Fifth stage
PsychiatryLec-21
د. الهام الجماس
26/3/2017
Child Psychiatry (2)Emotional disorders
Important differences between the disorders in adult & children:Some subtypes are different (separation anxiety)
Medications is rarely used
Equal male &female ratio(1/2in adult)
Most affected children do not become affected adults
SEPERATION AXIETY DISORDERS
Among 5-11 yr olds 3-4%have excessive, prolonged anxiety when faced with separation Older children may describe being harmful that the person will be harmed & not return can begin at the time of stress ,such as after a death or tragedy Some parents are noted to be very protectiveSymptoms of anxiety in children:
Behavioral
Clinging to parent
Unwilling to leave house
Unwilling to go to bed
Actions designed to avoid feared events (hiding)
Psychological
Feeling worried
Nightmares
Physical
Abdominal pans
Headaches
Managements:
Explanation& reassuranceIdentifications& resolution of stressors
Ensuring that the parents are not reinforcing the problem
Use specific interventions for secondary problems such as school refusal
Applying behavioral techniques
Somatoform disorder
Obsessive compulsive disorderMood disorders
School refusal
School refusal is not a psychiatric disorder, but is a common cause of child psychiatrist & frequently attributable to an emotional disorders.
Not attending school
Child not at home[-----------------] child remaining at home
Child kept at home ^ child reluctant to go to school (school refusal)
Social travel phobia
Fear of school
Separation anxiety
Social withdrawal
School refusal Truancy
Younger<11yr old older than 11yrUnderlying emotional disorders underlying conduct dis.
Good academic & behavioral record poor sch. Records
Good prognosis poor prognosis
Parents overprotective &anxious broken home
Management
Rapid return to school before avoidance is too ingrained Address any specific fears or stresses.Treat any associated psychiatric disorders.
Prognosis:
Younger children –good
Slightly increased risk of anxiety disorder in adulthood.
Conduct disorder
Conduct disorder is the commonest psychiatric disorder of childhood adolescence
Sex ratio=5/1(B/G)
Diagnosis usually made after age of 7yr
Conduct is disturbed & antisocial well beyond the range misbehavior normally observed.
Clinical features of conduct disorders:
preschool children
Aggressive behavior
Poor concentration
In mid childhood
LyingStealing
Disturbed & oppositional behavior bullying
In adolescence
StealingTruancy
Promiscuity
Substance misuse
Vandalism
Reckless behavior
Conduct disorder is associated with social deprivation, & poor parenting.Individual factors Brain damage,epilepsy, specific reading disorder.
Long term prognosis is poor
Management is a mixture of punishment & treatment
Attention deficit hyperactivity disorder
Prevalence =2% in UK (3/4boys)Etiology: genetic contribution, increased rate of depressive disorders, learning difficulties, alcoholism, antisocial personality disorder,neurodevelopmental disorder.
(Rare) social deprivation, food allergyFeatures: hyperactive, poor attention & concentration,distractable& impulsive, poor planning & organization.
Associated with: learning difficulties clumsiness low self-esteem, socially disinhibited,no localizing neurological signs, 50% coexist with conduct disorder
Management:
Support for the child & the familySpecific educational approaches (attention& learning difficulties)
Behavior modification
Stimulant (methylphenidate), careful about addiction & growth retardation
Prognosis variable---1/3 resolve completely.
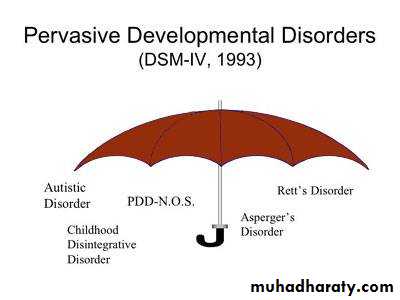
Pervasive Developmental Disorders
Group of disorders characterized by abnormalities in communication and social interaction and by restricted repetitive activities and interest.Most cases manifest before 5 years.
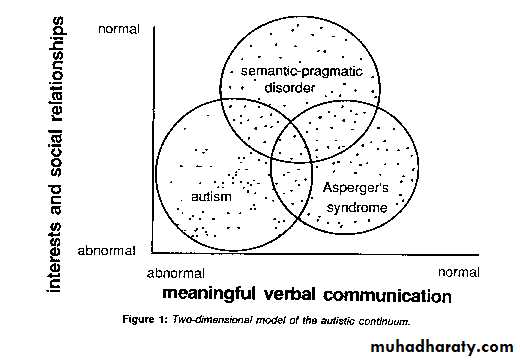
Autistic Disorder
Childhood autism (ICD-10)Autistic Disorder ( DSM-IV)Abnormal development apparent before the age of 3 years.3 kinds of social development:
Abnormality of social development.
Abnormality of communication.
Restriction of interest and behavior.
Pervasive developmental disorders(AUTISM)
Is characterized by failure to develop normal communication (social emotional).They have restricted use of language, seems oblivious to nonverbal communication& emotional expressionHave limited solitary, repetitive behavior& resist attempts to change their routine
80% boys 1 in 2500 children age of onset <3 years autistic triad
Autistic aloneness
Impaired language & communication
Solitary repetitive behavior
Failure to develop Associated with:Mannerism & rituals, epilepsy in 25%, MR In75%
Etiology; genetic, no environmental risk factor
Neuropath logical involvement of the cerebellum&Oliveary nuclei has been reported
Prognosis: poor
Needs special school & residential care.
PTSD
Epidemiology
The lifetime prevalence ~ 8%
Among high-risk groups ~ 5 to 75%
Significantly higher in women
First-responders like firemen, and police officers are at risk for PTSD-particularly when children are involved, research suggests. Likewise, journalists covering catastrophes are similarly susceptible to PTSD. Taken together, the DSM indicates about 5% of American men and 10% of American women have the disorder.
The most severe stresses resulted in the occurrence of the syndrome in more than 75% of the victims
Comorbidity
About 2/3 have at least two other disorders like: depressive disorders, substance-related disorders, other anxiety disorders, and bipolar disorders.
Etiology
Biological Factors
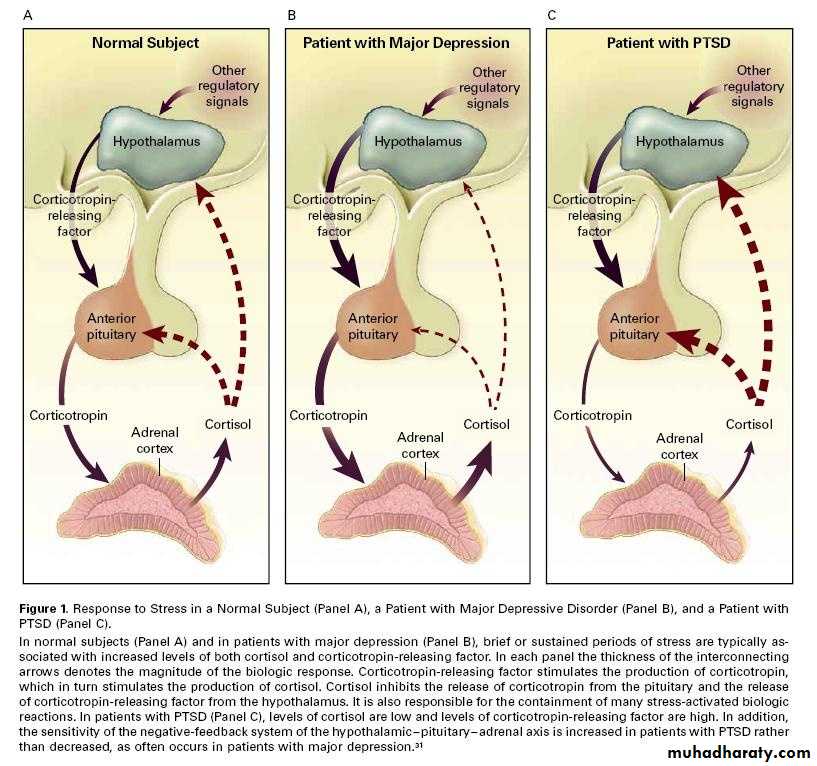
HPA axis
Etiology biological factors (brain imaging)
Faced with scores of traumatized veterans of the Viet Nam war, researchers have been studying the underlying physiology of PTSD since the late 1960s.Animal studies have shown repeatedly that prolonged stress releases hormones that can damage the hippocampus, a region of the brain associated with memory.
In a series of brain imaging studies conducted with humans in the mid-1990s, researchers found that the hippocampi of PTSD sufferers were smaller than average.
These findings lead some to hypothesize that the damage extreme stress does to the hippocampus causes PTSD; however, a study published in the October 2002 issue of Nature Neuroscience suggests otherwise.
The hippocampus, a region of the brain associated with memory, can be damaged by the prolonged release of stress hormones
Diagnosis
Clinical features divided into 3groups:
Hyper arousal (persistent anxiety, irritability, insomnia, and poor concentration)
Intrusions (intense intrusive imagery, flashbacks, and recurrent distressing dreams)
Avoidance (difficulty in recalling stressful events at will, avoidance of reminders of the events, detachment, inability to feel emotion “numbness”, and diminished interest in activities
Course and Prognosis
PTSD usually develops sometime after the trauma. The delay can be as short as I week and as long as 30 years. Untreated, ~30% recover completely, 40% continue to have mild symptoms, 20% moderate, and 10% remain unchanged or become worst.After 1 year 50% recover