pg.
1
Fifth stage
Radiology
Lec-1
د.زينة
14/11/2016
Mediastinum and Heart
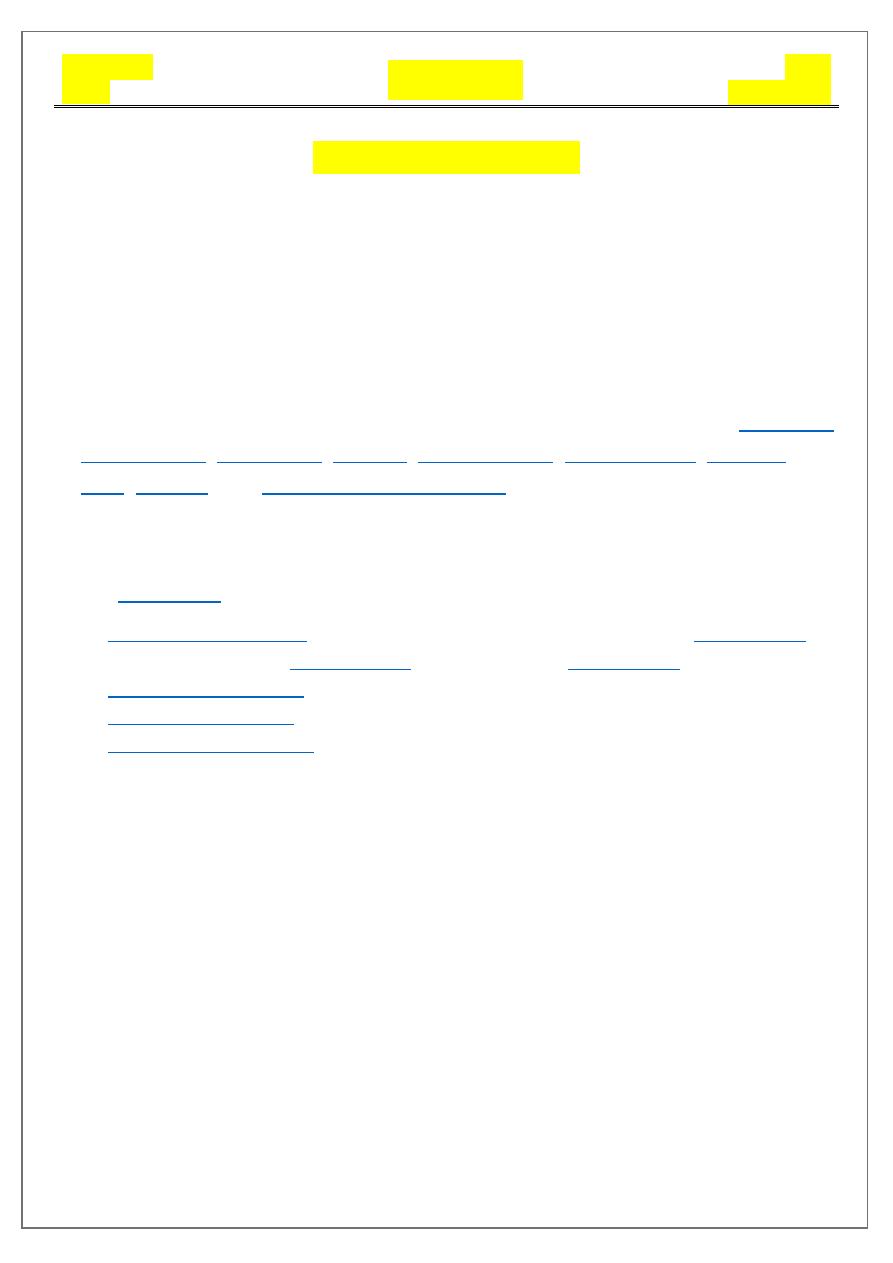
Mediastinum
Mediastinum is a space in the thorax that contains a group of non-delineated
organs and their surrounding connective tissue.
It lies in the midline of the chest between the pleural surfaces of
each lung and extends from the sternum to the vertebral column.
The mediastinum contains all the thoracic viscera except the lungs:
Anatomical division
The mediastinum can be divided into parts based on their relationship to the
1.
: is an artificially divided compartment of the
2.
: anterior to the pericardium
3.
: within the pericardium
4.
: posterior to the pericardium
Relations
1. superiorly: continuous with the loose connective tissue of the neck
2. anteriorly: chest wall
3. laterally: lungs and pleura
4. posteriorly: thoracic spine
5. inferiorly: diaphragm
pg.
2
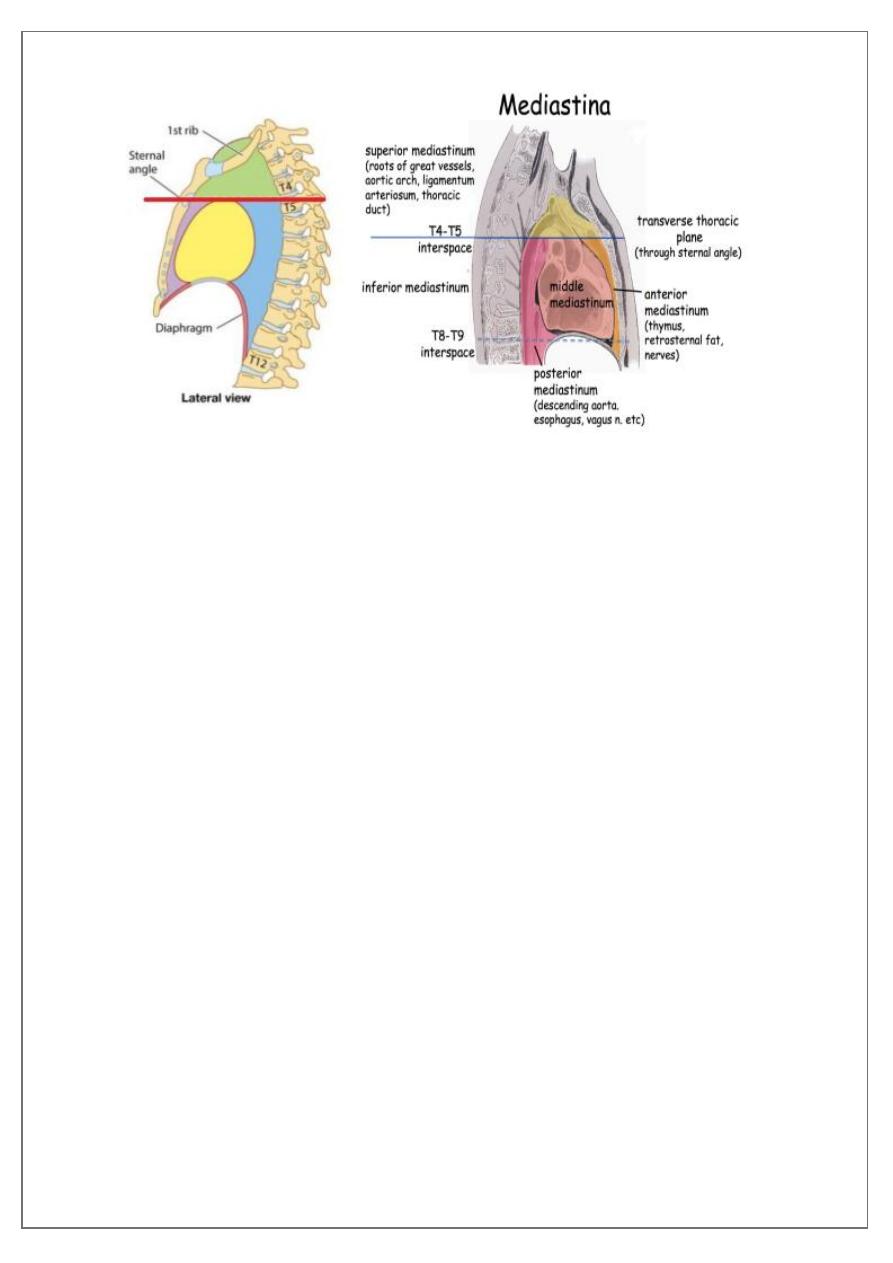
Mediastinal lesion
The differential diagnosis for an
anterior
mediastinal mass includes:
1. thymus
a. thymoma: most common primary neoplasm of the antero superior
mediastinum
b. thymic cyst
2.
a. thyroid neoplasms
b. thyroid goitre
c. parathyroid neoplasms
3.
a. Hodgkin lymphoma
b. non-Hodgkin lymphoma (NHL)
4.
5.
6.
pg.
3
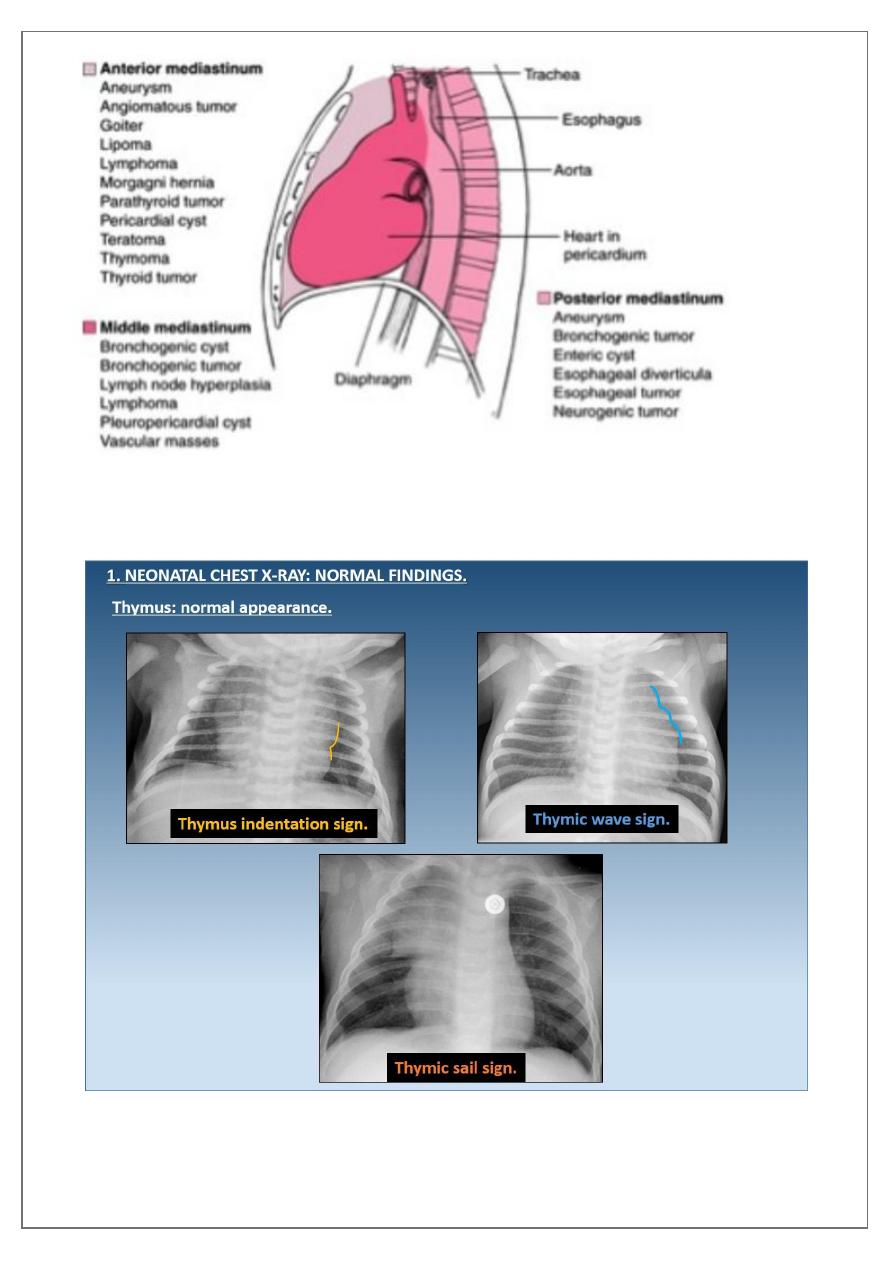
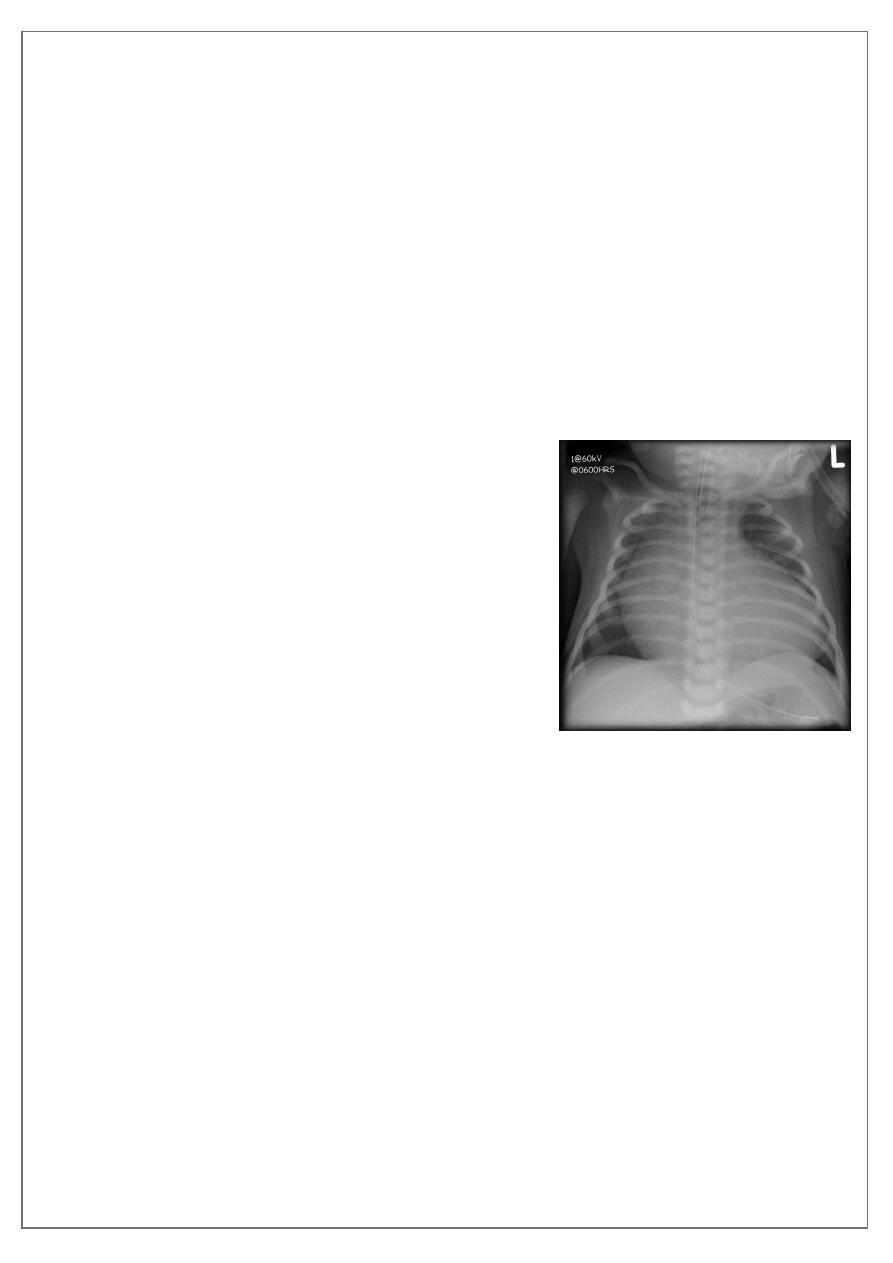
Normal thymus gland ( sail shape sign )
pg.
4
Retro sternal goiter
Radiographic features
Chest radiograph
It may show a superior mediastinal radio-opacity causing the deviation of trachea to
opposite site. The superior
margin of the radio-opacity/mass is untraceable (
.
pg.
5
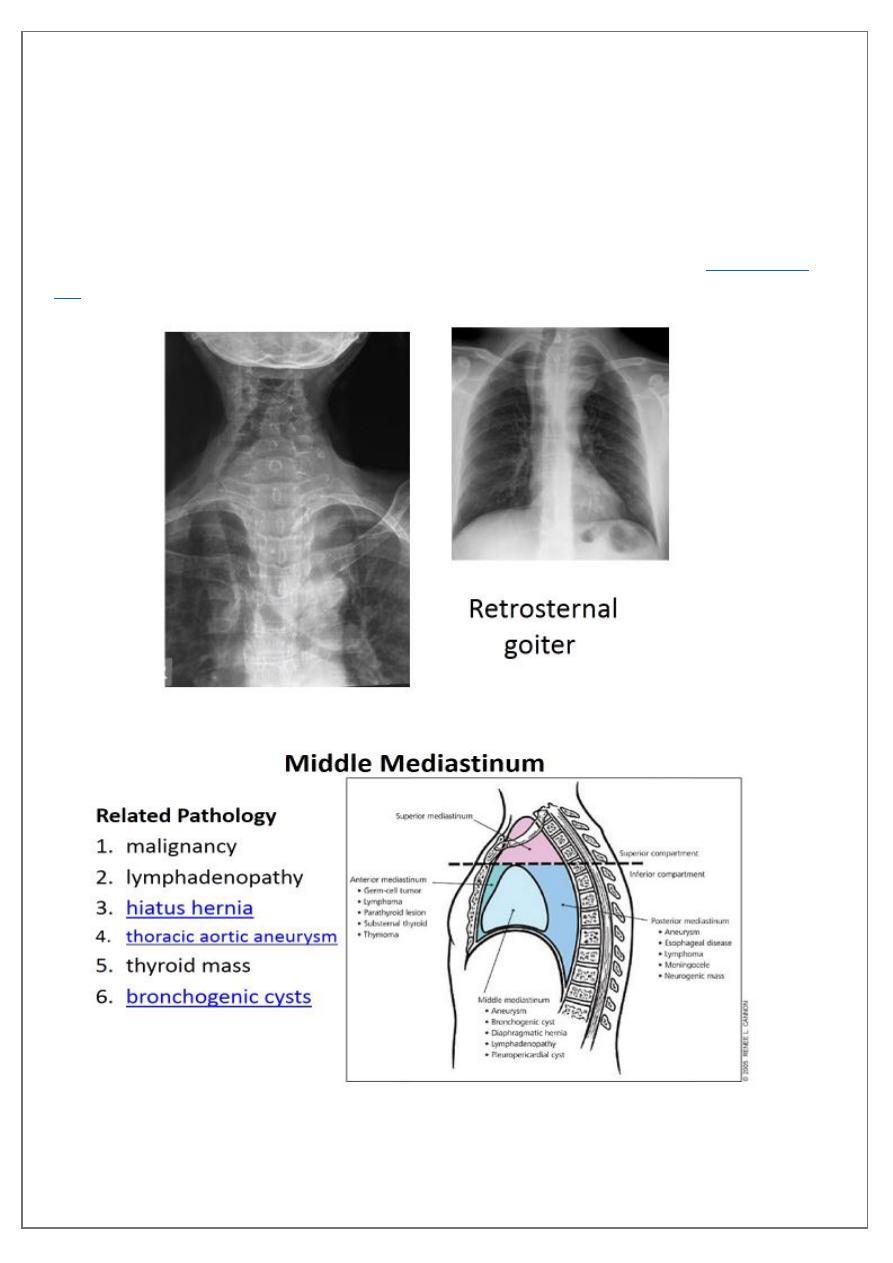
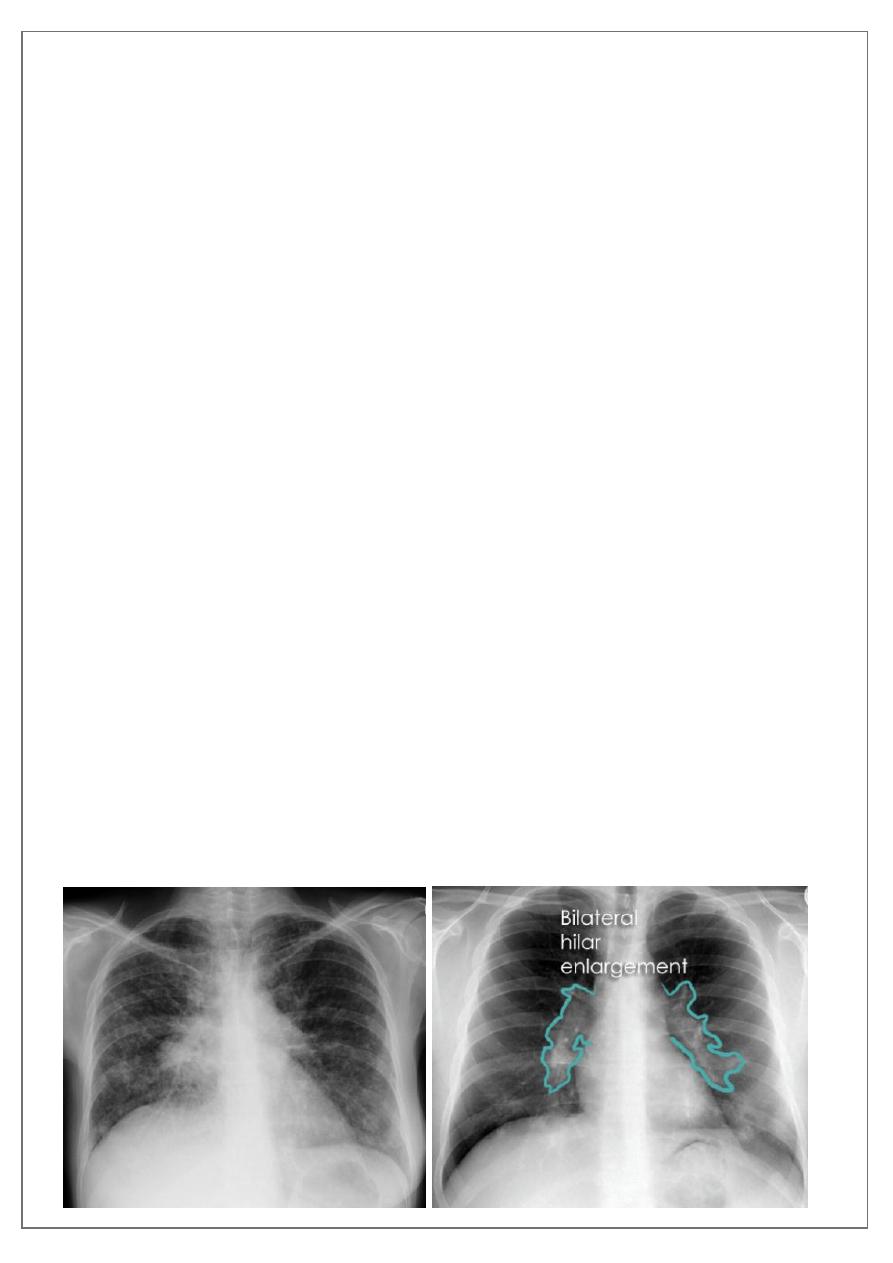
Lymph adeno pathy
The spectrum of conditions than can result in mediastinal lymph adenopathy is exhaustive
and includes:
2. metastatic malignancies to the mediastinum from other sites common
a.
b.
c.
3.
primary mediastinal large B-cell lymphom
4. Sarcoidosis
5. infective (acute suppurative)
6. reactive
a. follicular hyperplasia
b. granulomatous TB , fungal infection
c. neoplastic
d. drugs: e.g. cyclosporin, phenytoin, methotrexate
Lymphoma
is a malignancy arising from lymphocytes or lymphoblasts. Lymphoma can be
restricted to the lymphatic system or can arise as extra nodal disease. This, along
with variable aggressiveness results in a diverse imaging appearance.
Nodal disease
Hodgkin's disease is usually almost entirely confined to the lymph nodes.
Extra nodal disease
Extra nodal HD although uncommon may be found in any organ system, either as a
primary manifestation or as dissemination of systemic disease.
pg.
6
Hodgkin lymphoma of te middle mediastinum

pg.
7
The differential diagnosis for
a posterior
mediastinal mass includes:
1. neoplasm
a) neurogenic tumours most common nerve sheath tumours
b) non-neurogenic tumours
c) schwannoma
d) neurofibromaa
e) oesophageal neoplasm
f) lymphoma
g) metastasis
2.
infection
3. inflammation
b) sarcoidosis
4.
vascular
5. hernias
a) hiatus hernia
b) Bochdalek hernia
6. trauma
7. paraspinal hematoma
8. lymphadenopathy
9. extramedullary haematopoiesis
10. foregut duplication cysts
11. neurenteric cyst
12. oesophageal duplication cyst
pg.
8
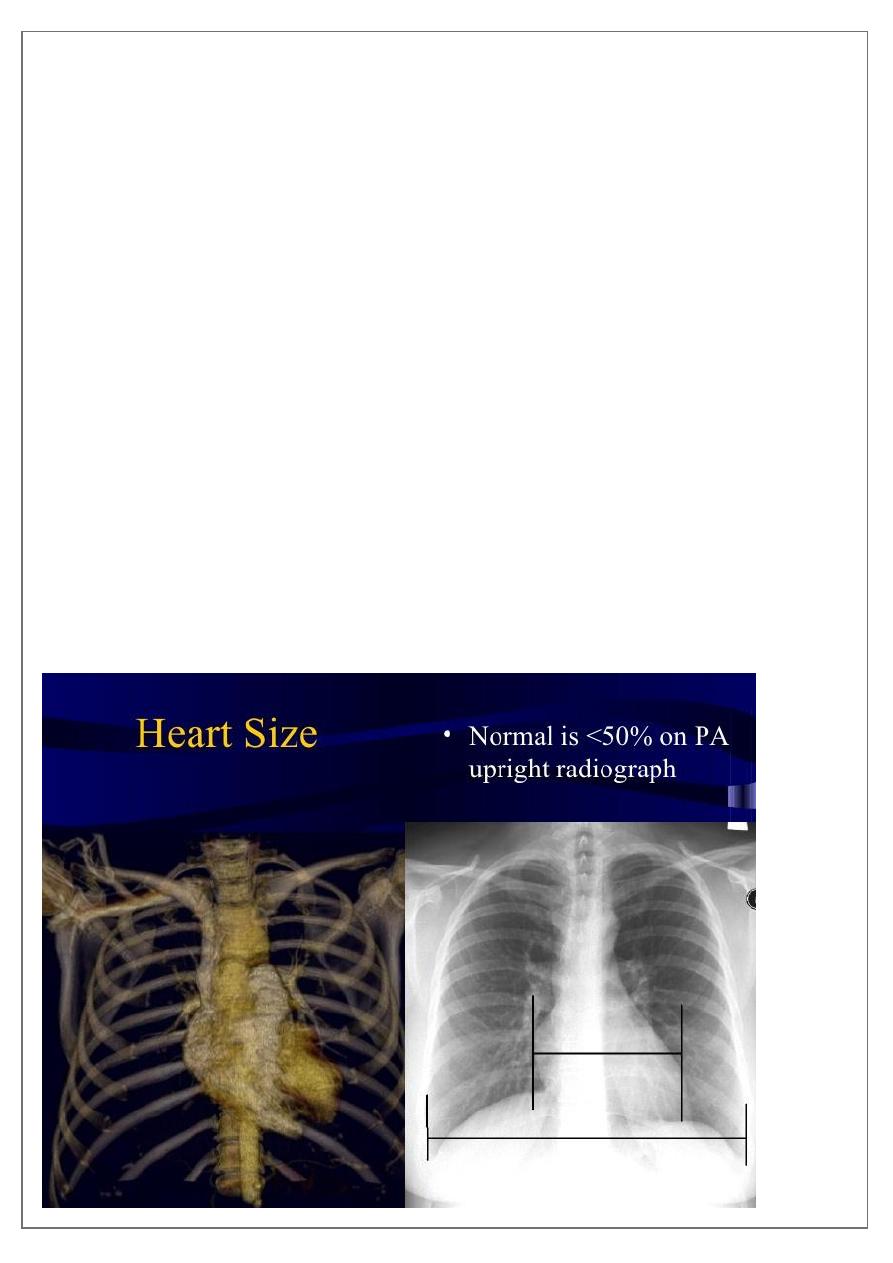
Heart
Assessment & measurement
The heart has a somewhat conical form and is enclosed by pericardium. It is positioned
posteriorly to the body of the sternum with one-third of it is situated on the right and two-
thirds on the left of the midline .
The heart has four borders:
, right atrium
, SVC
2) left border: left ventricle, left atrium, pulmonary trunk and arch of aorta
3) inferior border: right ventricle
4) superior border: right and left atria, SVC, ascending aorta and pulmonary trunk
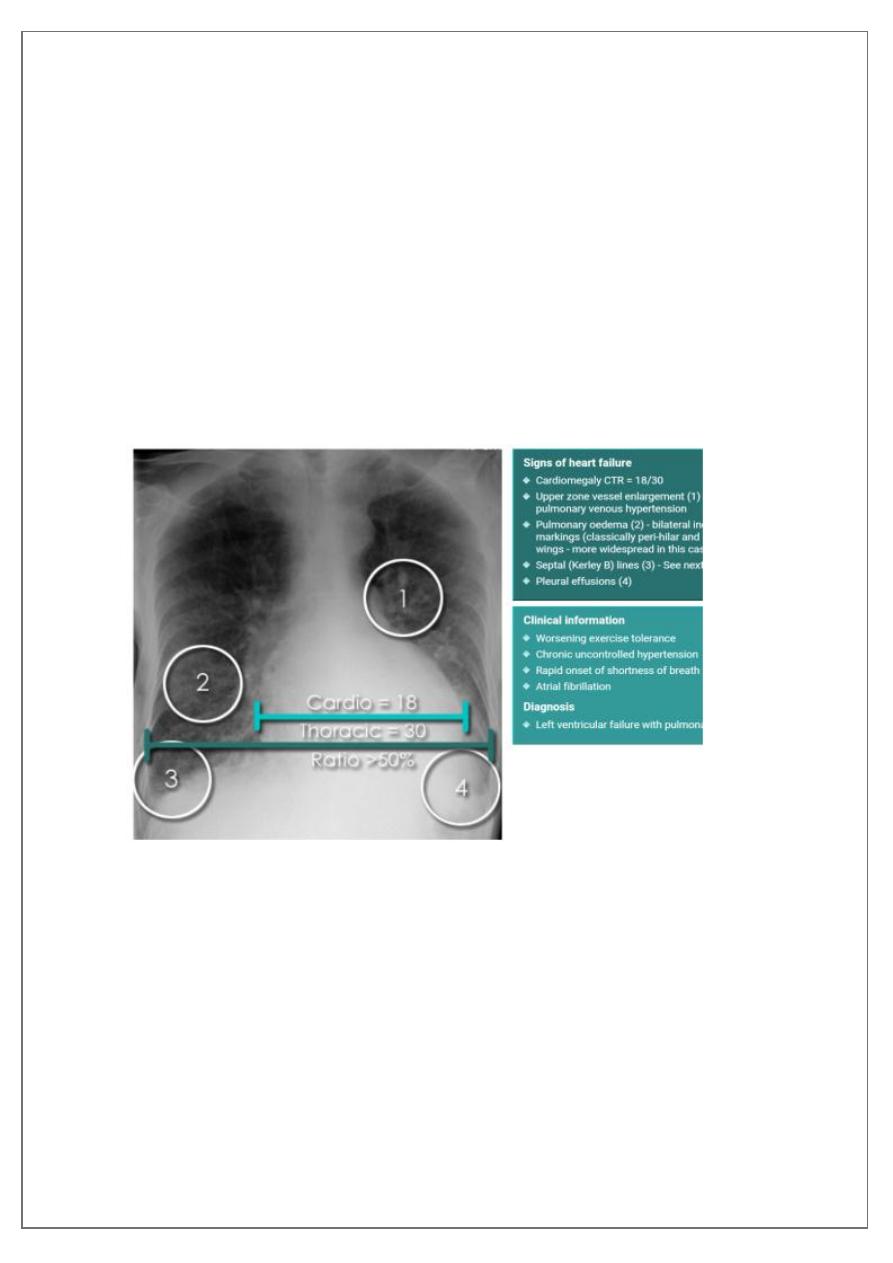
Cardiothoracic ratio (CTR) = Cardiac Width : Thoracic Width
A CTR of greater than 1:2 (50%) is considered abnormal. This however, assumes the
projection is Posterior-Anterior (PA), and that cardiac size is not exaggerated by factors
such as patient rotation or an incomplete breath in .
The cardiothoracic ratio aids in the detection of
, or more
pg.
9
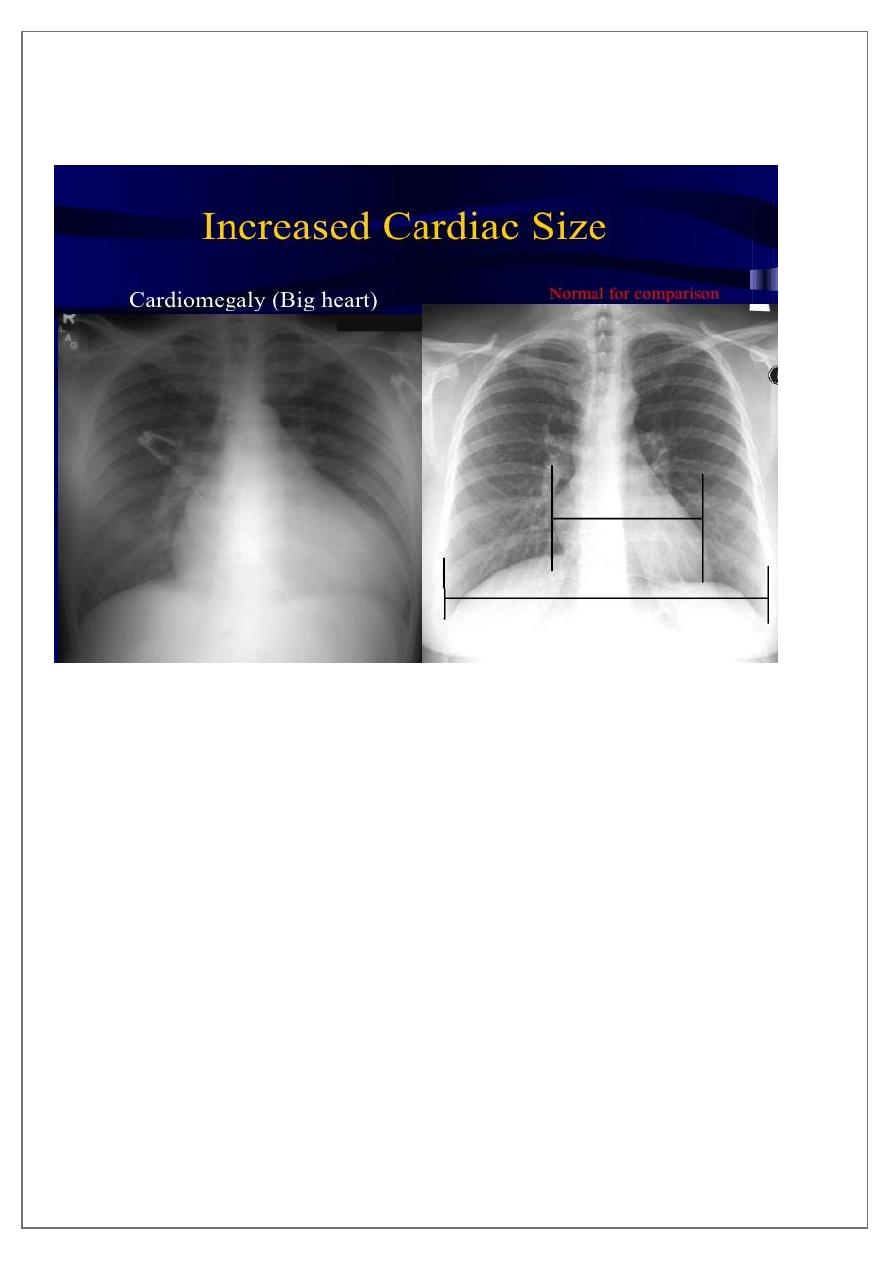
Enlargement of the cardiac silhouette on chest x-ray can be due to a number of causes :
1. cardiomegaly (most common cause by far)
2. pericardial effusion
3. anterior mediastinal mass
4. prominent epicardial fat pad
Causes of cardiomegaly
There are many aetiologies for cardiomegaly. The list includes:
1. Mitral valve disease
2. Congestive heart failure
3. Congenital heart disease
a. -tetralogy of Fallot
b. -Ebstein anomaly
pg.
11
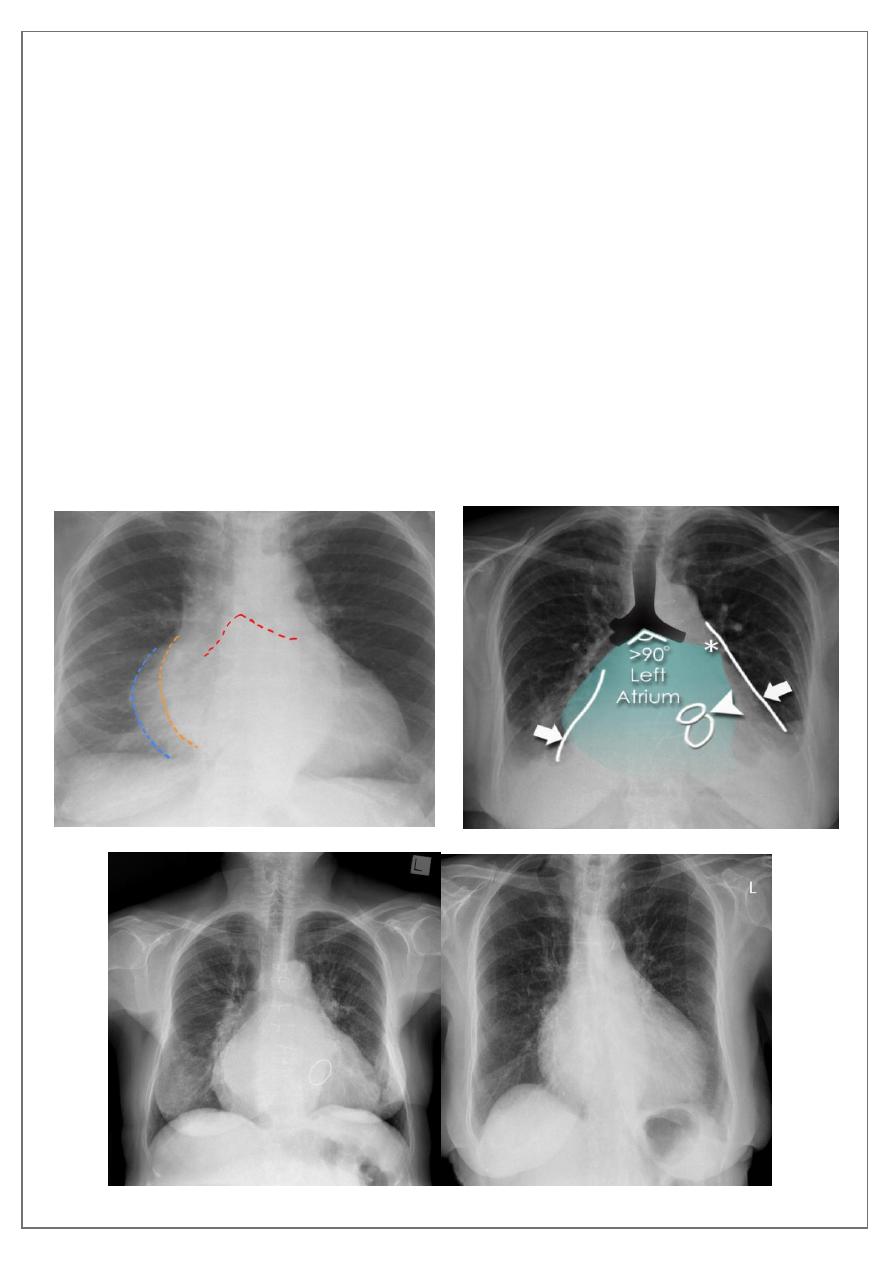
Mitral valve disease
Radiographic features
Plain film
Typical radiographic features of mitral regurgitation include :
frontal projection
1. left atrial enlargement
convexity or straightening of the left atrial appendage just below the main
pulmonary artery (along left heart border)
2.
double density sign
: the right side of the enlarged left atrium pushes into the
adjacent lung and creates an addition contour superimposed over the right heart
3. elevation of the left main bronchus and splaying of the carina
4. upper zone venous enlargement due to pulmonary venous hypertension
5. left ventricular enlargement is also eventually present due to volume overload
6.
Features of pulmonary oedema may also be present
.
pg.
11
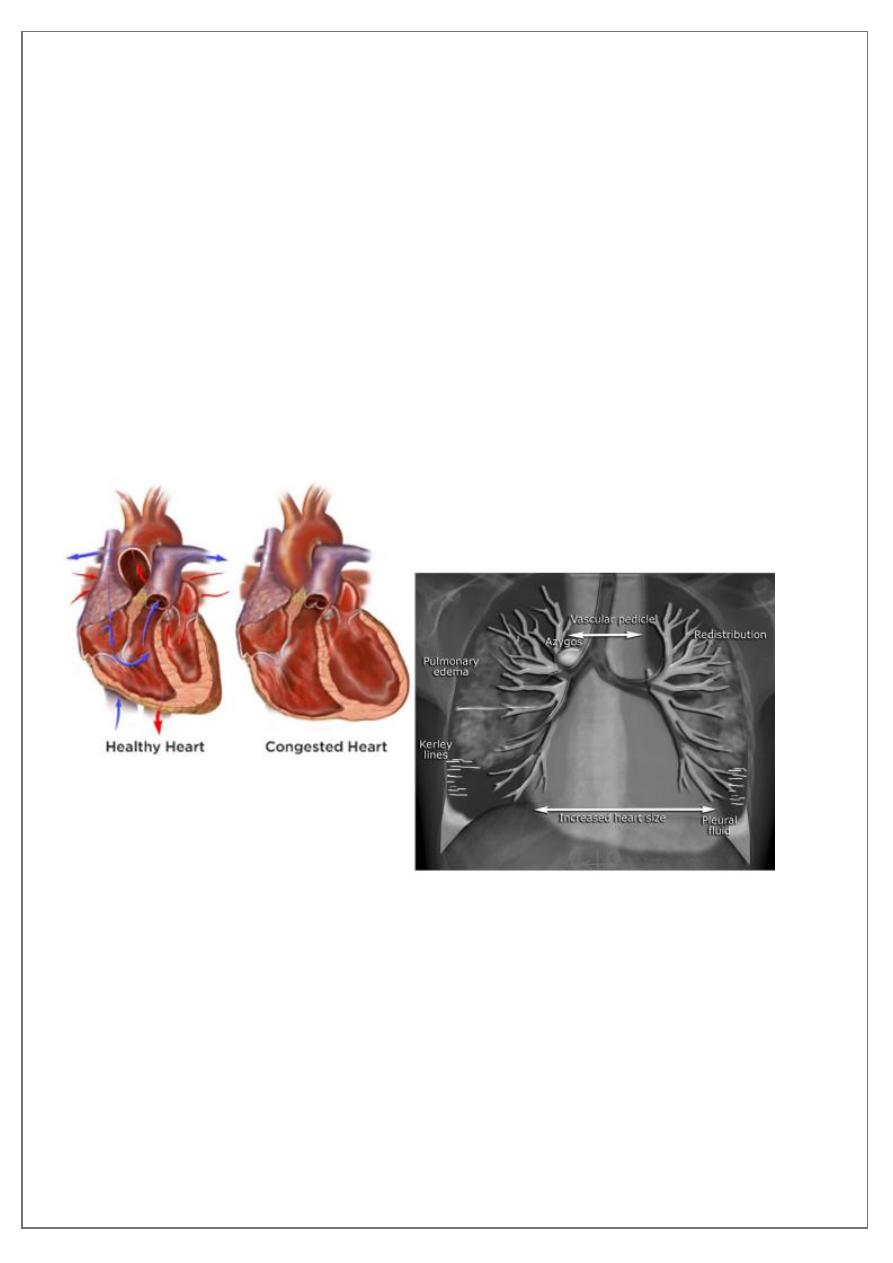
Congestive cardiac failure (CCF)
is a form of cardiac failure which is primarily
manifested by the heart inability to pump the volume of blood. It can affect the left
(common) or right cardiac chambers or both.
Radiographic features
Chest radiograph
With left sided congestive cardiac failure, the features are that of pulmonary edema which
includes:
1. central pulmonary venous congestion ( prominent hilum )
2. cephalisation of pulmonary veins ( upper lobe pulmonary venous diversion )
3. pulmonary interstitial oedema
4. pulmonary alveolar oedema
5. Cardiomegaly
6. Pleural effusion
pg.
12
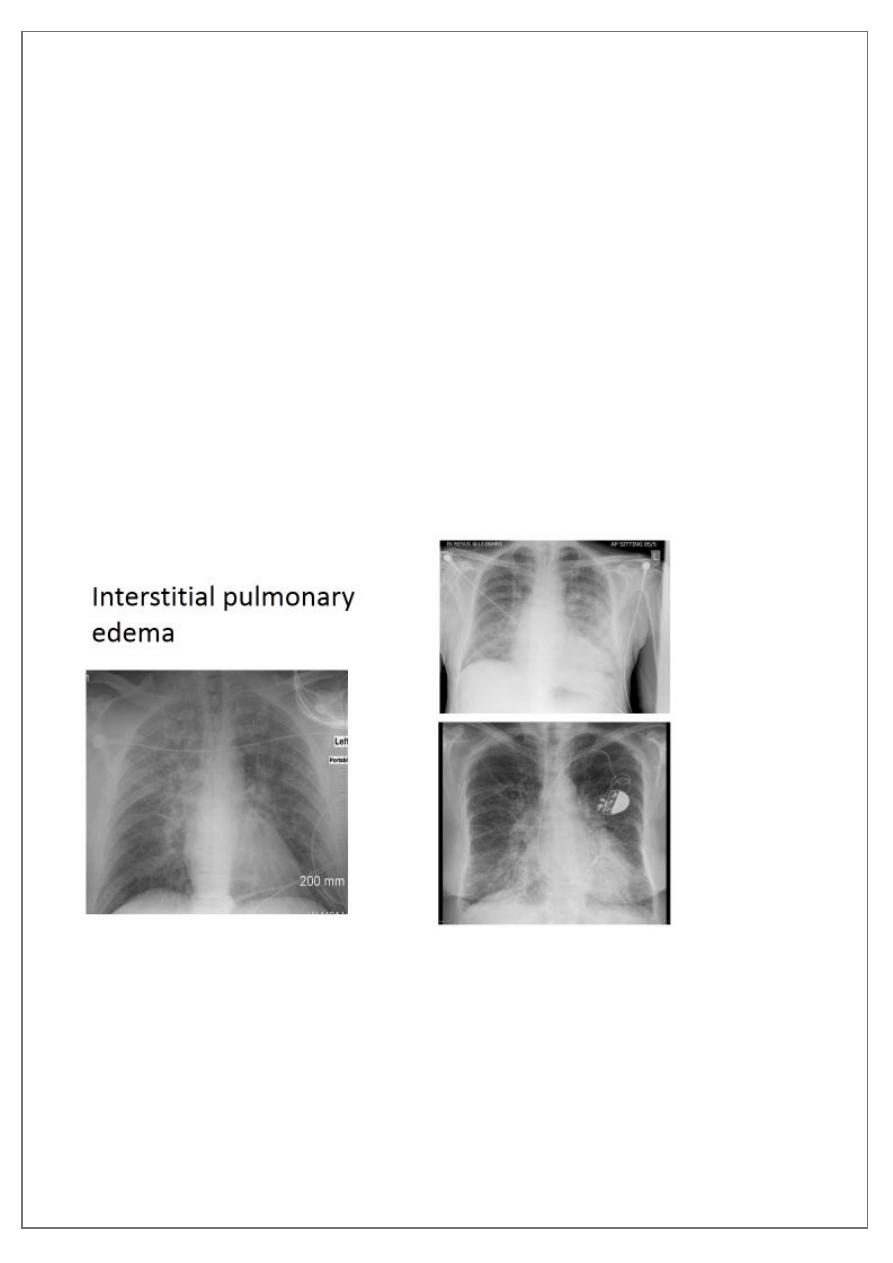
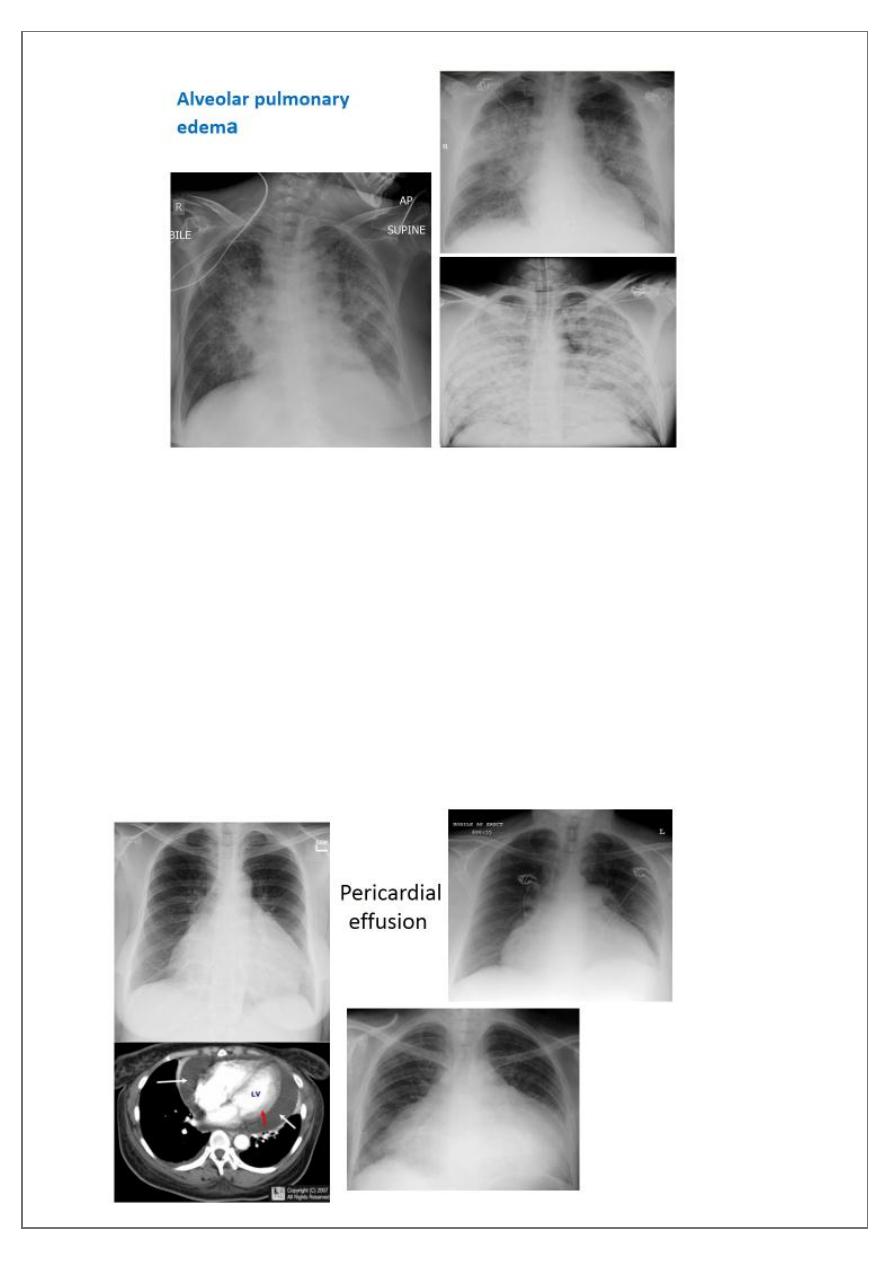
Pulmonary edema
is a broad descriptive term and is usually defined as an abnormal
accumulation of fluid in the extra-vascular compartments of the lung .
Radiographic features
Septal lines
, also known as
Kerley lines
in the
become prominent. This may be because of lymphatic engorgement
or edema of the connective tissues of the interlobular septa. They usually occur when
pulmonary capillary wedge pressures reach 20-25 mmHg ,
Classification
1. Kerley A lines
These are 2-6 cm long oblique lines that are <1 mm thick and course towards
the hila. They represent thickening of the interlobular septa
2. Kerley B lines
These are 1-2 cm thin lines in the peripheries of the lung. They are perpendicular
to and extend out to the pleural surface . They represent thickened sub pleural
interlobular septa and are usually seen at the lung bases.
pg.
13
radiograph include if pressure > 25 mmHg the findings of :
1. cardiac size/
: useful for assessing for an underlying
cardiogenic cause or association
2. bat wing pulmonary opacities
3. presence of peri-bronchial cuffing
4.
Kerley lines become more prominent
6.
/pulmonary blood flow distributionupper lobe
pg.
14
Pericardial effusions
occur when fluid collects in the pericardial space (a normal
pericardial sac contains approximately 30-50 mL of fluid).
Radiographic features
Plain radiograph
a very small pericardial effusion can be occult on plain film there can be globular
enlargement of the cardiac shadow giving
shape heart or pumpkin shape heart
pg.
15
.
Congenital heart disease
A . CCHD
A number of entities can present as cyanotic congenital heart disease. These can be divided
into those with increased or decreased pulmonary vascularity. They include:
1) increased pulmonary vascularity
a) total anomalous pulmonary venous return (TAPVR) (types I and II)
b) transposition of the great arteries (TGA)
c) truncus arteriosus (types I, II and III)
d) large AVSD
e) single ventricle without pulmonary stenosis
2) decreased pulmonary vascularity
a) tetralogy of Fallot
b) pentalogy of Cantrell
c) many other combined and infrequent anomalies such as
d) Ebstein anomaly with atrial septal defect
B . ACCHD
There are numerous causes of acyanotic congenital heart disease and can be divided into
those that have increased pulmonary vascularity and those that do not. They include:
1) increased pulmonary vascularity
a) ventricular septal defect (VSD)
b) atrial septal defect (ASD)
c) atrioventricular septal defect (AVSD)
d) patent ductus arteriosus (PDA)
2) normal pulmonary vascularity
a) small shunts (see above)
b) aortic valve stenosis
c) aortic coarctation
d) pulmonary stenosis
pg.
16
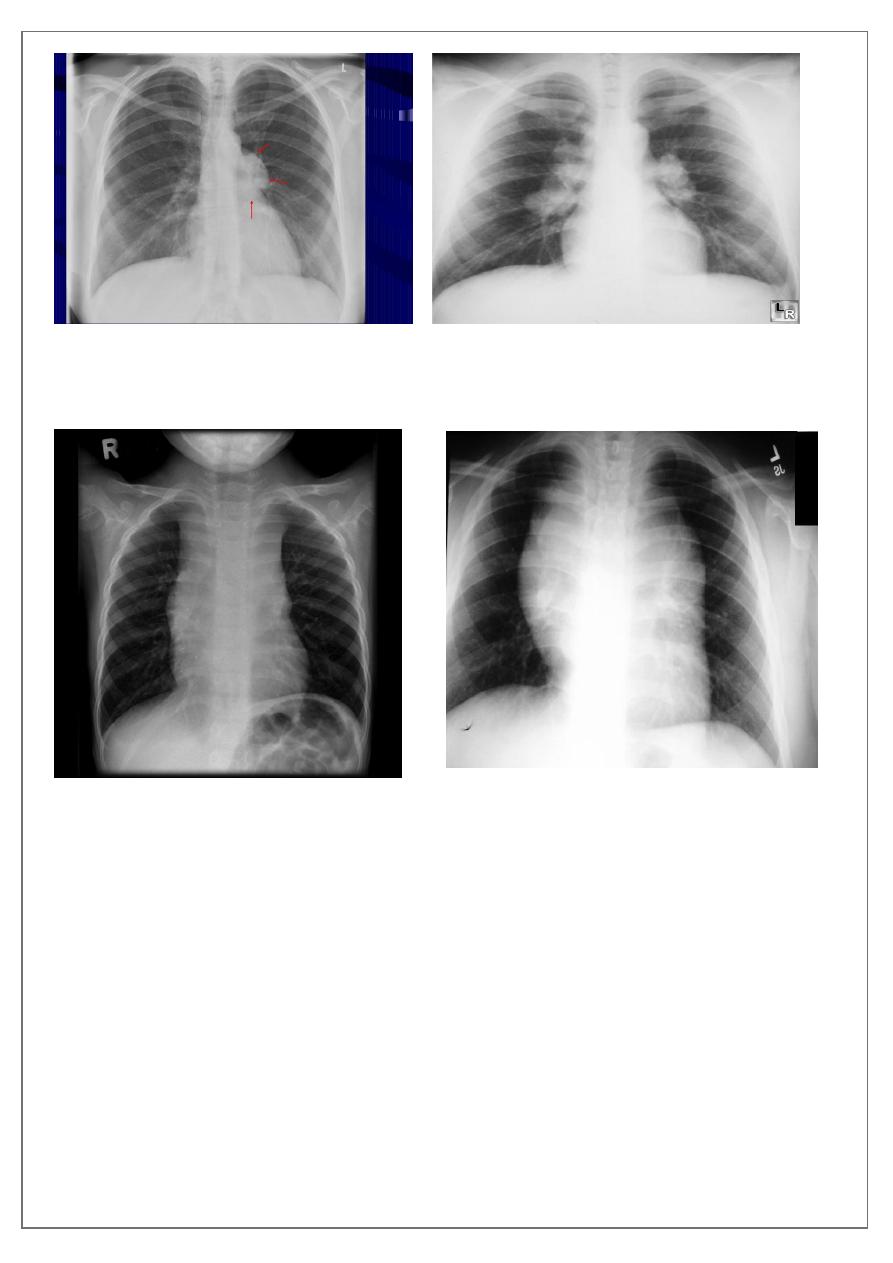
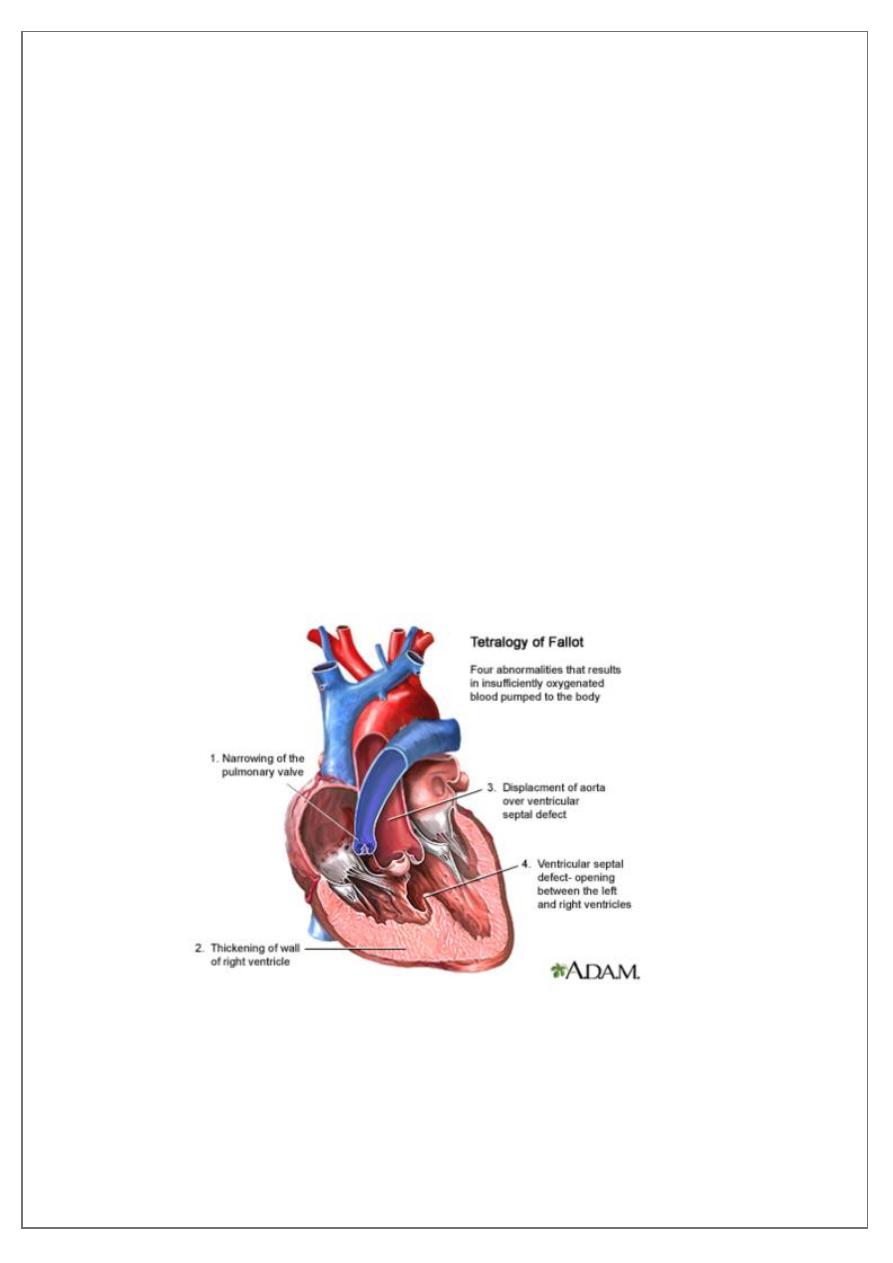
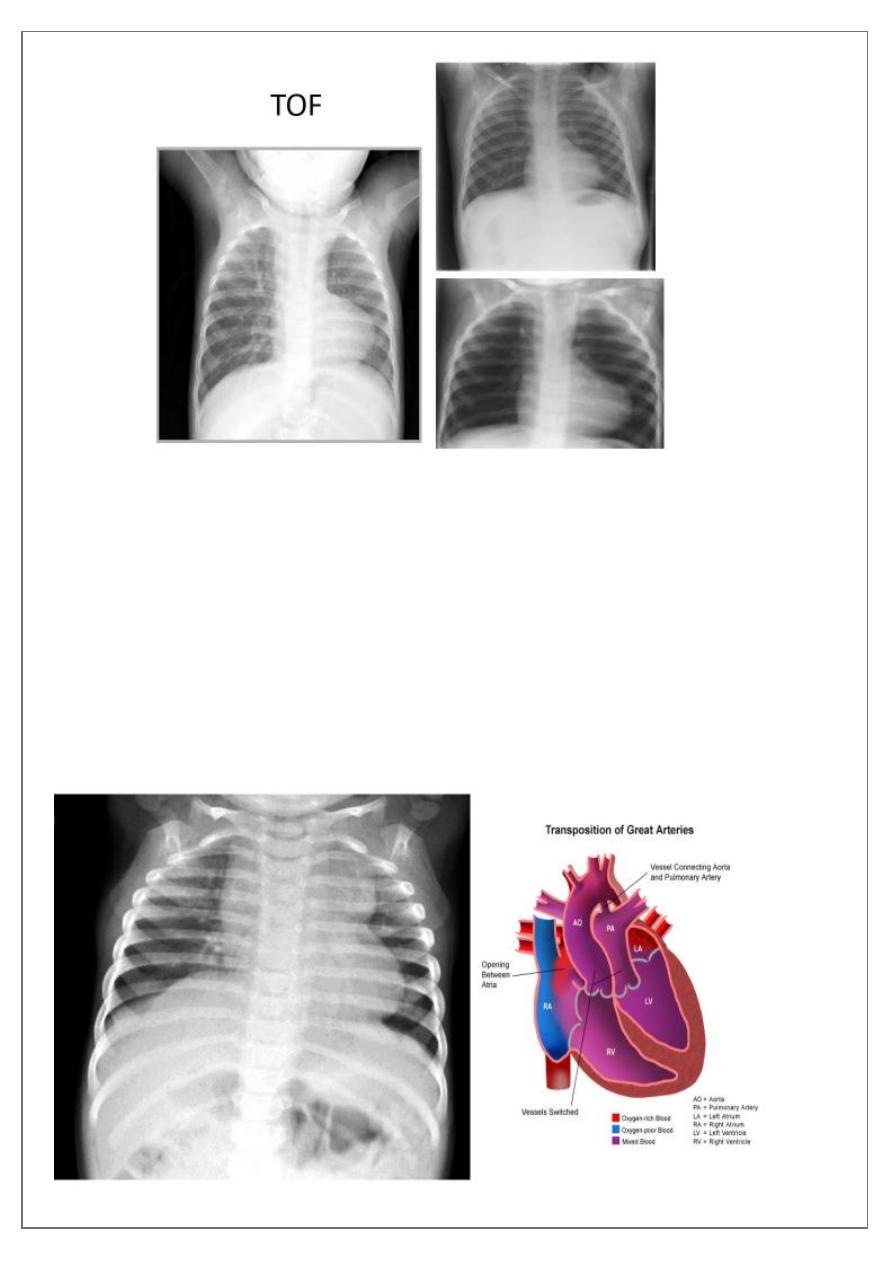
Tetralogy of Fallot (TOF)
is one of the most common cyanotic congenital heart
conditions and continues to be a major source of morbidity .
Tetralogy of Fallot is classically characterised by four features which are:
1) ventricular septal defect (VSD)
6
2) right ventricular outflow tract obstruction (RVOTO) due to:pulmonary artery
stenosis
3) overriding aorta
4) right ventricular hypertrophy
Radiographic features
Plain film
Plain films may classically show :
1) "boot shaped" heart with an upturned cardiac apex due to right ventricular
hypertrophy and concave pulmonary arterial segment.
2) Pulmonary oligaemia due to decreased pulmonary arterial flow.
3) Right sided aortic arch is seen in 25%.
pg.
17
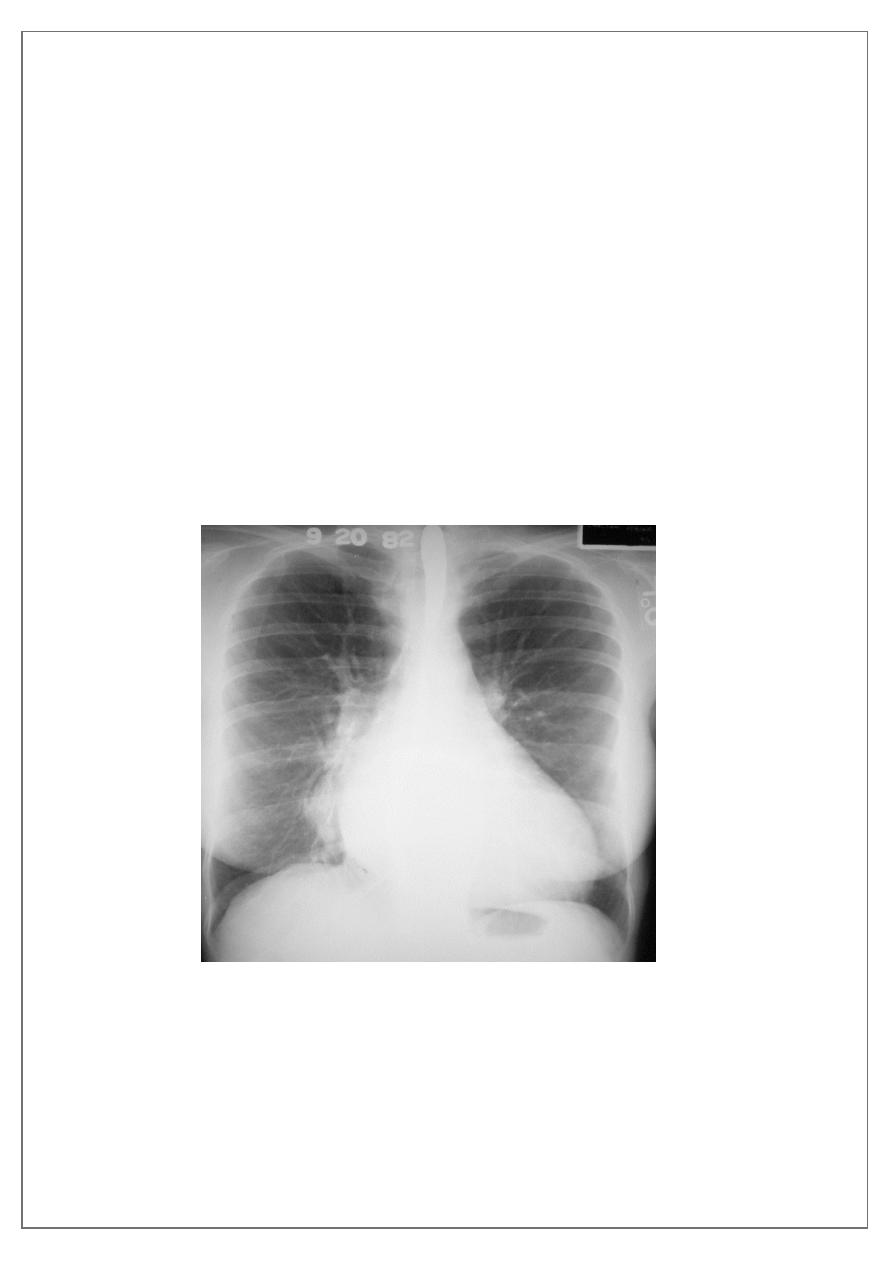
Transposition of the great arteries (TGA
)
is the most common cyanotic congenital
cardiac anomaly with cyanosis in first 24 hours of life. It accounts for up to 7% of all
congenital cardiac anomalies
Chest radiograph
A frontal chest radiograph classically shows cardiomegaly with a cardiac contours classically
described as appearing like an
. There is often an apparent narrowing of the
superior mediastinum as result of the aortic and pulmonary arterial configuration .
Egg-on-a-string sign ( TGA )
pg.
18
Ventricular septal defects (VSD)
They represent one of the most common congenital
cardiac anomalies and up to 40% associated with such anomalies . They are considered the
most common congenital cardiac abnormality diagnosed in children and the second most
common diagnosed in adults
Ventricular septal defects (VSD)
represent defects in the inter ventricular septum that allow
a hemodynamic communication between the right and left ventricles. It typically results in
a left to right shunt.
Radiographic features
Plain film
The chest radiograph can be normal with a small VSD.
Larger VSDs may show
1) cardiomegaly (particularly left atrial enlargement although the right and left
ventricle can also be enlarged).
2) A large VSD may also show features of pulmonary arterial hypertension.
3) pulmonary oedema
4) pleural effusion and/or increased pulmonary vascular markings.
Pulmonary arterial hypertension
results from elevation of the resistance in the pulmonary arterial bed, usually at the
arteriolar level. It is characterized radiographically by enlargement of the pulmonary trunk
and right and left main pulmonary arteries with disproportionately small peripheral vessels
This has been referred to as "pruning" of the pulmonary arteries
So the Plain radiograph
1) elevated cardiac apex due to right ventricular hypertrophy
2) enlarged right atrium
3) prominent pulmonary outflow tract
4) enlarged pulmonary arteries
5) pruning of peripheral pulmonary vessels
pg.
19
Pulmonary venous hyper tension
Pulmonary venous hypertension (PVH) results from an increase in pressure in the
pulmonary veins, usually as a result of left atrial hypertension. This is measured clinically as
an increase in the pulmonary capillary wedge pressure (PCWP) over the normal 12 to 14
mmHg.
Mild elevation of the PCWP results in redistribution of the pulmonary blood flow to the
non-dependent lung zones
As the pressure approaches 20 mmHg, interstitial edema develops
Common causes of PVH:
1.obstruction to LV inflow,
2.LV systolic dysfunction,
3.severe mitral regurgitation,
4.acute pulmonary and systemic volume overload.
pg.
21
Eisenmenger syndrome
is a complication of an uncorrected high-flow, high-
pressure congenital heart anomaly leading chronic pulmonary arterial hypertension and
shunt reversal
.
Important Complications of VSD
Eisenmenger phenomenon with shunt reversal (i.e. L to R becomes R to L)
Very important to consider
1)
contour abnormality of the aorta with inferior rib notching
: Roesler sign in Coarctation of the aorta
2)
"box shape"
heart in Ebstein anomaly
3)
boot shaped heart (
TOF )
4) Egg-on-a-string sign (
TGA
)
5) figure of 8 heart or cottage loaf heart in Total
anomalous pulmonary venous return (
TAPVR
)
"box shape" heart in Ebstein anomaly
