
1
Fifth stage
Pediatric
Lec-1
د. بسام
30/11/2015
NEONATAL JAUNDICE
Hyperbilirubinemia is common, affects 60% of term babies and 80% of preterm babies and,
in most cases it is benign problem in neonates.
It is either:
1. Indirect (unconjugated) which is the most common and it is either
Physiologic (benign non pathologic).
Hemolytic (pathologic), it carry a risk of CNS damage known as kernicterus when
bilirubin exceed certain limit.
Breast Milk jaundice (benign).
2. Direct hyperbilirubinemia: this is when the direct bilirubin is more than 2mg/dl, no risk
of kernicterus, caused by:
Common causes:-
- biliary atresia.
- idiopathic neonatal hepatitis.
Less common causes as:-
cystic fibrosis, galactosemia, Wilson disease, tyrosinemia, fructosemia, alpha 1 antitrypsin
deficiency, TORCH infection, choledochal cyst, total parenteral nutrition.
Physiologic Jaundice:
To say it is physiologic jaundice, the following criteria must be found:
1. It starts during the 2
nd
or the 3
rd
day of life.
2. The peak of jaundice in full term baby is at the 2
nd
to 4
th
day
3. of life, while in preterm baby it peaks at 5
th
to 7
th
day of life.
4. Decline to below 2mg/dl by the 7
th
day of life in term & by
5. the 10
th
day in preterm baby.
6. Jaundice disappear completely within 2 weeks of life.
2
7. The raise in the bilirubin is less than 5 mg/dl/24 hours.
8. The peak level of bilirubin is less than 12mg/dl, although 10% of these babies having
higher bilirubin level as in babies of diabetic mothers, prematurity, polycythemia, vit k
administration, male sex, Down syndrome, cephalhematoma, cutaneous bruising,
oxytocin during labor, dehydration and calory deprivation, delay bowel motion.
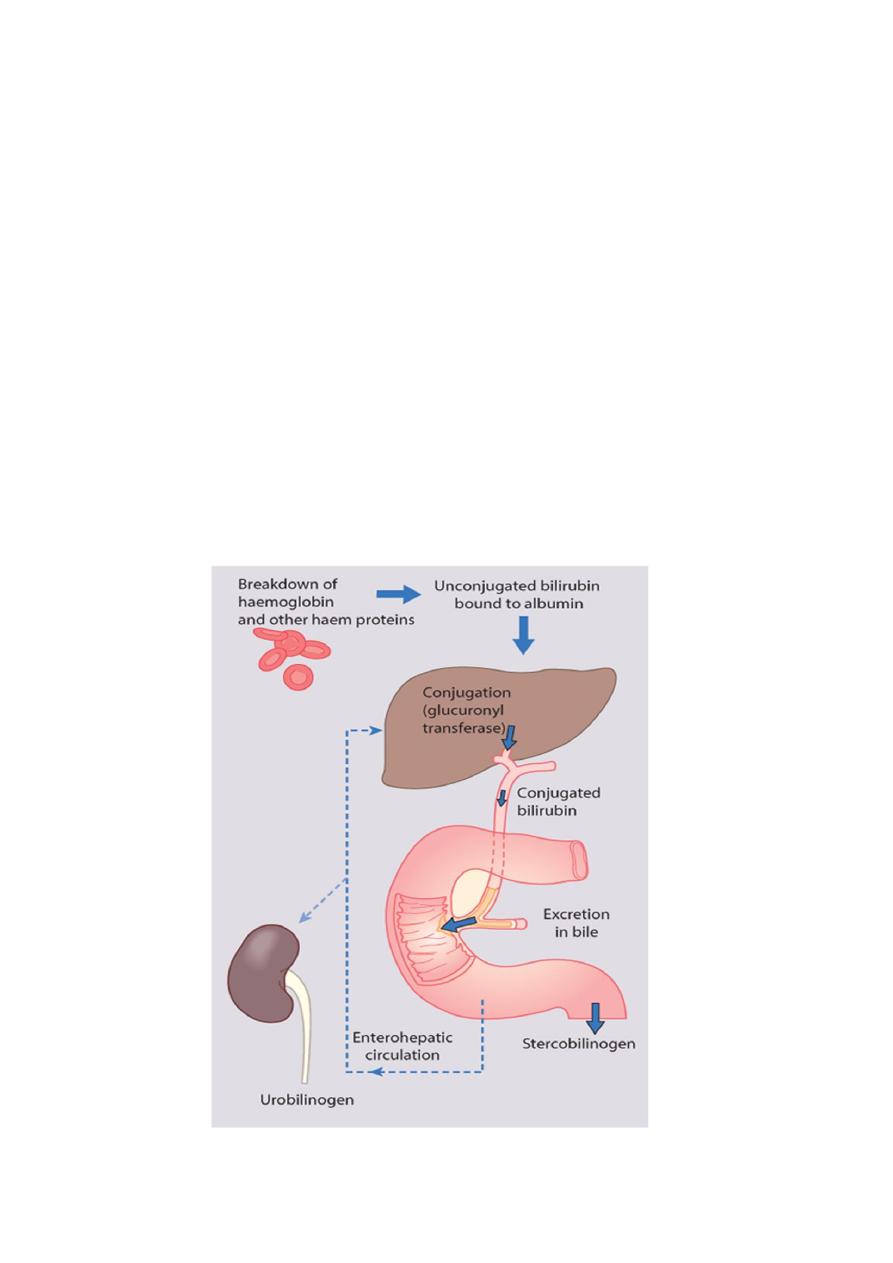
Why physiologic jaundice occur:
There is marked physiological release of haemoglobin from the breakdown of red cells
because of the high Hb concentration at birth.
The red cell life span of newborn infants (70-90 days) is markedly shorter than that of
adults (120 days) .
Hepatic bilirubin metabolism is slow during the first few days of life.

3
Pathologic Jaundice (hemolytic)
The criteria of this jaundice are:
It starts during the 1
st
24 hr of life.
The rise in serum bilirubin is more than 5mg/dl/24 hr.
The serum bilirubin is higher than 12mg/dl.
Jaundice persist for more than 2 weeks.
May be positive family history of hemolytic disease, pallor, hepatosplenomegaly, signs
of kernecterus.
Lab. findings may show evidence of Rh or ABO incompatability low hemoglobin,
reticulocytosis, and may be a positive Coombs test.
Breast Milk Jaundice:
An estimated of 2% of breast fed term infants develops an elevated level of uncongugated
bilirubin after the7th day of life reaching maximal concentrations as high as 10-30mg per dl
during the 2nd & 3rd week.If breast feeding continued the hyperbilirubinemia gradually
decreases & then may persist for 3-10 weeks at lower levels. These infants show no signs
of illness and kernicterus is very rarely reported.
Kernicterus
Is a neurologic syndrome results from a deposition of unconjugated bilirubin in the brain
cells particularly in the basal ganglia, hippocumpus,and cerebellum. Lipid soluble indirect
bilirubin may cross the blood brain barrier and enter the brain by diffusion.
Clinical Features
signs & symptoms of kernicterus usually appear in the 1
st
week of life although kernicterus
can occur at any time during the neonatal period.
The early signs may be subtle & indistinguishable from sepsis, asphyxia, hypoglycemia or
intracranial hemorrhage which are:-
Lethargy, poor feeding & absence Moro reflex are common initial signs.
In advanced cases there is irritability, increased muscle tone causing the baby to lie with
an arched back (opisthotonos),twitching, seizures, high pitched cry, bulging fontanel,
coma with the infant stiffly extended his arms with inward rotation.
4
Many infants who progress to these severe neurologic signs die, the survivors are
usually seriously damaged and may appear to recover & after 2-3 months they show few
abnormalities.
Later in the 1st year of life opisthotonos, muscular rigidity, irregular movements, and
convulsions tends to recur.
In the 2nd year opisthotonos & convulsions abate,but irregular involuntary movements,
muscular rigidity or in some infants hypotonia increase gradually.
By 3 years of age the syndrome is completely developed consisting of bilateral
chorioathetosis with involuntary muscle spasm,seizures, mental deficiency, dysarthric
speech, high frequency hearing loss,squints, and defective upward movement of the
eyes.
In mildly affected infants, the syndrome may be characterized only by mild to moderate
neuromuscular incoordination, partial deafness, or minimal brain dysfunction.
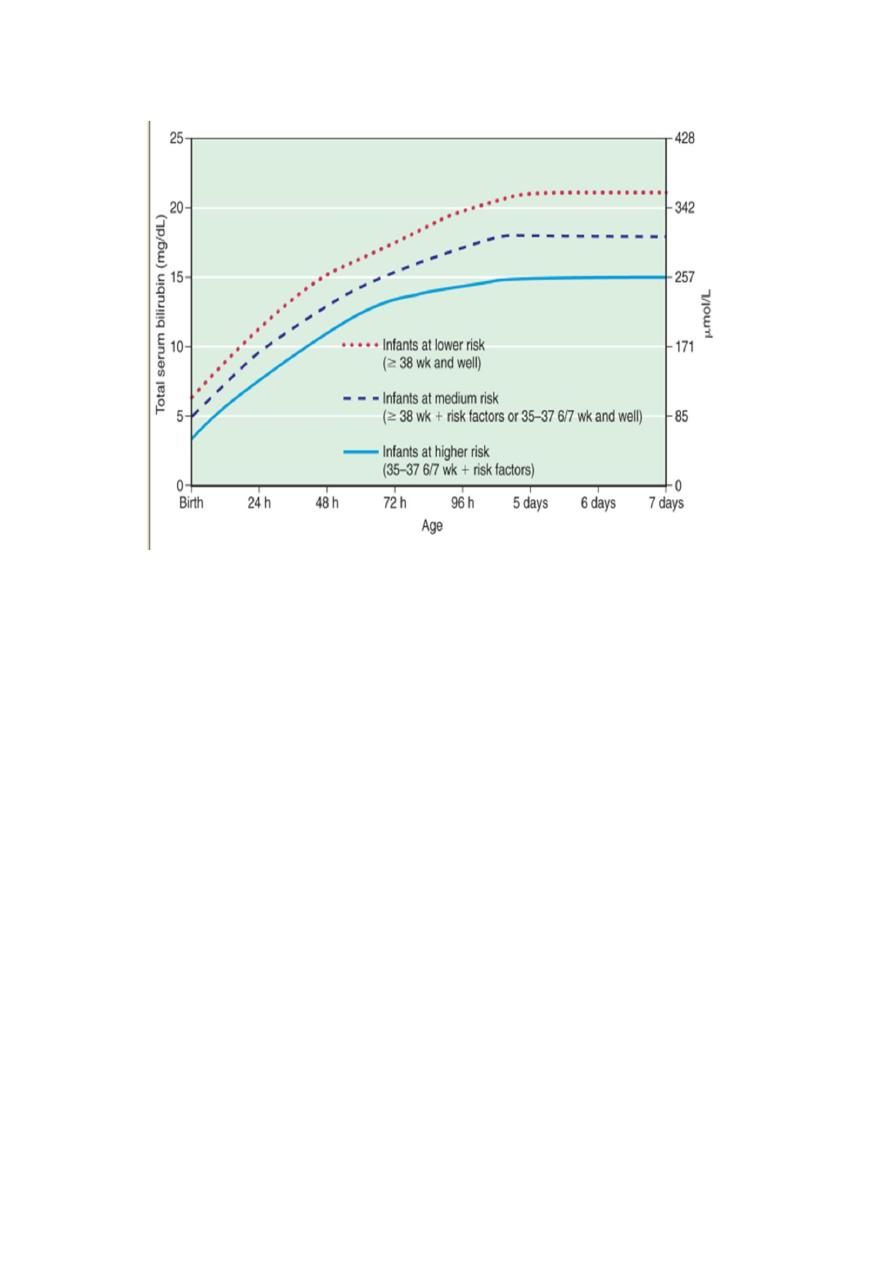
Treatment of hyperbilirubinemia:
1. Either there is no need for treatment especially if there is no hemolysis, full term baby,
healthy active & the jaundice is not deep with criteria of physiologic jaundice.
2. Phototherapy
3. Exchange transfusion.
4. Intravenous immunoglobulin: for ABO and Rh incompatability
5.
in a dose of 0.5-1 grams/kg/dose repeated every 12 hours
.
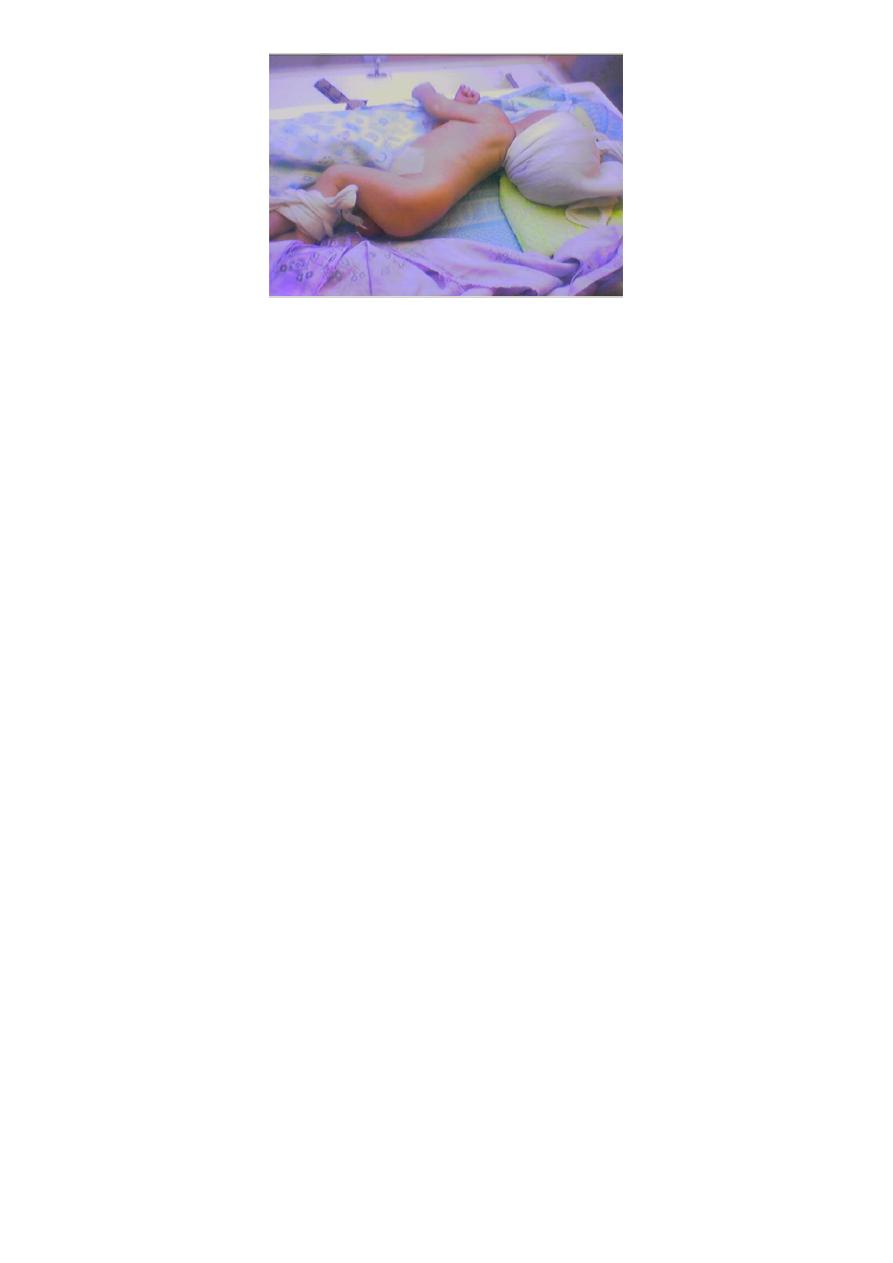
Phototherapy
Clinical jaundice & indirect hyperbilirubinemia reduced on exposure to a high intensity of
light in a wave length of 420-470nm. Bilirubin in the skin absorbs light energy which by
photoisomerization converts the toxic unconjugated bilirubin to a product which can be
excreted in bile without the need for conjugation, also phototherapy converts uncojugated
bilirubin to lumirubin which excreted in urine by the kidney.
5
Prophylactic phototherapy in VLBW infants may prevents hyperbilirubinemia & may reduce
the need for exchange transfusion.
Monitoring should continue for at least 24 hrs after cessation of phototherapy in infants
with hemolytic disease that unexpected rise of bilirubin sometimes occur & require further
treatment.
Skin color cannot be relied on for evaluation of the effectiveness of phototherapy that the
skin of babies exposed to light may appear without jaundice in the presence of marked
hyperbilirubinemia.
The infants eyes should be closed & adequately covered to prevent exposure to light. Body
temp also should be monitored.
Complications of phototherapy
1. loose stool.
2. Erythematous macular rashes.
3. Overheating.
4. Dehydration.
5. Bronze baby syndrome when there is direct
hyperbilirubinemia.
6. Eye injury and nasal obstruction.
6
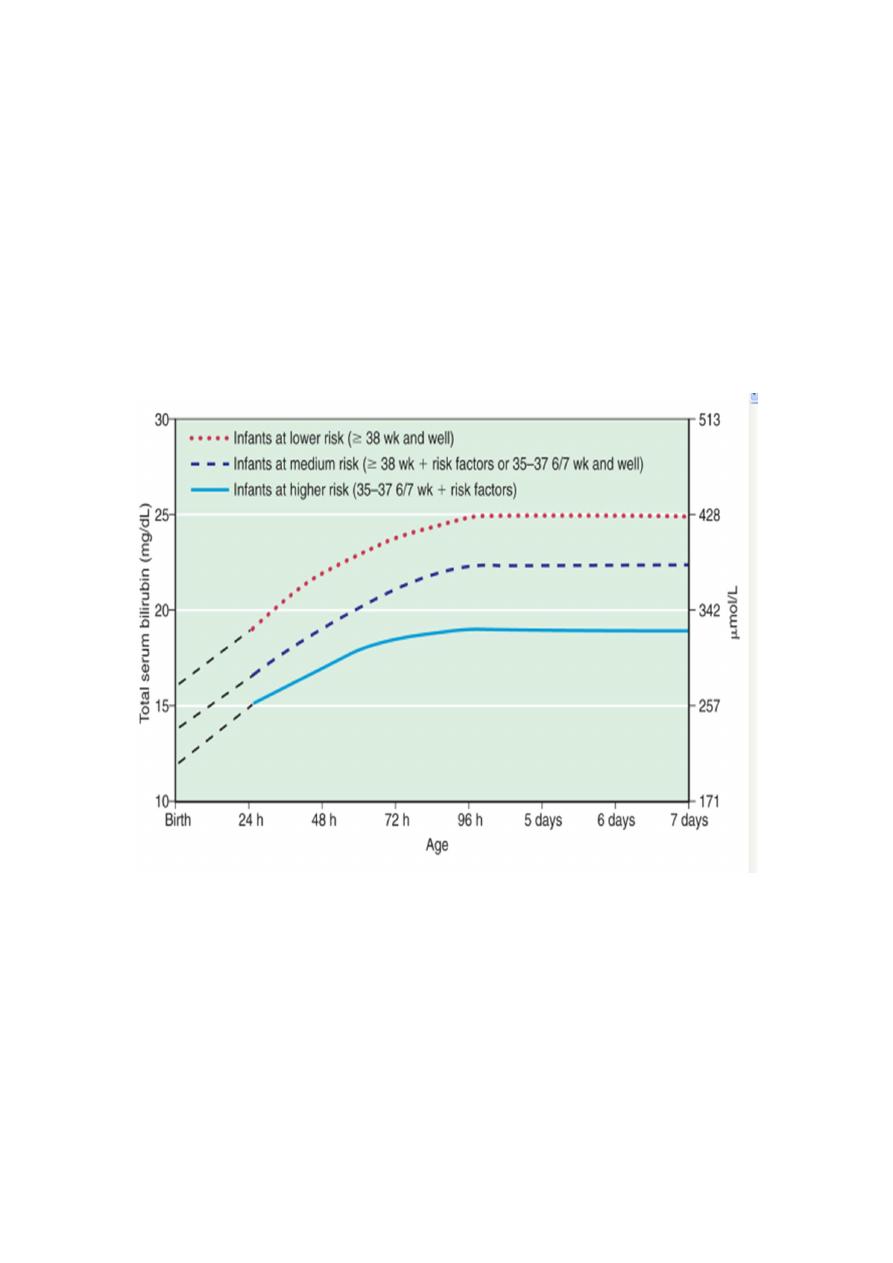
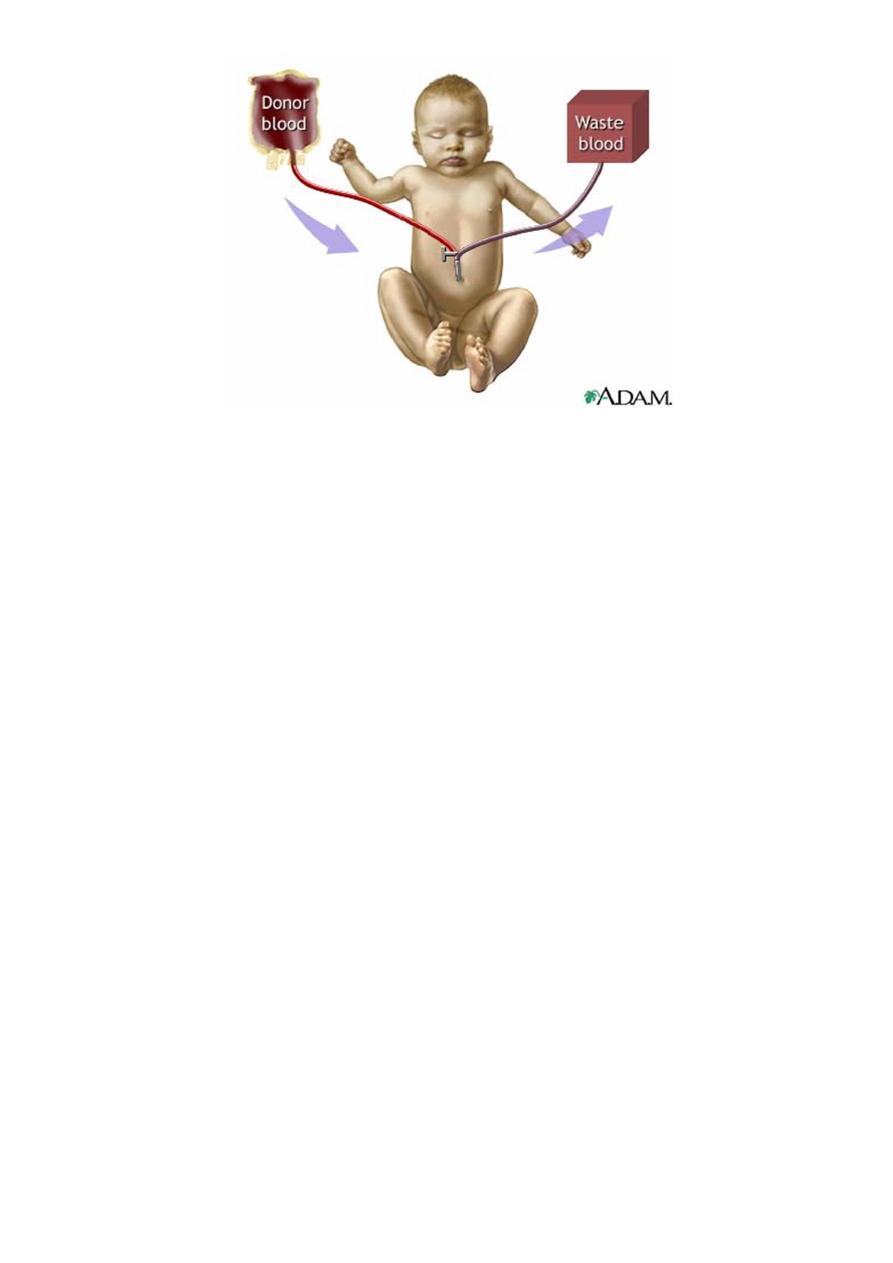
Exchange transfusion
It is used to remove bilirubin from the circulation when phototherapy fails, is especially
used for infants with increased in bilirubin production from immune mediated hemolysis
because the circulating antibodies and the sensitized RBCs are also removed.
Functions of exchange transfusion:
1. Clear excess bilirubin.
2. Correct the anemia without causing circulatory overload.
3. Removes maternal antibodies.
4. Removes sensitized RBCs.
Procedure of Exchange Transfusion:
Volume of blood needed is double the blood volume of the baby, so it will be the boy
weight multiplied by 170ml (as the blood volume of the newborn is 85ml/Kg body weight.
The procedure involves placement of a central catheter into the umbilical vein, then
alternatively remove then give 15-20ml of blood in a repeated way until completing the
required amount of blood.
After the procedure serum bilirubin falls to approximately 1/2 of the pre exchange value,
then increase to approximately 2/3 of that level as the extravascular & vascular bilirubin
reequilibirate.
7
Complications of Exchange Transfusion
1. blood born infection.
2. thrombocytopenia.
3. metabolic acidosis.
4. volume overload.
5. coagulopathy.
6. graft versus host disease.
7. necrotizing enterocolitis.
8. portal vein thrombosis and portal hypertension years later.
9. electrolytes disturbance.
10. hypoglycemia, hypocalcemia.
11. cardiac arrhythmias.
12. sudden death.
