Fifth stage
Pediatric
Lec-3
.د
خليل
19/10/2016
The cardiovascular system
Cyanotic Congenital Heart Disease
Lesions Associated with Decreased Pulmonary Blood Flow
Tetralogy of Fallot
Epidemiology and pathology
Tetralogy of Fallot is the most common
cyanotic congenital heart defect,
representing about 10% of all congenital
heart defects .
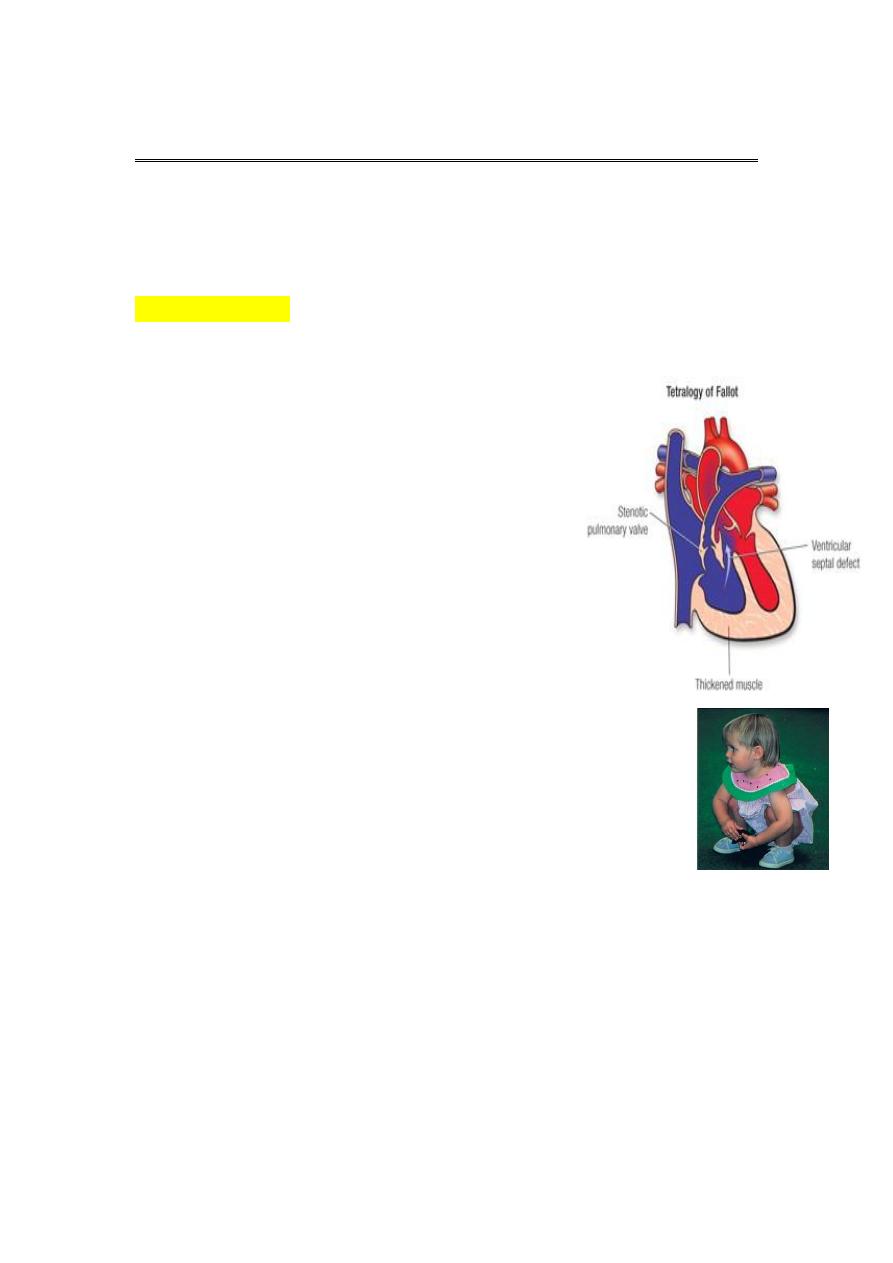
Anatomically, there are four structural
defects: VSD, pulmonary stenosis,
overriding aorta and right ventricular
hypertrophy.
The VSD is large and the pulmonary
stenosis is most commonly
subvalvularor (infundibular).
Clinical features
A- Symptoms
Most patients are symptomatic with cyanosis at birth or
shortly thereafter. Dyspnea on exertion, squatting, or
hypoxic spells develop later, even in mildly cyanotic infants .
Occasional infants with acyanotic TOF may be asymptomatic or
may show signs of CHF from a large left-to-right ventricular shunt.
Immediately after birth, severe cyanosis is seen in patients with
TOF and pulmonary atresia.
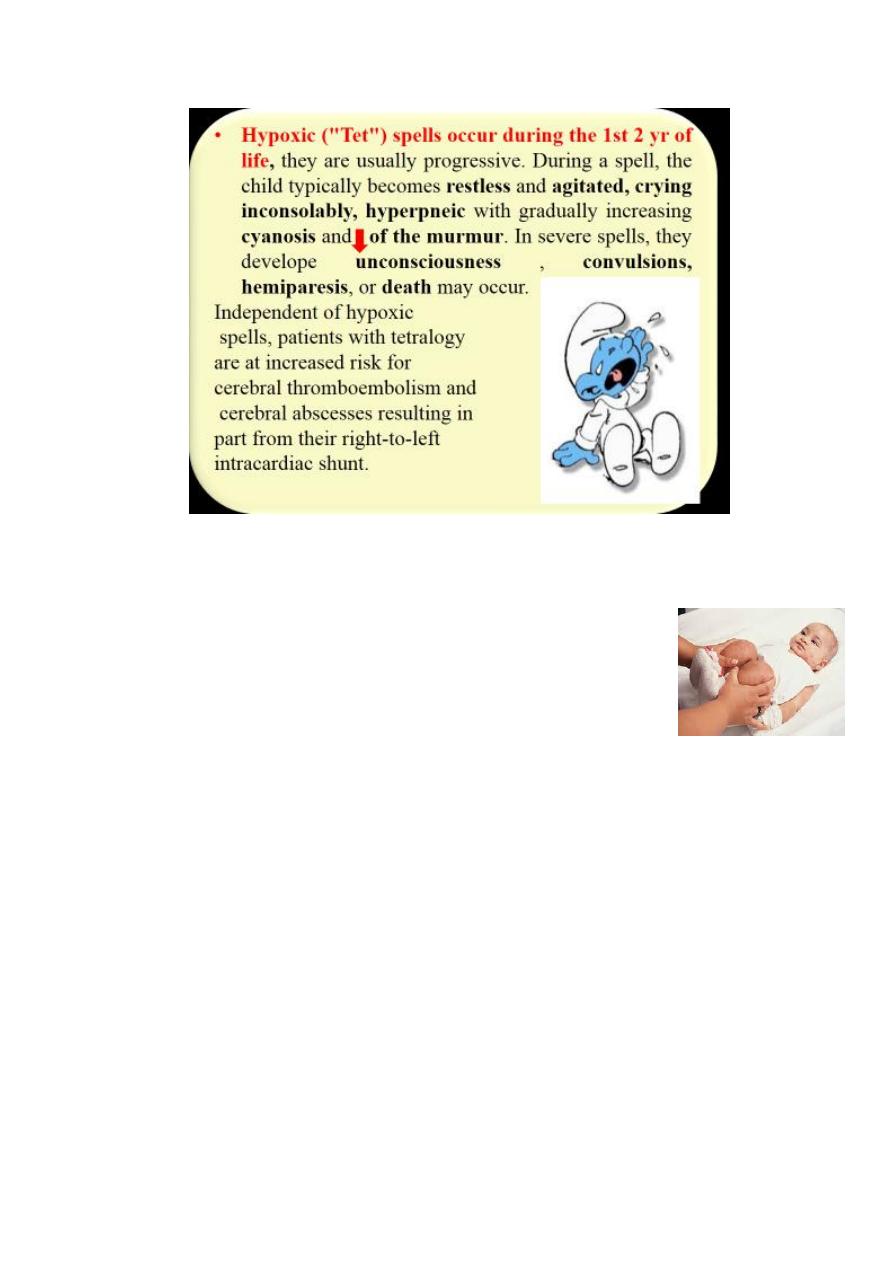
Treatment of spells
Placement of the infant on the abdomen in the knee-
chest position while making certain that the infant's
clothing is not constrictive. Premature attempts to
obtain blood samples may cause further agitation and –
ve effect.
O2 adminstration
S.c morphine not > 0.2mg/kg.
B-adrenergic blockers e.g propranolol (0.1-0.2) mg /kg i.v and
slowly.

Physical examination
Growth and developmental delay in patients with severe
untreated tetralogy of Fallot, particularly when oxygen saturation
is chronically <70%. Puberty may also be delayed in patients who
do not undergo Surgery.
Varying degrees of cyanosis, tachypnea, and clubbing (in older
infants and children) are present.
The pulse is usually normal, as is venous and arterial pressure.
The left anterior hemithoraxmay bulge anteriorly because of RVH.
In about half the cases, a systolic thrill is felt along theleft sternal
border .
The murmur is usually loud, systolic, most intense at the left
sternal border. It is due to PS and generally ejection in quality , but
it may sound more holosystolic toward the lower sternal border.
Natrural history and complications
Worsening of cyanosis with time.
Physicians need to watch for the development of relative iron-deficiency
state (i.e., hypochromia).
Polycythemia develops secondary to cyanosis.
Growth retardation may be present if cyanosis is severe.
Hypoxic spells may develop in infants.
Brain abscess and cerebrovascular accident rarely occur
SBE is occasionally a complication.
8.Coagulopathy is a late complication of a long-standing cyanosis.
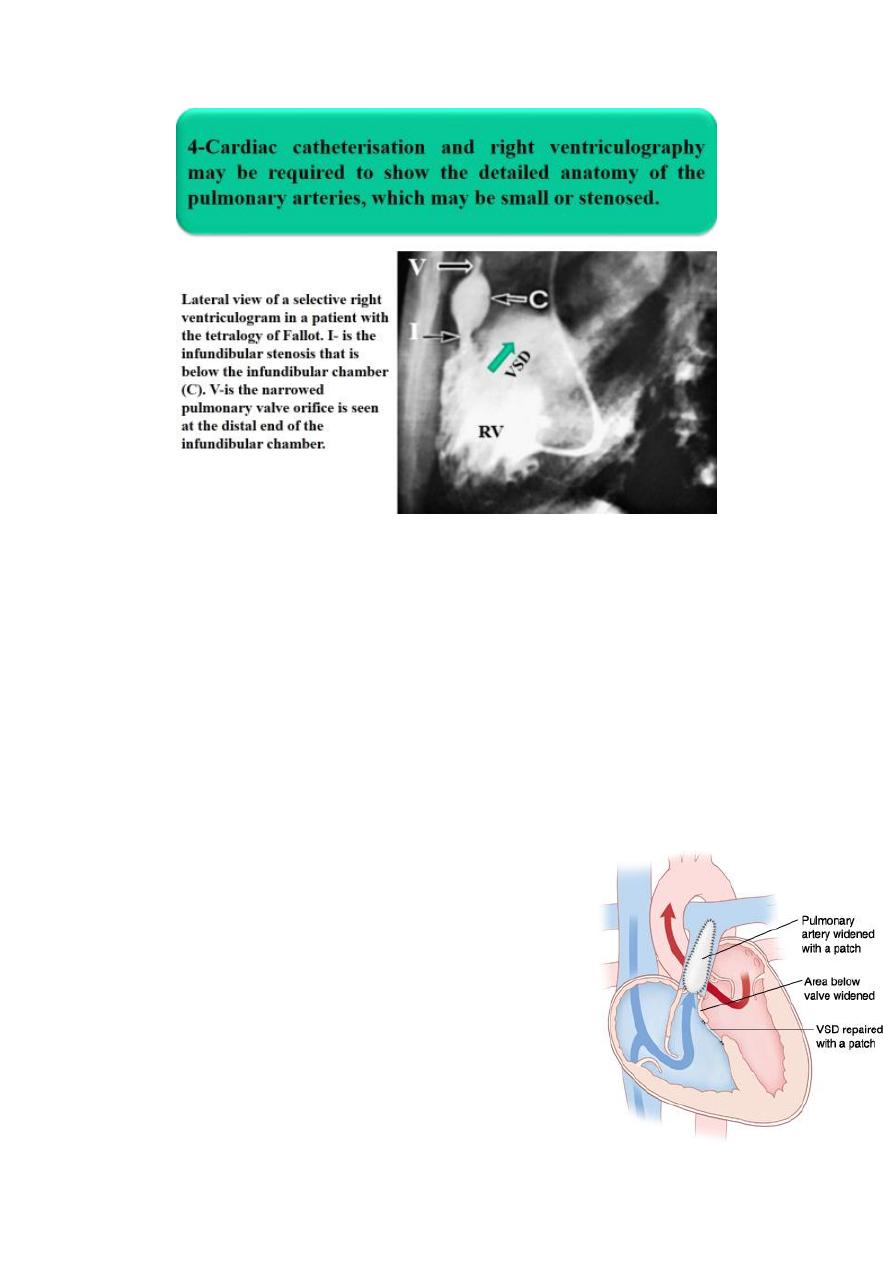
Management
Initial management is medical, with
corrective surgery at around 6 months of
age. It involves closing the VSD and
relieving right ventricular outflow tract
obstruction with an artificial patch, which
sometimes extends across the pulmonary
valve.

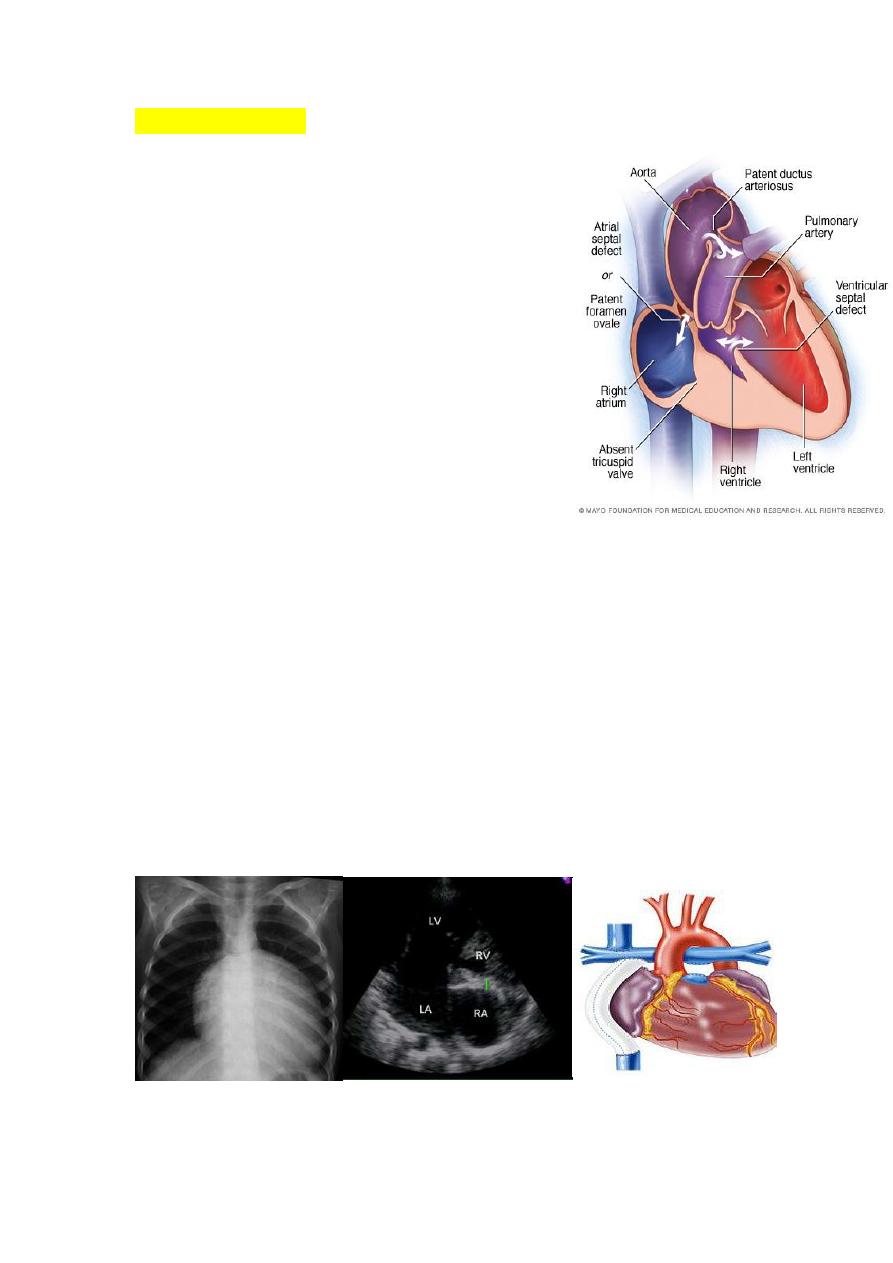
TRICUSPID ATRESIA
Etiology, Epidemiology and pathophysiology
Tricuspid atresia accounts for approximately 2% of all
congenitalheart defects . The absence of the
tricuspidvalve results in a hypoplastic right ventricle. All
systemic venous return must cross the atrial septum Into
the left atrium. A PDA or VSD is
necessary for pulmonary blood flow andsurvival.
Clinical Manifestations
1. Severe cyanosis
2. If a VSD is present, there may be a murmur. A
diastolic murmur across the mitral valve may be
audible.
*Frequently there is no significant murmur.
Diagnosis
ECG shows LVH and Lt axis deviation.
CXR shows cardiomegaly with decreased pulmonary blood flow
Echo is diagnostic and shows the abnormalities.
Treatment
If there is no VSD PGE1 is infused to maintain ductal patency and
pulmonary flow.
Surgical correction involve (Blalock-Taussig procedure) then
Fontan opertation.
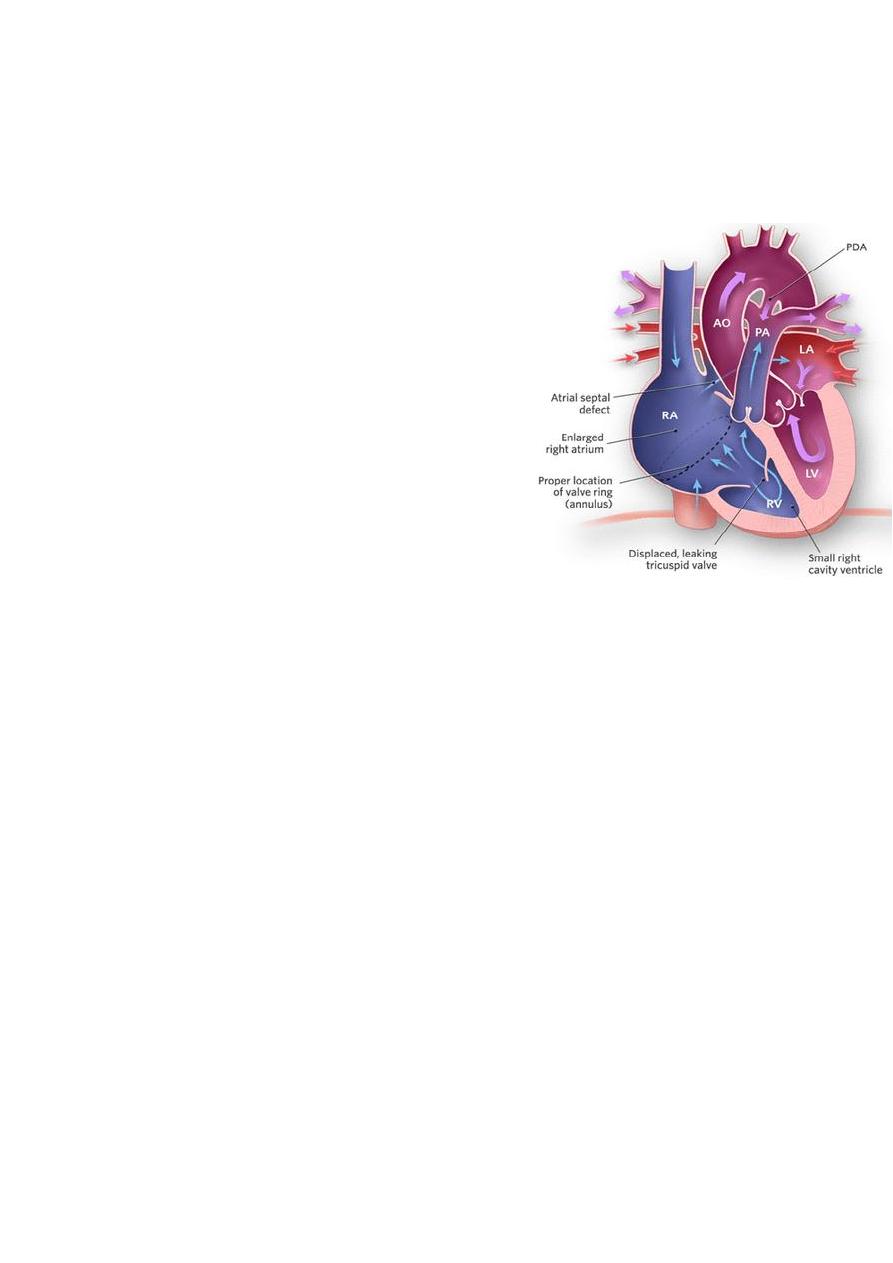
Ebstein Anomaly
Ebstein anomaly consists of downward displacement of an abnormal
tricuspid valve into the right ventricle.
Pathophysiology
The right ventricle is divided into 2
parts by the abnormal tricuspid valve:
the 1st, a thin-walled “atrialized”
portion, is continuous with the cavity
of the right atrium; the 2nd, often
smaller portion consists of normal
ventricular myocardium.
RV output is decreased due to a
combination of the poorly
functioning small right ventricle and
tricuspid valve regurgitation,
Clinical Manifestations
Symptoms
• Severity is variable depending on the severity of pathology.
• Mild cases present at teenage or adulthood with fatigue and
palpitation as a result of cardiac dysrhythmias.
• There may be atrial right-to-left shunt through an ASD
causing cyanosis and polycythemia.
Physical signs
High JVP.
A holosystolic murmur caused by tricuspid regurgitation is
audible over most of the anterior left side of the chest.
*Neonates with severe form present with severe cyanosis, heart failure
and pulmonary hypoplasia and may die.
Diagnosis
ECG shows RBB, large tall p wave, prolonged PR interval and
SVT due to Wolf-Parkinson white syndrome.
CXR shows cardiomegaly
Echo is diagnostic and shows the abnormalities.
Treatment
In non severe cases by surgical repair of TV
In severe cases by single ventricle repair ( Fontan opertation)
Lesions Associated with Increased Pulmonary Blood Flow
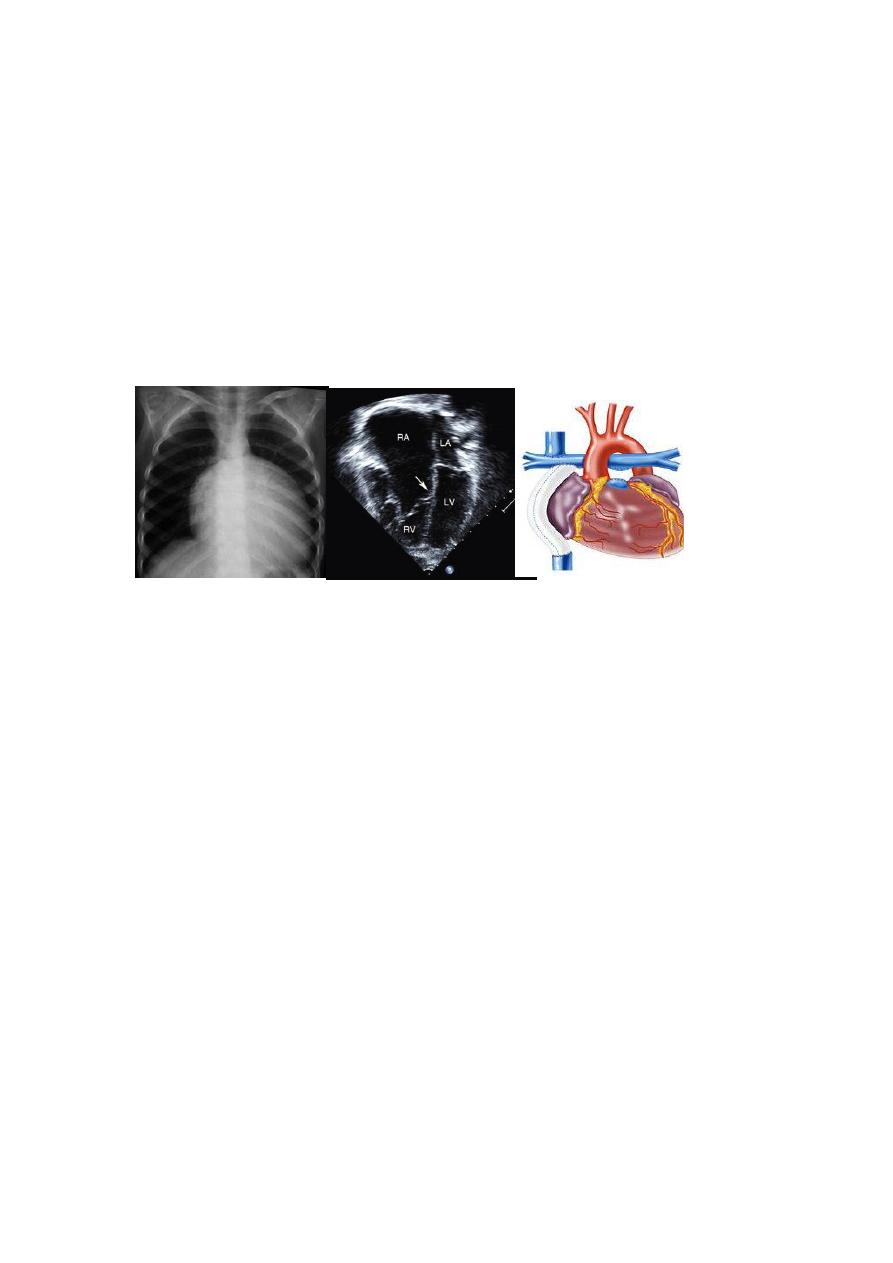
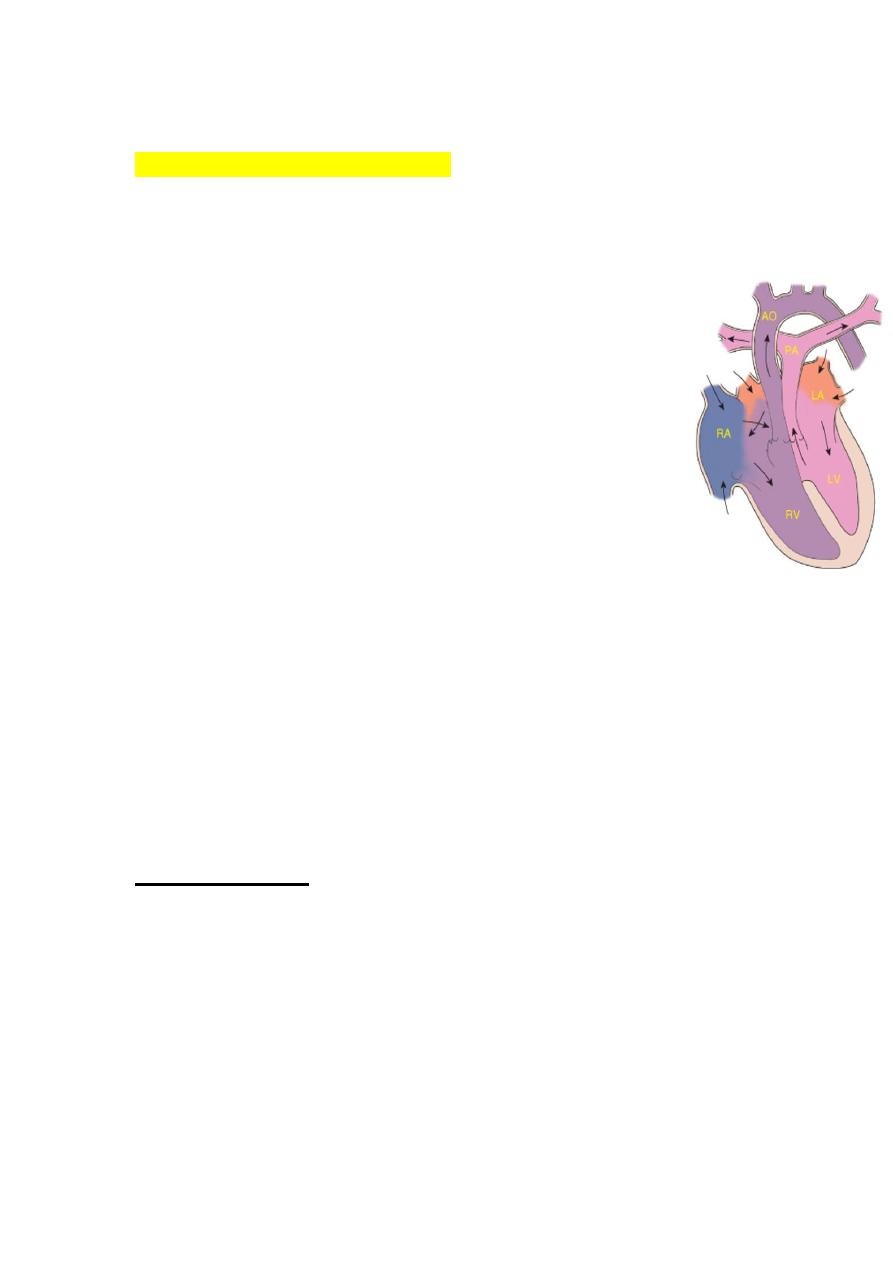
D-Transposition of the Great Arteries
Etiology and Epidemiology
T.G.A represents about 5% of congenital heart defects, and it is
the most common cyanotic lesion to present in the Newborn
period . T.G.A is ventriculoarterial discordance secondary to
abnormalities of septation of the truncus arteriosus, the aorta
arises from the right ventricle, anterior and to the right of the
pulmonary artery, which arises from the left
ventricle. This transposition results in desaturated blood
returning to the right heart and being pumped back out to the
body, while well-oxygenated blood returning from the lungs
enters the left heart and is pumped back to the lungs. Without
mixing of the two circulations, death occurs quickly. Mixing can
occur at the atrial (patent foramen ovale/ASD), ventricular (VSD), or
great vessel (PDA) level
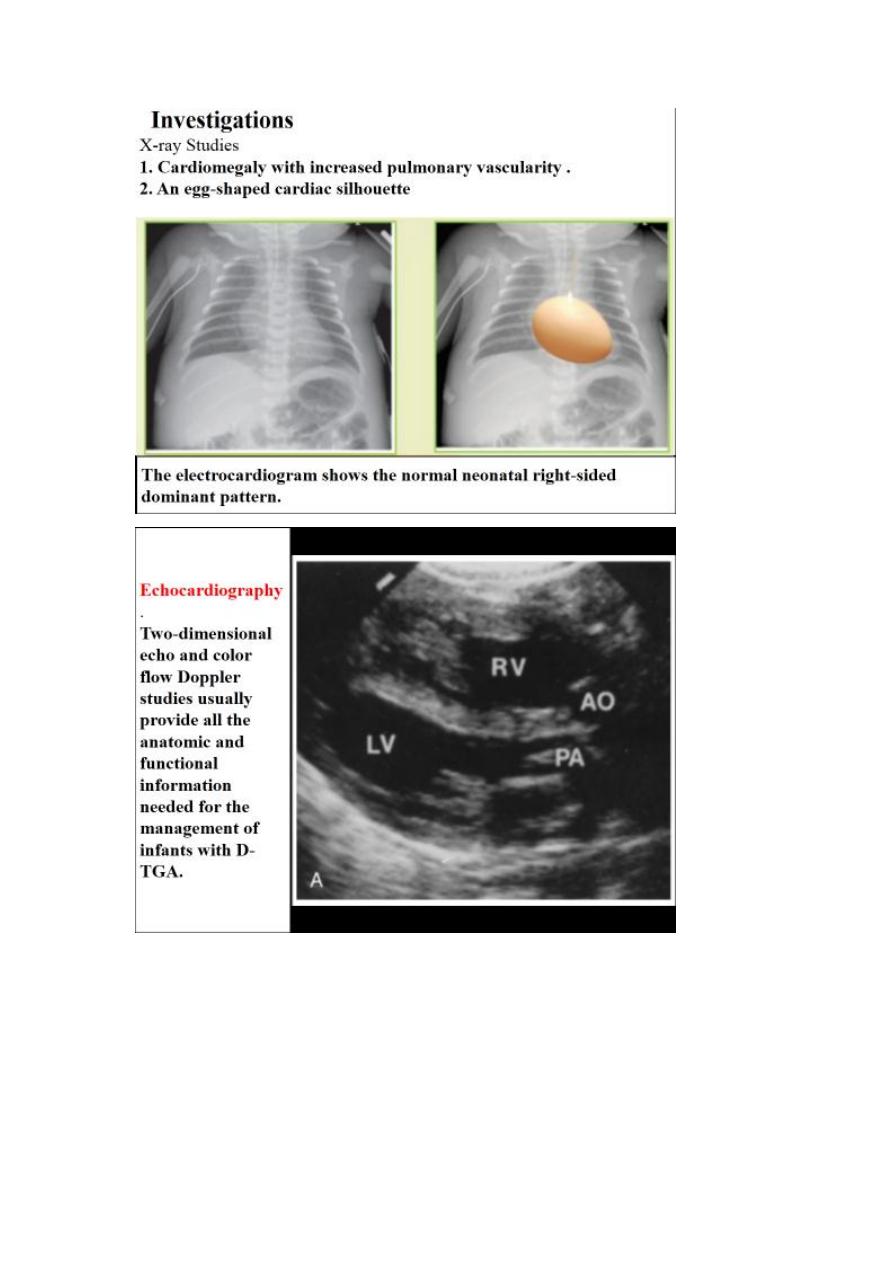
CLINICAL MANIFESTATIONS
History of cyanosis from birth is always present.
Symptoms of congestive heart failure (CHF) with
dyspnea and feeding difficulties may develop during
the newborn period
On examination:-
Moderate to severe cyanosis and tachypnea.
No VSD no murmur, VSD holosystolic murmur, and there may be
murmur of RVOT or LVOT obstruction.
There may be features of heart failure.
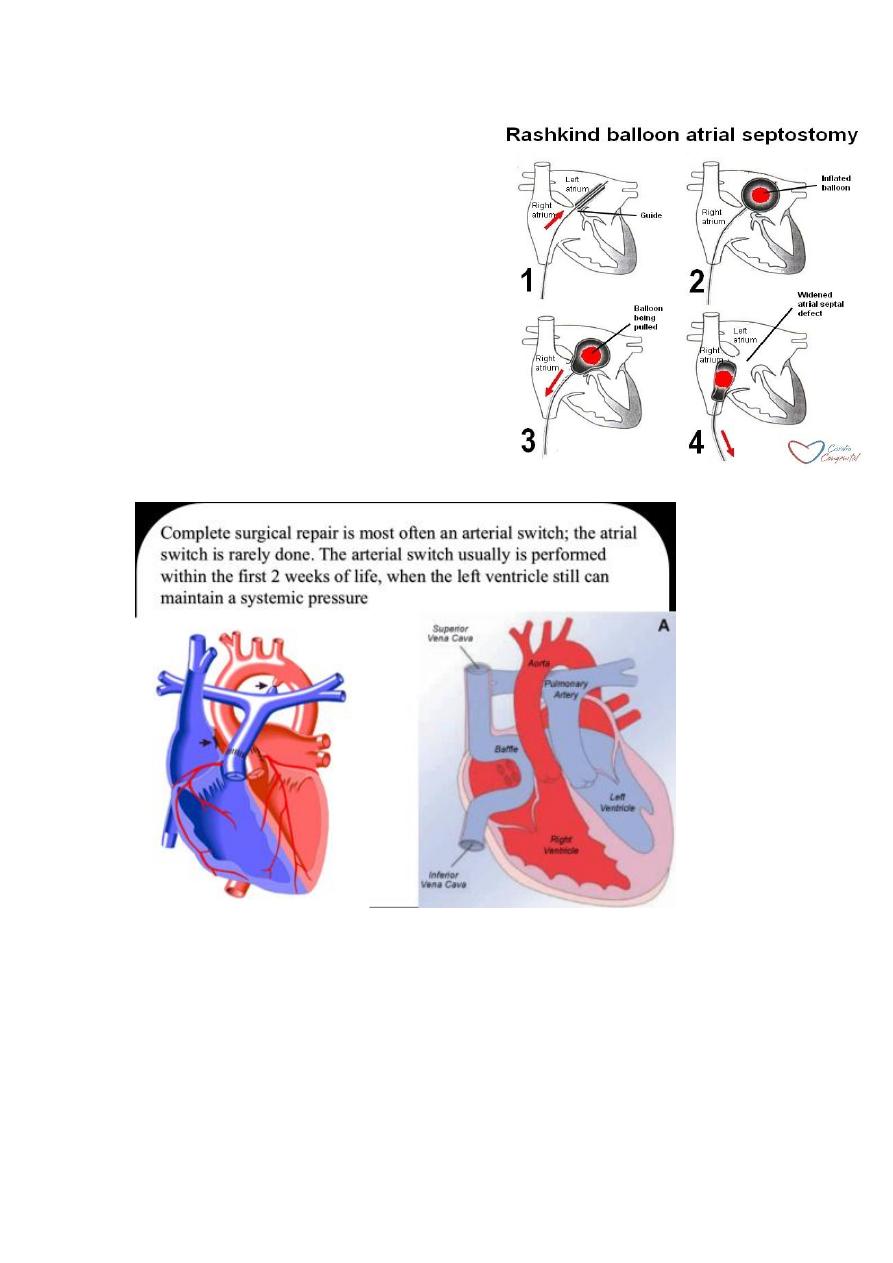
Treatment
Initial medical management
includes prostaglandin E
1
to
maintain ductal patency.
If the infant remains significantly
hypoxic on prostaglandintherapy,
a balloon atrial septostomy is
performed to improve mixing
between the two circulations.