Fifth stage
DermatologyLec-14
د. عمر
18/4/2016
Light Related DisordersSunlight has profound effects on the skin and is associated with a variety of diseases.
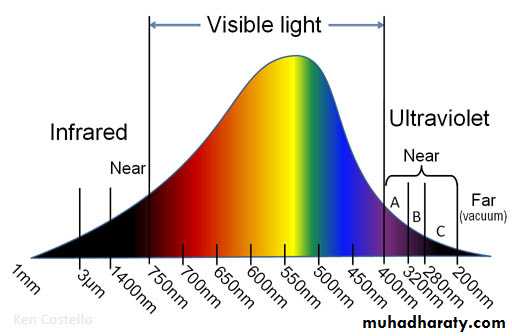
Ultraviolet (UV) light causes most photobiologic skin reactions and diseases.UV light is divided into UVA (320 to 400 nm), UVB (290 to 320 nm), and UVC (100 to 290 nm).
UVA is further subdivided into UVA I (long wave) and UVA II.
The ratio of UVA to UVB is 20:1, and two thirds of this UVA is UVA I.
More than 90% of UV radiation may penetrate clouds!!!
UV radiation generates reactive oxygen species that damage skin.
UVA
UVA causes immediate and delayed tanning and contributes little to erythema and burning.
Constant throughout the day and throughout the year.
The longer wavelengths of UVA can penetrate more deeply, reaching the dermis and subcutaneous fat.
Chronic exposure causes connective tissue degeneration (photoaging), photocarcinogenesis, and immunosuppression.
UVA augments the carcinogenic effects of UVB
UVA penetrates window glass and interacts with topical and systemic chemicals and medications.
It produces photoallergic and phototoxic reactions.
UVB
UVB 290- 320nmUVB produces the most harmful effects and is greatest during the summer.
Snow and ice reflect UVB radiation (decrease in winter).
UVB delivers a high amount of energy to the stratum corneum and superficial layers of the epidermis.
It is primarily responsible for sunburn, suntan, inflammation, delayed erythema, and pigmentation changes.
Chronic effects include photoaging, immunosuppression, and photocarcinogenesis.
It is most intense when the sun is directly overhead between 10 am and 2 pm.
UVB is absorbed by window glass.
Prior exposure to UVA enhances the sunburn reaction from UVB.
UVC
UVC is almost completely absorbed by the ozone layer and is transmitted only by artificial sources such as germicidal lamps.So what happens?
DNA is mutated by UVB.
Absorption of UVA leads to the release of reactive oxygen species.
These reactive oxygen species cause oxidation of lipids and proteins that affect DNA repair, produce dyspigmentation, and cause photoaging and carcinogenesis.
Normal Aging
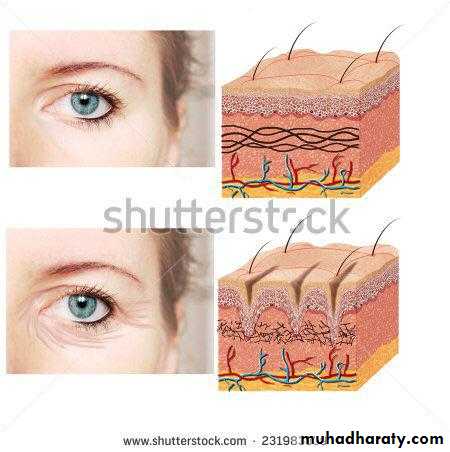
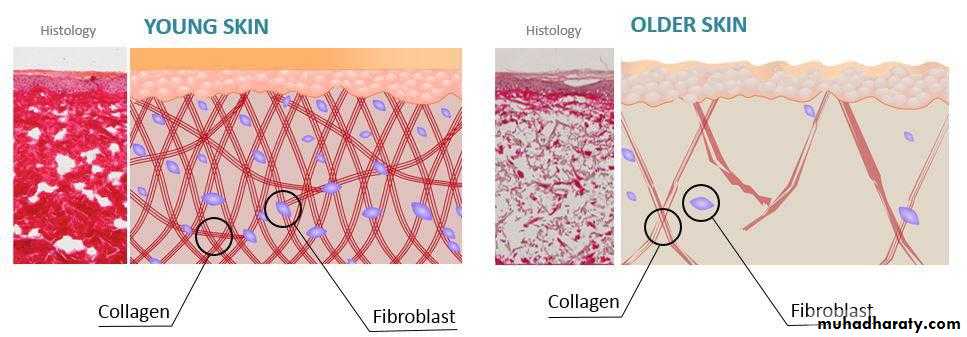
The skin begins to show signs of aging by ages 30 to 35.Aged skin is thin, fragile, and inelastic. The epidermis becomes thin.
There is a gradual loss of blood vessels, dermal collagen, subcutaneous fat, and the number of elastic fibers.
There is a reduction in the density of hair follicles, sweat ducts, and sebaceous glands, resulting in a reduction in perspiration and sebum production.
The skin becomes atrophic and fragile when subcutaneous tissue is lost.
Loss of elastic fibers results in fine wrinkles that disappear by stretching. The skin is easily distorted, but it recoils slowly.
Potent steroids should not be used on aged skin.
Photoaging
Photoaging refers to those skin changes superimposed on intrinsic aging by chronic sun exposure.Unprotected, chronically exposed children can acquire significant actinic damage by the time they reach 15.
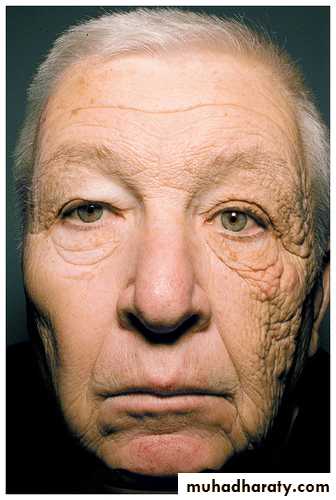
Sun-damaged skin is characterized by elastosis (a coarsening and yellow discoloration of the skin), irregular pigmentation, roughness or dryness, telangiectasia, deep wrinkling, follicular plugging, and a variety of benign and malignant neoplasms. The epidermis thickens.
Normal Aging
Normal AgingPhotoaging
Photoaging
Solar Elastosis
Is a sign highly characteristic of severe sun damageThere is massive deposition in the upper dermis of an abnormal, yellow, amorphous elastotic material that does not form functional elastic fibers.
This altered connective tissue does not have the resilient properties of elastic tissue.
Wrinkling becomes coarse and deep rather than fine, and the skin is thickened. These wrinkles do not disappear by stretching.
Sun-induced wrinkling on the back of the neck shows a series of crisscrossed lines that form a rhomboidal pattern (cutis rhomboidalis nuchae).
Reddish-brown, reticulate pigmentation with atrophy and telangiectasia is seen on the sides of the neck (poikiloderma of Civatte).
Slightly elevated seborrheic keratoses occur on the back of the hands and may be misdiagnosed as solar lentigines.
Blood vessels diminish in number, and the walls of the remaining vessels become thin. Bleeding occurs with the slightest trauma to the sun-damaged surfaces of the forearms and hands but not to the unexposed surfaces. Fragile sun-damaged skin is easily torn and heals with haphazard scars called stellate pseudoscars.
Actinic comedones. Open and closed comedones are present in the periorbital areas. Acne-like inflammation does not occur.
Actinic comedones may become very large but can easily be expressed with a comedone extractor.
Actinic comedones
Actinic comedonesTreatment of photoaging:
Photoaging is treated with either topical treatments (tretinoin cream) or resurfacing through chemical peels, dermabrasion, or lasers.Sun protection: Sunscreens are topical agents that absorb, scatter, or reflect UV radiation and visible light.
SPF???
Estrogen replacement
Skin phototypes:
Type
Characteristic
Examples
I
Always burns easily, never tans
Celtic or Irish extraction; often blue eyes, red hair, freckles
II
Burns easily, tans slightly
Fair-skinned individuals; often have blond hair; many whites
III
Sometimes burns, then tans gradually and moderately
Mediterraneans and some Hispanics
IV
Burns minimally, always tans well
Darker Hispanics and Asians
V
Burns rarely, tans deeply
Middle Easterners, Asians, some blacks
VI
Almost never burns, deeply pigmented
Some blacks
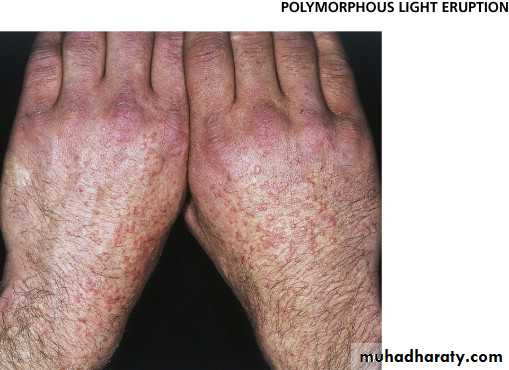
Polymorphous Light Eruption
Polymorphous light eruption (PLE) is the most common light-induced skin disease.
It is a long-standing, slowly ameliorating disease.
It is simply an itchy rash caused by sun exposure in people who have developed photosensitivity.
Starts in spring and early summer when a person’s exposure to the sun increases.
There are several morphologic subtypes, but individual patients tend to develop the same type each year.
The eruption appears first on limited areas but becomes more extensive during subsequent summers.
Most people with PLE have exacerbations each summer for many years; a few have temporary remissions.
The amount of light exposure needed to elicit an eruption varies greatly from one patient to another.
Most patients have symptoms 2 hours after exposure.
Light sensitivity decreases with repeated sun exposure; this phenomenon is referred to as hardening. Therefore, the eruption may cease to appear after days or weeks of repeated sun exposure.
Those exposed to sunlight all year rarely acquire PLE.
Women are affected more often than are men. The mean age at onset is 34 years (5 to 82 years).
The most common initial symptoms are burning, itching, and erythema.
The eruption usually lasts for 2 or 3 days, but in some cases it does not clear until the end of summer.
Many patients experience malaise, chills, headache, and nausea starting few hours after exposure but lasting only 1 or 2 hours.
The most commonly involved areas are the V of the chest (the area exposed by open-necked shirts), the backs of the hands, extensor aspects of the forearms, and the lower legs of women.
Lesions usually heal without scarring.
Many patients react to UVB, others to UVA, or some to both.
Plaque type
Is the second most common pattern.
Plaque type
Is the second most common pattern.
Papulovesicular type This type is less common. It occurs almost exclusively in women. Itching is common.
Papulovesicular type This type is less common. It occurs almost exclusively in women. Itching is common.
Papular type
The papular type is the most common form. Small papules are disseminated or densely aggregated on a patchy erythema.Papular type
The papular type is the most common form. Small papules are disseminated or densely aggregated on a patchy erythema.
Other types include:
Eczematous type: Erythema, papules, scale, and sometimes vesicles occur. It occurs almost exclusively in men.Erythema multiforme-like type.
Hemorrhagic type.
Treatment of PLE:
Patients can become disease free by using sunscreens and gradually increasing sun exposure in the spring. Phototherapy and photochemotherapy are most effective.Topical and oral steroids
Sun protection
Desensitization with phototherapy (UVB and/or UVA)
PUVA
Antimalarial drugs
Cyclosporine or azathioprine may be used for rare severe disabling cases.
Phototoxic Reactions
Phototoxicity occurs when a photosensitizer is absorbed into the skin either topically or systemically in appropriate concentrations and is exposed to adequate amounts of specific wavelengths of light, usually UVA.
There is a variety of topical and systemic agents like perfumes, plants {phytophotodermatitis} (eg., lime juice), and drugs (eg., antibacterials, NSAIDs, diuretics, retinoids, antifungals).
Feature
Phototoxic reactionPhotoallergic reaction
Incidence
High
Low
Amount of agent required
Large
Small
Onset of reaction
Minutes to hours
24-72 hours
More than one exposure to agent required
No
Yes
Distribution
Sun-exposed skin only
Sun-exposed skin; may spread to unexposed areas
Clinical characteristics
Resembles exaggerated sunburn or blisters
Dermatitis
Immunologically mediated
No
Yes; type IV