Fifth stage
Pediatric
Lec. 8
.د
منار
2/3/2017
ALOPECIA
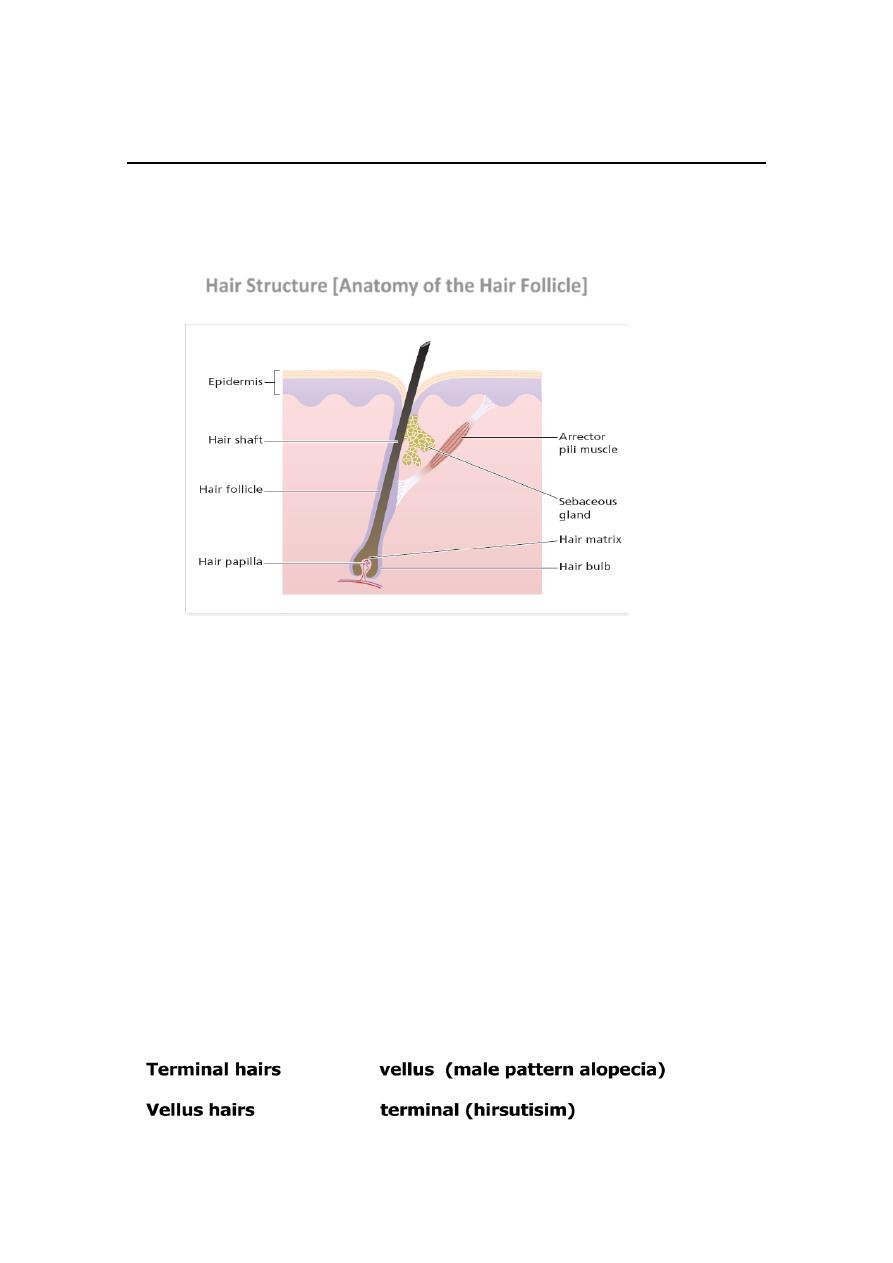
Hair Structure [Anatomy of the Hair Follicle]
2
Classification of Hairs
Hairs are classified into three main types:
1. Lanugo hairs: Fine long depigmented hairs covering the
fetus, but shed about 1 month before birth.
2. Vellus hairs: Fine short unmedullated hairs, but coarses than
lanugo hairs covering much of the body surface. They replace
the lanugo hairs just before birth.
3. Terminal hairs: Long coarse medullated (pigmented) hairs
seen, for example, in the scalp, and pubic region.
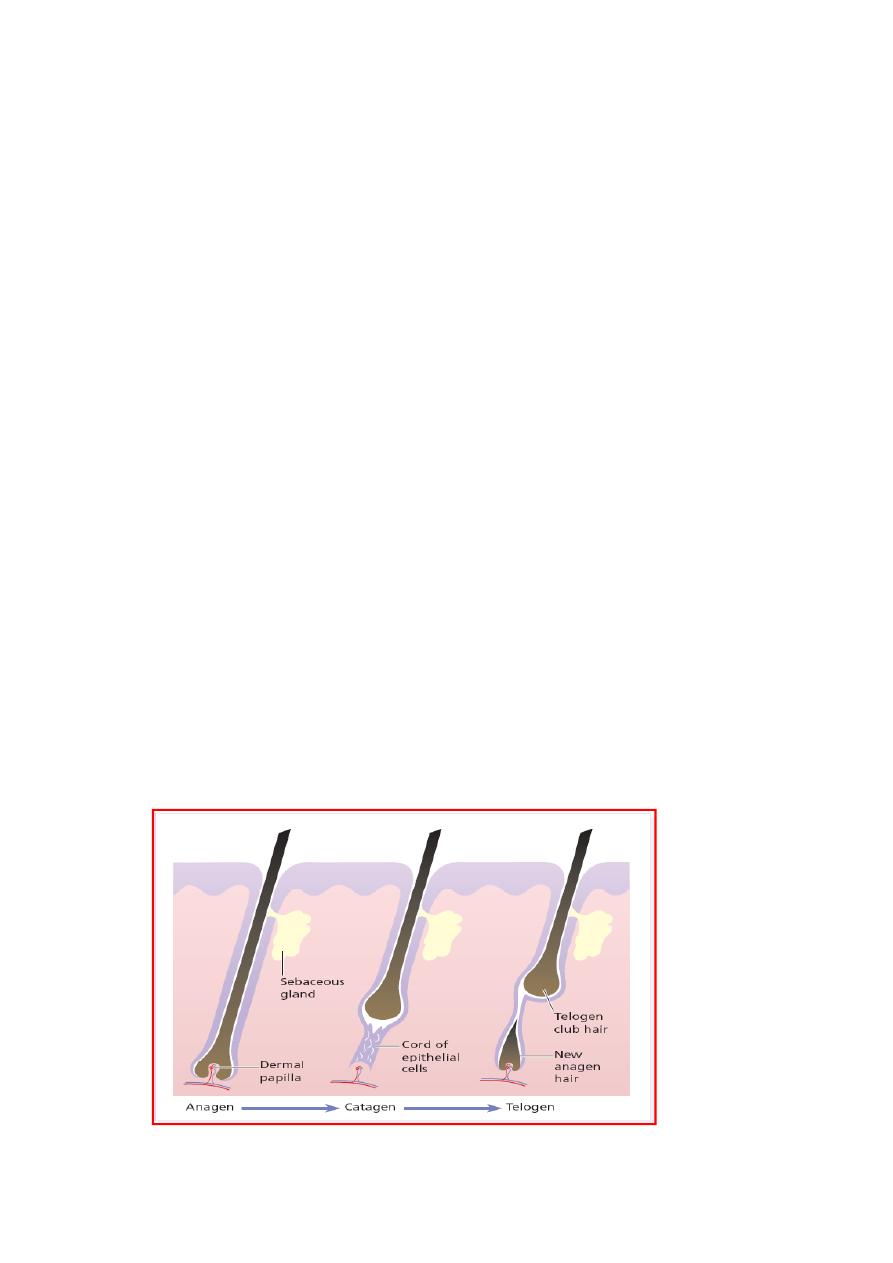
The Hair Cycle
Each follicle passes, independently of its neighbours, through
regular cycles of growth and shedding.
There are three phases of follicular activity:
1. Anagen:
The active phase of hair production.
lasts for 3-5 years. Account for 85% of scalp hair
2. Catagen:
A short phase of conversion from active growth to the
resting phase.
Growth stops, and the end of the hair becomes club-
shaped.
last about 3 weeks. Account 1-2 % of scalp hair.
3. Telogen:
A resting phase at the end of which the club hair is shed.
last about 3 months.
Account 14% of scalp hair.
The duration of each of these stages varies from region to region.
The scalp contains an average of 100 000 hairs.
As many as 100-150 hairs may be shed from the normal scalp
every day as a normal consequence of cycling.
Average scalp hair growth: 0.35 mm/day or ~ 1cm/month.
Cutting or shaving the hair have no effect on hair growth.
Female hair grows faster than male hair.
CLASSIFICATION OF
ALOPECIA
ALOPECIA
LOCALIZED
SCARRING
NON-SCARRING
DIFFUSE
Localized A. is characterized by well-defined patchy areas of hair
loss, while diffuse hair loss involves the whole scalp.
Non-scarring A. has better prognosis than scarring A. as the hair
usually grow again after a time because the hair roots are
preserved.
Hair loss in scarring A. is permanent [no hope for cure] due to
damaged hair roots by the scarring process.

CAUSES OF LOCALIZED NON-SCARRING ALOPECIA
1. Alopecia areata
2. Androgenetic alopecia (Early stages)
3. Tinea capitis (early treatment may prevent scarring)
4. Pyogenic infections e.g. boils or folliculitis.
5. Moth-eaten alopecia (Secondary syphilis)
6. Traumatic alopecia:
a) Trichotillomania [Hair pulling habit]
b) Traction alopecia
c) Neonatal frictional alopecia (Occipital)
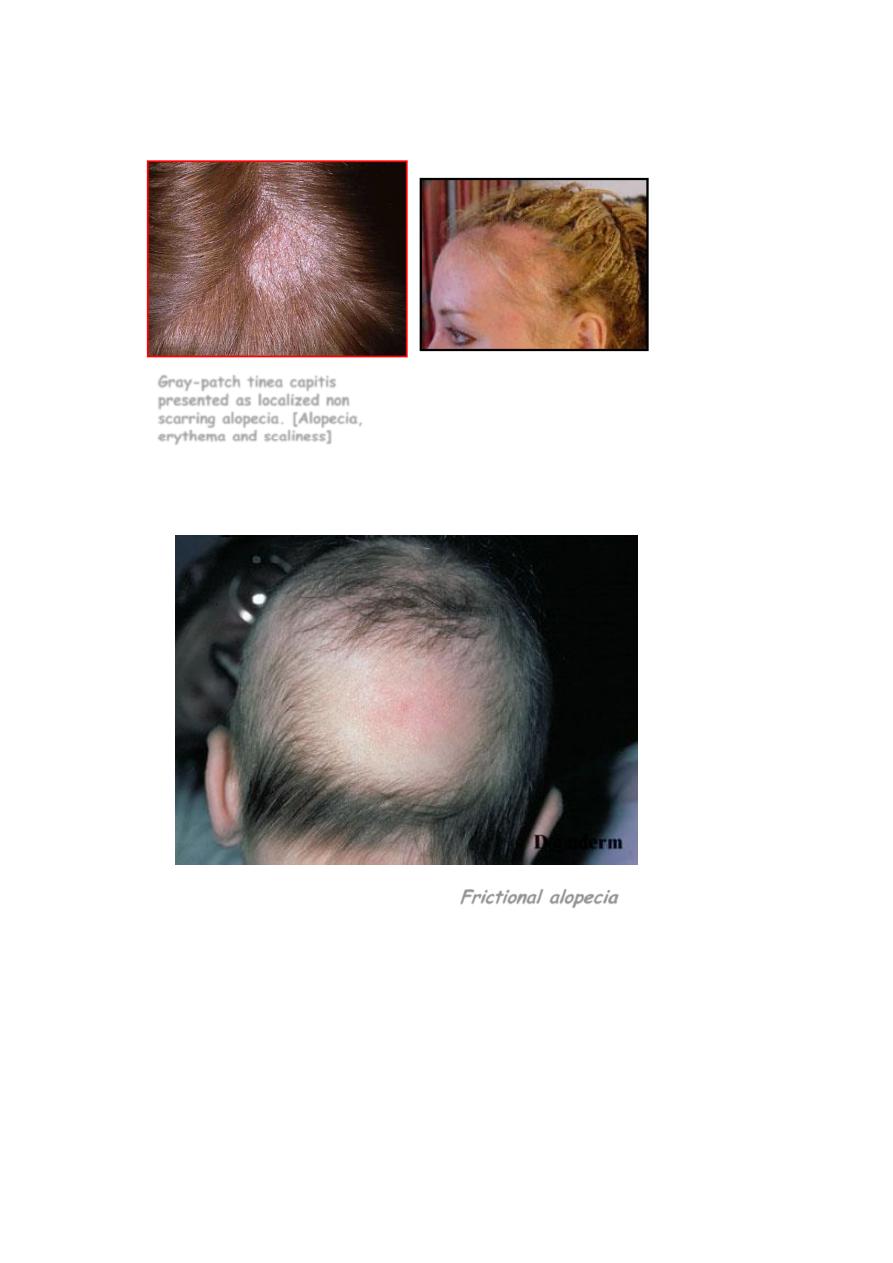
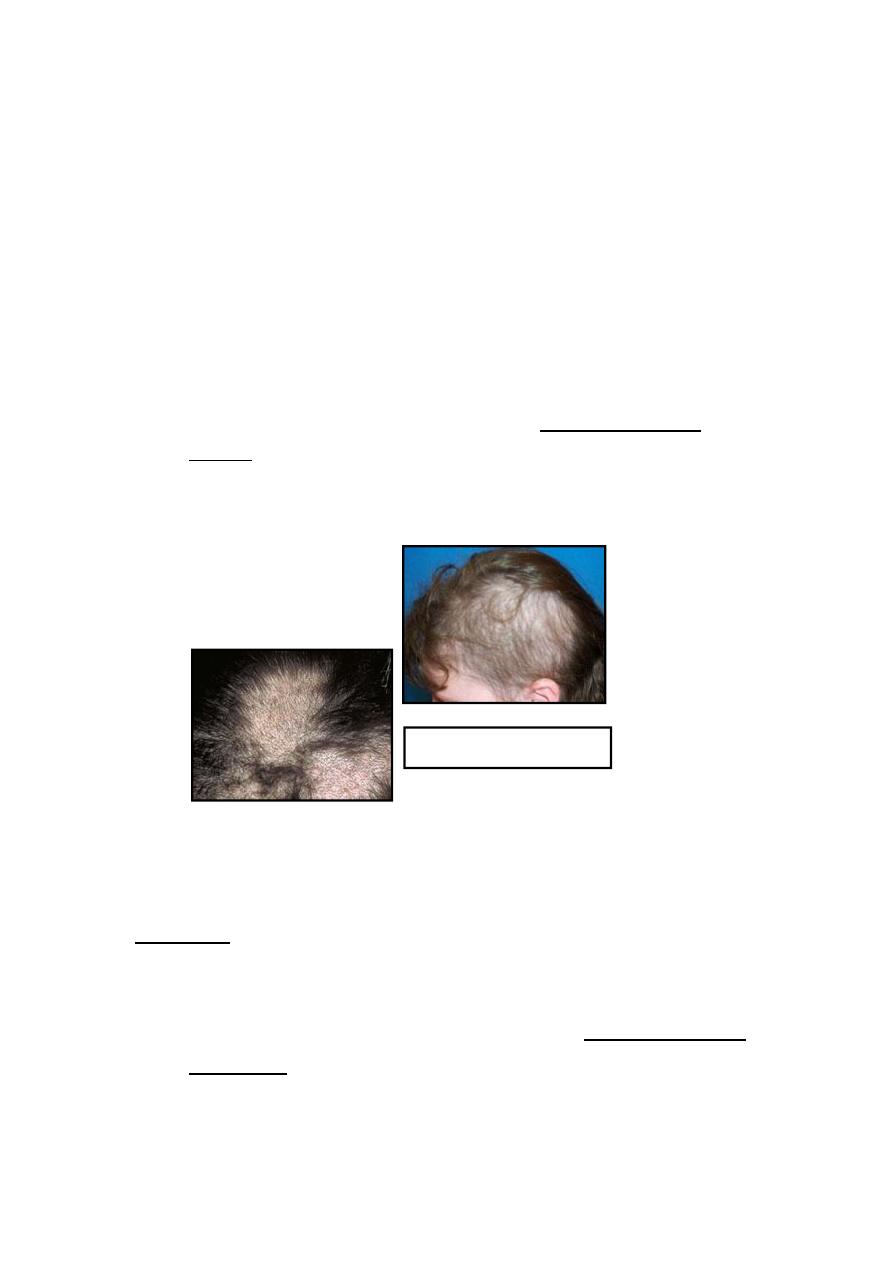
Gray-patch tinea capitis
presented as localized non
scarring alopecia. [Alopecia,
erythema and scaliness]
Traction alopecia
11
Traumatic hair loss in a newborn “
Frictional alopecia
”
CAUSES OF LOCALIZED SCARRING ALOPECIA
1. Physical injury e.g. trauma and burn
2. Severe infections
A. Fungal infections e.g. Kerion or Favus
B. Bacterial infections e.g. Boils and Carbuncles
C. Protozoal infestation (e.g. cut. leishmaniasis)
D. Viral infection e.g. Herpes zoster
5. Neoplasms: Cicatricial BCC, SCC, Metastatic Ca
6. Lichen planus (Lichenplanopilaris)
7. CTDs e.g. DLE and Morphea
8. Folliculitis decalvans
9. Sarcoidosis
10. Iatrogenic (IL-CS injections)
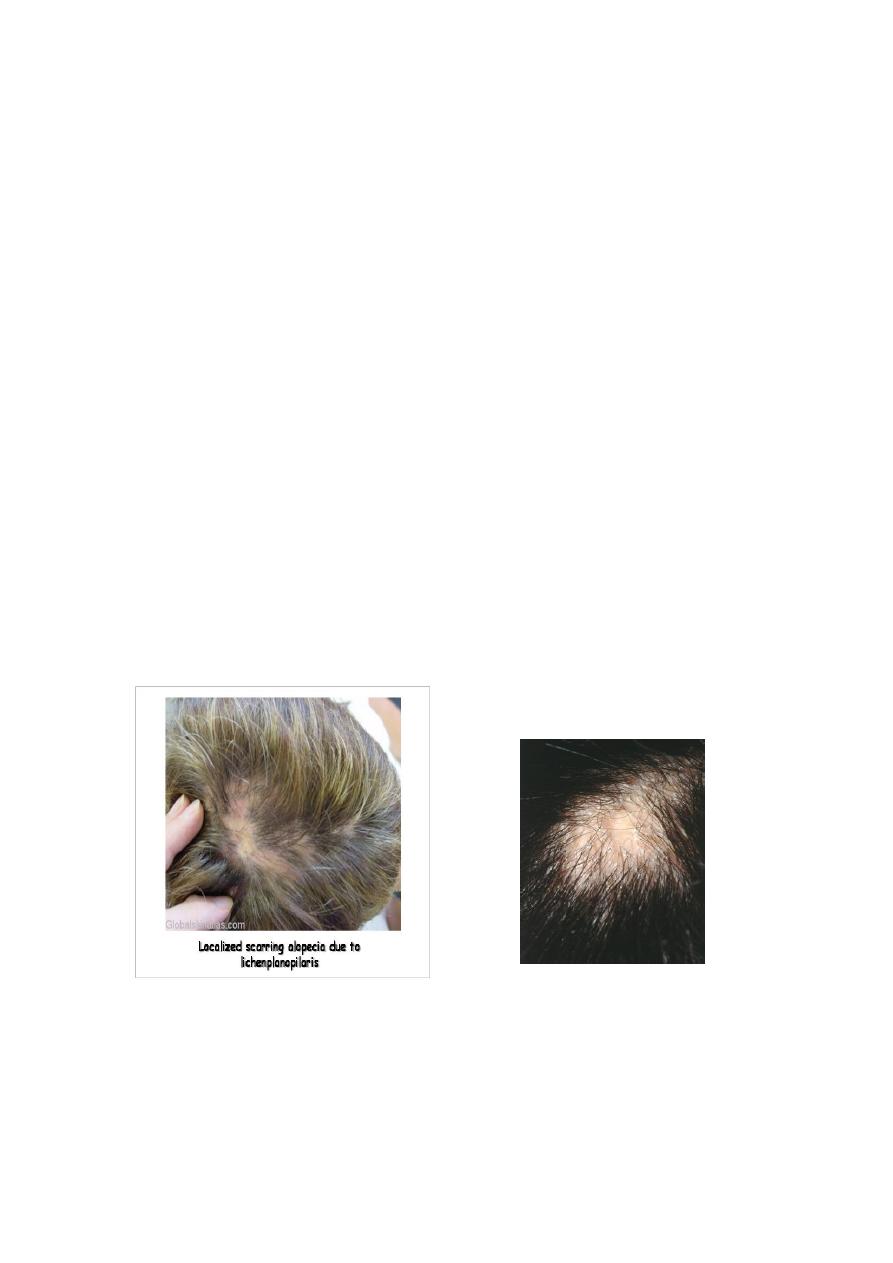
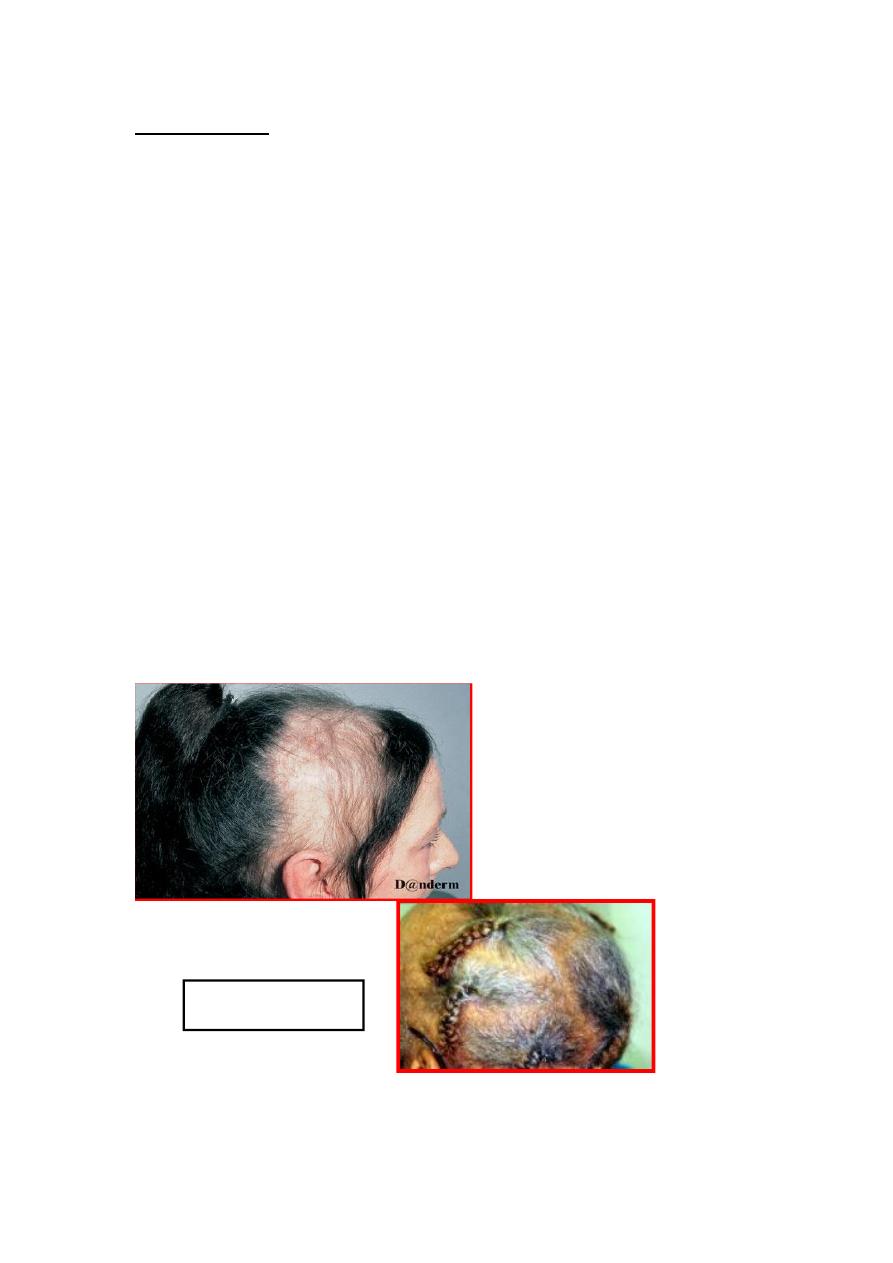
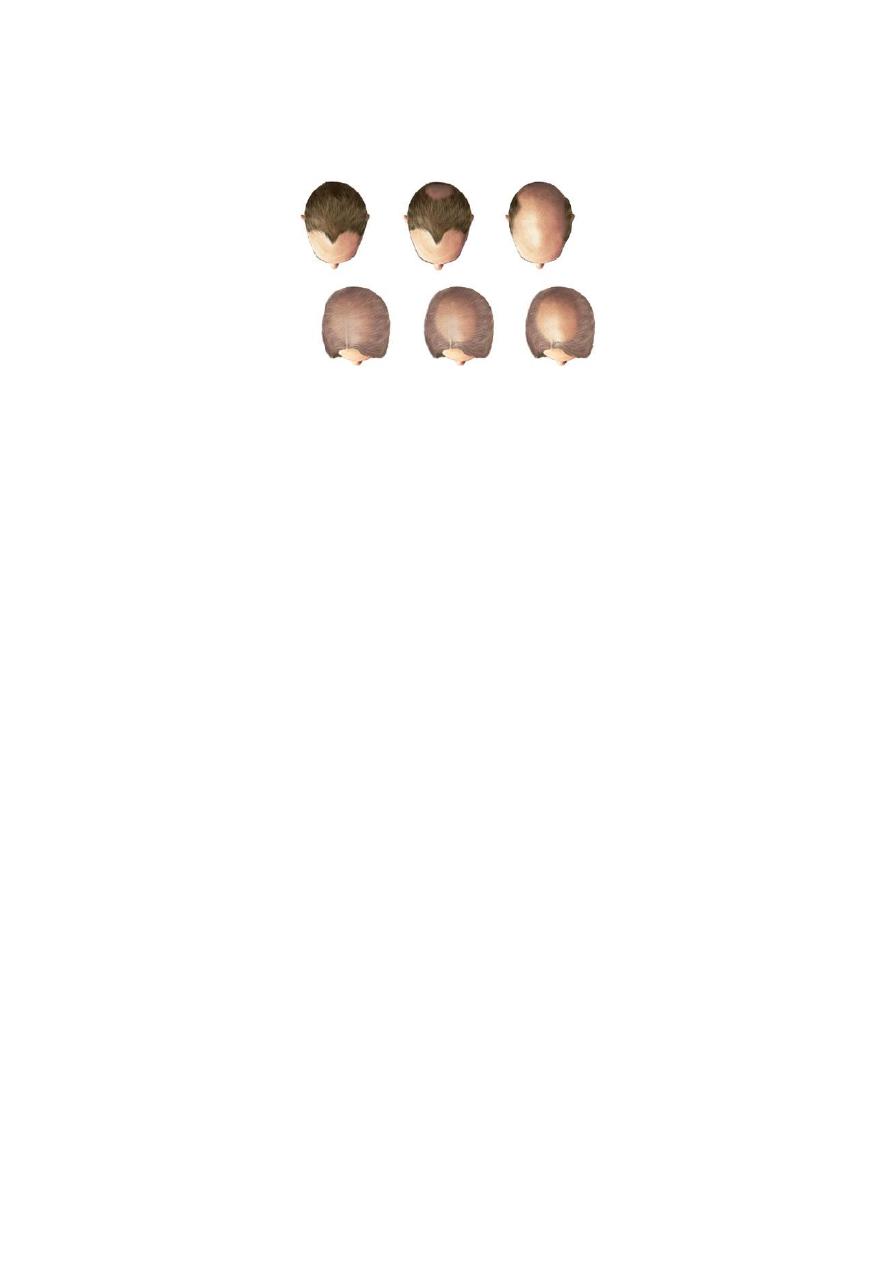
Localized cicatricial alopecia
(LP)
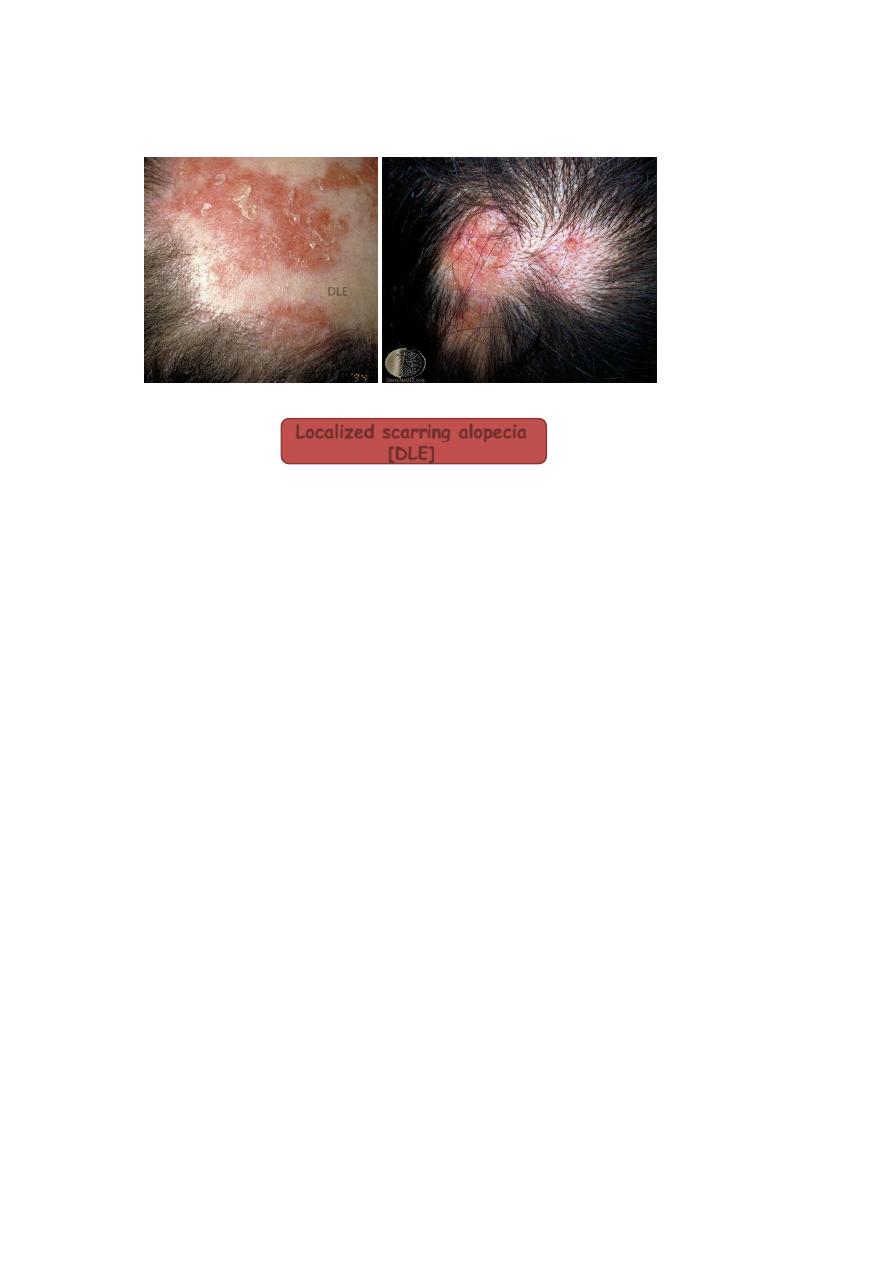
Localized scarring alopecia
[DLE]
DLE
CAUSES OF DIFFUSE ALOPECIA
1. Androgenitic alopecia
2. Diffuse alopecia areata (A. totalis and A. universalis)
3. Physiological (Neonatal alopecia)
4. Anagen effluvium
5. Telogen effluvium

Alopecia areata
*
AA is one of the commonest hair problems in dermatological daily
practice. It affects about 1-2% of the patients seen at out-patient
skin clinics.
*
It is an acquired idiopathic disorder characterized by well-defined,
single or multiple, non-cicatrical patches of hair loss.
*
It may affect any age group, although more common in young
people. Both sexes are equally affected.
*
AA can involve any hairy area in the body (scalp, eyebrows,
eyelashes, moustache, beard, axillary hair, pubic hair, body
“truncal” hair and hair of the extremities).
Aetiology of AA:
1. Immunological factors: AA may be considered as an autoimmune
disease for the following reasons:
a) Association with other autoimmune disorders like vitiligo, atopic
dermatitis, Hashimoto’s thyroiditis , Addison’s disease, DM,
Pernicious anemia …..etc.
b) Presence of circulating organ specific auto-antibodies e.g. anti-
thyroid antibodies .
c) Histologically, T lymphocytes around affected hair bulbs.
2. Genetic factor: about 10-25% of cases may be familial.
3. Psychological factor: Severe psychological upset probably acts as a
precipitating or triggering factor.
Clinical picture:
*
Patches of AA occur most commonly in the scalp and secondly in
the beard area.
*
The skin in the involved area is normal i.e. no scarring, scaling or
erythema.
*
Close examination of the alopecic patches may show the tendency
of hair at the periphery of these patches to be thinner proximally
and thicker distally and look like an exclamation mark [!].
Exclamation mark sign indicates active disease but not necessarily
bad prognosis.
*
AA may involve the nails and up to 50% of patients may show fine
pitting of the nails.
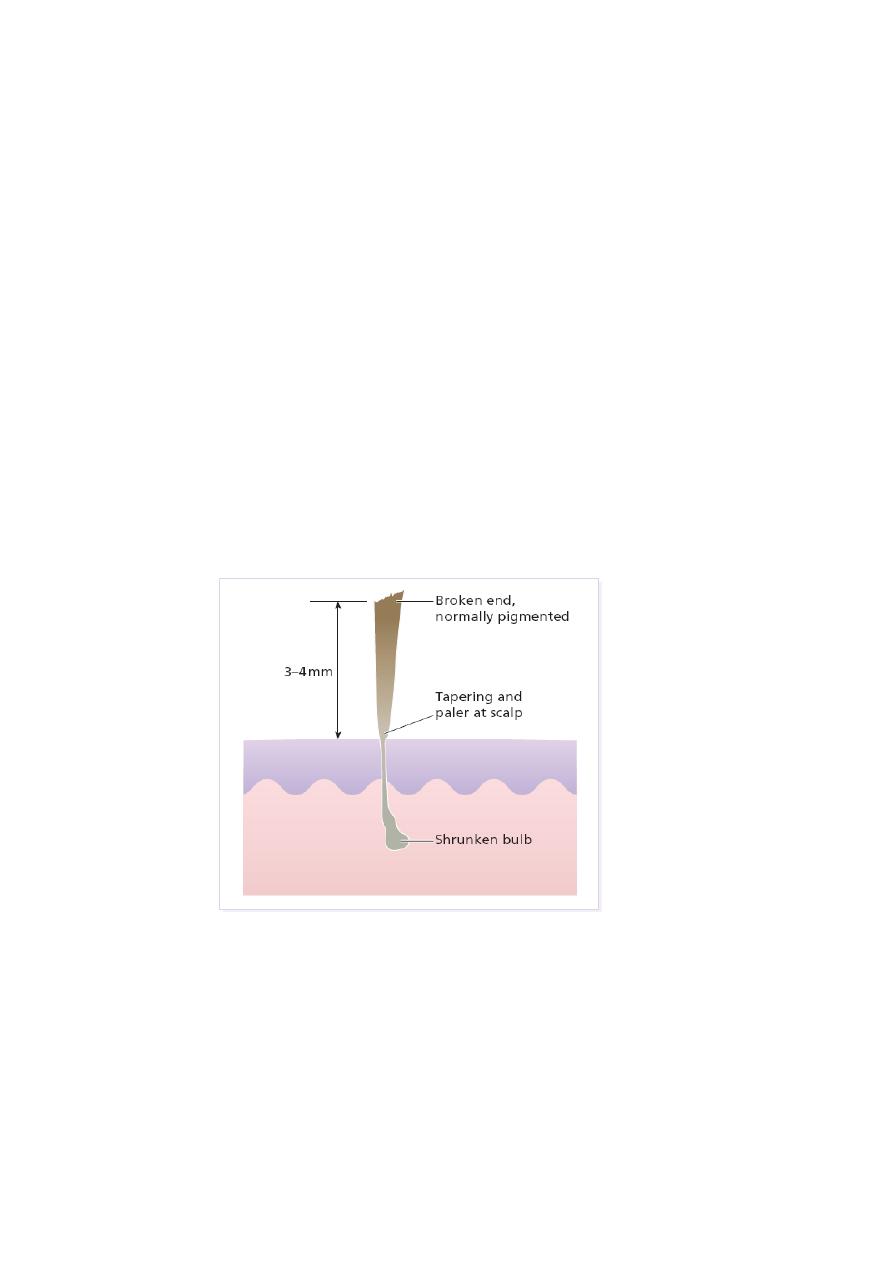
An exclamation-mark hair
Pathognomonic exclamation mark hairs seen around the edge
of alopecic areas. They are broken off about 4mm from
the scalp, and are narrowed and less pigmented proximally.
22
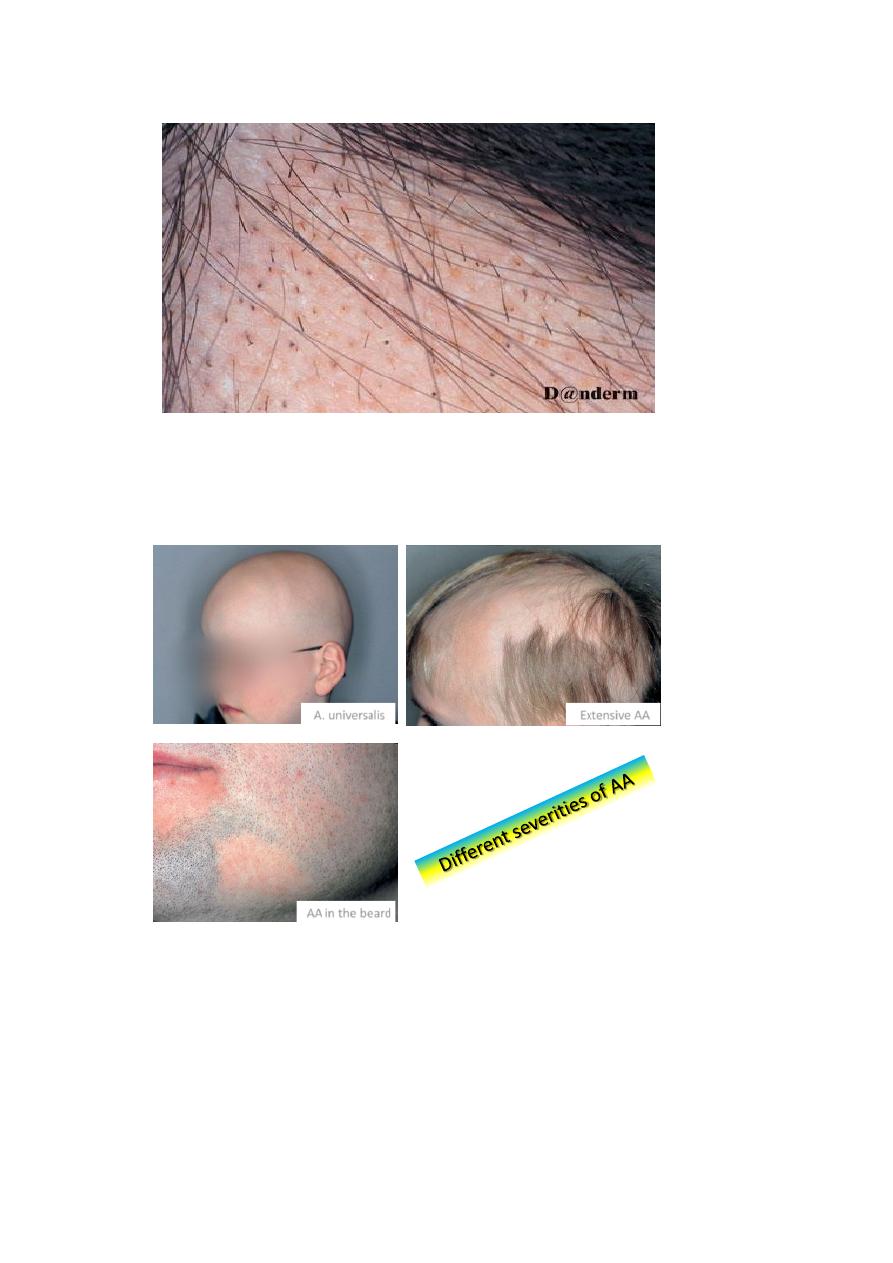
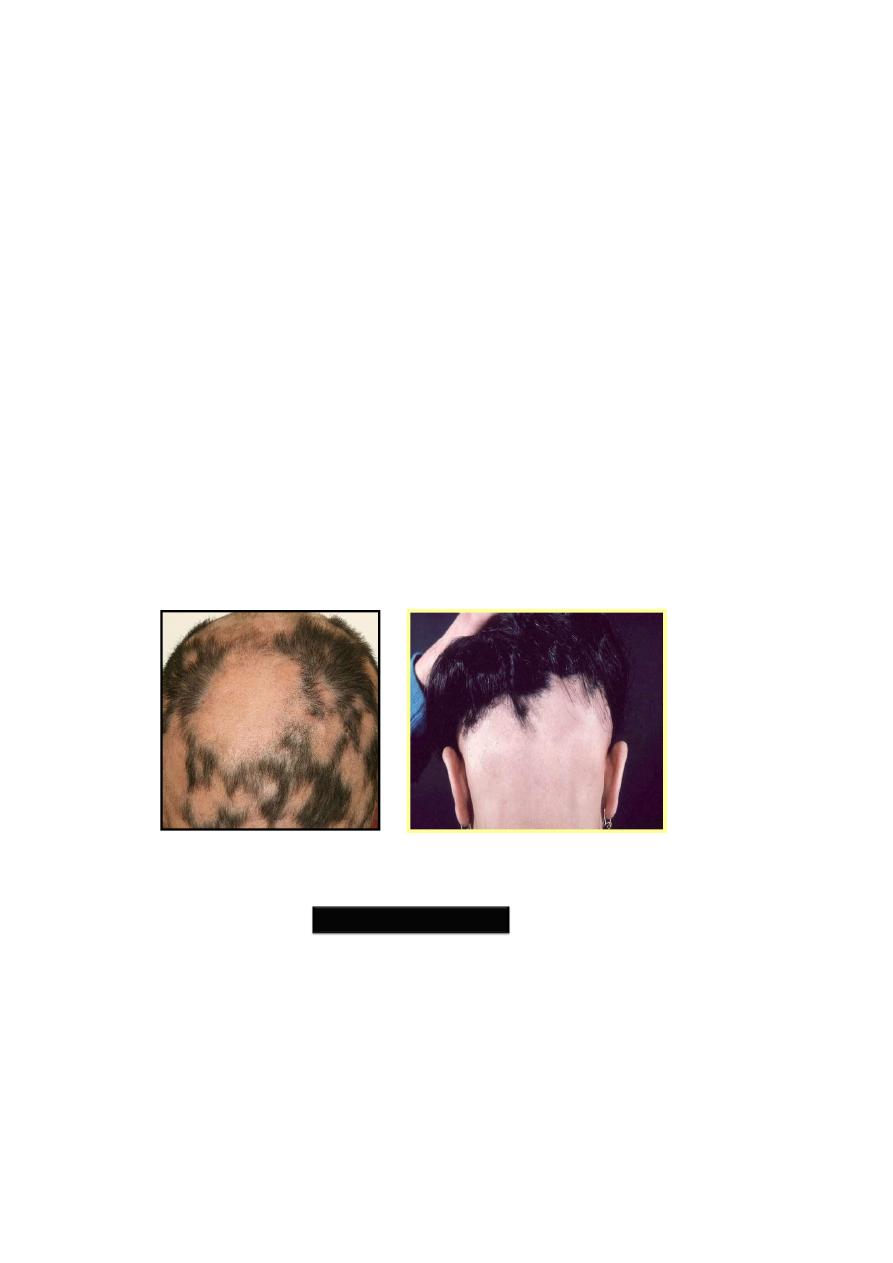
Extensive AA
AA in the beard
A. universalis

Course:
The outcome is unpredictable.
In the first attack, regrowth is usual within a few
months.
Subsequent episodes tend to be more extensive & regrowth is
slow.
Few patients loss all the scalp hair (alopecia totalis), or from the
whole skin surface (alopecia universalis).
The hair lost in AA may become grey-white in color on regrowth
especially on spontaneous regrowth i.e. without treatment.
AA usually dose not affect grey hair (only pigmented hair is
involved by AA).
White hair
Post A.A.
Bad Prognostic Pointers (Signs) in AA
1. Unusually widespread alopecia especially alopecia totalis and
alopecia universalis.
2. Early onset of the disease i.e. onset before puberty.
3. Multiplicity of the patches.
4. Chronicity (Recurrent cases).
5. Presence of nail changes.
6. Involvement of the scalp margin (Ophiasis),especially at the nape
of the neck.
7. Familial AA [Positive F.H of AA].
8. Association with atopy or Down’s syndrome.
Bad Prognostic signs

Differential diagnosis:
1.
Tinea capitis.
2. Traction alopecia.
3. Trichotilomania
4. Secondary syphilis.
5. DLE (DISCOID LUPUS ERYTHEMATOSUS )
6. Lichen planus
Management of AA :
1. Reassurance (not contagious with high rate of spontaneous
recovery). The aim of therapy is to facilitate recovery.
2. Topical irritants to stimulate hair growth such as dithranol (0.1–
0.25% ), Garlic, Plant extracts ….etc. are often used but with
limited success.
3. Topical minoxidil 5% solution.
4. Topical corticosteroids.
5. Intralesional steroids (triamcenolone 5-10 mg/ml)
6. PUVA may be considered in resistant cases unresponsive to other
therapies and in extensive cases like A. totalis and universalis.
7. Immunomodulators e.g. Oral zinc sulfate
8.
Wigs may be necessary for extensive cases.
Trichotillomania:
Trichotillomania ( Hair-pulling habit ) is a discomfort habit in
children like nail-biting and lip-licking. It is a type of traumatic
localized non-scarring alopecia not uncommonly seen in children
and occurs more in girls than in boys.
Affected individuals may have obsessive compulsive neurosis.
The usual involved sites are the sides of the scalp or the fronto-
vertical area.
The hairs in the affected area are usually broken at different
lengths from the scalp surface which is a characteristic feature of
trichotillomania.
Trichotillomania
Diagnosis
• can usually be made on the history.
• The patches are irregular in outline and hair loss is never
complete.
Management includes
-reassurance, explanation to the parents or the patient that it is due to
the habit of hair pulling,
- tranquilizers may be given and referral to psychiatrist may be necessary
in some cases.
Traction alopecia
Hair can be pulled out by many methods:
hot combing, tight hairstyle & using hair rollers.
Hair being lost in area of maximal tension.
Marginal alopecia is a common pattern, in which hair loss occur
around the edge of the scalp (at the sides or at the front).
The bald area show short broken hairs, folliculitis & sometime
scarring.
Traction
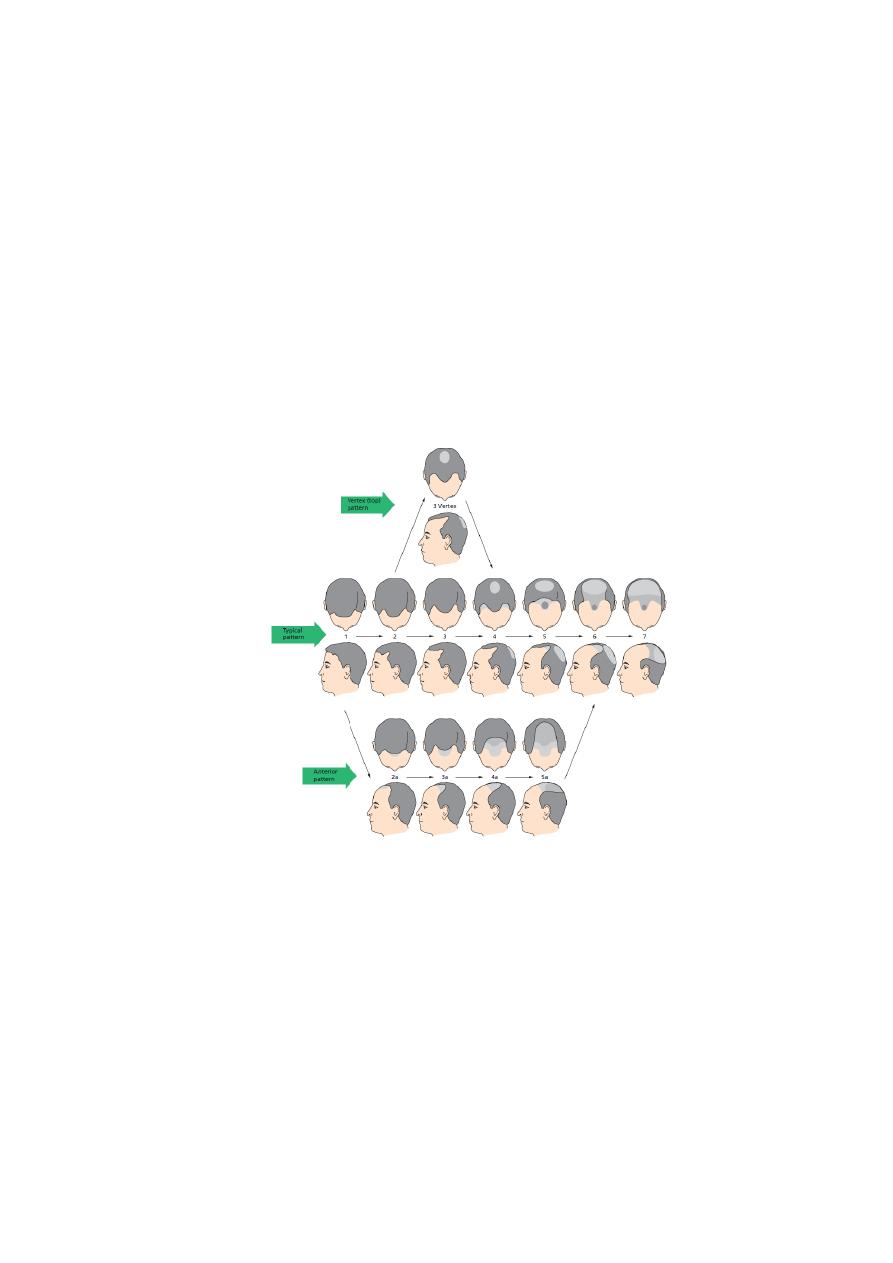
Male pattern alopecia:
Its a physiological reaction induced by androgen in genetically
predisposed men.
Its inheritance is polygenic.
Thinning of hair begin between 12 - 40 years.
About 50% of the population develop this condition before the
age of 50.
Its due to progressive shortening of successive anagen cycles.
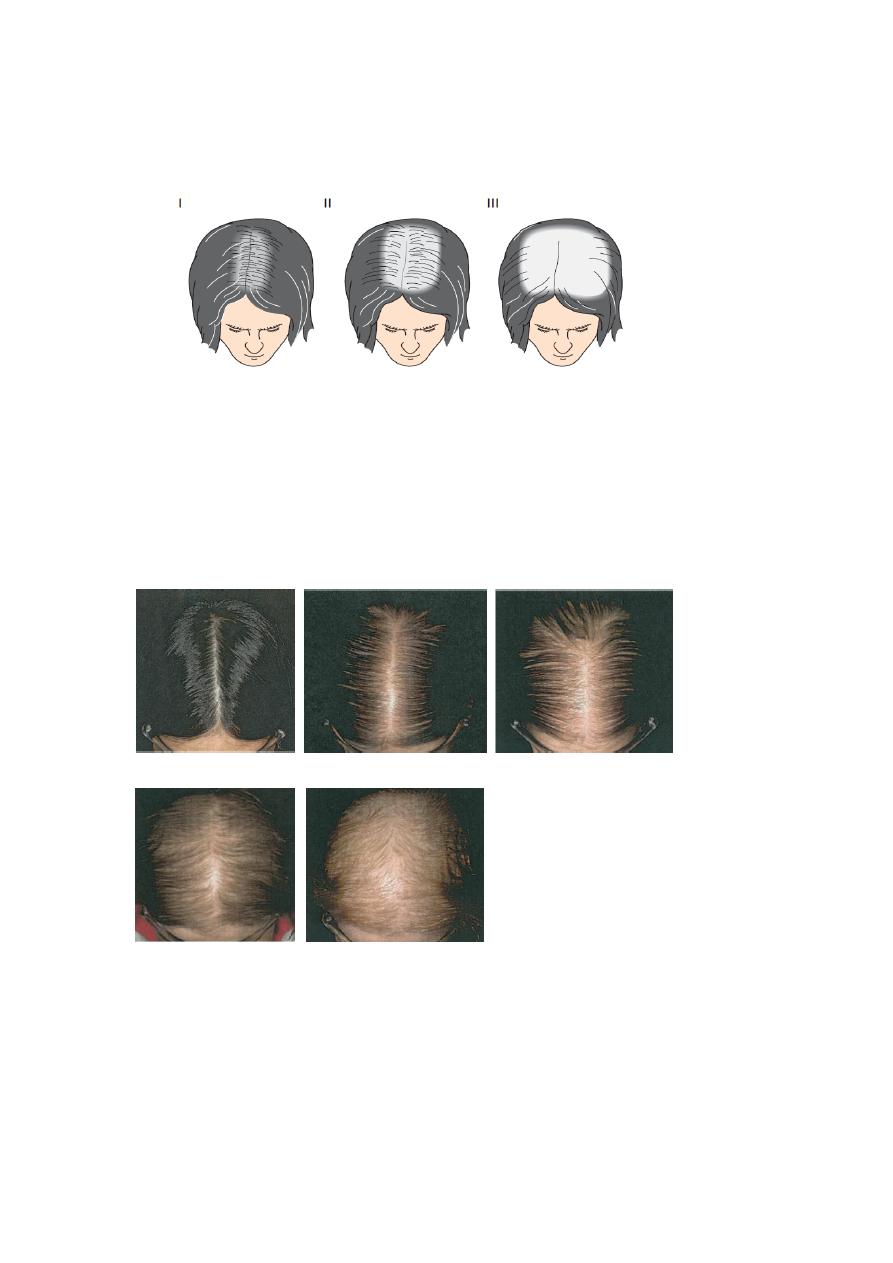
Hamilton
scale for
grading male
pattern hair
loss.
Treatment:
1. Topical minoxidil 2%, 5%.
2. Oral fenisteride 1mg, 5mg.
3. Hair transplant.
4. Scalp reduction & flap.
Female pattern alopecia:
In females, normal androgen level causes baldness only in strongly
predisposed women (less predisposed women need high androgen level
to produce baldness). The female hormone, estrogen, may have
protective role in preventing common baldness.
It affect females in their 20s or 30s.
There is gradual loss of hair on the central scalp, with retention of the
normal hair line without fronto-temporal recession.
Differ from male pattern baldness:
1. In females, diffuse thinning of the fronto-vertical hair with
preservation of the frontal line.
There may be a moderate loss of hair on the crown,
but this rarely progresses to total or near baldness
as in men.
2. Male pattern baldness can begin at puberty where
as female pattern baldness begins around thirty,
& it gets worse with menopause.
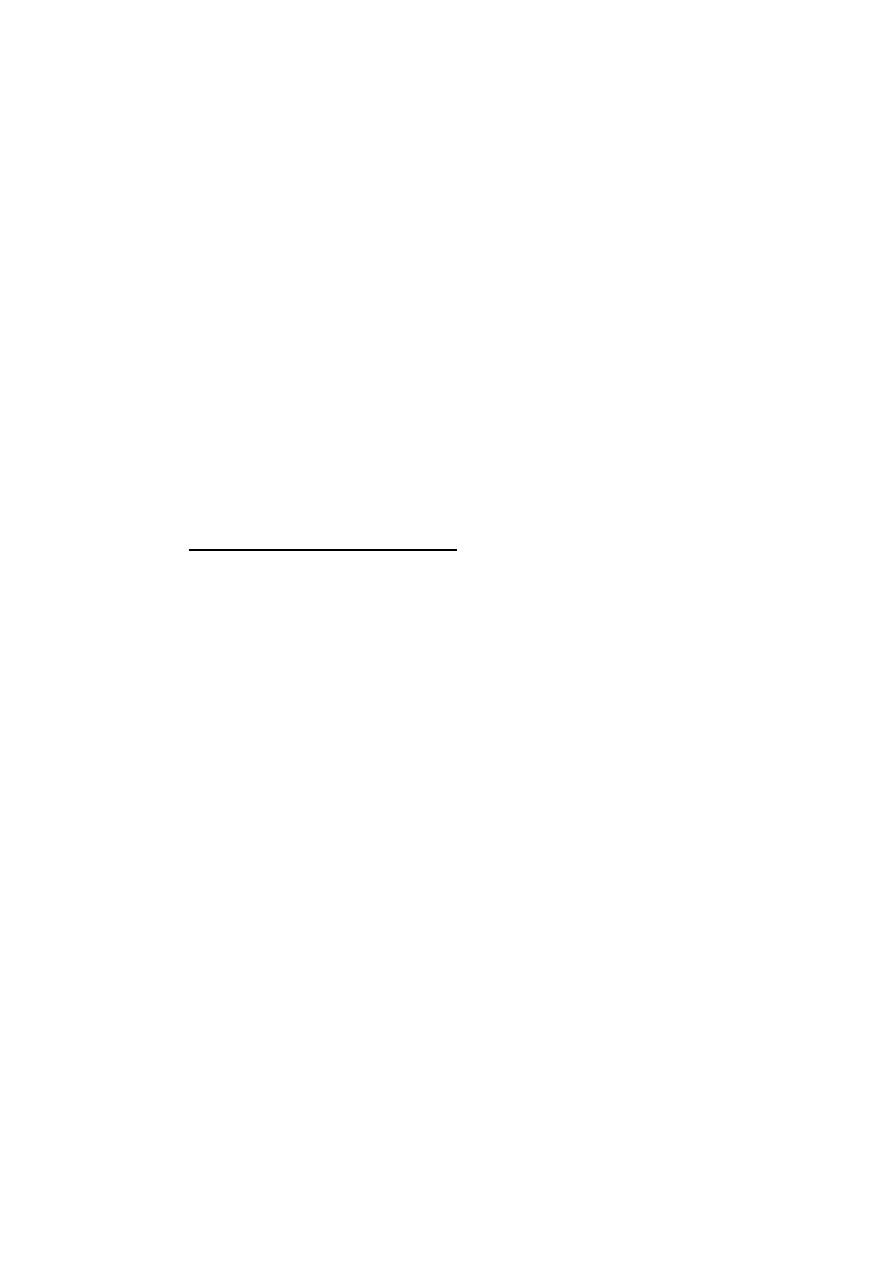
Ludwig scale for grading female pattern hair loss
Pattern of hair loss
in women with
androgenetic alopecia
Male
Female
Telogen Effluvium
Premature termination of anagen & high number of normal hairs
enter the resting telogen phase.
Usually no more than 50% of the hair is affected.
The follicle is not diseased, scarring & inflammation are absent.
Resting hairs on the scalp remain about 100 days before
they lost, so telogen hair loss should occurs approximately
3 months after the event.
The hair loss begins abruptly & last about 4 weeks.
Full recovery can be expected.
Causes of telogen effluvium:
Can be triggered by any severe illness or condition. The most common
causes are:
1. Parturition (Postpartum telogen effluvium)
2. Fever (Post febrile telogen effluvium): may be caused by any
febrile illness.
3. Severe dieting: Kwashiorkor, starvation diet, and inappropriate
weight reduction programs.
4. Severe stress (major surgery, hemorrhage, car accident, severe
psychological upset …..etc.)
5. Hypothyroidism
6. Renal dialysis
7. Drugs (Drug-induced telogen effluvium): the most common ones
are: Bromocreptine, Captopril, Coumarin anticoagulants,
Carbamazepine, etc…
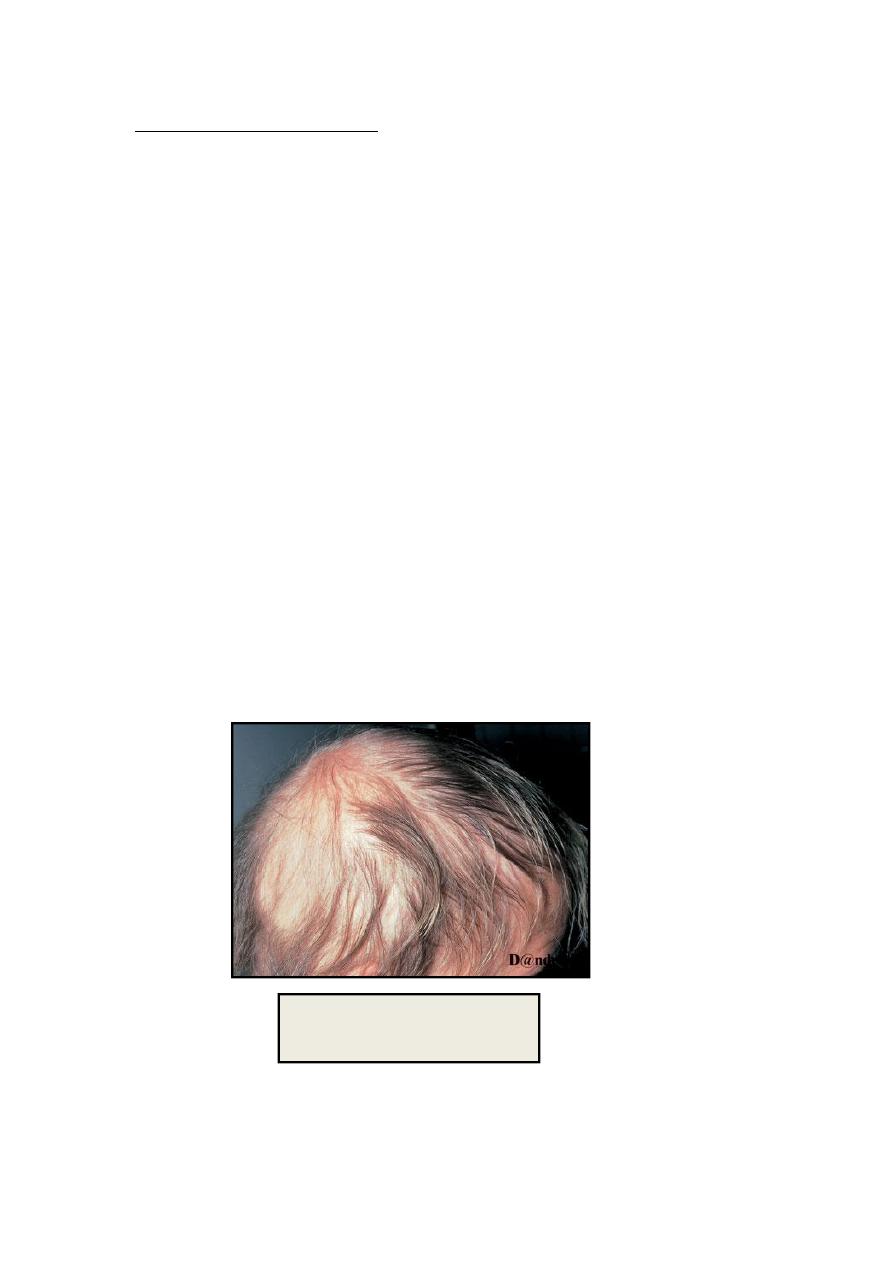
Post febrile telogen effluvium

Treatment:
There is no specific therapy for telogen effluvium but the patients can be
reassured that their hair fall will be temporary and hair will grow again
after few months.
Anagen Effluvium:
Abrupt loss of hair from follicles that are in their growing phase.
The only hair left are those in the telogen phase.
The rapidly dividing cells of the matrix & cortex are affected.
90% of the scalp hairs are in anagen phase, so a large number of hair can
be affected.

