Fifth stage
MedicineLec-11
د.محمد حارث
5/1/2016
LymphomaMost present as tumor Involving lymph nodes or other lymphoid organs such as the spleen. But extra nodal presentation may seen.
Hodgkin’s Lymphoma.
2.Non - Hodkin’s Lymphoma; Non-Hodgkin lymphomas are classified as low- or high-grade tumours on the basis of their proliferation rate.
High-grade tumours divide rapidly, are typically present for a matter of weeks before diagnosis, and may be life-threatening.
• Low-grade tumours divide slowly, may be present for many months before diagnosis, and typically behave in an indolent fashion.
Hodgkin lymphoma
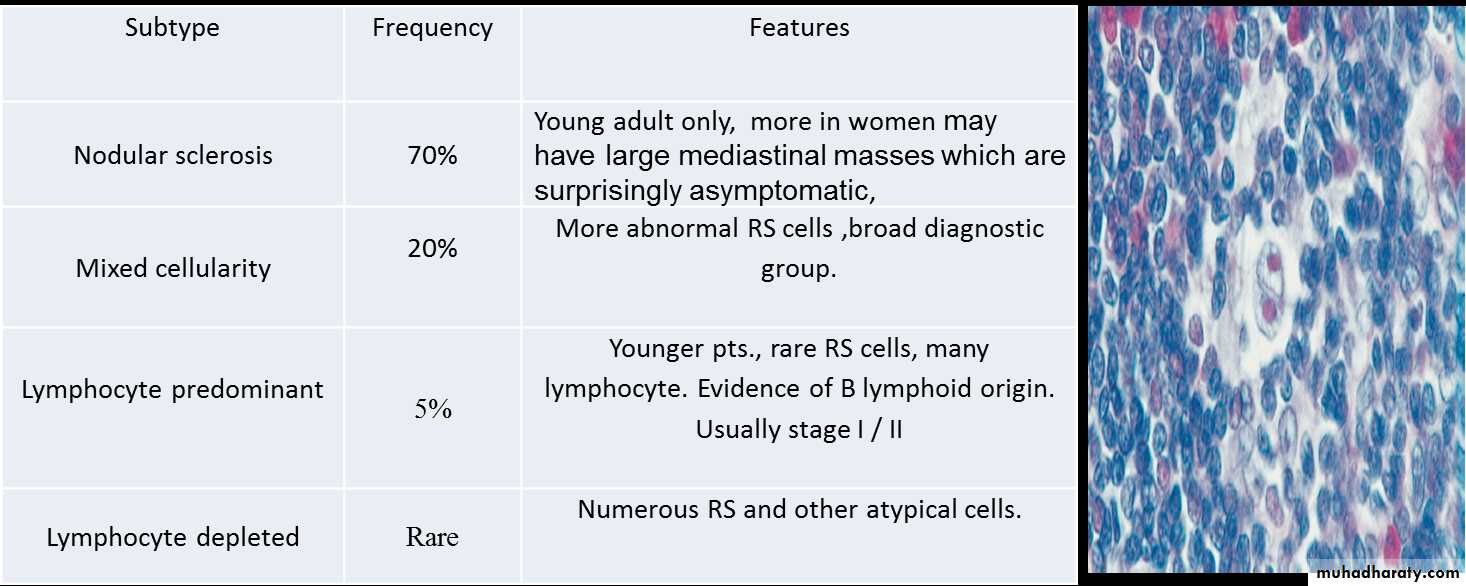
Histological WHO classification1-CLASSICAL HL
2- NODULAR LP HLis now clearly recognized to be indolent NHL 5%
Clinical featuresThere is painless, rubbery lymphadenopathy, usually in the neck or supraclavicular fossae; the lymph nodes may flucuate in size(wax an wan).
Hepatosplenomegaly may be present but does not always indicate disease in those organs.
Spread is contiguous from one node to the next and extranodal disease, such as bone, brain or skin involvement, is rare.
Investigations
FBC may be normal. If a normochromic, normocyticanaemia or lymphopenia is present, this is a poor
prognostic factor. An eosinophilia or a neutrophilia
may be present.
• ESR may be raised.
• Renal function tests are required to ensure function is normal prior to treatment.
• Liver function may be abnormal in the absence of disease or may reflect hepatic infiltration. An obstructive pattern may be caused by nodes at the porta hepatis.
LDH measurements showing raised levels are an adverse prognostic factor.
• Chest X-ray may show a mediastinal mass.
• CT scan of chest, abdomen and pelvis permits staging. Bulky disease (> 10 cm in a single nodemass) is an adverse prognostic feature.
• Lymph node biopsy may be undertaken surgically or by percutaneous needle biopsy under radiological guidance
Management
1-chemotherapy;
The ABVD regimen (doxorubicin,vinblastine,bleomycin and dacarbazine)
*cardiac and pulmonary toxicity, due to doxorubicin and bleomycin respectively.
2-radiotherapy
* The majority of HL patients are now treated with chemotherapy and adjunctive radiotherapy.
* Early-stage patients usually includes additional treatment with radiotherapy to the involved lymph nodes after four courses of ABVD.
* Advanced-stage disease are most commonly managed withchemotherapy alone. 6–8 cycles of ABVD.
* Patients with disease which is resistant to therapy may be considered for autologous HSCT.
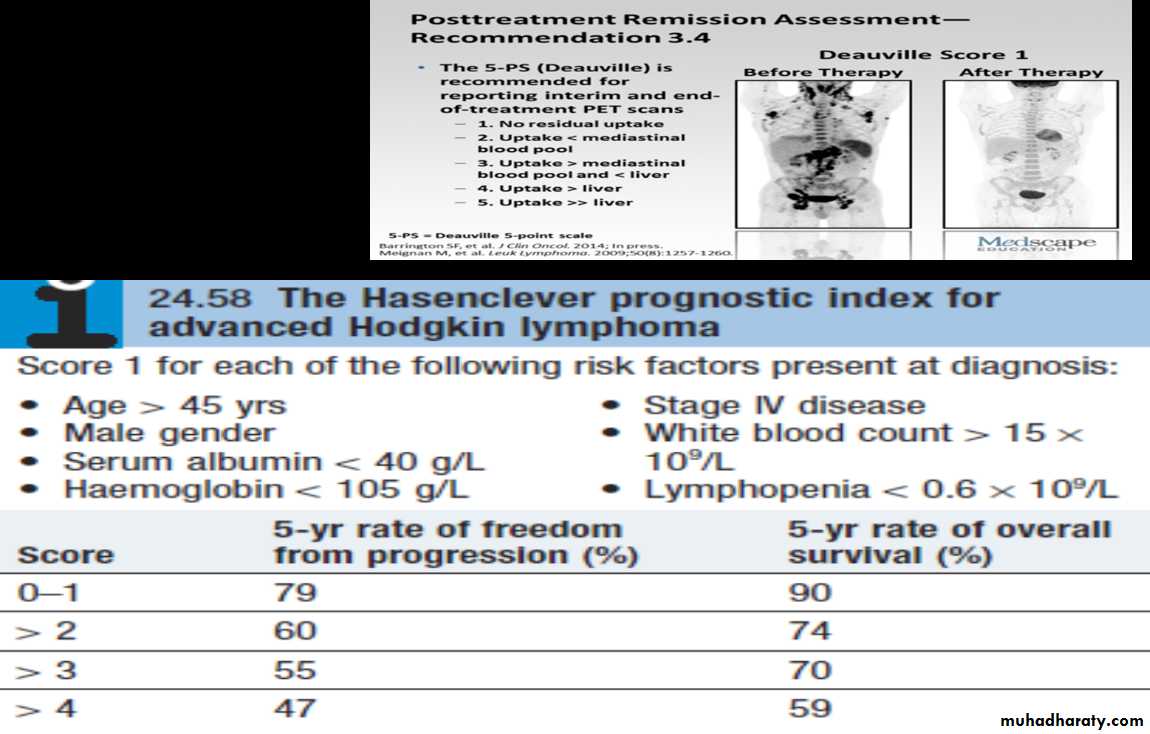
* Treatment response is assessed clinically and by repeat CT and newer (scanning modalities such as positron emission tomography (PET
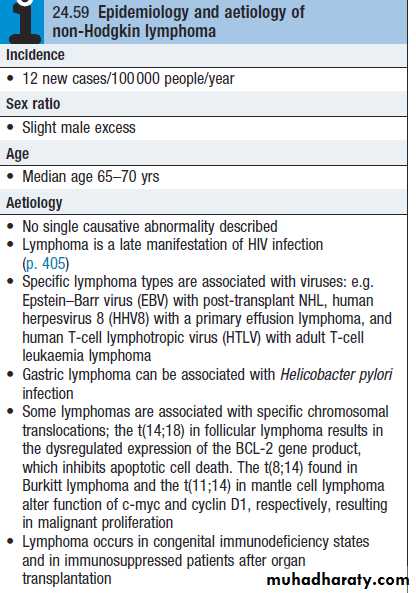
Non-Hodgkin lymphoma
Non-Hodgkin lymphoma (NHL) represents a monoclonal proliferation of lymphoid cells of B cell (70%) or T cell (30%) origin.Working formulation for lymphoma classification:
Low grade :diffuse small lymphocytic.
follicular small cleaved cell.
follicular mixed small and large cell.
Intermediate grade :
diffuse small cleaved cell.
diffuse small and large cell.
diffuse large cell lymphoma.
follicular large cell lymphoma.
High grade :
immunoblastic lymphoma.
small non cleaved cell (Burkitt-type).
lymphoblastic lymphoma.
Clinical presentation
1- most pt present with one or several enlarge painless LN. cervical, inguinal and axillary's nods are most frequently involved. Hepatosplenomegaly may be present2- 1/5-1/3 of pt with intermediate and high grade lymphoma present in extra- nodal site such as waldeyers ring, GIT, skin, salivary gland, bone.
3- compression syndromes may occur, gut obstruction, ascites, superior vena caval obstruction and spinal cord compression.
4 - BM involvement in high grade 10% and 50-60% in low grade.
5- T cell lymphoma are usually first diagnosed in the skin lead to cutaneous T cell lymphoma (sezary syndrome), erthro-derma and circulating lymphoam cells with hyper convoluted nuclei.
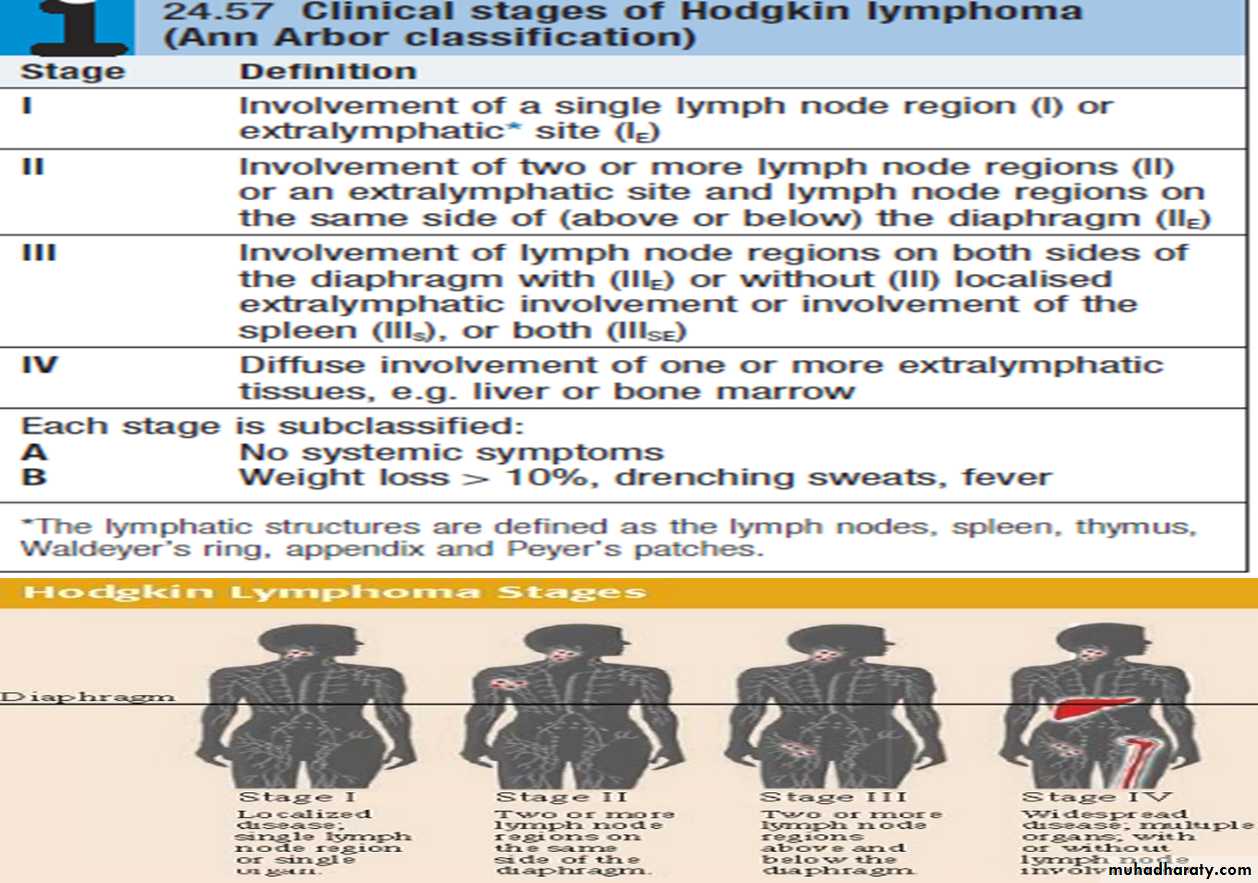
**The same staging system is used for both HL and NHL, but NHL is more likely to be stage III or IV at presentation.
Investigations:
Same as HD inaddition;
Bone marrow aspiration and trephine.
Immunophenotyping of surface antigens to distinguish T from B cell tumours.
Cytogenetic analysis to detect chromosomal translocations.
Immunoglobulin determination.
Measurement of uric acid levels.
HIV testing.
Treatment
Low grade NHL |:A symptomatic pts may not require treatment
Radiotherapy : for stage I disease.
Chemotherapy : oral therapy with chlorambucil.
The anti-CD20 antibody rituximab.
Rituximab (R) in combination with cyclophosphamide, vincristine and prednisolone (R-CVP).
Transplantation.
High-grade NHL *Prognosis
Chemotherapy; R-CHOP
Radiotherapy
HSCT
HAEMATOPOIETIC STEM ELL TRANSPLANTATION (HSCT)
A process in which abnormal, malignant, or non-functioning marrow cells are replaced with normal marrow stem cells.
Two Kinds of Stem Cells
Embryonic (also called “pluripotent”) stem cells are capable of developing into all the cell types of the body.Adult stem cells are less versatile and more difficult to identify, isolate, and purify.
Source of Stem cells
Stem cells may be derived from autologus, allogeneic or xenogenic sources. Histocompatability is prerequisite for transplantation of allogeneic stem cells.Fetal tissue is the best current tissue source for human neural stem cells, however ethical issues are a major concern.
Sources of haemopoetic stem cells
Bone marrow.Peripheral blood stem cells(PBSC).
Placental (cord blood) blood transplant.
Fetal liver.
Placenta a Source of Stem Cells
Placental stem cells, like umbilical cord blood and bone marrow stem cells, can be used to cure chronic blood-related disorders such as sickle cell disease, thalasemia, and leukaemia.Umbilical Cord Blood Stem Cell Transplant
Umbilical cord blood stem cell transplants are less prone to rejection than either bone marrow or peripheral blood stem cells.This is probably because the cells have not yet developed the features that can be recognized and attacked by the recipient's immune system
Types of HSCT
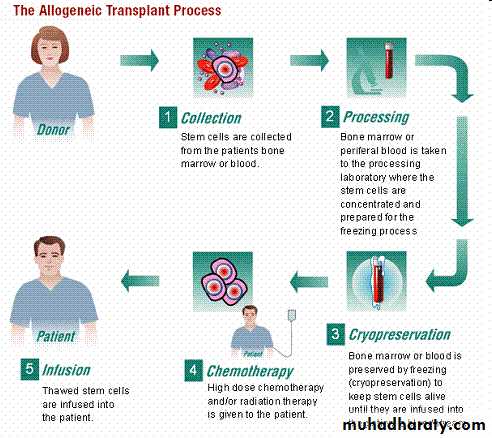
Allogeneic stem cell transplantation:
Normal BM cells are harvested from the donor& infusion into the pts after aggressive marrow ablative therapy.
The success is compromised by the fact that the transplanted lymphocytes may treat with recipients tissues.
Sources of stem cells from another donor (allogeneic) are primarily relatives (familial-allogeneic) or completely unrelated donors (unrelated-allogeneic). The stem cells in this situation are extracted from either the donor's body or cord blood
Autologus stem cell transplantation:
Is the process of harvesting, purging (treating for residual malignancy) and cryopreserving the patient's own marrow cells for re-infusion after high does chemotherapy or total body irradiation(TBI).Sources of the patient's own stem cells (autologous) are either the cells from patient's own body or his or her cord blood. For autologous transplants physicians now usually collect stem cells from the peripheral blood rather than the marrow.
This procedure is easier, unlike a bone marrow harvest, it can take place outside of an operating room and the patient does not have to be under general anaesthesia.
INDICATIONS OF BMT
1-MalignancyAML (1st remission)
ALL (high risk 1st CR, good risk 2nd CR)
CML
CLL
MDS
Hodgkins disease
NHL
Multiple myeloma.
2-Defective haemopoiesis
Aplastic anaemia.
Sickle cell anaemia.
Thalassimia major.
Granulocyte disease.
3-Immunedeficiency
sever combined immune deficiency(SCID).
Adenosine deaminase(ADA) deficiency
Complications:
20-50% of pts will experience one or more of the following :
1-Chemotherapy and radiation toxicity :
mucositis : GIT, respiratory tract, bladder.
Intrahepatic vascular occlusive disease (VOD).
Toxic pneumonitis .
CNS toxicity.
Endocrine dysfunction lead to hypothyoidisim.
Cataract.
2. Graft Versus host disease (GVHD):
Acute 20-100 days
* Due to engrafment of donor T cell, that react against the recipient tissues.
It can affect the skin,causing rashes, the liver, causing jaundice, and the gut, causing diarrhoea, and may vary from mild to lethal. Prevention includes HLA-matching of the donor, immunosuppressant drugs, including methotrexate, ciclosporin, alemtuzumab or antithymocyte globulin.
Chromic 6-12 months
It often resembles a connective tissue disorder (scleroderma-like), treated with corticosteroids and prolonged immunosuppression with, for example, ciclosporin.
Graft versus leukaemia effect?.
3. Infections:
Due to immundeficiency & granulocytopenia :a-Bacterial infection G+ve, G.-ve .
b-Fungal infection : candida albicans.
c-Viral : Herpes zoster, CMV.
d-Parasitic infection : Interstitial pneumonitis caused by Pneumocystis jiroveci
Interstitial pneumonitis :
-chemotherapy & radiation toxicity.
-Mortality 50-90%.