Fifth stage
DermatologyLec-7
د.هيثم
30/3/2017
Basal Cell CarcinomaEpidemiology:
Most common human cancer(~80-90%)600,000 to 800,000 cases per year in U.S.
Male:Female 2-3:1
80% arise in head and neck
Age
Likelihood increases with age
BCCa over 40 years old
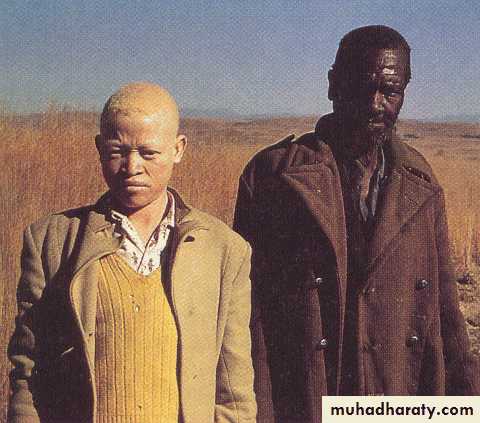
Race
Most often in light-skinned, rare in dark-skinned races
Etiology:
Ultraviolet radiation
ethnicity
ionizing radiation exposure
chemical exposure - arsenic
burns, scarring
immunosuppression
Basics of BCC:
Typically slow-growingRarely metastasizes (<0.1%)
Typically sporadic
No cellular anaplasia (a true carcinoma?)
Very low mortality
Significant morbidity with direct invasion of adjacent tissues, especially when on face or near an eye
Variants of Basal Cell Carcinoma:
SuperficialNodular
Micronodular
Infiltrating (5%)
Sclerosing/ morpheaform (5%)
Metatypical
Infundibulocystic
Nodulocystic
Adenoid
Clear cell
Follicular
Sebaceous
Perineurally invasive
Basal Cell Carcinoma – Subtypes:
Superficial
Single or multiple patches
Trunk
Indurated scaly
D/D- eczema, psoriasis tinea.
Nodular Ulcerative
Most common
Usually on the face
Small, slow growing
Firm
Telangectasias
Ulceration
Sclerosing (Morpheaform)
Yellow white plaques
Ill defined boarders
Most aggressive
Most likely to recur
Central sclerosis & scarring
Pigmented
Similar to nodular type
Deep brown pigmentation
Differential- malignant melanoma
FIBROEPITHELIOMAPINKUS TUMOUR
Raised
Moderately firm
Erythematous and smooth
Lower trunk (lumbosacral area)_
BCC - Syndromes
BASAL CELL NEVUS (GORLIN’S) SYNDROMEAD, no sex linkage, low penetrance
? Mutated tumour suppressor at Ch 9q23.1-q31
Childhood onset
BCC (average age 20y)
Pitting of palms and soles
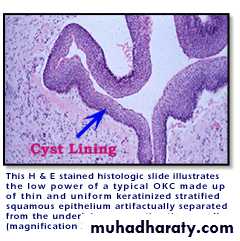
odontogenickeratocysts (epithelial jawline cysts)
CNS calcifications (dura), MROther Associated Syndromes:
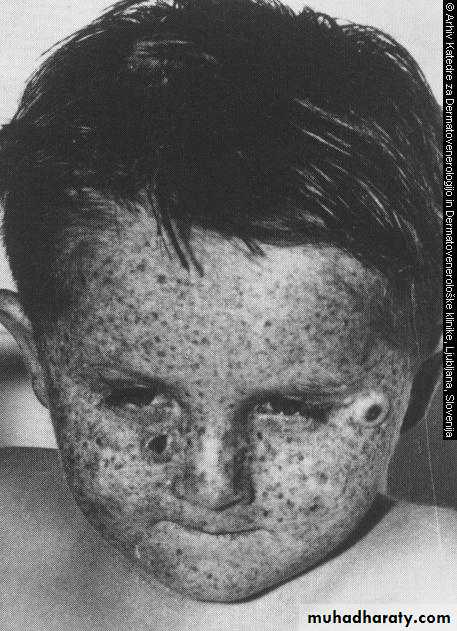
XERODERMA PIGMENTOSUMIncomplete sex-linked recessive
Deficiency of endonuclease
Childhood onset
Extreme sun sensitivity
BCC,SCC,Melanoma
ALBINISM
Genetic abnormality of the pigment system.
Basal Cell Carcinoma - Histopathology
Resemble normal basal cells
Hyperchromatic nuclei, scant cytoplasm
Clustered separate from stroma
Peripheral palisading
Desmoplastic reaction
Nests or in continuity
Clinical course:
Nodulo-ulcerarive type begins as a flesh coloured waxy nodule with telangectasia → enlarges → central ulceration → deepens → rolled out, beaded edges → destroys structures locally as deep as bone/ cartilage → aptly named rodent ulcer
Rare metastasis, but recurrence known after inadequate treatment
DIFFERENTIAL DIAGNOSIS:
CystInfected spot
Sebaceous hyperplasia
Naevus
Molluscumcontagiosum
Wart
Bowens disease
Tinea
Eczema/psoriasis
Malignant melanoma
Seborrhoeic keratosis
Erosions and leg ulcers
Treatment Options:
Electrodessication and curettageCurettage alone
Surgical excision
Mohs micrographically controlled surgery
Cryosurgery
Ionizing radiation
Surgical excision plus radiation
Imiquimod cream
Factors Considered in Treatment Planning:
Pt preference to keep eye
Pt age
Surgical excision-considered definitive tx
“Careful frozen section controlled excision of periocular BCCs yields cure rates comparable to Mohs micrographic surgery at 5-year follow-up”
5 year recurrence of 2.2% in one study
Therefore, avoiding exenteration was considered a good possibility