Neurosurgical investigations
Cerebrospinal fluid (CSF) examination
1. Spinal : lumber puncture LP aspirating CSF from lumbar cistern (L4-5/L3-4)
2. Cranial : lateral ventricular puncture
LP indicated in :
1. suspected meningitis
2. subarachnoid hemorrhage SAH
3. neurological diseases like Gullaine Barre Syndrome GBS and multiple sclerosis MS
4. cytology in neoplastic diseases
5. measurement of intracranial pressure
6. therapeutic CSF aspiration (benign raised intracranial pressure)(pseudotumor cerebri).
7. contrast injection in conventional myelography
8. intraspinal injection of anesthetic drugs in spinal anesthesia
LP is contraindicated in
1. raised intracranial pressure other than pseudotumor cerebri . e.g. brain tumors ,
obstructive hydrocephalus and brain abscess and cyst. Features suggestive include focal
neurological deficit and recent seizure and papilloedema.
2. Local sepsis at the site of LP
3. Bleeding tendency
4. Abnormal respiration i.e. moribund patient
5. Vertebral deformities ( kyphosis and scoliosis ).
Complications of LP
Post spinal headache with nausea is the most common complication; it often
responds to analgesics and infusion of fluids and maintaining supine posture
Cerebellar tonsillar herniation if there is raised ICP.
Injury to the neural structure
Back pain
Local infection and meningitis
Implantation of cutaneous tissue with subsequent epidermoid cyst
Bleeding
Imaging Studies
Skull x-ray may reveal
it can reveal
Skull fractures
Hyper stosis as in meningioma
Bone erusion tumors
Abnormal calcification as in meningioma , craniopharyngioma and calcified cyst or
aneurysm
Lateral displacement of calcified pineal body by a neoplasm
Features of long standing raised ICP
Erusion of the sella torcica clinoids
Double floor sella torsica
Beaten copper appearance
Suture diastasis
Spinal x-ray
1. Vertebral alignment.
2. Presence of degenerative disease with narrowing of the neural foramina and spinal
canal.
3. Evidence of metastatic tumor with erosion or sclerosis of the vertebra
4. Enlargement of a neural foramen indicating a spinal schwannoma.
5. Congenital abnormalities such as spina bifida.
Computerised tomography CT scanning
Non invasive test , useful in evaluating patient with head injury and stroke
Contrast study can be used but it carry risk of pain, nausea, thermal sensation, bronchospasm
and anaphylaxis.
So useful in stroke because it clearly differentiate hemorrhage from ischemia, also in head
injuries by showing fractures , hematomas and brain oedema and pathology.
in cases of brain neoplasm can identify it with its surrounding oedema and associated midline
shift and whether solid or cystic and if any associated hydrocephalus or brain abscess
Magnetic resonance imaging (MRI)
The patient lies within a magnetic field that aligns some protons along with magnetic axis. The
protons resonate when stimulated with radiofrequency energy producing strong echo enough to
be detected and recorded .the signal intensity depend on concentration of mobile hydrogen nuclei
of the tissue. In comparison to CT,
MRI is better for evaluating posterior fossa and lesions of multiple sclerosis
it is free from bone artifact with primary multi plane imaging ( axial, sagittal and
coronal)
High resolution for spinal cord together with non invasive MR myelography.
It involve no radiation so it can be repeated as necessary
Can detect ischemic areas few hours from the onset unlike CT that may require 48 hr
Contraindications include
1. Metalic foreign bodies e.g. Intracranial clips, cochlear implants, pace maker…etc
2. Claustrophobia
3. Gross obesity
4. Uncontrolled movement, Parkinsonism
5. Respiratory diseases RDS requiring ventilation or carry risk of apnea
Indications for Magnetic Resonance Imaging are:
1. IntracranialSOL .like Glioma and Meningioma and Hydatid cyst
2. CNS infection—cerebral abscess
3. Arteriovenous malformations.AVM
4. Venous sinus thrombosis.
5. Craniospinal abnormalities such as the Chiari malformation.
6. Syringomyelia.
7. Spinal tumours.
8. Disc prolapse (including cervical, lumbar and dorsal disc prolapse).
9. Spinal canal stenosis (lumbar or cervical stenosis) and cervical myelopathy.
Cerebral and spinal angiography

images of blood vessels in and around the brain,
AVM
and aneurysms.
Myelography
1.
Conventional myelography(invasive)
2.
CT myelography(invasive)
3.
MR myelography (non invasive)
Positron emission tomography PET
(PET) scan is an imaging test that can map tissue biochemistry and physiology.
The most commonly used PET tracer being a labeled form of glucose ( Fludeoxyglucose
(18F) (FDG). Useful in differentiating ischemic from neoplastic areas.
MR spectroscopy
(MRS) is a non-invasive, ionizing radiation free analytical technique used to study metabolic
changes in brain tumors, strokes, seizure disorders.
MR tractography
Visual representation of neural tracts
Neurophysiological studies
1) Electroencephalography (EEG)
records the spontaneous electrical activity of the brain through scalp electrodes
The main indication
Diagnosis and follow up of epileptic patients
To differentiate
psychogenic non-epileptic seizures
to localize the region of brain from which a seizure originates for work-up of
possible seizure surgery
waves pattern :
1. delta wave: is the frequency range up to 4 Hz.It is seen normally in adults in
. It is also seen normally in babies.
2.
is the frequency range from 4-7 Hz. Theta is seen normally in young
3.
-
14 Hz. It emerges with closing of the eyes
and with relaxation, and attenuates with eye opening or mental exertion.
Alpha can be abnormal; for example, an EEG that has diffuse alpha occurring in
coma and is not responsive to external stimuli is referred to as "alpha coma"
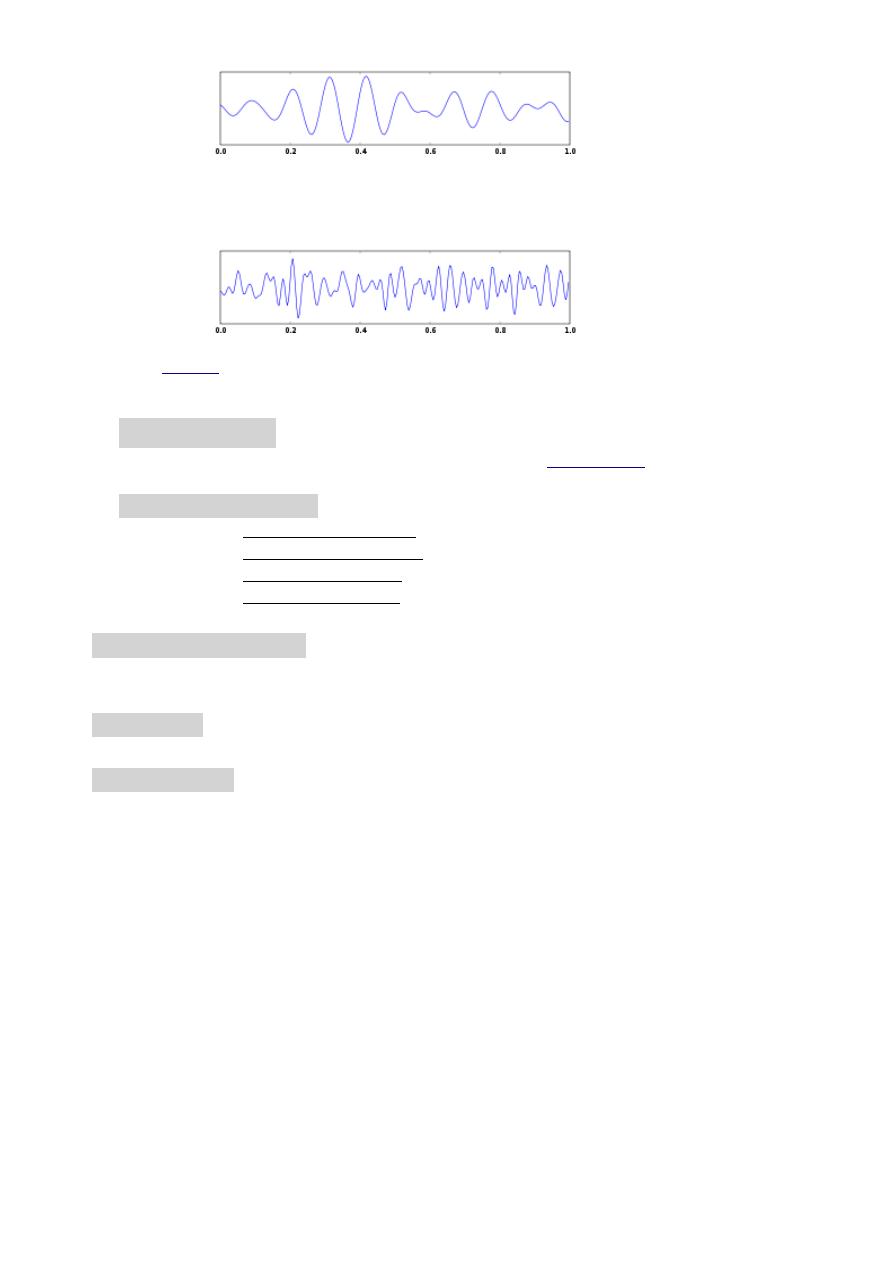
4. Beta wave is the frequency range from 15-30 Hz. It may be absent or reduced in
areas of cortical damage. It is the dominant rhythm in patients who are alert or
anxious or who have their eyes open
5.
is the frequency range approximately 30–100 Hz. It is seen in persons
carrying out a certain cognitive or motor function.
2)
Electromyography
a technique for evaluating and recording the electrical activity produced by
3) Nerve conduction study
Muscle and nerve biopsy
Muscle biopsy , is useful to determine whether the weakness is neorogenic or myogenic in origin
Brain biopsy
Hormonal assay
i.e. pituitary hormones like Prolactine, GH, FSH, LH, ACTH …. etc
