Pathogenesis of Bacterial Infection
Microbial PathogenicityInitiation the infectious
Mechanism that lead to the development of signs and symptoms of disease
If a microorganism is capable of causing disease, it is called a pathogen.Fortunately, only a minority of the microorganisms in nature are pathogenic.
Whereas some organisms are highly virulent and cause disease in healthy individuals, even with a small inoculum.Others cause disease only in compromised individuals when their defense are weak. The latter are called opportunistic organisms, as they take the opportunity offered by reduced host defenses to cause disease. These opportunists are frequently members of the body’s normal flora.
General aspects of infection
Virulence:- is a quantitative measure of pathogenicity and is related to an organism’s toxigenic potential and invasivenessVirulence can be measured
by the number of organisms required to cause disease and is designated as LD50 or ID50: the
LD50 (50% lethal dose)
is the number of organisms needed to kill half the hosts.
ID50 (50% infectious dose)
is the number needed to cause infection in half the hosts. These values are determined by inoculation of laboratory animals.Communicable diseases
Infections are called ‘communicable diseases’if they are spread from host to host. Many, but not all, infections are communicable; for example, tuberculosis is communicable, as it is spread by airborne droplets produced by coughing,
but staphylococcal food poisoning is not, as the exotoxin produced by the organism and present in the contaminated food affects only those eating that food.
If a disease is highly communicable, it is called a ‘contagious disease’ (e.g. chickenpox).
Depending on the degree of incidence and prevalence of infectious disease in a community, it may be called an endemic, an epidemic or a pandemic infection.
endemic infection is constantly present at a low level in a specific population (e.g. endemic malaria in some African countries
An infection is an epidemic if it occurs much more frequently than usual (e.g. an epidemic of influenza in the winter)
An infection is a pandemic if it has a worldwide
distribution (e.g. human immunodefciency virus (HIV) infection).Natural history of infectious disease
An acute infection generally progresses through four stage
1-The incubation period: time between the acquisition of the organism or the toxin and the commencement of symptoms (this may vary from hours to days to weeks).
2. The prodromal period: non- specific symptoms such as fever, malaise and loss of appetite appear during this
period.
3. The acute specific illness: the characteristic signs and symptoms of the disease are evident during this period.
4. The recovery period: the illness subsides and the patient returns to health during this final phase.
Pathogenesis can be Divided into
1- Pathogenesis of Bacterial disease.2- Pathogenesis of Viral disease.
3- Pathogenesis of fungal disease
Pathogenesis of bacterial disease
the ways and means by which bacteria cause disease. The major steps are1- Transmission:-
Most infections are acquired by transmission from
external sources; i.e. they are exogenous in origin. Others are caused by members of the normal flora behaving as opportunist pathogens; i.e. they are endogenous in origin.
Transmission
Transmission can be by:
• inhalation – the air borne route
• ingestion –fecal contamination of food and water
• inoculation –by sexual contact, contaminated needles, skin contact, blood transfusions or biting insects
There are four important portals (or gates) of entry of
pathogens :-
1. skin
2. respiratory tract
3. gastrointestinal tract
4. genitourinary tract
Adherence to host surfaces
adherence is the first step in infection.Some bacteria and fungi have specialized structures or produce substances that facilitate their attachment to the surface of human cells or prostheses (e.g. dentures, artificial heart valves),
These adherence mechanisms are critical for organisms that attach to mucous membranes;
mutants that lack these mechanisms are often non-pathogenic (e.g. the hair-like pili of Neisseria gonorrhoeae and Escherichia coli mediate their attachment to the urinary tract epithelium;
the extracellular polysaccharides of Streptococcus mutans help it adhere to enamel surfaces)
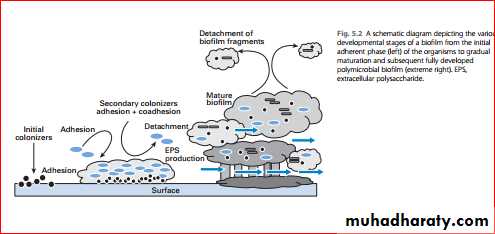
Biofilm formation
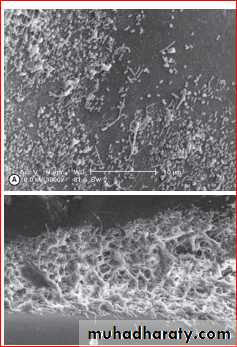
A biofilm:- is defined as an aggregate of interactive bacteria attached to a solid surface (such as a denture prosthesis or an intravenous catheter) or to each other, encased in an extracellular polysaccharide matrix. Up to 65% of human infections are thought to be associated with microbial biofilmsDental plaque on solid enamel surfaces is a classic example of a biofilm.
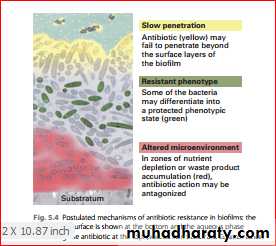
Known infections associated with biofilms are difficult to eradicate as sessile organisms in biofilms exhibit higher resistance to antimicrobials than their free living The reasons for this
• protection offered by the extracellular polysaccharide matrix from the host immune mechanisms
• poor penetration of the antimicrobials into the deeper layers of the biofilm
• degradation of the antimicrobials as they penetrate the biofilm
Some examples of important recalcitrant human infections mediated by biofilms, difficult to manage by antimicrobials alone, include Pseudomonas aeruginosa infections of the respiratory tract in cystic fibrosis patients,
Staphylococcus aureus infections in central venous catheters, chronic candidal infections of HIV-infected individuals and chronic periodontal infections due to dental plaque.
Invasiveness& Virulence factors
Invasiveness of bacteria plays a critical role in pathogenesis; this property is dependent upon secreted bacterial enzymes. A few examples are:• Collagenase and hyaluronidase degrade their respective intercellular substances, allowing easy spread of bacteria through tissues, and are especially important in skin infections caused by Streptococcus pyogenes.
• Coagulase, produced by Staphylococcus aureus, accelerates the formation of a fbrin clot (from fbrinogen). It helps protect the organisms from phagocytosis by walling off the infected area and by coating the organisms with a fibrin layer.
• Immunoglobulin A (IgA) protease degrades protective IgA on mucosal surfaces, allowing organisms such as N. gonorrhoeae, Haemophilus influenzae and Streptococcus pneumoniae to adhere to mucous membranes.
• Leukocidins can destroy both neutrophilic leukocytes and macrophages.
Bacterial infectionmay lead to two categories of inflammation:
1-pyogenic (pus-producing)
2- granulomatous (granuloma-forming).
1- Pyogenic inflammation (pus-producing)
The neutrophils are the predominant cells in this type ofinflammation. Streptococcus pyogenes, Staphylococcus aureus and Streptococcus pneumoniae are the common pyogenic bacteria.
categories of inflammation of Bacterial infection
• 2- Granulomatous inflammation(granuloma-forming)• Macrophages and T cells predominate in this type of inflammation. The most notable organism in this category is Mycobacterium tuberculosis.
• Here, the bacterial antigens stimulate the cell-mediated immune system, resulting in sensitized T-lymphocyte and macrophage activity.
Toxigenicity
Toxins are of two categories: endotoxins and exotoxins.
Endotoxins
Endotoxins are the cell wall lipopolysaccharides of Gram negative bacteria (both cocci and bacilli) and are not actively released from the cell. (Note: thus, by defnition, Gram positive organisms do not possess endotoxins.)
Endotoxins cause fever, shock and other generalized symptoms.
These are mainly due to the production of host factors such as interleukin-1 (IL-1) and tumor necrosis factor (TNF) from macrophages.
• Fever is due to the release of endogenous pyrogens (IL-1) by macrophages; these act on the hypothalamic temperature regulatory center and reset the ‘thermostat’ at a higher temperature.
2. Hypotension, shock and reduced perfusion of major organs due to vasodilatation, are brought about bybradykinin release, increased vascular permeability anddecreased peripheral resistance.
3. Activation of the alternative pathway of the complement cascade results in inflammation and tissue damage.
4. Generalized activation of the coagulation system (via factor XII) leads to disseminated intravascular
coagulation (DIC), thrombosis and tissue ischaemia.
5. There is increased phagocytic activity of macrophages and polyclonal B cell activation (but not T lymphocytes).
6. There is increased antibody production.
Endotoxin-like effects may also occur in Gram-positive bacteremic infections. However, as endotoxin is absent in Gram-positive bacteria, other cell wall components, such as teichoic acid or peptidoglycan, are thought to trigger the release of
TNF and IL-1 from macrophages
Exotoxins
Both Gram-positive and Gram-negative bacteria secrete exotoxins, whereas endotoxin is an integral component of the cell wall of Gram-negative organisms.Exotoxins in particular can cause disease in distant parts of the body as a result of diffusion or carriage of the toxin via systemic route
Exotoxins
are polypeptides whose genes are frequentlylocated on plasmids or lysogenic bacterial viruses. Essentially, these polypeptides consist of two domains or subunits: one for binding to the cell membrane and entry into the cell, and the other possessing the toxic activity
Bacterial exotoxins can be broadly categorized as:
• neurotoxins• enterotoxins
• miscellaneous exotoxins
Neurotoxins
Tetanus toxin, diphtheria toxin and botulinum toxin are all neurotoxins and their action is mediated via neuronal pathways
enterotoxins
EnterotoxinsThese toxins act on the gut mucosa and cause gastrointestinal disturbances
Miscellaneous exotoxins
An array of exotoxins are produced by C. welchii and other species of clostridia that cause gas gangrene.
These include the α-toxin (a phospholipase that hydrolyses lecithin, present in all eukaryotic cell membranes), collagenase, protease, hyaluronidase and deoxyribonuclease (DNAase).
Pathogenesis of viral disease
Viral pathogenesis can be defined
as the methods by which viruses produce disease in the host.
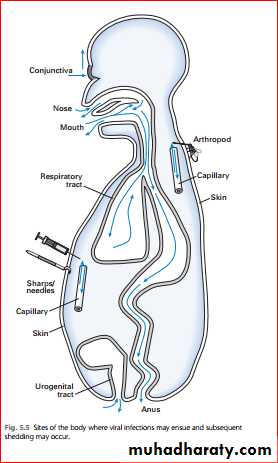
Entry of viral infections :-
As in bacterial infections, viruses gain entry into the host by:• inoculation (via the skin and mucosa)• inhalation (via the respiratory tract)• ingestion (via the gastrointestinal tract
Mechanisms of viral spread in the body
1-direct local spread on epithelial and sub epithelial surfaces2- lymphatic spread
3- viraemic spread
4- central nervous system and peripheral nerve spread
1- Local spread on body surfaces
A number of viruses cause disease on epithelial surfaces without systemic spread. Such infections are characterized by:• their localized nature
• direct viral shedding into the exterior or lumen (e.g. respiratory tract and alimentary tract infections with rhinoviruses and rotaviruses, respectively)
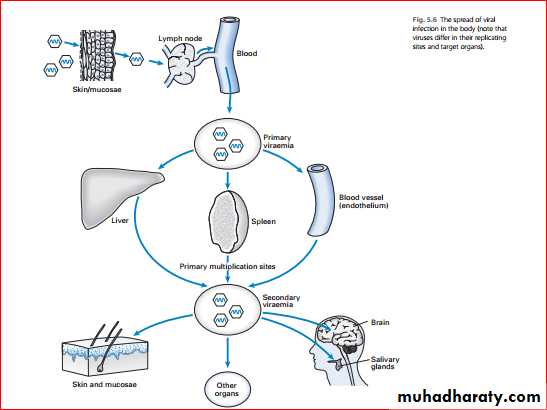
Lymphatic spread
The phagocytosed and free viral particles lurking beneath the epithelium rapidly enter the subepithelial /mucosal network of lymphatic capillaries and are carried to regional lymph nodes (Fig. 5.6). Lymph nodes serve two main functions:
1. They act as flters of extraneous microbes that gain
access to the lymphatic system.
2. They are the sites where immune responses are
generated
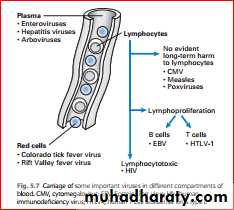
Viraemia and spread to organs
The entry of virus into the blood and its subsequent spread is called viraemia. Once a virus reaches the blood stream, it is effectively disseminated within minutes. The first episodeof viral entry into the blood is called a primary viraemia
The virus may then be seeded in various distant
organs, after which there is further replication at these sites and a second wave of viral entry into the blood stream – a secondary viraemia.This is usually larger than the primary viraemia and the virus is more easily detected in blood samples.
The secondary viraemia often leads to infection of other organs
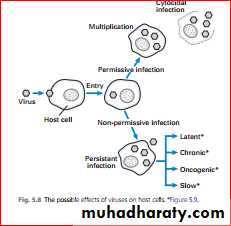
Virus and host cell interactions
Once the virus enters the host cell, it can interact with the
host cell in two main ways:
1. permissive infection, in which there is synthesis of viral components, their assembly and release.
2. non-permissive infection, in which the infection can result in cell transformation, often with the integration of viral DNA into the host genome.
Permissive infection
The infection of a cell by a virus may have one or moresequelae
The most common sequela is for the virus to replicate in a lytic or cytocidal infection, causing the cells to die and producing an acute illness. A virus infected cell may die as a result of:
• ’shut-down’ of host cell protein and nucleic acid
synthesis• cell lysis, by the release of progeny virions
• intracellular release of lysosomal enzymes
• damage to cell membranes.
Non-permissive infection
Cell death is not an inevitable accompaniment of viral replication. Sometimes a persistent infection may ensue inwhich there may be viral replication within the cell but the
cell remains alive. Many viruses can produce persistent infections. herpesviruses and retroviruses.
Factors that favour persistence include:
• low pathogenicity of the virus
• ineffective or no antibody-mediated or cell-mediatedhost immune responses
• defective or no interferon production
• infection of lymphocytes and macrophages by the virus
During the early phase of infection , befor cell death characteristic alteration in the infected cell membrane may occur
Hemadsorption (hemagglutinin)
In viruses leave the cell by budding through the plasma membrane viral glycoproteins first inserted into membrane. Acommon envelope protein is hemaglutinin . This protein enables an infected cell to attract red cell at the surface, aphenomena called hemadsorption.
Hemadsorption can be used in the laberatory to detect cell infected with certain viruses(e.g orthoviruses &Paramyxoviruses)
2- Gaint cell formation
Some viruses , Such as herpes simplex and Hiv promote cell fusion in with membranes of adjacent cell coalesce to produce multinucleated gaint cells. Other markers of viral infection include intra neuclear or cytoplasmic inclusion bodies .Pathogenesis of fungal disease
In general medically important fungi do not possess the virulent attributes of bacteria such as exotoxin and endotoxin( an exception is the exotoxin , aflatoxin, produce by Aspergillus Species) hence they cause slowly progressive chronic infection rather then the acute disease commonly seen in bacterial or viral diseases. However they may cause life – threating acute infections in immunocomprised patients (e.g. those with acquired immune deficiency syndrome (AIDES)
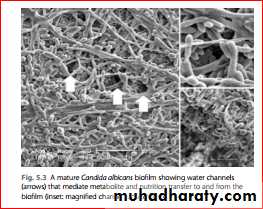
The oral fungal pathogen candida possesses a number of virulent attributes including:-
1- ability to adhere to host tissue(e.g. dentures) and form biofilms2- the ability to form hyphae that helps in tissue invasion
3- extracellular phospholipase and hemolysin production which break down physical defence barriers of the host