of the sternum about 1 finger and
press up to one third of AP diameter of chest wall
2) By two fingers above lower third of the sternum about 1 finger and
press up to one third of AP diameter of chest wall
for children use heel of your hand
15- If there is response put the child in recovery position (left later position)
118
"
ضمخٌا
فظٌٕبث
ٚ
ٙبسحٌّا
..
ع١ؼ
ال
٠مٙش
"
لورج
ربرت
Intraosseous Access:
Features of IO infusion:
used when intravascular access cannot be obtained
Rapidly and easily inserted
Low complication rate
Roughly has the same absorption rate as iv access
Safe with resuscitation medications
Not for long term use ( usually 24-48 hrs )
Require less skill and practice than central and umbilical line
placement
Recommended in <6 yrs but can be used in all age groups
Procedure:
1- Prepare the necessary equipment, i.e.:
— bone marrow aspiration or intraosseous needles (15–18 gauge or,
if not available, 21 gauge). If these are not available, large-bore
hypodermic or butterfly needles can be used in young children
— antiseptic solution and sterile gauze to clean the site
— a sterile 5-ml syringe filled with normal saline
— a second sterile 5-ml syringe
— IV infusion equipment
— sterile gloves.
2- Place padding under the child’s knee so that it is bent 30° from the
straight (180°) position, with the heel resting on the table.
3- Locate the correct position (described above and shown in the
illustration).
4- Wash the hands and put on sterile gloves.
5- Clean the skin over and surrounding the site with an antiseptic
solution.
6- Stabilize the proximal tibia with the left hand (this hand is now not
sterile) by grasping the thigh and knee above and lateral to the
cannulation site, with the fingers and thumb wrapped around the
knee but not directly behind the insertion site.
7- Palpate the landmarks again with the sterile glove (right hand).
119
"
النالحون
قدرونٌ
على
النلاح
ألنهم
عتقدونٌ
ا
نهم
قدرونٌ
"
لٌلرف
8- Insert the needle at a 90° angle with the bevel pointing towards the
foot.
Advance the needle slowly using a gentle but firm, twisting or
drilling motion.
9- Stop advancing the needle when you feel a sudden decrease in
resistance
or when you can aspirate blood. The needle should now be fixed in
the bone.
10- Remove the stylet.
11- Aspirate 1 ml of the marrow contents (looks like blood), using the
5-ml syringe, to confirm that the needle is in the marrow cavity.
12- Attach the second 5-ml syringe filled with normal saline.
13- Stabilize the needle in place in the antero-medial surface
at the junction of the upper and middle third of the tibia.
and slowly inject 3 ml while palpating the area for any
leakage under the skin. If no infiltration is seen, start
the infusion.
14- Apply dressings and secure the needle in its place.
Note: Failure to aspirate marrow contents does not mean that the
needle is not correctly placed.
15- Monitor the infusion by the ease with which the fluid flows and by
the clinical response of the patient.
16- Check that the calf does not swell during the infusion.
Stop the intraosseous infusion as soon as venous access is available.
In any case, it should not continue for more than 8 hours.
Complications:
1- Incomplete penetration of the bony cortex
Signs: The needle is not well fixed; infiltration occurs under the
skin.
2- Penetration of the posterior bone cortex (more common)
Signs: Infiltration occurs, calf becomes tense.
3- Infection Cellulites at the site of the infusion, osteomyelitis
4- Compartmental syndrome
5- Hematoma
6- Fracture
Note: you need to read about Contrindication of intraosseoss
infusion
120
"
معظمنا
فضلٌ
ن
هدمهٌ
حٌدملا
على
ن
نقذذٌ
النقد
"
نورمان
فنسنت
لٌب
Measurement of blood pressure:
WIPE
Ask about patient's name , age and sex
1- Inform the child and the mother that you will measure the blood pressure
2- The child must be relaxed in sitting position if can sit
3- Choose a suitable cuff by:
Measuring the length of the arm from acromion to olecranon
Calculate two thirds of this length
Measure the width of the cuff and connect it with the
sphygmomanometer
4- Apply the cuff to the arm, ensuring that it fits securely.
5- Localize the brachial artery at about
2
cm above the cubital fossa
.
6- The level of the arm (cubital fossa) must be at the level of the heart
7- Palpate brachial pulse and Inflate the cuff till the pulse disappears
8- Inflate the cuff to 20-30 mmHg more than that point. You can estimate the
systolic blood pressure by palpating the brachial or radial artery pulse and
inflating the cuff until you can no longer feel it.
9- Place the stethoscope over the brachial artery pulse, ensuring that it does not
touch the cuff. and start to deflate the cuff slowly 2-3mm/sec.
10-
Record the points when the sound appears and disappears as systolic
and diastolic blood pressure
11- Measure the height of the patient and plot it on the centile chart
12- plot your reading on special chart for blood pressure
13- You also should mention that you need to measure blood pressure in other
hand and in standing position.
After the procedure
14- Ensure that the patient is comfortable.
15- Tell the child or the mother about the blood pressure and explain its
significance. Hypertension can only be confirmed through several blood
pressure measurements taken over time.
16- Thank the patient.
121
"
النلاح
...
و
ان
تنتقل
من
فشل
الى
فشل
بدون
ان
تفقد
حماسك
"
تشرشل
Procedures:
Phototherapy
WIPE
Ask about name and age
1. Confirm the indication
Jaundice on day 1
Deep jaundice involving palms and soles of the feet
Prematurity and jaundice
Jaundice due to haemolysis
2. Admission
3. The child must be naked
4. The eyes are Covered
5. Place the child under the phototherapy ( wave length 450 nm)
6. The distance is 50 cm
7. Operate the device
8. Advice the mother to change the position of the baby
9. Encourage breast feeding every 2 hrs
10. Measures TSB every 6 hrs
11. Seek for complications like
Skin rash
Dehydration: so
the child need more fluid than" the usual
maintenance volumes"
Hyperthermia
Hypothermia
Diarrhea
12.
Continue phototherapy until serum bilirubin level is lower
than threshold range or until baby is well and there is no
jaundice of palms and soles. If the bilirubin level is very
elevated and you can safely do exchange transfusion, consider
doing so.
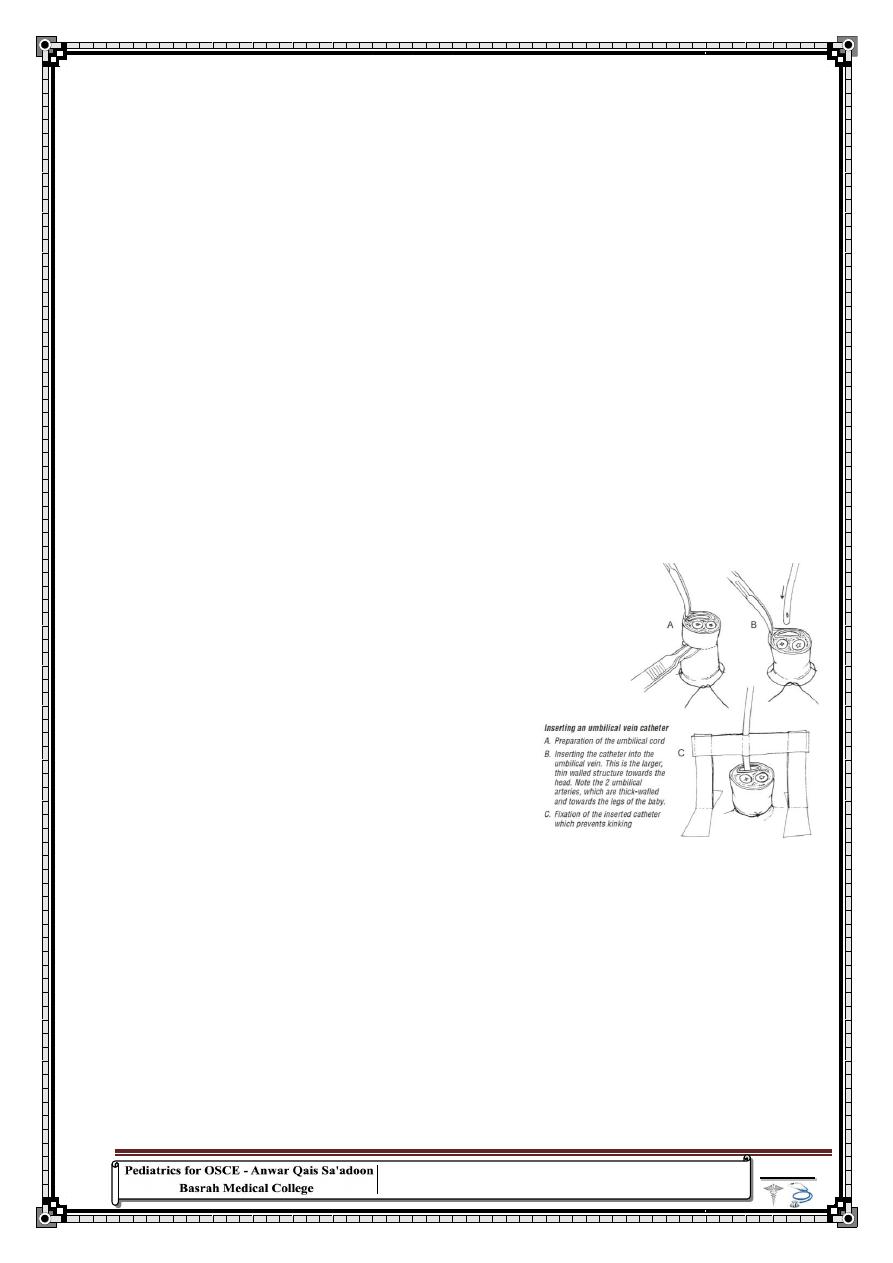
122
"
التردد
و
اطالة
رٌكفتلا
ًف
امٌقلا
بعمل
ما
،
غالبا
ما
تحولٌ
الى
سبب
البطاله
"
ونجٌ
Exchange transfusion:
Ask about name, age
1-
See if there is indication for exchange
2-
Prepare the instrument and calcium and warm fresh
compatible blood
3-
Call for an assistant
4-
At room temperature 25 C
5-
Under aseptic technique
6-
Wash your hands and wear gloves
7-
Catheterize umbilical vein ( As in figure below )
8-
Draw 20 ml of blood in term and 10 ml in preterm baby and
replace it with the donar blood then repeat the process
9-
The total volume that must be exchanged is 80-85 ml/kg x 2
10- Inject calcium 1cc after each 100 ml of blood
11- Look for any allergy or complication
Acute complication (5-10 %)
1) transient bradycardia
2) Apnea
3) Cyanosis
4) Transient vasospasm
Late
1) Infection ( CMV, HIV,Hepatitis)
2) Anemia
3) Cholestasis
4) Mild graft versus host reaction, diarrhea, Rash, hepatitis, eosinophlia
5) Inspissated syndrome
6) Portal vein thrombosis
12-
After finishing the process remove the transfusion set but not
the catheter because you may need it for further transfusion.
123
"
ئالَاٛلاا ِٓ هم٠ذف سزؽاٚ نٚذػ تٕغرٚ ه١ٕؼ٠ لا بِ يضزػاٚ كؾٌبث ُل
خؾٟ هللآِ لائ ٓ١ِأ لاٚ ، ٓ١ِاا
"
جبلشٌا َبِلإا
(
ع
)
Ventolin nebulizer:
1) Place the air compressor on a sturdy surface that will support its
weight plug the cord from the compressor into properly grounded
(three prong) electrical outlet.
2) Wash your hands with soap and water and dry completely with a clean
towel.
3) Carefully measure the medicine exactly as you have been instructed.
use a separate syringe for each medicine
4) see the expire date of the drug
5) the average dose for a single treatment is (0.25 to 2.5 mg of salbutamol)
diluted in 2-5 ml of sterile normal saline
6) remove the top part of the nebulizer cup.
7) Place the medicine in the bottom of the nebulizer cup.
8) Attach the top portion of the nebulizer cup and connect the
mouthpiece or face mask to the cup
9) Connect the tubing to both the aerosol compressor and nebulizer cup.
10) Turn on the compressor with the on/off switch. Once you turn on the
compressor you should see a light , mist coming from the back of the
tube opposite the mouthpiece
11) Let the pt. sit up straight on a comfortable chair
12) If you are using a mask , position it comfortably and securely on the
face
13) If you are using a mouth piece place it between the pt. teeth and lips
around it.
14) Take slow , deep breaths through the mouth , if possible , hold each
breath for two to three second before breathing out, this allow the
medication to settle into the airways
15) Continue the treatment for 7-10 minutes
16) Turn the compressor off
17) Ask the pt. to take several deep breath and cough
18) Wash your hands with warm water and soap and dry them with dry
towel.
Care for nebulizer
1. after each treatment rise the nebulizer cup with warm water ,shake off
excess water and let it air dry
2.at the end of each day , the nebulizer cup , mask or mouth piece should be
washed in warm , soapy water
3.no need to clean the tube that connect the nebulizer to the air compressor
4. every third day , after washing your equipment disinfect the equipment
using a vinegar/water solution or other disinfectant solution
124
"
رلل
بال
خالق
و
وحش
تم
طالقه
على
ذا
العالم
"
رٌبلا
كامو
Blood transfusion
1-
Name , Age of the patient
2-
weight of the patient
3-
Confirm the indication of transfusion
4-
type of transfusion
5-
See the blood is the correct group and the patient’s name and
number are on both the label and the form calculate the volume
you need
6-
see the blood transfusion bag for any leaks
7-
the blood pack has not been out of the refrigerator for more than
2 hours, the plasma is not pink , and the red cells do not look
purple or black
8-
any signs of heart failure. If present, give 1mg/kg of furosemide
IV at the start of the transfusion in children whose circulating
blood volume is normal. Do not inject into the blood pack.
During transfusion:
1- record the time of start of transfusion
2- if available, use an infusion device to control the rate of the
transfusion
3- check that the blood is flowing at the correct speed
4- look for signs of a transfusion reaction particularly carefully in the
first 15 minutes of the transfusion
5- Observe and record the child’s general appearance, temperature,
pulse and respiratory rate, urine output, urine color , skin rash every
30 minutes
After transfusion:
record the time the transfusion was started and ended, the volume of
blood transfused, and the presence of any reactions.
Reassess the child. If more blood is needed, a similar quantity
should be transfused and the dose of furosemide (if given) repeated.
Note:
Desferal pump and its use is very important subject so
Please read about it.
125
"
بَع
ّل
بَتو سانلا م
ِعلم ع
ِ فتكون قد تقنت ع، كرٌغ مل
بَعو كمل
ِل
مت ما ال تعلم
"
اإلمام الحسن
(
ع
)
Family counseling
:
Note : the following information are taken from the portfolios of
previous years with slight modifications.
Febrile convulsion:
Inform parents that these dramatic events do not indicate future
neurologic dysfunction or disease& There is no evidence that they cause
death, brain damage, epilepsy, mental retardation, a decrease in IQ, or
learning difficulties
also inform them Febrile seizures are age dependent & rarely occur after
6 year old.
Educate the parents what to do during seizure :
leave the child on the floor.
slide a blanket under the child if the floor is hard.
Move him only if he is in a dangerous location.
Remove objects that may injure him.
Loosen any tight clothing, especially around the neck. If possible, open
or remove clothes from the waist up.
If he vomits, or if saliva and mucus build up in the mouth, turn him on
his side or stomach. This is also important if it looks like the tongue is
getting in the way of breathing.
Don’t try to force anything into his mouth to prevent him from biting
the tongue, as this increases the risk of injury.
Don’t try to restrain their child or try to stop the seizure movements.
If possible try to time the seizure using watch or a clock. Because they're
so alarming, seizures often seem to last longer than they really do
Also try to note which part of child's body begins to shake first, and look
for other signs of illness.
Focus their attention on bringing the fever down:
o Insert an acetaminophen suppository (if have some) into the
child's rectum.
o DO NOT try to give anything by mouth.
o Apply cool Washcloths to the forehead and neck. Sponge the
rest of the body with lukewarm (not cold) water. Cold water
may make the fever worse.
126
"
القلق
مثل
ًالكرس
الهزاز
،
لعلكٌس
تتحرك
اًامئاد
و
لكنه
لن
وصلكٌ
الى
ي
مكان
"
لو
آن
ثٌمس
o After the seizure is over and child is awake, give the normal
dose of ibuprofen or acetaminophen.
When to Contact a Medical Professional:
If the seizure is lasting several minutes bring the child to the
hospital.
if repeated seizures occur during the same illness, or if this looks
like a new type of seizure for your child.
if other symptoms occur before or after the seizure, such as:
1) Abnormal movements
2) Agitation
3) Confusion
4) Drowsiness
5) Nausea
6) Problems with coordination
7) Rash
8) Sedation
9) Tremors
Possible Complications
Biting oneself
Breathing fluid into the lungs, pneumonia
Complications if a serious infection, such as meningitis, caused the fever
Injury from falling down or bumping into objects
Injury from long or complicated seizures
Seizures not caused by fever
Side effects of medications used to treat and prevent seizures (if prescribed)
prognosis: Febrile seizures are not associated with reduction in later
intellectual performance, and most children with febrile seizures have
only a slightly greater risk of later epilepsy than the general population.
Factors that are associated with a substantially greater risk of later
epilepsy include the presence of complex features during the seizure or
postictal period, a positive family history of epilepsy, an initial febrile
seizure before 12 mo of age, delayed developmental milestones, or a pre-
existing neurologic disorder. The risk of epilepsy is much higher than in
the general population in children with one or more complex febrile
seizures, especially if the seizures are focal in children with an underlying
neurologic disorder. The incidence of epilepsy is >9% when several risk
factors are present, compared with an incidence of 1% in children who
have febrile convulsions and no risk factors.
127
Diabetic ketoacidosis (DKA):
The child's family must understand clearly that diabetes
is a life long illness and their child must be kept on
insulin for the rest of his life.
one should emphasize that insulin is not harmful and
must not discontinued by the family also education about
herbal medicine and traditional medicine which causes a
significant proportion of poor compliance to treatment
The parent must also have an idea about the Long-term
complications of DM1 which include retinopathy,
nephropathy, neuropathy, and macrovascular disease.
Before hospital discharge, the family and child must
show competence in glucose monitoring
insulin administration including how to calculate the dose
of insulin ,how to give subcutaneous injections ,the site
of injection(thigh, abdomen ,arms ….etc)
this site should be periodically ;
various aspects of nutrition, especially related to
carbohydrate intake instruction must be given so that the
family understand that no diet apart from refined sugar is
restricted (refined sugar is allowed once or twice monthly
or if the child is participating for example in a birthday
party provided that the insulin dose is increased)
the ideal diet consist of carbohydrates 50% to 65% of the
total calories; protein, 12% to 20%; and fat, less than
30%. Saturated fat should contribute less than 10% of the
total caloric intake, and cholesterol intake should be less
than 300 mg/24 hours.
High fiber content is recommended because it improve
glycemic control
recognition and management of
hypoglycemia(Symptoms of hypoglycemia include
headache, visual changes, confusion, irritability, or
"
اًابلاغ
ما
ًتأت
الفرص
ناٌلا
متنكرة
ابٌثب
العمل
الشاق
،
و
لذلك
معظم
الناس
ال
لمحونهاٌ
"
آن
الندرز
128
"
أفذلبؤن صالصخ ٚأػذاؤن صالصخ
:
فأفذلبؤن
:
فذ٠مه ٚفذ٠ك فذ٠مه ٚػذٚ
ػذٚن ٚاػذاؤن صالصخ
:
ػذٚن ٚػذٚ فذ٠مه ٚفذ٠ك ػذٚن
"
ٍٟػ َبِلإا
(
ع
)
seizures tremors, tachycardia, diaphoresis, or anxiety)
and hyperglycemia; when and how to check for urinary
ketones; and what to do during intercurrent illnesses .
The child must be given close follow-up care in the
outpatient clinic and by telephone and be given 24-hour
access to a physician in the event of an emergency.
Families need clear guidelines on when and how to call
for help. In the early stages, many families need daily
telephone calls for reassurance, to assess glucose control,
and to adjust the insulin regimen.
A visiting home health nurse can help assess the family's
management skills and facilitate the transition to
outpatient therapy.
Also they must be told that exercise in controlled D.M
reduce insulin requirement by 10%
After the initial period the child must be followed every
3-4 month with screening for possible complication of
diabetes.
Prognosis
T1DM is a serious, chronic disease. It has been estimated
that the average life span of individuals with diabetes is
about 10 yr shorter than that of the non diabetic population.
Although diabetic children eventually attain a height
within the normal adult range, puberty may be delayed,
and the final height may be less than the genetic potential
Note: counseling to family about insulin injection
and storage it's so important and frequently
Coming in OSCE so please read about it.
129
"
ستكثروا من اإلخوان فإن لكل مؤمن دعوة مستلابة
"
اإلمام الصادق
(
ع
)
Nephrotic syndrome
You should tell the family these facts and advices:
Nephrotic syndrome is not infectious. May be hereditary.
High percentage of patient will not achieve complete remission
The child should be bring to the medical attention if he develops abdominal
pain, fever, or look ill.
Diet:
Should provide adequate energy & protein.
Sodium restriction participates in reduction of edema.
Fluid restriction per se is not required.
Micronutrient supplement: - According to the condition of the patient may
need supplement with iron , vitamin D ,Ca
Activity: There are no activity restrictions for patients with nephrotic
syndrome. Ongoing activity, rather than bed rest, will reduce the risk
of blood clots.
Vaccinations should be taken: -
Yearly influenza vaccination is recommended to prevent serious illness
in the immunocompromised patient, as well as to prevent this possible
trigger of relapse.
Pneumococcal vaccination should be administered to all patients with
INS upon presentation. Vaccination should be repeated every 5 years
while the patient continues to have relapses.
Routine childhood vaccines with live virus strains are contraindicated
during steroid therapy and for a minimum of 1 month afterward.
Care
must be taken in administering live viral vaccines to children in
remission from FRNS, who might need to restart steroid therapy shortly
after vaccination.
Because of the high risk of varicella infection in the
immunocompromised patient, post exposure prophylaxis with varicella-
zoster immune globulin is recommended in the non immune patient.
Patient with varicella-zoster infection should be treated with acyclovir
and carefully monitored.
Varicella immunization is safe and effective in
patients with INS who are in remission and off steroid treatment (with
the usual precautions for administering live viral vaccines to patients
who have received steroids).
Routine non live viral vaccines should be administered according to their
recommended schedules. Despite the former belief that routine
130
"
قد
شكٌ
الناس
ماٌف
تقول
،
و
لكنهم
سوف
ؤمنونٌ
بما
تفعل
"
سٌول
سٌاك
immunization can trigger relapse of nephrotic syndrome, no solid
evidence supports this, and the risk of these preventable childhood
illnesses exceeds the theoretical, unproven risk for triggering relapses.
Explain to the parents about the possible complications of the disease and
the side effects of the treatment .
Long-term monitoring
Ambulatory monitoring of the child's condition and response to treatment
is a very important aspect of the overall management of nephrotic
syndrome.
Home monitoring of urine protein and fluid status is an important aspect
of management.
Parents and/or caregivers should be trained to monitor first morning urine
proteins at home with urine dipstick.
Weight should be checked every morning as well and a home logbook
should be kept recording the patient’s daily weight, urine protein, and
steroid dose if the child is receiving steroids.
Families and patients are instructed to call for any edema, weight gain, or
urine testing 2+ or more for protein for more than 2 days. Rapid detection of
relapse of proteinuria by home testing of urine can allow early initiation of
steroid treatment before edema and other complications develop. Urine
testing at home is also useful in monitoring response (or non response) to
steroid treatment.
131
"
اذا
ردت
ان
تعرف
اخالق
رلل
فضع
السلطة
ًف
دذٌ
ثم
انظر
فٌك
تصرفٌ
"
سكوٌتنوم
Bronchial asthma
Asthma is not an infectious disease
Lifestyle and home remedies:
Taking steps to reduce your child's exposure to his or her asthma triggers will
lessen the possibility of asthma attacks. Steps to help avoid triggers vary depending
on what triggers your child's asthma. Here are some things that may help:
Maintain low humidity at home.
Keep indoor air clean.
Reduce pet dander. If your child is allergic to dander, it's best to avoid pets
with fur or feathers. Regularly bathing or grooming your pets also may
reduce the amount of dander in your surroundings.
Use your air conditioner. Air conditioning helps reduce the amount of
airborne pollen and lowers indoor humidity and can reduce your child's
exposure to dust mites. If you don't have air conditioning, try to keep your
windows closed during pollen season.
Make your home more asthma friendly. Minimize dust that may aggravate
nighttime symptoms by replacing certain items in your bedroom. For
example, encase pillows, mattresses and box springs in dust-proof Covers.
Consider removing carpeting and installing hard flooring, particularly in
your child's bedroom. Use Washable curtains and blinds.
Clean regularly. Clean your home at least once a week to remove dust and
allergens.
Reduce your child's exposure to cold air. If your child's asthma is worsened
by cold, dry air, wearing a face mask outside can help.
Make treatment a regular part of life. If your child has to take daily medication,
don't make a big deal out of it , it should be as routine as eating breakfast or
brushing teeth.
Make sure your child gets exercise. Don't let asthma sideline your child. Regular
exercise reduces symptoms and is important for your child's overall health. With
132
"
بّٕ١ث
٠مٛي
ذ٠شٌّا
:
ار٘ت
،
٠مٛي
مباذٌا
:
٘١ب
بٕث
"
ي
م
ًلٌك
asthma under control, there should be no limit to your child's physical activity
level.
Help your child to maintain a healthy weight. Being overweight can worsen
asthma symptoms, and it puts your child at risk of other health problems.
Regular clinic visit 2-4 per year to maintain good control to check up
Treatment of co-morbid condition (sinusitis, rhinitis ,Gastroesophageal reflux).
Prognosis
The prognosis for asthma is good, especially for children with mild disease. Of
asthma diagnosed during childhood, 54% of cases will no longer carry the
diagnosis after a decade. The extent of permanent lung damage in people with
asthma is unclear. Airway remodeling is observed, but it is unknown whether
these represent harmful or beneficial changes. Although conclusions from studies
are mixed, most studies show that early treatment with glucocorticoids prevents
or ameliorates decline in lung function as measured by several parameters. For
those who continue to suffer from mild symptoms, corticosteroids can help most
to live their lives with few disabilities. It is more likely to consider immediate
medication of inhaled corticosteroids as soon as asthma attacks occur. According
to studies conducted, patients with relatively mild asthma who have received
inhaled corticosteroids within 12 months of their first asthma symptoms achieved
good functional control of asthma after 10 years of individualized therapy as
compared to patients who received this medication after 2 years (or more) from
their first attacks. Though they (delayed) also had good functional control of
asthma, they were observed to exhibited slightly less optimal disease control and
more signs of airway inflammation. Asthma mortality has decreased over the last
few decades due to better recognition and improvement in care.
133
"
ٓز٠ٌا
ْ٠ؼنٛ
١ذٌا
زٌٟا
ُّٙؼطر
،
ػبدح
بِ
ْؼمٍٛ٠
ؾزاءٌا
زٌٞا
ٍُٙوش٠
"
اس٠ه
٘ٛفش
Breast feeding
1
.
َألٌٚ غ١مشٌٍ حذ١فِ خ١ؼ١جطٌا خػبمشٌا
2
.
ٛالدحٌا ذؼث خػبع يٚأ ٟف خػبمشٌا أذجر ْا تغ٠
3
.
ًٝ االٍػٚ ًفطٌا ٝىث بٍّو خػبمشٌبث شّزغرٚ
8
شاد فِٟ
ٛاؽذٌا َٛ١ٌا
4
.
ً١ٌٍا ءبٕصأ خػبمشٌا ٝغٕر لا
5
.
٠ذ٠ٙبَاا ًغغر ْا تغ٠
ًغغٌ خعبؽ لاٚ خػبمشٌا ذؼثٚ ًجل
ِٟٛ١ٌا َبّؾٌا ٍٝػ دبّزػلاا ومف ٞذضٌا
6
.
بءٌّا ٌٝا خعبؾٌا ْٚد سذقٌا ِٓ ومف ْٛىر ْا تغ٠ خػبمشٌا
ذحٌّ ٝزؽ
6
اؽٙش
7
.
شمبػخٌا خم٠شه
:
شفغٌ ءٟؽ غمٚ غِ ٟعشو ٍٝػ َاا ظٍغر ْا تغ٠
غهّر ٜشخااٚ ًفطٌا دبٕعلإ بٙ٠ذ٠ ٜذؽئ غنرٚ بٙ١ِذل
ضذٌٞبث
دْاٚ
خٌٛٙغث ٞذضٌا ٌٝا ًق٠ ش١ؾث بٕٙنؽ ٟف ًفطٌا غم
غ سأعِٗ ُ١مزغِ وخث ْٛى٠ ْا تغ٠ ًفطٌا ُغع
ًطفٌا ُف ٟف بٙث و١ؾ٠ بِٚ ٞذضٌا خٍّؽ ًو ًخذر ْا
ًذح وبف١خ لجٌّ ٓ١٠ذضٌا ذؽا ِٓ خػبمشٌبث ًفطٌا َٛم٠ ْا
ضذٞ ااخشٌا ٌٝا يبمزٔلاا
نبػفبِ ٞا ٖبجزٔلاٌ خػبمشٌا ءبٕصأ ًفطٌا خجلاشِ
د أٚ
بقٕزخا
شاعؼخ الشة هج١تِ تغ٠ ٞذضٌا ٟف ًوبؾِ ٞأث سٛؼؾٌا ذٕػ
134
"
زةٌملا
دةٌحولا
ًالت
تلمع
نٌب
نٌحلانلا
ًف
العالم
تكمن
ًف
قدرتهم
على
تحمل
ةٌلوؤسملا
"
كلٌام
كوردا
ٍٝػ ٚأ بٕٙنؽ ٟف ًفطٌا غنر خػبمشٌا ِٓ ءبٙزٔلإا ذٕػ
ٝ ظٙشٍٖػ ذّثشرٚ بٙفزو
شمبػخٌا خٕ١ٕل ٚأ خ١ٌٍّٙا َاذخزعا َذػ
ٚئدساسٖ ٚخشٚعْٗصٌٍٛ ٗثبغزوا ًفطٌا َٛٔ خظؽلاِ
ًطفٌا ٌٝا ٜشخأ خ١ٍ١ّىر خ٠زغأ ءبطػاث َاا أذجر شٙؽا خزع ذؼث
بء ايّو خٍابغٌا ٗجؽ خ٠زغابث أذجر
سص
خّّػذٌّا ِٗثٛجؽٚ
ؾذ٠ذٌبث
.
ج١لٌا اش١خأٚ ،ٗواٛفٌا ، داٚشنخٌا خفبماث أذجر هٌر ذؼث
َؾٌٍٛاٚ
رؼطٝ فْٟأ تغ٠ خ٠زغاا ٖز٘
شمبػخٌا ذلٚ ش١غ ذلٚ
أٚ أوضشَبؼه خمؼٍِ ُص ِٓٚ ةٛو خمؼٍّث ْٛىر خ٠اذجٌا
ًطفٌا شّػ غِ تعبٕزٌبث
ئػطبء غزاءُص ِٓٚ َبؼطٌا ِٓ ذؽاٚ عٕٛث لاٚأ ءذجٌا تغ٠
ًأخش و
3
-
4
ب ؽبثِٗ ٚأ خ١عبغؽ ٞأ خجلاشٌّ َب٠أ
ٓز١ٕع حذٌّ خ١ؼ١جطٌا خػبمشٌا شّزغر
Note: you need to read something about the
difference between bottle and breast feeding
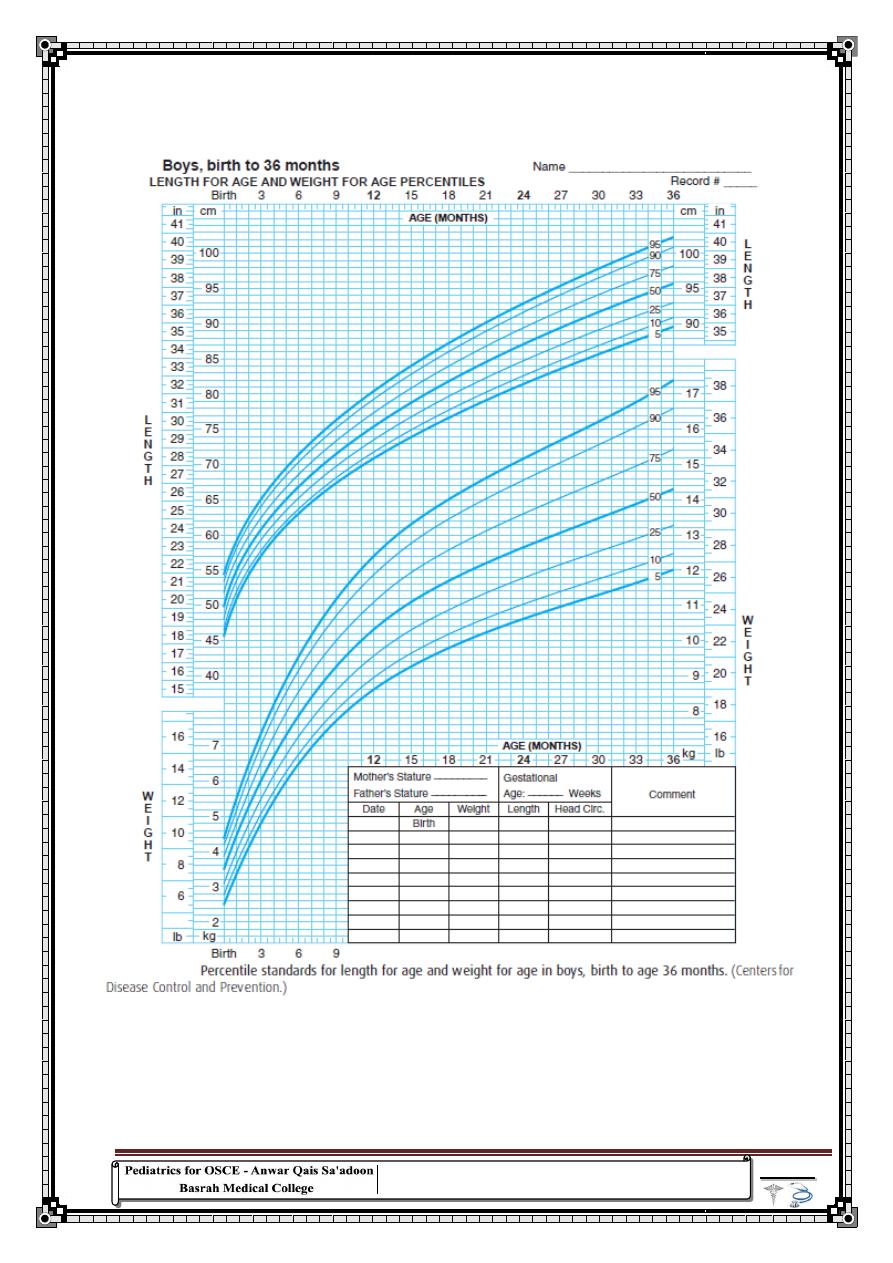
135
"
اةٌحلا
...
ً
فن
الرسم
بدون
ممحاة
"
لون
لاردنر
Appendices
Chart 1 :
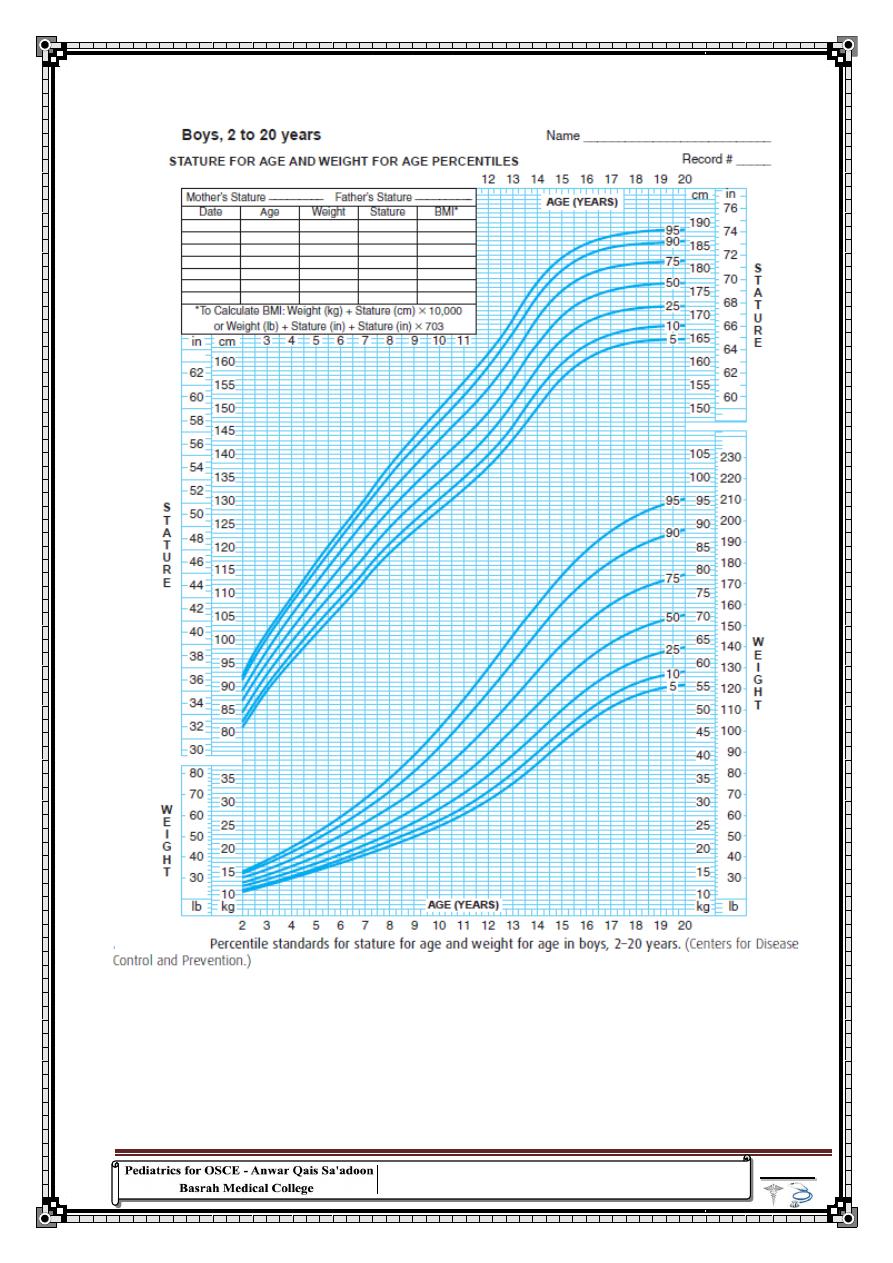
136
"
الحكمة
...
ً
التلربة
اًافاضم
هاٌلا
التأمل
"
رسطو
Chart 2 :
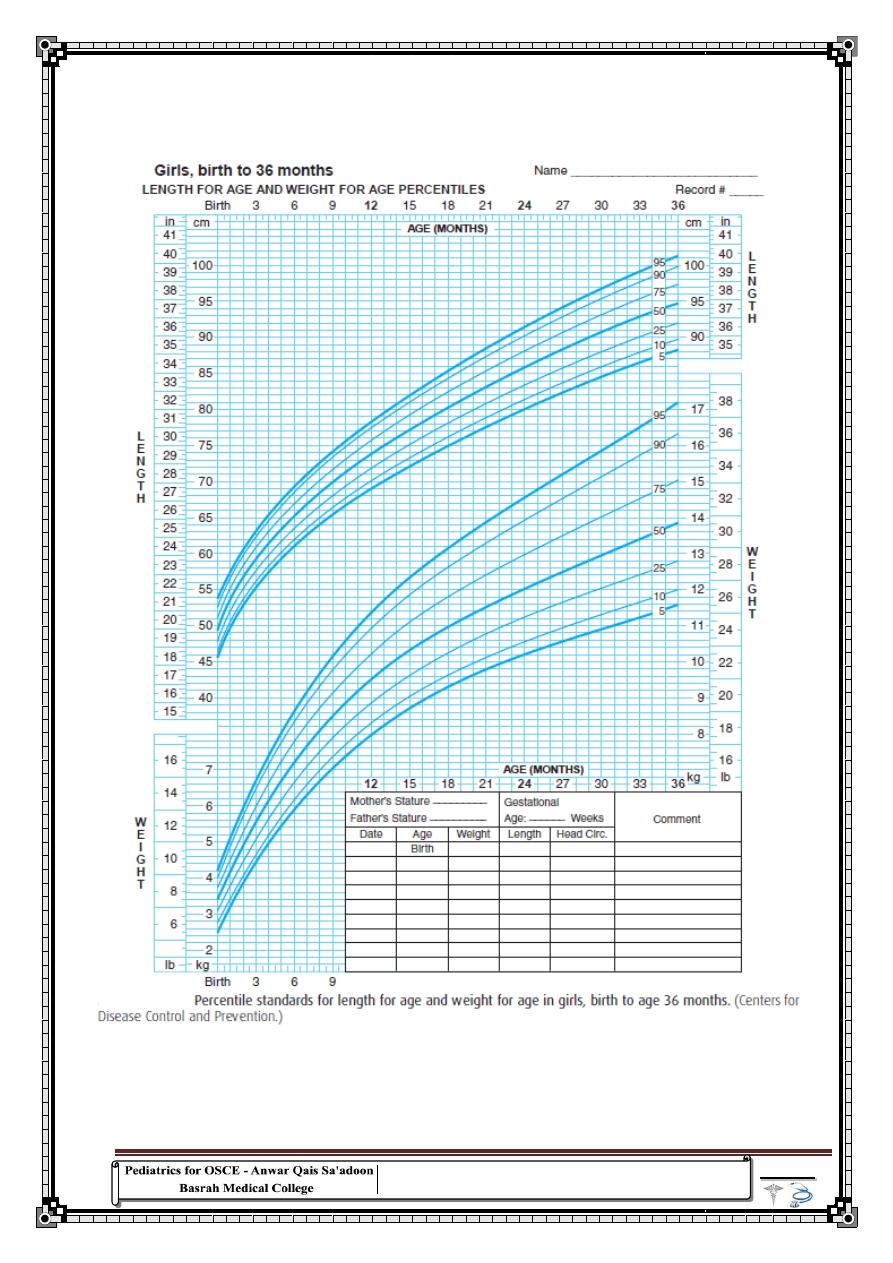
137
"
خِبغزثلاا
..
ٟ٘
بءٕؾٔا
ً٠غؼ
ًو
ػ
ٞء
اًبّ١مزغِ
"
سٌلٌف
لرٌد
Chart 3 :
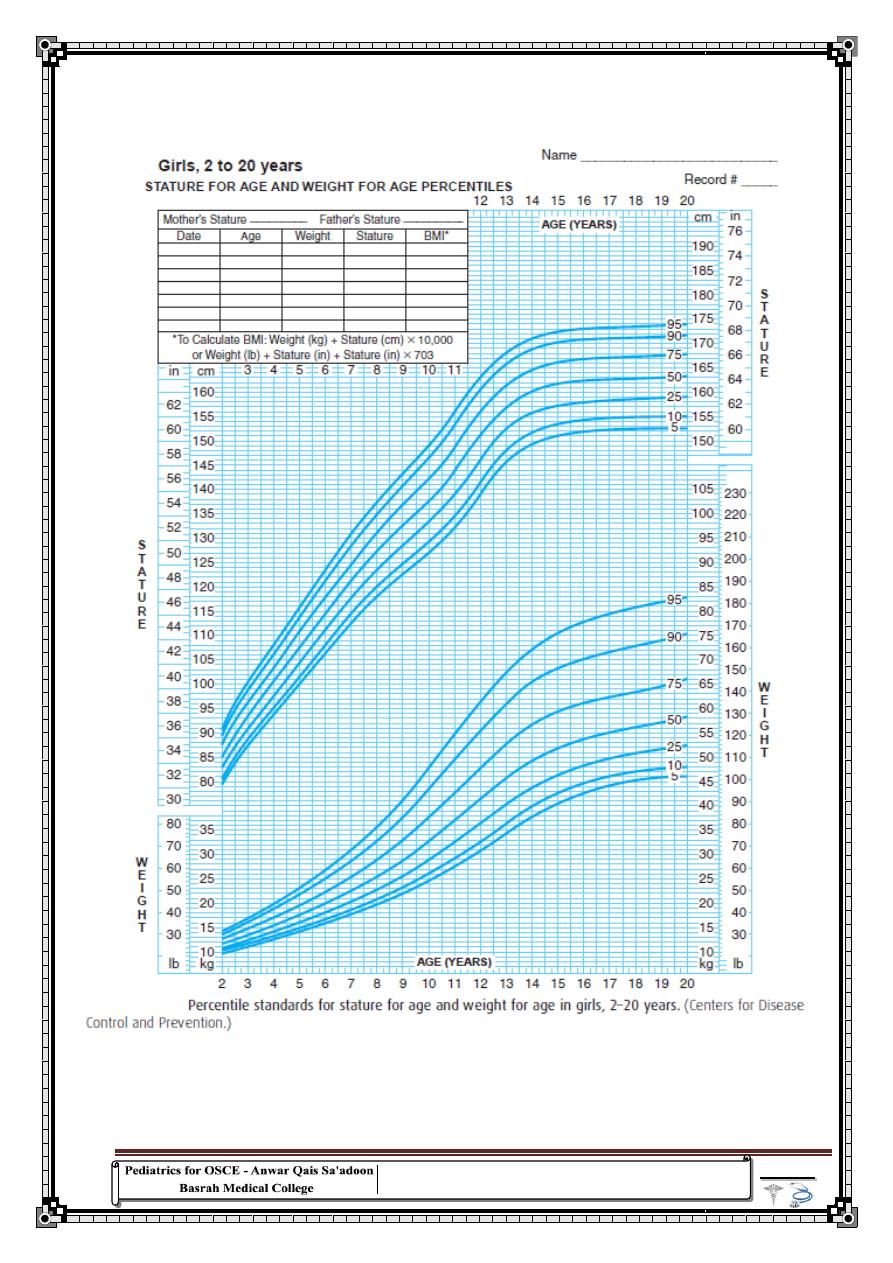
138
"
بٕ٠ذٌ
ؽ١بح
ٚاؽذح
بّػٚ
لش٠ت
عزقجؼ
ِٓ
بمٌّٟا
بِٚ
ٍّٗؼٔ
هلل
٘ٛ
زٌٞا
ع١جمٝ
"
ذّؾِ
ٟ والٍٞػ
Chart 4 :
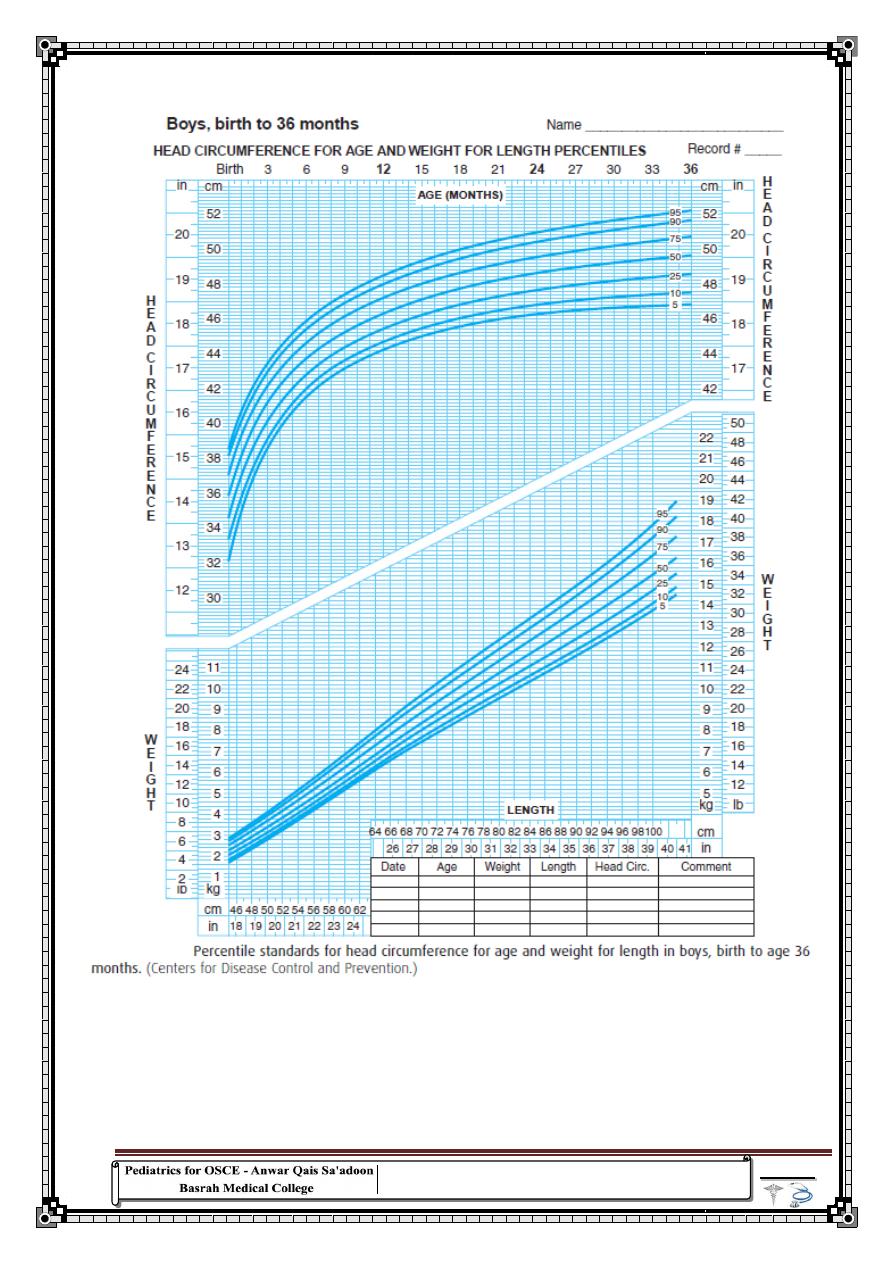
139
"
ذٔأ
رؼ١ؼ
ؽ١بره
شحِ
ٚاؽذح
فمو
،
ٚ
ٓىٌ
ْئ
ػؾزٙب
اًاذ١ع
ْفب
شحِ
ٚاؽذح
رىفٟ
"
آدم
مارشال
Chart 5 :
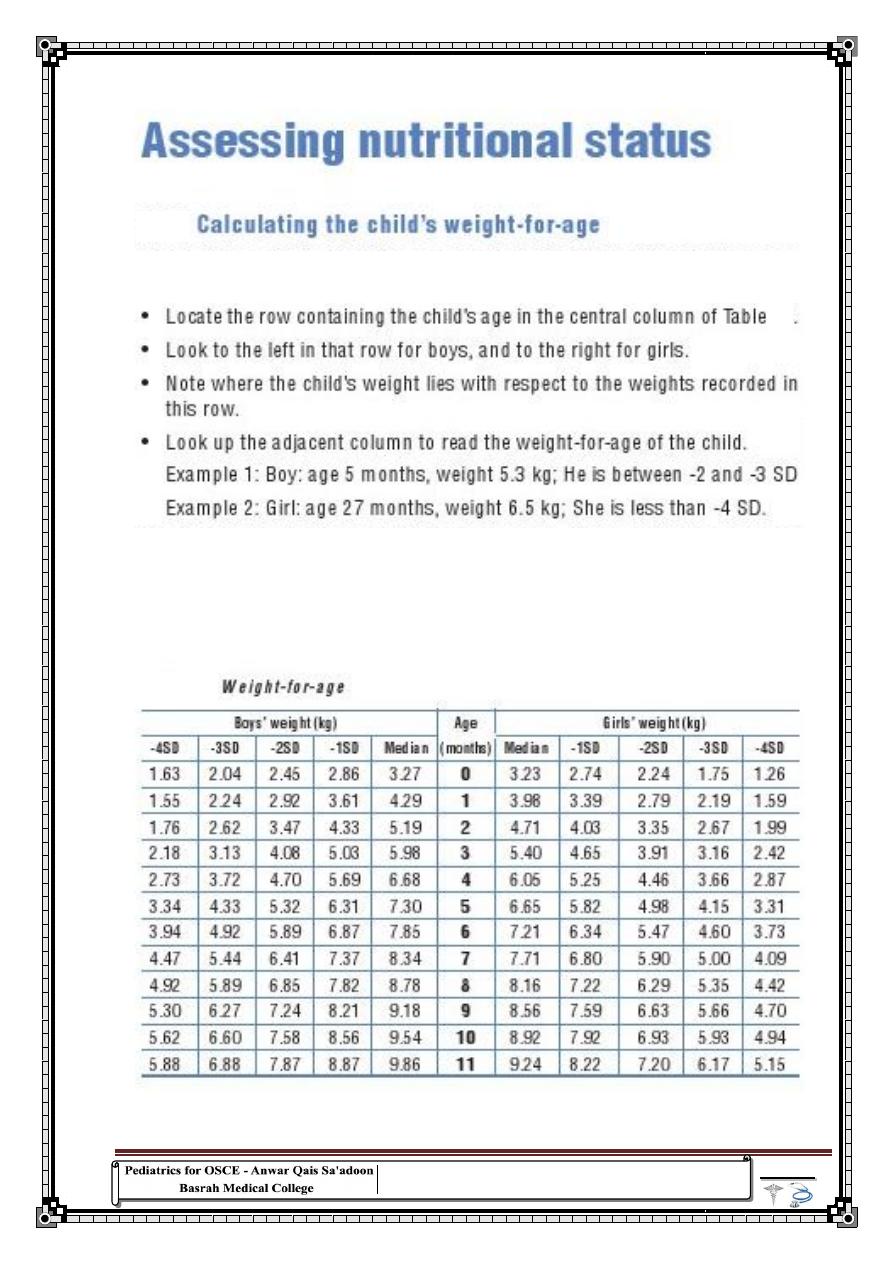
140
"
بِ
فباذح
١بٔذٌا
ٛاعؼخٌا
ارا
ْوب
ؽزاؤن
اًبم١م
؟
"
لون
امزٌلو
Table 7
7
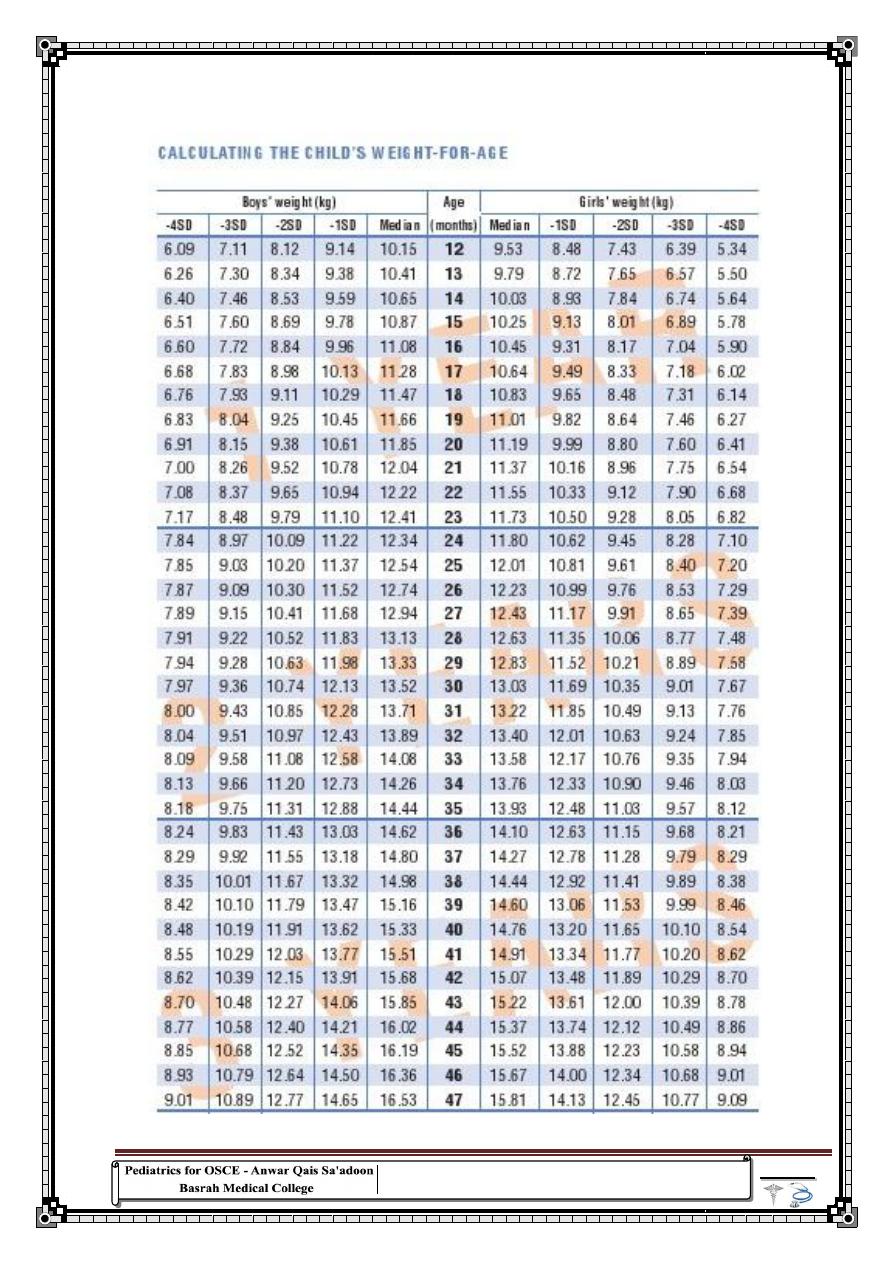
141
"
الرغبة
نصف
اةٌحلا
..
و
الال
مباالة
نصف
الموت
"
ل لبرانٌلخ ناربل
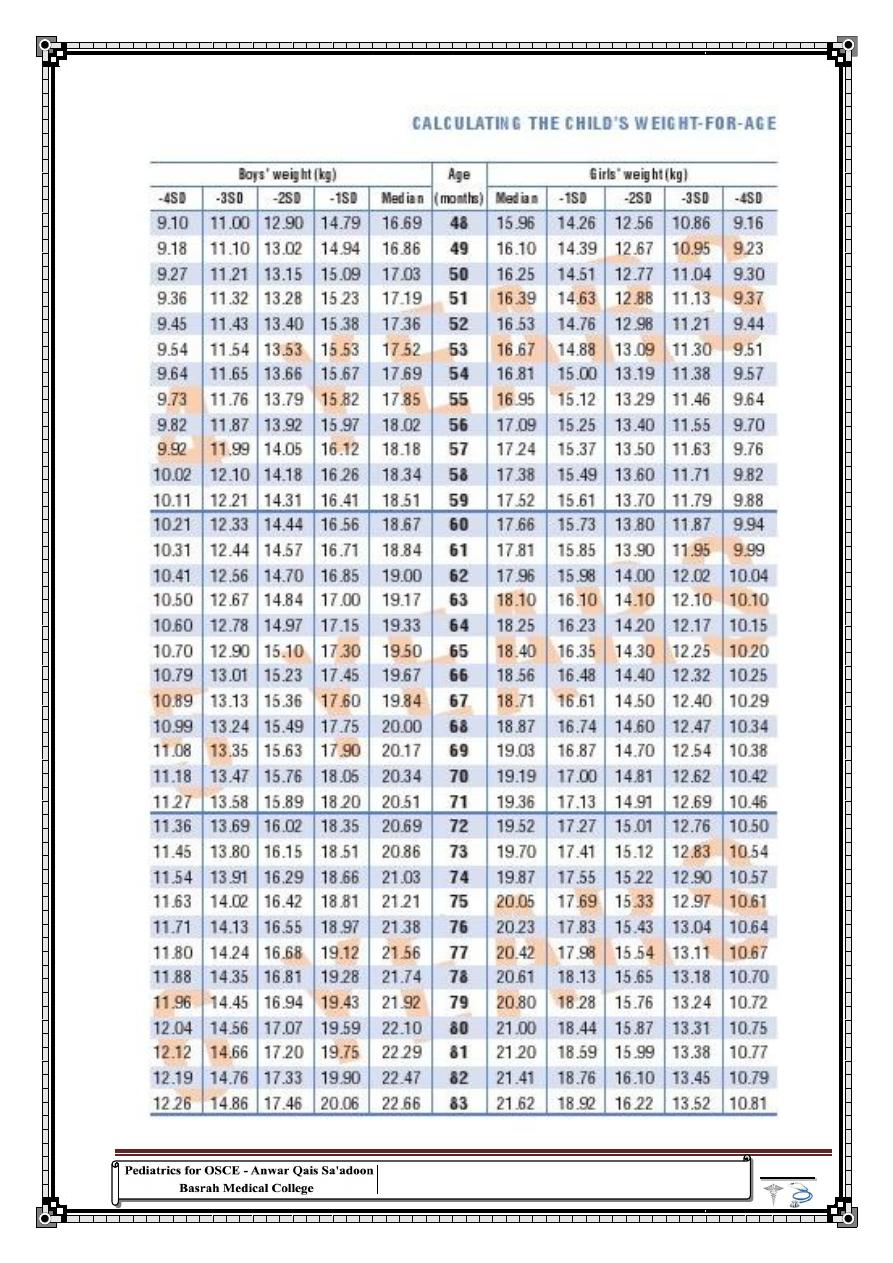
142
"
لو
ننا
فعلنا
ما
نحن
نٌرداق
على
فعله
لصعقنا
نفسنا
"
سونٌدا ساموت
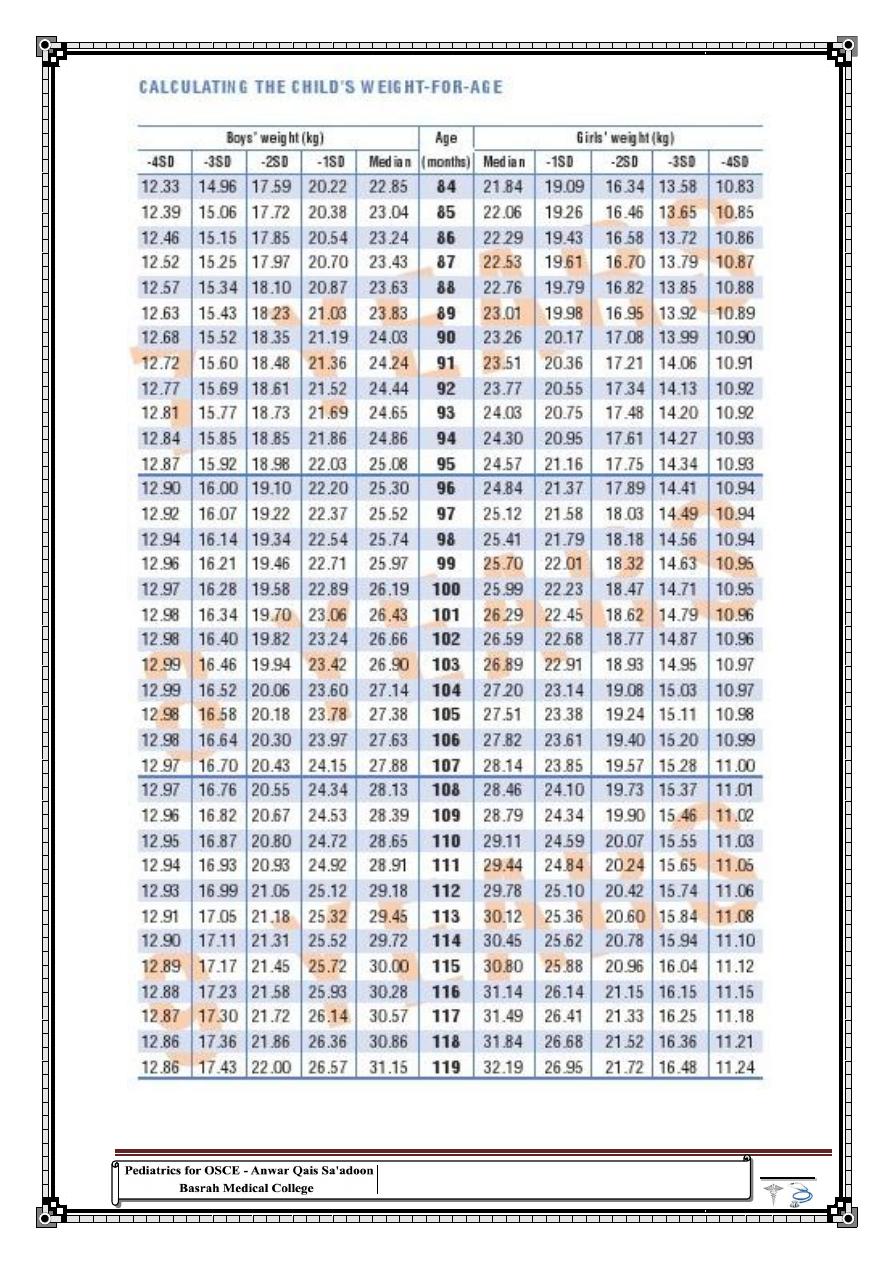
143
"
ِٓ
ااخطبء
ؾباؼخٌا
..
ْا
ٓظٔ
ْثأ
ؽذٚد
بٕرسذل
ٍٝػ
االدسان
ٟ٘
ؽذٚد
بِ
بٕٕىّ٠
ئدساوٗ
"
تشارلز
دٌل
ترٌب
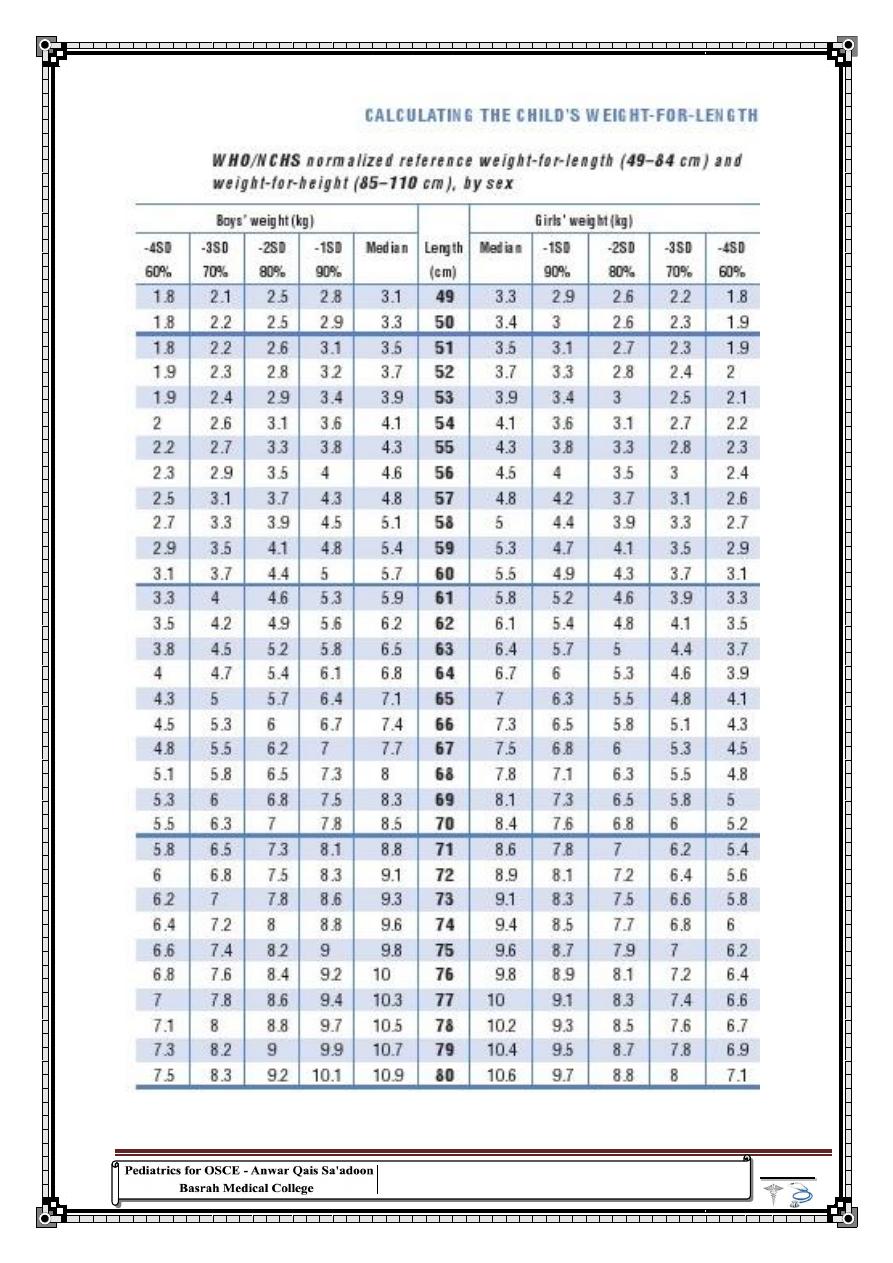
144
"
ْئ
هبلخ
ْغبٔلإا
ٌٛ
ُر
ٙبٍ١فٛر
ذٍجث
ٙبٕىّ٠
ْأ
ذٌٛر
وٙشثبء
ذحٌّ
اعجٛع
ًِوب
"
تٌان
اند
لٌل
Table 8 :
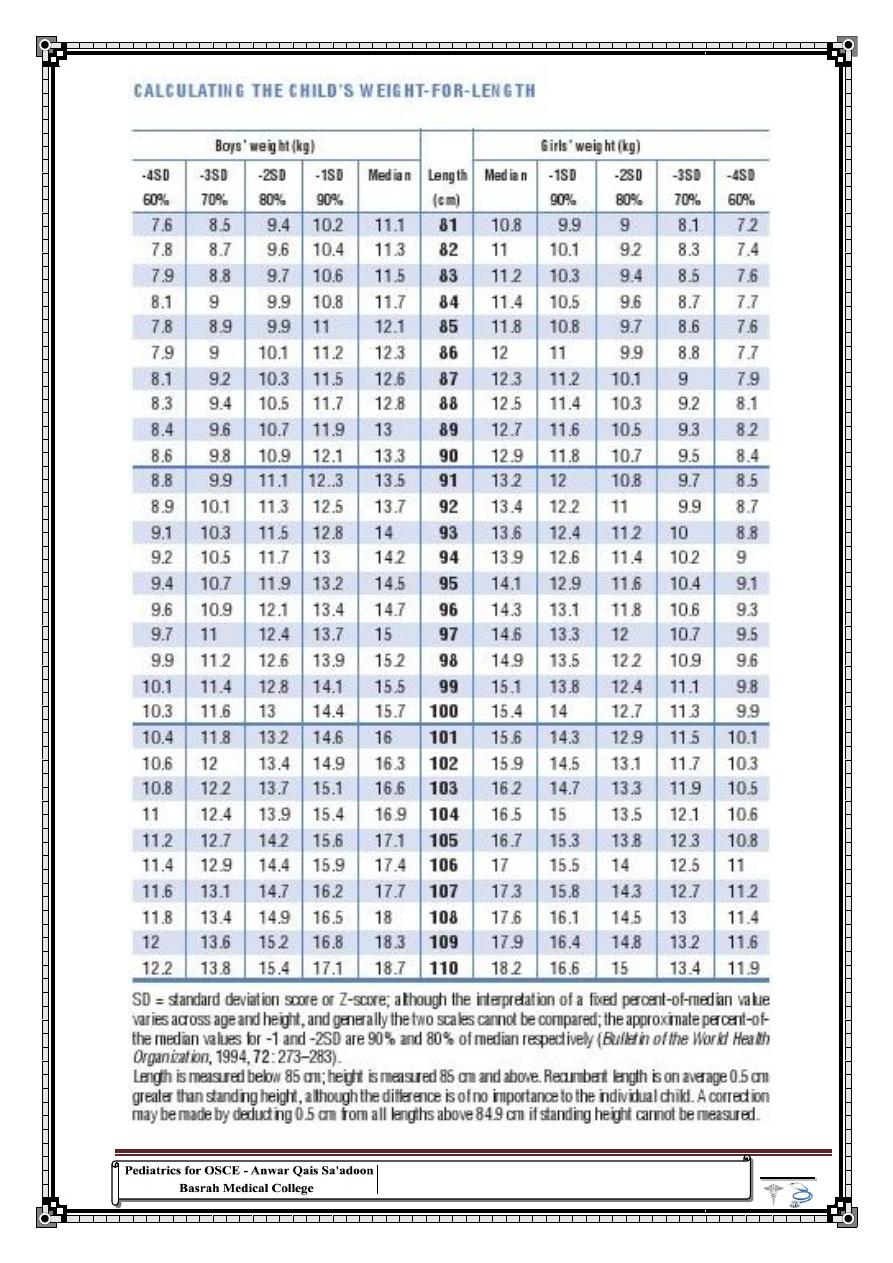
145
"
ًافن
غبصادٔلاا
زٌٟا
ٓىّ٠
رؾم١مٙب
٘ٛ
ْا
نفٟٔ
قشٕػ
زؼخٌّا
ٚ
زؾٛ٠كٌا
ٌٝا
ًّؼٌا
"
ارنولد
ًنبٌوت
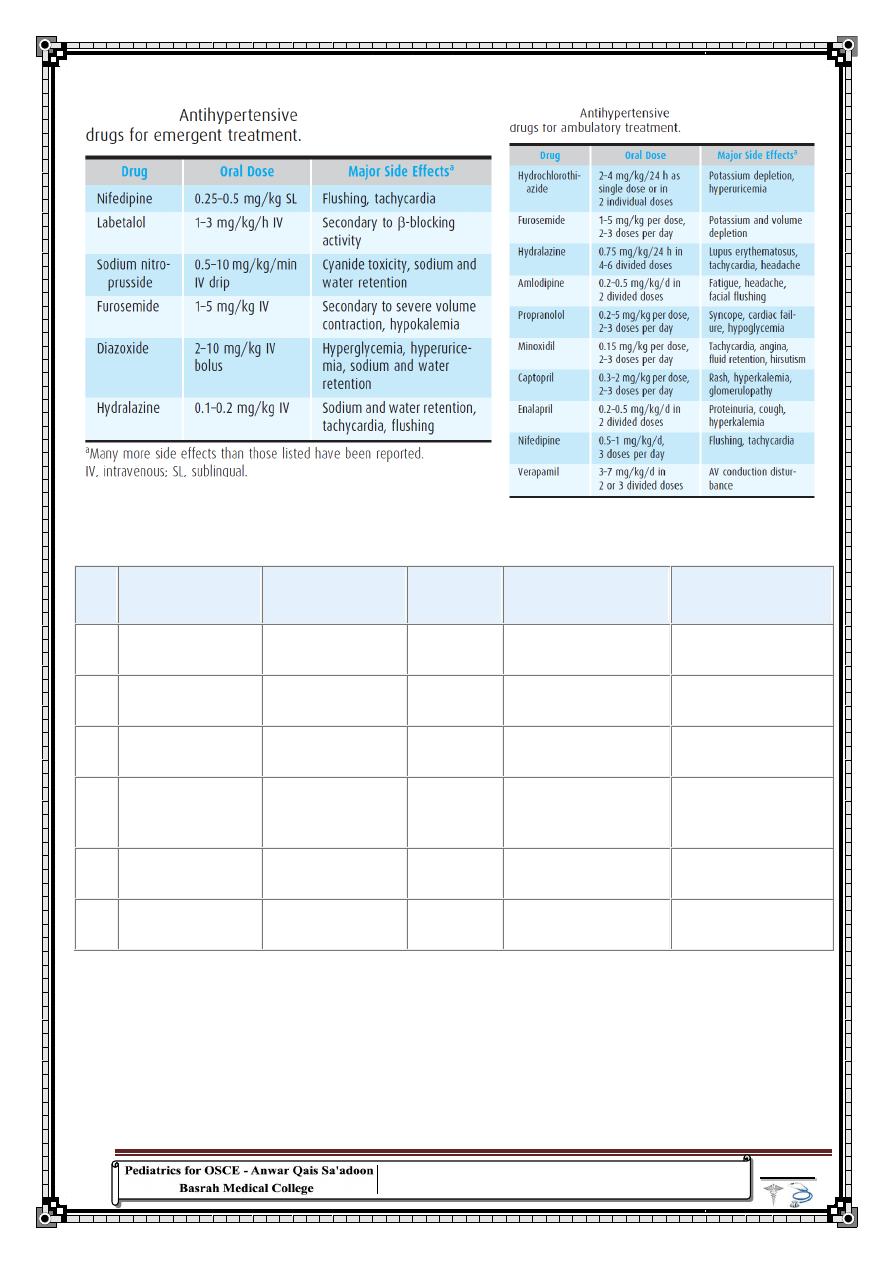
146
"
لقد
اكتشفت
ان
ناك
قةٌرط
واحدة
لمعاللة
الخوف
و
ً
ان
تخرج
و
فٌخت
نفسك
"
اج
داونز
Table 11 -- Growth and Caloric Requirements
AGE
APPROXIMATE
DAILY WEIGHT
GAIN (g)
APPROXIMATE
MONTHLY
WEIGHT GAIN
GROWTH
IN LENGTH
(cm/mo)
GROWTH IN HEAD
CIRCUMFERENCE
(cm/mo)
RECOMMENDED
DAILY ALLOWANCE
(Kcal/kg/day)
0–3
mo
30
2 lb
3.5
2.00
115
3–6
mo
20
1.25 lb
2.0
1.00
110
6–9
mo
15
1 lb
1.5
0.50
100
9–
12
mo
12
13 oz
1.2
0.50
100
1–3
yr
8
8 oz
1.0
0.25
100
4–6
yr
6
6 oz
3 cm/yr
1 cm/yr
90–100
Adapted from National Research Council, Food and Nutrition Board: Recommended Daily
Allowances. Washington, DC, National Academy of Sciences, 1989; Frank D, Silva M, Needlman
R: Failure to thrive: Myth and method. Contemp Pediatr 1993;10:114.
Table 9
Table 10
147
"
من
السهل
ان
تكون
اًاعالش
و
نت
على
مسافة
آمنة
"
سوبٌا
Table 12 : Cerebrospinal Fluid Findings in Central Nervous System Disorders
CONDITION
PRESSURE
(MM H
2
O)
LEUKOCYTES (MM
3
)
PROTEIN
(MG/DL)
GLUCOSE
(MG/DL)
COMMENTS
Normal
50–80
<5, ≥75% lymphocytes
20–45
>50 (or 75%
serum glucose)
COMMON FORMS OF MENINGITIS
Acute bacterial
meningitis
Usually
elevated
(100–300)
100–10,000 or more;
usually 300–2,000;
PMNs predominate
Usually
100–500
Decreased,
usually <40 (or
<50% serum
glucose)
Organisms usually seen
on Gram stain and
recovered by culture.
Partially treated
bacterial meningitis
Normal or
elevated
5–10,000; PMNs usual
but mononuclear cells
may predominate if
pretreated for extended
period of time
Usually
100–500
Normal or
decreased
Organisms may be seen
on Gram stain.
Pretreatment may
render CSF sterile.
Antigen may be
detected by
agglutination test
Viral meningitis or
meningoencephalitis
Normal or
slightly
elevated (80–
150)
Rarely >1,000 cells.
Eastern equine
encephalitis and
lymphocytic
choriomeningitis (LCM)
may have cell counts of
several thousand. PMNs
early but mononuclear
cells predominate
through most of the
course
Usually 50–
200
Generally normal;
may be decreased
to <40 in some
viral diseases,
particularly
mumps (15–20%
of cases)
HSV encephalitis is
suggested by focal
seizures or by focal
findings on CT or MRI
scans or EEG.
Enteroviruses and HSV
infrequently recovered
from CSF. HSV and
enteroviruses may be
detected by PCR of CSF
UNCOMMON FORMS OF MENINGITIS
Tuberculous
meningitis
Usually
elevated
10–500; PMNs early, but
lymphocytes predominate
through most of the
course
100–
3,000;may
be higher in
presence of
block
<50 in most
cases; decreases
with time if
treatment is not
provided
Acid-fast organisms
almost never seen on
smear. Organisms may
be recovered in culture
of large volumes of
CSF. Mycobacterium
tuberculosis may be
detected by PCR of CSF
Fungal meningitis
Usually
elevated
5–500; PMNs early but
mononuclear cells
predominate through
most of the course.
Cryptococcal meningitis
may have no cellular
inflammatory response
25–500
<50;decreases
with time if
treatment is not
provided
Budding yeast may be
seen. Organisms may be
recovered in culture.
Cryptococcal antigen
(CSF and serum) may
be positive in
cryptococcal infection
Syphilis (acute) and
leptospirosis
Usually
elevated
50–500;lymphocytes
predominate
50–200
Usually normal
Positive CSF serology.
Spirochetes not
demonstrable by usual
techniques of smear or
culture; darkfield
examination may be
positive
Amebic (Naegleria)
Elevated
1,000–10,000 or more;
PMNs predominate
50–500
Normal or
slightly decreased
Mobile amebae may be
seen by hanging-drop
examination of CSF at
room temperature
148
"
٠زؼشك
بءٕجغٌا
ؾغبسادٌ
أوضش
وض١شا
ِٓ
ألٛ٠بء
ؾخق١خٌا
"
توماس
فرسونٌل
Table 13 -- Antibiotics Used for the Treatment of Bacterial meningitis
NEONATES
DRUG
0–7 Days
8–28 Days
INFANTS AND
CHILDREN
Amikacin
[†][‡]
15–20 divided q12h
20–30 divided q8h
20–30 divided q8h
Ampicillin
200–300 divided q8h
300 divided q4h or q6h 300 divided q4–6h
Cefotaxime
100 divided q12h
150–200 divided q8h or
q6h
200–300 divided q8h or
q6h
Ceftriaxone
[§]
—
—
100 divided q12h or q24h
Ceftazidime
150 divided q12h
150 divided q8h
150 divided q8h
Gentamicin
[†][‡]
5 divided q12h
7.5 divided q8h
7.5 divided q8h
Meropenem
—
—
120 divided q8h
Nafcillin
100–150 divided q8h or
q12h
150–200 divided q8h or
q6h
150–200 divided q4h or
q6h
Penicillin G
250,000–450,000 divided
q8h
450,000 divided q6h
450,000 divided q4h or
q6h
Rifampin
—
—
20 divided q12h
Tobramycin
[†][‡]
5 divided q12h
7.5 divided q8h
7.5 divided q8h
Vancomycin
[†][‡]
30 divided q12h
30–45 divided q8h
60 divided q6h
Modified from Klein JO:Antimicrobial treatment and prevention of meningitis. Pediatr Ann 1994;23:76;and from Kliegman RM,
Greenbaum LA, Lye PS: Practical Strategies in Pediatric Diagnosis and Therapy, 2nd ed. Philadelphia, Elsevier, 2004, p 963.
Table 14 :
Age-specific Vital Signs and Laboratory Variables (Lower Values for Heart Rate,
Leukocyte Count, and Systolic Blood Pressure are for the 5th and Upper Values for Heart Rate,
Respiration Rate, or Leukocyte Count for the 95th Percentile)
HEART RATE (BEATS/MIN)
RESPIRATORY RATE
(BREATHS/MIN)
LEUKOCYTE COUNT
(LEUKOCYTES × 10
3
/MM)
SYSTOLIC BLOOD
PRESSURE (MM HG)
AGE
GROUP
TACHYCARDIA BRADYCARDIA
0 day–1
wk
>180
<100
>50
>34
<65
1 wk–1
mo
>180
<100
>40
>19.5 or <5
<75
1 mo–1
yr
>180
<90
>34
>17.5 or <5
<100
2–5 yr
>140
NA
>22
>15.5 or <6
<94
6–12 yr
>130
NA
>18
>13.5 or <4.5
<105
13–18 yr >110
NA
>14
>11 or <4.5
<117
From Goldstein B, Giroir B, Randolph A, et al
149
"
فلتكن
شلاعا
و
تخاطر
فال،
مكنٌ
استبدال
الخبرة
بأي
ءًش
آخر
"
باولو
لوٌوك
Table 15 : Normal values of blood tests
ANALYTE OR PROCEDURE
SPECIMEN
REFERENCE
VALUES (USA)
CONVERSION
FACTOR
REFERENCE
VALUES (SI)
COMMENTS
Complete Blood Count
Hematocrit (HCT, Hct)
Calculated from mean
corpuscular volume (MCV)
and RBC count (electronic
displacement or laser)
W(E)
% of packed red
cells (V red cells/V
whole blood cells ×
100
Volume fraction
(V red cells/V
whole blood)
1 day (cap)
48–69%
× 0.01
0.48–0.69
2 days
48–75%
0.48–0.75
3 days
44–72%
0.44–0.72
2 mo
28–42%
0.28–0.42
6–12 yr
35–45%
0.35–0.45
12–18 yr M
37–49%
0.37–0.49
F
36–46%
0.36–0.46
18–49 yr M
41–53%
0.41–0.53
F
36–46%
0.36–0.46
Hemoglobin (Hb)
W(E)
g/dL
mmol/L
1–3 days (cap) 14.5–22.5
× 0.155
2.25–3.49
MW Hb =
64,500
2 mo
9.0–14.0
1.40–2.17
6–12 yr
11.5–15.5
1.78–2.40
12–18 yr M
13.0–16.0
2.02–2.48
F
12.0–16.0
1.86–2.48
18–49 yr M
13.5–17.5
2.09–2.27
F
12.0–16.0
1.86–2.48
P(H)
See Chemical
Elements
Erythrocyte indices (RBC
indices)
Mean corpuscular hemoglobin
(MCH)
W(E)
pg/cell
fmol/cell
Birth
31–37
× 0.0155
0.48–0.57
1–3 days (cap) 31–37
0.48–0.57
1 wk–1 mo
28–40
0.43–0.62
2 mo
26–34
0.40–0.53
3–6 mo
25–35
0.39–0.54
0.5–2 yr
23–31
0.36–0.48
2–6 yr
24–30
0.37–0.47
6–12 yr
25–33
0.39–0.51
12–18 yr
25–35
0.39–0.54
18–49 yr
26–34
0.40–0.53
Mean corpuscular hemoglobin
concentration (MCHC)
W(E)
% Hb/cell or g
Hb/dL RBC
mmol Hb/L RBC
Birth
30–36
× 0.155
4.65–5.58
1–3 days (cap) 29–37
4.50–5.74
150
ANALYTE OR PROCEDURE
SPECIMEN
REFERENCE
VALUES (USA)
CONVERSION
FACTOR
REFERENCE
VALUES (SI)
COMMENTS
1–2 wk
28–38
4.34–5.89
1–2 mo
29–37
4.50–5.74
3 mo–2 yr
30–36
4.65–5.58
2–18 yr
31–37
4.81–5.74
>18 yr
31–37
4.81–5.74
Mean corpuscular volume
(MCV)
W(E)
μ m
3
fL
1–3 days (cap) 95–121
× 1
95–121
0.5–2 yr
70–86
70–86
6–12 yr
77–95
77–95
12–18 yr M
78–98
78–98
F
78–102
78–102
18–49 yr M
80–100
80–100
F
80–100
80–100
Leukocyte count (WBC count) W(E)
× 1,000 cells/mm
3
(μ L)
× 10
9
cells/L
Birth
9.0–30.0
× 1
9.0–30.0
24 hr
9.4–34.0
9.4–34.0
1 mo
5.0–19.5
5.0–19.5
1–3 yr
6.0–17.5
6.0–17.5
4–7 yr
5.5–15.5
5.5–15.5
8–13 yr
4.5–13.5
4.5–13.5
Adult
4.5–11.0
4.5–11.0
Leukocyte differential
W(E)
%
Number fraction
Myelocytes
0%
× 0.01
0
Neutrophils (―bands‖)
3–5%
0.03–0.05
Neutrophils (―segs‖)
54–62%
0.54–0.62
Lymphocytes
25–33%
0.25–0.33
Monocytes
3–7%
0.03–0.07
Eosinophils
1–3%
0.01–0.03
Basophils
0–0.75%
0–0.0075
Cells/mm
3
(μ L)
× 10
6
cells/L
Myelocytes
0
× 1
0
Neutrophils (―bands‖)
150–400
150–400
Neutrophils (―segs‖)
3,000–5,800
3,000–5,800
Lymphocytes
1,500–3,000
1,500–3,000
Monocytes
285–500
285–500
Eosinophils
50–250
50–250
Basophils
15–50
15–50
Platelet count (thrombocyte
count)
W(E)
× 10
3
/mm
3
(μ L)
× 10
9
/L
Newborn 84–478 (after 1 wk, same
as adult)
× 10
6
84–478
(Buck, 1996)
Adult 150–400
150–400
"
ئ
را
ٌُ
ُرزؾى
فٟ
هٍمػ
ْفب
اًبقخؽ
آخش
ًع١فؼ
"
لون
الستون
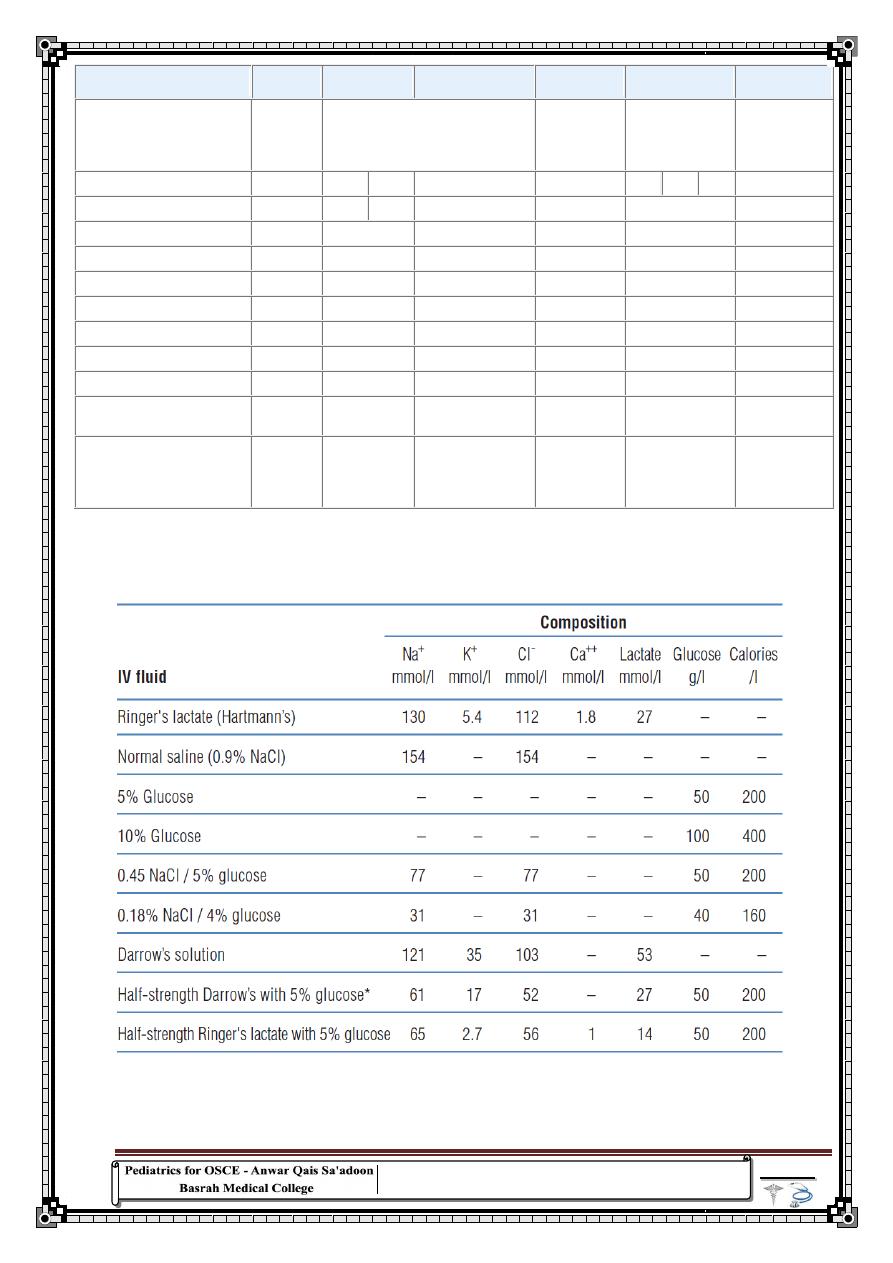
151
ANALYTE OR PROCEDURE
SPECIMEN
REFERENCE
VALUES (USA)
CONVERSION
FACTOR
REFERENCE
VALUES (SI)
COMMENTS
Reticulocyte count
W(E, H,
O)
Adults 0.5–1.5% of erythrocytes or
25,000–75,000/mm
3
(μ L)
× 0.01
0.005–0.015
(number fraction)
or 25,000–75,000
× 10
6
/L
× 10
6
%
Number fraction
W(cap)
1 day
0.4–6.0%
× 0.01
0.004–0.060
7 days
<0.1–1.3%
<0.001–0.013
1–4 wk
<1.0–1.2%
<0.001–0.012
5–6 wk
<0.1–2.4%
<0.001–0.024
7–8 wk
0.1–2.9%
0.001–0.029
9–10 wk
<0.1–2.6%
<0.001–0.026
11–12 wk
0.1–0.3%
0.001–0.013
Alanine aminotransferase
(ALT, SGPT)
S
0–5 days
6–50 U/L
× 1
6–50 U/L
37°bw
1–19 yr
5–45
5–45
(Lockitch,
Halstead, and
Albersheim,
1988)
Table 16: IV fluid composition
"
مائة
شخص
تقدمونٌ
خطوة
افضل
من
شخص
واحد
تقدمٌ
مائة
خطوة
"
ًشٌوك
تازوكاموتو
152
Table 17 : The Thalassemias
THALASSEMIA
GLOBIN
GENOTYPE
FEATURES
EXPRESSION
HEMOGLOBIN
ELECTROPHORESIS
α-THALASSEMIA
1 gene deletion
-,α/α,α
Normal
Normal
Newborn: Bart 1–2%
2 gene deletion trait
-,α/-,α-,-/
α,α
Microcytosis, mild
hypochromasia
Normal, mild anemia
Newborn: Bart 5–10%
3 gene deletion
hemoglobin H
-,-/-,α
Microcytosis,
hypochromic
Mild anemia, transfusions not
required
Newborn: Bart 20–30%
2 gene deletion +
Constant Spring
-,-/α,αConstant
Spring
Microcytosis,
hypochromic
Moderate to severe anemia,
transfusion, splenectomy
2–3% Constant Spring, 10–15%
hemoglobin H
4 gene deletion
-,-/-,-
Anisocytosis,
poikilocytosis
Hydrops fetalis
Newborn: 89–90% Bart with
Gower 1 and 2 and Portland
Nondeletional
α,α/α,αvariant
Microcytosis, mild
anemia
Normal
1–2% variant hemoglobin
β-THALASSEMIA
β
0
or β
+
heterozygote:trait
β°/A,β
+
/A
Variable
microcytosis
Normal
Elevated A
2
, variable elevation
of F
β°-Thalassemia
β°/β°, β
+
/β°, E/β°
Microcytosis,
nucleated RBCs
Transfusion-dependent
F 98%, A
2
2%
E 30–40%
β
+
-Thalassemia
severe
β
+
/β
+
Microcytosis,
nucleated RBCs
Transfusion-
dependent/thalassemia intermedia
F 70–95%, A
2
2%, trace A
Silent
β
+
/A
Microcytosis
Normal with only microcytosis
A
2
3.3–3.5%
β
+
/β
+
Hypochromic,
microcytosis
Mild to moderate anemia
A
2
2–5%, F 10–30%
Dominant (rare)
B°/A
Microcytosis,
abnormal RBCs
Moderately severe anemia,
splenomegaly
Elevated F and A
2
δ-Thalassemia
A/A
Normal
Normal
A
2
absent
(δβ)°-Thalassemia
(δβ)°/A
Hypochromic
Mild anemia
F 5–20%
(δβ)
+
-Thalassemia
Lepore
βLepore/A
Microcytosis
Mild anemia
Lepore 8–20%
Lepore
βLepore/βLepore
Microcytic,
hypochromic
Thalassemia intermedia
F 80%, Lepore 20%
γδβ-Thalassemia
(γAγδβ)°/A
Microcytosis,
microcytic,
hypochromic
Moderate anemia, splenomegaly,
homozygote: thalassemia
intermedia
Decreased F and A
2
compared
with δβ-thalassemia
γ-Thalassemia
(γAγG)°/A
Microcytosis
Insignificant unless homozygote
Decreased F
HEREDITARY PERSISTENCE OF FETAL HEMOGLOBIN
Deletional
A/A
Microcytic
Mild anemia
F 100% homozygotes
Nondeletional
A/A
Normal
Normal
F 20–40%
In α-thalassemia, there are relatively fewer α-globin chains and an excess of β- and γ-globin chains. These
excess chains form Bart's hemoglobin (γ
4
) in fetal life and Hb H (β
4
) after birth. These abnormal tetramers
are not as lethal, but lead to extravascular hemolysis. Prenatally, a fetus with α-thalassemia may become
symptomatic because Hb F requires sufficient α-globin gene production, whereas postnatally, infants with
β-thalassemia become symptomatic because Hb A requires adequate production of β-globin genes
"
كل
ةٌادب
لها
ةٌاهن
،
و
ذذ
ةٌاهنلا
ً
ةٌادبلا
ءًشل
آخر
"
افالطون
153
متت حبمد اهلل
References
1)
Kleigman RM , Stanton BF , Jenson HB, Behrman RE .Nelson text
book of pediatrics .18
th
ed. WB Saunders, Philadelphia, 2007
2)
William WH, Mayron JL, Judith MS, Robin RD, Current Diagnosis
and Treatment Pediatrics.19
th
ed. McGraw Hill, 2009
3)
Joanne S, Terry N. Pediatric hand book .6
th
ed. Melbourne,2000
4)
Hassan MK, Assim AK, Ashor AI, Al-Ethan B. History-taking and
clinical examination of the child. Basrah
5)
WHO. Pocket book of hospital care for children: guidelines for the
management of common illnesses with limited resources,
2005.
6)
Elizabeth K. Current Clinical Strategies Pediatric History and Physical
Examination.4
th
ed. Laguna Hills, California. 2003
7)
Strak SK, Al-Khaqani FA. Skill in clinical history taking. 2
nd
ed.
Basrah, 2011
8)
Zaid A, Qais A, Abdul-Rahman M, Abdul-Ameer A, Muhammad H,
Sa'ad A, Jamal B,Mustafa R, Adnan I, Qasim Z, Anmar S, Abdul-
Muhsin Z, Adnan M, Hasan W. Pediatrics history guide for OSCE.
Basrah , 2011
9)
Nabeel A. Your guide to be a good man: Gardens of the wisdom: well-
chosen remarks from the life's school . 1
st
ed. 2010 (Arabic)
"
ًف
كل
ش
يء
،
ةٌاهنلا
ً
األ م
"
رسطو
