Other Papulosequamous Disease
Pityriasis RoseaLichen Planus
Fifth class / dermatology
3rd / November/ 2016Lec. 3
DR. MANAR GHANEM
M.B.CH.B. F.I.C.M.S.
PITYRIASIS ROSEA
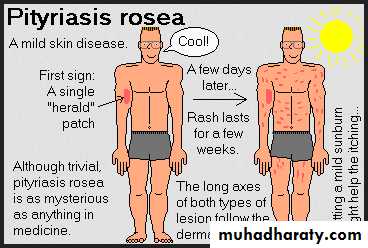
Pityriasis rosea (PR) is a common, benign, usually asymptomatic, self-limiting skin eruption .human herpesvirus 6 (HHV-6) and 7 (HHV-7) may be involved in the etiology
More than 75% of cases occur between 10 and 35 years of age with an age range of 4 months to 78 years.
Recurrence rate is about 2%.
The incidence is higher during winter time.Upper respiratory tract infection occurs before the eruption in about 70% of cases.
CLINICAL MANIFESTATIONS
Typically, the herald patch, a single 2- to 10-cm round-to-oval lesion, abruptly appears in 17% of patients. May occur anywhere, but is most frequently located on the trunk or proximal extremities.
Within a few days to several weeks the disease enters the eruptive phase and reach its maximum in 1 to 2 weeks.
Lesions are typically limited to the trunk (lower trunk) and proximal extremities, but any area could be affected.
Individual lesions are salmon pink in whites and hyperpigmented in blacks.
Typically 1- to 2-cm oval plaques appear, a fine, wrinkled, tissue-like scale remains attached within the border of the plaque, giving the characteristic ring of scale, called collarette scale.The long axis of the oval plaques is oriented along skin lines.
Numerous lesions on the back, oriented along skin lines, give the appearance of “Christmas-tree distribution.”
Remits spontaneously in 6 weeks
50% itching
Differential Diagnosis
Secondary syphilisGuttate psoriasis
Viral exanthems
Tinea corporis
Nummular eczema
Drug eruptions
Management of PR
The disease is benign and self-limited and can resolve spontaneously within 6 weeks
Oral erythromycin 250 mg 4 times daily for 2 weeks.Topical steroids
Oral antihistamines may be used as needed for itching.
Uvb phototherapy five times per week for 2 weeks.
Oral acyclovir (800 mg five times daily for 1 week)??
Lichen Planus
Lichen planus (LP) is an inflammatory cutaneous , mucous membrane , hair and nail diseasEtiology : immunological mechanism mediate its development
The mean age of onset is 40 years
it is rare in children younger than 5 years.
The main eruption clears within 1 year in about 70% of patients, but 50% of eruptions recur.
Approximately 10% of patients have a positive family history.
Cutaneous and oral LP may be associated with hepatitis C virus (HCV)-related, chronic, active hepatitis.
Various patterns of lichen planus
Most common siteActinic
Sun-exposed areas
Annular
Trunk, external genitalia
Atrophic
Any area
Erosioulcerative
Soles of feet, mouth
Follicular (lichen planopilaris)
Scalp
Guttate (numerous) small papules
Trunk
Hypertrophic
Lower limbs (especially ankles)
Linear
Zosteriform (leg), scratched area
Nail disease
Fingernails
Papular (localized)
Flexor surface (wrists and forearms)
Vesiculobullous
Lower limbs, mouth
Eruptions from drugs (e.g., gold, chloroquine, methyldopa, penicillamine)
chemical exposure (film processing), bacterial infections (secondary syphilis)
post–bone marrow transplants (graft-versus-host reaction) that have a similar appearance are referred to as lichenoid.Description
The five (ps) rule of lichen planus:Pruritic, plane (flat-topped), polygonal, purple papules.
Close inspection of the surface shows a lacy, reticular pattern of crisscrossed, whitish lines (wickham’s striae) that can be accentuated by a drop of immersion oil.
Symmetrical
Papules aggregate into different patterns, they may also koebnerize.
Itching is variable; 20% of patients with LP do not itch.
Itch does not necessarily correlate with disease severity.Flexural distribution on wrists and forearms, the legs immediately above the ankles and the lumbar region.
Many patients have persistent post inflammatory hyperpigmentation many years after the rash has cleared.
(Wickham’s striae)
Treatment For Cutaneous Lichen Planus
Topical steroidsIntralesional steroids
Systemic steroids
Acitretin
AzathioprineCyclosporine
Antihistamines
Tacrolimus ointment: Ulcerative lichen planus of the sole may respond to topical tacrolimus 0.1% ointment.
Light therapy
PUVA (psoralen + UVA light) and broadband and narrow-band UVB therapy.Therapy for mucous membrane lichen planus
The course of oral and vaginal lichen planus can extend for years.
Consider a biopsy to establish the diagnosis.
Most patients are asymptomatic (non-erosive type) and do not need treatment.
Tacrolimus ointment and pimecrolimus cream.
Corticosteroids (topical, systemic and intralesional)Dapsone
HydroxychloroquineAzathioprine
Mycophenolate mofetil