Genital infections in gynaecology lec.3
Dr. Alyaa2016/2017
Other genital infections:
Human papillomavirus
Epidemiology
• DNA virus, many subtypes.
• Subtypes 6 and 11 cause genital warts (condylomata acuminata).
• 25% of people presenting with warts have other concurrent STIs.
• Commonest viral STI in England.
• Subtypes 16 and 18 associated with CIN and cervical neoplasia.
Symptoms
- Majority asymptomatic.
- Irritation.
- Painless lumps anywhere in the genitoanal area
- Warts may be exophytic, single or multiple, keratinized or not keratinized, broad base or pedunculated, and some are pigmented
Genital warts
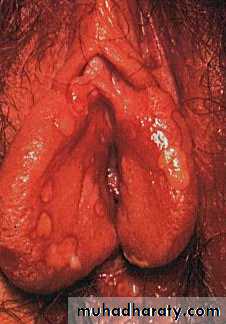
Florid vulval warts
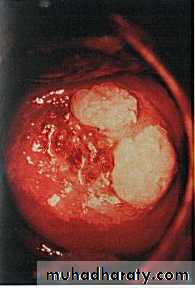
Cervical warts
Diagnosis
- clinical appearance.- Biopsy & Histology of removed wart
- on cervical cytology (smear tests) or colposcopy
Complications
HPV 16 and 18 associated with high-grade CIN and cervical neoplasia.
Smoking and immunosuppression both affect viral clearance thereby increasing the risk.
Treatment for genital warts
Removal of the visible wart. High rate of recurrenceClinic treatment
• Cryotherapy.
• Trichloroacetic acid.
• Electrosurgery/scissors excision/laser.
Home treatment (both contraindicated if pregnancy risk):
• Podophyllotoxin cream or solution: this is self-applied and must be used for about 4–6wks.
• Imiquimod cream: this is also a self-applied immune response modifier. It may need to be used for up to 16wks.
Implications in pregnancy
• Genital warts tend to grow rapidly in pregnancy, but usually regress after delivery.
• Very rarely, babies exposed perinatally may develop laryngeal or genital warts so we should reduce neonatal exposure to the virus & it is not an indication for CS.
Genital ulcer disease
Classification of genital ulcersInfective causes:
- Herpes simplex
- Primary syphilis
- Lymphogranuloma veneri
- Chancroid
- HIV
Non infective causes
- Aphthous ulcer
- Trauma
- Skin disease
- Bahcet syndrome
- Sarcoidosis
Herpes simplex
Epidemiology• DNA virus—herpes simplex type 1 (orolabial/genital) and type 2 (genital only).
• Third most common STI in England in 2010.
Symptoms
Primary HSV infection is usually the most severe Involve vulva, vagina and cervix, and often results in:
• Prodrome (tingling/itching of skin in affected area).
• Flu-like illness +/– inguinal lymphadenopathy.
• Painful vesicles and multiple ulcerations on vulva
• urinary retention.
Primary herpes of vulva
Vulval herpis infection
Recurrent attacks : result from reactivation of latent virus in the dorsal root ganglia, and are normally shorter and less severe. triggered by:
- Stress.
- Sexual intercourse.
- Menstruation
• The spectrum of severity is:
• asymptomatic shedding of the virus.
• Ulcers resembling small abrasions on the vulva.
• Localized clusters of vesicles & ulcers 1-2 cm in diameters
• Wide spread or chronic ulceration, like primary one seen in pregnant women.
• Large atypical chronic ulcers in immunosuppresed patient.
Complications of HSV infection (usually of primary infection)
• Psychological distress• Neurological involvement like aseptic meningitis and transverse myelitis
• Herpes keratitis causing corneal scarring and blindness.
• Sacral radiculopathy—causing urinary retention and constipation.
• Disseminated infection.
Diagnosis
• Usually from appearance of the typical rash.
• PCR testing of vesicular fluid (most sensitive—gold standard).
• Culture of vesicular fluid.
• Serum antibody tests are of no use for diagnosing primary herpes.
Treatment
• Symptomatic relief with simple analgesia, saline bathing, and topical anaesthetic.
• Oral aciclovir (200mg 5x day for 5 days), double dose/length if immunosuppressed.
• Topical aciclovir is not beneficial.
• Condoms/abstinence may reduce transmission rates.
• If recurrent episodes: long term suppression with aciclovir 400 mg twice a day
• Suppressive antiviral treatment—considered if >6 recurrences/year.
Syphilis
Primary syphilis:• First manifestation is painless ulcer (chancre)
• The chancre is in form of shallow punched-out ulcer with well defined edges &smooth shiny floor with rubbery consistency &exudes serous discharge.
• Usually single but can be multiple
• regional lymph nodes enlargement
• common site is cervix
• it arise 3-6 weeks after infection
• resolve spontaneously without treatment after few weeks
• diagnosis done by
- darkfield microscope.
- serological test: specific like (FTA) test, and (TPHA) test or non specific test like (VDRL) test can be used.
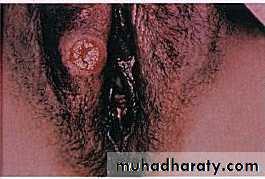
chancre
Secondary syphilis
• occur 6 months after the disappearance of chancre• systemic non itchy maculopapular rash, involving the palms and soles
• florid lesions resembling warts (condylomata lata) mainly in peri-anal area
• mucous patch and linear ulcers (snail track) on the mucosal surfaces
• generalized lymphadenopathy
• alopecia, arthritis and meningitis
• diagnosis by serological test which are positive with VDRL titer 1/32 or more
Syphilis: condylomata lata
Tertiary syphilis
• A firm elastic tumours may occur in skin, mucosa, bones & viscera called gummata• neurosyphilis manifest within 5 years of infection in form of meningovascular syphilis with stroke
• 20% has cardiovascular syphilis like thoracic aortic aneurysm or aortic regurgitation.
Treatment
• Treatment of choice is penicillin like:
- procaine penicillin 1.2 MU daily i.m., for 12 .days or
- Benzathine penicillin 2.4 MU i.m. repeated after 7 days.
• Doxycycline 100 mg twice a day for 14 days
• Erythromycin 500 mg, four times a day for 14 days 5
• There is risk of vertical transmission, neonate at risk should be evaluated and received penicillin injection
• Less severe infection occur late in life manifest as a congenital syphilis including nerve deafness, interstitial keratitis, and- abnormal teeth.
Lymphogranuioma venereum
• It is caused by specific serovars of Chlamydia trachomatis( L1- L3)• Small superficial ulcer slowly increase in size
• Enlarged inguinal lymph nodes which can matted together and discharging pus forming bubo
• Treatment by tetracycline and surgical interference
Chancroid
• Caused by Haemophilus Ducreyi bacilli
• Small, shallow ulcers, multiple and painful with irregular edge
• Localized lymphadenopathy
• Diagnosed via Specialized culture, Isolation of Ducrey’s bacillus on biopsy
• Treatment either by Single oral dose of azithromycin 2 g, Ceftriaxone, or Erythromycin
Granuloma inguinale
• Caused by Klebsiella granulomatosis
• Discrete papules on the skin or vulva which enlarge and form beefy red painful ulcers
• Healing end with fibrosis lead to lymphoedema and elephantiasis
• Diagnosis :Donovan bodies: intracellular inclusions seen in phagocytes or histiocytes.
• Treatment by Erythromycin.
Genital tuberculosis
• Caused by Mycobacterium tuberculosis• clinical features:.1. Amenorrhoea (affects endometrium). 2. Infertility (affects tube). 3. Acute/chronic pelvic pain. 4. Frozen pelvis due to severe multiple adhesions.
• diagnosis: 1. Histological confirmation from endometrium and Fallopian tube. 2. Mantoux test. 3. Heaf test. 4. Chest x-ray.
• Treatment: Rifampicin, Isoniazid, Pyrazinamide. Treatments can last from six to 12 months.