1
Fifth stage
radiology
Lec-4
د.هديل
27/3/2017
G.I.T
Stomach & duodenum
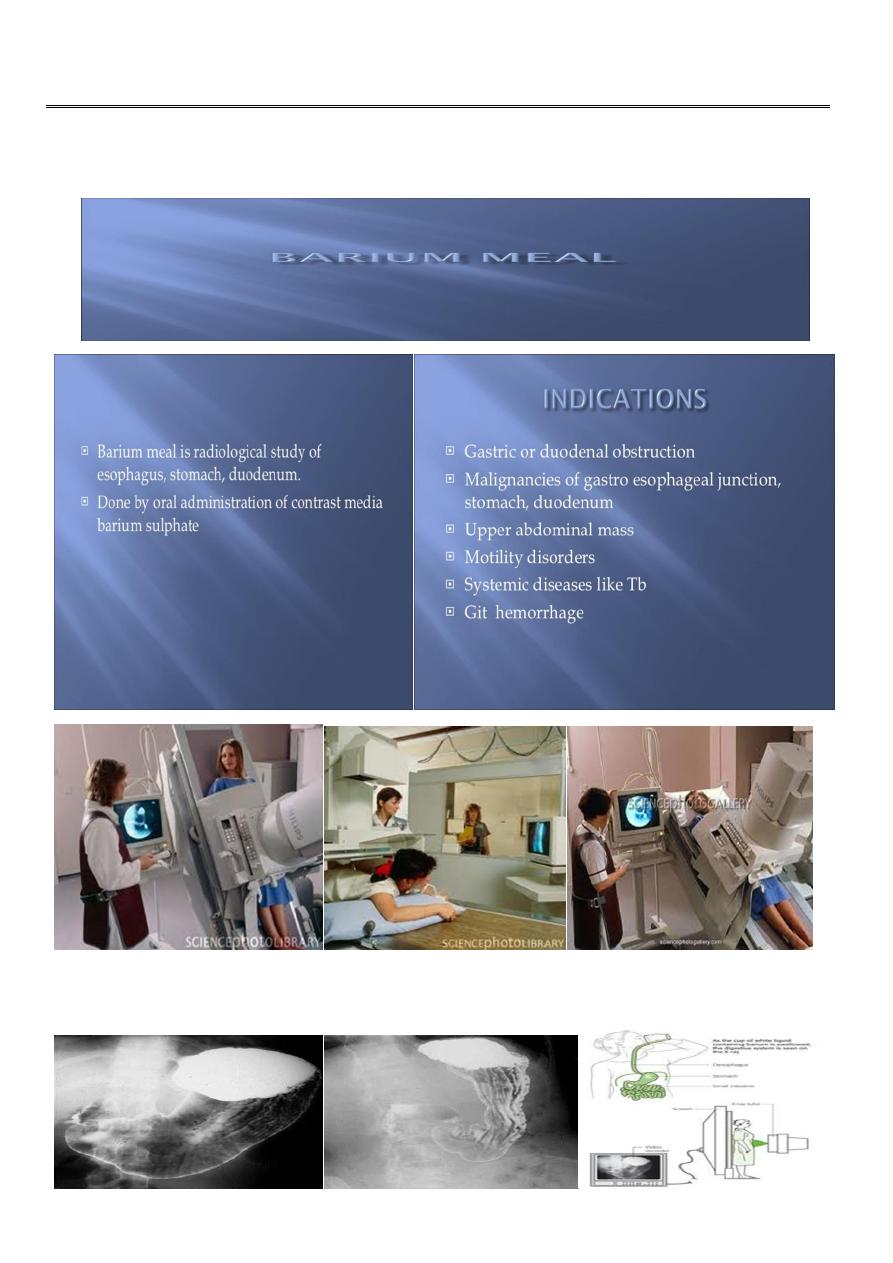
Barium meal
Fluoroscopy + spot films Preparation
2
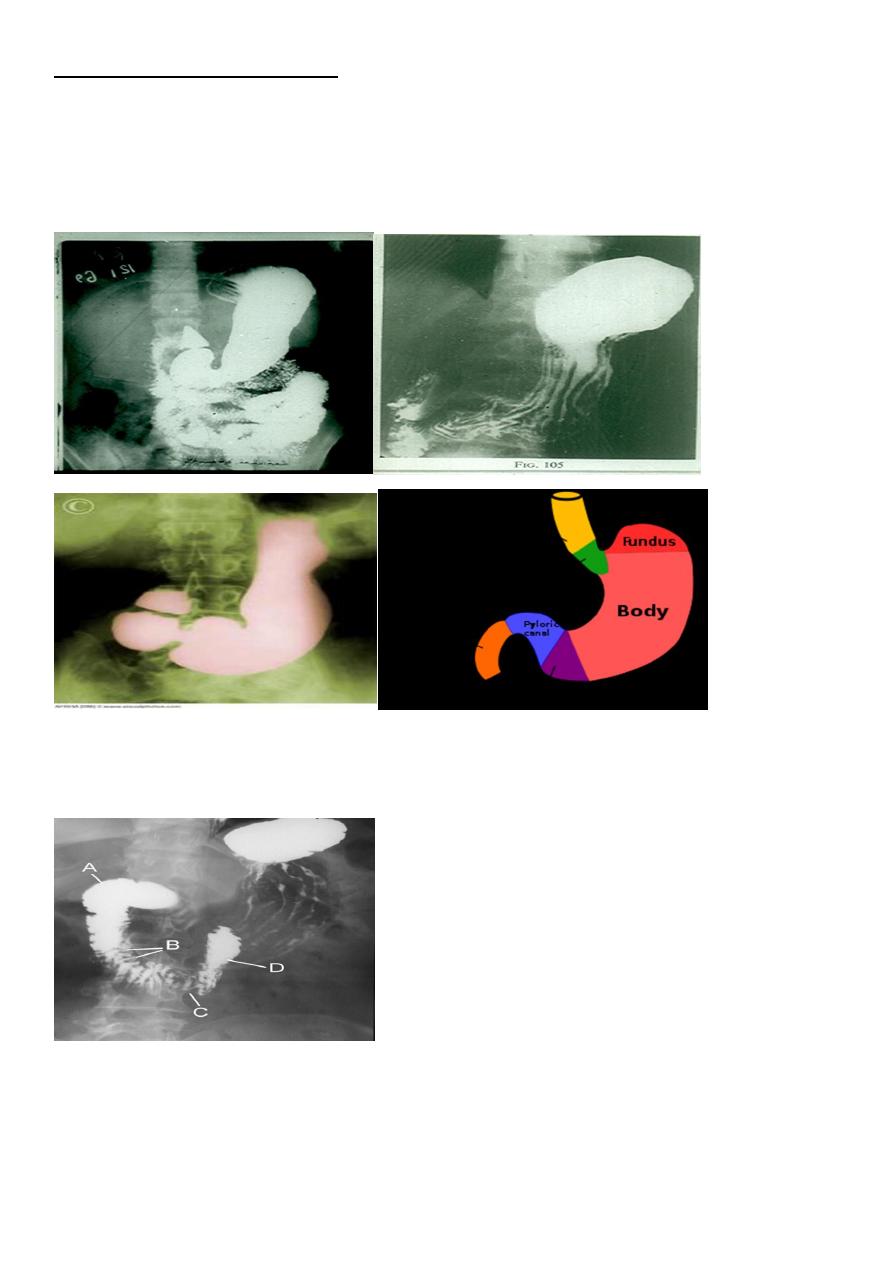
The Normal Anatomy of Stomach
1- Shape.
2-Size.
3-Site.
4-Anatomical parts.
5-Mucosal pattern.
Normal Anatomy of Duodenum
Duodenal cap.
Duodenal loop
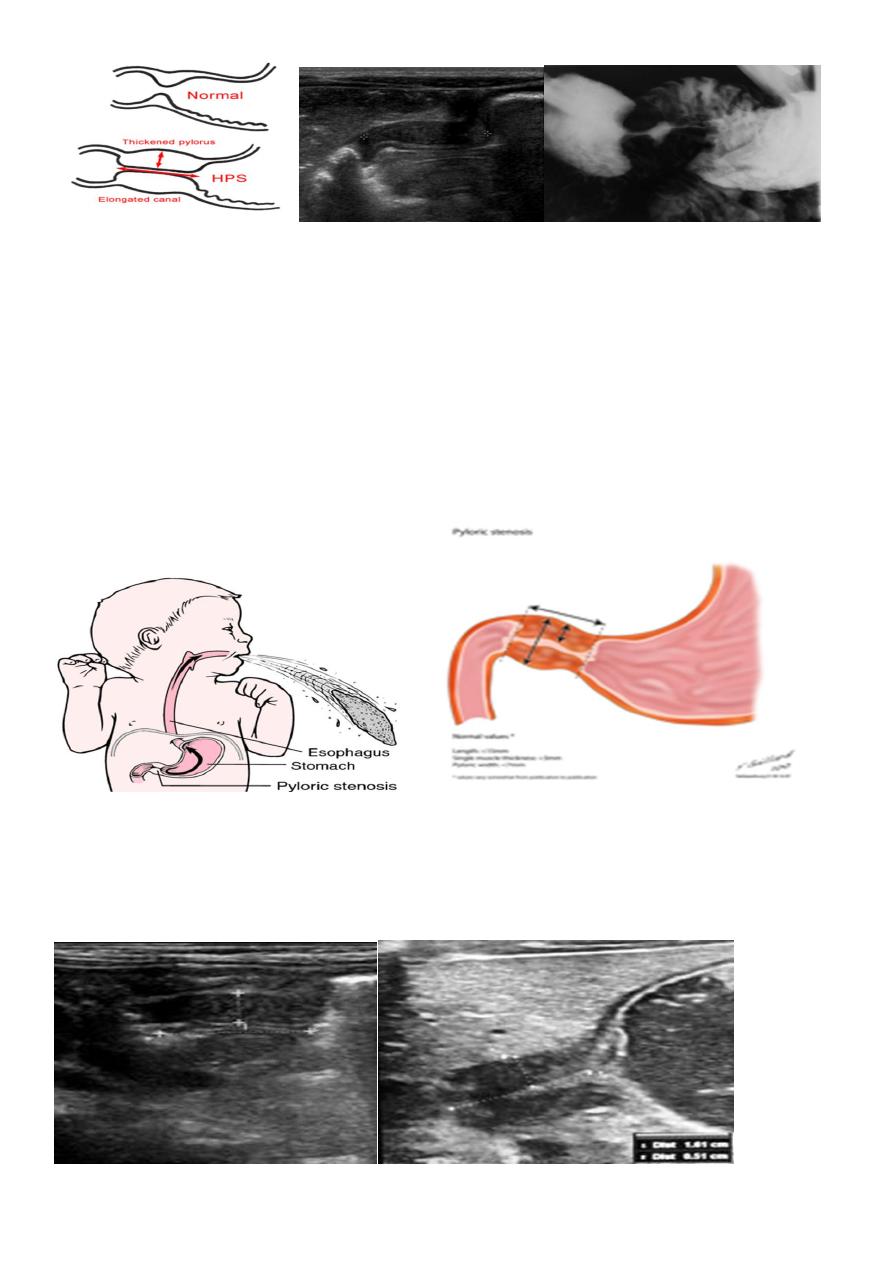
Hypertrophic pyloric stenosis
Cause:
A. Congenital type
B. Adult type
3
Hypertrophic pyloric stenosis refers to idiopathic thickening of gastric pyloric musculature
which then results in progressive gastric outlet obstruction.
Epidemiology
Pyloric stenosis is relatively common and has a male predilection (M:F ~ 4:1), and is
more commonly seen in Caucasians 4. It typically occurs between the 4-8 weeks of life.
There may be a positive family history. Incidence of hypertrophic pyloric stenosis is
approximately 2-5 per 1,000 births per year in most white populations,
In a normal situation, the pyloric muscle thickness (diame-ter of a single muscular wall on a
transverse image) should normally be less than 3 mm (most accurate 3) and the length
(longitudinal measurement) should not exceed 15 mm.
4
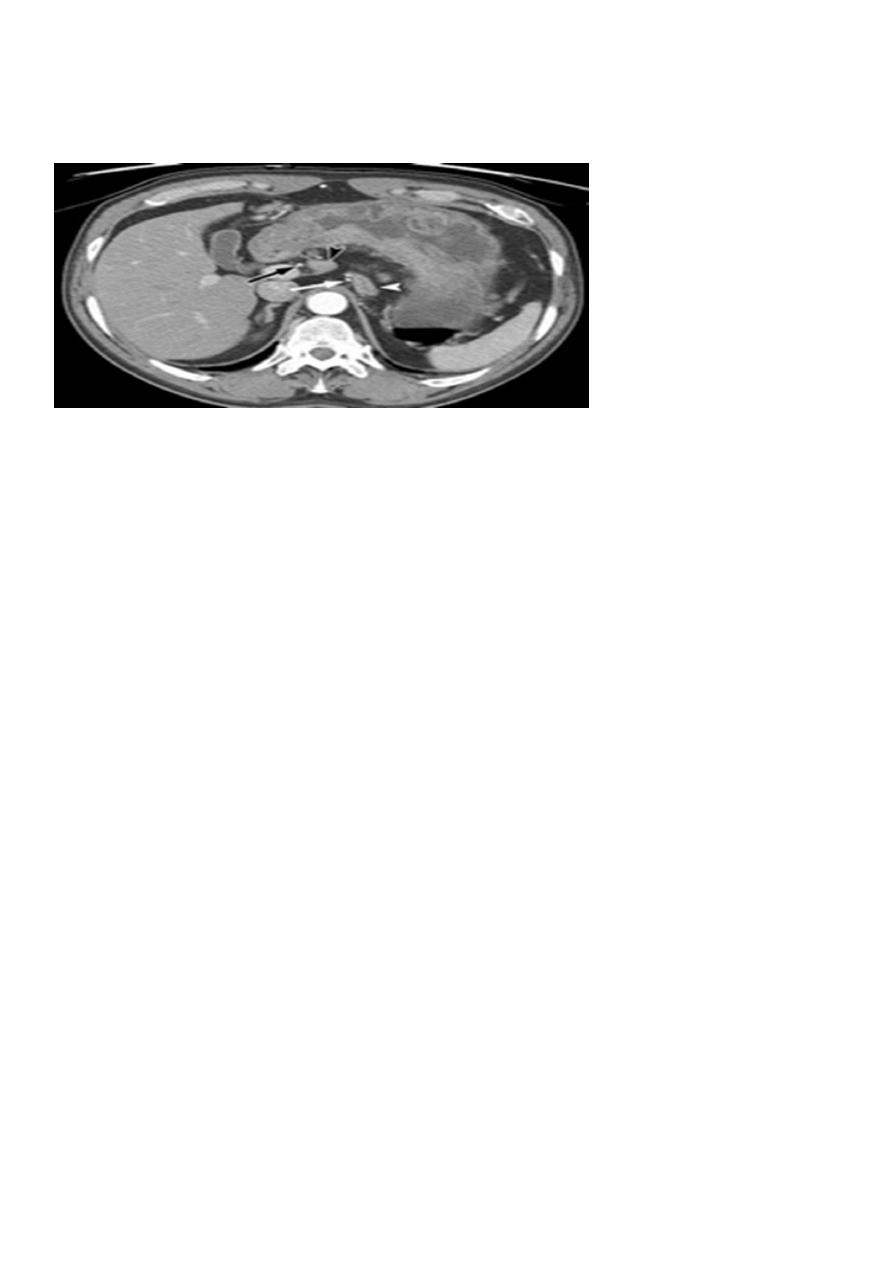
Gastric outlet obstruction (often abbreviated as GOO) is a medical condition where there is
an obstruction at the level of the pylorus, which is the outlet of the stomach. Individuals
with gastric outlet obstruction will often have recurrent vomiting of food that has
accumulated in the stomach, but which cannot pass into the small intestine due to the
obstruction. The stomach often dilates to accommodate food intake and secretions. Causes
of gastric outlet obstruction include both benign causes (such as peptic ulcer
disease affecting the area around the pylorus), as well as malignant causes, such as gastric
cancer.
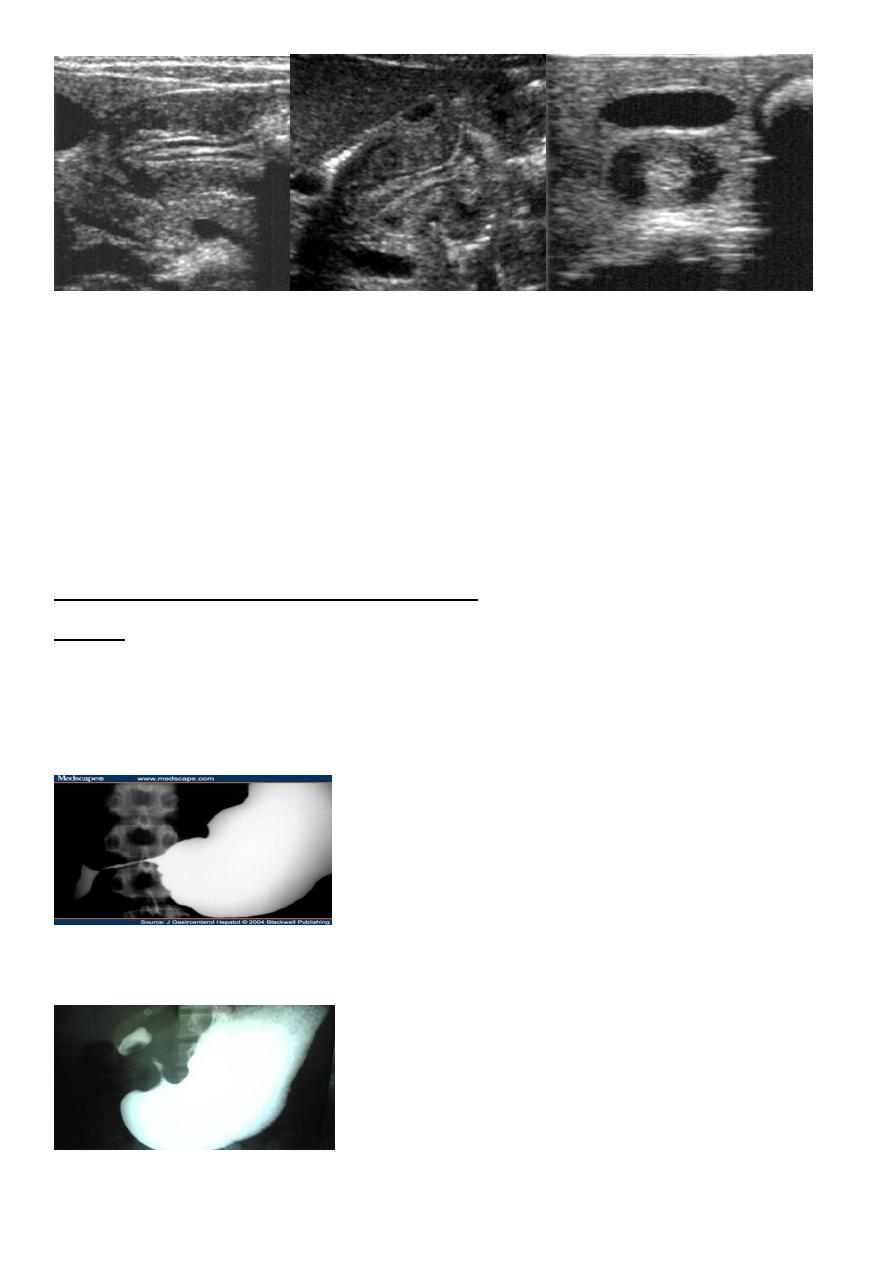
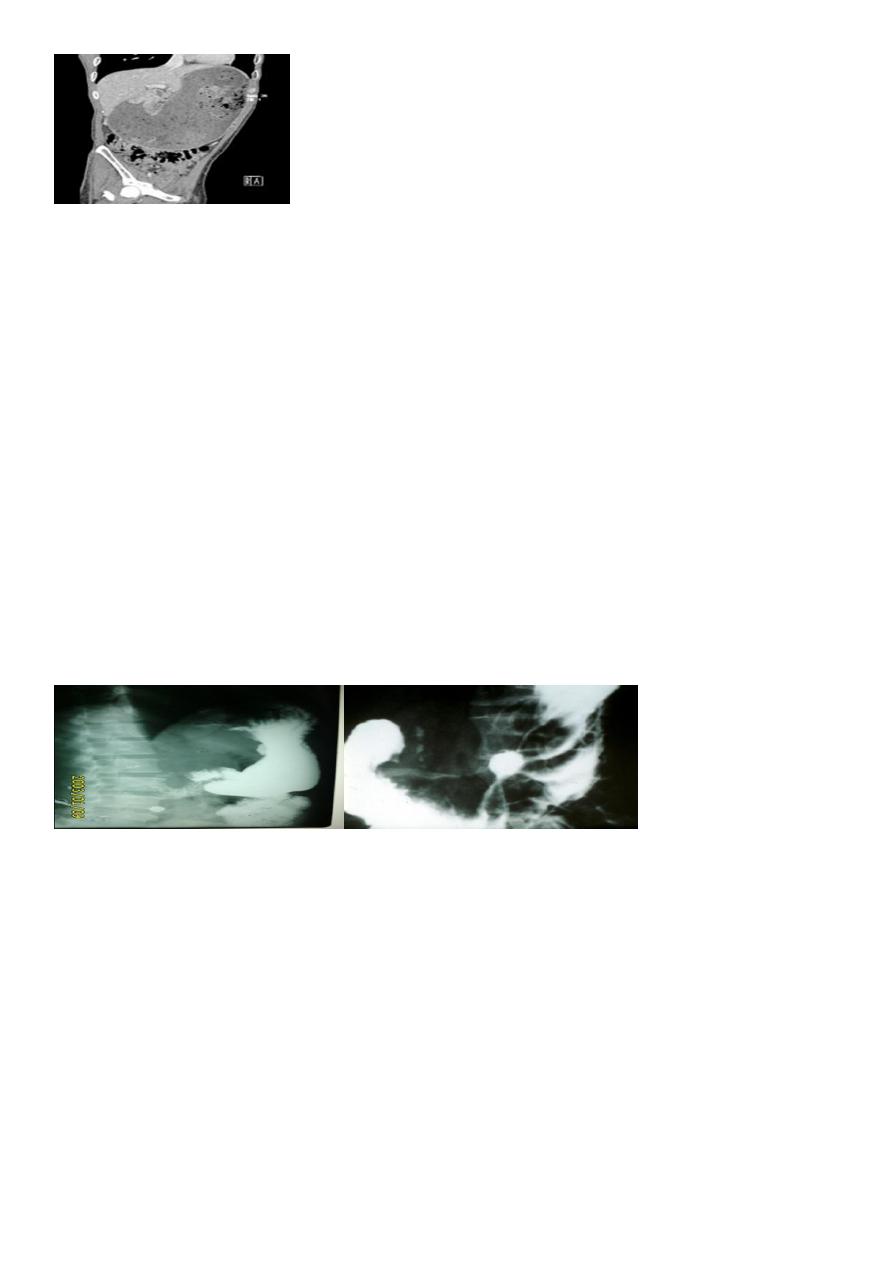
Radiographic Ba meal examination of the Pyloric
stenosis
1 .Marked dilatation of the stomach attends the pelvic cavity
2.Failure of passage of contrast into the duodenum.
3.Multiple filing defects are seen within the stomach due to retained food material .
Barium meal image of a case of corrosive-induced gastric outlet obstruction benign
narrowing.
GASTRIC CA
5
PEPTIC ULCER
GU, DU and IU.
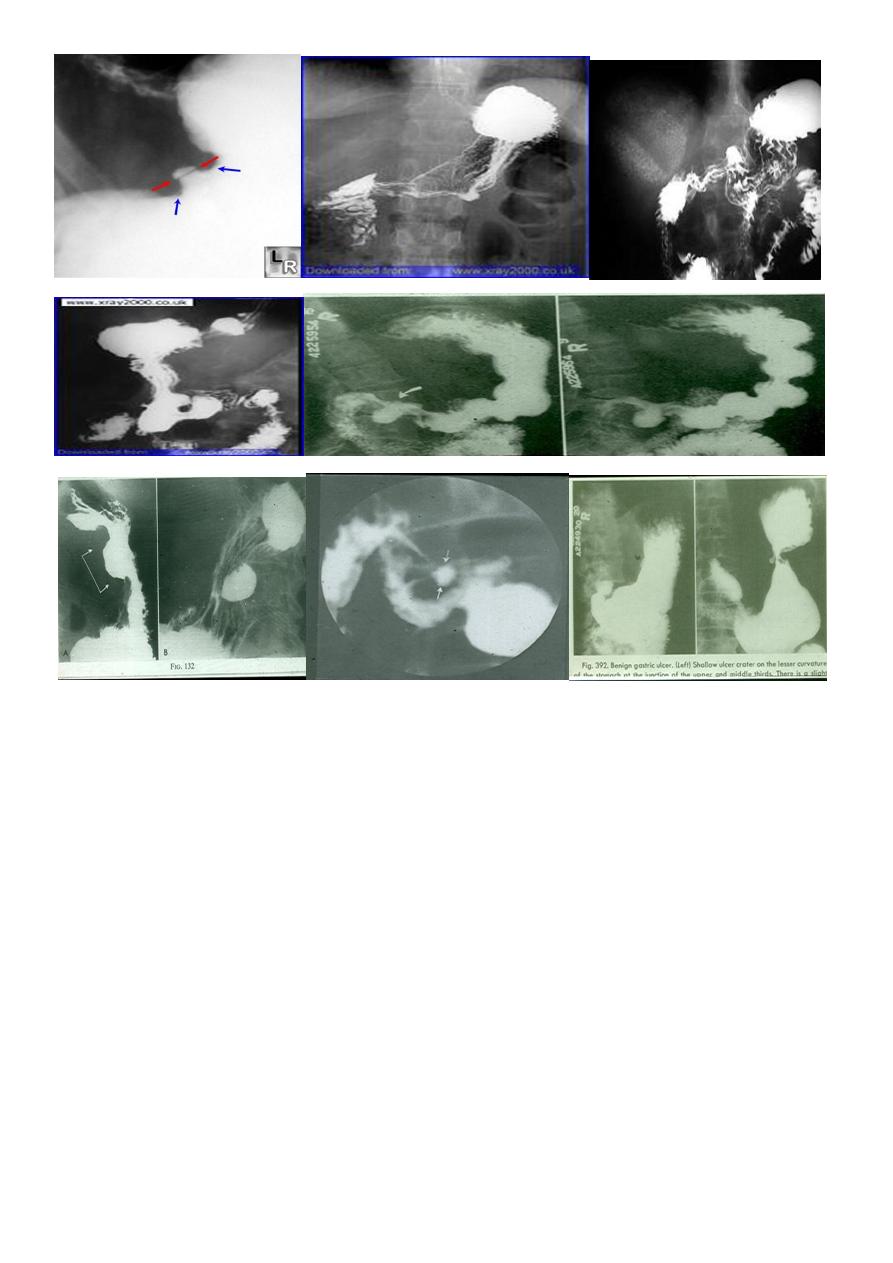
The Ba. meal findings are :
1-Direct signs :
* Ulcer crater ( nitch):
Either in enface or in profile
* Associated signs:
I. Spasm
II. Radiated mucosal folds.
III. Edema (Hampton's line).
2- Indirect signs :
I. Hyper peristaltic waves.
II. Companion B sign.
III. Thick mucosal folds & hyper peristaltic stomach
(angry mucosa)
Radiographic Signs of a benign gastric ulcer:
Ulcer crater-collection of barium on dependent surface which usually projects beyond
anticipated wall of stomach in profile (penetration)
Hampton’s line-1 mm thin straight line at neck of ulcer in profile view which represents the
thin rim of undermined gastric mucosa
lesser curvature gastric ulcer. Red arrows point to Hampton's Line, a thin, straight line at
neck of ulcer in profile view which represents the thin rim of undermined gastric mucosa.
The blue arrows point to the
ulcer mound, a smooth, sharply delineated soft-tissue mass surrounding a benign ulcer.
Note how the ulcer projects beyond the confines of the expected wall of the stomach.
6
Gastric carcinoma refers to a primary malignancy arising
from the gastric epithelium.
3presentation
Polypoidal
Infiltrative * localized * generalized
Ulcertaive type
barium meal presentation of the CA stomach
1.Carcinoma produce single or multiple irregular
filling defect with alteration of near by mucosal
Pattern
.
2.Localized or generalized narrowing of the stomach rigid in appearance with shoulding
sign on either sided aspect of the narrowing .
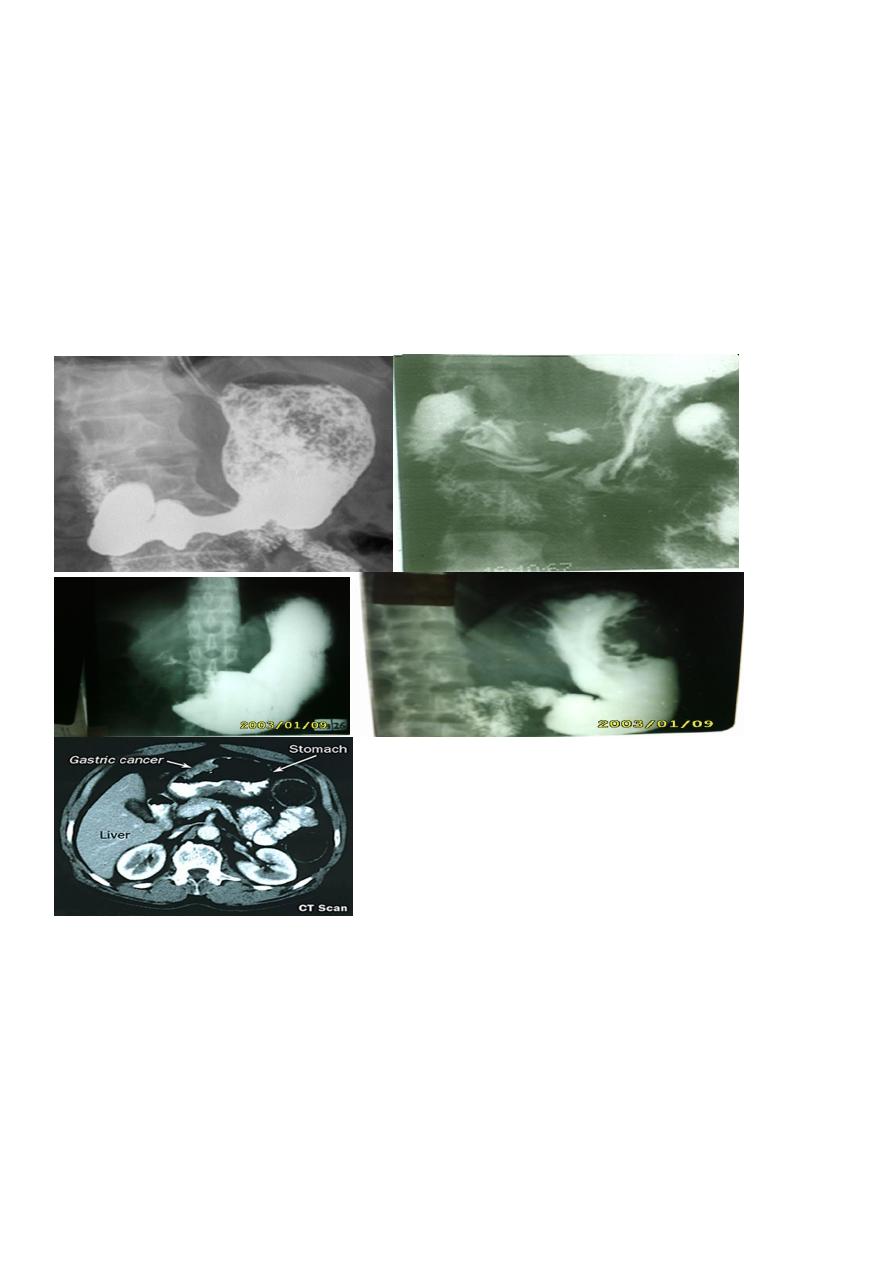
7
3- Ulcerative Ca Either :
I.Polypoidal tumour with ulceration or
II. Complicated benign gastric ulcer
on Ba. Meal :
* Filling defect with central ulcer crater
* No mucosal radiation , due to destruction .
* The ulcer crater is not projected out side the
lumen ( meniscus sign )
* Hour glass deformity ( X ) of stomach
Duodenal ulcers (DUs)
affect nearly 10% of the adult population at some time,[1]and these lesions account for two
thirds of all peptic ulcers, which are defined as mucosal breaks of 3 mm or greater; gastric
ulcer accounts for the rest
Most duodenal ulcers are depicted as round or ovoid pools of barium; about 5% may be
linear, and most are smaller than 1 cm in diameter. Giant duodenal ulcers, defined as those
>2 cm in diameter, have an increased risk of perforation, obstruction, and bleeding.
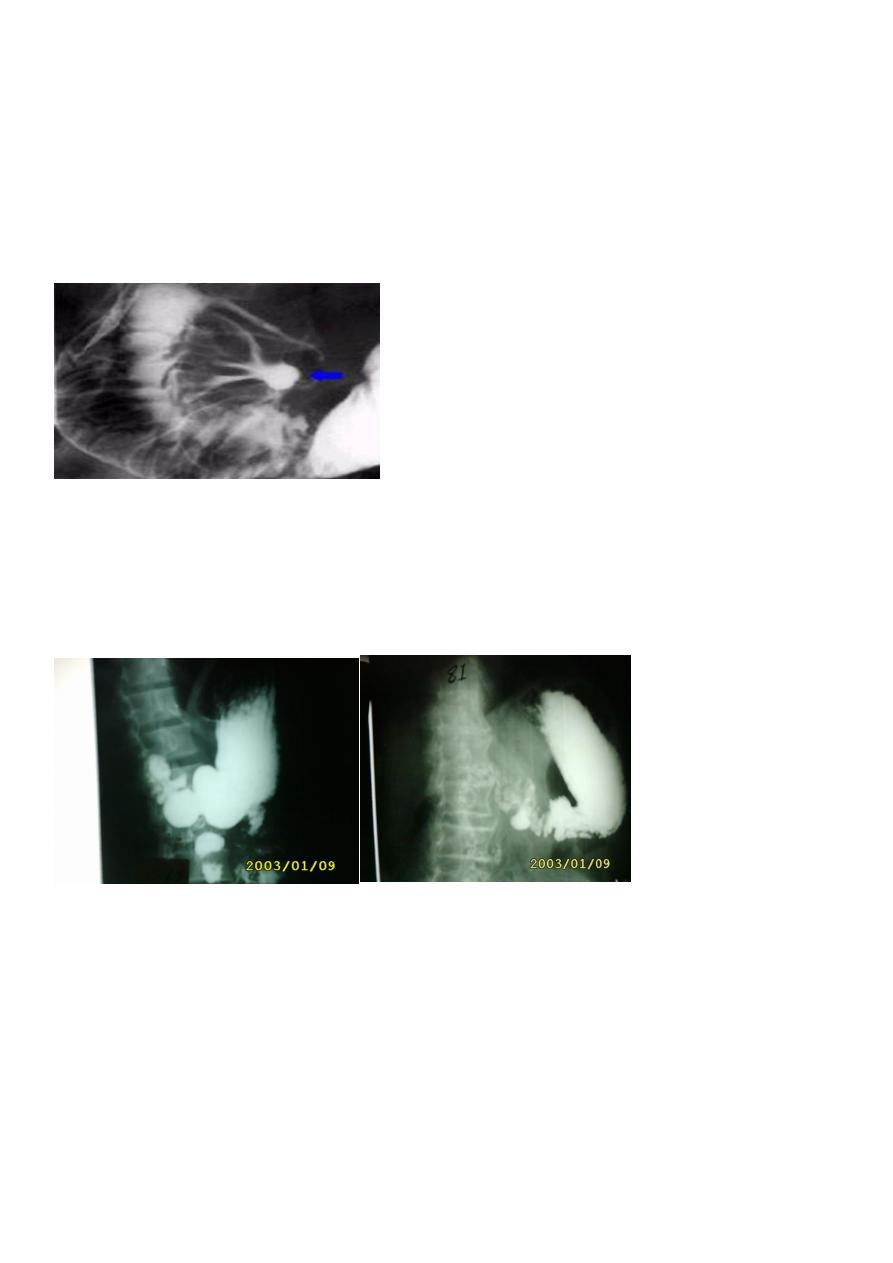
8
Multiple ulcers occur in about 15% of patients[1] ;Zollinger-Ellison syndrome should be
considered in these patients.
About 95% of duodenal ulcers occur in the duodenal bulb,[1] and the rest occur in the post
bulbar duodenum, bulber U which consists of the proximal 2 cm of the descending
duodenum above the ampulla of Vater. As many as half of all duodenal ulcers occur in the
anterior wall of the bulb.
Complicated Chronic DU
1-Tri foil deformity ( tri foil tree )
2-Pseudo diverticulum (Akerland diverticulum)
3-Gastric outlet obstruction.( pyloric obstruction ).
During Ba examination
� Bird's Beak deformity of lower oesophagus - Achalsia cardia (Barium Swallow)
� Cork screw oesophagus-- Diffuse oesophageal spasm (Barium Swallow)
� Commonest radiological
appearance of gastric
� Trifoliate duodenum - Chronic duodenal ulcer with scarring (Barium Meal)
� Hour Glass stomach - Peptic ulcer
� Single-bubble appearance - pyloric stenosis
� Double-bubble sign--Duodenal atresia, duodenal stenosis,
9
� Triple-bubble sign - Jejunal atresia
� Coiled spring appearance -Intussusception
