
1
Fifth stage
Pediatric
Lec. 1
.د
اروى
9
2 /3/2017
NEUROLOGY
Assessment
The process and interpretation of the neurologic examination vary with age. The
examination of a newborn is unique with transient and primitive reflex patterns. The
examination of an adolescent is similar to that of an adult.
Primary symptoms of neurological disease
Visual or hearing loss.
Impairment of swallowing or respiration.
Weakness.
Numbness or parasthesia.
Difficulty walking or talking.
Incontinence.
Deterioration in thinking.
Change in personality.
Seizures.
Headache and dizziness.

2
Congenital anomalies of the nervous system
Spina bifida:
It range in severity from simple defect at L5 or S1 vertebral arch, to major defect that
uncovered by skin or bone on baby's back(myelocele).or the defect involve the skull
(encephalocele).
Symptoms:
Total paralysis , loss of sensation in the legs , incontinence of bowel and bladder.
Meningocele :
The spinal canal and the cystic meninges are exposed but the spinal cord is functionally and
anatomically normal.
Prevention: folic acid
Macrocephaly and microcephaly
Macrocephaly : (large head )
1-Macrocrania-
2-Hydrocephalus-
3-Megalencephaly-
Microcephaly: (small head)
Is defined as a head circumference that measures more than 3 standerd deviations below
the mean for age and sex.
3
Etiology of microcephaly
1- familial : AD ,AR.
2-syndromes : Down , Edward, Cri-du-chat.
3- congenital infections : cytomegalovirus , rubella , toxoplasmosis.
4- drugs: fetal alcohol syndrome, radiation, meningitis / encephalitis .
5-hypoxic-ischemic encephalopathy.
CNS reflexes of infancy
Moro :start at birth disappear at 4 months
Grasp :
Rooting :
Placing :
Tonic neck:
Trunk incurvation:
Parachute: start at 6-8 months and never disappear.
Increased intracranial pressure(ICP)
A symptom of serious intracranial pathology and a cause of irreversible neurological injury.
The skull is rigid container ,brain accounts for 80-85% of volume, CSF 10-15%,blood 5-10%,
Brain herniation:
It occur when the brain shift in response to the continuing elevation of ICP
4
Etiology: mass lesion , hydrocephalus , brain swelling
Symptoms: headache ,vomiting , lethargy ,irritability ,6
th
nerve palsy , diplopia ,
papilledema .
Sign: bulging fontanel , suture diastasis , distended scalp veins , sun set eyes , rapid growth
of OFC.
Cushing triad :↑ICP ,↓pulse , irregular respiration.
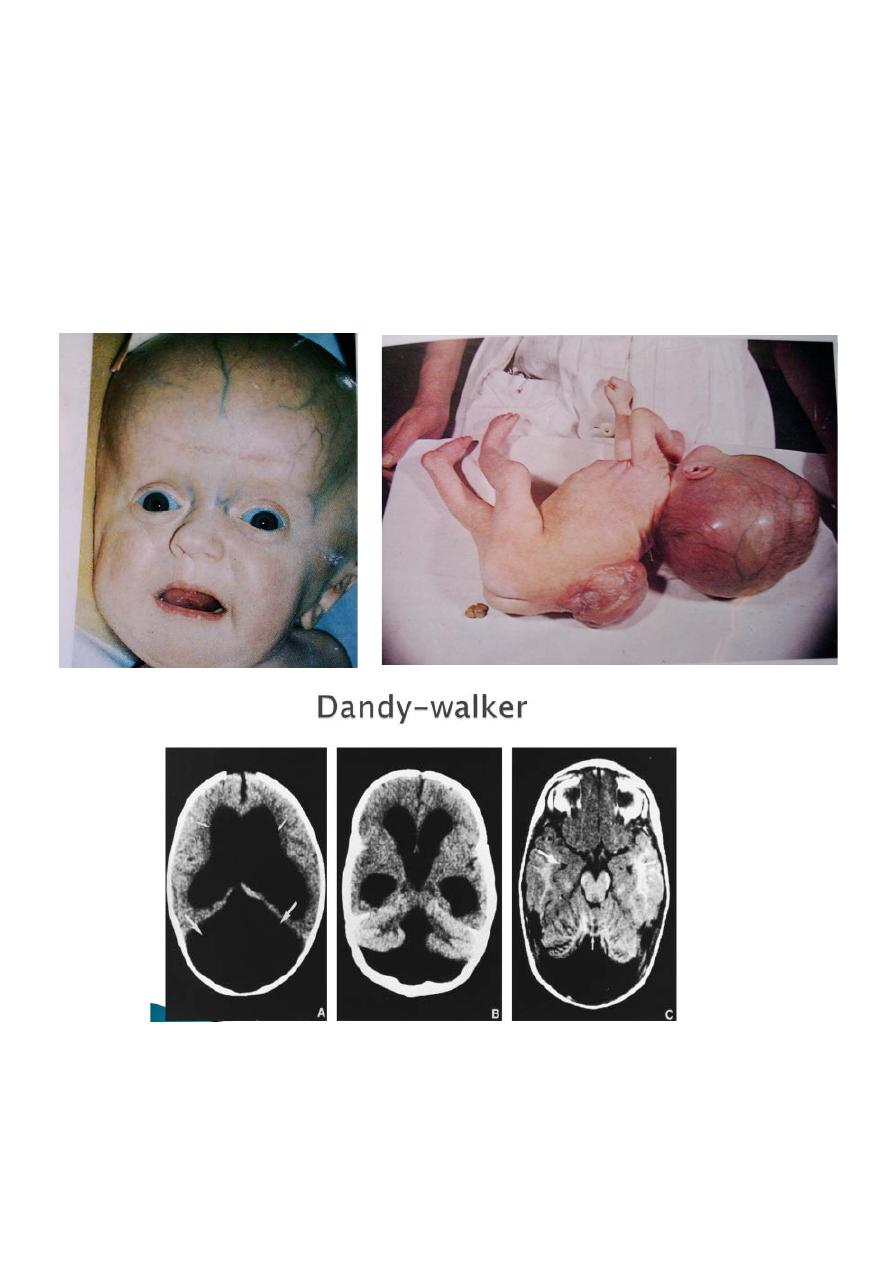
Hydrocephalus
Hydrocephalus is not a specific disease, it represents a diverse group of conditions that
result from impaired circulation and absorption of CSF or, in rare circumstance, from
increased production of CSF by a choroid plexus papilloma.
Physiology:
CSF is formed primarily in the ventricular system by the choroid plexus, which is situated in
the lateral , 3
rd
and 4
th
ventricles. In a normal child, about 20 ml /hr of CSF is produced. The
total volume of CSF approximates 50 ml in an infant and 150ml in adult.
Flow from lateral v →3
rd
V through foramen of Monro then through aqueduct of sylvius
→4
th
V then through foramen of Magendie and Luschka to the subarachnoid space.
Absorption: by arachnoid villi.
Etiology
Obstructive (noncommunicating)
1-congenital:
a- Arnold-Chiari malformation .
b-Dandy-Walker.
c- aqueduct stenosis.
2-mass lesions:
a- abscess
b- hematoma
c- tumors of neurocutaneous disorders
d- vein of Galen malformation

5
Non obstructive (communicating)
1- achondroplasia
2-beningn enlargement of subarachnoid space
3-choroid plexus papilloma
4-meningeal malignancy.
5-meningitis.
6-posthemorrhagic.
Clinical feature
1-symptoms&sign of ↑ICP.
2-ataxia&spasticity (lower limb)
3-endocrine dysfunction.
4-visual dysfunction.
5-˝sun set eyes˝.
6-dilated scalp veins.
7-widly opening fontanel.
8-rappid ↑in OFC by serial measures.
9- percussion of the skull might produce a cracked pot sound or McEwan's sigh.
Diagnosis
1-clinically
2-imiging :
* Plain skull films show separation of the sutures (beaten
-silver appearance)
*The CT scan and /or MRI along with the ultrsonography in an infant are the most
important studies to identify the specific cause and severity of hydrocephalus.
6
Treatment
1. Medical :
(Meningitis, subarachnoid Hr)
acetazolamide
2. Surgery :
-(cyst ,tumer ,AVM)
Removal.
-shunt placing.
7
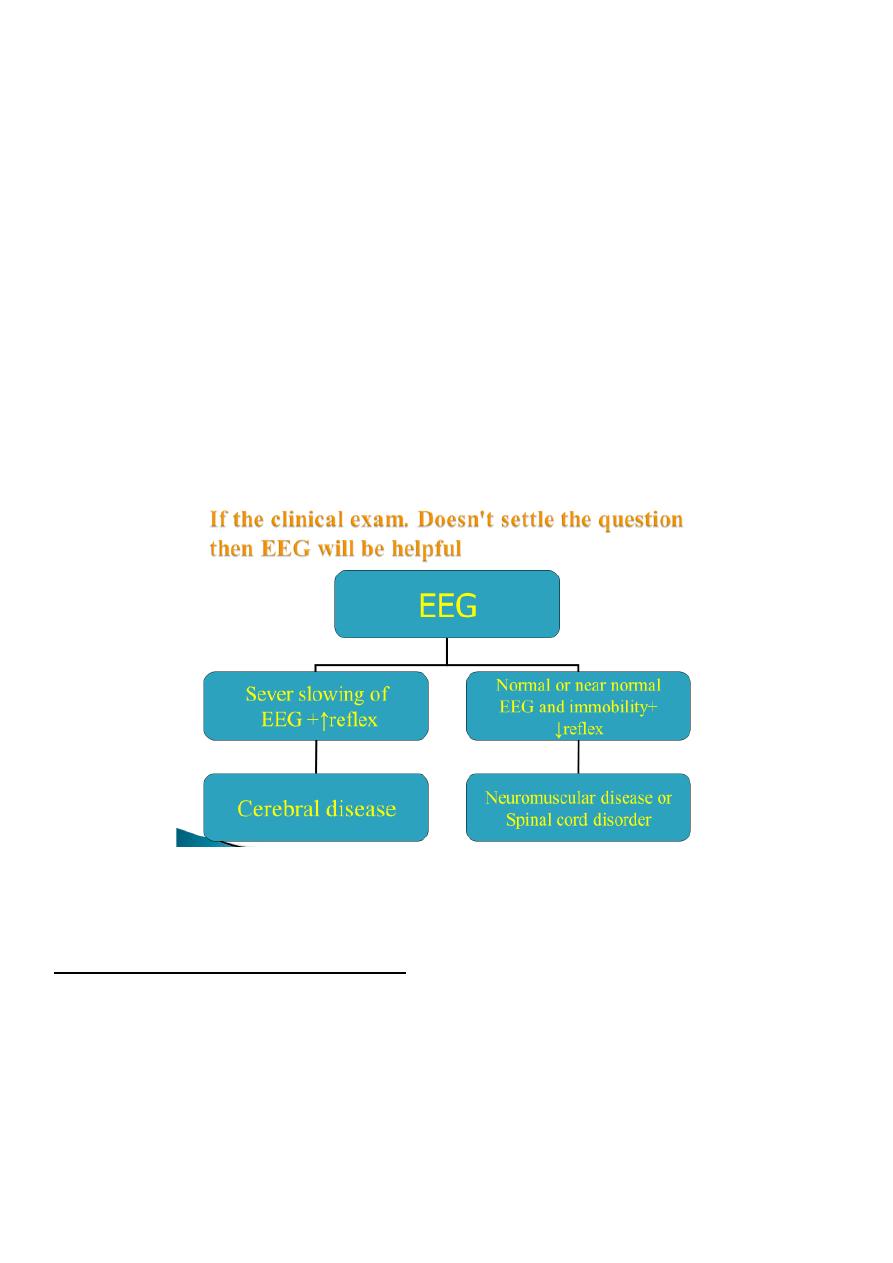
Floppy baby
Neonatal immobility:
The 1
st
step in evaluations of an infant who doesn't move spontaneously or in response to
stimuli is to determine whether awareness is intact ?
The cortical activity is intact if the baby is bright eyed able to follow and try to smile but is
unable to move .
If the face and eyes are immobile the problem is more difficult .
Clinical questions:
Does the infant response to :flashlight , bell , nasal cotton stimuli?
Does the eyes follow if the lids are lifted?
Are reflexes increase?
Etiology of neonatal immobility
Sever hypoxic ischemic encephalopathy:
Flaccidity
Areflexia
Complete ptosis
Ophthalmoplegia
Absent cornea l& gag reflex

8
Intoxication :
Mg sulfate
Barbiturate
Narcotics
Benzodiazepines
General anesthesia
Metabolic encephalopathy:
Hypoglycemia
Hyperbilirubinemia
Hypotonia without major weakness
*acute systemic illness.
*Mental retardation:
*Specific syndromes:
-Down syndrome
-Cerebrohepatorenal syndrome
-Kinky hair syndrome
-Prader-willi syndrome
*Connective tissue disorder:
-Ehlers-Danlos syndrome
-Marfan syndrome
*Nutritional-metabolic disease:
Rickets
Renal tubular acidosis
Celiac disease
Biliary Artesia
Congenital heart disease
*Benign congenital hypotonia:
Exhibit the condition at 9-12 months.
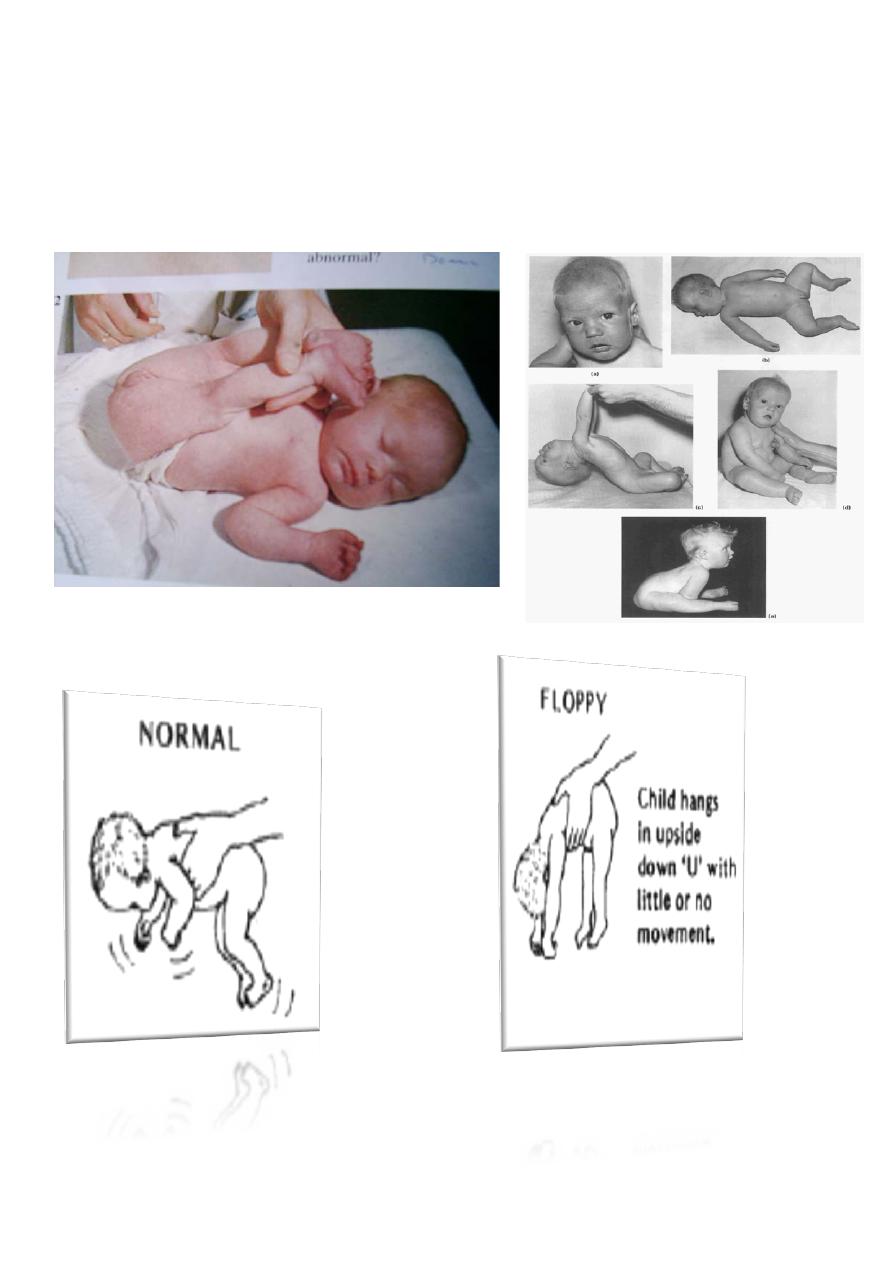
9
Delayed motor milestone.
Normal social , intelligence , fine motor movement.
Head lag , slip-through ventral suspension.
Complete lab. Investigation are necessary.
Most of children become normal by 3 yrs.
