Papulosequamous disorders Psoriasis
Fifth class / dermatology3rd / November/ 2016
Lec. 2
DR. MANAR GHANEM
M.B.CH.B. F.I.C.M.S.Common Papulosequamous Disease
PsoriasisLichen planus
Pityriasis rosea
Tinea corporis
Pityriasis versicolor
Discoid eczema
Seborrhic dermatitis
Secondery syphilis
Drug eruptions
Introduction
Psoriasis occurs in 1% to 3% of the population.
Male and female equally
The disease is transmitted genetically .
the disease is lifelong and characterized by chronic, recurrent
exacerbations and remissions that are emotionally and physically debilitating.
There may be many millions of people with the potential to develop psoriasis but certain environmental factor(s) is (are)
needed to precipitate the disease (stress, drugs, infection).
Environmental factors also may modify the course and severity of disease.
Extent and severity of the disease vary widely from patient to another as well as itching .
Pathogenesis
Psoriasis is a genetic, immune-mediated , affect skin and/or joint .Inflammatory disease in which intra lesional inflammation stimulates basal keratinocytes to hyper proliferate.
Environmental factors play an important role in the pathogenesis of psoriasis, including drugs, skin trauma (Koebner phenomenon), infection, and stress.
Drugs that precipitate or exacerbate psoriasis
Lithium
Antimalarial agents
Beta blocking agents
Systemic steroids
Interferon
Comorbidities associated with psoriasis
Patients with psoriasis are at a higher risk for the following comorbidities than is the general population:• Crohn’s dis. and UC (3.8 to 7.5 times).
• Cardiovascular disease
• Metabolic syndrome???
• Lymphoma
• Depression/suicide
• Psychological/sexual dysfunction
• Smoking
• Alcohol
• Obesity
• Quality of life
Clinical Presentations
A. Variations in the morphology of psoriasis:Chronic plaque psoriasis : psoriasis vulgaris 90% most common
Guttate psoriasis : good prognosis
Pustular psoriasis
Erythrodermic psoriasis
Light-sensitive psoriasis
HIV-induced psoriasis
Keratoderma blennorrhagicum (Reiter syndrome)
B. Variations in the location of psoriasis:
Psoriasis vulgaris ( extremities and trunk )
Scalp psoriasis
Psoriasis of the palms and soles
Pustular psoriasis of the palms and soles
Psoriasis inversus ( flexural psoriasis )
Psoriasis of the penis and Reiter syndrome
Nail psoriasis
Psoriatic arthritis
Chronic Plaque Psoriasis
Well-defined plaques.The plaques are irregular, round to oval.
Predilection for extensor surfaces such as the elbows and knees but any site can be affected.
White - Silvery scale.
Tend to be symmetrically distributed.
Plaques enlarge and then tend to remain stable for months or years( chronic )
A temporary brown, white, or red macule remains when the plaque subsides.
Auspitz sign!!!
Guttate psoriasis (Acute Eruptive Psoriasis)
30% their first episode before age 20An episode of guttate psoriasis might be the first indication of the patient’s propensity for the disease.
Streptococcal pharyngitis or a viral upper respiratory tract infection may precede the eruption by 1 or 2 weeks.
Scaling papules suddenly appear on the trunk and extremities, excluding palms and soles.
The scalp and face may also be involved
Number varies, and their size may be that of a pinpoint up to 1 cm.
It may resolve spontaneously and it responds more readily to treatment than does chronic plaque psoriasis.
Dx? treat the infection
Psoriasis inversus (flexural psoriasis )
The gluteal fold, axillae, groin, submammary folds, retroauricular fold, and the glans of the uncircumcised penis may be affected.The deep red, smooth, glistening plaques may extend to and stop at the junction of the skin folds, as with intertrigo or Candida infections as ddx.
The surface is moist and contains macerated white debris.
Cracke and fissures are common at the base of the crease.
Infection, friction, and heat may induce flexural psoriasis, a Koebner phenomenon.Infants and young children may develop flexural psoriasis of the groin that extends onto the diaper area
Erythrodermic psoriasis
Is a severe, unstable, highly labile disease.It may appear as the initial manifestation of psoriasis but usually occurs in patients with previous chronic disease.
More than 90% of the body involved .
Precipitating factors include the
Administration of systemic corticosteroids
The excessive use of topical steroids
Use of tar and anthralin on acutely inflamed plaques
Abrupt discontinuation of systemic therapy.
Phototherapy complications
Severe emotional stress
Infection.
Treatment includes
bed restinitial avoidance of all UV light
wet compresses
liberal use of emollients
increased protein and fluid intake
antihistamines for pruritus
avoidance of potent topical steroid
in severe cases, hospitalization.
Methotrexate, cyclosporine, or acitretin is used if rapid control is not obtained with topical therapy.
Pustular psoriasis of the palms and soles
Deep pustules first appear on the middle portion of the palms and insteps of the soles; they may remain localized or spread.The pustules do not rupture but turn dark brown and scaly as they reach the surface.
The surrounding skin becomes pink, smooth, and tender.
A thick crust may later cover the affected area.
The course is chronic, lasting for years while the patient endures periods of partial remission followed by exacerbations so painful that mobility is affected.
• There is a considerably higher prevalence of smoking in these patients.
• Rx: Acitretin, methotrexate, PUVA, narrow-band UVB, and intermittent courses of topical steroids under plastic occlusions.Keratoderma blenorrhagicum
Scalp Psoriasis
Palmoplanter psoriasis
Psoriasis of the nails
Onycholysis ?Subungual hyperkeratosis?
Pitting?
Oil spot sign?
Nail dystrophy?
Distal Onycholysis Subangual Hyperkeratosis
Oil Spot Sign Nail Pitting
Psoriatic Arthritis
Psoriatic arthritis (PsA) is a chronic inflammatory arthropathy of the peripheral joints, spine, and entheses.It is associated with psoriasis in which rheumatoid factor and anti-cyclic citrullinated peptide (anti-CCP) measurements are usually negative.
It may precede (15%), accompany, or, more often, follow the skin manifestations.
Unlike in rheumatoid arthritis, the distal interphalangeal joints are regularly involved.
The presence of inflammatory arthritis in patients with psoriasis varies between 5% and 42%.
The prevalence of psoriatic arthritis is higher among patients with more severe cutaneous disease.
Nail involvement occurs in more than 80% of patients with psoriatic arthritis, compared with 30% of patients with uncomplicated psoriasis.
Patients with psoriatic arthritis who become pregnant improve or even remit in 80% of cases.
Despite active treatment and a reduction in joint inflammation and the rate of damage, psoriatic arthritis may be a progressively deforming arthritis.
Moll and Wright 1973 classification of psoriatic arthritis
• Oligoarticular assymmetric arthritis: small joints of fingers and toes.• Polyarticular symmetric arthritis (RA-like): small joints of hands and feet, wrists, ankles, knees and elbows.
• Distal interphalangeal joint predominant: Mild, chronic, not disabling, and associated with nail disease. Involves hands and feet. This is the most characteristic presentation of arthritis with psoriasis.
• Destructive polyarthritis (arthiritis mutilans): small joints of hands and feet (gross deformity and subluxation).
• Ankylosing spodylitis and sacroiliitis: May occur alone or in association with peripheral joint disease (Male +sacroiliitis; HLA-B27+spondylitis).
• To meet the Moll and Wright classification criteria , a patient with psoriasis and inflammatory arthritis who is seronegative for rheumatoid arthritis (RA) must present with one of the above five clinical subtypes.
Skin and joint psoriasis
Treatment of psoriasis
EducationTopical treatment
Photo therapy
Systemic treatment
Topical therapy :
All topicals require length treatment time to give relief that is often temporary.
Compliance is a problem, patients become discouraged with moderately effective and expensive topical treatment that lasts weeks or months.
Limited disease (<20% body surface area) can be managed with topical therapy only.
Determining the degree of inflammation
The most common form of psoriasis is the localized chronic plaque disease involving the skin and scalp.It must be determined whether the plaque is inflamed ?? before instituting therapy.
Red, sore plaques can be irritated by tar, calcipotriol, and anthralin.
Irritation can induce further activity.
Inflammation should be suppressed with topical steroids and/or antibiotics before initiating other
Determining The End of Treatment
Induration disappeared.Residual erythema, hypopigmentation, or brown hyperpigmentation is common when the plaque clears.
Patients frequently mistake the residual color for disease and continue treatment.
If the plaque cannot be felt by drawing the finger over the skin surface, treatment may be stopped.Stress Control
There is a positive correlation between the severity of psoriatic symptoms and psychologic distress.Stress reduction techniques may be appropriate for certain patients.
• Topical steroids
Rapid response.Control inflammation and itching.
Best for intertriginous areas and face.
Convenient, and not messy.
Temporary relief.
Tolerance occurs.
Brief remissions.
Best results occur with pulse dosing (e.g., 2 weeks of medication and 1 week of lubrication only).
Plastic occlusion is very effective but not used in intertriginous areas and not with superpotent steroids.
S.E. ??
• Intralesional steroid
Patients witha few
small
chronic psoriatic plaques of the scalp or body can be effectively treated with a single or few intralesional injection of triamcinolone acetonide.
Remissions are long.
The face and intertriginous areas are avoided here.
• Calcipotriene (Dovonex cream) 0.005%
Is a vitamin D3 analogue
Inhibits epidermal cell proliferation and enhances cell differentiation.
Well tolerated.
Long remissions possible.
Burning, skin irritation, expensive.
Valuable for long-term scalp treatment programs (Dovonex scalp solution).
Not more than 100g per week is used
Newer combination product (Dovobet) is more effective (calcipotriene hydrate plus betamethasone dipropionate).
Hypercalcemia can occur.
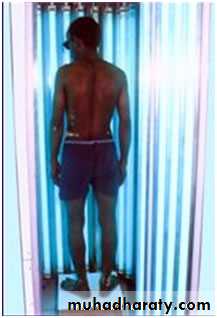
Phototherapy
Narow band Ultraviolet therapy – B( NB- UVB ) :Wave length = (290-320nm)
The most effective topical programs use UVB in combination with lubricating agents, tar, or tazarotene.
Also, the combination of UVB phototherapy with systemic agents can be very effective.
Combining methotrexate (or acitretin) and UVB results in clearing of extensive psoriasis and reduces the cumulative dose (and thus toxicity) of both.
Treatment with narrow-band UVB (311 nm) is superior to treatment with broadband UVB.
UVB is the treatment of choice in guttate psoriasis
• Photochemotherapy
Also called PUVA because of the use of psoralens (P) (photosensitizers), along with exposure to long-wave ultraviolet light (UVA- 1 (340-400)).PUVA can control severe psoriasis with relatively few maintenance sessions, and can be done on an outpatient basis.
PUVA is indicated for the symptomatic control of severe, recalcitrant, and disabling plaque psoriasis that is not responsive to other forms of therapy
Pustular psoriasis of the palms and soles responds best to PUVA-acitretin.
Psoriatic arthropathy (nonspondylitic) may respond to PUVA.
Because of the concerns about long-term toxicity, PUVA is most appropriate for severe psoriasis in patients older than 50 years of age.
Light does not penetrate hair
PUVA Side Effects
Short-term side effects include dark tanning, pruritus, nausea, and severe sunburn.Long term side effects (most of which are dose-dependant):
Skin tumors.
PUVA promotes skin aging, actinic keratoses, and squamous cell
carcinoma (SCC).
Risk of genital tumors in males with exposure to PUVA and UVB.
Approximately 15 years after the first treatment with PUVA, the risk of
malignant melanoma increases, especially among patients who receive
250 treatments or more.
Lentigines. Small black macules occur in PUVA-exposed sites.
Cataracts. The incidence seems to be very low if eye protection is used during the first two days of PUVA treatment (from the time the drug is ingested until the end of the following day).
Phototherapy Device
Treatment of scalp psoriasis
Scale must be removed first to facilitate penetration of medicine, by :Superficial, thin scale can be removed with shampoos that contain tar and salicylic acid (e.g., T/Gel).
Thicker scale is removed by massaging the scalp with 10% liquor carbonis detergens (LCD) in Nivea oil and washing the scalp 6 to 8 hours later with shampoo.
Combing during washing helps dislodge scale.
Nightly applications are continued until the scalp is acceptably clear.
Treating Scalp Psoriatic Lesions:
Steroid gels (e.g., fluocinonide gel, clobetasol gel).Betamethasone foam and clobetasol foam are also effective.
intralesional injections of triamcinolone acetonide.
Dovobet is a topical suspension for the treatment of moderate-to-severe psoriasis of the scalp in adults.
10% LCD in Nivea oil applied to the scalp, covered with a shower cap and washed out each morning, removes scale and suppresses inflammation.
Treatment of psoriatic arthritis
Non-steroidal anti-inflammatory drugsIntra-articular steroid injections
Methotrexate
Biologics
Cyclosporine
PUVA
Systemic treatment of psoriasis
Indications
Moderate-to-severe psoriasis (20% or more involvement of body surface area).
Patient is unresponsive to topical therapy.
A number of systemic drugs are available, some of which have potentially serious side effects.
Methotrexate is highly effective, relatively safe, and well-tolerated
Photochemotherapy (PUVA) is effective and relatively safe.
Acitretin is used to potentiate the effects of PUVA and as a monotherapy for plaque, pustular, and erythrodermic forms of psoriasis.Cyclosporine is rapidly effective, but long-term use may be associated with loss of kidney function.
Biologic drugs (eg., adalimumab and etanercept) are safe and effective and are rapidly becoming the preferred systemic therapy for psoriasis. Very expensive.