Metabolic bone diseases
Bone functions1- support
2- protection3- leverage
4- minerals reservoir
Bone composition
1- the matrix2- bone mineral
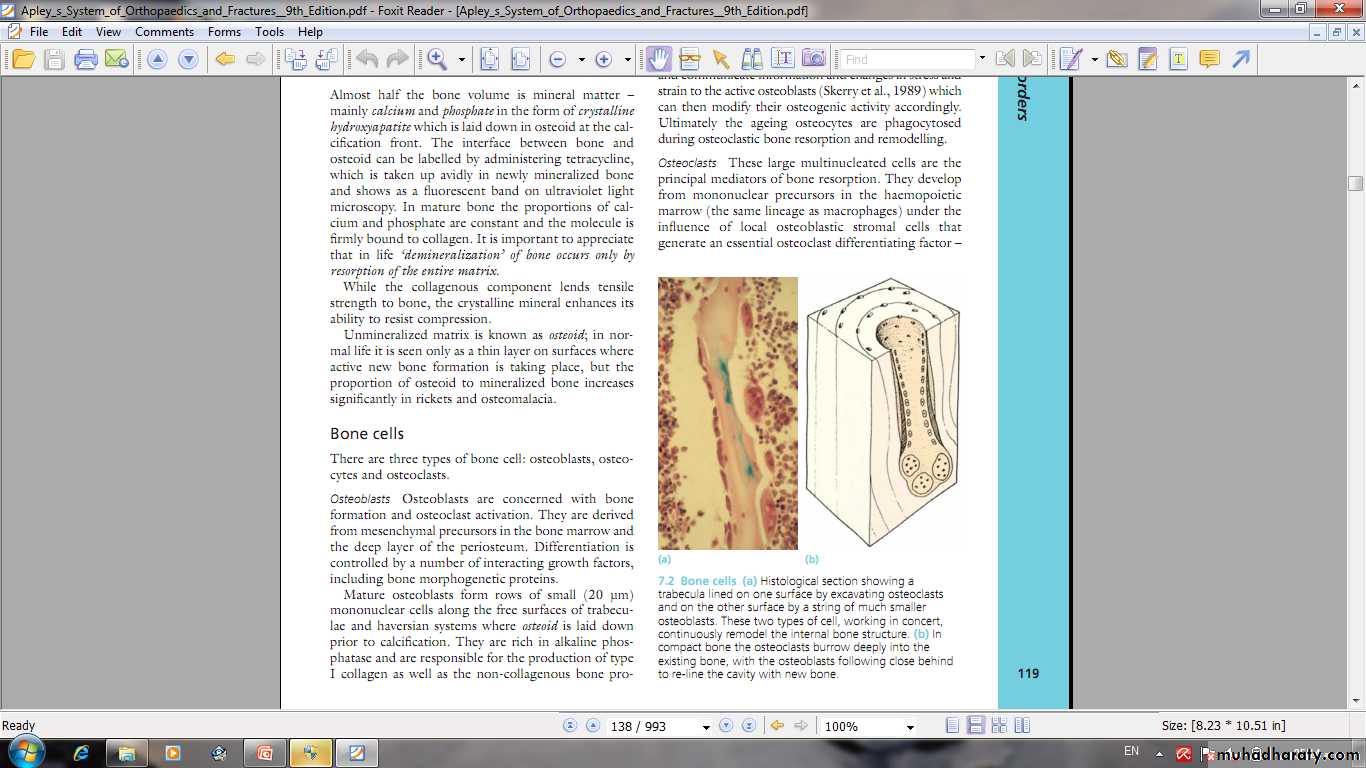
3- bone cells
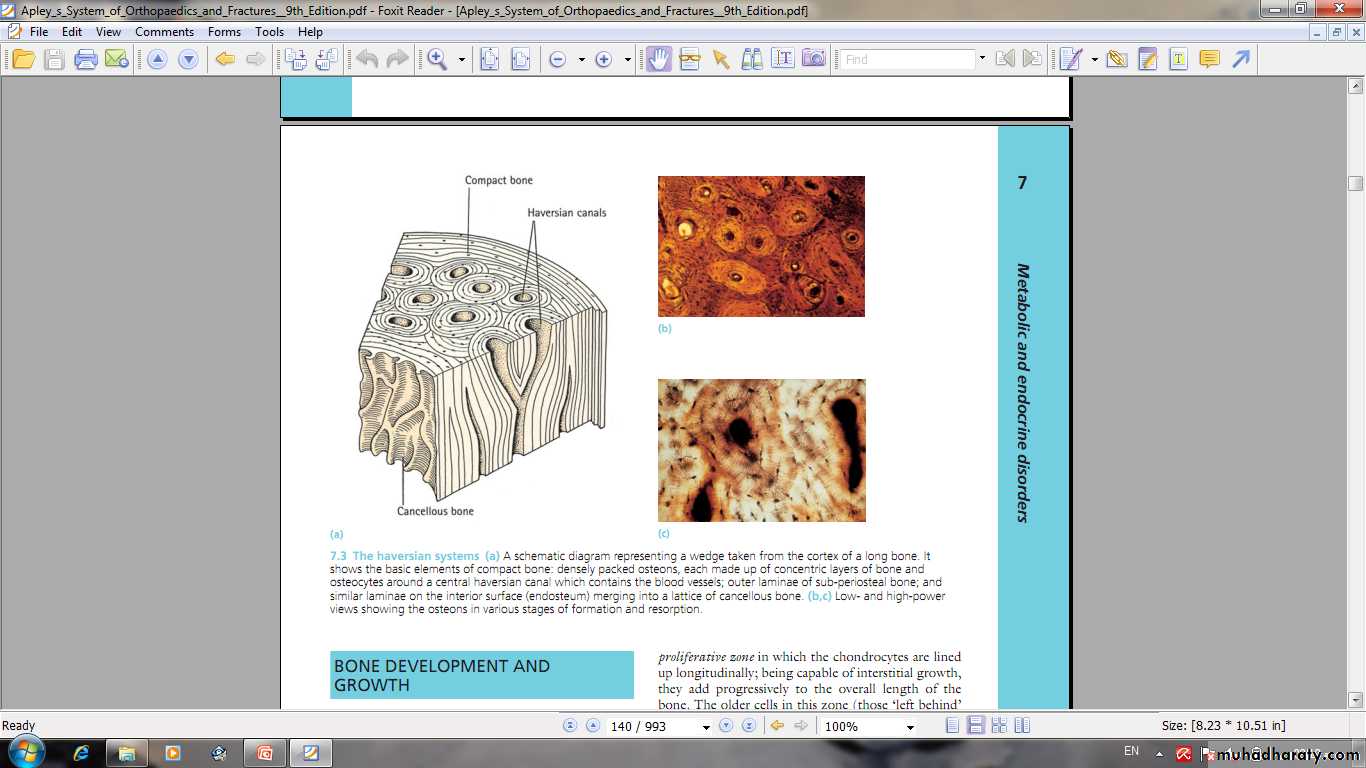
Bone structure
Compact boneCancellous bone
Haversian system
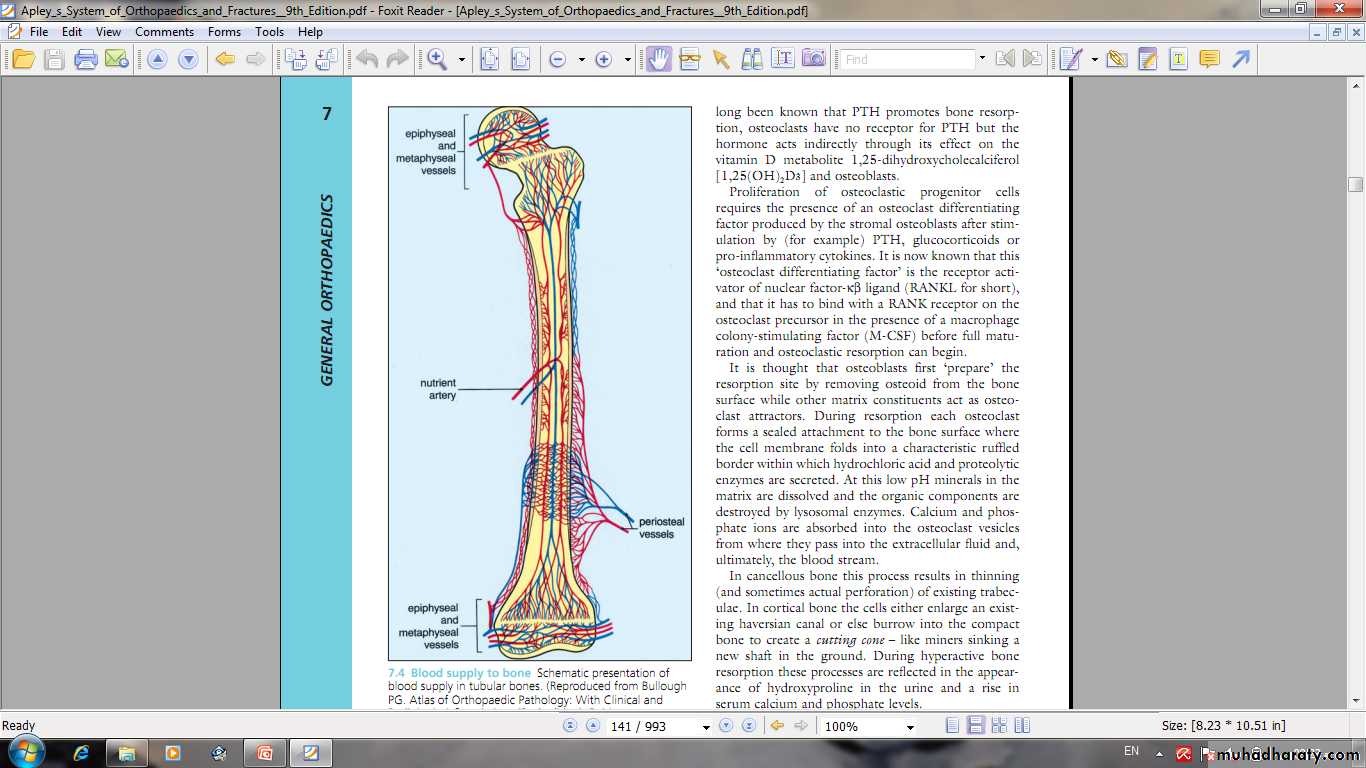
Bone blood supply
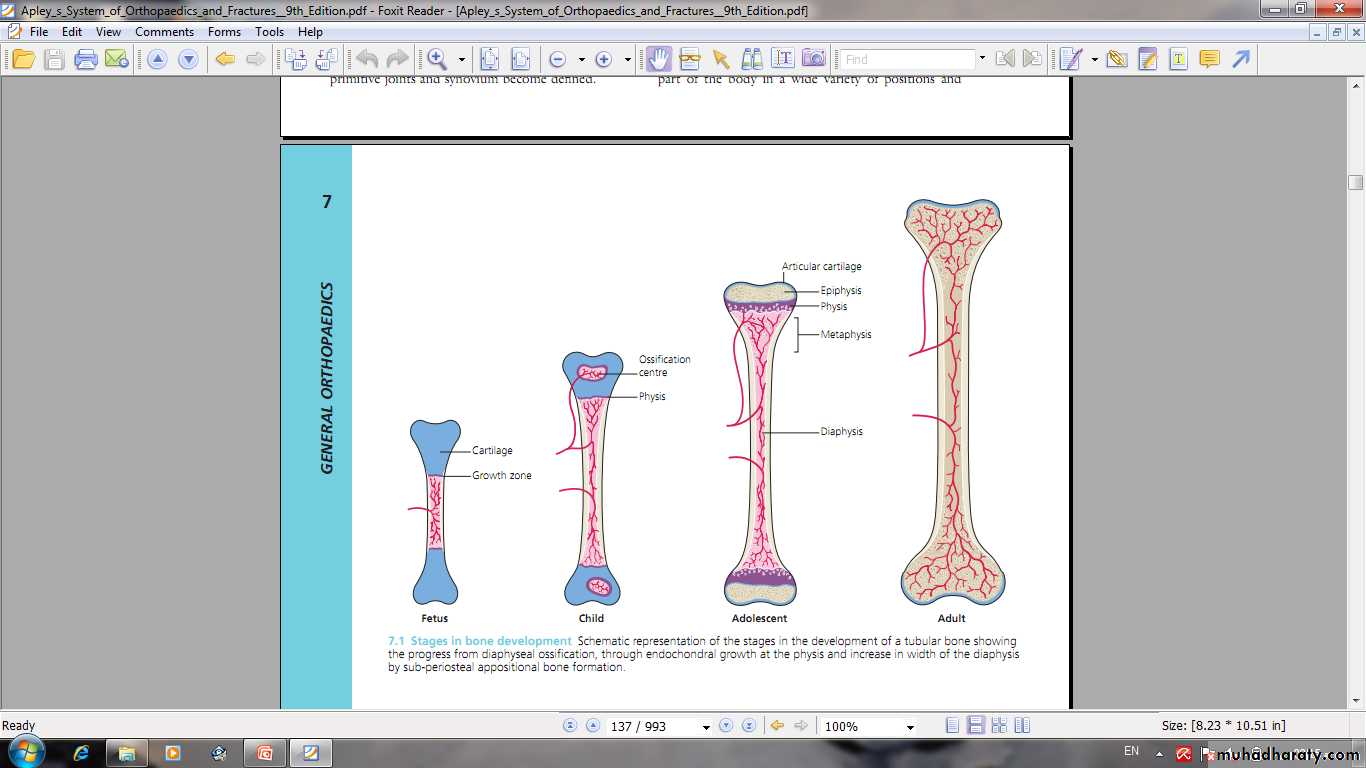
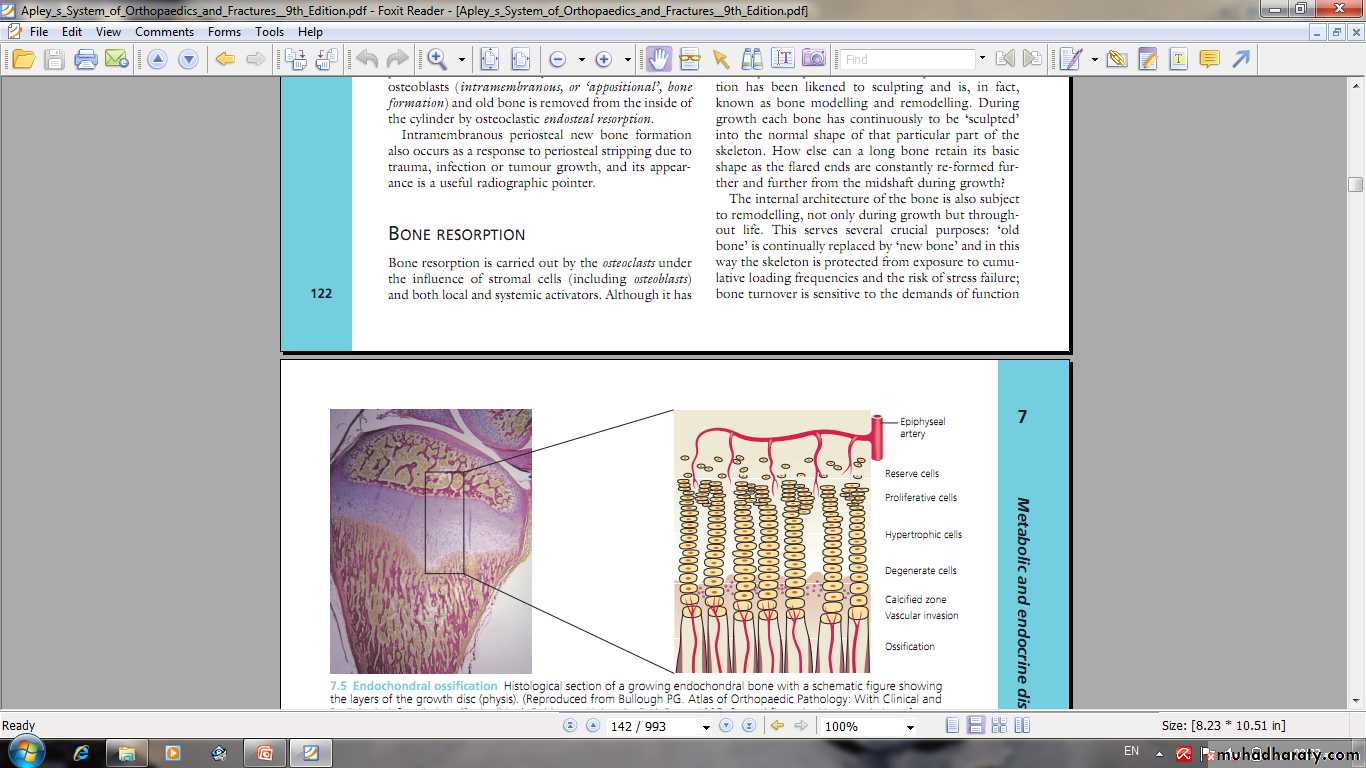
Endochondral ossification
Epiphyseal growth plate
Intramembranous ossification
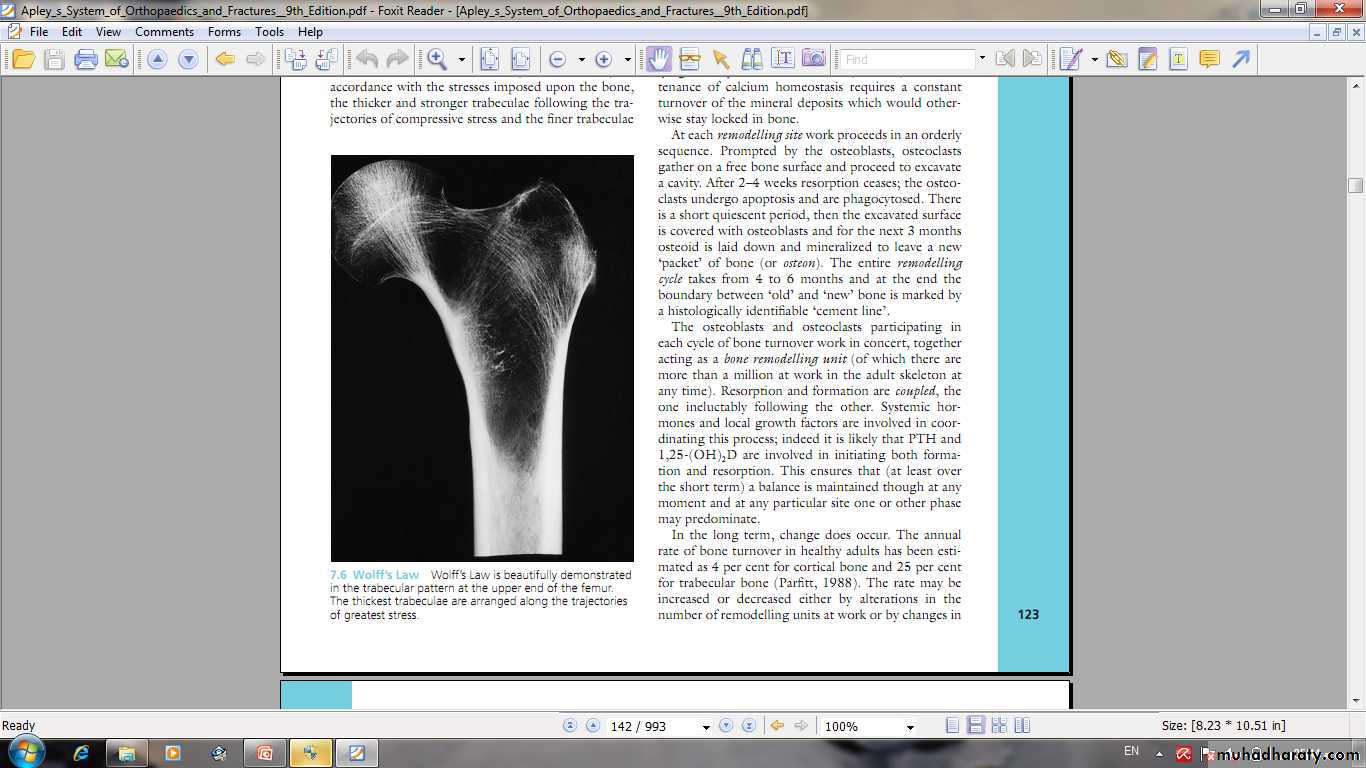
Periosteal new bone formationBone formation and resorption.Bone remodelling
Minerals and Factors affect bone metabolism
1- calcium.2- phosphorus.
3- magnesium and fluoride.
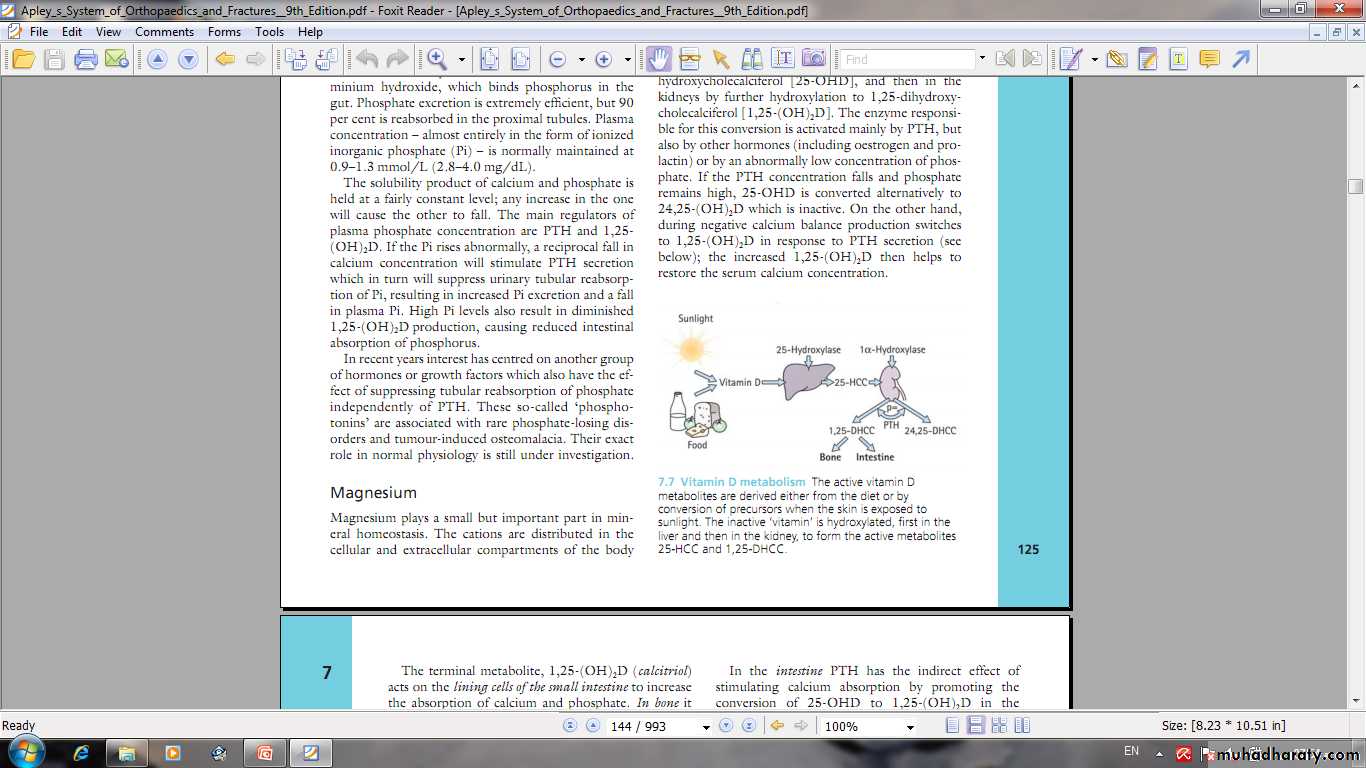
4- Vitamin D .
5- Parathyroid hormone.
6- calcitonin.
7- glucocorticoids, gonadal hormone, thyroxine , growth hormone.
8- mechanical factors.
9- electrical stimulation and other factors.
Factors adversely affecting bone mass
1- Early onset menopause.2- Malnutrition and ill health
3-Lack of Vit D, calcium and phosphate.
4- Chronic illness.
5- High consumption of alcohol.
6- Smoking.
7- Inactivity.
8- Drugs ( corticosteroids, anti-inflammatory drugs, diuretics, anticoagulants, thyroid hormone, antiepileptics ).
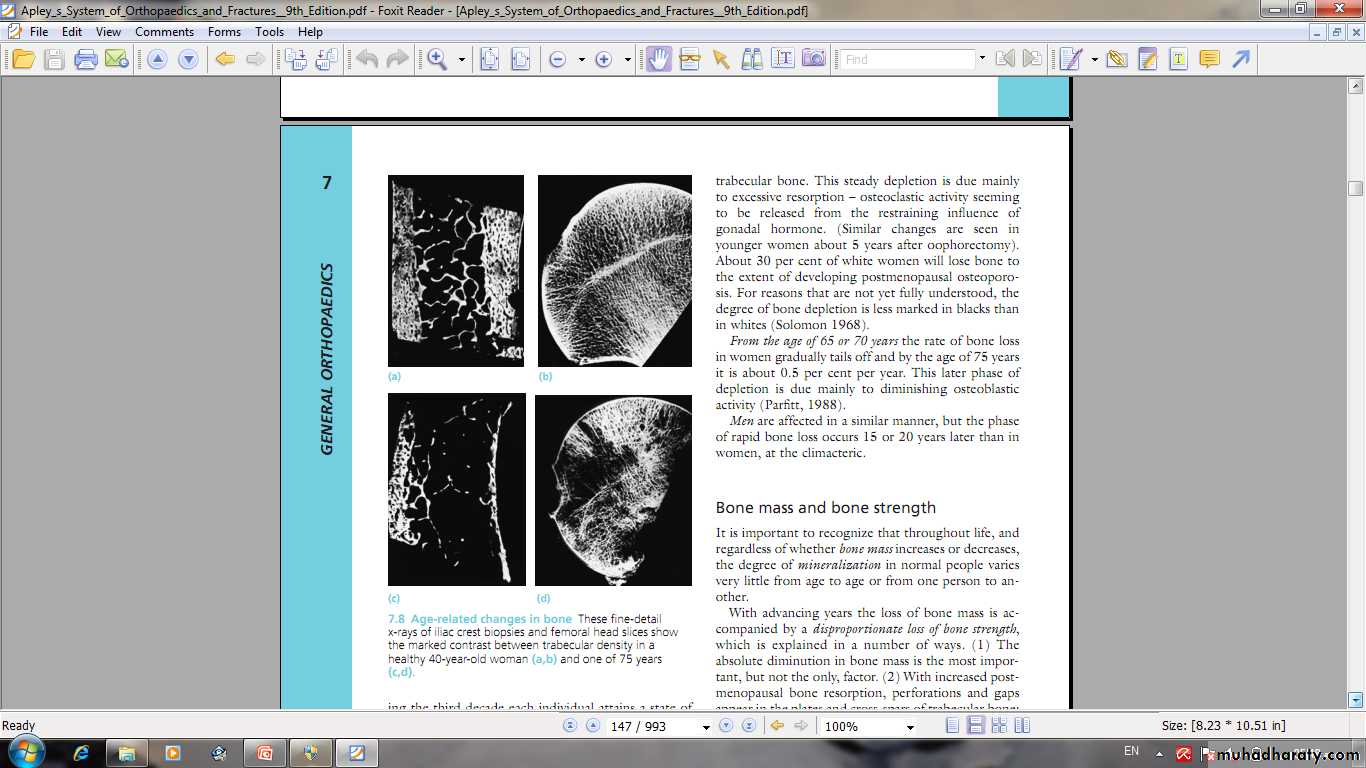
OSTEOPOROSIS Reduction of normally mineralized bone mass per volume.
It is a clinical disorder characterized by an abnormally low bone mass and defects in bone structure, render the bone fragile.
A state in which bone is fully mineralized but its structure is abnormally porous and its strength is less than normal person of that age and sex
OSTEOPOROSIS
It may result from increased bone resorption ordecrease bone formation or both.
Osteopenia: bone which appears to be less dense than normal X-ray.
Any density reduction in DEXA more than 2.5 standard deviation define as osteoporosis.
Between 1-2.5 name osteopenia
Osteoporosis
1- Osteoporosis is one of the most serious global disease andwill increase due to increased aging.
2- Osteoporosis is a problem in both genders.
3- Osteoporosis may primary or secondary.
Primary osteoporosis may be postmenopausal or senile .
4- Osteoporosis is common cause of fractures especially femoral neck fractures , vertebral fractures and distal radial fractures .
5- Bone mineral density commonly measured by dual-energy X-ray absorptiometry ( DEXA)
Secondary osteoporosis
Malnutrition .Hypercortisonism ( Cushing’s disease).
Gonadal hormone insufficiency.
Hyperthyroidism and hyperparathyroidism.
Multiple myeloma & carcinomatosis.
Drugs ( steroids, heparin, antiepileptic, cytotoxic, ….).
Alcohol and smoking.
Immobilization.
Chronic disease ( renal failure, TB, rhumatic disaeses... )
Other factors
Treatment of osteoporosis
Hormone therapy.Bisphosphonates Bisphosphonates is the first-line drugs for treating postmenopausal women with osteoporosis, Alendronate and risedronate reduce risk of both vertebral and nonvertebral fractures.
Parathyroid hormone: Teriparatide (PTH 1-34) is reserved for treating women at high risk for fracture, including those with very low bone mineral density (BMD) with a previous vertebral fracture. PTH improves BMD and reduces the risk of vertebral and non-vertebral fractures. Dosage requirements of daily subcutaneous injections may limit use.
Fluoride, calcium, and vitamin D, calcinotin.
Fracture treatment
Osteoporosis
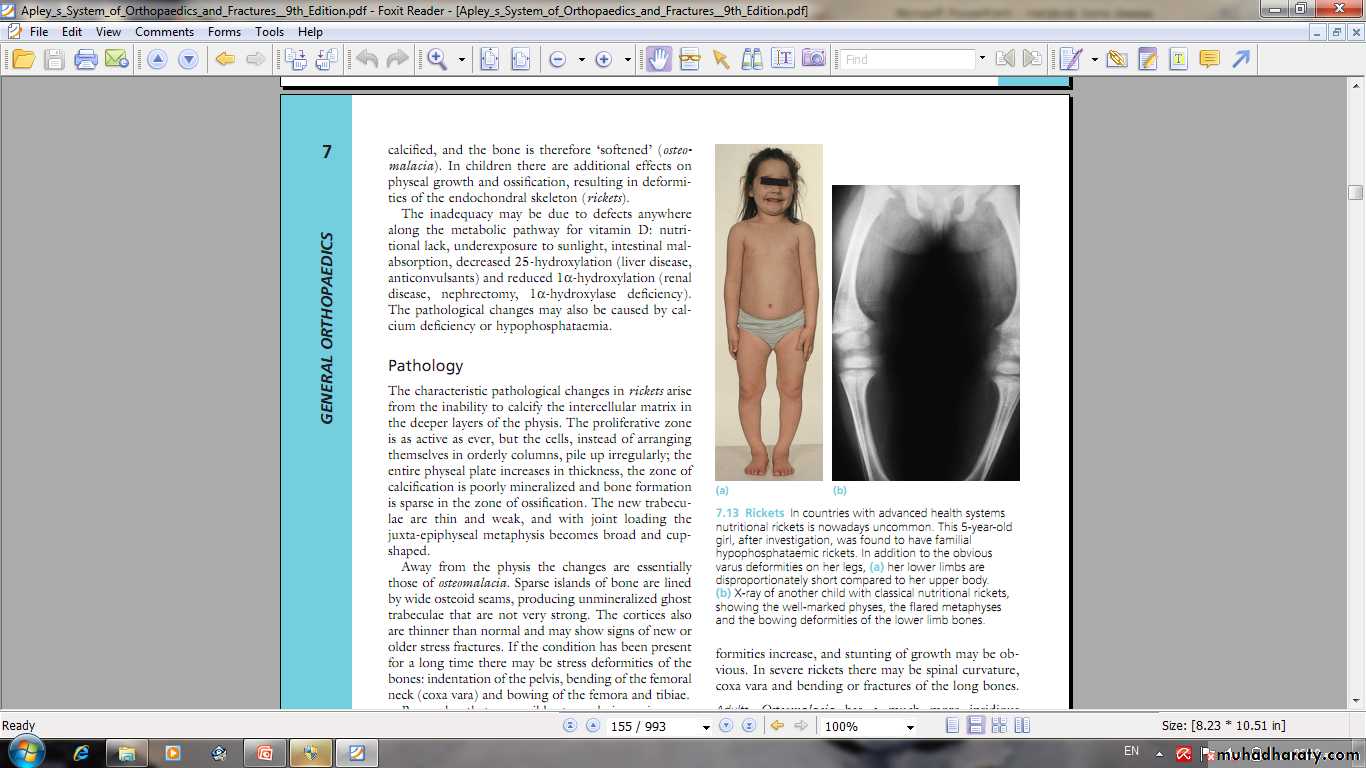
Osteomalacia and ricketsinadequate mineralization of bone
Bone tissue throughout the skeleton is abnormally calcified and therefore soften ( Osteomalacia).Rickets and Osteomalacia is same disease.
Osteoporosis and Osteomalaciacommon in aging women, prone to pathological fractures, and decreased bone density.
Osteomalacia
-------------------------------
Unwell
Generalized chronic ache
Muscles weak.
Losser’s zone
decreased serum phosphate
elevated serum alka. Phosphatase.
Ca × p< 2.4 mmol/ L
Osteoporosis
--------------
Well
Pain after fractures
Muscles normal.
No Losser's zone
Normal serum phosphate
Normal serum alka.
Phosphatase
Ca × p>> 2.4 mmol/ L
Osteomalacia treatment
Treatment of the cause.Treatment of pathological fractures.
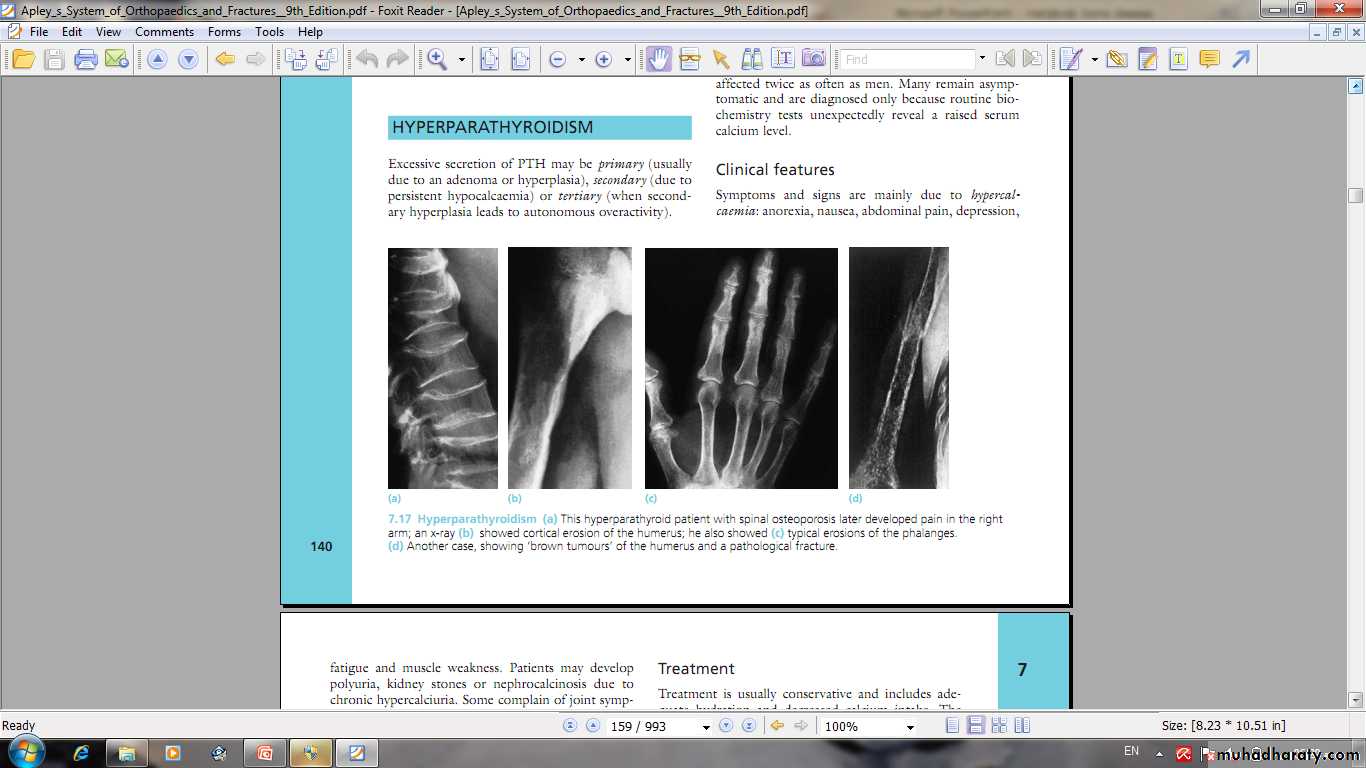
hyperparathyroidism
Excessive secretion of PTH.May be primary , secondary, or tertiary.
PTH- enhance calcium conservation resulting in hypercalcaemia and hypercalciuria and
Hyperphosphouria.Bone resorption manifest by ostitis fibrosa cystica and subperiosteal resorption.
hyperparathyroidism
Clinical features1- features of
hypercalcaemia.
2-polyuria and renal disorders
3- bone pain and pathological fractures.
Treatment
1- treatment of hypercalcaemia.
2- surgery.
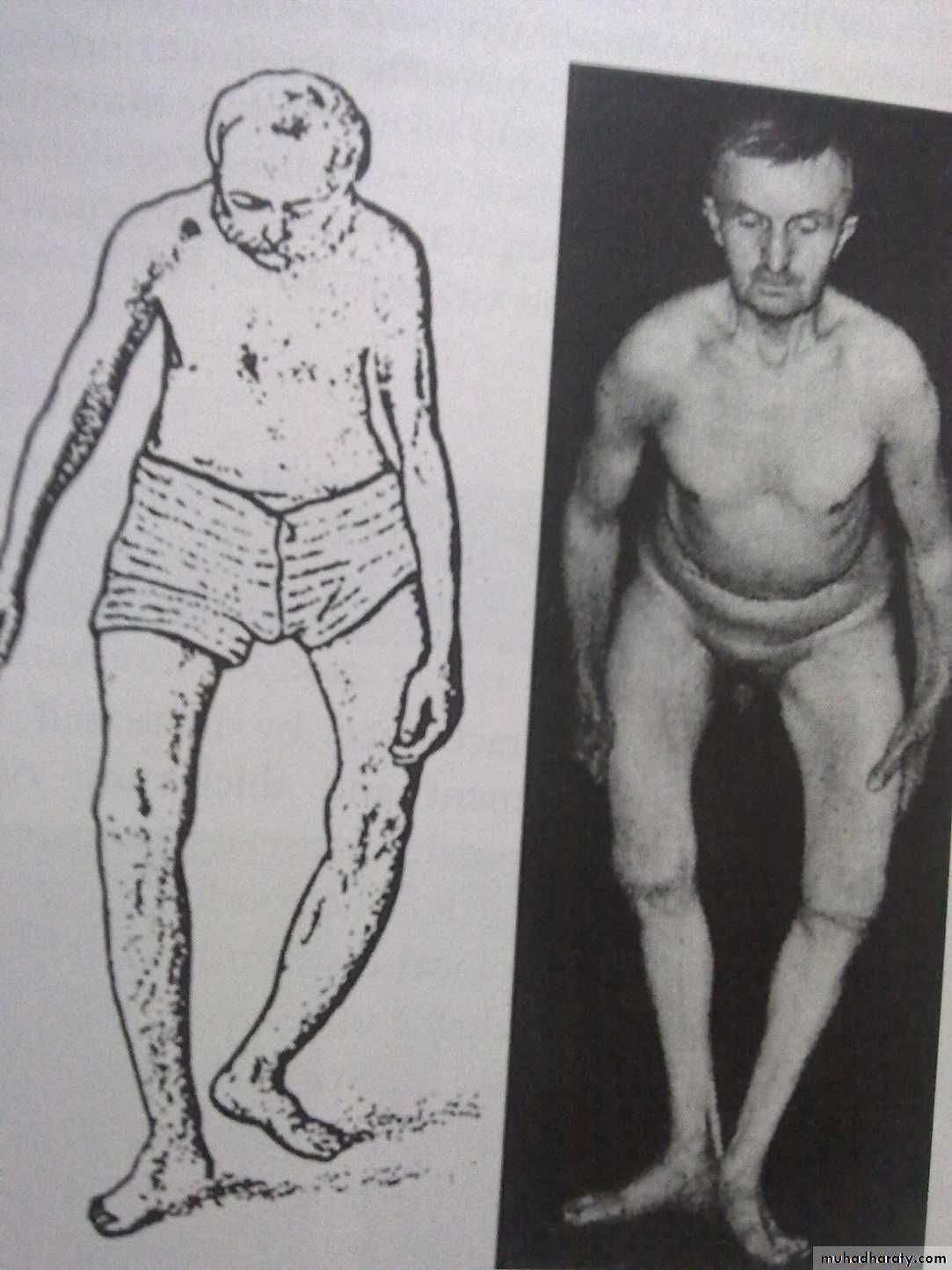
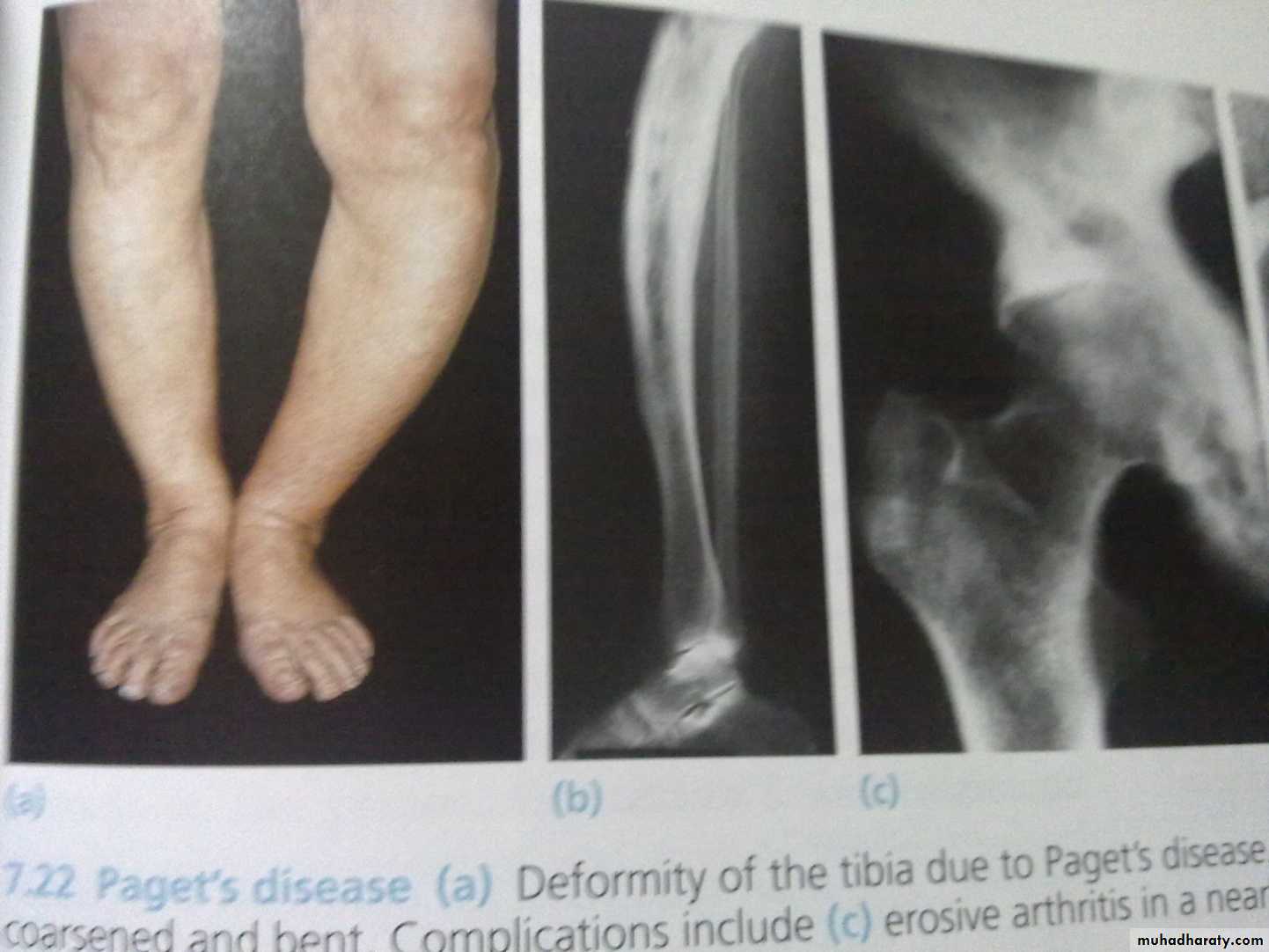
Paget’s disease
This disease characterized by increased bone turnover and enlargement and thickening of bone, but internal architecture is abnormal and bone is usually brittle.Paget’s disease
Complications1- fractures.
2- osteoarthritis
3- nerve compression and spinal stenosis.
4- bone sarcoma.
5- high cardiac output failure.
6- hypercalcaemia in immobilization.
Treatment
1- calcitonin.2- Bisphosphonate.
3- surgery