
1
Fifth stage
Pediatric
Lec-2
.د
فار
س
الصواف
16/11/2015
Respiratory
Acute bronchitis
Very common in neonate.
Commonly viral, rarely bacteria.
Preceded by upper respiratory tract infection.
Followed by dry cough.
Older children may experience chest pain exacerbating by coughing.
Investigation
No need
CXR may be normal or show peri-bronchial thickening.
Treatment
No need for hospital admission.
Supportive measure:
1. Humidification (steam inhaler)
2. Rest
3. Change position
4. Expectorant not helpful
5. Antibiotic not indicated
6. Cough suppressant not helpful.
2
Pneumonias
Definition
Inflammation of the lung parenchyma due to infectious and non-infectious agents.
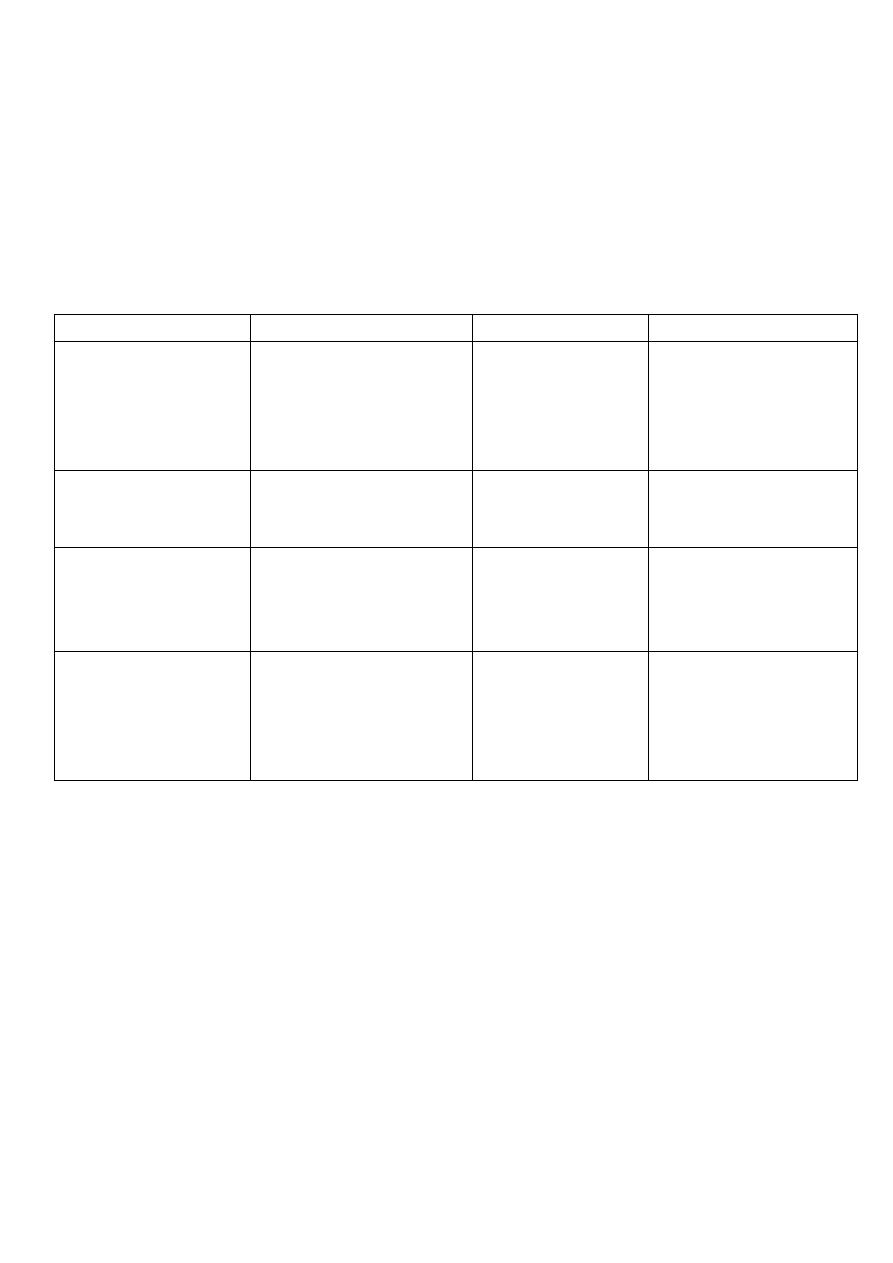
Etiology
Age
Bacteria
Viru
s
other
Neonate
-Group B streptococci*
-G -ve bacilli (E. coli)
-Streptococcus
pneumoniae
-H.influnzae
-Chlamydia
trachomatis
3 months
-Streptococcus
pneumoniae
-H.influnzae
-RSV *
-Rhinovirus
-Influenza
virus
-Chlamydia
trachomatis
4months - 4 years
-Streptococcus
pneumoniae
-Group A streptococci
Staph. aureus
RSV*
>5 years
-Streptococcus*
pneumoniae
-H.influnzae
-Mycoplasma
pneumoniae
-Influenza v.
-RSV
-Legionella
pnemophilia
-Chlamydia
pneumophilia
* most common m.o in that age group
N.B :
in neonate, there is no viral infection only bacteria. The neonate catch group B
streptococci from birth canal during delivery and G -ve bacilli from mother rectum.
Virus cause bronchopneumonia (generalized)
Bacteria cause lobar pneumonia (localized)

3
Symptoms and signs
1. Respiratory distress
2. Dyspnoea
3. Tachypnea
4. Grunting (pathognomonic)
5. flaring nostrils
6.
intercostal
recession, sub costal retraction
7. tachycardia
8. fatigability
9. fever, malaise, vomiting, delirium, anxiety
10.lower lobe pneumonia may cause abdominal pain
11.upper lobe pneumonia may cause CNS manifestation (
Neck
stiffness).
physical finding:
1. diminished breath sound
2. scattered rhonchi & crackles
3. lobar consolidation
4. dull to percussion
5. increase diminished breath sound.
6. bronchial breathing
7. palpable liver due to downward displacement of the diaphragm or due to CHF
8. signs of CHF
9. abdominal distension (paralytic ileus)
4
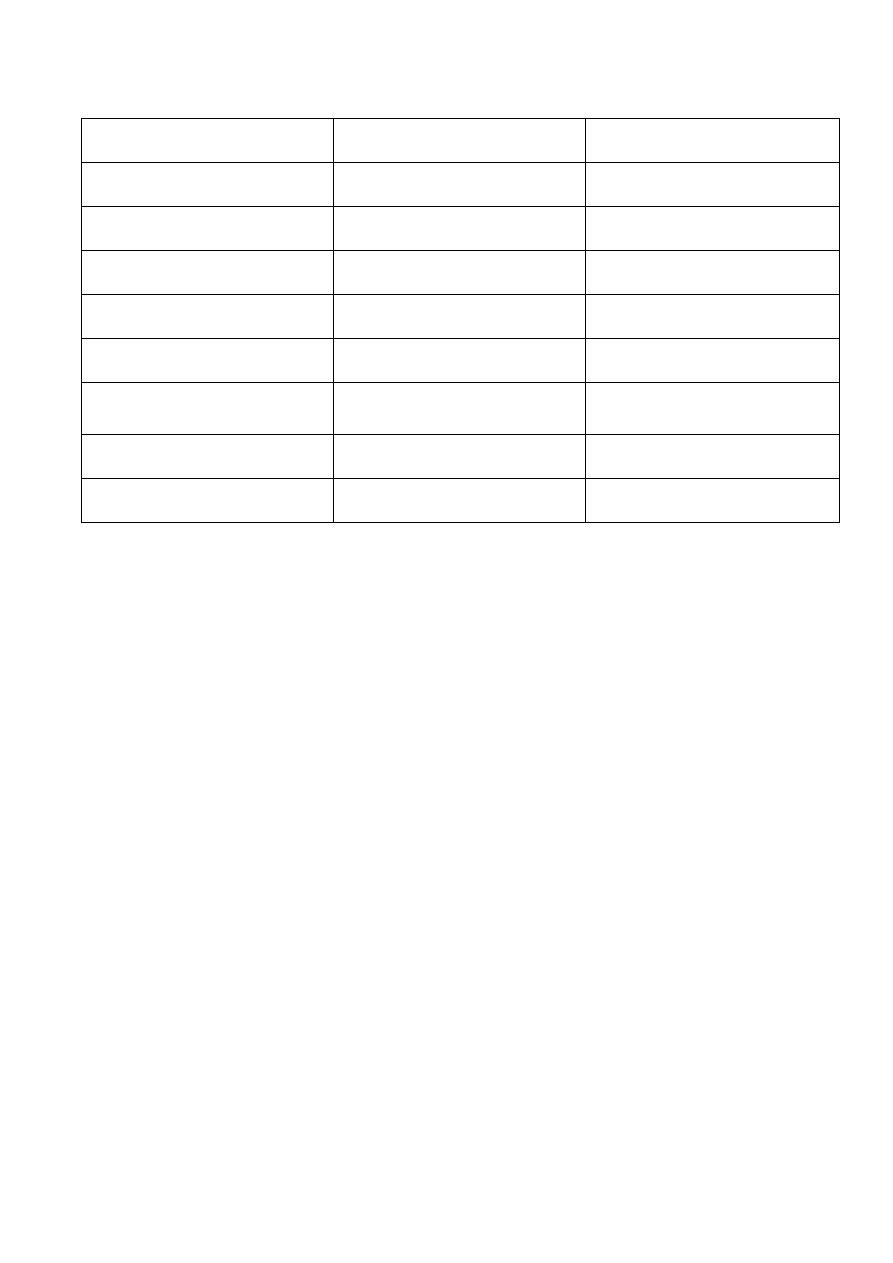
Differentiate between Bacterial and viral pneumonia
Bacteria
Virus
Fever
High
Slight
Respiratory symptoms
Severe
Less severe
Neurological symptoms
Present
Absent
Pleuritic chest pain
Present
Absent
WBC
Leukocytosis (PMN)
Lymphocytosis or normal
Onset
Abrupt and not preceded
by URTI
Take few days and
preceded by URTI
Chest
Lobar consolidation
Bilateral infiltration
Diagnosis
Culture
isolation
Investigation
From age and clinical history
Sputum for culture and serology not beneficial
Blood culture positive only in 10% in bacterial pneumonia
CXR may show lobar consolidation in bacterial pneumonia and bilateral infiltrate in
viral pneumonia.
Staph pneumonia
Very severe, stormy, fatal course .
Respiratory distress, dyspnoea, bacteraemia, septicaemia toxic and may collapse.
High fever
affect young babies & may cause Broncho pulmonary fistula
CXR: characteristic may show pleural effusion, empyema, pneumatocele.
Treatment
Admission to hospital
Oxygen
Hydration: IV fluid

5
Parenteral antibiotic (Anti-staph.) give 2 antibiotic Flucloxacillin 100 mg/kg in two
divided dose Or Clindamycin + Vancomycin.
Mycoplasma pneumonia
Atypical pneumonia
extra-pulmonary feature: fever, malaise, headache
poor response to Penicillin
-ve culture, need Special culture
need specific investigation (cold agglutinin, PCR, Mycoplasma specific IgG level)
Diffuse bilateral infiltrate
Age>5 years
Treatment
Azithromycin (10-20mg/ Kg) single dose for 7-10 days, fluoroquinolone also effective
clinical improved in 3-6 days
Radiological improvement need 6-8 weeks
Antibiotics should be stopped once clinical improvement occur.
Treatment of pneumonia in general
Mild cases treated at home, give amoxicillin 40-50 mg/kg/day for 7-10 days
indication for Hospital admission for pneumonia
1. Multiple lobe opacity
2. Sickle cell anemia
3. previous cardiac or pulmonary disease
4. No response to oral antibiotic
5. Not compliant parent
6. Baby <6 months
7. Need O2
8. Severe respiratory distress.
9. Toxic
10. Poor oral intake
11.Vomiting
12.Dehydration
13.Immune deficiency

6
Complications
Local spread: to intrathoracic structure (especially in Staph.aurues, Strept.pyogens and
Strept.pneumoniae)
Pleural effusion
Empyema
Pericarditis
Systemic spread: septicaemia
Meningitis
Suppurative arthritis
Osteomyelitis
Slowly resolving pneumonia
Causes
1. Bacteria (resistance)
2. Virus
3. Poor compliance
4. Empyema
5. Noxious M.O (T.B pneumonia)
6. F.B inhalation (bronchoscope)
7. Congenital tracheoesophageal fistula (barium swallow)
8. Cystic fibrosis (sweat chloride test + clubbing of fingers + malabsorption )
9. Immune deficiency
Recurrent pneumonia
More than 2 pneumonia/year or > 3 pneumonia in his life. Causes :
1. Cystic fibrosis.
2. Sickle cell anemia.
3. As above in slowly resolving pneumonia

7
Asthma
Most common chronic disease in children.
Chronic inflammation of lung airway result in episodic attack of airway obstruction
(bronchospasm) due to airway hyper responsiveness due to various immunological &
non-immunological exposure triggers.
Common cause of morbidity.
Further episode worsens the condition.
Trigger
1. Exercises
2. Crying
3. Laughter
4. Hyperventilation
5. Common viral infection
6. Aero inhalant allergen (dust mite,
molds
, indoor allergen)
7. Season allergen (pollens)
8. Environment (tobacco smoking)
9. Air pollution
10.Noxious strong odour
11.Cold dry airs
12.Occupational allergen
13. Drugs (aspirin, B-blocker)
14.Additives
Pathology
Hyper responsiveness result in:
1. spasm (bronchospasm due to smooth muscle contraction ).
2. edema.
3. Excessive mucous secretions
All these lead to air way obstruction.
8
Signs & symptoms
Intermittent dry cough
Dyspnoea
Wheeze (expiratory)
Chest tightness
+ve family history of atopy
Symptoms of asthma worse at night
Physical findings: -
1. Wheeze.
2. Rhonchi, crepitation.
3. Diminished breath sound.
4.
In severe exacerbations,
inspiratory & expiratory wheeze & silent chest.
Differential diagnosis
1. Bronchiolitis due to RSV.
2. Foreign body inhalation
3. GERD
4. Mucociliary clearance disorder: cystic fibrosis & bronchiectasis
5. Vascular ring
6. Tracheomalasia
7. Pulmonary sequestration
8. Interstitial lung disease
9. Heart failure
10.Tracheoesophageal fistula
11.Immune deficiency
12.Anaphylaxis
13. Allergy

9
Diagnosis
1. Clinical
2. CXR: Normal or Hyperinflation, flat diaphragm, narrow mediastinum.
N.B: we do x-ray at first attack to exclude other DDx, unnecessary thereafter
unless suspect complication (atelectasis, pneumothorax, pneumo mediastinum)
3. Pulmonary function test: objective measure to measure the degree of airways
obstruction:
A. spirometry: FEV1/FVC ratio according to age, gender, height, ethnicity.
Usually can do it after 6 years of age.
FEV1/FVS < 60 % .......... Severe obstruction
FEV1/FVS 60_80 % ...... Moderate
FEV1/FVS > 80% ........... Mild
B. Peak expiratory flowmeter (PEF): Simple device, home used, at morning three
attempts & take the highest attempt. Used to show response to bronchodilator
4. Skin prick test: in atopic
5. Complete blood picture: show eosinophilia
6. Sputum eosinophil
7. Level of IgE (RAST) Radio Allegro Sorbent Test.
Treatment
Four keys:
1. Check-up: every 2-4 wks. until control achieved, then 2-3 times per years to
maintain a good control.
2. Eliminate the triggers
3. Pharmacotherapy
4. Education: how to use inhaler, symptoms of disease, side effect of drug .

10
Pharmacotherapy: two type of drugs
1. Long term controller drug
2. Quick reliever rescue drugs
Long term controller drug:
1. Inhaled corticosteroids (ICS) such as beclomethasone, betamethasone & budesonide
dry powder inhaler, spacer, nebulizer, inhaler, rinse the month with water to prevent
candidiasis or dysphonia.
2. Long acting inhaled B-against (LABA) salmeterol, formoterol.
3. Theophylline: bronchodilator & anti-inflammatory. Not used nowadays because of
narrow therapeutic range and many drug interactions.
4. NSAID: promoline, nedocromil very effective for exercise 2-4 time daily
5. Leukotriene modifier: montelukast, zafirlukast
6. Anti IgE monoclonal antibodies: omalizumab
Quick reliever rescue drugs
1. Short acting B-agonist (SABA) salbutamol, terbutaline.
Side effect: tachycardia, tremor, hypokalaemia.
2. Short course systemic steroid: 1-2mg/kg/day orally for 3-10 days.
3. Anticholinergic: ipratropium bromide with SABA .
Step up -step down classification of asthma
1. Mild intermittent ≤ 2day/weeks
≤2 bad night /months
Rx: only reliever on need (best SABA).
2. Mild persistent: >2day symptom/week
>2 bad night /month
Rx: 1 controlled at regular base (low dose ICS) + reliever on need
11
3. Moderate persistent:
daily symptoms,
> 1bad night/week
Rx: 2 controllers (best low or moderate doseICS +LABA) + reliever on need
4. Sever persistent: continuous symptoms
frequent bad night
Rx : 3 controls ICS + LABA + short course oral systemic steroid
Three comorbid conditions make asthma difficult to control
1. Rhinitis
2. Sinusitis
also called indirect triggers
3. GERD
Prognosis
35% recurrent wheeze and cough in the pre-school age.
2/3 of patient grow out of it in pre-teen ages.
1/3 continue as asthma in later childhood and adult.
Prophylaxis
Encourage breast feeding
Discourage smocking
Good hygiene, active life style
Rural area better than urban area

12
Complications
Atelectasis
Respiratory failure
Pneumothorax & pneumomediastinum
Collapse
Death
Severe asthma exacerbation (SAE) Status asthmaticus
Risk factor
1. Male gender
2. Air pollution, tobacco smoking
3. Younger uneducated mother
4. Poverty
5. Crowding
6. Previous severe attack
7. Previous rapidly occurring attacks
8. Chronic wheezier
9. Poor compliance to drugs
10.Low birth wt.
11.Allergens
Symptoms and Signs
Dyspnea, tachypnea, use of accessory muscle of respirations, silent chest, inability to
talk, excessive sweating, tripod position, pulsus paradoxus , poor air exchange,
cyanosis ,respiratory muscle fatigue & respiratory failure & may die .
PSO2 <90 %

13
Treatment
Admission to hospital (ICU)
Oxygen (oxygen saturation should be above 92%)
Hydration
CXR if there is complication (atelectasis, pneumothorax)
Complete electrolyte may be abnormal.
SABA nebulizer every 20 min
Systemic steroid
Monitoring
Ipratropium bromide, terbutaline, adrenaline 0.1 mg /kg
Aminophylline infusion 5mg/kg loading dose IV slowly for 30 min then 1mg/kg/hr
infusion
Mg sulphate, Hilux
Mechanical ventilation
Discharge after 2-3 days but continue short rescue drugs and short course systemic
steroid for 2-3 days.
