Benign diseases of the uterus
Benign dis. of the uterus can be classified in terms of the tissue of origin:The uterine cervix
the endometrium
the myometrium.
The endometrium :
1.endometrium polyps:-
Symptomes :
May cause abnormal bleeding, especially intermenstrual bleeding
Investigations :
Transvaginal ultrasound.
Sonohysterography
Hysteroscopy
Endometrial biopsy
Curettage
Treatment :
Medications: such as progestins or gonadotropin-releasing hormone agonists.the symptoms will return after the medications are stopped.
Hysteroscopy to remove any polyps that are found.
Curettage : to scrape the lining and remove any polyps
A hysterectomy:in cases where cancer cells are found in the uterine polyps.
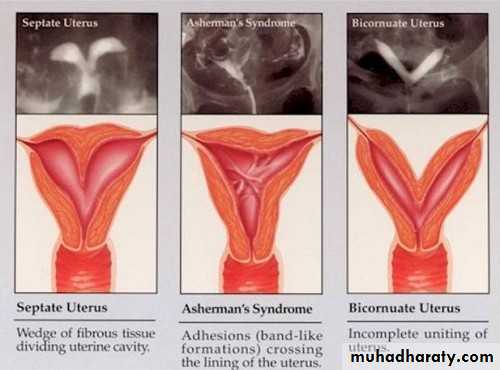
2.Asherman`s syndrome:-
It is the process of adhesion of anterior and posterior layers of the uterine wall caused by removal of basalis layer after agressive curetage following labour or abortion.
Symptoms : amenorrhea or oligomenorrhea.
Diagnosis: HSG
Treatment: by hysteroscopy lysis of the adhesion and put IUCD or gave high dose of estrogen.
Myometrium:
Uterine fibroids :-Pathology:
A fibroid is a benign tumor of uterine smooth muscle, termed a leiomyoma.
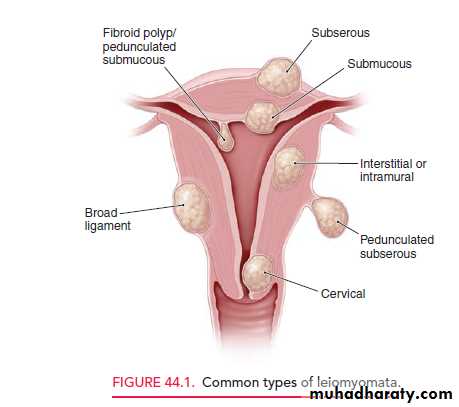
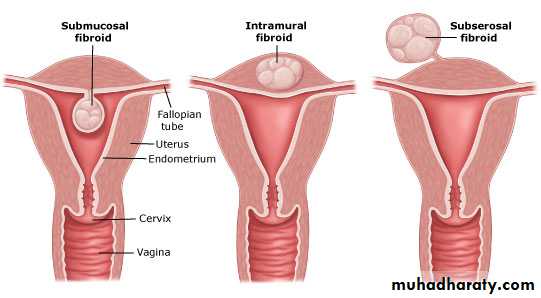
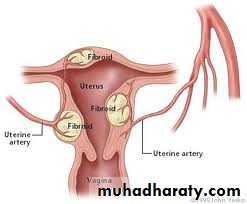
Classification :
Submucous leiomyoma
Pedunculated submucous
Intramural or interstitial
Subserous or subperitoneal
Pedunculated abdominal
Parasitic
Intraligmentary
Cervical
Fibroids are often described according to their location in the uterus :
Clinical features:-
Fibroids being detectable clinically in about 20% of women over 30 years of age.
Abnormal uterine Bleeding
Pelvic pressure & pain
Reproductive Dysfunction
Risk factors
Nulliparity
Obesity
positive family history
African racial origin
OCP
depot DMPA injections may be associated with reduced risk
Common presenting complaints :
1.menstrual disturbance;Menorrhagia may occur, it is likely that only submucous fibroid distorting the endometrial cavity and increasing the surface area
Dysmenorrhoea
2.pressure symptoms especially;
Nerves pressure:backache
Bladder— frequency / retention /Difficulty in micturition /Incomplete bladder emptying / incontinence
Ureter— Unilateral ureteral obstruction; hydroureter, hydronephrosis
Bowel—constipation/tenesmus. / difficult defecation can caused by large posterior fibroid
Vessels: Varicosity or edema of the lower extremities.
3.Pain is unusual. Uncomplicated uterine fibroid usually do not produce pain.
Acute pain is usually caused by either
torsion of pedunculated fibroid
Red degeneration of fibroid
extrusion from the uterus (In submucous fibroid; the uterus contracts to try to deliver the fibroid through the cervical os)
Associated endometriosis
Adhesions to other organs.
Malignant changes(sarcomatous change)
Other Rare clinical manifestations:
myomatous erythrocytosis syndrome: result from excessive erythropoietin production by the kidneys or by the leiomyomas themselves, in either case, red cell mass returns to normal following hysterectomy.
pseudo-Meigs syndrome: Meigs syndrome consists of ascites and pleural effusions that accompany benign ovarian fibromas. However, any pelvic tumor including large, cystic leiomyomas or other benign ovarian cysts can cause this.from discordancy between the arterial supply and the venous and lymphatic drainage from the leiomyomas. Resolution of ascites and hydrothorax follows hysterectomy.
Complications of fibroids :1.Torsion of pedunculated fibroid2.Degenerations:
1.Red degeneration :
5% of pregnant women with fibroids, undergo red degeneration
DDX. :
Appendicitis
twisted ovarian cyst
placental abruption
ureteral stone
pyelonephritis
Symptoms and sighs :
sudden onset of focal pain and tenderness on palpation localized to an area of the uterus
low-grade fever
vomiting
Investigations:
leukocytosis
raised ESR
Ultrasound
Treatment : is treated conservatively
Bed rest and observation
Analgesia to relieve pain.
Sedatives
Antibiotics: If required
Most often, acut symptoms subsid within a 3-10 days, but inflammation may stimulate labor.
Surgery is rarely necessary during pregnancy.
2.Hyaline degeneration : the most common type
3.Cystic degeneration
4.Infection of a leiomyoma
5.Mucoid degeneration
6.Atrophy
7.Fatty degeneration
8.Calcification of leiomyomas :is a common finding in postmenopausal patients. May be detected incidentally on an abdominal X-ray.
3.Malignancy: Leiomyosarcoma: occur in less than 0.1-0.5%.
Sarcoma may be suspected clinically when a leiomyoma, usually in a postmenopausal woman, becomes painful and tender and grows rapidly, producing systemic upset and pyrexia.4.Hemorrhage – It can be intracapsular or intraperitoneal due to rupture of surface veins of a subserous fibroid
5.Rare paraneoplastic complications – polycythemia, thromboembolism, hypoglycemia, hypokalemia
6.Inversion of uterus
7.Pregnancy related complications:
Effect of the fibroid on the pregnancy:
Infertility
Less successful results with in vitro fertilization in patients who have large submucosal fibroids.
ectopic pregnancy
Abortion and premature labor:
Malposition and malpresentation of the fetus
Obstructed labour
Cesarean section
placental abruption
Red degeneration
Torsion of a pedunculated fibroid.
Postpartum hemorrhage, inertia of uterus &delayed involution.
Myomectomy not done during pregnancy because bleeding may be profuse, resulting in hysterectomy.
Rupture of myomectomy scar during pregnancy
Effects of pregnancy on fibroid :
Red degeneration
Increased size in 20 to 30% cases
Torsion of a pedunculated fibroid, may cause gradual or acute symptoms of pain and tenderness.
Infection during puerperium
Expulsion
Necrosis
Abdominal examination
firm mass arising from the pelvis
on bimanual examination the mass is felt to be part of the uterus, usually with some mobility.
Pelvic examination.
uterine enlargement
The shape of the uterus is usually asymmetric and irregular in outline
The uterus is usually freely movable unless concomitant pelvic disease exists such as endometriosis or pelvic adhesions.
Differential diagnosis:-
pregnancyOvarian tumor
Adenomyosis
Malignancy :(eg. Ca.endometrium,choriocarcinoma,Leiomyosarcoma)
pelvic kidney
Investigations:-
CBC: indicate anemia if there is clinically significant menorrhagia.
Ultrasonography/Doppler ultrasound
Used to assess
uterine dimension
leiomyoma location,size, growth
Adnexal anatomy.
Detect hydroureter and hydronephrosis in the patient with marked uterine enlargement.
Sonohysterography or intrauterine infusion of sterile saline at the time of ultrasound examination identify the presence of :
pedunculated submucous fibroid
endometrial polyps.
Hysteroscopy or hysterosalpingography
- in the evaluation of patients with uterine fibroid and infertility or recurrent pregnancy loss.
5. Magnetic resonance imaging (MRI): used to exclude other DDX. Including adenomyosis and adnexal masses.
6. Imaging of the renal tract
7. Clinical suspicion of sarcoma will be an indication for needle biopsy or, urgent laparotomy.
Treatment:-
Treatment decisions are based on
Symptoms
fertility status
uterine size
rate of uterine growth
1.Expectant management(Conservative management)-
Indication :
In the absence of pain, abnormal bleeding, pressure symptoms
Size <12 weeks (of pregnancy size)
The patient near menopause, at which time the leiomyomas will atrophy as estrogen levels fall.
observation with periodic examination is appropriate
Bimanual examinations every 3 to 6 months
Follow-up with pelvic ultrasound or MRI
Endometrial biopsy if abnormal bleeding.
Regular blood counts: iron deficiency anemia is common with menorrhagia, and iron replacement may be required
2.Medical treatment
Non-hormonal options: such as NSAIDs (e.g. mefenamic acid) and antifibrinolytics (e.g. tranexamic acid) are limited at treating symptoms of dysmenorrhea and heavy, prolonged bleeding and anemia.Hormonal options include :
combined oral contraceptive pills,progestins(medroxyprogesterone acetate, Mirena IUD, norethindrone acetate)
mifepristone
androgenic steroids(danazol and gestrinone)
gonadotropin-releasinghormone (GnRH) agonists
Antiprogesterones (Mifepristone): effective in shrinking fibroids at a low dose
3.Surgery
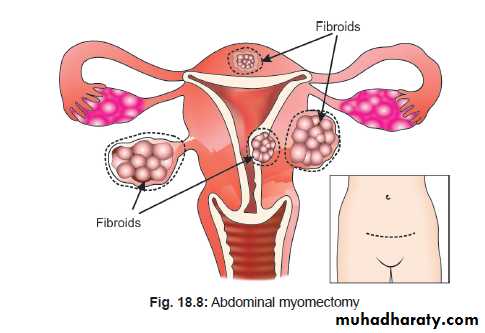
Myomectomy
involves the removal of single or multiple fibroid while preserving the uterus.
Indications for myomectomy :
Large myomas (especially the submucosal or intramural type)
Any symptomatic fibroid (persistent uterine bleeding despite medical therapy, excessive pain or pressure symptoms)
Unexplained infertility with distortion of the uterine cavity by fibroid
Recurrent pregnancy wastage due to fibroid.
When IVF is indicated (especially if the myoma results in the distortion of the uterine cavity)
Types of myomectomy (may be done by)
LaparotomyLaparoscopy
Hysteroscopy
vaginaly
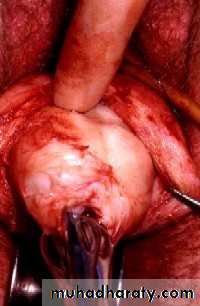
1.Abdominal myomectomy
Risks of this procedure include
Bleeding
prolonged operative time
increased postoperative hemorrhage compared to hysterectomy
It may be necessary to open the uterine cavity to remove intramural or submucous fibroid completely. This is a risk factor for future uterine rupture and an indication for cesarean section in future pregnancies
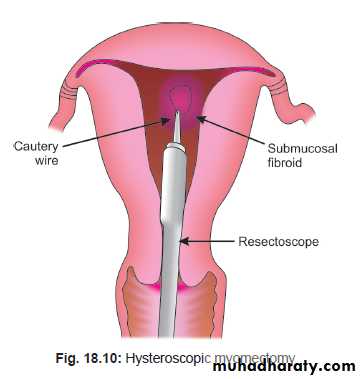
2.Hysteroscopic resection
submucous fibroid
3.laparoscopic myomectomy
Used for removing subserosal fibroids& intramural fibroid
4. vaginal myomectomy: in submucos pedenculated fibroid
2.Hysterectomy
Indications for hysterectomy :Asymptomatic fibroid of such size that they are palpable abdominally and are a concern to the patient
Excessive uterine bleeding
Pelvic discomfort caused by myomata
Patient complete her family and wishes for amenorrhea
Other treatment options (medical, myomectomy, UAE, etc) have failed or contraindicated
Rapid increase in size
Ultrasound features suggestive of sarcoma
4. Destruction of the fibroids
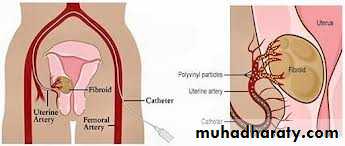
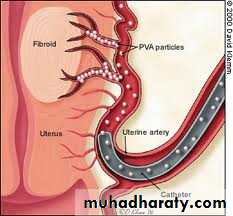
1.Uterine artery embolization (UAE)
By occludes the vessel feeding the uterus and leiomyomas, depriving the tumors of their vascular supply and causing shrinking or necrosis and death of the leiomyomas.Used:
approaching menopause
no longer desire fertility
have a large uterus
have multiple health risks for surgery
The most common complication
vaginal dischargeinfection
premature ovarian failure
Amenorrhoea
Treatment failure
Failed canulation of uterine artery
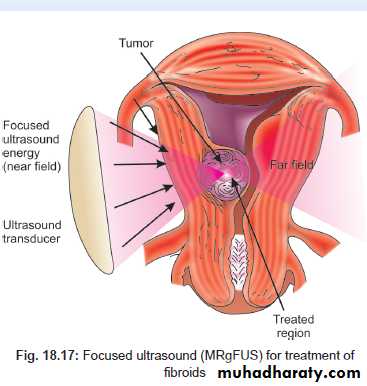
2.MRI-guided focused ultrasound fibroid ablation:
is a new procedure involves a focussed ultrasound energy beam using MRI to plot where the fibroids are located.
The beam heats the fibroids which results in local necrosis and subsequent shrinkage