DISEASES OF THE ESOPHAGUSTUCOMInternal Medicine4th class Dr Hasan. I. Sultan
Learning objectivesReview the functional anatomy and physiology of esophagus.
Understand the concept of Gastro-esophageal reflux disease (GERD).
List the factors that associated with development of GERD.
Explain the clinical features of GERD.
List the important investigations and it’s indications in patients with GERD.
Review the treatment of GERD.
List the complications of GERD.
List other causes of esophagitis.
List the motility disorders of esophagus.
Describe the definition, pathogenesis, and clinical presentation of achalasia.
11. Outline the important investigations of achalasia.
12. review the treatment of achalasia.
13. List the types of esophageal tumours.
14. Recognized the epidemiology of esophageal carcinoma.
15. Understand the difference between squamous cell carcinoma and adenocarcinoma of esophagus.
16. Known the clinical features of esophageal carcinoma.
17. List the important investigations of esophageal carcinoma.
18. Outline the treatment of esophageal carcinoma.
Esophagus: This muscular tube extends 25 cm from the cricoid cartilage to the cardiac orifice of the stomach. It has an upper and a lower sphincter. it is lined by stratified squamous epithelium. The muscle layers of the upper esophagus are striated skeletal muscle, while the muscles of lower part are smooth. A peristaltic swallowing wave propels the food bolus into the stomach. DISEASES OF THE ESOPHAGUS
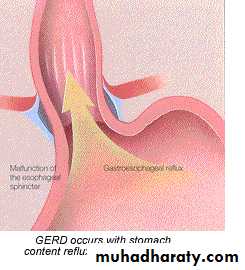
GASTRO-ESOPHAGEAL REFLUX DISEASE Gastro-esophageal reflux resulting in heartburn affects approximately 30% of the general population.Gastro-esophageal reflux disease (GERD) develops when the esophageal mucosa is exposed to gastric contents for prolonged periods of time, resulting in symptoms and, in a proportion of cases, esophagitis. Several factors are known to be involved;
Factors associated with the development of (GERD)
Hiatus hernia Hiatus hernia: An anatomical abnormality in which part of the stomach protrudes up through the diaphragm into the chest.Causes reflux because the pressure gradient between the abdominal and thoracic cavities, which normally pinches the hiatus, is lost. In addition, the oblique angle between the cardia and esophagus disappears. Many patients who have large hiatus hernias develop reflux symptoms.
Types of hiatus hernia
Clinical features of GERD Major symptoms; are heartburn and regurgitation, often provoked by bending, straining or lying down.Waterbrash; which is salivation due to reflex salivary gland stimulation as acid enters the gullet.Others develop odynophagia or dysphagia. A few present with atypical chest pain which may be severe, can mimic angina and is probably due to reflux-induced esophageal spasm.
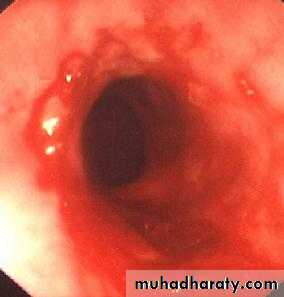
Complications 1- Esophagitis: A range of endoscopic findings, from mild redness to severe, bleeding ulceration with stricture formation.2- Barrett's esophagus: ('columnar lined oesophagus'-CLO) is a pre-malignant glandular metaplasia of the lower esophagus, in which the normal squamous lining is replaced by columnar mucosa composed of a cellular mosaic containing areas of intestinal metaplasia . CLO is the major risk factor for esophageal adenocarcinoma.
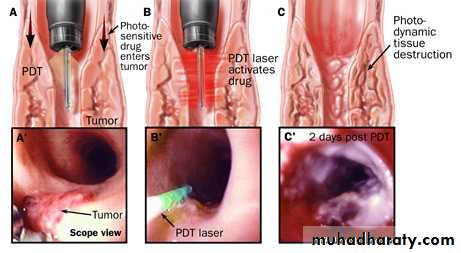
Diagnosis of Barrett's esophagus; This requires multiple systematic biopsies to maximise the chance of detecting intestinal metaplasia and/or dysplasia. Surveillance is currently recommended every 2-3 years for those without dysplasia and at 6-12-monthly intervals for those with low-grade dysplasia. Management of Barrett's esophagus; Neither potent acid suppression nor antireflux surgery will stop progression or induce regression of CLO.Endoscopic ablation therapy or photodynamic therapy can induce regression.Esophagectomy is widely recommended for those with HGD as the resected specimen harbours cancer in up to 40%.
Barretts columnar epithelium on left and squamous epithelium on right. intestinal metaplasia (note the goblet cells in the columnar mucosa).
Photodynamic therapy is the use of laser light in combination with a light-sensitive drug, called Photofrin, to destroy diseased tissue. The light activates the drug and kills diseased cells without affecting normal tissue.
3- Anaemia; Iron deficiency anaemia occurs as a consequence of chronic, insidious blood loss from long-standing esophagitis.4- Benign esophageal stricture; Fibrous strictures develop as a consequence of long-standing esophagitis.5- Gastric volvulus; Occasionally a massive intra-thoracic hiatus hernia may twist upon itself.
Investigations Young patients who present with typical symptoms of gastro-esophageal reflux, without worrying features such as dysphagia, weight loss or anaemia, can be treated empirically without investigation.Investigation; Is advisable if patients present in middle or late age, if symptoms are atypical or if a complication is suspected.
Endoscopy is the investigation of choice. This is performed to exclude other upper gastrointestinal diseases which can mimic gastro-esophageal reflux, and to identify complications.Twenty-four-hour pH monitoring is indicated if, despite endoscopy, the diagnosis is unclear or surgical intervention is under consideration.
episodes of pain are noted and related to pH. A pH of less than 4 for more than 6-7% of the study time is diagnostic of reflux disease. a slim catheter with a terminal radiotelemetry pH-sensitive probe above the gastro-esophageal junction.
Management Lifestyle advice; including weight loss, avoidance of dietary items which the patient finds worsen symptoms, elevation of the bed head in those who experience nocturnal symptoms, avoidance of late meals and giving up smoking. Antacids and alginates; also provide symptomatic benefit. H2-receptor antagonist drugs; also help symptoms without healing esophagitis.
Proton pump inhibitors; are the treatment of choice for severe symptoms and for complicated reflux disease. Anti-reflux surgery; Patients who fail to respond to medical therapy, those who are unwilling to take long-term proton pump inhibitors and those whose major symptom is severe regurgitation.
OTHER CAUSES OF ESOPHAGITIS Infection; Esophageal candidiasis , Herpes simplex virus , Cytomegalovirus (CMV) ,and HIV infection .Corrosives; Strong household bleach or battery acid .Drugs; Tetracyclines, potassium preparations, nonsteroidal anti-inflammatory drugs, iron sulfate, and the bisphosphonate alendronate.
Candida esophagitis is often associated with oral thrush and tends to present with dysphagia and only mild pain on swallowing. It has a characteristic appearance on endoscopy, and esophageal brushings and biopsies demonstrate fungal hyphae. Treatment with oral fluconazole is generally very effective.
Herpes simplex virus causes multiple esophageal ulcers and presents clinically with severe odynophagia. Acyclovir is the treatment of choice for herpes esophagitis
Cytomegalovirus (CMV) also causes esophageal ulceration and odynophagia. Endoscopy usually demonstrates a single large ulcer in the distal esophagus, and biopsies often detect viral inclusions that confirm the diagnosis. Both ganciclovir and foscarnet are effective treatments for CMV esophagitis.
MOTILITY DISORDERS PHARYNGEAL POUCH; Incoordination of swallowing within the pharynx leads to herniation through the cricopharyngeus muscle and formation of a pouch.ACHALASIA OF THE OESOPHAGUS OTHER ; Diffuse esophageal spasm, and 'Nutcracker' esophagus .SECONDARY CAUSES ; systemic sclerosis , Dermatomyositis, rheumatoid arthritis and myasthenia gravis .
episodic chest pain which may mimic angina, but is sometimes accompanied by transient dysphagia. Some cases occur in response to gastro-esophageal reflux. Treatment is based upon the use of proton pump inhibitor drugs when gastro-esophageal reflux is present. Oral or sublingual nitrates or nifedipine may relieve attacks
ACHALASIA OF THE OESOPHAGUS Pathophysiology; Achalasia is characterised by: A hypertonic lower esophageal sphincter which fails to relax in response to the swallowing wave. Failure of propagated esophageal contraction, leading to progressive dilatation of the gullet.Cause; Is unknown. Abnormal nitric oxide synthesis within the lower esophageal sphincter. Degeneration of ganglion cells within the sphincter and the body of the esophagus occurs. Loss of the dorsal vagal nuclei within the brain stem. Chagas disease.
Clinical features Usually develops in middle life; Dysphagia develops slowly, and is initially intermittent, it is worse for solids and is eased by drinking liquids, and by standing and moving around after eating. Episodes of severe chest pain due to esophageal spasm('vigorous achalasia'). Nocturnal pulmonary aspiration develops.Predisposes to squamous carcinoma of the esophagus.
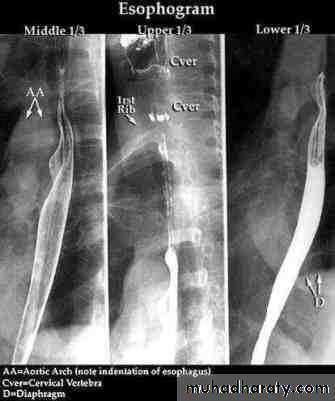
Investigations Chest X-ray; widening of the mediastinum, aspiration pneumonia.A barium swallow; tapered narrowing of the lower esophagus, esophageal body is dilated, aperistaltic and food-filled.Endoscopy; must always be carried out, carcinoma of the cardia can mimic the presentation and radiological and manometric features of achalasia ('pseudo-achalasia').Manometry; confirms the high-pressure, non-relaxing lower esophageal sphincter with poor contractility of the esophageal body.
Management Endoscopic Forceful pneumatic dilatation improves symptoms in 80% of patients. Some patients require more than one dilatation, injection of botulinum toxin into the lower esophageal sphincter. Surgical myotomy ('Heller's operation') with anti-reflux procedure. Proton pump inhibitor therapy is also often necessary. Because it may be complicated by gastro-esophageal reflux.
OESOPHAGEAL STRICTURE ;CAUSES; Gastro-esophageal reflux disease Webs and rings Carcinoma of the esophagus or cardia Extrinsic compression from bronchial carcinoma Corrosive ingestion Post-operative scarring following esophageal resection Post-radiotherapy Following long-term nasogastric intubation
TUMOURS OF THE OESOPHAGUS BENIGN TUMOURS; gastrointestinal stromal tumour (GIST)CARCINOMA OF THE ESOPHAGUS; 1-Squamous cancer; rare in Western, common in Iran, parts of Africa and China, mostly in upper 2 third of the esophagus. AETIOLOGICAL FACTORS; Smoking Alcohol excess Chewing betel nuts or tobacco Coeliac disease Achalasia of the esophagus Post-cricoid web Post-caustic stricture Tylosis (familial hyperkeratosis of palms and soles)
2-Adenocarcinoma; In Western populations , in the lower third of the esophagus from Barrett's esophagus or from the cardia of the stomach.
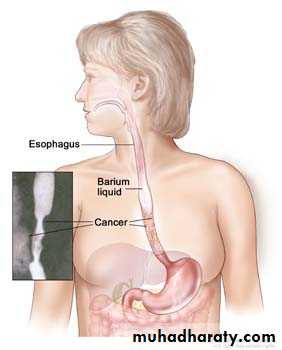
Clinical features Progressive, painless dysphagia for solid foods.In late stages weight loss is often extreme.Chest pain or hoarseness suggests mediastinal invasion.Fistulation between the esophagus and the trachea or bronchial tree; pneumonia and pleural effusion. Metastatic spread is common.
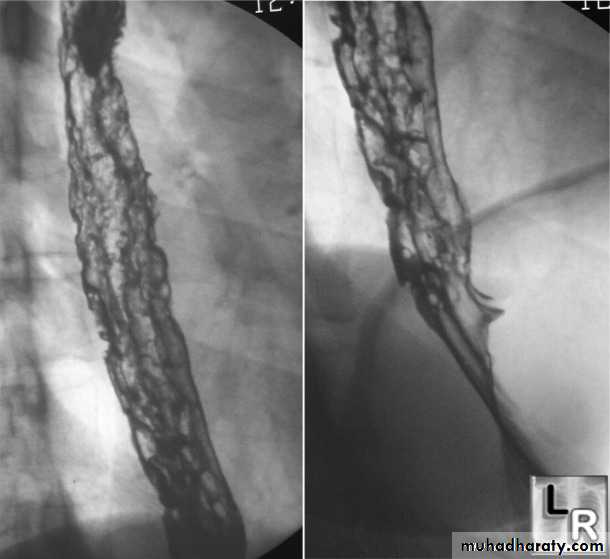
Investigations Endoscopy; The investigation of choice, with cytology and biopsy.Barium swallow ; site and length of the stricture .Thoracic and abdominal CT Endoscopic ultrasound (EUS)
Management Esophageal resection; overall 5-year survival rate is 6-9%. 70% of patients have extensive disease at presentation.Neoadjuvant (pre-operative) chemotherapy with agents such as cisplatin and 5-fluorouracil.Radiotherapy; squamous carcinomas are radiosensitive.
Palliative treatment;
Relief of dysphagia and pain, laser therapy.
Insertion of stents.
Radiotherapy to shrink tumour size.
Nutritional support.
Analgesia.