Fifth stage
ENTعملي-كتابة الطلاب
د.سعد
7/12/2015
ENT = Ear Nose ThroatORL = otorhinolaryngology
1- The Ear:
Symptoms of the ear:Pain:
Primary or secondary.
Otogenic (caused be otitis media for example).
Non-otogenic (cause be problems in the tooth, glossopharyngeal nerve, C2 and C3, maxillary division of trigeminal nerve, temporomandibular joint, cervical spine).
Discharge:
Mucus: due to perforated tympanic membrane.
Serious: due to otitis externa or perforated tympanic membrane.
Hearing loss.
Tinnitus.
Vertigo.
Note: anything cause hearing loss could lead to tinnitus.
Examination of the ear:
Introduce yourself to the patient:
Check hearing function, Any deafness?
Communication
Position the patient:
At the same level
In chair
Can walk around patient
Inspect the pinna
Front and behind
Skin condition
Lesions
Scars
Pre-auricular area (common place for sinus)
Condition of cartilage
Findings in inspection of the pinna
Photos
Post auricular scar
Indications:
1-Tympanoplasty
2-mastoid surgery (mastoidectomy)
3-resection of benign parotid gland tumor
Benefit: cosmetic.
Discharging ear
Causes:1-wax
2-otitis media
3-otits externa
4-mastoiditis
5-F.B. in the ear
Preauricular sinus
Cause: congenital.Treatment: no treatment unless infected antibiotics or surgery.
Could convert to fistula (discharge) or abscess (closed).
Auricular hematoma
Causes:
1-trauma
2-bleeding tendency
3-infection.
4-allergic skin diseases
Treatment: complete surgical evacuation of the subperichondrial blood and prevent its recurrence.
It need drainage if not deformity of the ear.
Main complication: cauliflower ear.
Cauliflower ear
Due to repeated trauma and hematomaCommon in boxers.
Treatment: cosmetic surgery.
Auricular ulcer
Occur in squamous cell carcinomaAcute mastoiditis
Causes: untreated acute otitis media(commonest) + traumaMedical treatment: long term antibiotics.
Surgical treatment:
1-tympanostomy tube.
2-mastoidectomy.
Complications:
1-subperiosteal abscess 2-skin fistula
3-hearing loss 4-facial palsy
5-meningitis 6-brain abscess
Right acute mastoiditis
The right pinna pushed forward and downward.Postauricular Hearing aid
orbehind the ear (BTE)
BAHA: Bone Anchored Hearing Aid
Palpation:
Tragal tenderness: due to otitis externa.
Tenderness on mastoid bone: due to acute mastoiditis.
Inspect the external auditory meatus:
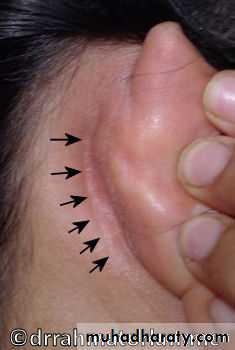
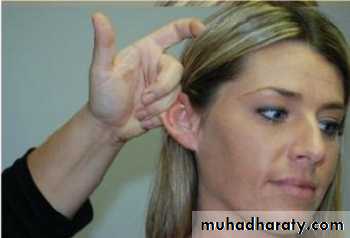
Pull pinna upwards, outwards and backwards
In infants downwards and backwards
In children pull backwards
See: Otorrhoea, otomycosis, Wax, Canal stenosis, Exostoses, osteomas.
There are three methods of inspection of external auditory meatus:
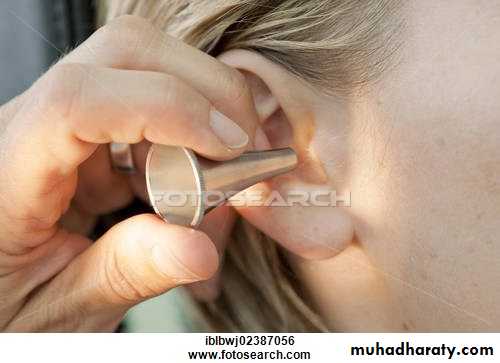
1- Aural (ear) speculum:
It is unaided eye method:
Use head light or mirror.
The pinna is pulled upward and backward.
Findings:
Wax.Otitis externa: red, pain, pus.
Otomycosis: due to candida albicans (white) or aspergillus niger (dots) both called wet newspaper.
Foreign body: very severe irritation / put light or esperto or oil.
Foreign body in the ear
Foreign body in the ear
Otomycosis
Otomycosis
Wax,
Conductive hearing loss
Wax,
Conductive hearing lossOtitis Externa
Otitis Externa
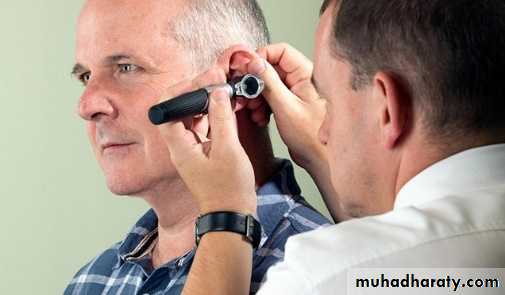
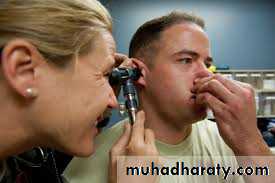
2- Otoscope:
It is aided eye method.
Examine right ear with right hand.
Pull the pinna upward, outward and backward.
The auroscope magnification is 1.5-2.0 times.
3- Microscope:
It is aided eye method.
Its magnification is 6-20 times.
Uses:
1-detailed examination of the ear (magnified up to 6-20 times)
2-certain surgical operations
3-biopsy
4-cleaning
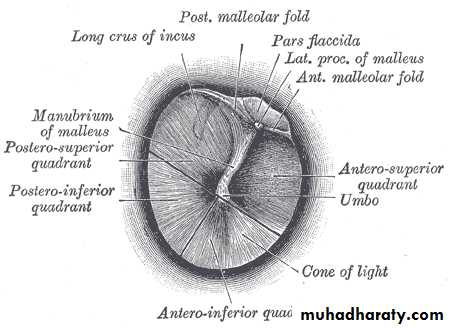
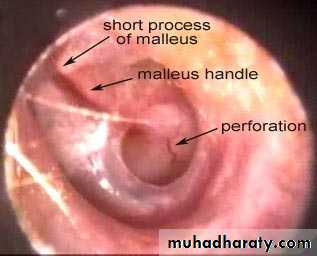
Examination of the tympanic membrane:
Oval – pearly gray color.There is handle of malleus.
There is cone of light shatter اختفاء the cone of light when the tympanic membrane is pulled or pushed.
Divided by two lines into 4 quadrants.
Congested tympanic membrane with loss of cone of light, redness and pulging of the membrane
Dx: acute otitis media
Pain occur at night because there is no swallowing (eustachian tube is open)
Congested tympanic membrane with loss of cone of light, redness and pulging of the membrane
Dx: acute otitis media
Pain occur at night because there is no swallowing (eustachian tube is open)
Normal tympanic membrane
Normal tympanic membrane
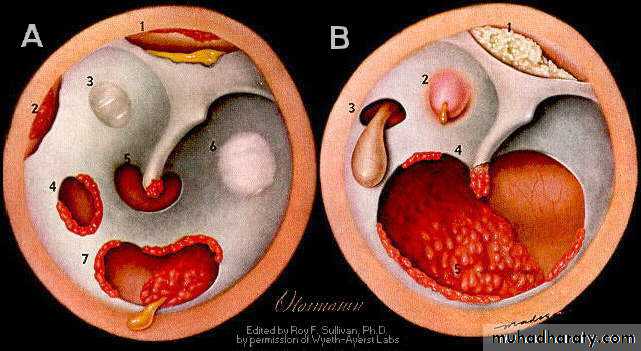
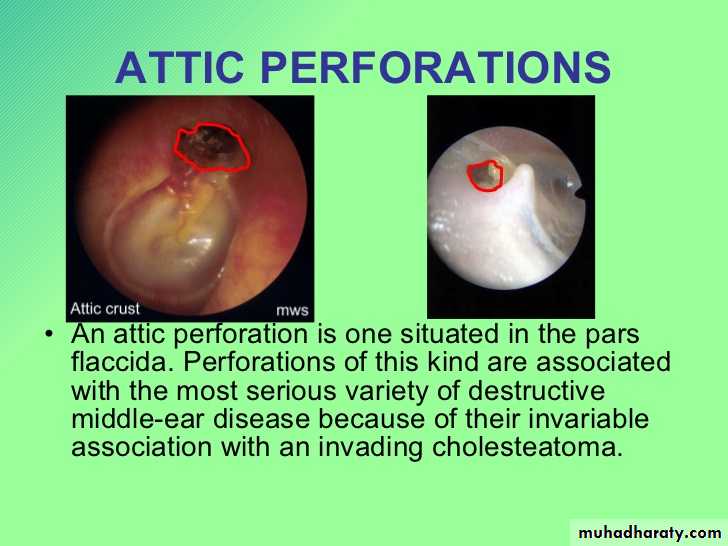
Tympanic membrane perforations:
Causes :
1-trauma
2-infection
3-iatrogenic (medical mistakes)
Types of perforation:
1- Safe (Central) the perforation is surrounded by part of the tympanic membrane.
cholesteatoma
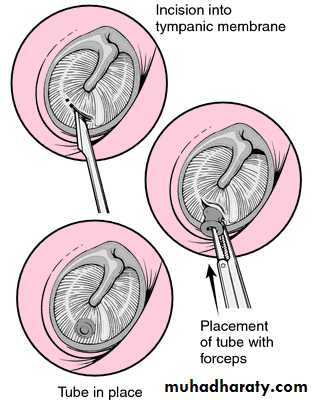
Otitis media with effusion Eustachian tube dysfunction is the commonest cause
Myringotomy with insertion of Grommet ventilation tube
-indication
1-CHRONIC O.M. with effusion (commonest in child)
2-recuurent O.M.
3-Eustachian tube dysfunction with recurrent s and s (commonest in adult)
4-recuurent episodes of barotrauma
Complication: blockage , otorrhea , chloesteatoma , tympanosclerosis
Tympanosclerosis
Precipitation of ca carbonate after healing of repeated perforation or myringotomy
Perforation of the tympanic membrane
cholesteatoma
Otitis media with effusion Eustachian tube dysfunction is the commonest causeMyringotomy with insertion of Grommet ventilation tube
-indication1-CHRONIC O.M. with effusion (commonest in child)
2-recuurent O.M.
3-Eustachian tube dysfunction with recurrent s and s (commonest in adult)
4-recuurent episodes of barotrauma
Complication: blockage , otorrhea , chloesteatoma , tympanosclerosis
Tympanosclerosis
Precipitation of ca carbonate after healing of repeated perforation or myringotomy
Perforation of the tympanic membrane
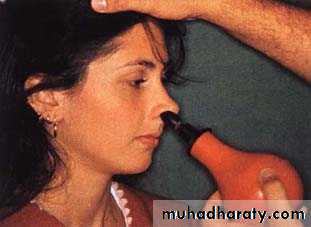
2- Unsafe (Marginal and Attic perforations).Assessment of tympanic membrane mobility
Valsava manover (close mouth and nose and swallow)Seigle pneumatic speculum (also used for magnification)
Politzerization (balloon in the nose and drink water)
Causes of fixed tympanic membrane fluid behind the membrane (otitis media), fibrosis, calcifications (tymeno-sclerosis), perforation.
Assessment of Hearing
While assessing the auditory function it is important to find out:
Type of hearing loss ( CHL, SNHL or mixed )
Degree of hearing loss.
Site of lesion.
Cause of hearing loss.
Causes of conductive hearing loss:
Sclerosis of bone.
Calcification of oval window.
Fluid behind the membrane.
Clinical tests of hearing:
Finger friction test: rubbing the thumb and finger close to the ear.
Watch test: by clicking watch.
Speech (voice) test: conversation voice, distance of 6 meters.
Tuning fork tests.
Tuning fork tests:
Traditionally 512Hz (الاهتزاز أطول لهذا التردد)
Rinne and Weber (they were both German)
Help differentiate between conductive and sensorineual hearing loss
Rinne`s test:
Compare Air and Bone conduction in the same ear
Normal subject = AC > BC (Rinne +ve)
CHL = BC > AC (Rinne -ve)
SNHL = AC > BC (Rinne +ve) and often the BC is not heard.
False negative Rinne in very severe SNHL.
Weber test:
In normal subjects the sound is heard in the midline or in both ears equally.
In CHL the sound is heard in the affected ear (absence of environmental noise), i.e.; lateralized toward the affected ear
In SNHL the sound is heard in the non-affected ears.
Assessment of Balance ( Labyrinthine function)
Cranial nerves examination
=================================================================2- The Nose:
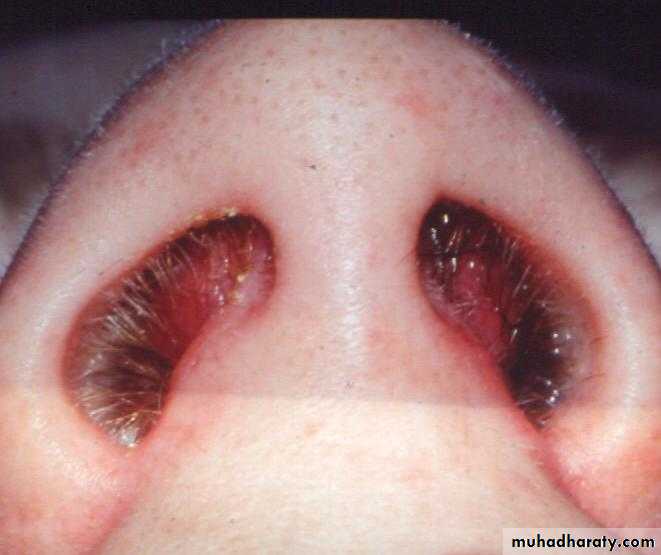
Symptoms of the nose:Discharge (rhinorrhea).
Epistaxis.
Obstruction or block causes of nasal obstruction:
Vestibule: big boil.
Nasal cavity: turbinate hypertrophy, septal deviation, sinusitis, polyp.
Post-nasal space: tumor, adenoid hypertrophy (it is the most common cause of nasal obstruction in children)
Nasal fetor:
Unilateral offensive nasal discharge in children foreign body.
Unilateral offensive nasal discharge in adult rhinolith, tumor, chronic infection.
Examination of the nose:
Introduce yourselfAny hyponasal speech (rhinolalia clausa )?
Position the patient
Head-mirror or headlight?
Inspect the external nose
Compare nose to rest of face
Size
Skin
Swelling, bruising, ulcers
Rhinophyma:
Due to untreated rosacea (heavy alcohol aggravate it)
Treatment: carbon dioxide laser or complete excision with skin graft)
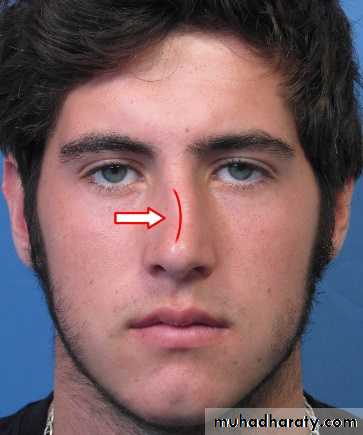
Shape
Banana nose=deviated nose trauma, septal deviation.
High arched nose=roman nose=prominent nose Congenital, Trauma.
Saddle nose HOT SALT (septal haematoma _operation_trauma_syphilis_septal abscess_leprosy_TB)
Prominent nose
Prominent nose
Saddle nose
Saddle nose
Deviated nose
Deviated nose
Rhinophyma
Rhinophyma
Ulcer
Ulcer
Examine the nasal tip, vestibule, and assess the nasal airwaysNasal tip elevation of nasal tip to see the vestibule.
Nostrils and air flow
Mist test For airway patency
Mist Test
Mist Test
Elevation of nasal tip
Elevation of nasal tip
Septal hematoma
Septal hematoma
Palpation and Percussion
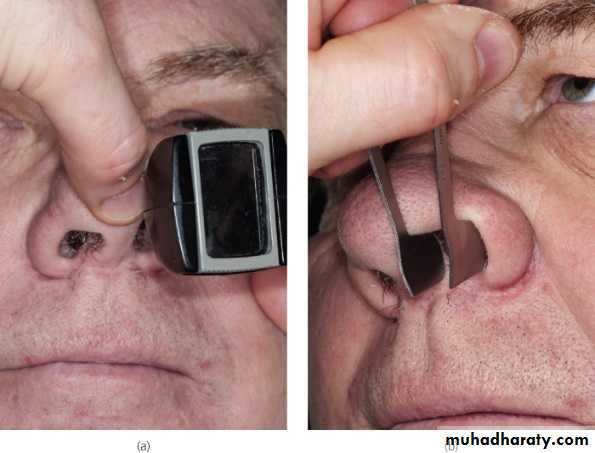
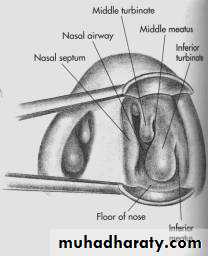
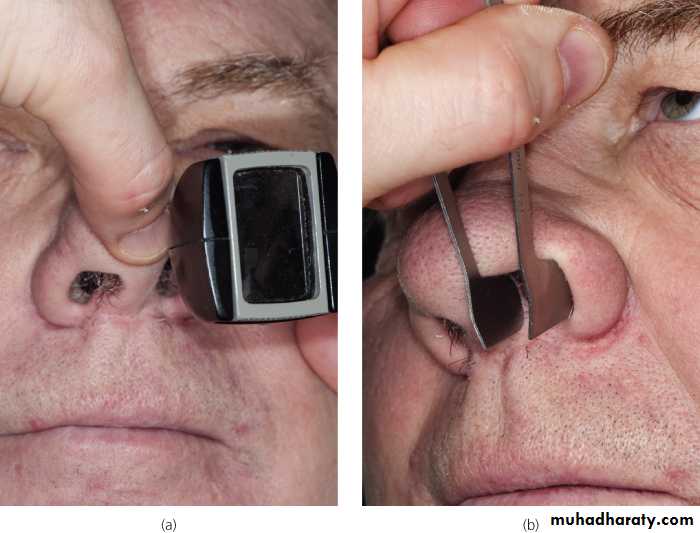
Anterior rhinoscopy:
Thudichum’s speculum, Killian speculum, otoscope?Obvious lesions
Mucosa
Septum
Turbinates (and osteomeatal complex)
Thudichum’s nasal speculum
Used to examine the nasal cavity.
See septum, floor of nose, middle and inferior turbinate, middle meatus.
Polyp
Post nasal space examination:With mirror ( nasopharyngeal mirror) (also use tongue depressor)
Rigid endoscope
Flexible endoscope
=================================================================
3- The Throat:Symptoms of the throat:
Horsiness (don’t horsiness of the voice, but only horsiness).
Sore throat.
Dysphagia and odynophagia.
Cough.
Strider.
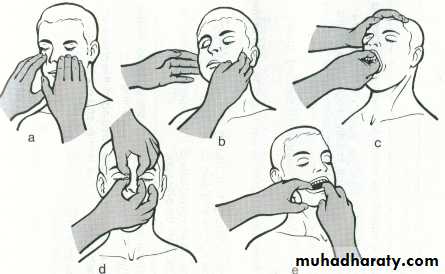
Examination of the throat:
Introduce yourselfPosition the patient:
Headlamp, mirror or other light source
Seated in chair with space to examine from all sides
Assess speech:
Stridor
Hoarseness
Any other dysphonia
Oral examination
Lips, perioral lesions
1 or 2 tongue depressors
Inspect tongue, buccal mucosa and oropharynx
Salivary duct orifaces
Say ‘Ahhh’ (movement of soft palate) // Say 'Eeee' (movement of vocal cords)
Finger examination of floor of mouth, cheeks
Tongue depressor
Used for examination of oral cavity and oropharynx
Can use with nasopharyngeal mirror r to examine posterior nasal space.
Tongue depressor
Used for examination of oral cavity and oropharynxCan use with nasopharyngeal mirror r to examine posterior nasal space.
Peri-oral eczema
Peri-oral eczema
Herpes labialis
Herpes labialis
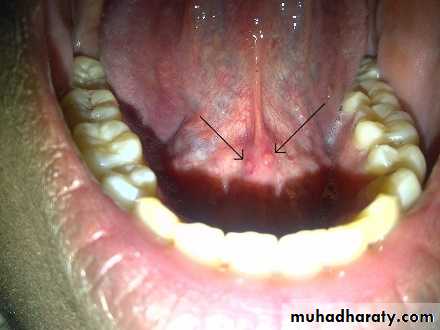
The orifice of sublingual duct of Brtholine
The orifice of sublingual duct of Brtholine
Angular stomatitis:
Iron d. anemia
Vit. B. deficiency
Bacterial
Fungal
Contact dermatitis
Angular stomatitis:
Iron d. anemiaVit. B. deficiency
Bacterial
Fungal
Contact dermatitis
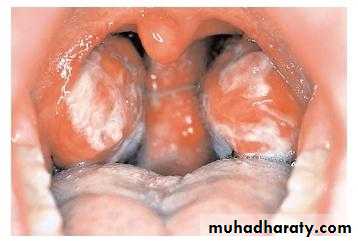
Acute follicular tonsilitis
Acute follicular tonsilitis
Antrochoanal polyp
Antrochoanal polyp
Parotid gland orifice
Using gauze to dry the area and watching the flow by pressing above Stenson’s duct is a good indicator of salivary flow.
Parotid gland orifice
Using gauze to dry the area and watching the flow by pressing above Stenson’s duct is a good indicator of salivary flow.Membranous tonsilitis
DDx:
Diphtheria
Fungi
IMN
Vincent angina
Mention 2 Ix:
WBC count
throat swab
Membranous tonsilitis
DDx:Diphtheria
Fungi
IMN
Vincent angina
Mention 2 Ix:
WBC count
throat swab
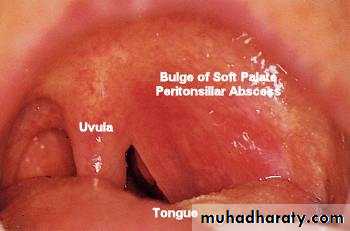
Peritonsillar abscess
Peritonsillar abscess
Post-tonsillectomy
Post-tonsillectomy
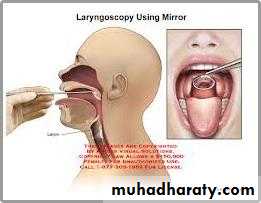
Indirect laryngoscopy
With mirror or nasendoscope
Can assess the base of the tongue, vallecula, Epiglottis, false and true vocal cords.
Look for abnormality in the mucosa ( e.g. congestion , mass, vocal cord nodule>>>)
Check vocal cord mobility by asking the patient to say (EEE)
The mirror is warmed before examination to avoid fogging
Examination of neck
Head and neck cancers metastasise to neck nodes and to the lungs
Tonsillar infections are the commonest cause of enlarged lymph nodes
Skin Skin lesions, Ulceration, Scars and wounds, Stoma, Obvious large masses.
Swallow Larynx should rise, a goitre may rise, too.
Examine from behind Let patient know what you are doing, Tender areas, Gentle, One side at a time.
Lymph nodes in the anterior and posterior triangle
Thyroid gland
Laryngeal skeleton
Position of trachea