LEC:4
E.N.Tد. عماد ناظم الكواز
Management of Stridor
Definition and AetiologyHistory
History may have to be obtained from anxious parents.
Time and mode of onset: Wheather congenital or acquired. Sudden stridor as in foreign body inhalation whereas gradual stridor refers to laryngomalacia or haemangioma.
Associated symptoms: Hoarseness of voice, dysphagia, cough and apnea.
Relation to feeding: Aspiration indicates laryngeal paralysis or oesophageal atresia.
Cyanosis: Indicates need for airway maintenance.
Laryngeal injuries: Blunt or intubation injury.
Other diseases: Neurological, GERD or corrective cardiac surgery.
Examination
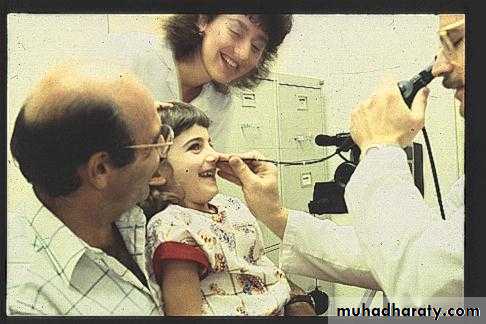
Let parent to hold child
Full ENT examination including fibroptic endoscopy.
Severity: Intercostal recession and use of accessory muscles of respiration.
Phase: Wheather inspiratory, expiratory or both.
Cyanosis: is a late sign.
Fever.
Drooling.
Auscultation over nose, open mouth, neck and chest helps to localize the probable site.
Position: Stridor of laryngomalacia, macroglossia and micrognathia disappears when baby lies in prone position.
Assess urgency: Is there acute distress?
Nasal flaring
Tachypnea
Cyanosis
Retractions
Tripod position
Investigations
X.ray of soft tissue of neck and chest.
CT scan and MRI.
ECG to exclude any cardiac problem.
Endoscopy
Flexible nasopharyngoscope: Gold standard of office evaluation. It is dynamic assessment, easy to do, minimal morbidity and well tolerated.
Rigid bronchoscopy, laryngoscopy and oesophagoscopy: Is the gold standard for diagnosis and treatment can be done at same session as foreign body removal . After slow induction rigid bronchoscopy is done first followed by intubation. This is followed by rigid direct laryngoscopy and oesophagoscopy.
Treatment
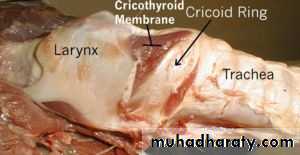
Treatment of cause. Tracheostomy, cricothyroidotomy and intubation may be required.Surgical anatomy of the trachea
Is a fibromuscular tube supported by 20 hyaline cartilages which are opened posteriorly. The soft tissue posterior wall is in contact with the oesophagus. About 7-8 cartilaginous rings constitute the cervical portion. Neck extension draws more rings to the cervical portionThe blood supply is primarily supported by the bracheocephalic artery and through the inferior thyroid and bronchial arteries.
The nerve supply is by parasympathetic and sympathetic fibres.The sympathetic system causes an increase in heart rate and relaxes the bronchi and muscle of the gut wall.The parasympathetic supply to the trachea is by the recurrent laryngeal nerve – a branch of the vagus nerve – it can slow the heart rate, increase the acidity to the stomach and constrict the bronchi.
Position
The trachea begins just below the larynx at approximately the 6th cervical vertebra. It is flexible to accommodate varying depths of ventilation, coughing and speech. The trachea is more superficial at its upper end, it became deeper as it passes downward and backward so that at the manuberum it is one inch from surface.
The length and width is continually changing to accommodate head, neck and diaphragmatic movements. In adults it is 12-16 cm long and 13-16 mm wide in women and 16-20 mm wide in men. It is slightly to the right of the midline and divides at the carina into the right and left bronchi. The carina lies under the junction of the sternum at the level of the 4th thoracic vertebra.
MANAGEMENT OF THE OBSTRUCTED AIRWAY
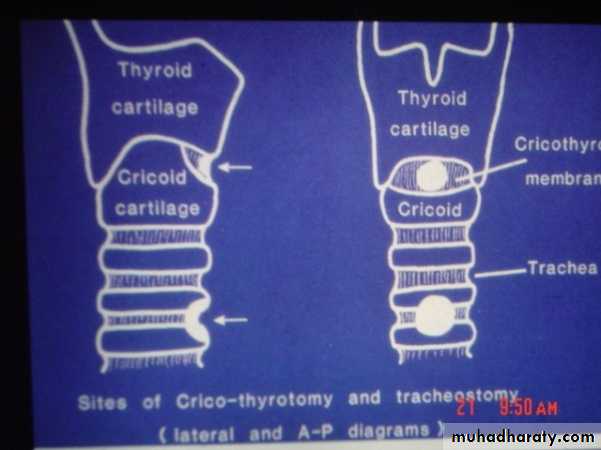
I. Laryngotomy (Cricothyroidotomy)
An opening through the cricothyroid membrane.
Indications
Sudden laryngeal obstruction when intubation is impossible and facilitates for tracheostomy is not available.
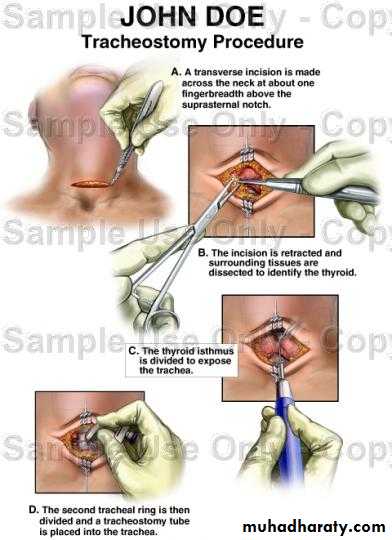
Technique
It is performed without anaesthesia by transverse incision to open the cricothyroid membrane. An elective tracheostomy is performed within a few hours if the obstruction is still present.
Complications
Haemorrhage.
Surgical emphysema.
Subglottic stenosis.
II.Tracheostomy
The creation of surgical opening into the trachea and converting it into a stoma on the skin surface.
Types
Emergency tracheostomy: Its usually done under local anaesthesia in conditions such as acute respiratory failure, or large laryngeal tumour presenting with stridor.
Elective temporary tracheostomy: This is performed as planned procedure, usually under GA as in management of upper airway obstruction, recoverable coma or inflammatory lesions such as acute epiglottitis.
Permanent tracheostomy: The trachea is brought to the surface as a permanent mouth to the respiratory tract as following laryngectomy.
Indications
I. Emergency
Relief of upper respiratory obstruction.
Congenital: Subglottic stenosis.
Inflammatory lesions: Ludwig,s angina, acute epiglottitis and acute laryngotracheobronchitis.
Laryngeal tumours.
Impacted F.B.
Trauma: External injury iatrogenic by endoscopy.
Bilateral abductor paralysis.
Signs of upper airway obstruction
Accessory Muscle use
Pallor, diaphoresis, restlessness
Tachycardia
Cyanosis and altered concious state
Intercostal recession
Nasal Flaring
Exhaustion
Bradycardia – most dangerous sign
2. Respiratory insufficiency: severe head and chest injuries, drug intoxication. Here, tracheostomy aids respiration by:
a-Reduction of the dead space by 50%.
b-Reducing resistance to airflow.
c. The ability to use mechanical ventilator.
3. Respiratory difficulty due to secretions (bronchial toilet): coma, CVA and neurological lesions (cervical cord lesions, tetanus and mysthenia gravis).
II. Elective: in cases of major head and neck surgery to maintain the airway and to protect it against haemorrhage.
Tracheostomy Tubes
Metal tubes
More traumatic.
Reusable, last many years (Permanent tracheostomy).
Have inner and outer tube for easy cleansing.
Not used with MRI and DXT.
Has no cuff so cannot be used with mechanical ventilator and does not prevent aspiration.
Portex tubes
Less traumatic.
For temporal procedures as it has a cuff which allows ventilation and prevents aspiration.
Cleansing is more difficult.
Can be used with MRI and DXT.
High cuff pressure can be damaging
Postoperative Management
Nursing: constant attention is essential for the first 24 hours. The patient should have a paper to write and a bell to get assistance.
Care of the tube:
The inner tube should be removed regularly and cleaned whenever it is blocked by secretions. Outer tube unless ,blocked or displaced, should not be removed for 3-4 days to allow a tract to be formed.
It is essential not to tie the tube too tight and not to tie the knot in a bow. The safest way is to stitch it to the skin with a silk.
If cuffed tube is used, it should be periodically deflated to prevent pressure necrosis of the trachea.
Suction of secretions: excessive secretions occur after the operation, since the trachea is exposed to cold dry air and the tube acts as a F.B. stimulating secretions.
Humdification: by instilling normal saline down to the tracheostomy tube or by using a moistened gauze over the tube.
5. Decanulation: difficult decanulation can occur in children if the tracheostomy has been present for a long time. For this a small cork should be used to fill a progressive area of the tube each day until the patient is able to breathe through the mouth.
Complications
Haemorrhage: occurs if haemostasis is not secured or ulceration of a major blood vessel by the tip of the tracheostomy tube if it is passed anterior to the tracheal opening or a tube with a wrong curvature.Aprea: a result from sudden discharge of CO2 and the obstruction has been bypassed. It is managed by allowing the patient to breath a mixture of 95% O2 and 5% CO2.
3. Displacement of the tracheostomy tube caused by:
Thick neck.
Short tracheostomy tube.
Postoperative oedema and haemorrhage causing broadening of the distance between the skin surface and the anterior tracheal wall.
4. Obstruction of the tracheostomy tube: this occurs if there is lack of humidification or poor toilet. It is treated by changing the tube.
5. Surgical emphysema:
Too tight suturing of the wound.
Small tracheostomy tube.
Patient on positive pressure ventilation.
6. Pneumothorax: Due to injury to apical pleura. It is common in children and in low tracheostomy procedures.
7. Infection: wound
Chest
8. Subglottic stenois: especially if the cricoid cartilage is injured.
III. Intubation versus tracheostomy.
Intubation
TracheostomyTime
Nursing
Quick procedure
Needs specialized I.C.U because the risk of obstruction and dislodgment
Takes longer time
Less specialized facilities
Talking and coughing
Impossible
Possible by closing the tube
Feeding
By NGT
Normal
Sedation
Necessary
Not necessary
Complications
a. Pneumothorax and surgical emphysema
–
+
b. Scar
–
+
c. Dislodgment
Dangerous
Less dangerous
d. Obstruction
Common
Less
The old adage states that “the time to do a tracheotomy is the time you first think of it”. The newer adage might be: “when you think of doing a tracheostomy, intubate and think again”.