Fifth stage
Ophthalmology
Lec-2
.د
نزار
30/11/2016
The lacrimal system
INTRODUCTION
Disorders of the lacrimal system are common and may produce
chronic symptoms with a significant morbidity. The lacrimal glands
normally produce about 1.2
i
μl of tears per minute. Some are lost
via evaporation.
The remainder are drained via the naso-lacrimal system.
The tear film is reformed with every blink.
Abnormalities are found in:
•
00
tear composition;
•
00
the drainage of tear
ABNORMALITIES IN COMPOSITION
If certain components of the tear film are deficient or there is a
disorder of eyelid apposition then there can be a disorder of ocular
wetting.
Aqueous insufficiency
—dry eye (Fig. 6.1)
A deficiency of lacrimal secretion occurs with age and results
in keratoconjunctivitis sicca (KCS) or dry eyes.
When this deficiency is associated with a dry mouth and
dryness of other mucous membranes the condition is called
primary
Sjögren’s syndrome (an auto-immune
exocrinopathy).
When KCS is associated with an auto-immune connective
tissue disorder the
condition is called secondary Sjögren’s
syndrome. Rheumatoid arthritis is the commonest of these
associated disorders.
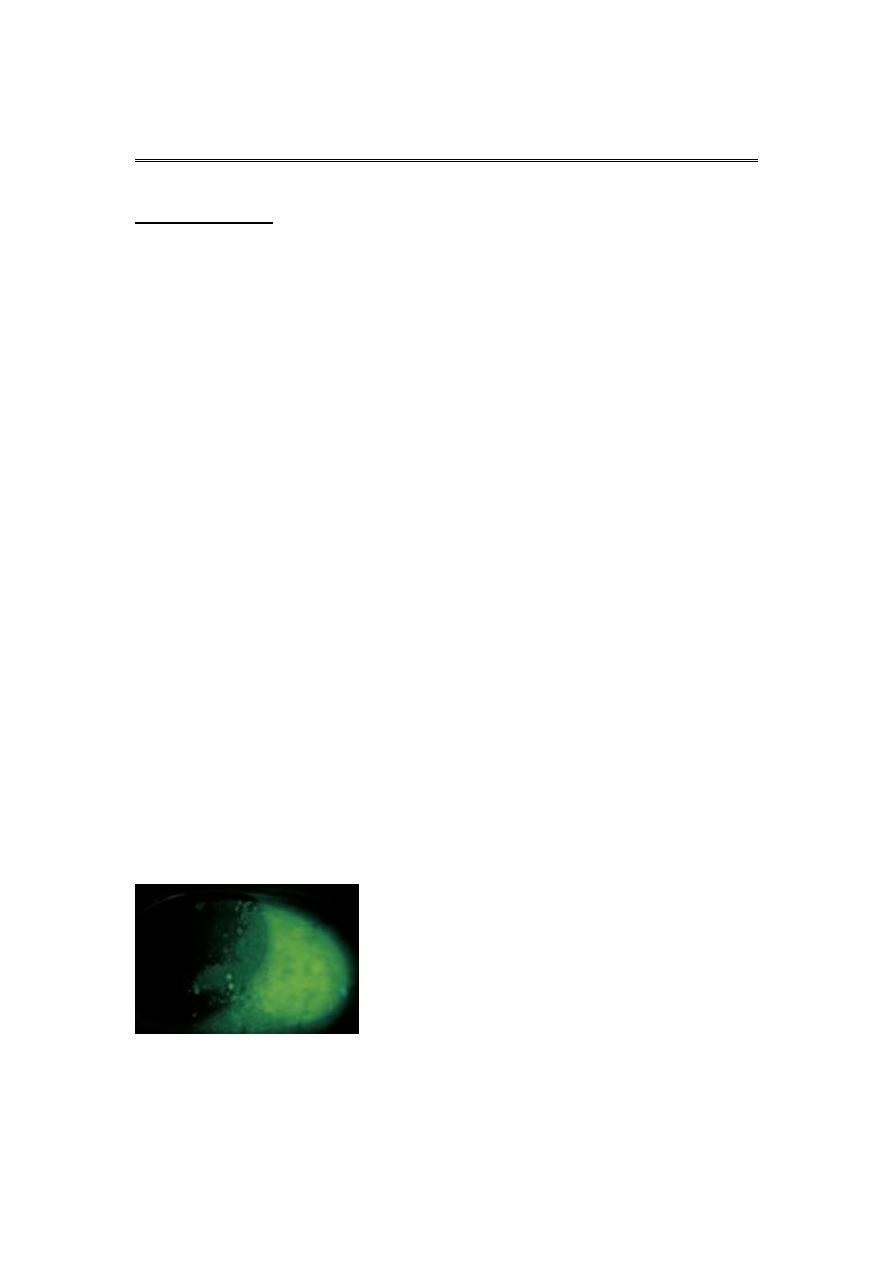
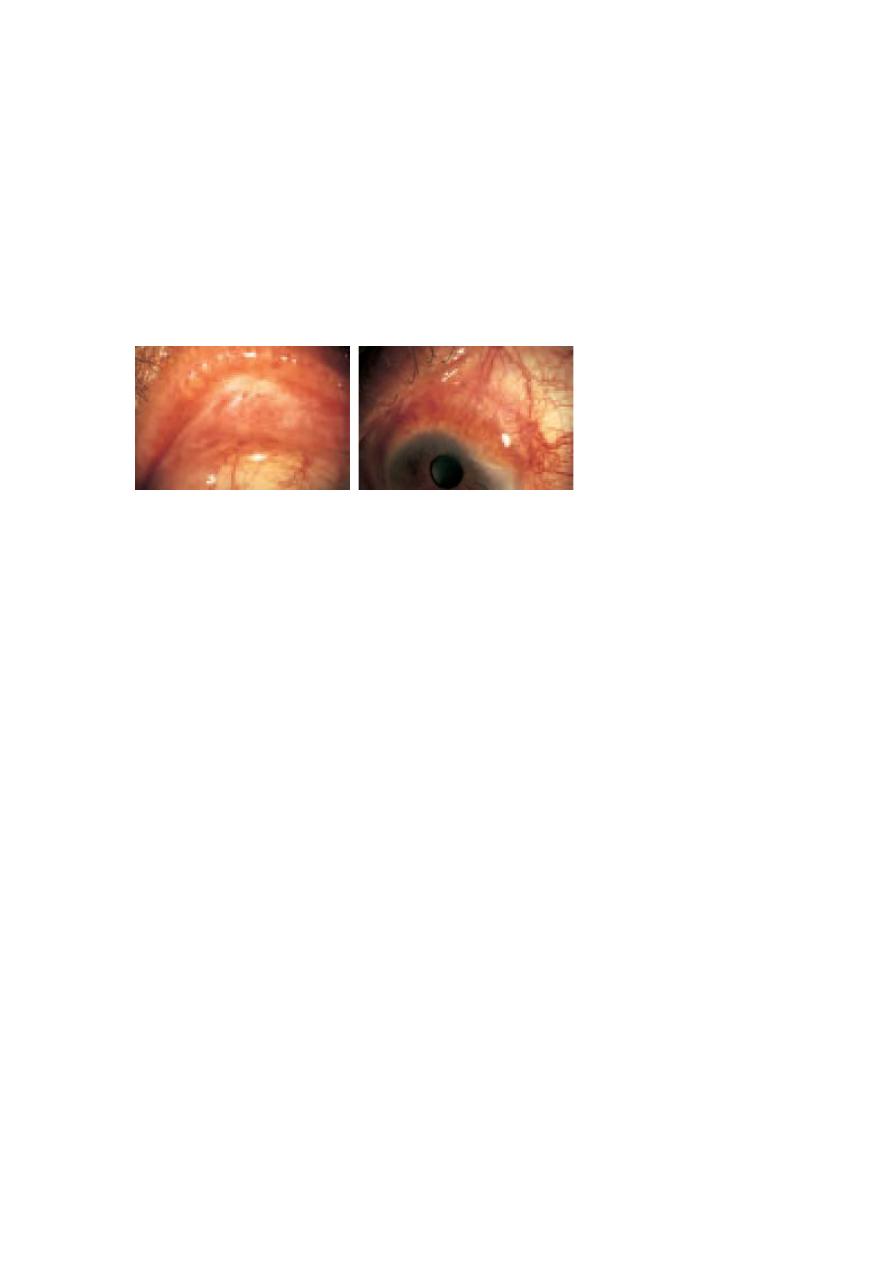
Fig. 6.1
0
Fluorescein staining of
cornea and conjunctiva in a severe
dry eye.

SYMPTOMS
Patients have non-specific symptoms of grittiness, burning,
photophobia, heaviness of the lids and ocular fatigue.
These symptoms are worse in the evening because the eyes dry during
the day. In more severe cases visual acuity may be reduced by corneal
damage
.
SIGNS
In mild cases there are few obvious signs. Staining of the eye with
fluorescein will show small dots of fluorescence (punctate staining) over
the exposed corneal and conjunctival surface. In severe cases tags of
abnormal mucus may attach to the corneal surface (filamentary
keratitis) causing pain due to tugging on these filaments during blinking.
TREATMENT
Supplementation of the tears with tear substitutes helps to reduce
symptoms and a humid environment around the eyes can be created
with shielded spectacles.
In severe cases it may be necessary to occlude the punta with plugs, or
more permanently with surgery, to conserve the tears.
PROGNOSIS
Mild disease usually responds to artificial tears. Severe disease such as
that in rheumatoid Sjögren
’s can be very difficult to treat
.
Inadequate mucus production
Destruction of the goblet cells occurs in most forms of dry eye, but
particularly in cicatricial conjunctival disorders such as erythema
multiforme (Stevens
–Johnson’s syndrome).
In this there is an acute episode of inflammation causing macular
‘target’ lesions on the skin and discharging lesions on the eye, mouth
and vulva. In the eye this causes conjunctival shrinkage with adhesions
forming between the globe and the conjunctiva
(symblepharon).
There may be both an aqueous and mucin deficiency and
problems due to lid
deformity and trichiasis. Chemical burns of the eye,
particularly by alkalis and
trachoma (chronic inflammation of the conjunctiva
caused by a type of
chlamydial infection may also have
a similar end result.
The symptoms are similar to those seen with an aqueous deficiency.
Examination may reveal scarred, abnormal conjunctiva and areas of
fluorescein staining.

Treatment requires the application of artificial lubricants.
Vitamin A deficiency (xerophthalmia) is a condition causing childhood
blindness on a worldwide scale.
It is associated with generalized malnutrition in countries such as India and
Pakistan. Goblet cells are lost from the conjunctiva and the ocular surface
becomes keratinized (xerosis).
An aqueous deficiency may also occur.
The characteristic corneal melting and perforation which occurs in this
condition (keratomalacia) may be prevented by early treatment with vitamin A.
Abnormal or inadequate production of meibomian oil
Absence of the oil layer causes tear film instability, associated with
blepharitis (see p. 52).
Malposition of the eyelid margins
If the lid is not apposed to the eye (ectropion), or there is insufficient
closure of the eyes (e.g. in a seventh nerve palsy or if the eye protrudes
(proptosis) as in dysthyroid eye disease) the preocular tear film will not
form adequately.
Correction of the lid deformity is the best answer to theproblem.
If the defect is temporary, artificial tears and lubricants can be applied.
If lid closure is inadequate a temporary ptosis can be induced with
a local injection of botulinum toxin into the levator muscle.
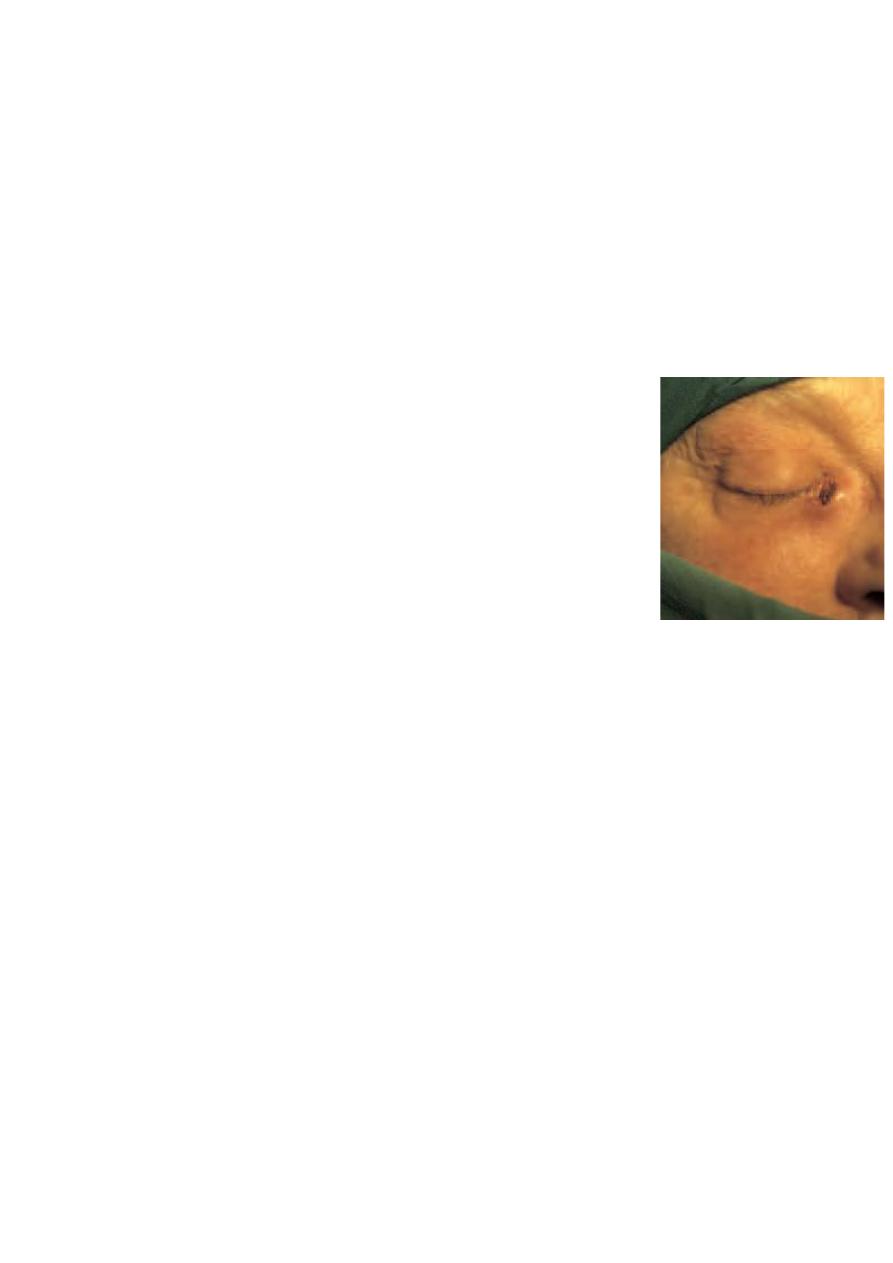
A more permanentresult can be obtained by suturing together part of the
apposed margins of the upper and lower lids (e.g. lateral tarsorrhaphy; Fig.
6.2).
DISORDERS OF TEAR DRAINAGE
When tear production exceeds the capacity of the drainage system,
excess tears overflow onto the cheeks. It may be caused by:
•
00
irritation of the ocular surface, e.g. by a corneal foreign body, infection
or blepharitis;
•
00
occlusion of any part of the drainage system (when the tearing is
termed epiphora).

Obstruction of tear drainage (infant)
The naso-lacrimal system develops as a solid cord which subsequently
canalizes and is patent just before term.
Congenital obstruction of theduct is common.
The distal end of the naso-lacrimal duct may remain imperforate,
causing a watering eye.
If the canaliculi also become partly obstructed the non-draining pool of
tears in the sac may become infected and accumulate as a mucocoele
or cause dacrocystitis.
Diagnostically the discharge may be expressed from the puncta by
pressure over the lacrimal sac.
The conjunctiva, however, is not inflamed.
Most obstructionsresolve spontaneously in the first year of life.
If epiphora persists beyondthis time, patency can be achieved by
passing a probe via the punctum through the naso-lacrimal duct to
perforate the occluding membrane(probing).
A general anaesthetic is required.
Obstruction of tear drainage (adult)
The tear drainage system may become blocked at any point, although the
most common site is the naso-lacrimal duct. Causes include infection or
direct trauma to the naso-lacrimal system.
HISTORY
The patient complains of a watering eye sometimes associated with
stickiness. The eye is white.
Symptoms may be worse in the wind or in cold weather.There may be a
history of previous trauma or infection
.
SIGNS
A stenosed punctum may be apparent on slit lamp examination.
Epiphora is unusual if one punctum continues to drain.
Acquired obstruction
beyond the punctum is diagnosed by syringing the naso-lacrimal system with
saline using a fine cannula inserted into a canaliculus.
A patent systemis indicated when the patient tastes the saline as it reaches
the pharynx.
If there is an obstruction of the naso-lacrimal duct then fluid will regurgitate
from the non-canulated punctum.
The exact location of the obstruction can be confirmed by injecting a radio-
opaque dye into the naso-lacrimal system (dacrocystogram); X-rays are then
used to follow the passage of the dye through the system.
TREATMENT
It is important to exclude other ocular disease that may contribute to
watering such as blepharitis .
Repair of the occluded naso-lacrimal duct requires surgery to connect the mucosal
surface of the lacrimal sac to thenasal mucosa by removing the intervening bone
(dacryocystorrhinostomy or DCR (Fig. 6.3)).
The operation can be performed through an incision on the side of the nose but it
may also be performed endoscopically through the nasal passages thus avoiding a
scar on the face.
INFECTIONS OF THE NASO-LACRIMAL SYSTEM
Closed obstruction of the drainage system predisposes to
infection
of the sac (dacryocystitis; Fig. 6.4).
The organism involved is usually Staphylococcus.
Patients present with a painful swelling on the medial side of the
orbit, which is the enlarged, infected sac
Treatment is with systemic antibiotics. A mucocoele results from
a collection of mucus in an obstructed sac, it is not infected. In
either case a DCR may be necessary to prevent recurrence
CHAPTER 7
Conjunctiva, cornea
and sclera
INTRODUCTION
Disorders of the conjunctiva and cornea are a common cause of symptoms.
The ocular surface is regularly exposed to the external environment
and subject to trauma, infection and allergic reactions which account for
the majority of diseases in these tissues.
Degenerative and structural abnormalities account for a minority of problems.
Symptoms
Patients may complain of the following:
1
00
Pain and irritation. Conjunctivitis is seldom associated with anything
more than mild discomfort. Pain signifies something more serious such as
corneal injury or infection. This symptom helps differentiate conjunctivitis
from corneal disease.
2
00
Redness. In conjunctivitis the entire conjunctival surface including that
covering the tarsal plates is involved. If the redness is localized to the
limbus ciliary flush the following should be considered:
(a)
0
keratitis (an inflammation of the cornea);
(b)
0
uveitis;
(c)
0
acute glaucoma.
3
00
Discharge. Purulent discharge suggests a bacterial conjunctivitis. Viral
conjunctivitis is associated mainly with a watery discharge.
4
00
Visual loss. This occurs only when the central cornea is affected. Loss
of vision is thus an important symptom requiring urgent action.
5
00
Patients with corneal disease may also complain of photophobia.
Signs
The following features may be seen in conjunctival disease:
•
00
Papillae.These are raised lesions on the upper tarsal conjunctiva, about
1
i
mm in diameter with a central vascular core.They are non-specific signs
of chronic inflammation.They result from fibrous septa between the
conjunctiva and subconjunctiva which allow only the intervening tissue to
swell with inflammatory infiltrate.
Giant papillae, found in allergic eye disease, are formed by the coalescence
of papillae (see Fig. 7.4).
•
00
Follicles.These are raised, gelatinous, oval lesions about 1
i
mm
in diameter found usually in the lower tarsal conjunctiva and upper tarsal
border, and occasionally at the limbus. Each follicle represents a lymphoid
collection with its own germinal centre. Unlike papillae, the causes of follicles
are more specific (e.g. viral and chlamydial infections).
•
00
Dilation of the conjunctival vasculature (termed
‘injection’).
•
00
Subconjunctival haemorrhage, often bright red in colour because it is
fully oxygenated by the ambient air, through the conjunctiva.
The features of corneal disease are different and include the following:
•
00
Epithelial and stromal oedema may develop causing clouding of the
cornea.
•
00
Cellular infiltrate in the stroma causing focal granular white spots.
•
00
Deposits of cells on the corneal endothelium (termed keratic
precipitates or KPs, usually lymphocytes or macrophages, see p. 92).
•
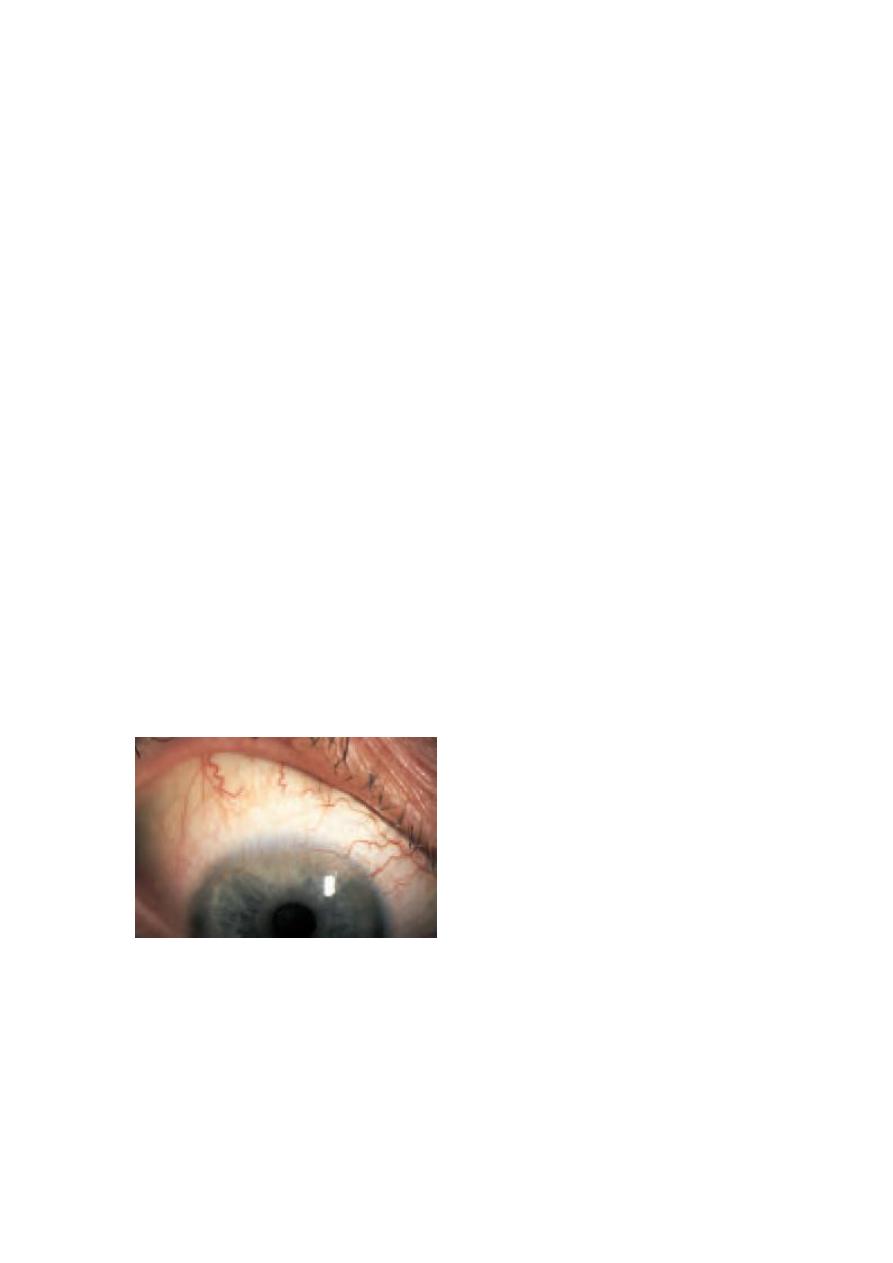
00
Chronic keratitis may stimulate new blood vessels superficially, under
the epithelium (pannus; Fig. 7.2) or deeper in the stroma. Stromal oedema,
which causes swelling and separates the collagen lamellae, facilitates vessel
invasion.
Signs
The following features may be seen in conjunctival disease:
•
00
Papillae.These are raised lesions on the upper tarsal conjunctiva, about
1
i
mm in diameter with a central vascular core.They are non-specific signs
of chronic inflammation.They result from fibrous septa between the
conjunctiva
and subconjunctiva which allow only the intervening tissue to
swell with inflammatory infiltrate. Giant papillae, found in allergic eye
disease, are formed by the coalescence of papillae (see Fig. 7.4).
Fig. 7.2
0
Pannus.
•
0
Epithelial erosions are punctate or more extensive patches of epithelial
loss which are best detected using fluorescein dye and viewed with a blue
light.

CONJUNCTIVA
Inflammatory diseases of the conjunctiva
BACTERIAL0CONJUNCTIVITIS
Patients present with:
•redness of the eye;
•discharge;
•ocular irritation.
The commonest causative organisms are Staphylococcus,
Streptococcus, Pneumococcus and Haemophilus. The condition is
usually self-limiting although a broad spectrum antibiotic eye drop will
hasten resolution.
Conjunctival swabs for culture are indicated if the condition fails to
resolve.
ANTIBIOTICS:
0
Some of the antibiotics available for topical ophthalmic use. Chloramphenicol
is an effective broad spectrum agent, a small risk of bonemarrow aplasia is a moot point.
Ceftazidine
Chloramphenicol
Ciprofloxacin
Fusidic acid
Gentamicin
Neomycin
Ofloxacin
Tetracycline
Ophthalmia neonatorum, which refers to any conjunctivitis that
occurs in the first 28 days of neonatal life, is a notifiable disease. Swabs for
culture are mandatory. It is also important that the cornea is examined to
exclude any ulceration.
The commonest organisms are:
•
00
Bacterial conjunctivitis (usually Gram positive).
•
00
Neisseria gonorrhoea. In severe cases this can cause corneal perforation.
Penicillin given topically and systemically is used to treat the local and
systemic disease respectively.
•
00
Herpes simplex, which can cause corneal scarring.Topical antivirals are
used to treat the condition.
•
00
Chlamydia. This may be responsible for a chronic conjunctivitis and
cause sight-threatening corneal scarring.Topical tetracycline ointment and
systemic erythromycin is used is used to treat the local and systemic
disease respectively.

VIRAL
0
CONJUNCTIVITIS
This is distinguished from bacterial conjunctivitis by:
•
00
a watery and limited purulent discharge;
•
00
the presence of conjunctival follicles and enlarged pre-auricular lymph
nodes;
•
00
there may also be lid oedema and excessive lacrimation.
The conjunctivitis is self-limiting but highly contagious. The commonest
causative agent is adenovirus and to a lesser extent Coxsackie and
picornavirus.
Adenoviruses can also cause a conjunctivitis associated with the formation of
a pseudomembrane across the conjunctiva.
Certain adenovirus serotypes also cause a troublesome punctate keratitis.
Treatment for the conjunctivitis is unnecessary unless there is a secondary
bacterial infection.
Patients must be given hygiene instruction to minimize the spread of infection
(e.g. using separate towels).
Treatment of keratitisis controversial.
The use of topical steroids damps down symptoms and causes corneal
opacities to resolve but rebound inflammation is common when the steroid is
stopped.
CHLAMYDIAL
0
INFECTIONS
Different serotypes of the obligate intracellular organism Chlamydia
trachomatis are responsible for two forms of ocular infections.
Inclusion keratoconjunctivitis
This is a sexually transmitted disease and may take a chronic course (up to
18 months) unless adequately treated. Patients present with a mucopurulent
follicular conjunctivitis and develop a micropannus (superficial
peripheral
corneal vascularization and scarring)
associated with subepithelial scarring. Urethritis or cervicitis is common.
Diagnosis is confirmed by detection of chlamydial antigens, using
immunofluorescence, or by identification of typical inclusion bodies by Giemsa
staining in conjunctival swab or scrape specimens.
Inclusion conjunctivitis is treated with topical and systemic tetracycline.
The patient should be referred to a sexually transmitted diseases
clinic.
Trachoma (Fig. 7.3)
This is the commonest infective cause of blindness in the world although it
is uncommon in developed countries.
The housefly acts as a vector and the disease is encouraged by poor hygiene
and overcrowding in a dry, hot climate. The hallmark of the disease is
subconjunctival fibrosis caused by frequent re-infections associated with the
unhygienic conditions.
Blindness may occur due to corneal scarring from recurrent keratitis and
trichiasis.
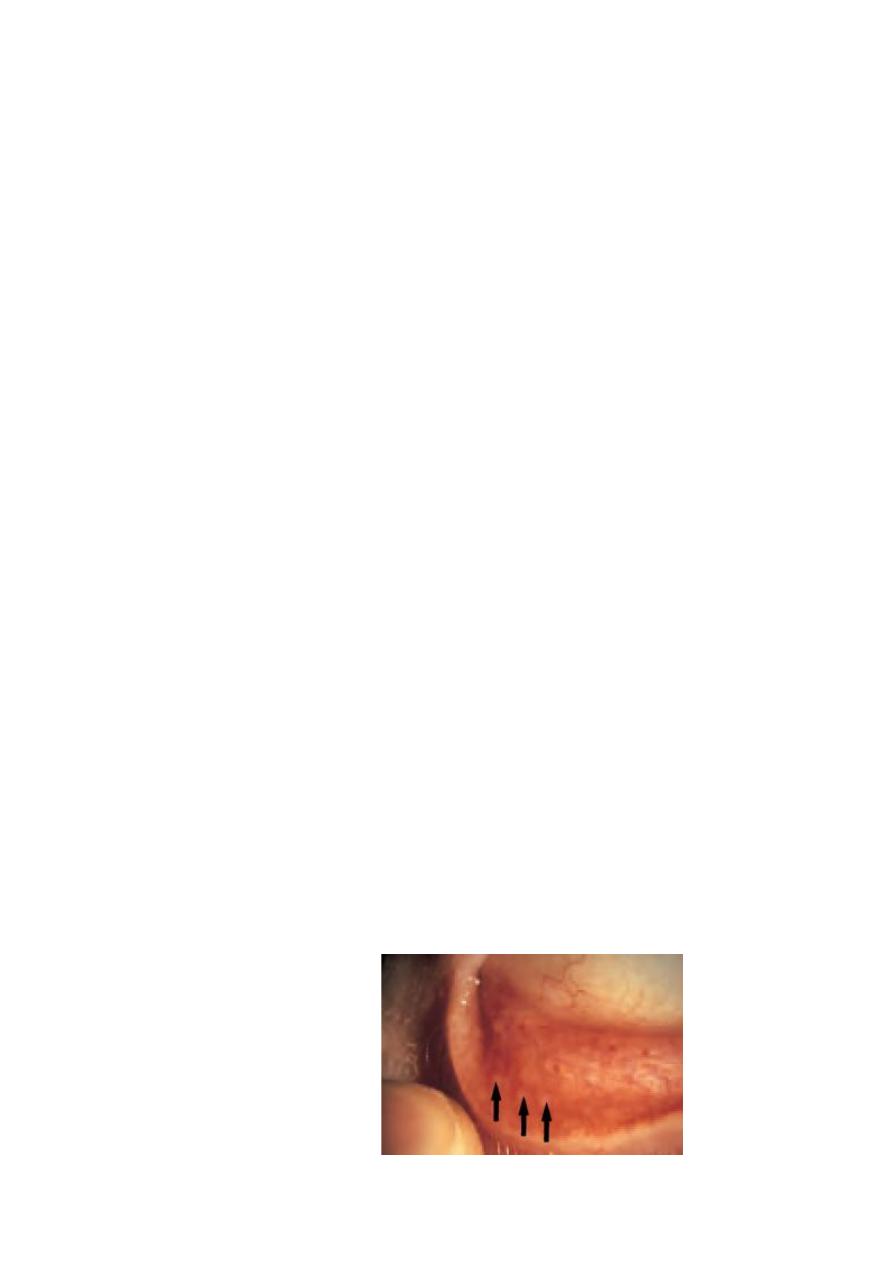
A B
Fig. 7.3
0
Scarring of (a) the upper lid (everted) and (b) the cornea in trachoma.
Trachoma is treated with oral or topical tetracycline or erythromycin.
Azithromycin, an alternative, requires only one application.
Entropion and trichiasis require surgical correction
.
ALLERGIC CONJUNCTIVITIS
This may be divided into acute and chronic forms:
1
00
Acute (hayfever conjunctivitis). This is an acute IgE-mediated reaction
to airborne allergens (usually pollens).
Symptoms and signs include:
(a)
0
itchiness;
(b)
0
conjunctival injection and swelling (chemosis);
(c)
0
lacrimation.
2
00
Vernal conjunctivitis (spring catarrh) is also mediated by IgE.
It often affects male children with a history of atopy. It may be present all year
long.
Symptoms and signs include:
(a)
0
itchiness;
(b)
0
photophobia;
(c)
0
lacrimation;
(d)
0
papillary conjunctivitis on the upper tarsal plate (papillae may
coalesce to form giant cobblestones; Fig. 7.4);
(e)
0
limbal follicles and white spots;
(f )
0
punctate lesions on the corneal epithelium;
(g)
0
an opaque, oval plaque which in severe disease replaces an upper
zone of the corneal epithelium.
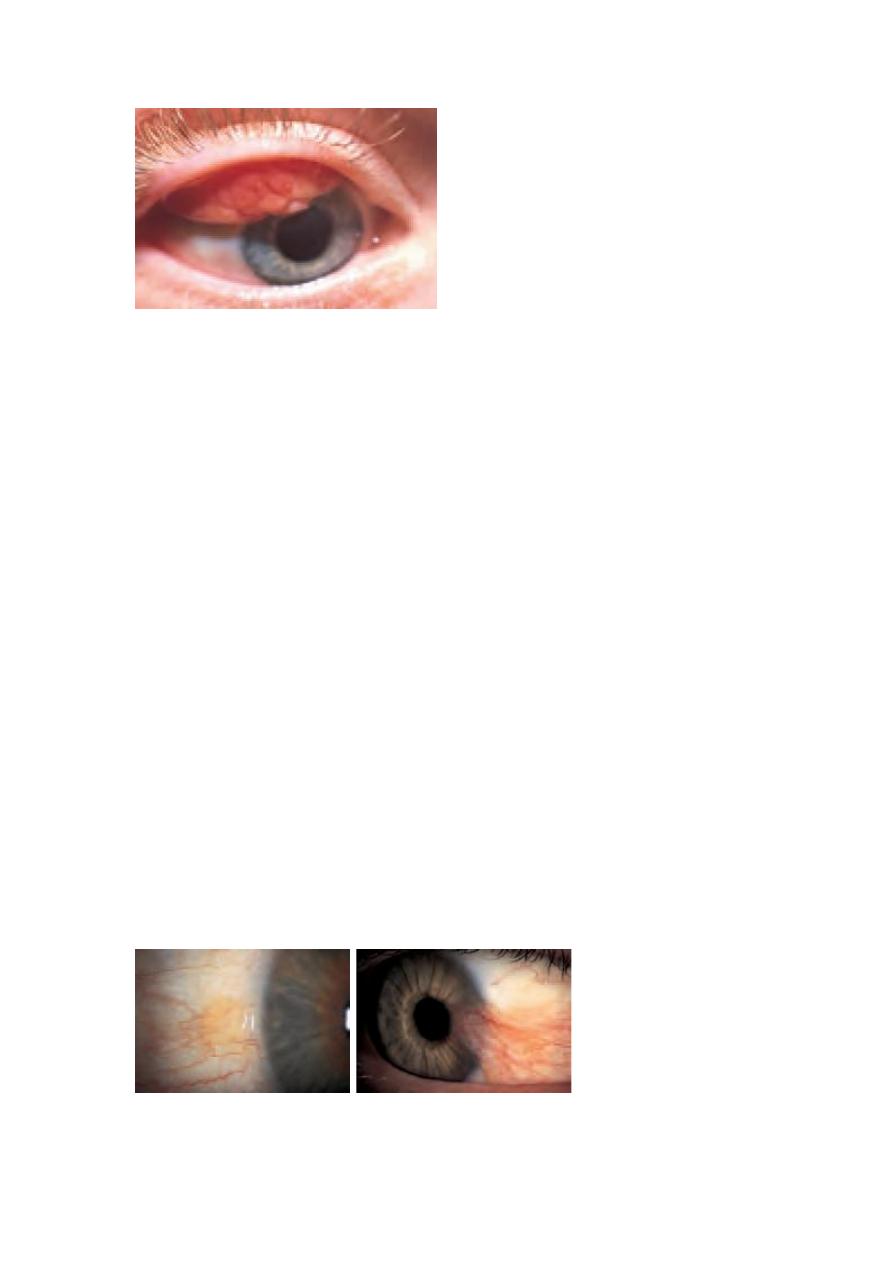
Fig. 7.4
0
The appearance of
giant (cobblestone) papillae
in vernal conjunctivitis
.
Initial therapy is with antihistamines and mast cell stabilizers (e.g.
sodium cromoglycate; nedocromil; lodoxamide).
Topical steroids are required in severe cases but long-term use is avoided if
possible because of the possibility of steroid induced glaucoma or cataract.
Contact lens wearers may develop an allergic reaction to their lenses
or to lens cleaning materials leading to a giant papillary conjunctivitis (GPC)
with a mucoid discharge.
Whilst this may respond to topical treatment with mast cell stabilizers it is
often necessary to stop lens wear for a period or even permanently. Some
patients are unable to continue contact lens wear due to recurrence of the
symptoms.
Conjunctival degenerations
Cysts are common in the conjunctiva. They rarely cause symptoms but if
necessary can be removed.
Pingueculae and pterygia are found on the interpalpebral bulbar conjunctiva.
They are thought to result from excessive exposure to the reflected or
direct ultraviolet component of sunlight. Histologically the collagen
structure is altered.
Pingueculae are yellowish lesions that never impinge on the cornea.
Pterygia are wing shaped and located nasally, with the apex towards
the cornea onto which they progressively extend
(Fig. 7.5). They may cause irritation and, if extensive, may encroach
onto the visual axis.They can be excised but may recur.
7.5
0
The clinical appearance of: (a) a pingueculum; (b) a pterygium

CONJUNCTIVAL
0
TUMOURS
These are rare.They include:
•
00
Squamous cell carcinoma.An irregular raised area of conjunctiva which
may invade the deeper tissues.
•
00
Malignant melanoma. The differential diagnosis from benign pigmented
lesions (for example a naevus) may be difficult.
Review is necessaryto assess whether the lesion is increasing in size. Biopsy,
to achieve a definitive diagnosis, may be required
.
